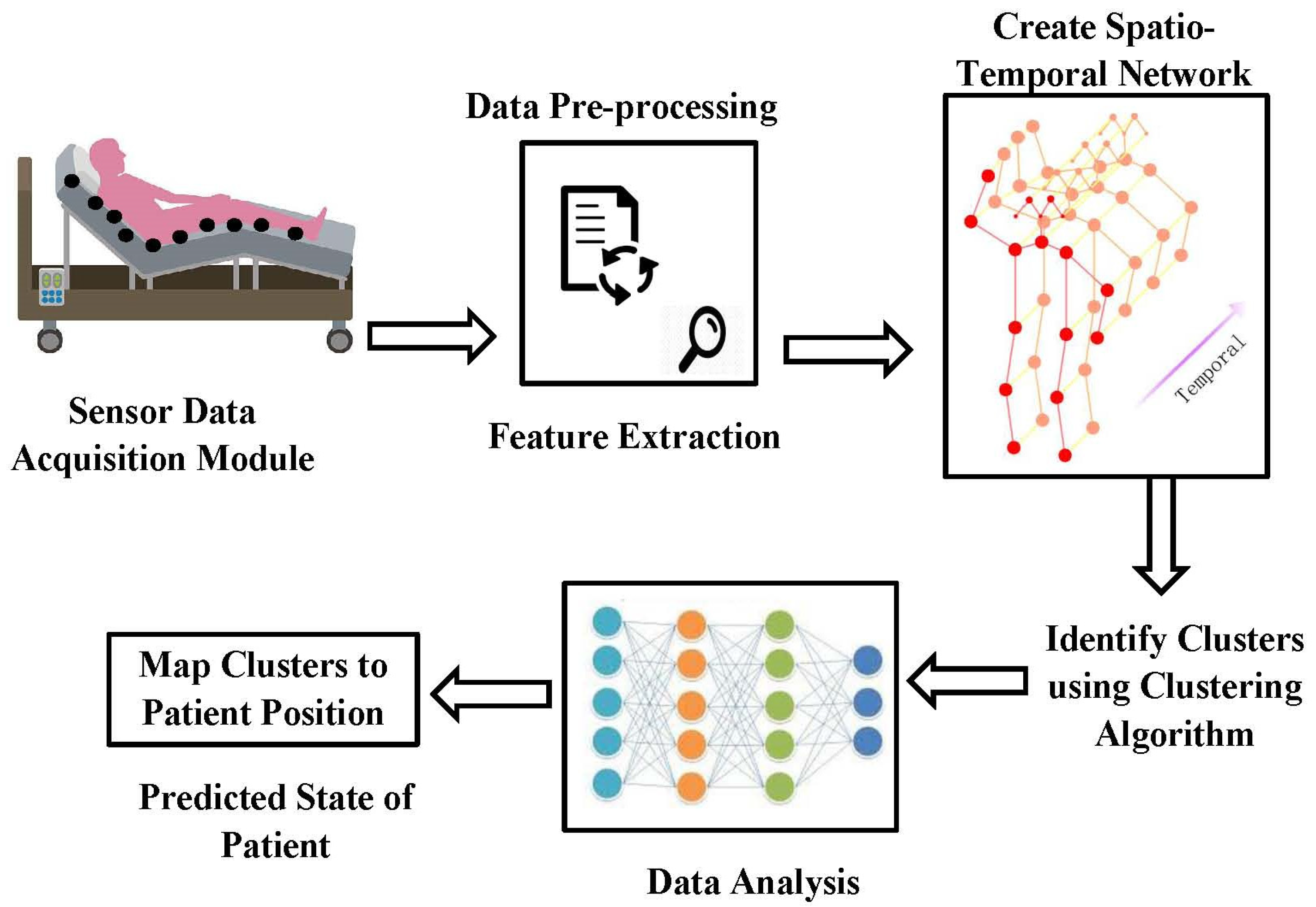
Spatio-Temporal Cluster Mapping System in Smart Beds for Patient Monitoring
Abstract
1. Introduction
2. Bed Regions and Event Logs
2.1. Modeling Smart Bed Parameters from Behaviour Record Logs
2.1.1. Pseudocode 1: Pseudocode for Handling Pressure Sensor Data by Network Cluster
2.1.2. Pseudocode 2: Pseudocode for Handling (from Infrared Sensor, Motion Sensor, Weight Sensor, Bed Exit Sensor, Breathing Rate Sensor and Heart Rate Sensor) Data by Network Cluster
2.1.3. Pesudocode 3: For Cloud Data Storage
- A.
