Heart Rate Variability Measurement Can Be a Point-of-Care Sensing Tool for Screening Postpartum Depression: Differentiation from Adjustment Disorder
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Ethical Background
2.3. Heart Rate Variability Measurement
2.4. Statistics
2.5. Linear Discriminant Analysis
3. Results
3.1. HRV and HR Indices
3.2. Task Performance
3.3. Linear Discriminant Analysis
4. Discussion
4.1. HRV and HR Profiles of PPD and AJD during the Three-Behavioral-State Paradigm
4.2. Clinical Applicability of HRV and HR Measurement as a Sensing Tool for Screening PPD
4.3. Limitations and Future Directions
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stewart, D.E.; Vigod, S. Postpartum Depression. N. Engl. J. Med. 2016, 375, 2177–2186. [Google Scholar] [CrossRef] [PubMed]
- Suryawanshi, O., 4th; Pajai, S. A Comprehensive Review on Postpartum Depression. Cureus 2022, 14, e32745. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Lee, Y.L.; Tien, Y.; Bai, Y.S.; Lin, C.K.; Yin, C.S.; Chung, C.H.; Sun, C.A.; Huang, S.H.; Huang, Y.C.; Chien, W.C.; et al. Association of Postpartum Depression with Maternal Suicide: A Nationwide Population-Based Study. Int. J. Environ. Res. Public. Health 2022, 19, 5118. [Google Scholar] [CrossRef] [PubMed]
- Leahy-Warren, P.; McCarthy, G. Postnatal depression: Prevalence, mothers’ perspectives, and treatments. Arch. Psychiatr. Nurs. 2007, 21, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Halbreich, U.; Karkun, S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. J. Affect. Disord. 2006, 91, 97–111. [Google Scholar] [CrossRef] [PubMed]
- Arifin, S.R.M.; Cheyne, H.; Maxwell, M. Review of the prevalence of postnatal depression across cultures. AIMS Public Health 2018, 5, 260–295. [Google Scholar] [CrossRef] [PubMed]
- Premji, S.; McDonald, S.W.; Metcalfe, A.; Faris, P.; Quan, H.; Tough, S.; McNeil, D.A. Examining postpartum depression screening effectiveness in well child clinics in Alberta, Canada: A study using the All Our Families cohort and administrative data. Prev. Med. Rep. 2019, 14, 100888. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Shibata, Y.; Suzuki, S. Comparison of the Edinburgh Postnatal Depression Scale and Whooley questions in screening for postpartum depression in Japan. J. Matern. Fetal Neonatal Med. 2020, 33, 2785–2788. [Google Scholar] [CrossRef]
- Rowe, H.J.; Fisher, J.R.W.; Loh, W.M. The Edinburgh Postnatal Depression Scale detects but does not distinguish anxiety disorders from depression in mothers of infants. Arch. Women’s Ment. Health 2008, 11, 103–108. [Google Scholar] [CrossRef]
