Biomechanical Effects of a Passive Lower-Limb Exoskeleton Designed for Half-Sitting Work Support on Walking
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Equipment
2.3. Experimental Conditions
2.4. Measurements
2.5. Data Analysis
2.5.1. Gait Parameters
2.5.2. Inverse Dynamics
2.5.3. Peak Moments
2.6. Statistics
3. Results
3.1. Gait Parameters
3.2. Contact Force and Moment
- The results of the contact force
- At the medio-lateral interface, the device initially pushed medially, then reversed direction, and rose steadily to a peak lateral force near mid-stance, before declining toward zero during late swing.
- At the anterior–posterior interface, a posterior-directed force emerged in early stance and reached a peak posterior force near mid-stance. The direction switched to anterior around three-quarters of the gait cycle, peaking just during terminal stance.
- At the vertical interface, downward loading dominated mid-stance, followed by an upward rebound during terminal stance.
- The medio-lateral trace showed a shallow biphasic pattern similar in shape to that at thigh but with about half the amplitude;
- Conversely, the anterior–posterior trace displayed an inverted profile, peaking anteriorly at mid-stance and remaining close to zero through terminal stance and swing;
- Vertical forces remained close to zero.
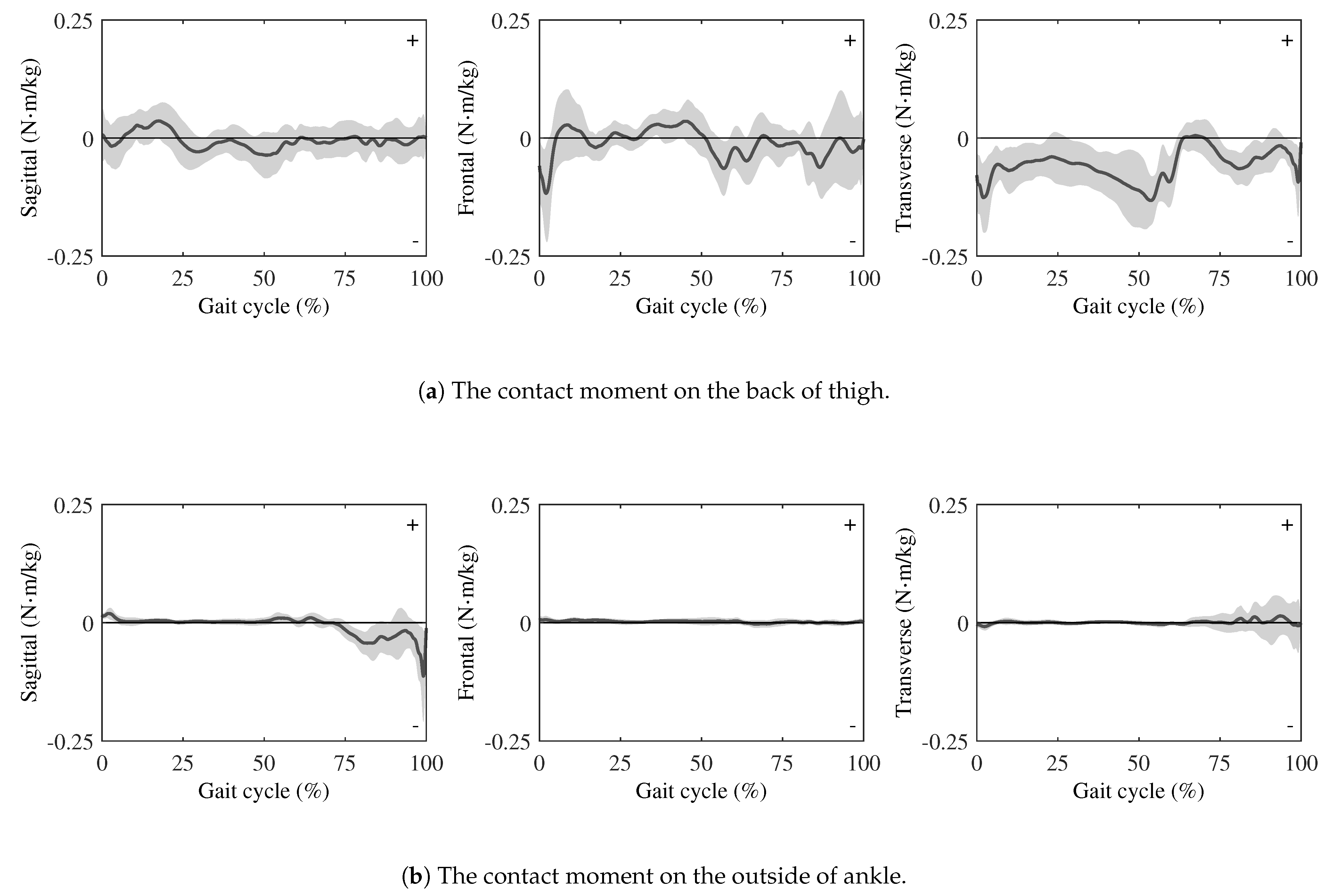
- The results of the contact moment
- In the sagittal plane, a brief negative deflection appeared just after heel strike, followed by a shallow positive peak. The curve then oscillated gently about zero during mid-stance and swing.
