An Innovative Application of High-Fidelity Medical Simulators to Objectively Demonstrate the Impact of Sports on the Development of Fine Motor Skills—A Pilot Study
Abstract
Highlights
- High-fidelity medical simulators with basic training modules can give useful feedback for fine motor skill development.
- Table tennis has been identified as a sport that can be used to maintain or improve arthroscopy and develop moderate catheter manipulation skills on simulators.
- Table tennis could improve fine motor skills that are important in good performance on high-fidelity medical simulators to prepare for the clinical practice.
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. The Table Tennis Program
2.3. Skill Assessment on Simulators
2.3.1. Vascular Catheter Simulator Exercise
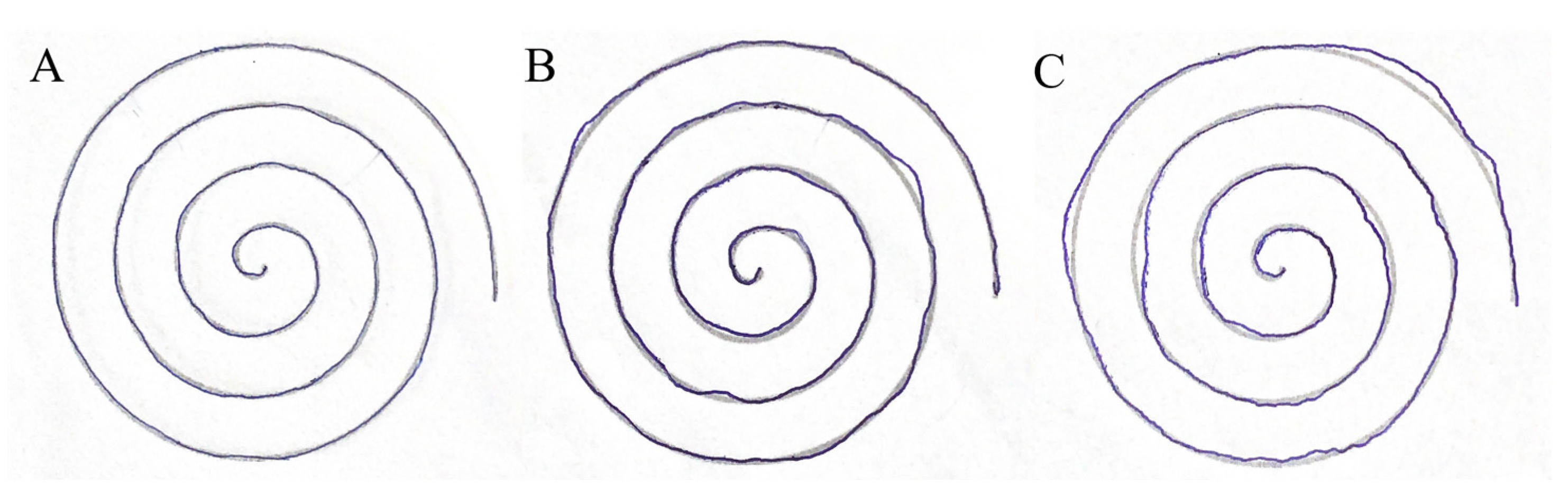
2.3.2. Arthroscopy Simulator Exercise
2.4. Statistical Analysis
3. Results
3.1. Evaluation of the Questionnaire
3.2. Skill Assessment on Vascular Catheterization Simulator
3.3. Skill Assessment on Arthroscopy Simulator
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beattie, K.L.; Hill, A.; Horswill, M.S.; Grove, P.M.; Stevenson, A.R.L. Aptitude and Attitude: Predictors of Performance during and after Basic Laparoscopic Skills Training. Surg. Endosc. 2022, 36, 3467–3479. [Google Scholar] [CrossRef] [PubMed]
- Fargen, K.M.; Turner, R.D.; Spiotta, A.M. Factors That Affect Physiologic Tremor and Dexterity During Surgery: A Primer for Neurosurgeons. World Neurosurg. 2016, 86, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Birkmeyer, J.D.; Finks, J.F.; O’Reilly, A.; Oerline, M.; Carlin, A.M.; Nunn, A.R.; Dimick, J.; Banerjee, M.; Birkmeyer, N.J.O. Surgical Skill and Complication Rates after Bariatric Surgery. N. Engl. J. Med. 2013, 369, 1434–1442. [Google Scholar] [CrossRef]
- Choi, Y.; Kim, Z.; Hur, K. Learning Curve for Laparoscopic Totally Extraperitoneal Repair of Inguinal Hernia. Can. J. Surg. 2012, 55, 33–36. [Google Scholar] [CrossRef]
- Treuting, R. Minimally Invasive Orthopedic Surgery: Arthroscopy. Ochsner J. 2000, 2, 158–163. [Google Scholar]
- Ahn, J.-M.; Park, D.-W.; Lee, C.W.; Chang, M.; Cavalcante, R.; Sotomi, Y.; Onuma, Y.; Tenekecioglu, E.; Han, M.; Lee, P.H.; et al. Comparison of Stenting Versus Bypass Surgery According to the Completeness of Revascularization in Severe Coronary Artery Disease: Patient-Level Pooled Analysis of the SYNTAX, PRECOMBAT, and BEST Trials. JACC Cardiovasc. Interv. 2017, 10, 1415–1424. [Google Scholar] [CrossRef] [PubMed]
- DeNiese, P.; Bhatia, D.N. Recent advances and future trends in shoulder arthroscopy. J. Arthrosc. Surg. Sports Med. 2020, 1, 16–22. [Google Scholar] [CrossRef]
- Mohammad, M.A.; Persson, J.; Buccheri, S.; Odenstedt, J.; Sarno, G.; Angerås, O.; Völz, S.; Tödt, T.; Götberg, M.; Isma, N.; et al. Trends in Clinical Practice and Outcomes After Percutaneous Coronary Intervention of Unprotected Left Main Coronary Artery. J. Am. Heart Assoc. 2022, 11, e024040. [Google Scholar] [CrossRef]
