A State-of-the-Art of Exoskeletons in Line with the WHO’s Vision on Healthy Aging: From Rehabilitation of Intrinsic Capacities to Augmentation of Functional Abilities
Abstract
1. Background
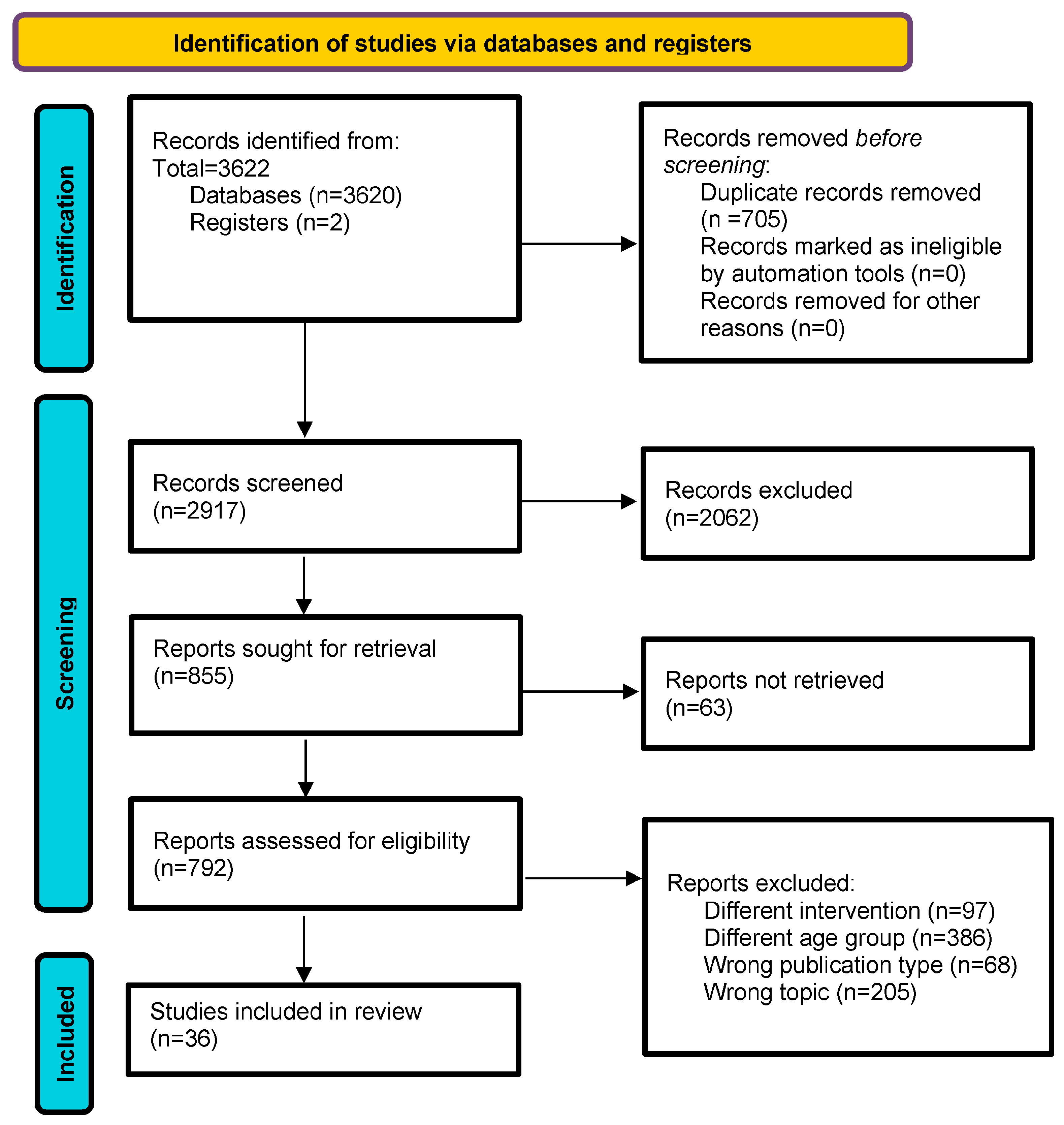
2. Methods
2.1. Study Registration
2.2. Search Strategy and Study Selection Criteria
2.3. Data Extraction and Analysis
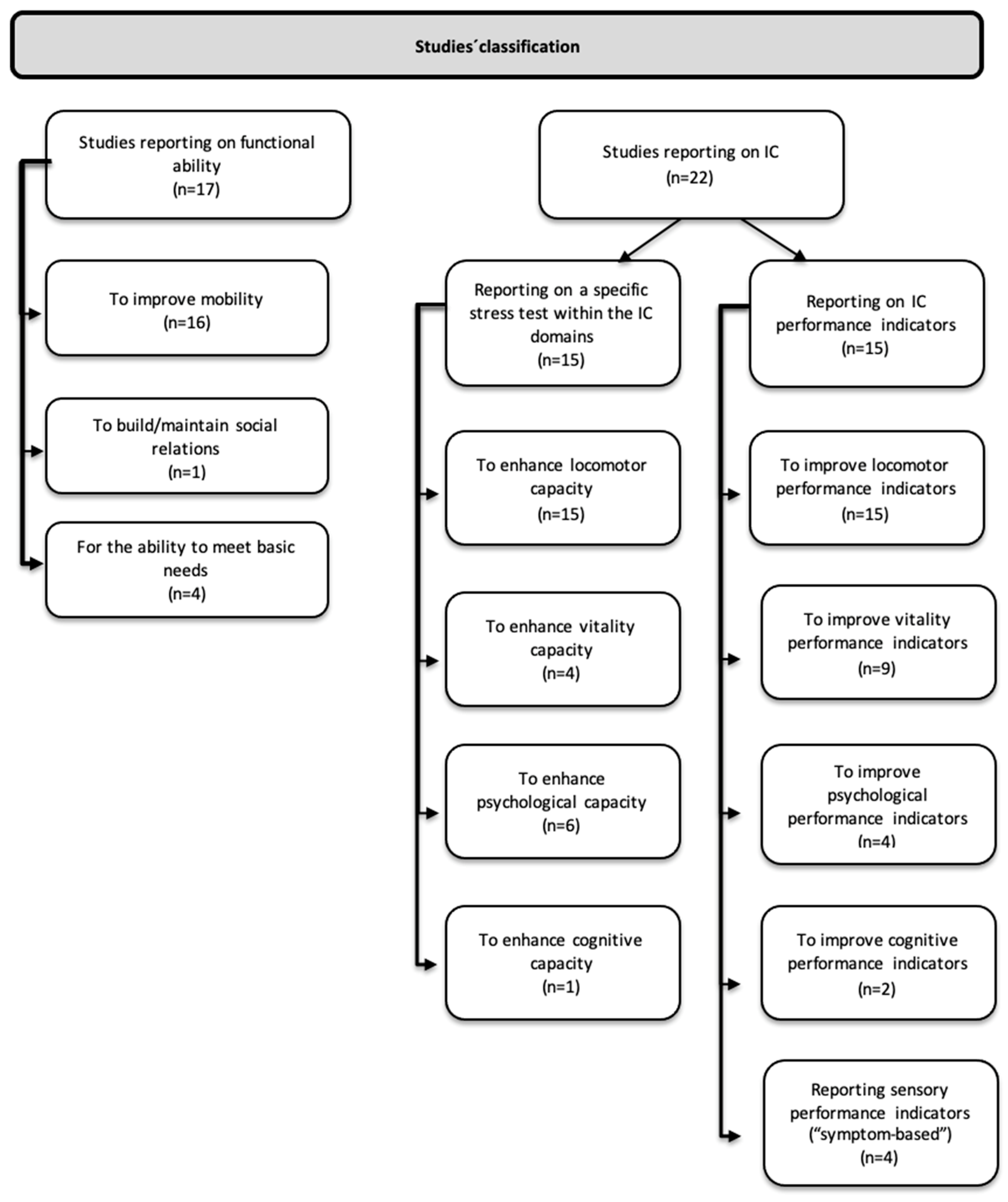
2.4. Data Classification
2.5. Quality Assessment
3. Results
3.1. Studies’ Methodological Quality
3.2. Demographic and Study Characteristics
3.3. LLEs to Improve Functional Ability
3.3.1. LLEs to Improve Mobility
3.3.2. LLEs to Improve Older Persons’ Ability to Build/Maintain Social Relations
3.3.3. LLEs to Improve the Ability to Meet Basic Needs
3.4. LLEs to Enhance IC
3.4.1. LLEs to Enhance Locomotor Capacity
3.4.2. LLEs to Enhance Vitality Capacity
3.4.3. LLEs to Enhance Psychological Capacity
3.4.4. LLEs to Enhance Cognitive Capacity
3.5. LLEs to Improve Performance Indicators
3.5.1. LLEs to Improve Locomotor Performance Indicators
3.5.2. LLEs to Improve Vitality Performance Indicators
3.5.3. LLEs to Improve Psychological Performance Indicators
3.5.4. LLEs to Improve Cognitive Performance Indicators
3.5.5. Sensory Performance Indicators (“Symptom-Based”)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Systematic Search’s Full String
- PubMed
- Concept 1: older adults
- “Aged”[Mesh] OR “oldest old”[tiab] OR quinquagenarian*[tiab] OR sexagenarian*[tiab] OR septuagenarian*[tiab] OR octogenarian*[tiab] OR nonagenarian*[tiab] OR frail*[tiab] OR “functionally impair*” [tiab] OR “older adult*” [tiab] OR senior*[tiab] OR retire*[tiab] OR “Geriatrics”[Mesh:NoExp] OR geriatric*[tiab] OR ((50[tiab] OR 55[tiab] OR 65[tiab] OR 70[tiab] OR 75[tiab] OR 80[tiab] OR 85[tiab] OR 90[tiab] OR 95[tiab] OR 100[tiab]) AND (age[tiab] OR aged[tiab] OR ages[tiab] OR old[tiab] OR year*[tiab])) OR Aged[tiab] OR “advanced age*”[tiab] OR “advancing years” [tiab] OR ageing[tiab] OR aging[tiab] OR elder*[tiab] OR gerontology[MeSH] OR gerontolog*[tiab] OR “old adult*” [tiab] OR “old age*” [tiab] OR “rest home*”[tiab] OR “very old”[tiab] OR “Nursing Homes”[Mesh] OR “nursing home*”[tiab] OR “Health Services for the Aged”[Mesh] OR “Homes for the Aged”[Mesh] OR “Housing for the Elderly”[Mesh] OR “senior center*” [tiab]
- Concept 2: exoskeletons
- “Exoskeleton Device”[Mesh] OR “exoskeleton*”[tiab] OR “Exoskeleton Device*”[tiab] OR “robotic exoskeleton*”[tiab]
- Embase
- Concept 1: older adults
- ‘aged’/exp OR ‘aged’:ti,ab,kw OR ‘elderl*’:ti,ab,kw OR ‘geriatric care’/exp OR ‘geriatric nursing’/exp OR ‘home for the aged’/exp OR ‘old age assistance’:ti,ab,kw OR ‘aged hospital patient’/exp OR ‘senior center’/exp OR ‘geriatric rehabilitation’/exp OR ‘nursing home’/exp OR ‘nursing home*’:ti,ab,kw OR ‘skilled nursing facilit*’:ti,ab,kw OR ‘nursing home patient’/exp OR ‘frail elderly’/exp OR ‘geriatric’/exp OR ‘geriatric*’:ti,ab,kw OR ((50 OR 55 OR 65 OR 70 OR 75 OR 80 OR 85 OR 90 OR 95 OR 100) NEAR/3 (age OR ages OR aged OR old OR year*)):ti,ab,kw OR ‘oldest old’:ti,ab,kw OR ‘quinquagenarian*’:ti,ab,kw OR ‘sexagenarian*’:ti,ab,kw OR ‘septuagenarian*’:ti,ab,kw OR ‘octogenarian*’:ti,ab,kw OR ‘nonagenarian*’:ti,ab,kw OR ‘frail*’:ti,ab,kw OR ‘functionally impair*’:ti,ab,kw OR ‘older adult*’:ti,ab,kw OR ‘senior*’:ti,ab,kw OR ‘retire*’:ti,ab,kw OR ‘advanced age*’:ti,ab,kw OR ‘advancing years’:ti,ab,kw OR ‘ageing’:ti,ab,kw OR ‘aging’:ti,ab,kw OR ‘gerontolog*’:ti,ab,kw OR ‘old adult*’:ti,ab,kw OR ‘old age*’:ti,ab,kw OR ‘rest home*’:ti,ab,kw OR ‘very old’:ti,ab,kw
- Concept 2: exoskeletons