- Extraction of Features from the Behavior Logs
- B.
- Spatial-Temporal Clustering
| Algorithm 1: Algorithm for the proposed spatio temporal clustering |
| Input: First phase place vector |
| Output: Output clusters in the second phase clustering (in this work it is limited to 5). |
- ●
- Let stand for the cluster that includes a place vector , and let stand for the place vector at time .
- ●
- The time series of location vectors and is then translated into a time series of clusters and , and finally into a time series of two.
- ●
- Each interval on the timeline has a length, which is a predetermined parameter.
- ●
- Each time period of length is further broken down into subintervals, where is likewise a predetermined integer.
- ●
- At the outer interval, we obtain the time series of the following n clusters: Be aware that some of the clusters in this series could be repeated.
- ●
- According to the definition, if denotes which is the first cluster in the next interval.
- ●
- A change from to in the time series is represented by an edge from node to . The number of these transitions is counted by the function .
- ●
- The total of the edge weights is the same amount for whatever duration of time. The graphs are normalized in this way. On the other hand, the number of nodes could vary. Note that most edges form self-loops in situations with little movement.
- C.
- Cluster to Situation Mapping
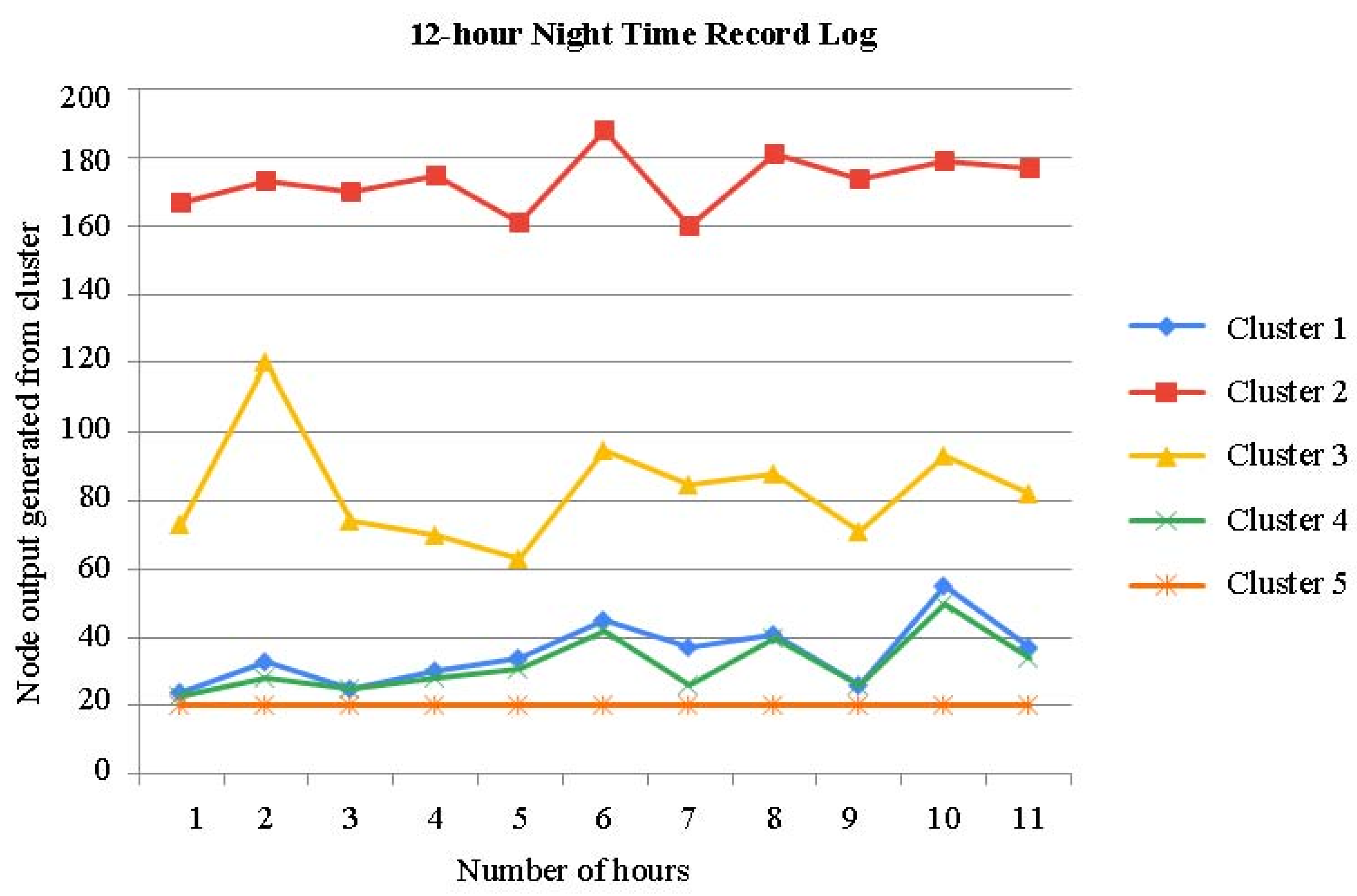
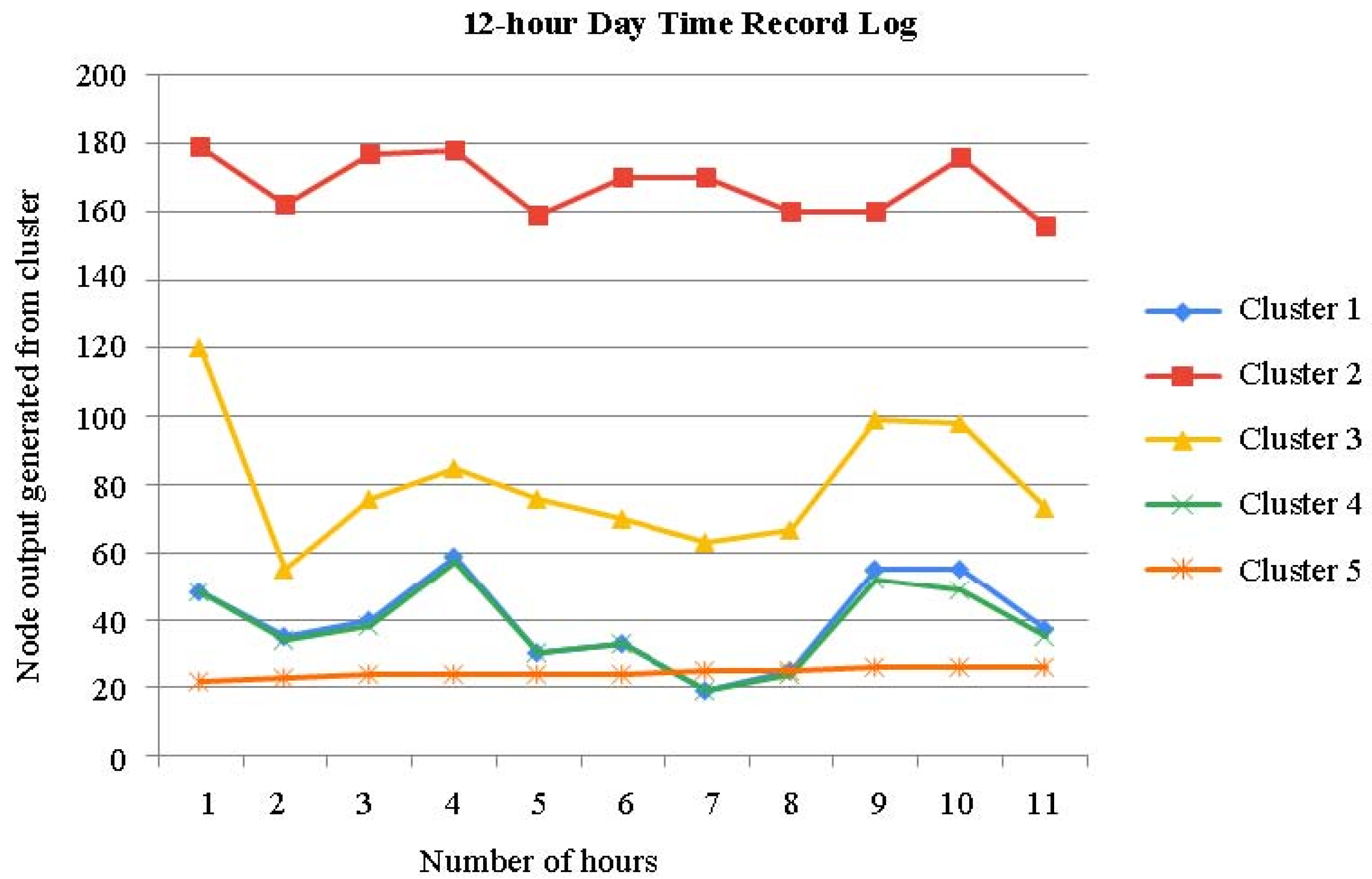
3. Record Logs Data Analytics
Cluster Strategy
- ●
- We utilize the usage logs for three days. There are six behavior logs in total each day.