- Ferrari, B.; Mesiano, L.; Benacchio, L.; Ciulli, B.; Donolato, A.; Riolo, R. Prevalence and risk factors of postpartum depression and adjustment disorder during puerperium—A retrospective research. J. Reprod. Infant Psychol. 2021, 39, 486–498. [Google Scholar] [CrossRef]
- Ding, X.; Liang, M.; Wang, H.; Song, Q.; Guo, X.; Su, W.; Li, N.; Liu, H.; Ma, S.; Zhou, X.; et al. Prenatal stressful life events increase the prevalence of postpartum depression: Evidence from prospective cohort studies. J. Psychiatr. Res. 2023, 160, 263–271. [Google Scholar] [CrossRef]
- Saharoy, R.; Potdukhe, A.; Wanjari, M.; Taksande, A.B. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus 2023, 15, e41381. [Google Scholar] [CrossRef]
- Wang, X.; Qiu, Q.; Shen, Z.; Yang, S.; Shen, X. A systematic review of interpersonal psychotherapy for postpartum depression. J. Affect. Disord. 2023, 339, 823–831. [Google Scholar] [CrossRef]
- Elwood, J.; Murray, E.; Bell, A.; Sinclair, M.; Kernohan, W.G.; Stockdale, J. A systematic review investigating if genetic or epigenetic markers are associated with postnatal depression. J. Affect. Disord. 2019, 253, 51–62. [Google Scholar] [CrossRef]
- Konjevod, M.; Gredicak, M.; Vuic, B.; Tudor, L.; Perkovic, M.N.; Milos, T.; Strac, D.S.; Pivac, N.; Erjavec, G.N. Overview of metabolomic aspects in postpartum depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 2023, 127, 110836. [Google Scholar] [CrossRef]
- Schoretsanitis, G.; Gastaldon, C.; Ochsenbein-Koelble, N.; Olbrich, S.; Barbui, C.; Seifritz, E. Postpartum hemorrhage and postpartum depression: A systematic review and meta-analysis of observational studies. Acta Psychiatr. Scand. 2023; in press. [Google Scholar] [CrossRef] [PubMed]
- Skalkidou, A.; Hellgren, C.; Comasco, E.; Sylvén, S.; Sundström Poromaa, I. Biological aspects of postpartum depression. Women’s Health 2012, 8, 659–672. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zou, W.; Huang, Y.; Wen, X.; Huang, J.; Wang, Y.; Sheng, X. A Preliminary Study of Uric Metabolomic Alteration for Postpartum Depression Based on Liquid Chromatography Coupled to Quadrupole Time-of-Flight Mass Spectrometry. Dis. Markers 2019, 2019, 4264803. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Lu, B.; Wang, G. The role of gut microbiota in the pathogenesis and treatment of postpartum depression. Ann. Gen. Psychiatry 2023, 22, 36. [Google Scholar] [CrossRef] [PubMed]
- Batt, M.M.; Duffy, K.A.; Novick, A.M.; Metcalf, C.A.; Epperson, C.N. Is Postpartum Depression Different From Depression Occurring Outside of the Perinatal Period? A Review of the Evidence. Focus (Am. Psychiatr. Publ.) 2020, 18, 106–119. [Google Scholar] [CrossRef]
