Smartphone Assessment of the Sitting Heel-Rise Test
Abstract
1. Introduction
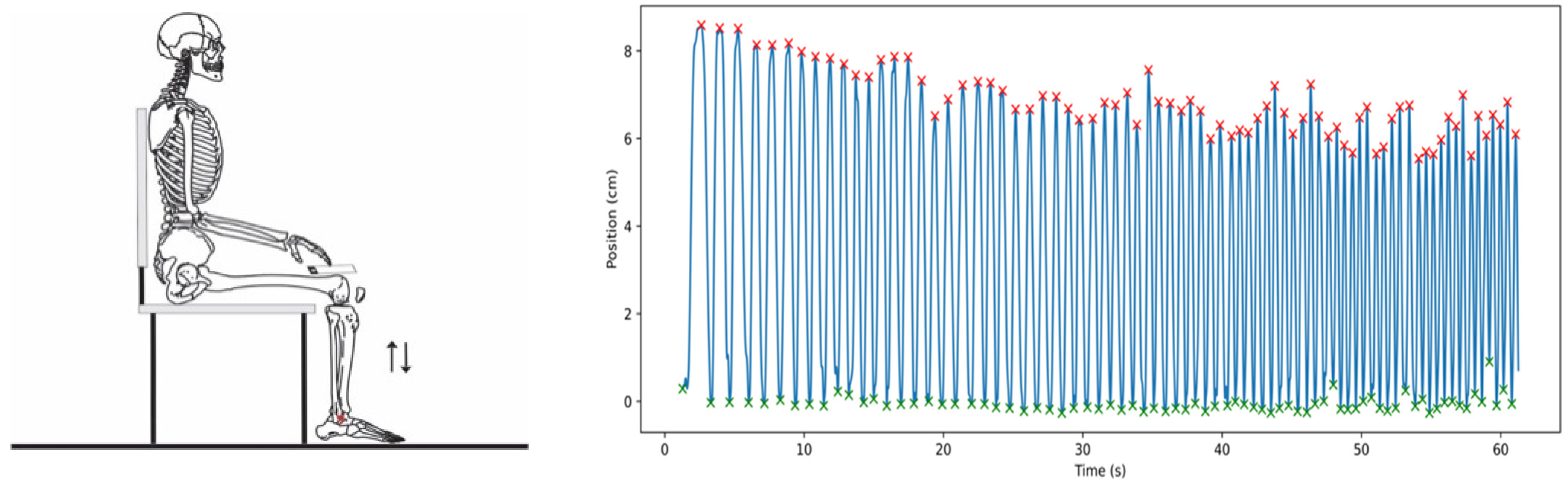
2. Materials and Methods
2.1. Materials
2.2. Protocol
2.3. Signal Processing
2.4. Statistics
3. Results
4. Discussion
4.1. Number of Cycles
4.2. Temporal Aspects
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hébert-Losier, K.; Schneiders, A.G.; Newsham-West, R.J.; Sullivan, S.J. Scientific bases and clinical utilisation of the calf-raise test. Phys. Ther. Sport 2009, 10, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Kocaman, A.A.; Demirci, C.; Aydoğan Arslan, S.; Yildirim Şahan, T.; Vergili, Ö.; Oral, M.A.; Bezgin, S.; Uğurlu, K.; Önal, B.; Keskin, E.D.; et al. The Cutoff Value of the Calf-Raise Senior Test for Older Faller. Phys. Occup. Ther. Geriatr. 2020, 39, 206–217. [Google Scholar] [CrossRef]
- Monteiro, D.P.; Britto, R.R.; de Freitas Fregonezi, G.A.; Dias, F.A.L.; da Silva, M.G.; Pereira, D.A.G. Reference values for the bilateral heel-rise test. Brazilian Journal of. Braz. J. Phys. Ther. 2017, 21, 344–349. [Google Scholar] [CrossRef]
- Bohannon, R.W. The heel-raise test for ankle plantarflexor strength: A scoping review and meta-analysis of studies providing norms. J. Phys. Ther. Sci. 2022, 34, 528–531. [Google Scholar] [CrossRef]
- Hébert-Losier, K.; Schneiders, A.G.; Sullivan, S.J.; Newsham-West, R.J.; García, J.A.; Simoneau, G.G. Analysis of knee flexion angles during 2 clinical versions of the heel raise test to assess soleus and gastrocnemius function. J. Orthop. Sports Phys. Ther. 2011, 41, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Chitre, D.P.; Prabhu, D.S. Decade Wise Analysis of Ankle Plantar Flexors Strength in Adults Using One Leg Heel Raise Test (OLHR). IOSR J. Nurs. Health Sci. 2017, 6, 106–109. [Google Scholar] [CrossRef]
- Lunsford, B.R.; Perry, J. The standing heel-rise test for ankle plantar flexion: Criterion for normal. Phys. Ther. 1995, 75, 694–698. [Google Scholar] [CrossRef] [PubMed]
- Sara, L.K.; Gutsch, S.B.; Hunter, S.K. The single-leg heel raise does not predict maximal plantar flexion strength in healthy males and females. PLoS ONE 2021, 16, e0253276. [Google Scholar] [CrossRef]
- Tapanya, W.; Maharan, S.; Sangkarit, N.; Poncumhak, P.; Konsanit, S. Using a Standing Heel-Rise Test as a Predictor of Ankle Muscle Strength in the Elderly. Sports 2023, 11, 146. [Google Scholar] [CrossRef]