- Fan, Y.; Xu, L.; Liu, S.; Li, J.; Xia, J.; Qin, X.; Li, Y.; Gao, T.; Tang, X. The State-of-the-Art and Perspectives of Laser Ablation for Tumor Treatment. Cyborg Bionic Syst. 2024, 5, 0062. [Google Scholar] [CrossRef]
- Li, Z.; Xu, Q. Multi-Section Magnetic Soft Robot with Multirobot Navigation System for Vasculature Intervention. Cyborg Bionic Syst. 2024, 5, 0188. [Google Scholar] [CrossRef]
- Huri, G.; Popescu, I.A.; Rinaldi, V.G.; Marcheggiani Muccioli, G.M. The Evolution of Arthroscopic Shoulder Surgery: Current Trends and Future Perspectives. J. Clin. Med. 2025, 14, 2405. [Google Scholar] [CrossRef]
- Uttal, D.H.; Meadow, N.G.; Tipton, E.; Hand, L.L.; Alden, A.R.; Warren, C.; Newcombe, N.S. The Malleability of Spatial Skills: A Meta-Analysis of Training Studies. Psychol. Bull. 2013, 139, 352–402. [Google Scholar] [CrossRef] [PubMed]
- Chandra, S.; Hayashibe, M.; Thondiyath, A. Dominant Component in Muscle Fatigue Induced Hand Tremor during Laparoscopic Surgical Manipulation. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; pp. 6539–6542. [Google Scholar]
- Ahlborg, L.; Hedman, L.; Murkes, D.; Westman, B.; Kjellin, A.; Felländer-Tsai, L.; Enochsson, L. Visuospatial Ability Correlates with Performance in Simulated Gynecological Laparoscopy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 157, 73–77. [Google Scholar] [CrossRef]
- Davis-Pollard, J.; Christensen, B.; Morgan, K.; Dea, M.; Link, K.; Nigh, A.; Zapata, I.; Carter, S. Assessing Contributing Factors to Fine Motor Skills in Preclinical Medical Students. Global Surg. Educ. 2023, 2, 29. [Google Scholar] [CrossRef]
- Gallagher, A.G.; Leonard, G.; Traynor, O.J. Role and Feasibility of Psychomotor and Dexterity Testing in Selection for Surgical Training. ANZ J. Surg. 2009, 79, 108–113. [Google Scholar] [CrossRef]
- Nemeth, N.; Miko, I.; Furka, I. Experiences with Basic Microsurgical Training Programs and Skill Assessment Methods at the University of Debrecen, Hungary. Acta Cir. Bras. 2018, 33, 842–852. [Google Scholar] [CrossRef]
- Hamstra, S.J.; Dubrowski, A. Effective Training and Assessment of Surgical Skills, and the Correlates of Performance. Surg. Innov. 2005, 12, 71–77. [Google Scholar] [CrossRef]
- Rajaratnam, V.; Abdul Rahman, N.; Dong, C.; Jia Hui Ng, H. Redefining Surgical Skill Acquisition. In Medical Education for the 21st Century; Firstenberg, M.S., Stawicki, S.P., Eds.; IntechOpen: London, UK, 2022; ISBN 978-1-83969-731-9. [Google Scholar]
- Moulton, C.-A.E.; Dubrowski, A.; Macrae, H.; Graham, B.; Grober, E.; Reznick, R. Teaching Surgical Skills: What Kind of Practice Makes Perfect?: A Randomized, Controlled Trial. Ann. Surg. 2006, 244, 400–409. [Google Scholar] [CrossRef] [PubMed]
- Kalore, N.V. Simulation in Arthroscopy Training: Where We Are at, Where We Are Going. Available online: https://www.aana.org/education/publications/inside-aana-e-newsletter/2021-e-newsletters/january-2021/simulation-in-arthroscopy-training-where-we-are-at-where-we-are-going/?WebsiteKey=10f6eed0-bcab-4019-8f57-18dad8aaf2d7 (accessed on 9 April 2025).