- ‘exoskeleton’/de OR ‘exoskeleton*’:ti,ab,kw OR ‘Exoskeleton Device*’:ti,ab,kw OR ‘robotic exoskeleton*’:ti,ab,kw
- WOS
- Concept 1: older adults
- “aged” OR “elderl*” OR “oldest old” OR ‘’quinquagenarian*’’ OR ‘’sexagenarian*’’ OR ‘’septuagenarian*’’ OR ‘’octogenarian*’’ OR ‘’nonagenarian*’’ OR ‘’ frail*’’ OR “functionally impair*” OR “older adult*” OR ‘’senior*’’ OR ‘’retire*’’ OR ‘’geriatric*’’ OR “advanced age*”OR “advancing years” OR ‘’ageing’’ OR ‘’aging’’ OR ‘’gerontolog*’’ OR “old adult*” OR “old age*” OR “rest home*” OR “very old” OR ‘’nursing home*’’OR “old age assistance“ OR ‘’skilled nursing facilit*’’ OR “50” OR “55” OR “65” OR “70” OR “75” OR “80” OR “85” OR “90” OR “95” OR “100”
- Concept 2: exoskeletons
- “exoskeleton*” OR “Exoskeleton Device*” OR “robotic exoskeleton*”
- Cochrane
- Concept 1: older adults
- #1: [mh “Aged”]
- #2: [mh “Health Services for the Aged”]
- #3: [mh “Senior Centers”]
- #4: [mh “Geriatrics”]
- #5: [mh “Gerontology”]
- #6: [mh “Housing for the Elderly”]
- #7: [mh “Nursing Homes”]
- #8: (“oldest old” OR quinquagenarian* OR sexagenarian* OR septuagenarian* OR octogenarian* OR nonagenarian* OR frail* OR (functionally NEXT impair*) OR (older NEXT adult*) OR senior* OR retire* OR geriatric* OR
- ((50 OR 5565 OR 70 OR 75 OR 80 OR 85 OR 90 OR 95 OR 100) NEAR/3 (age OR aged OR ages OR old OR year*))
- OR Aged
- OR (advanced NEXT age*) OR “advancing years” OR ageing OR aging OR elder* OR gerontolog* OR (old NEXT adult*) OR (old NEXT age*) OR (rest NEXT home*) OR “very old” OR (nursing NEXT home*) OR ‘’geriatr*’’):ti,ab,kw
- #9: #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8
- Concept 2: traumatic brain injury
- #10: [mh “Exoskeleton Device”]
- #11: exoskeleton NEXT device OR robotic NEXT exoskeleton* OR exoskeleton:ti,ab,kw
- #12: #10 OR #11
- #13: #9 AND #12
- Cinahl
- Concept 1: older adults
- (MH “Aged+”) OR (MH “Health Services for the Aged”) OR (MH ‘’Aged, Hospitalized”) OR (MH “Senior Centers”) OR (MR” Rehabilitation, Geriatric’’) OR (MH “Housing for the Elderly”) OR (MH “Gerontologic Nursing+”) OR (MH “Gerontologic Care”) OR (MH “Nursing Homes+”) OR (MH “Nursing Home Patients”) OR (MH “Frail Elderly”)
- OR TI(“aged” OR “elderl*” OR ‘’oldest old’’ OR ‘’ quinquagenarian *’’ OR ‘’sexagenarian*’’ OR ‘’septuagenarian*’’ OR ‘’octogenarian*’’ OR ‘’nonagenarian*’’ OR ‘’ frail*’’ OR “functionally impair*” OR “older adult*” OR ‘’senior*’’ OR ‘’retire*’’ OR ‘’geriatric*’’ OR “advanced age*”OR “advancing years” OR ‘’ageing’’ OR ‘’aging’’ OR ‘’gerontolog*’’ OR “old adult*” OR “old age*” OR “rest home*” OR “very old” OR ‘’nursing home*’’ OR ‘’old age assistance’’ OR ‘’skilled nursing facilit*’’
- OR ((50 OR 55 OR 65 OR 70 OR 75 OR 80 OR 85 OR 90 OR 95 OR 100) N3 (age OR ages OR aged OR old OR year*)))
- OR AB(“aged” OR “elderl*” OR ‘’oldest old’’ OR ‘’ quinquagenarian *’’ OR ‘’sexagenarian*’’ OR ‘’septuagenarian*’’ OR ‘’octogenarian*’’ OR ‘’nonagenarian*’’ OR ‘’ frail*’’ OR “functionally impair*” OR “older adult*” OR ‘’senior*’’ OR ‘’retire*’’ OR ‘’geriatric*’’ OR “advanced age*”OR “advancing years” OR ‘’ageing’’ OR ‘’aging’’ OR ‘’gerontolog*’’ OR “old adult*” OR “old age*” OR “rest home*” OR “very old” OR ‘’nursing home*’’ OR ‘’old age assistance’’ OR ‘’skilled nursing facilit*’’
- OR ((50 OR 55 OR 65 OR 70 OR 75 OR 80 OR 85 OR 90 OR 95 OR 100) N3 (age OR ages OR aged OR old OR year*)))
- Concept 2: exoskeletons
- (MH “Exoskeleton Device”) OR TI(“exoskeleton*” OR “Exoskeleton Device*” OR “robotic exoskeleton*”)OR AB(“exoskeleton*” OR “Exoskeleton Device*” OR “robotic exoskeleton*”)
- PEDro
- Concept 1: older adults
