Abstract
Traditional respiratory rehabilitation training fails to achieve visualization and quantification of respiratory data in improving problems such as decreased lung function and dyspnea in people with respiratory disorders, and the respiratory rehabilitation training process is simple and boring. Therefore, this article designs a biofeedback respiratory rehabilitation training system based on virtual reality technology. It collects respiratory data through a respiratory sensor and preprocesses it. At the same time, it combines the biofeedback respiratory rehabilitation training virtual scene to realize the interaction between respiratory data and virtual scenes. This drives changes in the virtual scene, and finally the respiratory data are fed back to the patient in a visual form to evaluate the improvement of the patient’s lung function. This paper conducted an experiment with 10 participants to evaluate the system from two aspects: training effectiveness and user experience. The results show that this system has significantly improved the patient’s lung function. Compared with traditional training methods, the respiratory data are quantified and visualized, the rehabilitation training effect is better, and the training process is more active and interesting.
1. Introduction
With the rise of modern industrialized cities, fossil fuel emissions have also increased air pollution, seriously endangering the health of the respiratory system [1]. In China, the number of patients with chronic obstructive pulmonary disease (COPD) has exceeded 100 million, and is still on the rise, according to the “China Adult Lung Health Study” released in 2022. According to the World Health Organization, COPD is the third leading cause of death in the world [2]. So far, the global prevalence and mortality rates have further increased [3], seriously affecting patients’ daily travel problems [4], which shows that it is extremely harmful. As the number of COPD patients increases year by year, research on the prevention of respiratory diseases is particularly important.
The improvement of people’s awareness of prevention has led to a greater development of preventive science and rehabilitation, among which respiratory rehabilitation treatment is a branch of rehabilitation medicine. Respiratory rehabilitation application [5] refers to the use of active and effective respiratory exercise training to reduce the symptoms of patients’ dyspnea and improve the patient’s lung function, thereby improving the patient’s quality of life. Therefore, rehabilitation training for respiratory diseases is very necessary.
Conventional respiratory function training includes cough training, pursed-lip breathing, abdominal breathing, balloon breathing training, etc. [6]. Xiaoyan Liu [7] and others conducted pulmonary function training on patients with COPD through pursed-lip breathing and abdominal breathing training, which effectively improved the patients’ pulmonary function. Liu Guofang [8] used abdominal breathing training combined with balloon training in the treatment of patients with chronic persistent asthma, and Zheng Liping [9] used intensive cough breathing training for patients undergoing pulmonary drainage surgery, which significantly improved lung function and various physical conditions. Noman Sadiq [10] and others studied the problem of breathing exercise regulating heart rate variability and found that the breathing exercise of blowing a balloon enhanced lung function.
Through the analysis of the above studies, it is found that regular breathing training can improve the lung function and symptoms of dyspnea in people with breathing disorders. However, the breathing training process is monotonous and boring, and there are problems such as unquantified breathing data and poor feedback of breathing training results. The effect of the patient’s breathing training and the real-time breathing training data cannot be reflected in time.
With the development of virtual reality technology, people have introduced it into rehabilitation training. This study applies virtual reality technology combined with biofeedback to respiratory rehabilitation training to visualize respiratory training data and intuitively understand the effect of respiratory rehabilitation training. This system can not only improve users’ attention and enthusiasm for training, but also enable users to train efficiently and orderly through personal training tasks.
2. Related Work
2.1. Application of Virtual Reality Technology in Medical Field
With the development of virtual reality technology, virtual reality technology has penetrated into many medical fields. In the rehabilitation training of neuromotor injuries [11], the use of virtual reality scenes can provide patients with sensory experience and play an important role in their rehabilitation training. In psychotherapy [12], the use of virtual reality technology for mindfulness intervention can distract attention and reduce anxiety and stress. In respiratory rehabilitation training, KC Lan [13] studied multi-modal virtual reality for respiratory training, which improved the enthusiasm of patients for respiratory rehabilitation training. Colombo [14] and others summarized and analyzed the latest technology in the rehabilitation of COPD patients using virtual reality technology, which can distract patients from fatigue and dyspnea. Mitsea et al. [15] introduced a virtual slow breathing training system that provides immersive relaxation scenes to achieve a stable breathing rate. Irini Patsaki [16] applied VR rehabilitation training in the treatment of COPD patients to effectively increase the treatment effect. In rehabilitation training after musculoskeletal injuries [17], scholars have developed virtual reality-based rehabilitation training to help athletes recover from musculoskeletal injuries. In low vision rehabilitation [18], researchers summarized the application of virtual reality technology in visual field expansion and visual acuity improvement in the rehabilitation of low vision people, and found that virtual reality equipment can expand the visual field and improve visual acuity. In the rehabilitation training of children with autism [19], virtual reality technology has good effects in training language skills, life skills, and emotional expression. In the rehabilitation treatment of stroke patients [20], the designed virtual scene is used for rehabilitation treatment, so that the patient’s neuromotor system begins to recover its functions.
In the above research, virtual reality technology can provide an immersive virtual scene, using the advantages of the virtual scene to make the originally boring content lively and interesting, and improve the enthusiasm and participation of participants. In the process of rehabilitation training, the patient’s attention is improved, mental stress is relieved, and the effect of rehabilitation training is improved.