- Bogar, P.Z.; Toth, L.; Rendeki, S.; Matyus, L.; Nemeth, N.; Boros, M.; Nagy, B.; Nyitrai, M.; Maroti, P. Az Egészségügyi Szimulációs Oktatás Jelene És Jövője Magyarországon [The present and the future of medical simulation education in Hungary]. Orvosi Hetil. 2020, 161, 1078–1087. [Google Scholar] [CrossRef] [PubMed]
- Moglia, A.; Morelli, L.; Ferrari, V.; Ferrari, M.; Mosca, F.; Cuschieri, A. Distribution of Innate Psychomotor Skills Recognized as Important for Surgical Specialization in Unconditioned Medical Undergraduates. Surg. Endosc. 2018, 32, 4087–4095. [Google Scholar] [CrossRef]
- Kramp, K.H.; van Det, M.J.; Hoff, C.; Veeger, N.J.G.M.; ten Cate Hoedemaker, H.O.; Pierie, J.-P.E.N. The Predictive Value of Aptitude Assessment in Laparoscopic Surgery: A Meta-Analysis. Med. Educ. 2016, 50, 409–427. [Google Scholar] [CrossRef]
- Grantcharov, T.P.; Funch-Jensen, P. Can Everyone Achieve Proficiency with the Laparoscopic Technique? Learning Curve Patterns in Technical Skills Acquisition. Am. J. Surg. 2009, 197, 447–449. [Google Scholar] [CrossRef]
- Groenier, M.; Schraagen, J.M.C.; Miedema, H.A.T.; Broeders, I.A.J.M. The Role of Cognitive Abilities in Laparoscopic Simulator Training. Adv. Health Sci. Educ. 2014, 19, 203–217. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.-K.; Shin, H.-Y.; Kim, K.H.; Seo, J.H.; Chun, K.J.; Ryu, D.R.; Cho, B.-R. Vascular Access: The Alpha and Omega of Cardiovascular Intervention. J. Cardiovasc. Interv. 2023, 2, 170. [Google Scholar] [CrossRef]
- Lee, E.; Kirtane, A.J. Distal Embolisation in Acute Myocardial Infarction. Intervent. Cardiol. Rev. 2007, 2, 49–51. [Google Scholar] [CrossRef]
- Korzeniowski, P.; White, R.J.; Bello, F. VCSim3: A VR Simulator for Cardiovascular Interventions. Int. J. Comput. Assist. Radiol. Surg. 2018, 13, 135–149. [Google Scholar] [CrossRef] [PubMed]
- Dayal, R.; Faries, P.L.; Lin, S.C.; Bernheim, J.; Hollenbeck, S.; DeRubertis, B.; Trocciola, S.; Rhee, J.; McKinsey, J.; Morrissey, N.J.; et al. Computer Simulation as a Component of Catheter-Based Training. J. Vasc. Surg. 2004, 40, 1112–1117. [Google Scholar] [CrossRef]
- Joshi, A.; Wragg, A. Simulator Training in Interventional Cardiology. Intervent. Cardiol. Rev. 2016, 11, 70. [Google Scholar] [CrossRef]
- Anetzberger, H.; Reppenhagen, S.; Eickhoff, H.; Seibert, F.J.; Döring, B.; Haasters, F.; Mohr, M.; Becker, R. Ten Hours of Simulator Training in Arthroscopy Are Insufficient to Reach the Target Level Based on the Diagnostic Arthroscopic Skill Score. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1471–1479. [Google Scholar] [CrossRef]
- Jafar, M.; Rinaldy, A.; Yunus, M. Improving Student Motor Skills through a Structured Physical Training Program. J. Adv. Sport Phys. Edu. 2023, 6, 82–95. [Google Scholar] [CrossRef]