- old*quinquagenarian*sexagenarian*septuagenarian*octogenarian*nonagenarian*frail* impair*seni*retire*geriatric*age*aging*elder*gerontolog*adult*rest*nursing*senior*
- Concept 2: exoskeletons
- exoskeleton*
- IEEE Xplore Digital Library
- Concept 1: older adults
- oldest old OR quinquagenarian OR sexagenarian OR septuagenarian OR octogenarian OR nonagenarian OR frail OR functionally impair* OR older adult* OR senior OR retire* OR geriatric OR Aged OR advanced age* OR advancing years OR ageing OR aging OR elder OR gerontology* OR old adult OR old age* OR rest home OR very old OR nursing home* OR senior center
- Concept 2: exoskeletons
- exoskeleton OR Exoskeleton Device OR robotic exoskeleton
Appendix B. Studies’ Quality Assessment Based on the Downs and Blacks Scale [31]
| Author (Year) | Reporting | External Validity | Internal Validity-Bias | Internal Validity—Confounding (Selection Bias) | P | T | Quality | ||||||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | |||
| Aprigliano (2019) [32] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 12 | Poor |
| Calabrò (2018) [59] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 25 | Good |
| Carral (2022) [40] | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 15 | Fair |
| Fang (2022) [33] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 12 | Poor |
| Firouzi (2022) [24] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 15 | Fair |
| Fujikawa (2022) [34] | 1 | 1 | 1 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 12 | Poor |
| Galle (2022) [35] | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 11 | Poor |
| Gryfe (2022) [60] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 21 | Good |
| Jayaraman (2022) [36] | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 12 | Poor |
| Jin (2017) [37] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 14 | Poor |
| Jin (2019) [41] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 16 | Fair |
| Kawashima (2022) [61] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 20 | Good |
| Koseki (2021) [42] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 18 | Fair |
| Lee (2017) [43] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 15 | Fair |
| Lee (2017) [44] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 17 | Fair |
| Lee (2022) [62] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 21 | Good |
| Lefeber (2018) [45] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 16 | Fair |
| Longatelli (2021) [46] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 18 | Fair |
| Martini (2019) [47] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 19 | Fair |
| Monaco (2017) [48] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 15 | Fair |
| Norris (2007) [49] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 17 | Fair |
| Panizzolo (2022) [50] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 15 | Fair |
| Park (2021) [51] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 19 | Fair |
| Roggeman (2022) [52] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 17 | Fair |
| Rojek (2020) [63] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 21 | Good |
| Romanato (2022) [38] | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 11 | Poor |
| Setoguchi (2022) [53] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 18 | Fair |
| Shore (2022) [39] | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 13 | Poor |
| Son (2021) [64] | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 20 | Good |
| Taki (2020) [54] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 18 | Fair |
| Verrusio (2018) [55] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 18 | Fair |