- Guintivano, J.; Sullivan, P.F.; Stuebe, A.M.; Penders, T.; Thorp, J.; Rubinow, D.R.; Meltzer-Brody, S. Adverse life events, psychiatric history, and biological predictors of postpartum depression in an ethnically diverse sample of postpartum women. Psychol. Med. 2018, 48, 1190–1200. [Google Scholar] [CrossRef] [PubMed]
- Mehta, D.; Rex-Haffner, M.; Søndergaard, H.B.; Pinborg, A.; Binder, E.B.; Frokjaer, V.G. Evidence for oestrogen sensitivity in perinatal depression: Pharmacological sex hormone manipulation study. Br. J. Psychiatry 2019, 215, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Meltzer-Brody, S.; Stuebe, A.; Dole, N.; Savitz, D.; Rubinow, D.; Thorp, J. Elevated corticotropin releasing hormone (CRH) during pregnancy and risk of postpartum depression (PPD). J. Clin. Endocrinol. Metab. 2011, 96, E40–E47. [Google Scholar] [CrossRef] [PubMed]
- Oon-Arom, A.; Suradom, C.; Srichairatanakool, S.; Luewan, S.; Petiwathayakorn, T.; Maneeton, B.; Maneeton, N.; Kawilapat, S.; Srisurapanont, M. Serum oxytocin and corticotropin-releasing hormone levels in the third trimester of pregnancy for predicting postpartum depression in Thai women. Asian J. Psychiatr. 2023, 80, 103392. [Google Scholar] [CrossRef] [PubMed]
- Skrundz, M.; Bolten, M.; Nast, I.; Hellhammer, D.H.; Meinlschmidt, G. Plasma oxytocin concentration during pregnancy is associated with development of postpartum depression. Neuropsychopharmacology 2011, 36, 1886–1893. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Nakatochi, M.; Kunimoto, S.; Okada, T.; Aleksic, B.; Toyama, M.; Shiino, T.; Morikawa, M.; Yamauchi, A.; Yoshimi, A.; et al. Methylation analysis for postpartum depression: A case control study. BMC Psychiatry 2019, 19, 190. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, A.; Nishiumi, H.; Okumura, Y.; Watanabe, K. No relation between HRV and psychological measures. J. Affect. Disord. 2015, 179, 175–182. [Google Scholar] [CrossRef]
- Solorzano, C.S.; Violani, C.; Grano, C. Pre-partum HRV as a predictor of postpartum depression: The potential use of a smartphone application for physiological recordings. J. Affect. Disord. 2022, 319, 172–180. [Google Scholar] [CrossRef]
- Kemp, A.H.; Quintana, D.S.; Gray, M.A.; Felmingham, K.L.; Brown, K.; Gatt, J.M. Impact of depression and antidepressant treatment on heart rate variability: A review and meta-analysis. Biol. Psychiatry 2010, 67, 1067–1074. [Google Scholar] [CrossRef]
- Akselrod, S.; Gordon, D.; Madwed, J.B.; Snidman, N.C.; Shannon, D.C.; Cohen, R.J. Hemodynamic regulation: Investigation by spectral analysis. Am. J. Physiol. 1985, 249, H867–H887. [Google Scholar] [CrossRef]