2.2. Biofeedback Technology
Biofeedback is the breathing data detected by sensors and fed back to the user in real time. It can observe one’s own breathing data in real time and improve the user’s behavior through feedback [21]. Biofeedback is also a form of stress reduction, providing physical and psychological comfort. Sebastian Rutkowski et al. [22] have shown that training parameters that provide feedback will increase patients’ motivation to actively achieve health. Zhou Lina [23] and others studied that stress reduction therapy combined with music biofeedback therapy can reduce patients’ negative emotions and improve their sleep quality. The combination of virtual reality technology and biofeedback has shown better results. The virtual reality game designed by Rakesh Patibanda [24] and others is combined with biofeedback. Changes in breathing rhythm drive the color changes of trees and the lushness of branches, thereby giving feedback to the patient’s own breathing status. Robert Greinacher [25] and others have significant effects on adjusting the user’s breathing rhythm through tactile and visual feedback of virtual scenes. Johannes Blum [26] and others proved that in VR-based breathing training, the feedback method of environmental biological changes has lower cost and better effectiveness in increasing breathing awareness and promoting diaphragmatic breathing.
Through the analysis of the above studies, it is found that biofeedback technology has been widely used in the field of medical rehabilitation. It increases the patient’s awareness of breathing, helps them assess their current breathing pattern, can improve the patient’s breathing pattern if necessary, and provides patient learning through sensory feedback stimulation. When biofeedback is combined with virtual reality technology, the effect of feedback will be more obvious and vivid, which can improve the effect of self-feeling during rehabilitation training. But so far, during rehabilitation training, most patients with virtual reality need to wear heavy physiological sensors. For patients who are physically inconvenient or recovering in hospital beds, there will be movement restrictions and physical burdens, which prevent them from fully achieving a high degree of immersion and easy and natural interaction [27].
3. System Architecture
In order to overcome the above obstacles, a biofeedback respiratory training rehabilitation system based on virtual reality technology is designed to improve the patient’s respiratory function and achieve visual biofeedback to obtain the patient’s own real-time respiratory training effects and data. The system is designed to be an intuitive and portable breathing training system that does not require expensive and heavy measurement sensors. A portable vital capacity sensor is used combined with HTC Vive pro2 VR equipment to form a respiratory rehabilitation training system that uses respiratory data to drive virtual scene changes. The respiratory training effect is presented in the form of visual feedback in biofeedback. This paper provides an overview of the designed respiratory rehabilitation training system and conducts an empirical evaluation of its experience and training effects.
3.1. System Framework Structure
This system is a set of rehabilitation training system built to simulate the real environment for the rehabilitation needs of patients with respiratory disorders. The system uses the virtual reality scene developed by Unity 3D as the core, and builds a scene processing system. Respiratory data are used as the input part of the training system, and the head-mounted display is used as the output part of the system data. Patients can be immersed in the virtual environment for respiratory rehabilitation training. The respiration data are collected through the respiration sensor, and the respiration data are sent to the PC and interacts with the virtual scene through the interactive processing unit. The spatial locator recognizes the position of the person through the handle controller and the sensor in the head-mounted display, and maps the recognition result to the virtual training scene to obtain the spatial position in the current virtual scene. Finally, the virtual scene is output through the head-mounted display, and the respiratory data are presented to the patient in the form of visual feedback. Finally, wecomplete the task of system design. The system framework structure is shown in Figure 1.
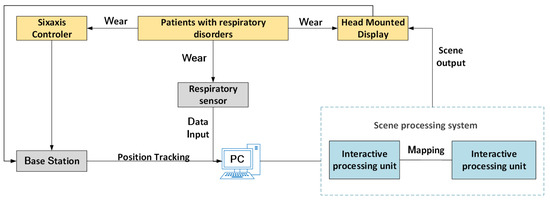
Figure 1.
System frame structure diagram.
3.2. Hardware Equipment
The VR device used in this study is HTC Vive pro2 device. HTC Vive pro2.0 equipment includes handle controller, head-mounted display, base station and HDMI equipment, as shown in Figure 2. The device is equipped with ultra-high resolution, allowing users to enjoy more delicate images in the virtual reality experience, while providing 3D spatial sound effects and an immersive sound experience, allowing users to better immerse themselves in virtual reality.

Figure 2.
HTC Vive pro2 device.
The HTC Vive pro2.0 device uses infrared tracking technology, which emits infrared rays from the base station transmitter and covers the entire room. Since the handle controller and the head-mounted display are equipped with a large number of sensors, the base station recognizes the sensors through infrared rays, so as to obtain the current external location of the handle controller and the head-mounted display. Data transmission and tracking technology are shown in Figure 3.
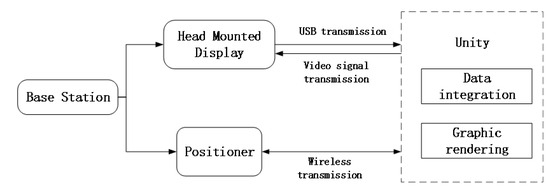
Figure 3.
Data transmission and tracking technology.
The respiratory data sensor used is the HKF-20C vital capacity sensor. The HKF-20C vital capacity sensor is a sensor used to measure vital capacity and respiratory function. It introduces the breathing gas of the measured person into the sensor through the breathing tube for analysis and calculation. The sensor will measure the flow rate, volume and time of the subject’s inhalation and exhalation, thereby calculating vital capacity, respiratory rate, breathing depth and other indicators. Figure 4 shows the HKF-20C vital capacity sensor.
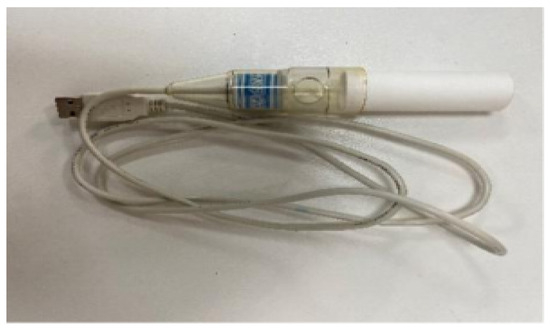
Figure 4.