- ●
- There are now six nodes employed across all of the use logs.
- ●
- Eight clusters will be used in the initial round of clustering.
- ●
- The graph building step’s time interval length and number of sub-intervals are both set to 200 s and 10, respectively.
- ●
- Five clusters will be used in the second step of clustering.
- A.
- Initial stage Clustering
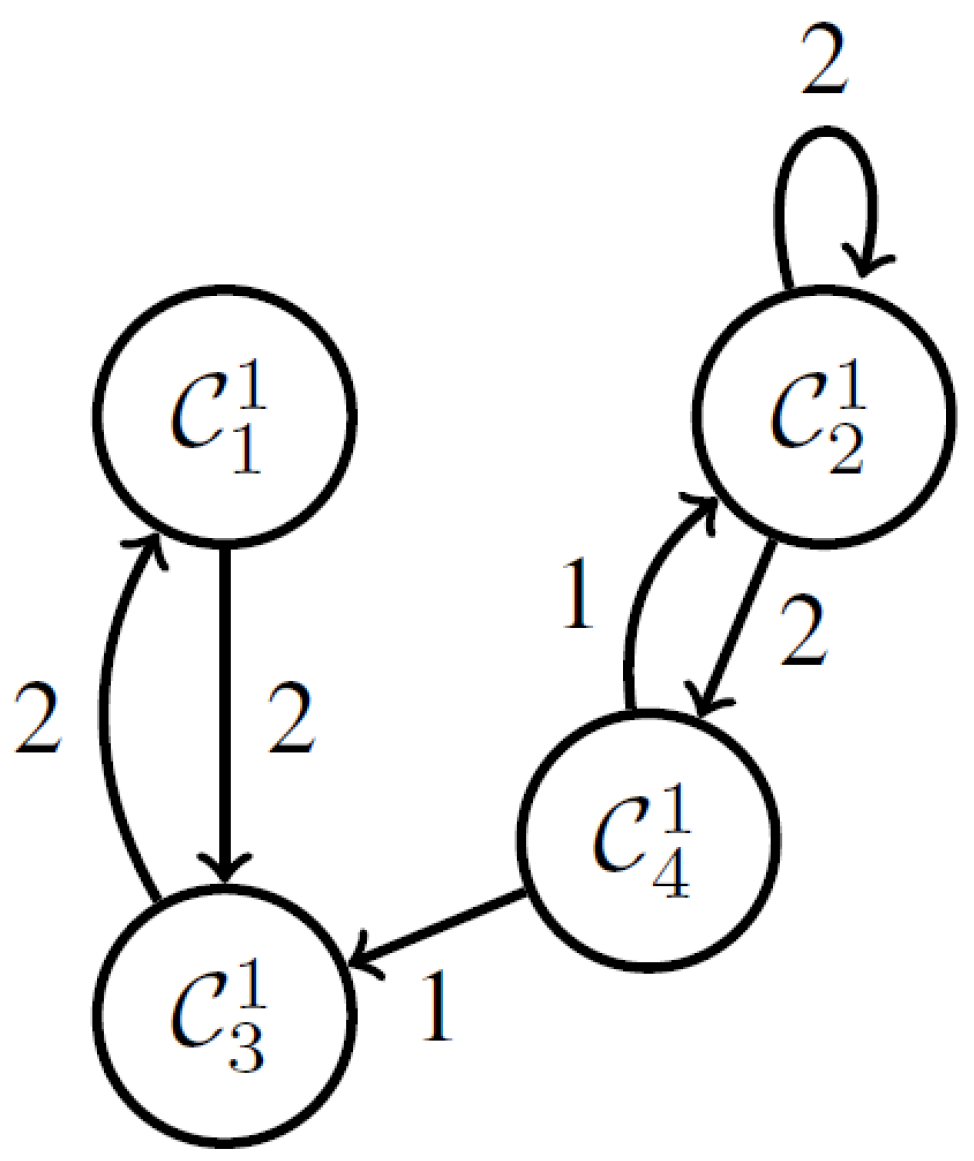
- B.