- Malik, M. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Shinba, T. Major depressive disorder and generalized anxiety disorder show different autonomic dysregulations revealed by heart-rate variability analysis in first-onset drug-naïve patients without comorbidity. Psychiat. Clin. Neurosci. 2017, 71, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Shinba, T.; Kuratsune, D.; Shinba, S.; Shinba, Y.; Sun, G.; Matsui, T.; Kuratsune, H. Major depressive disorder and chronic fatigue syndrome show characteristic heart rate variability profiles reflecting autonomic dysregulations: Differentiation by Linear Discriminant Analysis. Sensors 2023, 23, 5330. [Google Scholar] [CrossRef] [PubMed]
- Kanaya, N.; Hirata, N.; Kurosawa, S.; Nakayama, M.; Namiki, A. Differential effects of propofol and sevoflurane on heart rate variability. Anesthesiology 2003, 98, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Sawada, Y.; Ohtomo, N.; Tanaka, Y.; Tanaka, G.; Yamakoshi, K.; Terachi, S.; Shimamoto, K.; Nakagawa, M.; Satoh, S.; Kuroda, S.; et al. New technique for time series analysis combining the maximum entropy method and non-linear least squares method: Its value in heart rate variability analysis. Med. Biol. Eng. Comput. 1997, 35, 318–322. [Google Scholar] [CrossRef]
- Elghozi, J.L.; Laude, D.; Girard, A. Effects of respiration on blood pressure and heart rate variability in humans. Clin. Exp. Pharmacol. Physiol. 1991, 18, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Shinba, T.; Shinozaki, T.; Kariya, N.; Ebata, K. Random number generation deficit in schizophrenia characterized by oral vs written response modes. Percept. Mot. Skills. 2000, 91, 1091–1105. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, D.S.; Bentho, O.; Park, M.Y.; Sharabi, Y. Low-frequency power of heart rate variability is not a measure of cardiac sympathetic tone but may be a measure of modulation of cardiac autonomic outflows by baroreflexes. Exp. Physiol. 2011, 96, 1255–1261. [Google Scholar] [CrossRef]
- Shinba, T. Characteristic Profiles of Heart Rate Variability in Depression and Anxiety. In Biosignal Processing; Asadpour, V., Karakus, S., Eds.; IntechOpen: London, UK, 2022. [Google Scholar]
- Matthey, S.; Henshaw, C.; Elliott, S.; Barnett, B. Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale: Implications for clinical and research practice. Arch. Women’s Ment. Health 2006, 9, 309–315. [Google Scholar] [CrossRef]
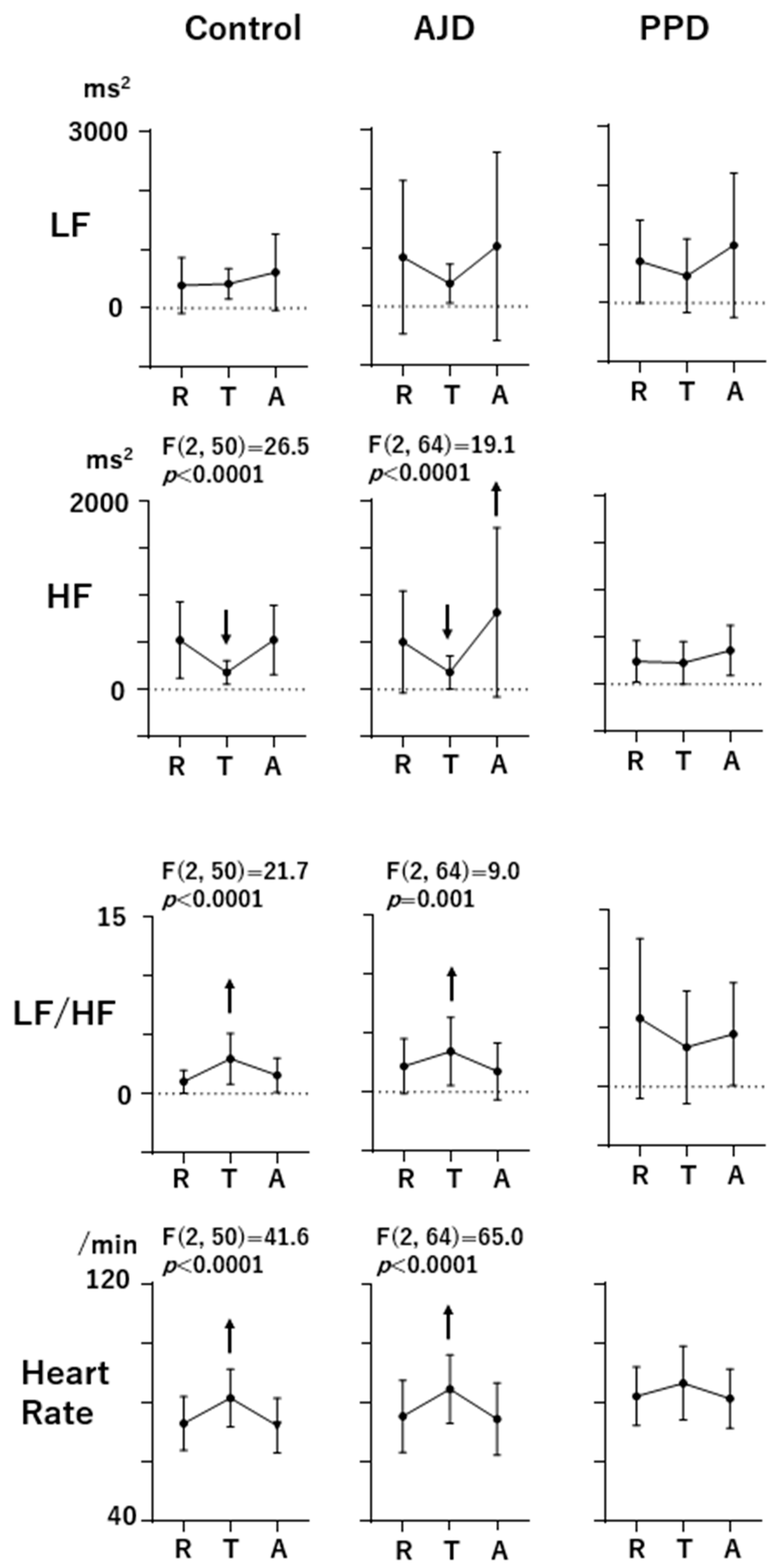


| LF | Rest (ms2) | Task (ms2) | After (ms2) | Task/Rest | After/Rest |
|---|---|---|---|---|---|
| Control | 388.9 ± 474.4 | 413.3 ± 256.7 | 612.7 ± 648.0 | 1.65 ± 1.20 | 1.82 ± 1.01 |
| AJD | 837.4 ± 1300.6 | 391.5 ± 330.6 | 1024.8 ± 1599.8 | 1.02 ± 0.77 | 1.60 ± 1.52 |