- In the frontal plane, a brief negative deflection was shown immediately after heel strike, followed by a small positive excursion in early stance. It then remained near zero with low-amplitude oscillations, exhibited a slight negative bias from mid-stance to terminal stance, and returned toward zero during swing.
- In the transverse plane, the component remained negative through most of stance, rose sharply around mid-stance and exhibited a brief positive excursion, then stayed slightly negative during terminal stance.
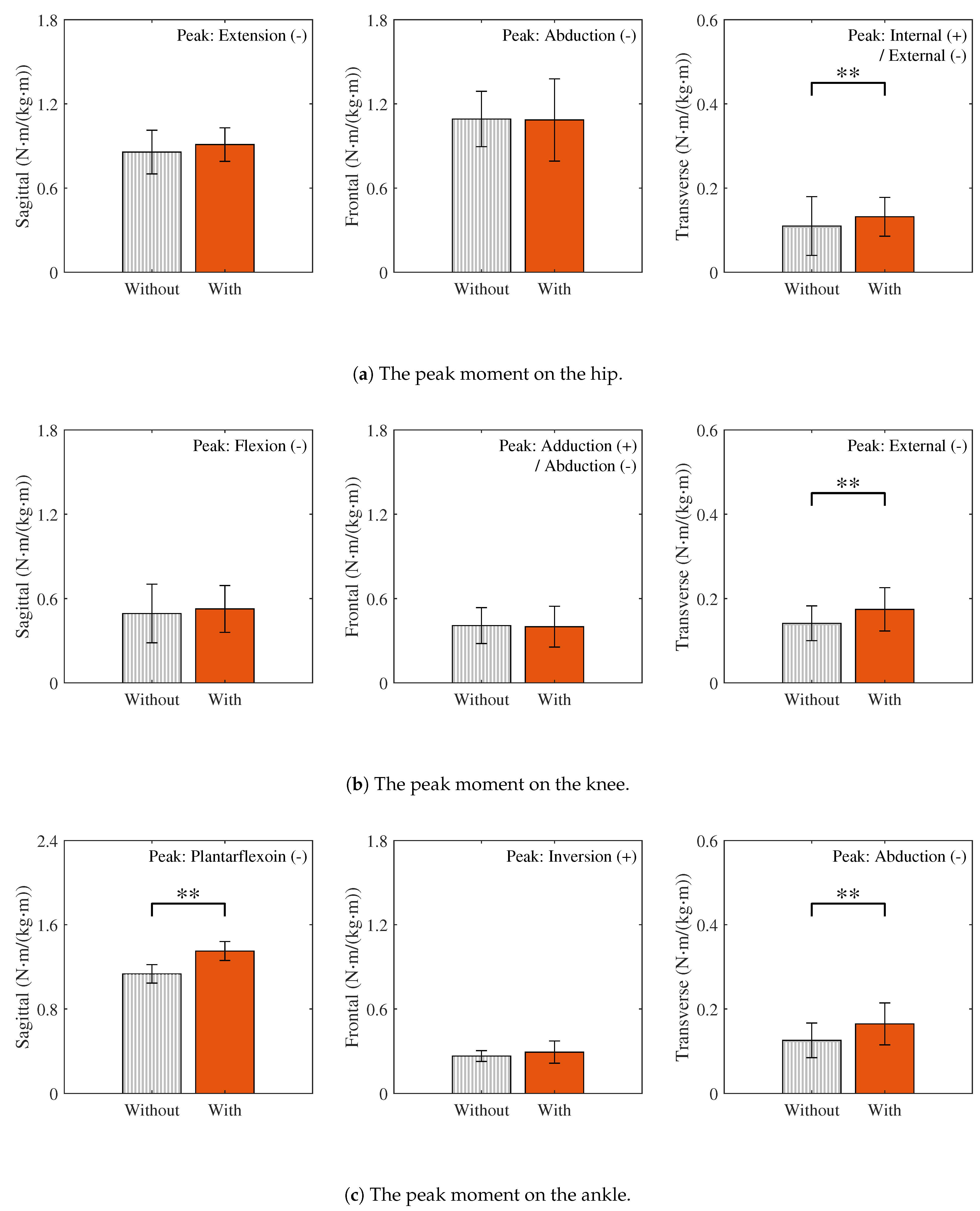
3.3. Joint Moments
- Sagittal plane: The hip flexion, knee extension, and ankle dorsiflexion moments, which are primarily responsible for sagittal plane kinetics, mainly represent the generation and absorption of forward propulsion. Among these, the peak moment at the ankle joint increased significantly with the wearable chair and exhibited a large effect size (). In contrast, no statistically significant increase was observed at the hip and knee joints. The corresponding effect sizes at these joints were small (hip: Cohen’s ; knee: Cohen’s ).