- Zarei, H.; Norasteh, A.A.; Dehghani, N.; Lieberman, L.J.; Ertel, M.W.; Brian, A. Effects of Exercise Training Programs on Motor Skills of Individuals with Intellectual Disabilities: A Systematic Review and Meta-Analysis. Disabil. Rehabil. 2024, 46, 6001–6010. [Google Scholar] [CrossRef]
- Chadwick, S. How Damaging Is an Adidas Decision to Pull Its Athletics Sponsorship? Available online: https://theconversation.com/how-damaging-is-an-adidas-decision-to-pull-its-athletics-sponsorship-53689 (accessed on 9 April 2025).
- Johnson, S.R.; Wojnar, P.J.; Price, W.J.; Foley, T.J.; Moon, J.R.; Esposito, E.N.; Cromartie, F.J. A coach’s responsibility: Learning how to prepare athletes for peak performance. Sport J. 2011, 14, 1–11. [Google Scholar]
- Ruwe, P.A.; Wright, J.; Randall, R.L.; Lynch, J.K.; Jokl, P.; McCarthy, S. Can MR Imaging Effectively Replace Diagnostic Arthroscopy? Radiology 1992, 183, 335–339. [Google Scholar] [CrossRef]
- Pérez Ayme, A.P.; Caiza Suárez, J.M.; Paredes Ortega, M.M.; Gualoto Gualoto, G.G.; Santillán Lima, S.L.; Rivera Campoverde, A.E.; Rivera Ticona, A.A.; Coello Vergara, C.V.; Martínez Serrano, G.D. Advancements in Minimally Invasive Surgical Techniques: A Comprehensive Review. Salud Cienc. Tecnol. 2024, 3, 745. [Google Scholar] [CrossRef]
- Gu, Y.; Chen, Y.; Ma, J.; Ren, Z.; Li, H.; Kim, H. The Influence of a Table Tennis Physical Activity Program on the Gross Motor Development of Chinese Preschoolers of Different Sexes. Int. J. Environ. Res. Public Health 2021, 18, 2627. [Google Scholar] [CrossRef]
- Gasparini, G.L.; Bongiovanni, D. The vessel is dissected and I cannot wire it! Card. Interv. Today 2021, 15, 31–33. [Google Scholar]
- Sun, Z. Coronary CT Angiography with Prospective ECG-Triggering: An Effective Alternative to Invasive Coronary Angiography. Cardiovasc. Diagn. Ther. 2012, 2, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Catapano, F.; Moser, L.J.; Francone, M.; Catalano, C.; Vliegenthart, R.; Budde, R.P.J.; Salgado, R.; Hrabak Paar, M.; Pirnat, M.; Loewe, C.; et al. Competence of Radiologists in Cardiac CT and MR Imaging in Europe: Insights from the ESCR Registry. Eur. Radiol. 2024, 34, 5666–5677. [Google Scholar] [CrossRef]
- Carr, A.J.; Price, A.J.; Glyn-Jones, S.; Rees, J.L. Advances in Arthroscopy-Indications and Therapeutic Applications. Nat. Rev. Rheumatol. 2015, 11, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Tajti, P.; Brilakis, E.S. Medical Simulation in Interventional Cardiology: “More Research Is Needed”. Cathet. Cardiol. Intervent. 2018, 91, 1060–1061. [Google Scholar] [CrossRef] [PubMed]
- Sun, R.R.; Wang, Y.; Fast, A.; Dutka, C.; Cadogan, K.; Burton, L.; Kubay, C.; Drachenberg, D. Influence of musical background on surgical skills acquisition. Surgery 2021, 170, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Comeau, G.; Chen, K.J.; Swirp, M.; Russell, D.; Chen, Y.; Gawad, N.; Jabagi, H.; Tran, A.; Balaa, F. From Music to Medicine: Are Pianists at an Advantage When Learning Surgical Skills? Music Med. 2020, 12, 6–18. [Google Scholar] [CrossRef]