HKF-20C vital capacity sensor.
The respiratory data sensor mainly collects respiratory signals and transmits the data to the PC in real time, which is used as a basis for judging the effect of rehabilitation training. The head-mounted display maps the virtual scene onto the display, providing patients with a realistic and immersive virtual environment. The hand controller serves as a controller in the virtual environment, performing functions such as selecting virtual scenes and moving virtual characters. The base station sets the size range of the real environment occupied by the virtual scene to standardize the movable range of breathing training. At the same time, the locator performs real-time data transmission with the head-mounted display and hand controller to track the user’s real-time location.
3.3. Interaction between Breathing Data and Virtual Scenes
Patients with respiratory disorders wear a respiratory data sensor and a head-mounted display to collect respiratory signals synchronously. At the same time, the respiratory data sensor will send the collected data to the PC, and then send the data to the training scene to interact with the training scene. Among them, various breathing training methods are built into the VR breathing training game scene. During the breathing interactive training process, patients can observe changes in the surrounding environment according to their own breathing rhythm. At the same time, the patient’s respiratory data will be detected, the respiratory information parameters will be calculated and the characteristic values of the respiratory airflow will be extracted to realize the visualization of the respiratory data. After the training is over, visual feedback is given to the patient in the form of quantification and visualization, which is conducive to discussing the shortcomings of their own breathing training, and improving it. The interaction between breathing data and virtual scenes is shown in Figure 5.
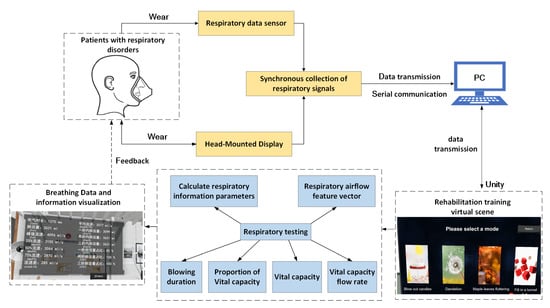
Figure 5.
Interaction between respiratory data and virtual scene.
3.4. Virtual Scene Design
Playful feedback relieves patient fatigue during training and prevents overly tedious therapy, which is crucial for long-lasting rehabilitation. This article designs a simple and interesting biofeedback virtual environment to meet the needs of people with different degrees of respiratory impairment. It provides users with training conditions for deep breathing and shallow breathing. Through approachable and easy-to-operate training scenarios, it makes user training operations convenient and concise. When developing the system, this article designed two virtual scenes of “blowing candles” or “blowing dandelions”, as shown in Figure 6 and Figure 7. After the system completes “blowing candles” or “blowing dandelions”, the data after breathing training is presented to the patient in the form of visual feedback to evaluate the training effect of the patient.
Figure 6.
Blowing out the candle scene.

Figure 7.
Blowing dandelion scene.
The “blow out candles” scene is designed based on the indoor environment. The scene includes tables, chairs, corridors, halls, bathrooms, furniture and other items. The user performs breathing training according to the voice prompt instructions, walks to the candle and blows on the candle. When the maximum forced respiratory volume (FVC) reaches the set threshold, the candle is extinguished.
The “Dandelion Blowing” scene is designed with the theme of a park, which contains a variety of trees, buildings, vegetation, rockeries, etc. Users can walk freely in the park. There are many dandelions in the grass. According to the task prompt, the user picks up the dandelions for breathing training, and blows on the dandelions after picking them up. When FVC reaches the set threshold, the dandelions are blown away, and the trained data is visually output. The system sets that the user needs to complete five breathing exercises to complete the task. At the same time, it is equipped with a voice prompt function, which can increase the fun and experience of the user.
3.5. Breathing Data Collection Interaction and Visualization
3.5.1. Respiratory Data Collection
The respiratory data are collected through the sensor, the data signal output of the vital capacity sensor is connected to the computer through the serial port, and the data are transmitted to the PC in the form of serial communication. First establish the communication format between the sensor and the scene-driven engine Unity3D, initialize the serial port, and configure the virtual serial port, baud rate, parity bit, data bit, and stop bit. Then, connect the disposable blowpipe to the sensor and hold the lower end of the sensor. After the preparation is completed, start to blow air. After blowing, data will be transmitted to the computer. When the breath stops or intermittent breath occurs during the blowing process, the sensor will determine that the data transmission has ended. At the same time, when collecting respiratory data, do not block the exhaust hole, otherwise it will affect the current vital capacity collection results. During use, avoid debris blocking the sensor’s internal detector, otherwise it will affect the accuracy of the sensor’s respiratory data collection.
3.5.2. Analysis of Respiratory Data
Functional data parsing enables the study of complex data and can be applied to observations of functions that vary on a continuum that appear in reality [28]. In order to realize the visualization and digitization of data, it is necessary to analyze the respiratory signal data and extract its eigenvalues. First, after the respiratory data are uploaded, the sensor will detect the respiratory data, and then the computer will analyze the respiratory data according to the communication protocol, so as to obtain the waveform data during the sensor testing process. From the extracted waveform data, the characteristic points, peaks, etc. of the signal can be observed. At the same time, the signal characteristic values are extracted and stored, and then the measurement parameters, namely breathing time, vital capacity, flow rate, etc., are output at a sampling frequency of 100 HZ. After the parsing is completed, the data characteristic value is returned to the array for storage. Algorithm 1 shows the respiratory data parsing algorithm.