- Frontal plane: The hip adduction, knee adduction, and ankle inversion moments, which are primarily responsible for frontal plane kinetics, mainly represent control of lateral balance and support against gravity. Although the additional weight of the wearable chair was expected to increase the gravitational load and thus these peak moments, no statistically significant differences were observed between walking with and without the wearable chair. Moreover, the corresponding effect sizes were also small (hip: Cohen’s ; knee: Cohen’s ; ankle: ).
- Transverse plane: The hip internal rotation, knee internal rotation, and ankle adduction moments, which are primarily responsible for transverse plane kinetics, mainly represent the rotational control of the body. The peak moments at all these joints showed statistically significant increases with the wearable chair. Moreover, the corresponding effect sizes were also large (hip: ; knee: Cohen’s ; ankle: Cohen’s ).
4. Discussion
4.1. Reliability of Experimental Results
4.2. Evaluation of Wearable Chair Effects on Lower-Limb Joint Loads
4.3. Risks from Altered Joint Loads and Design Implications
4.4. Limitations and Future Work
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 3D | three-dimensional |
| DOF | degree of freedom |
| GRF | Ggound reaction force |
| ISB | International Society of Biomechanics |
| SD | standard deviation |
| CMC | coefficient of multiple correlation |
Appendix A. Transformation of External Forces and Moments
References
- Gell, N.; Werner, R.A.; Hartigan, A.; Wiggermann, N.; Keyserling, W.M. Risk factors for lower extremity fatigue among assembly plant workers. Am. J. Ind. Med. 2011, 54, 216–223. [Google Scholar] [CrossRef]
- Jin, X.; Dong, Y.; Wang, F.; Jiang, P.; Zhang, Z.; He, L.; Forsman, M.; Yang, L. Prevalence and associated factors of lower extremity musculoskeletal disorders among manufacturing workers: A cross-sectional study in China. BMJ Open 2022, 12, e054969. [Google Scholar] [CrossRef]
- Kong, Y.-K.; Park, C.-W.; Cho, M.-U.; Kim, S.-Y.; Kim, M.-J.; Hyun, D.J.; Bae, K.; Choi, J.K.; Ko, S.M.; Choi, K.-H. Guidelines for working heights of the lower-limb exoskeleton (CEX) based on ergonomic evaluations. Int. J. Environ. Res. Public Health 2021, 18, 5199. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.M.; TormaKrajewski, J.; Steiner, L.J. Practical Demonstrations of Ergonomic Principles; Report of Investigations 9684; DHHS (NIOSH) Publication No. 2011-191; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health: Pittsburgh, PA, USA, 2011. [Google Scholar]
- de Looze, M.P.; Bosch, T.; Krause, F.; Stadler, K.S.; O’Sullivan, L.W. Exoskeletons for industrial application and their potential effects on physical workload. Ergonomics 2015, 59, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Theurel, J.; Desbrosses, K. Occupational exoskeletons: Overview of their benefits and limitations in preventing work-related musculoskeletal disorders. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 264–280. [Google Scholar] [CrossRef]
- Ashta, G.; Finco, S.; Battini, D.; Persona, A. Passive exoskeletons to enhance workforce sustainability: Literature review and future research agenda. Sustainability 2023, 15, 7339. [Google Scholar] [CrossRef]
- Gonsalves, N.; Akanmu, A.; Shojaei, A.; Agee, P. Factors influencing the adoption of passive exoskeletons in the construction industry: Industry perspectives. Int. J. Ind. Ergon. 2024, 100, 103549. [Google Scholar] [CrossRef]
- Yan, Z.; Han, B.; Du, Z.; Huang, T.; Bai, O.; Peng, A. Development and testing of a wearable passive lower-limb support exoskeleton to support industrial workers. Biocybern. Biomed. Eng. 2021, 41, 221–238. [Google Scholar] [CrossRef]
- Haraguchi, N.; Hase, K. Biomechanical analysis based on a full-body musculoskeletal model for evaluating the effect of a passive lower-limb assistive device on lumbar load. J. Biomech. Sci. Eng. 2023, 18, 23-00024. [Google Scholar] [CrossRef]
- noonee AG. Chairless Chair—Wearable Posture Support Device. Available online: https://www.noonee.com/ (accessed on 7 July 2025).