- Rui, M.; Lee, J.E.; Vauthey, J.N.; Conrad, C. Enhancing surgical performance by adopting expert musicians’ practice and performance strategies. Surgery 2018, 163, 894–900. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Lei, Y.; Li, X.; Li, N.; Si, X.; Chen, C. A dynamic barycenter bridging network for federated transfer fault diagnosis in machine groups. Mech. Syst. Signal Proc. 2025, 230, 112605. [Google Scholar] [CrossRef]




| Control Group (n = 13) | Table Tennis Group (n = 13) | |||
|---|---|---|---|---|
| First survey | Second survey | First survey | Second survey | |
| Male/Female | 11/2 | 11/2 | ||
| Age | 22 ± 1 years | 22 ± 2 years | ||
| BMI value | 23.19 ± 2.34 | 22.89 ± 2.3 | 24.4 ± 4.48 | 23.47 ± 3.18 |
| Right-handed/Left-handed | 12/1 | 9/4 | ||
| Control Group (n = 13) | Table Tennis Group (n = 13) | |||
|---|---|---|---|---|
| First Survey (s) | Second Survey (s) | First Survey (s) | Second Survey (s) | |
| Aortic root | 11.29 ± 3.27 | 19.31 ± 7.5 * | 14.38 ± 6.27 | 13.47 ± 5.9 # |
| Left main | 55 ± 21.64 | 95.54 ± 21.7 * | 68 ± 28.16 | 87.4 ± 38.84 |
| Left circumflex | 183.93 ± 58.67 | 213.31 ± 55.43 | 176 ± 58.25 | 186.67 ± 57.54 |
| Left anterior descendent | 204.14 ± 68.75 | 244.92 ± 99.51 | 188.94 ± 52.39 | 193.53 ± 59.54 |
| Right coronary artery | 407.5 ± 82.81 | 453.38 ± 107.69 | 382.12 ± 90.38 | 373.13 ± 86.17 # |
| Distal right coronary artery | 442.43 ± 93.85 | 480 ± 106.87 | 408.19 ± 88.42 | 405.33 ± 83.51 # |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szikra, P.; Matrai, A.A.; Varga, A.; Balogh, L.; Karacsonyi, Z.; Okros, K.; Horovitz, T.; Toth, M.; Nemeth, N. An Innovative Application of High-Fidelity Medical Simulators to Objectively Demonstrate the Impact of Sports on the Development of Fine Motor Skills—A Pilot Study. Sensors 2025, 25, 5316. https://doi.org/10.3390/s25175316
Szikra P, Matrai AA, Varga A, Balogh L, Karacsonyi Z, Okros K, Horovitz T, Toth M, Nemeth N. An Innovative Application of High-Fidelity Medical Simulators to Objectively Demonstrate the Impact of Sports on the Development of Fine Motor Skills—A Pilot Study. Sensors. 2025; 25(17):5316. https://doi.org/10.3390/s25175316
Chicago/Turabian StyleSzikra, Peter, Adam Attila Matrai, Adam Varga, Laszlo Balogh, Zoltan Karacsonyi, Konrad Okros, Tamas Horovitz, Miklos Toth, and Norbert Nemeth. 2025. "An Innovative Application of High-Fidelity Medical Simulators to Objectively Demonstrate the Impact of Sports on the Development of Fine Motor Skills—A Pilot Study" Sensors 25, no. 17: 5316. https://doi.org/10.3390/s25175316
APA StyleSzikra, P., Matrai, A. A., Varga, A., Balogh, L., Karacsonyi, Z., Okros, K., Horovitz, T., Toth, M., & Nemeth, N. (2025). An Innovative Application of High-Fidelity Medical Simulators to Objectively Demonstrate the Impact of Sports on the Development of Fine Motor Skills—A Pilot Study. Sensors, 25(17), 5316. https://doi.org/10.3390/s25175316