First, the respiratory data collected are cached in the cache as a byte array. If the cache contains data, the contained data are traversed. When the start measurement command 0xc1 of the respiration sensor and the end command 0xf0 of the respiration sensor are detected, the data in the cache cache are sequentially imported into endData for storage. Secondly, the byte type number endData is converted into a hexadecimal, and the collected data contain 25 bytes, as shown in Table 1. Among them, the first 21 bits obtain the high and low bytes of each type of breathing data, and the size of each measured data type is the combination of high and low bytes. Therefore, when i < 22, take an even number to combine the high and low bits. Then, use the ToString(“X2”) function to convert it to a hexadecimal, and finally output 16 for the lungData collection of breathing data.
| Algorithm 1: Respiratory data analysis algorithm. |
Input: collected respiratory data collection “cache” Output: Hexadecimal respiratory data set “lungData” 1. if cache.Count!=0 then 2. for int i = cache.Count-1; i >= 0; i– do 3. if i! = 0 then 4. if cache[i] == 0xc1&&cache[i-1] == 0xf0 then 5. Array.Copy(cache.ToArray(),i + 1,endData,0,endData.Length) 6. isReceived = true 7. cache.Clear() 8. if isReceived then 9. for int i = 0; i < endData.Length; i++ do 10. if i < 22 &&i % 2 == 0 then 11. hex += endData[i].ToString(“X2”) 12. hex += endData[i + 1].ToString(“X2”) 13. lungData.data.Add(Explain(hex)) 14. else if i < 25 then 15. hex += endData[i].ToString(“X2”) 16. data.Add(Explain(hex)) 17. lungData.GetDetail() |

Table 1.
Twenty-five respiratory data type bytes.
3.5.3. Analysis of Respiratory Data
In the virtual scene, the trainee performs breathing training according to the instructions. When the FVC exceeds the set threshold (1000), the candle will go out. This is because the image waveform cannot intuitively and better reflect the size of the data change each time. Therefore, the data of each breathing training is analyzed. While the breathing data drives the scene changes, the analyzed data are called and the data are presented in a visual and digital form, so that the trainees can observe the data more clearly. Algorithm 2 shows the respiratory data interaction and visualization algorithm, and Figure 8 shows the visualization of respiratory data. The data types include the duration of insufflation (TIME), vital capacity (FVC), peak flow rate (FEF), flow rate at 25% vital capacity (MEF25), flow rate at 50% vital capacity (MEF50), and flow rate at 75% vital capacity (MEF75), flow velocity difference (FEF), 25–75% average flow velocity (PEF), vital capacity in the previous second (FEV1), vital capacity in the first two seconds (FEV2), vital capacity in the first three seconds (FEV3), vital capacity ratio in one second (V1F), vital capacity in two seconds (V2F) and vital capacity in three seconds (V3F).

Figure 8.
Respiration data visualization.
First, assign values to the fields, fill the data data before assigning values, and store 14 data collected by the breath sensor into data. When the vital capacity is greater than the set threshold of 1000 mL (data.fvc > 1000), since the fire of the candle and the fluff of the dandelion are special effects, item.Stop() will turn off their special effects, and will use SetActive to turn off their active status. Then, determine whether the virtual target Target of the breathing training is the same as the original one. If the target changes, that is, the candle goes out or the dandelion fluff blows away, use StartPort() to visually output the blowing data locally, as shown in Figure 8.
| Algorithm 2: Respiratory data interaction and visualization algorithm. |
1. if data.Count == 14 then 2. time = data[0],fvc = data[1],fef = data[2],mef25 = data[3],mef50 = data[4], mef75 = data[5],fef25–75 = data[6],pef25-75 = data[7],fev1 = data[8], fev2 = data[9],fev3 = data[10],v1f = data[11],v2f = data[12],v3f = data[13] 3. data.Clear() 4. if data.fvc > 1000 then 5. foreach var item in particle then 6. item.Stop() 7. item.transform.GetChild(0).gameObject.SetActive(false) 8. if Target ! = null then 9. if flag == false then 10. StartPort port = new StartPort() 11. byte[] data = GetData(port) 12. localClient.Send(data) 13. StartPort() 14. DebugMessage.Log() 15. Break |
4. Experiments and Results
4.1. Participants
In order to understand the effectiveness of the system, this paper recruited 10 volunteers to participate in the test, and at the same time equipped two staff members to instruct how to use the research system; then, we trained the participants, distributed the equipment and managed the results of breathing training. The participants were divided into two groups: the first group was the control group, and 5 participants were given routine breathing training, blowing out candles and dandelion breathing training. The second observation group, the remaining 5 participants, performed breathing training in the virtual scene designed in this paper. The diagnosis of COPD was made according to a set of criteria developed by the Global Initiative for Chronic Obstructive Lung Disease (GPLD) [29]. To determine whether a person’s airway is blocked, clinicians compare the amount of air a patient can exhale in one second, known as forced expiratory volume (FEV1), to the total amount of air they can exhale, known as forced vital capacity (FVC). According to GOLD, a person can be diagnosed with COPD if their ratio of FEV1 to FVC is below 0.7, which means that a person exhales less than 70 percent of the air in their lungs in one second [30].
To ensure the validity of the assessment of effect, excluding patients with other lung function, participants met the following criteria:
- Meet the diagnostic criteria for COPD;
- During the rehabilitation training period, there is no resistance to cooperate with training and other behaviors;
- Good compliance during rehabilitation training and tolerance during training.
Table 2 shows the participants’ information. Participant screening is based on the fact that COPD patients are mainly concentrated in middle-aged and elderly people, and the age distribution is between 55 and 65 years old. At the same time, the prevalence of COPD in men is more than twice that of women in the same age group [31]. In order to eliminate the interference of participants with other medical conditions on the experiment, participants with no other medical conditions and who were able to perform breathing training on their own were selected for the experiment.

Table 2.
Participant information.