| Watanabe (2017) [56] | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 19 | Fair |
| Yeung (2021) [65] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 22 | Good |
| Yoshikawa (2018) [57] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 17 | Fair |
| Yoshimoto (2022) [66] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 6 | 22 | Good |
| Yun (2020) [58] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 18 | Fair |
| P = power; T = tot. | |||||||||||||||||||||||||||||
- Downs and Blacks Scale questions (Downs and Black, 1998):
- 1. Is the hypothesis/aim/objective of the study clearly described?
- 2. Are the main outcomes to be measured clearly described in the Introduction or Methods section?
- 3. Are the characteristics of the patients included in the study clearly described?
- 4. Are the interventions of interest clearly described?
- 5. Are the distributions of principal confounders in each group of subjects to be compared clearly described?
- 6. Are the main findings of the study clearly described?
- 7. Does the study provide estimates of the random variability in the data for the main outcomes?
- 8. Have all important adverse events that may be a consequence of the intervention been reported?
- 9. Have the characteristics of patients lost to follow-up been described?
- 10. Have actual probability values been reported (e.g., 0.035 rather than <0.05) for the main outcomes except where the probability value is less than 0.001?
- 11. Were the subjects asked to participate in the study representative of the entire population from which they were recruited?
- 12. Were those subjects who were prepared to participate representative of the entire population from which they were recruited?
- 13. Were the staff, places, and facilities where the patients were treated, representative of the treatment the majority of patients receive?
- 14. Was an attempt made to blind study subjects to the intervention they have received?
- 15. Was an attempt made to blind those measuring the main outcomes of the intervention?
- 16. If any of the results of the study were based on “data dredging”, was this made clear?
- 17. In trials and cohort studies, do the analyses adjust for different lengths of follow-up of patients, or in case-control studies, is the time period between the intervention and outcome the same for cases and controls?
- 18. Were the statistical tests used to assess the main outcomes appropriate?
- 19. Was compliance with the intervention/s reliable?
- 20. Were the main outcome measures used accurate (valid and reliable)?
- 21. Were the patients in different intervention groups (trials and cohort studies) or were the cases and controls (case-control studies) recruited from the same population?
- 22. Were study subjects in different intervention groups (trials and cohort studies) or were the cases and controls (case-control studies) recruited over the same period of time?
- 23. Were study subjects randomized to intervention groups?
- 24. Was the randomized intervention assignment concealed from both patients and health care staff until recruitment was complete and irrevocable?
- 25. Was there adequate adjustment for confounding in the analyses from which the main findings were drawn?
- 26. Were losses of patients to follow-up taken into account?
- 27. Did the study have sufficient power to detect a clinically important effect where the probability value for a difference being due to chance is less than 5%?
- All questions were scored on the following scale: yes = 1, unable to determine = 0, and no = 0.