- Li, L.; Chen, Z.; Hong, R.; Qu, Y.; Gao, X.; Wang, X. Research status and development trend of lower-limb squat-assistant wearable devices. Biomimetics 2025, 10, 258. [Google Scholar] [CrossRef]
- Luger, T.; Seibt, R.; Cobb, T.J.; Rieger, M.A.; Steinhilber, B. Influence of a passive lower-limb exoskeleton during simulated industrial work tasks on physical load, upper-body posture, postural control and discomfort. Appl. Ergon. 2019, 80, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Liang, X.; Li, L.; Gong, L.; Deng, L.; Hu, X.; Zhang, S.; Sun, S. Wearable chairless exoskeleton capable of flexible support to relieve muscle fatigue for industrial workers. Smart Mater. Struct. 2024, 33, 125041. [Google Scholar] [CrossRef]
- Baltrusch, S.J.; van Dieën, J.H.; van Bennekom, C.A.M.; Houdijk, H. The effect of a passive trunk exoskeleton on functional performance in healthy individuals. Appl. Ergon. 2018, 72, 94–106. [Google Scholar] [CrossRef]
- Steinhilber, B.; Seibt, R.; Rieger, M.A.; Luger, T. Postural control when using an industrial lower-limb exoskeleton: Impact of reaching for a working tool and external perturbation. Hum. Factors 2022, 64, 635–648. [Google Scholar] [CrossRef]
- Li, Y.Y.; Gan, J. Effect of wearable chair on gait, balance, and discomfort of new users during level walking with anterior loads. J. Saf. Res. 2023, 87, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Greggi, C.; Visconti, V.V.; Albanese, M.; Gasperini, B.; Chiavoghilefu, A.; Prezioso, C.; Persechino, B.; Iavicoli, S.; Gasbarra, E.; Iundusi, R.; et al. Work-related musculoskeletal disorders: A systematic review and meta-analysis. J. Clin. Med. 2024, 13, 3964. [Google Scholar] [CrossRef] [PubMed]
- Kim, U.; Lim, J.; Park, Y.; Bae, Y. Predicting fall risk through step width variability at increased gait speed in community-dwelling older adults. Sci. Rep. 2025, 15, 16915. [Google Scholar] [CrossRef]
- Davis, R.B., III; Ounpuu, S.; Tyburski, D.; Gage, J.R. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Winter, D.A. Biomechanics and Motor Control of Human Movement, 4th ed.; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Haraguchi, N.; Hase, K. Multibody model with foot-deformation approach for estimating ground reaction forces and moments and joint torques during level walking through optical motion capture without optimization techniques. Sensors 2024, 24, 2792. [Google Scholar] [CrossRef]
- Wang, S.; Pitts, J.; Purohit, R.; Shah, H. The influence of motion data low-pass filtering methods in machine-learning models. Appl. Sci. 2025, 15, 2177. [Google Scholar] [CrossRef]
- Horsak, B.; Slijepcevic, D.; Raberger, A.-M.; Schwab, C.; Worisch, M.; Zeppelzauer, M. GaitRec, a large-scale ground reaction force dataset of healthy and impaired gait. Sci. Data 2020, 7, 143. [Google Scholar] [CrossRef]
- Wang, S.; Cai, Y.; Hase, K.; Uchida, K.; Kondo, D.; Saito, T.; Ota, S. Estimation of knee joint angles during gait cycle using inertial measurement unit sensors: A method of sensors-to-clinical bone calibration on the lower-limb skeletal model. J. Biomech. Sci. Eng. 2022, 17, 21-00196. [Google Scholar] [CrossRef]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—Part I: Ankle, hip, and spine. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; van der Helm, F.C.T.; Veeger, H.E.J.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef]