4.2. Experimental Process
After each breathing session, each participant will receive a questionnaire to fill out regarding the training experience. This scale examines participants’ feelings about training through the following questions:
- During training, do you feel bored?
- During the training process, are you distracted and have trouble concentrating?
- During the training process, are you able to keep up with the training pace?
Each item in this experimental survey adopts a five-point Likert scale, with options ranging from 1 to 5, that is, strongly agree to strongly disagree. Each item is scored from 1 to 5 points, and the score is multiplied by the corresponding weight to obtain the final score, as shown in Table 3.

Table 3.
Experimental Training Feeling Scale.
4.3. Experimental Results and Analysis
During this respiratory rehabilitation training, the changes in respiratory data parameters of each participant before and after training were recorded to measure the effectiveness of the training system. The experiment found that the breathing training effect of each participant has improved. In this article, the breathing data of each participant before and after training are used as a measure of the effect of this experiment. At the same time, the mean values of the data before and after training for the two groups of participants were obtained for comparison.
Table 4 and Table 5 are the breathing data parameters before and after the rehabilitation training of the control group, and Table 6 and Table 7 are the breathing data parameters of the observation group before and after the rehabilitation training. Figure 9 and Figure 10 show the average breathing data of the control group before and after training, and Figure 11 and Figure 12 show the average breathing data of the observation group before and after training. Through Figure 9 and Figure 11, it can be found that the breathing data of the participants in the control group and the observation group have obvious changes before and after. Compared with the vital capacity and average flow rate in a short period of time, there are obvious improvements. The diagnosis of COPD patients is based on the ventilation volume in a short period of time, that is, the proportion of vital capacity in one second. From Figure 10 and Figure 12, it can be observed that the proportion of the vital capacity of the participants in the first second after training was significantly improved. It shows that both the traditional breathing training and the research system have significantly improved the respiratory function of the lungs of COPD patients. However, the flow rate (MEF75) at 75% vital capacity of the two groups of participants decreased to varying degrees. From Table 4, Table 5, Table 6 and Table 7, it can be observed that the MEF75 of individual participants decreased to varying degrees, because the sensor collected breathing data. The participants have insufficient strength, and the equipment produces corresponding noise and heat loss. In the later research, the respiratory data collection process and rehabilitation training process will be improved and optimized to improve the accuracy of the data.

Table 4.
The breathing data of the participants in the control group before training.

Table 5.
Breathing data of participants in the control group after training.

Table 6.
Respiration data of participants in the observation group before training.

Table 7.
Respiration data of participants in the observation group after training.
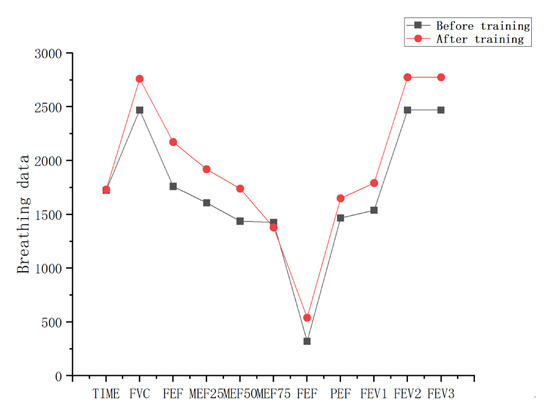
Figure 9.
Average respiratory data before and after training in the control group.
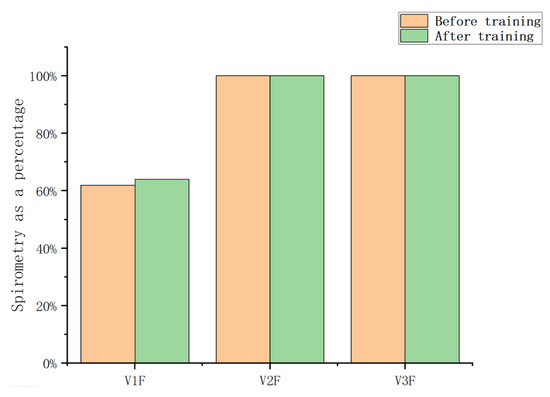
Figure 10.
Average vital capacity ratio before and after training in the control group.
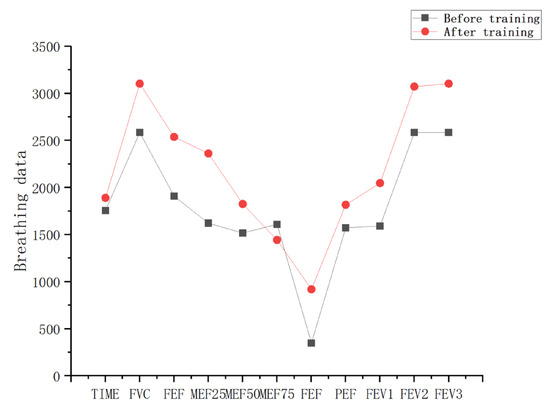
Figure 11.
Average respiratory data of the observation group before and after training.
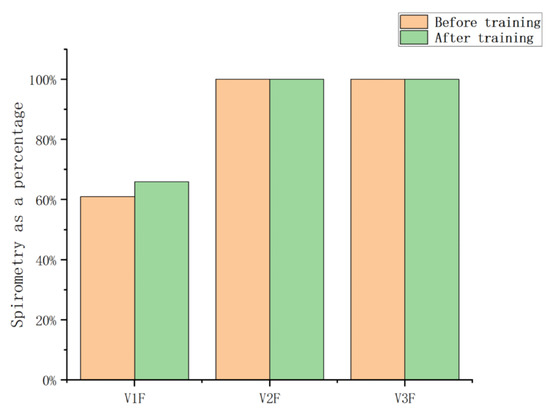
Figure 12.