References
- WHO. World Report on Ageing and Health; WHO Press: Geneva, Switzerland, 2015; p. 260. [Google Scholar]
- Grimmer, M.; Riener, R.; Walsh, C.J.; Seyfarth, A. Mobility related physical and functional losses due to aging and disease—A motivation for lower limb exoskeletons. J. Neuroeng. Rehabil. 2019, 16, 2. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.M.; Ludden, G.D.S. Potential of Exoskeleton Technology to Assist Older Adults with Daily Living. In Proceedings of the Extended Abstracts of the 2018 CHI Conference on Human Factors in Computing Systems, Montreal, QC, Canada, 21–26 April 2018; pp. 1–6. [Google Scholar]
- United Nations. Convention on the rights of persons with disabilities. Eur. J. Health Law 2007, 14, 281–298. [Google Scholar]
- Beard, J.R.; Jotheeswaran, A.T.; Cesari, M.; Araujo de Carvalho, I. The structure and predictive value of intrinsic capacity in a longitudinal study of ageing. BMJ Open 2019, 9, e026119. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Honvo, G.; Amuthavalli Thiyagarajan, J.; Rizzoli, R.; Cooper, C.; Bruyère, O.; Mikton, C.; Sumi, Y.; Diaz, T.; Reginster, J.Y.; et al. Attributes and definitions of locomotor capacity in older people: A World Health Organisation (WHO) locomotor capacity working group meeting report. Aging Clin. Exp. Res. 2022, 34, 481–483. [Google Scholar] [CrossRef] [PubMed]
- Bautmans, I.; Knoop, V.; Amuthavalli Thiyagarajan, J.; Maier, A.B.; Beard, J.R.; Freiberger, E.; Belsky, D.; Aubertin-Leheudre, M.; Mikton, C.; Cesari, M.; et al. WHO working definition of vitality capacity for healthy longevity monitoring. Lancet Healthy Longev. 2022, 3, e789–e796. [Google Scholar] [CrossRef] [PubMed]
- Gusi, N.; Adsuar, J.C.; Corzo, H.; del Pozo-Cruz, B.; Olivares, P.R.; Parraca, J.A. Balance training reduces fear of falling and improves dynamic balance and isometric strength in institutionalised older people: A randomised trial. J. Physiother. 2012, 58, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Cseke, B.; Uchida, T.K.; Doumit, M. Simulating Ideal Assistive Strategies to Reduce the Metabolic Cost of Walking in the Elderly. IEEE Trans. Biomed. Eng. 2022, 69, 2797–2805. [Google Scholar] [CrossRef] [PubMed]
- Peterson, M.J.; Giuliani, C.; Morey, M.C.; Pieper, C.F.; Evenson, K.R.; Mercer, V.; Cohen, H.J.; Visser, M.; Brach, J.S.; Kritchevsky, S.B.; et al. Physical activity as a preventative factor for frailty: The health, aging, and body composition study. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Rejeski, W.J.; Mihalko, S.L. Physical activity and quality of life in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, 23–35. [Google Scholar] [CrossRef]
- Gomes, M.; Figueiredo, D.; Teixeira, L.; Poveda, V.; Paúl, C.; Santos-Silva, A.; Costa, E. Physical inactivity among older adults across Europe based on the SHARE database. Age Ageing 2017, 46, 71–77. [Google Scholar] [CrossRef]
- Bean, J.F.; Vora, A.; Frontera, W.R. Benefits of exercise for community-dwelling older adults. Arch. Phys. Med. Rehabil. 2004, 85 (Suppl. S3), S31–S42; quiz S43–S44. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.D.; Wang, W.W.; Lee, K.W.; Lin, S.Y.; Fu, L.C.; Lai, J.S.; Chen, W.S.; Luh, J.J. Arm Exoskeleton Rehabilitation Robot with Assistive System for Patient after Stroke. In Proceedings of the 2012 12th International Conference on Control, Automation and Systems (ICCAS), Jeju, Republic of Korea, 17–21 October 2012; pp. 1943–1948. [Google Scholar]
- Zhou, Y.; Ma, L. Intrinsic Capacity in Older Adults: Recent Advances. Aging Dis. 2022, 13, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Suominen, H. Ageing and maximal physical performance. Eur. Rev. Aging Phys. Act. 2011, 8, 37–42. [Google Scholar] [CrossRef]
- Pahor, M.; Guralnik, J.M.; Ambrosius, W.T.; Blair, S.; Bonds, D.E.; Church, T.S.; Espeland, M.A.; Fielding, R.A.; Gill, T.M.; Groessl, E.J.; et al. Effect of structured physical activity on prevention of major mobility disability in older adults: The LIFE study randomized clinical trial. JAMA 2014, 311, 2387–2396. [Google Scholar] [CrossRef]
- Hsu, T.-H.; Tsai, C.-L.; Chi, J.-Y.; Hsu, C.-Y.; Lin, Y.-N. Effect of wearable exoskeleton on post-stroke gait: A systematic review and meta-analysis. Ann. Phys. Rehabil. Med. 2023, 66, 101674. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-H.; Mao, H.-F.; Hu, J.-S.; Wang, T.-Y.; Tsai, Y.-J.; Hsu, W.-L. The effects of gait training using powered lower limb exoskeleton robot on individuals with complete spinal cord injury. J. NeuroEng. Rehabil. 2018, 15, 14. [Google Scholar] [CrossRef] [PubMed]
- Normand, M.A.; Lee, J.; Su, H.; Sulzer, J.S. The effect of hip exoskeleton weight on kinematics, kinetics, and electromyography during human walking. J. Biomech. 2023, 152, 111552. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.N.; Wu, Y.N.; Yang, B.S. The neuromuscular control for lower limb exoskeleton- a 50-year perspective. J. Biomech. 2023, 158, 111738. [Google Scholar] [CrossRef] [PubMed]