| PPD | 707.0 ± 705.3 | 463.2 ± 629.3 | 981.1 ± 1224.9 | 1.12 ± 1.22 | 1.78 ± 1.11 |
| HF | |||||
| Control | 526.2 ± 405.4 | 182.0 ± 126.7 | 528.3 ± 368.0 | 0.49 ± 0.41 | 1.15 ± 0.39 |
| AJD | 505.0 ± 544.1 | 183.6 ± 176.1 | 820.0 ± 897.7 | 0.46 ± 0.32 | 1.94 ± 1.25 |
| PPD | 243.4 ± 218.6 | 227.7 ± 226.0 | 359.2 ± 266.4 | 1.10 ± 1.22 | 1.66 ± 1.06 |
| LF/HF | |||||
| Control | 1.04 ± 0.98 | 2.98 ± 2.16 | 1.57 ± 1.47 | 4.63 ± 3.78 | 1.71 ± 0.90 |
| AJD | 2.19 ± 2.34 | 3.46 ± 2.90 | 1.76 ± 2.41 | 3.04 ± 2.74 | 1.03 ± 1.10 |
| PPD | 5.82 ± 6.80 | 3.37 ± 4.80 | 4.48 ± 4.37 | 1.85 ± 2.39 | 1.34 ± 0.80 |
| HR | |||||
| Control | 73.1 ± 9.1 | 81.7 ± 9.7 | 72.4 ± 9.3 | 1.12 ± 0.10 | 0.99 ± 0.03 |
| AJD | 75.5 ± 12.2 | 84.7 ± 11.5 | 74.5 ± 12.3 | 1.13 ± 0.09 | 0.99 ± 0.05 |
| PPD | 82.3 ± 9.9 | 86.7 ± 12.5 | 81.5 ± 10.0 | 1.05 ± 0.08 | 0.99 ± 0.07 |
| D > 0 | D < 0 | Total | |
|---|---|---|---|
| PPD vs. normal | |||
| PPD | 9 | 3 | 12 |
| Normal | 4 | 24 | 28 |
| Total | 13 | 27 | |
| sensitivity | specificity | ||
| 75.0% | 84.6% | ||
| PPD vs. AJD | |||
| PPD | 9 | 3 | 12 |
| AJD | 3 | 30 | 33 |
| Total | 12 | 33 | |
| sensitivity | specificity | ||
| 75.0% | 90.9% | ||
| AJD vs. normal | |||
| AJD | 28 | 5 | 33 |
| Normal | 7 | 19 | 26 |
| Total | 35 | 24 | |
| sensitivity | specificity | ||
| 84.8% | 73.1% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shinba, T.; Suzuki, H.; Urita, M.; Shinba, S.; Shinba, Y.; Umeda, M.; Hirakuni, J.; Matsui, T.; Onoda, R. Heart Rate Variability Measurement Can Be a Point-of-Care Sensing Tool for Screening Postpartum Depression: Differentiation from Adjustment Disorder. Sensors 2024, 24, 1459. https://doi.org/10.3390/s24051459
Shinba T, Suzuki H, Urita M, Shinba S, Shinba Y, Umeda M, Hirakuni J, Matsui T, Onoda R. Heart Rate Variability Measurement Can Be a Point-of-Care Sensing Tool for Screening Postpartum Depression: Differentiation from Adjustment Disorder. Sensors. 2024; 24(5):1459. https://doi.org/10.3390/s24051459
Chicago/Turabian StyleShinba, Toshikazu, Hironori Suzuki, Michiko Urita, Shuntaro Shinba, Yujiro Shinba, Miho Umeda, Junko Hirakuni, Takemi Matsui, and Ryo Onoda. 2024. "Heart Rate Variability Measurement Can Be a Point-of-Care Sensing Tool for Screening Postpartum Depression: Differentiation from Adjustment Disorder" Sensors 24, no. 5: 1459. https://doi.org/10.3390/s24051459
APA StyleShinba, T., Suzuki, H., Urita, M., Shinba, S., Shinba, Y., Umeda, M., Hirakuni, J., Matsui, T., & Onoda, R. (2024). Heart Rate Variability Measurement Can Be a Point-of-Care Sensing Tool for Screening Postpartum Depression: Differentiation from Adjustment Disorder. Sensors, 24(5), 1459. https://doi.org/10.3390/s24051459