The average vital capacity ratio of the observation group before and after training.
It is observed in Table 4 and Table 5 that the vital capacity in the first second of all patients is low, but the vital capacity in the second and third seconds is high. This is because diseases such as pulmonary obstruction, emphysema, asthma, etc., can cause airway obstruction, making the lungs unable to exhale the full lung capacity in the first second. However, over time, lung capacity gradually increases in the second and third seconds, and the patient tries to expel as much gas as possible by increasing their breathing rate or changing their breathing pattern.
By observing Figure 13 and Figure 14, it is found that the training effect of the control group is significantly lower than that of the observation group. At the same time, the first-second vital capacity of the observation group increased by 5% compared with that before training, while the first-second vital capacity of the control group increased by 2% compared with that before training. It can be observed that the respiratory rehabilitation training of this research system is superior to the traditional respiratory rehabilitation training.
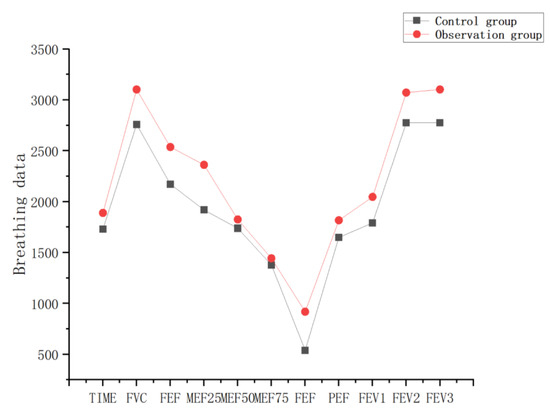
Figure 13.
Respiration data before and after training of the control group and observation group.
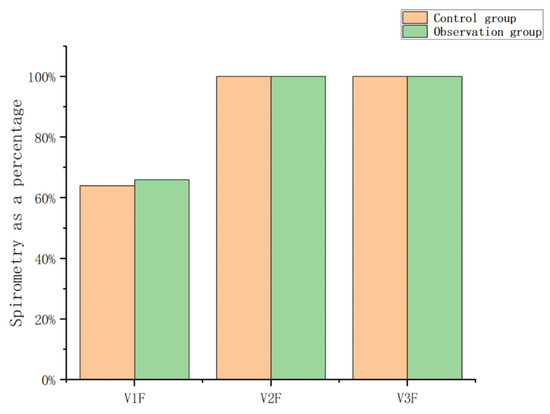
Figure 14.
The ratio of lung capacity before and after training in the control group and the observation group.
This experiment statistically summarizes the feelings of each participant during the training process, as shown in Figure 15, Figure 16 and Figure 17. From the figure, it can be observed that the observation group had high scores for feeling bored and bored after the first week of training, and low scores for inattention and ability to keep up with the rhythm, which may be caused by unfamiliarity with the system for the first time. Over the next few weeks, as the user mastered the use of the system, the scores for feelings of boredom also decreased, while the scores for feelings of lack of concentration and failure to keep up with the rhythm also gradually increased. In the control group, after the first week of training, the feeling of boredom was relatively low, and the scores of inattention and inability to keep up with the rhythm were higher. As the training progressed, the feeling of boredom increased during training, resulting in inattention and so on. This leads to an increase in the feeling score of boredom and a gradual decrease in the feeling score of the lack of concentration. On the whole, as the experiment progresses, this research system has a better sense of experience and provides users with a higher sense of immersion, participation and fun.
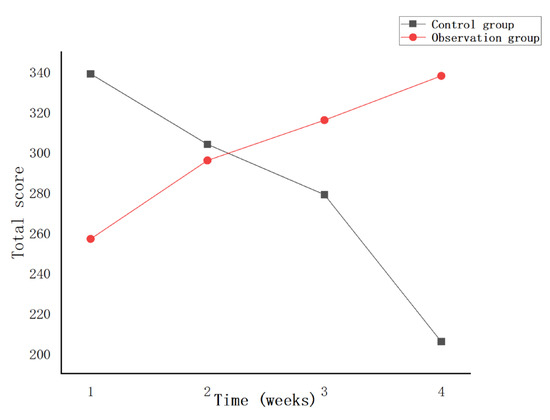
Figure 15.
Total score of boredom per week.
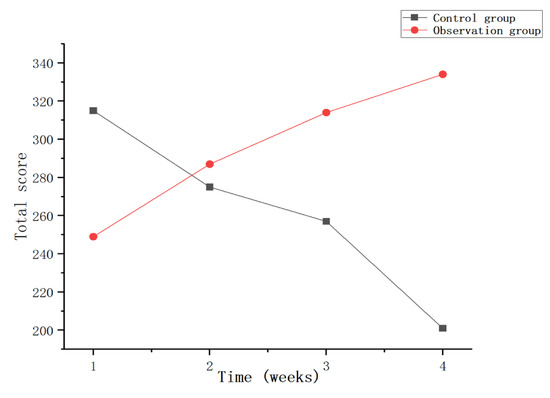
Figure 16.
Total Weekly Inattention Scores.
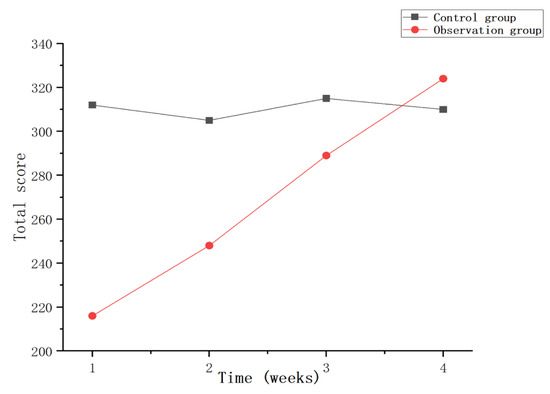
Figure 17.