- Derrick, T.R.; van den Bogert, A.J.; Cereatti, A.; Dumas, R.; Fantozzi, S.; Leardini, A. ISB recommendations on the reporting of intersegmental forces and moments during human motion analysis. J. Biomech. 2020, 99, 109533. [Google Scholar] [CrossRef]
- Hof, A.L. Scaling gait data to body size. Gait Posture 1996, 4, 222–223. [Google Scholar] [CrossRef]
- Teng, H.L.; Calixto, N.E.; MacLeod, T.D.; Nardo, L.; Link, T.M.; Majumdar, S.; Souza, R.B. Associations between patellofemoral-joint cartilage T1ρ and T2 and knee-flexion moment and impulse during gait in individuals with and without patellofemoral joint osteoarthritis. Osteoarthr. Cartil. 2016, 24, 1554–1564. [Google Scholar] [CrossRef]
- Gill, N.; O’Leary, T.; Roberts, A.; Liu, A.; Roerdink, M.; Greeves, J.; Jones, R. Enforcing walking speed and step-length affects joint kinematics and kinetics in male and female healthy adults. Gait Posture 2023, 103, 223–228. [Google Scholar] [CrossRef]
- van Hooren, B.; Hirsch, S.M.; Meijer, K. A comparison of five methods to normalize joint moments during running. Gait Posture 2023, 105, 81–86. [Google Scholar] [CrossRef]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E.; Gainey, J.; Gorton, G.; Cochran, G.V.B. Repeatability of kinematic, kinetic, and electromyographic data in normal adult gait. J. Orthop. Res. 1989, 7, 849–860. [Google Scholar] [CrossRef]
- Kazerooni, H.; Steger, R.; Huang, L. Hybrid control of the Berkeley lower extremity exoskeleton (BLEEX). Int. J. Robot. Res. 2006, 25, 561–573. [Google Scholar] [CrossRef]
- Duong, M.K.; Cheng, H.; Tran, H.T.; Jing, Q. Minimizing human-exoskeleton interaction force using compensation for dynamic uncertainty error with adaptive RBF network. J. Intell. Robot. Syst. 2016, 82, 413–433. [Google Scholar] [CrossRef]
- Sanchez-Villamañan, M.D.C.; Gonzalez-Vargas, J.; Torricelli, D.; Moreno, J.C.; Pons, J.L. Compliant lower limb exoskeletons: A comprehensive review on mechanical design principles. J. Neuroeng. Rehabil. 2019, 16, 55. [Google Scholar] [CrossRef]
- Winter, D.A. Energy generation and absorption at the ankle and knee during fast, natural, and slow cadences. Clin. Orthop. Relat. Res. 1983, 175, 147–154. [Google Scholar] [CrossRef]
- Neptune, R.R.; Kautz, S.A.; Zajac, F.E. Contributions of the individual ankle plantar flexors to support, forward progression and swing initiation during walking. J. Biomech. 2001, 34, 1387–1398. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.K. The effect of a vertical load on gluteus medius activity and gait characteristics during walking. J. Phys. Ther. Sci. 2013, 25, 1397–1399. [Google Scholar] [CrossRef][Green Version]
- Hwang, J.W.; Lee, S.K.; Park, J.S.; Ahn, S.H.; Lee, K.J.; Lee, S.J. The effects of ankle weight loading on the walking factors of adults without symptoms. J. Exerc. Rehabil. 2017, 13, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Bedi, A.; Warren, R.F.; Wojtys, E.M.; Oh, Y.K.; Ashton-Miller, J.A.; Oltean, H.; Kelly, B.T. Restriction in hip internal rotation is associated with an increased risk of ACL injury. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2024–2031. [Google Scholar] [CrossRef] [PubMed]
- Ye, B.; Liu, G.; He, Z.; Xu, J.; Pan, H.; Zhu, H. Biomechanical mechanisms of anterior cruciate ligament injury in the jerk dip phase of clean and jerk: A case study of an injury event captured on-site. Heliyon 2024, 10, e31390. [Google Scholar] [CrossRef]