- Pamungkas, D.; Caesarendra, W.; Soebakti, H.; Analia, R.; Susanto, S. Overview: Types of Lower Limb Exoskeletons. Electronics 2019, 8, 1283. [Google Scholar] [CrossRef]
- Di Natali, C.; Ortiz, J.; Caldwell, D.G. Quasi-passive lower limbs exosuit: An in-depth assessment of fatigue, kinematic and muscular patterns while comparing assistive strategies on an expert subject’s gait analysis. Front. Neurorobot. 2023, 17, 1127694. [Google Scholar] [CrossRef]
- Firouzi, M.; De Keersmaecker, E.; Lefeber, N.; Roggeman, S.; Joos, E.; Kerckhofs, E.; Swinnen, E. Immediate effects of the honda walking assist on spatiotemporal gait characteristics in individuals after stroke. Med. Nov. Technol. Devices 2022, 16, 100173. [Google Scholar] [CrossRef]
- Kim, S.H.; Han, J.Y.; Song, M.K.; Choi, I.S.; Park, H.K. Effectiveness of Robotic Exoskeleton-Assisted Gait Training in Spinocerebellar Ataxia: A Case Report. Sensors 2021, 21, 4874. [Google Scholar] [CrossRef] [PubMed]
- Goffredo, M.; Guanziroli, E.; Pournajaf, S.; Gaffuri, M.; Gasperini, G.; Filoni, S.; Baratta, S.; Damiani, C.; Franceschini, M.; Molteni, F. Overground wearable powered exoskeleton for gait training in subacute stroke subjects: Clinical and gait assessments. Eur. J. Phys. Rehabil. Med. 2019, 55, 710–721. [Google Scholar] [CrossRef] [PubMed]
- den Brave, M.; Beaudart, C.; de Noordhout, B.M.; Gillot, V.; Kaux, J.F. Effect of robot-assisted gait training on quality of life and depression in neurological impairment: A systematic review and meta-analysis. Clin. Rehabil. 2023, 37, 876–890. [Google Scholar] [CrossRef] [PubMed]
- Diaz, T.; Banerjee, A. Welcome to the supplement on measurement of healthy ageing. Age Ageing 2023, 52 (Suppl. S4), iv1–iv2. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Bmj 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, Version 6.4; Cochrane: London, UK, 2023. [Google Scholar]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Aprigliano, F.; Monaco, V.; Tropea, P.; Martelli, D.; Vitiello, N.; Micera, S. Effectiveness of a Robot-Mediated Strategy While Counteracting Multidirectional Slippages. Robotica 2019, 37, 2119–2131. [Google Scholar] [CrossRef]
- Fang, Y.; Harshe, K.; Franz, J.R.; Lerner, Z.F. Feasibility evaluation of a dual-mode ankle exoskeleton to assist and restore community ambulation in older adults. Wearable Technol. 2022, 3, e13. [Google Scholar] [CrossRef]
- Fujikawa, T.; Takahashi, S.; Shinohara, N.; Mashima, N.; Koda, M.; Takahashi, H.; Yasunaga, Y.; Sankai, Y.; Yamazaki, M.; Miura, K. Early Postoperative Rehabilitation Using the Hybrid Assistive Limb (HAL) Lumbar Type in Patients With Hip Fracture: A Pilot Study. Cureus J. Med. Sci. 2022, 14, e22484. [Google Scholar] [CrossRef]
- Galle, S.; Derave, W.; Bossuyt, F.; Calders, P.; Malcolm, P.; De Clercq, D. Exoskeleton plantarflexion assistance for elderly. Gait Posture 2017, 52, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Jayaraman, C.; Embry, K.R.; Mummidisetty, C.K.; Moon, Y.; Giffhorn, M.; Prokup, S.; Lim, B.; Lee, J.; Lee, Y.; Lee, M.; et al. Modular hip exoskeleton improves walking function and reduces sedentary time in community-dwelling older adults. J. Neuroeng. Rehabil. 2022, 19, 144. [Google Scholar] [CrossRef]
- Jin, S.; Iwamoto, N.; Hashimoto, K.; Yamamoto, M. Experimental Evaluation of Energy Efficiency for a Soft Wearable Robotic Suit. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 1192–1201. [Google Scholar] [CrossRef]
- Romanato, M.; Fichera, F.; Pegolo, E.; Spolaor, F.; Volpe, D.; Sawacha, Z. Neuromusculoskeletal modeling-based evaluation of physical treatment outcomes: Assessing how an exoskeleton rehabilitation treatment affects people with PD. Gait Posture 2022, 97, S210–S211. [Google Scholar] [CrossRef]
- Shore, L.; de Eyto, A.; O’Sullivan, L. Technology acceptance and perceptions of robotic assistive devices by older adults—implications for exoskeleton design. Disabil. Rehabil. Assist. Technol. 2022, 17, 782–790. [Google Scholar] [CrossRef] [PubMed]
- Carral, M.D.; Bourqui, V.; Vuilleumier, N.; Ortieb, A.; Bouri, M. Are Functional Measures Sufficient to Capture Acceptance? A Qualitative Study on Lower Limb Exoskeleton Use for Older People. Int. J. Soc. Robot. 2022, 14, 603–616. [Google Scholar] [CrossRef]
- Jin, S.H.; Xiong, X.G.; Zhao, D.J.; Jin, C.F.; Yamamoto, M. Long-Term Effects of a Soft Robotic Suit on Gait Characteristics in Healthy Elderly Persons. Appl. Sci. 2019, 9, 1957. [Google Scholar] [CrossRef]
- Koseki, K.; Mutsuzaki, H.; Yoshikawa, K.; Iwai, K.; Hashizume, Y.; Nakazawa, R.; Kohno, Y. Early Recovery of Walking Ability in Patients After Total Knee Arthroplasty Using a Hip-Wearable Exoskeleton Robot: A Case-Controlled Clinical Trial. Geriatr. Orthop. Surg. Rehabil. 2021, 12, 21514593211027675. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Lee, S.; Chang, W.H.; Seo, K.; Shim, Y.; Choi, B.O.; Ryu, G.H.; Kim, Y.H. A Wearable Hip Assist Robot Can Improve Gait Function and Cardiopulmonary Metabolic Efficiency in Elderly Adults. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 1549–1557. [Google Scholar] [CrossRef]