Total score for failing to keep up with the rhythm every week.
5. Conclusions
Traditional rehabilitation training lacks clear breathing data, and the training process is very tedious. In contrast, this article studies a biofeedback respiratory rehabilitation training system based on virtual reality technology, which reflects the interaction between respiratory data and virtual scenes during the rehabilitation training process, and realizes the quantification and visualization of respiratory data. At the same time, the effect of the user’s rehabilitation training is improved, and the enthusiasm and interest of the user are increased.
The purpose of this research system is to improve the lung function of patients with respiratory disorders and relieve symptoms such as dyspnea. Through VR equipment and respiratory data sensors, the interactive virtual scene of human breathing in the form of biofeedback is realized. We perform data analysis on the respiratory data, use the respiratory data to drive changes in the virtual scene, and realize the interaction between the respiratory data and the virtual scene. We use data visualization algorithms to quantify and visualize respiratory data to evaluate the effectiveness of patient breathing training. In the virtual scene of breathing training, interesting ways such as music and stories are used to guide patients to continuously perform breathing training in a comfortable process, so as to complete specific rehabilitation training tasks and goals. The system is evaluated from two aspects, including training effectiveness and user experience. Comparing the experimental results and experiences of 10 participants, the results show that compared with traditional respiratory rehabilitation training, this research system has better training effects and experience, and rehabilitation training is more positive.
The system enables patients with respiratory disorders to improve their respiratory function by completing training tasks in a virtual scene. It is easy to operate and has no restrictions on site and usage time, making it possible to incorporate it into a long-term pulmonary rehabilitation plan. Due to the interference of respiratory equipment in the process of respiratory data transmission, certain Gaussian white noise and random noise will be generated. The focus of follow-up research is to further improve and perfect the respiratory data collection and improve the accuracy of respiratory data transmission.
Author Contributions
Conceptualization, F.L.; Methodology, F.L.; Software, F.L. and Y.L.; Validation, F.L.; Resources, R.W.; Data curation, J.Z. (Jing Zhang); Writing—original draft preparation, F.L.; Writing—review and editing, L.S. and J.Z. (Jian Zhao); Visualization, Z.Z.; Project administration, L.S. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported in part by the Jilin Provincial Department of Science and Technology (Grant/Award Number: No. YDZJ202301ZYTS496), Jilin Provincial Department of Human Resources and Social Security (2022QN05), and The Education Department of Jilin Province (No. JJKH20230673KJ).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Annesi-Maesano, I.; Forastiere, F.; Balmes, J.; Garcia, E.; Harkema, J.; Holgate, S.; Kelly, F.; Khreis, H.; Hoffmann, B.; Maesano, C.N.; et al. The clear and persistent impact of air pollution on chronic respiratory diseases: A call for interventions. Eur. Respir. J. 2021, 57, 2002981. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez Villegas, C.; Paz-Zulueta, M.; Herrero-Montes, M.; Parás-Bravo, P.; Madrazo Pérez, M. Cost analysis of chronic obstructive pulmonary disease (COPD): A systematic review. Health Econ. Rev. 2021, 11, 31. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Li, P.; Li, N.; Wang, Z.; Li, J.; Liu, X.; Wu, W. Effects of home-based breathing exercises in subjects with COPD. Respir. Care 2020, 65, 377–387. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.-Y.; Meijer, K.; Delbressine, J.M.; Willems, P.J.; Wouters, E.F.M. Spruit MA.Effects of Pulmonary Rehabilitation on Gait Characteristics in Patients with COPD. J. Clin. Med. 2019, 8, 459. [Google Scholar] [CrossRef]
- Respiratory Disease Branch of Chinese Geriatrics Society, Respiratory Rehabilitation Professional Committee of China Rehabilitation Medical Institutions Alliance. Chinese expert consensus on the application of inhalation therapy in respiratory rehabilitation. Chin. J. Tuberc. Respir. Med. 2022, 45, 753–761. [Google Scholar]
- Fen, D.; Ling, Y.; Lu, Z.; Lan, H. Respiratory function exercise for patients with frailty and pulmonary heart disease. Chin. J. Lung Dis. Electron. Vers. 2020, 13, 429–431. [Google Scholar]
- Liu, X.; Wang, J.; Sun, J.; Pan, K.; Wu, K.; Sun, C.; Ma, H. Effects of respiratory function exercise combined with psychological nursing on cardiopulmonary function index, exercise tolerance, and quality of life in patients with stable chronic obstructive pulmonary. Int. J. Early Child. Spec. Educ. INT-JECSE 2021, 30, 138–148. [Google Scholar]
- Liu, G. Application of abdominal breathing training + balloon blowing in rehabilitation care of patients with chronic persistent asthma. Heilongjiang Med. 2022, 46, 2518–2520. [Google Scholar]