- Hashish, R.; Samarawickrame, S.D.; Wang, M.-Y.; Yu, S.S.-Y.; Salem, G.J. The Association between Unilateral Heel-Rise Performance with Static and Dynamic Balance in Community-Dwelling Older Adults. Geriatr. Nurs. 2015, 36, 30–34. [Google Scholar] [CrossRef]
- Fernandez, M.R.; Hébert-Losier, K. Devices to measure calf raise test outcomes: A narrative review. Physiother. Res. Int. 2023, 28, e2039. [Google Scholar] [CrossRef] [PubMed]
- Zahid, S.A.; Celik, Y.; Godfrey, A.; Buckley, J.G. Use of ‘wearables’ to assess the up-on-the-toes test. J. Biomech. 2022, 143, 28–31. [Google Scholar] [CrossRef]
- Millor, N.; Lecumberri, P.; Gomez, M.; Martinez, A.; Martinikorena, J.; Rodriguez-Manas, L.; Garcia-Garcia, F.J.; Izquierdo, M. Gait Velocity and Chair Sit-Stand-Sit Performance Improves Current Frailty-Status Identification. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 2018–2025. [Google Scholar] [CrossRef] [PubMed]
- Elwardany, S.H.; El-Sayed, W.H.; Ali, M.F. Reliability of Kinovea Computer Program in Measuring Cervical Range of Motion in Sagittal Plane. OALib 2015, 2, 68651. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical Methods for Assessing Agreement between Two Methods of Clinical Measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Pizzigalli, L.; Filipinni, A.; Ahamaid, S.; Jullien, H.; Rainoldi, A. Prevention of Falling Risk in Elderly People: The Relevance of Muscular Strength and Symmetry of Lower Limbs in Postural Stability. J. Strength Cond. Res. 2011, 25, 567–574. [Google Scholar] [CrossRef]
- Chon, J.; Kim, H.S.; Lee, J.H.; Yoo, S.D.; Yun, D.H.; Kim, D.H.; Lee, S.A.; Han, Y.J.; Soh, Y.; Kim, Y.; et al. Association between asymmetry in knee extension strength and balance in a community-dwelling elderly population: A cross-sectional analysis. Ann. Rehabil. Med. 2018, 42, 113–119. [Google Scholar] [CrossRef]
- LaRoche, D.P.; Cook, S.B.; Mackala, K. Strength Asymmetry Increases Gait Asymmetry and Variability in Older Women. Med. Sci. Sports Exerc. 2012, 44, 2172–2181. [Google Scholar] [CrossRef]
- Skelton, D.A.; Kennedy, J.; Rutherford, O.M. Explosive power and asymmetry in leg muscle function in frequent fallers and non-fallers aged over 65. Age Ageing 2002, 31, 119–125. [Google Scholar] [CrossRef]
- Seo, J.; Suk Kim, S. Prevention of Potential Falls of Elderly Healthy Women: Gait Asymmetry. Educ. Gerontol. 2014, 40, 123–137. [Google Scholar] [CrossRef]