- Lee, S.H.; Lee, H.J.; Chang, W.H.; Choi, B.O.; Lee, J.; Kim, J.; Ryu, G.H.; Kim, Y.H. Gait performance and foot pressure distribution during wearable robot-assisted gait in elderly adults. J. Neuroeng. Rehabil. 2017, 14, 123. [Google Scholar] [CrossRef]
- Lefeber, N.; De Keersmaecker, E.; Henderix, S.; Michielsen, M.; Kerckhofs, E.; Swinnen, E. Physiological Responses and Perceived Exertion During Robot-Assisted and Body Weight–Supported Gait After Stroke. Neurorehabilit. Neural Repair. 2018, 32, 1043–1054. [Google Scholar] [CrossRef]
- Longatelli, V.; Pedrocchi, A.; Guanziroli, E.; Molteni, F.; Gandolla, M. Robotic Exoskeleton Gait Training in Stroke: An Electromyography-Based Evaluation. Front. Neurorobot. 2021, 15, 733738. [Google Scholar] [CrossRef] [PubMed]
- Martini, E.; Crea, S.; Parri, A.; Bastiani, L.; Faraguna, U.; McKinney, Z.; Molino-Lova, R.; Pratali, L.; Vitiello, N. Gait training using a robotic hip exoskeleton improves metabolic gait efficiency in the elderly. Sci. Rep. 2019, 9, 7157. [Google Scholar] [CrossRef]
- Monaco, V.; Tropea, P.; Aprigliano, F.; Martelli, D.; Parri, A.; Cortese, M.; Molino-Lova, R.; Vitiello, N.; Micera, S. An ecologically-controlled exoskeleton can improve balance recovery after slippage. Sci. Rep. 2017, 7, 46721. [Google Scholar] [CrossRef] [PubMed]
- Norris, J.A.; Granata, K.P.; Mitros, M.R.; Byrne, E.M.; Marsh, A.P. Effect of augmented plantarflexion power on preferred walking speed and economy in young and older adults. Gait Posture 2007, 25, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Panizzolo, F.A.; Cimino, S.; Pettenello, E.; Belfiore, A.; Petrone, N.; Marcolin, G. Effect of a passive hip exoskeleton on walking distance in neurological patients. Assist. Technol. 2022, 34, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Oh-Park, M.; Bialek, A.; Friel, K.; Edwards, D.; You, J.S.H. Abnormal synergistic gait mitigation in acute stroke using an innovative ankle-knee-hip interlimb humanoid robot: A preliminary randomized controlled trial. Sci. Rep. 2021, 11, 22823. [Google Scholar] [CrossRef] [PubMed]
- Roggeman, S.; Firouzi, M.; Lefeber, N.; De Keersmaecker, E.; Cuypers, L.; Swinnen, E.; Joos, E.; Schiltz, M.; Hatem, S.M. Intrinsic motivation for using a wearable hip exoskeleton. Technol. Disabil. 2022, 34, 123–131. [Google Scholar] [CrossRef]
- Setoguchi, D.; Kinoshita, K.; Kamada, S.; Sakamoto, T.; Kise, N.; Kotani, N.; Goto, K.; Shiota, E.; Inoue, T.; Yamamoto, T. Hybrid assistive limb improves restricted hip extension after total hip arthroplasty. Assist. Technol. 2022, 34, 112–120. [Google Scholar] [CrossRef]
- Taki, S.; Imura, T.; Iwamoto, Y.; Imada, N.; Tanaka, R.; Araki, H.; Araki, O. Effects of Exoskeletal Lower Limb Robot Training on the Activities of Daily Living in Stroke Patients: Retrospective Pre-Post Comparison Using Propensity Score Matched Analysis. J. Stroke Cerebrovasc. Dis. 2020, 29, 105176. [Google Scholar] [CrossRef]
- Verrusio, W.; Renzi, A.; Cecchetti, F.; Gaj, F.; Coi, M.; Ripani, M.; Cacciafesta, M. The Effect of a Physical Training with the Use of an Exoskeleton on Depression Levels in Institutionalized Elderly Patients: A Pilot Study. J. Nutr. Health Aging 2018, 22, 934–937. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, H.; Goto, R.; Tanaka, N.; Matsumura, A.; Yanagi, H. Effects of gait training using the Hybrid Assistive Limb® in recovery-phase stroke patients: A 2-month follow-up, randomized, controlled study. NeuroRehabilitation 2017, 40, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, K.; Mutsuzaki, H.; Sano, A.; Koseki, K.; Fukaya, T.; Mizukami, M.; Yamazaki, M. Training with Hybrid Assistive Limb for walking function after total knee arthroplasty. J. Orthop. Surg. Res. 2018, 13, 163. [Google Scholar] [CrossRef] [PubMed]
- Yun, S.J.; Lee, H.H.; Lee, W.H.; Lee, S.H.; Oh, B.M.; Seo, H.G. Effect of robot-assisted gait training on gait automaticity in Parkinson disease: A prospective, open-label, single-arm, pilot study. Medicine 2021, 100, e24348. [Google Scholar] [CrossRef] [PubMed]
- Calabro, R.S.; Naro, A.; Russo, M.; Bramanti, P.; Carioti, L.; Balletta, T.; Buda, A.; Manuli, A.; Filoni, S.; Bramanti, A. Shaping neuroplasticity by using powered exoskeletons in patients with stroke: A randomized clinical trial. J. Neuroeng. Rehabil. 2018, 15, 35. [Google Scholar] [CrossRef] [PubMed]
- Gryfe, P.; Sexton, A.; McGibbon, C.A. Using gait robotics to improve symptoms of Parkinson’s disease: An open-label, pilot randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2022, 58, 723–737. [Google Scholar] [CrossRef] [PubMed]
- Kawashima, N.; Hasegawa, K.; Iijima, M.; Nagami, K.; Makimura, T.; Kumon, A.; Ohtsuki, S. Efficacy of Wearable Device Gait Training on Parkinson’s Disease: A Randomized Controlled Open-label Pilot Study. Intern. Med. 2022, 61, 2573–2580. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Lee, H.J.; Kim, K.; Lee, B.H.; Kim, Y.H. Effect of Exercise Using an Exoskeletal Hip-Assist Robot on Physical Function and Walking Efficiency in Older Adults. J. Pers. Med. 2022, 12, 2077. [Google Scholar] [CrossRef] [PubMed]