- Zheng, L. Effect of intensive cough and respiratory function training on pulmonary rehabilitation in adult patients with spontaneous pneumothorax undergoing closed drainage. Tibet. Med. 2022, 43, 108–110. [Google Scholar]
- Sadiq, N.; Sadiq, T.; Baloch, W.A.; Khan, H.F.; Rajpoot, N.N.; Ali, S. Modulation of Heart Rate Variability in Stressed Medical Students Via Breathing Exercise. Pak. J. Med. Health Sci. 2023, 17, 117. [Google Scholar] [CrossRef]
- Bortone, I.; Leonardis, D.; Mastronicola, N.; Crecchi, A.; Bonfiglio, L.; Procopio, C.; Solazzi, M.; Frisoli, A. Wearable haptics and immersive virtual reality rehabilitation training in children with neuromotor impairments. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 1469–1478. [Google Scholar] [CrossRef] [PubMed]
- Chandrasiri, A.; Collett, J.; Fassbender, E.; De Foe, A. A virtual reality approach to mindfulness skills training. Virtual Real. 2020, 24, 143–149. [Google Scholar] [CrossRef]
- Lan, K.C.; Li, C.W.; Cheung, Y. Slow breathing exercise with multimodal virtual reality: A feasibility study. Sensors 2021, 21, 5462. [Google Scholar] [CrossRef]
- Colombo, V.; Aliverti, A.; Sacco, M. Virtual reality for COPD rehabilitation: A technological perspective. Pulmonology 2022, 28, 119–133. [Google Scholar]
- Mitsea, E.; Drigas, A.; Skianis, C. Breathing, Attention & Consciousness in Sync: The role of Breathing Training, Metacognition & Virtual Reality. Technium Soc. Sci. J. 2022, 29, 79. [Google Scholar]
- Patsaki, I.; Avgeri, V.; Rigoulia, T.; Zekis, T.; Koumantakis, G.A.; Grammatopoulou, E. Benefits from Incorporating Virtual Reality in Pulmonary Rehabilitation of COPD Patients: A Systematic Review and Meta-Analysis. Adv. Respir. Med. 2023, 91, 324–336. [Google Scholar] [CrossRef]
- Gouveia, É.R.; Campos, P.; França, C.S.; Rodrigues, L.M.; Martins, F.; França, C.; Gonçalves, F.; Teixeira, F.; Ihle, A.; Gouveia, B.R. Virtual Reality Gaming in Rehabilitation after Musculoskeletal Injury—User Experience Pilot Study. Appl. Sci. 2023, 13, 2523. [Google Scholar] [CrossRef]
- Pur, D.R.; Lee-Wing, N.; Bona, M.D. The use of augmented reality and virtual reality for visual field expansion and visual acuity improvement in low vision rehabilitation: A systematic review. Graefe’s Arch. Clin. Exp. Ophthalmol. 2023, 261, 1743–1755. [Google Scholar] [CrossRef]
- Si, T.; Zhu, Y.; Zongni, L. Application and Prospect of Immersive Virtual Reality Technology in Rehabilitation Practice of Autistic Children. Appl. Educ. Psychol. 2022, 3, 59–67. [Google Scholar]
- Ciorap, R.; Andriţoi, D.; Casuţă, A.; Ciorap, M.; Munteanu, D. Game-based virtual reality solution for post-stroke balance rehabilitation. IOP Conf. Ser. Mater. Sci. Eng. 2022, 1254, 012037. [Google Scholar]
- Rockstroh, C.; Blum, J.; Göritz, A.S. A mobile VR-based respiratory biofeedback game to foster diaphragmatic breathing. Virtual Real. 2021, 25, 539–552. [Google Scholar]
- Rutkowski, S.; Buekers, J.; Rutkowska, A.; Cieślik, B.; Szczegielniak, J. Monitoring physical activity with a wearable sensor in patients with copd during in-hospital pulmonary rehabilitation program: A pilot study. Sensors 2021, 21, 2742. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Zhou, Z.; Wu, Y.; Zhang, M. Application of mindfulness-based stress reduction therapy combined with music biofeedback therapy in infertile patients. Qilu Nurs. Mag. 2022, 28, 16–19. [Google Scholar]
- Patibanda, R.; Mueller, F.F.; Leskovsek, M.; Duckworth, J. Life Tree: Understanding the Design of Breathing Exercise Games. In Proceedings of the CHI PLAY ’17: The Annual Symposium on Computer-Human Interaction in Play, Amsterdam, The Netherlands, 15–18 October 2017; pp. 19–31. [Google Scholar]
- Greinacher, R.; Kojić, T.; Meier, L.; Parameshappa, R.G.; Möller, S.; Voigt-Antons, J.N. Impact of Tactile and Visual Feedback on Breathing Rhythm and User Experience in VR Exergaming. In Proceedings of the 2020 Twelfth International Conference on Quality of Multimedia Experience (QoMEX), Athlone, Ireland, 26–28 May 2020. [Google Scholar]
- Blum, J.; Rockstroh, C.; Göritz, A.S. Development and pilot test of a virtual reality respiratory biofeedback approach. Appl. Psychophysiol. Biofeedback 2020, 45, 153–163. [Google Scholar]
- Ji, W. Research on Interactive Design of Virtual Reality (VR) Animation; Central Academy of Fine Arts: Beijing, China, 2017. [Google Scholar]
- LoMauro, A.; Colli, A.; Colombo, L.; Aliverti, A. Breathing patterns recognition: A functional data analysis approach. Comput. Methods Programs Biomed. 2022, 217, 106670. [Google Scholar] [CrossRef]
- Keener, A. Redefining the diagnostic criteria for COPD. Nature 2020, 581, S4. [Google Scholar] [CrossRef]
- Agustí, A.; Celli, B.R.; Criner, G.J.; Halpin, D.; Anzueto, A.; Barnes, P.; Bourbeau, J.; Han, M.K.; Martinez, F.J.; de Oca, M.M.; et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Am. J. Respir. Crit. Care Med. 2023, 207, 819–837. [Google Scholar] [CrossRef]
- Adeloye, D.; Song, P.; Zhu, Y.; Campbell, H.; Sheikh, A.; Rudan, I.; NIHR RESPIRE Global Respiratory Health Unit. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: A systematic review and modelling analysis. Lancet Respir. Med. 2022, 10, 447–458. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).