- Wolfson, L.; Judge, J.; Whipple, R.; King, M. Strength Is a Major Factor in Balance, Gait, and the Occurrence of Falls. J. Gerontol. 1995, 50, 64–67. [Google Scholar]
- Sman, A.D.; Hiller, C.E.; Imer, A.; Ocsing, A.; Burns, J.; Refshauge, K.M. Design and reliability of a novel heel rise test measuring device for plantarflexion endurance. BioMed Res. Int. 2014, 2014, 91646. [Google Scholar] [CrossRef] [PubMed]
- André, H.; Carnide, F.; Borja, E.; Ramalho, F.; Santos-Rocha, R.; Veloso, A.P. Calf-raise senior: A new test for assessment of plantar flexor muscle strength in older adults: Protocol, validity, and reliability. Clin. Interv. Aging 2016, 11, 1661–1674. [Google Scholar] [CrossRef] [PubMed]
- Ugbolue, U.C.; Papi, E.; Kaliarntas, K.T.; Kerr, A.; Earl, L.; Pomeroy, V.M.; Rowe, P.J. The evaluation of an inexpensive, 2D, video based gait assessment system for clinical use. Gait Posture 2013, 38, 483–489. [Google Scholar] [CrossRef] [PubMed]
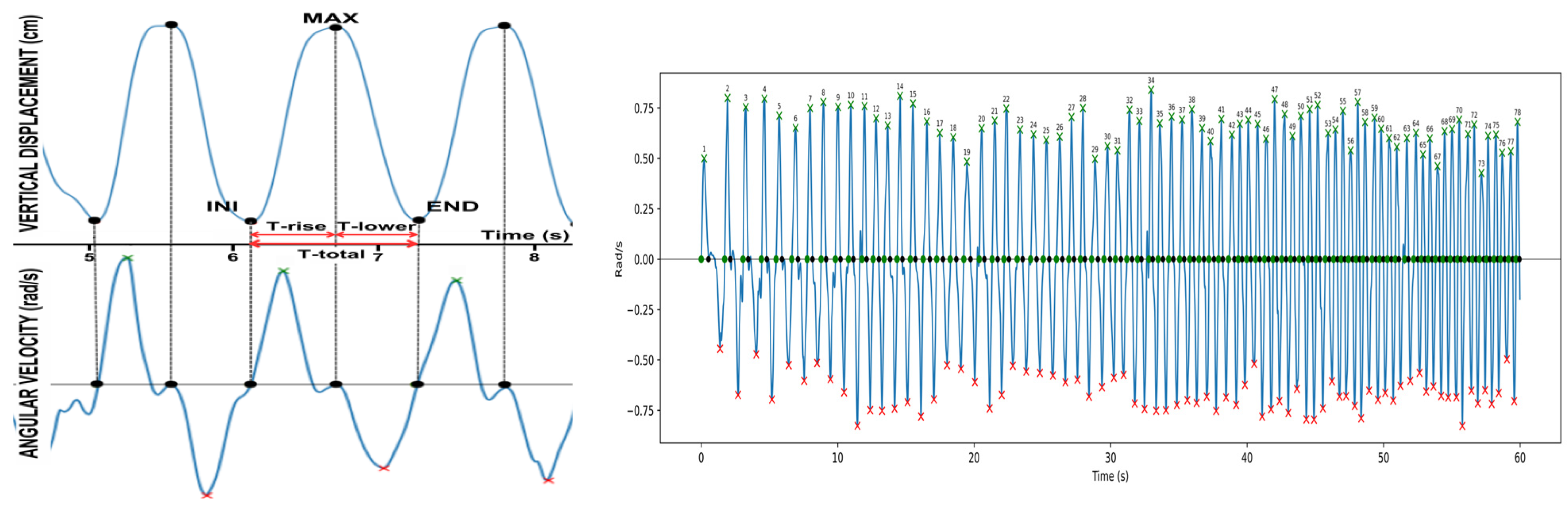


| Data Series | Mean (±SD) | Agreement | 95% CI | |
|---|---|---|---|---|
| Cycles (number) | Gyroscope/ Video | 82.1 (29.1) * | 0.00 | 0, 0 |
| T-rise (s) | Gyroscope | 0.359 ± 0.116 | 0.0005 | −0.1118, 0.1127 |
| Video | 0.360 ± 0.113 | |||
| T-lower (s) | Gyroscope | 0.454 ± 0.193 | 0.0013 | −0.1152, 0.1179 |
| Video | 0.455 ± 0.190 | |||
| T-total (s) | Gyroscope | 0.814 ± 0.299 | 0.0017 | −0.0763, 0.0797 |
| Video | 0.815 ± 0.297 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoffmann, G.O.; Borba, E.; Casarotto, E.H.; Devetak, G.F.; Jaber, R.; Buckley, J.G.; Rodacki, A.L.F. Smartphone Assessment of the Sitting Heel-Rise Test. Sensors 2024, 24, 6036. https://doi.org/10.3390/s24186036
Hoffmann GO, Borba E, Casarotto EH, Devetak GF, Jaber R, Buckley JG, Rodacki ALF. Smartphone Assessment of the Sitting Heel-Rise Test. Sensors. 2024; 24(18):6036. https://doi.org/10.3390/s24186036
Chicago/Turabian StyleHoffmann, Gustavo O., Edilson Borba, Eduardo H. Casarotto, Gisele Francine Devetak, Ramzi Jaber, John G. Buckley, and André L. F. Rodacki. 2024. "Smartphone Assessment of the Sitting Heel-Rise Test" Sensors 24, no. 18: 6036. https://doi.org/10.3390/s24186036
APA StyleHoffmann, G. O., Borba, E., Casarotto, E. H., Devetak, G. F., Jaber, R., Buckley, J. G., & Rodacki, A. L. F. (2024). Smartphone Assessment of the Sitting Heel-Rise Test. Sensors, 24(18), 6036. https://doi.org/10.3390/s24186036