- Fong, D.T.P.; Chan, Y.Y.; Mok, K.M.; Yung, P.S.; Chan, K.M. Understanding acute ankle ligamentous sprain injury in sports. BMC Sports Sci. Med. Rehabil. 2009, 1, 14. [Google Scholar] [CrossRef]
- Vap, A.R.; Schon, J.M.; Moatshe, G.; Cruz, R.S.; Brady, A.W.; Dornan, G.J.; Turnbull, T.L.; LaPrade, R.F. The role of the peripheral passive rotation stabilizers of the knee with intact collateral and cruciate ligaments: A biomechanical study. Orthop. J. Sports Med. 2017, 5, 2325967117708190. [Google Scholar] [CrossRef]
- Li, L.; Gollhofer, A.; Lohrer, H.; Dorn-Lange, N.; Bonsignore, G.; Gehring, D. Function of ankle ligaments for subtalar and talocrural joint stability during an inversion movement—An in vitro study. J. Foot Ankle Res. 2019, 12, 16. [Google Scholar] [CrossRef] [PubMed]
- Shin, C.S.; Chaudhari, A.M.; Andriacchi, T.P. The effect of isolated valgus moments on ACL strain during single-leg landing: A simulation study. J. Biomech. 2009, 42, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Breloff, S.P.; Dutta, A.; Dai, F.; Sinsel, E.W.; Warren, C.M.; Ning, X.; Wu, J.Z. Assessing work-related risk factors for musculoskeletal knee disorders in construction roofing tasks. Appl. Ergon. 2019, 81, 102901. [Google Scholar] [CrossRef] [PubMed]
- Brandl, C.; Bender, A.; Schmachtenberg, T.; Dymke, J.; Damm, P. Comparing risk assessment methods for work-related musculoskeletal disorders with in vivo joint loads during manual materials handling. Sci. Rep. 2024, 14, 6041. [Google Scholar] [CrossRef]
- Ghai, S.; Ghai, I. Virtual reality enhances gait in cerebral palsy: A training dose-response meta-analysis. Front. Neurol. 2019, 10, 236. [Google Scholar] [CrossRef]
- Ghai, S.; Ghai, I.; Lamontagne, A. Virtual reality training enhances gait poststroke: A systematic review and meta-analysis. Ann. N. Y. Acad. Sci. 2020, 1478, 18–42. [Google Scholar] [CrossRef]
- Ghai, S.; Ghai, I.; Schmitz, G.; Effenberg, A.O. Effect of rhythmic auditory cueing on parkinsonian gait: A systematic review and meta-analysis. Sci. Rep. 2018, 8, 506. [Google Scholar] [CrossRef]
- Koussou, A.; Desailly, E.; Dumas, R. Contribution of passive moments to inter-segmental moments during gait: A systematic review. J. Biomech. 2021, 122, 110450. [Google Scholar] [CrossRef]





| Without the Wearable Chair | With the Wearable Chair | |
|---|---|---|
| Gait cycle * (s) | ||
| Stride length ** (m) | ||
| Walking speed ** (m) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Q.; Haraguchi, N.; Yoshimura, B.; Wang, S.; Yoshida, M.; Hase, K. Biomechanical Effects of a Passive Lower-Limb Exoskeleton Designed for Half-Sitting Work Support on Walking. Sensors 2025, 25, 4999. https://doi.org/10.3390/s25164999
Li Q, Haraguchi N, Yoshimura B, Wang S, Yoshida M, Hase K. Biomechanical Effects of a Passive Lower-Limb Exoskeleton Designed for Half-Sitting Work Support on Walking. Sensors. 2025; 25(16):4999. https://doi.org/10.3390/s25164999
Chicago/Turabian StyleLi, Qian, Naoto Haraguchi, Bian Yoshimura, Sentong Wang, Makoto Yoshida, and Kazunori Hase. 2025. "Biomechanical Effects of a Passive Lower-Limb Exoskeleton Designed for Half-Sitting Work Support on Walking" Sensors 25, no. 16: 4999. https://doi.org/10.3390/s25164999
APA StyleLi, Q., Haraguchi, N., Yoshimura, B., Wang, S., Yoshida, M., & Hase, K. (2025). Biomechanical Effects of a Passive Lower-Limb Exoskeleton Designed for Half-Sitting Work Support on Walking. Sensors, 25(16), 4999. https://doi.org/10.3390/s25164999