- Rojek, A.; Mika, A.; Oleksy, Ł.; Stolarczyk, A.; Kielnar, R. Effects of Exoskeleton Gait Training on Balance, Load Distribution, and Functional Status in Stroke: A Randomized Controlled Trial. Front. Neurol. 2020, 10, 489493. [Google Scholar] [CrossRef]
- Son, C.; Lee, A.; Lee, J.; Kim, D.; Kim, S.J.; Chun, M.H.; Choi, J. The effect of pelvic movements of a gait training system for stroke patients: A single blind, randomized, parallel study. J. Neuroeng. Rehabil. 2021, 18, 185. [Google Scholar] [CrossRef]
- Yeung, L.F.; Lau, C.C.Y.; Lai, C.W.K.; Soo, Y.O.Y.; Chan, M.L.; Tong, R.K.Y. Effects of wearable ankle robotics for stair and over-ground training on sub-acute stroke: A randomized controlled trial. J. Neuroeng. Rehabil. 2021, 18, 19. [Google Scholar] [CrossRef] [PubMed]
- Yoshimoto, T.; Shimizu, I.; Hiroi, Y.; Kawaki, M.; Sato, D.; Nagasawa, M. Feasibility and efficacy of high-speed gait training with a voluntary driven exoskeleton robot for gait and balance dysfunction in patients with chronic stroke: Nonrandomized pilot study with concurrent control. Int. J. Rehabil. Res. 2015, 38, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Federici, S.; Meloni, F.; Bracalenti, M.; De Filippis, M.L. The effectiveness of powered, active lower limb exoskeletons in neurorehabilitation: A systematic review. NeuroRehabilitation 2015, 37, 321–340. [Google Scholar] [CrossRef] [PubMed]
- Chhetri, J.K.; Xue, Q.L.; Ma, L.; Chan, P.; Varadhan, R. Intrinsic Capacity as a Determinant of Physical Resilience in Older Adults. J. Nutr. Health Aging 2021, 25, 1006–1011. [Google Scholar] [CrossRef] [PubMed]
- López-Ortiz, S.; Lista, S.; Peñín-Grandes, S.; Pinto-Fraga, J.; Valenzuela, P.L.; Nisticò, R.; Emanuele, E.; Lucia, A.; Santos-Lozano, A. Defining and assessing intrinsic capacity in older people: A systematic review and a proposed scoring system. Ageing Res. Rev. 2022, 79, 101640. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Rodriguez, D.; Annweiler, C.; Gillain, S.; Vellas, B. Implementation of the Integrated Care of Older People (ICOPE) App in Primary Care: New Technologies in Geriatric Care during Quarantine of COVID-19 and Beyond. J. Frailty Aging 2021, 10, 139–140. [Google Scholar] [CrossRef] [PubMed]
- Varadhan, R.; Walston, J.D.; Bandeen-Roche, K. Can a Link Be Found Between Physical Resilience and Frailty in Older Adults by Studying Dynamical Systems? J. Am. Geriatr. Soc. 2018, 66, 1455–1458. [Google Scholar] [CrossRef]
- Chhetri, J.K.; Harwood, R.H.; Ma, L.; Michel, J.P.; Chan, P. Intrinsic capacity and healthy ageing. Age Ageing 2022, 51, afac239. [Google Scholar] [CrossRef]
- Daly, J.J.; Ruff, R.L. Construction of efficacious gait and upper limb functional interventions based on brain plasticity evidence and model-based measures for stroke patients. Sci. World J. 2007, 7, 2031–2045. [Google Scholar] [CrossRef]
- Viteckova, S.; Kutilek, P.; Boisboissel, G.; Krupicka, R.; Galajdova, A.; Kauler, J.; Lhotska, L.; Szabo, Z. Empowering lower limbs exoskeletons: State-of-the-art. Robotica 2018, 36, 1743–1756. [Google Scholar] [CrossRef]
- Kitatani, R.; Ohata, K.; Takahashi, H.; Shibuta, S.; Hashiguchi, Y.; Yamakami, N. Reduction in energy expenditure during walking using an automated stride assistance device in healthy young adults. Arch. Phys. Med. Rehabil. 2014, 95, 2128–2133. [Google Scholar] [CrossRef] [PubMed]
- Fischer, B.; Peine, A.; Ostlund, B. The Importance of User Involvement: A Systematic Review of Involving Older Users in Technology Design. Gerontologist 2020, 60, e513–e523. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gavrila Laic, R.A.; Firouzi, M.; Claeys, R.; Bautmans, I.; Swinnen, E.; Beckwée, D. A State-of-the-Art of Exoskeletons in Line with the WHO’s Vision on Healthy Aging: From Rehabilitation of Intrinsic Capacities to Augmentation of Functional Abilities. Sensors 2024, 24, 2230. https://doi.org/10.3390/s24072230
Gavrila Laic RA, Firouzi M, Claeys R, Bautmans I, Swinnen E, Beckwée D. A State-of-the-Art of Exoskeletons in Line with the WHO’s Vision on Healthy Aging: From Rehabilitation of Intrinsic Capacities to Augmentation of Functional Abilities. Sensors. 2024; 24(7):2230. https://doi.org/10.3390/s24072230
Chicago/Turabian StyleGavrila Laic, Rebeca Alejandra, Mahyar Firouzi, Reinhard Claeys, Ivan Bautmans, Eva Swinnen, and David Beckwée. 2024. "A State-of-the-Art of Exoskeletons in Line with the WHO’s Vision on Healthy Aging: From Rehabilitation of Intrinsic Capacities to Augmentation of Functional Abilities" Sensors 24, no. 7: 2230. https://doi.org/10.3390/s24072230
APA StyleGavrila Laic, R. A., Firouzi, M., Claeys, R., Bautmans, I., Swinnen, E., & Beckwée, D. (2024). A State-of-the-Art of Exoskeletons in Line with the WHO’s Vision on Healthy Aging: From Rehabilitation of Intrinsic Capacities to Augmentation of Functional Abilities. Sensors, 24(7), 2230. https://doi.org/10.3390/s24072230