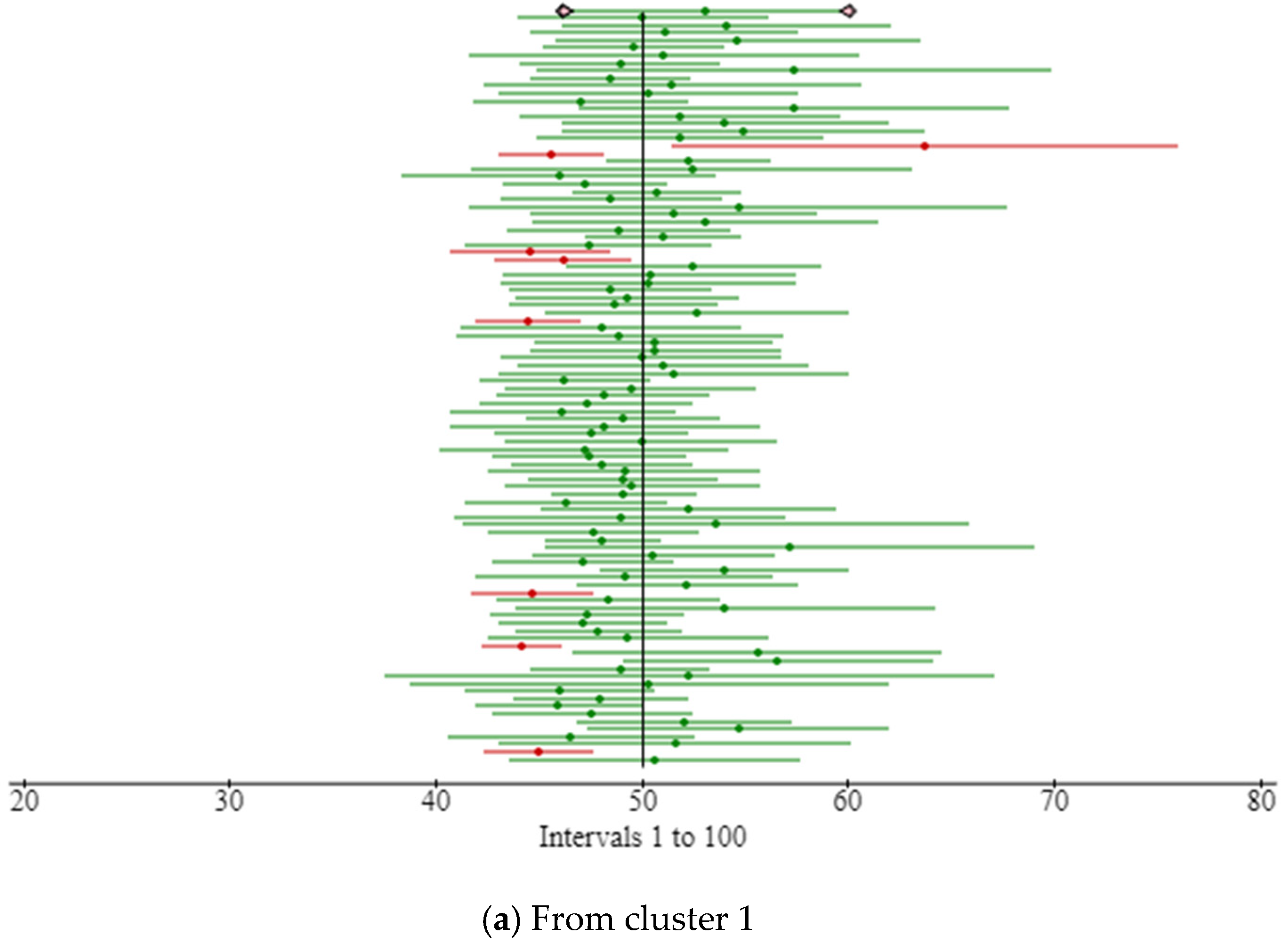
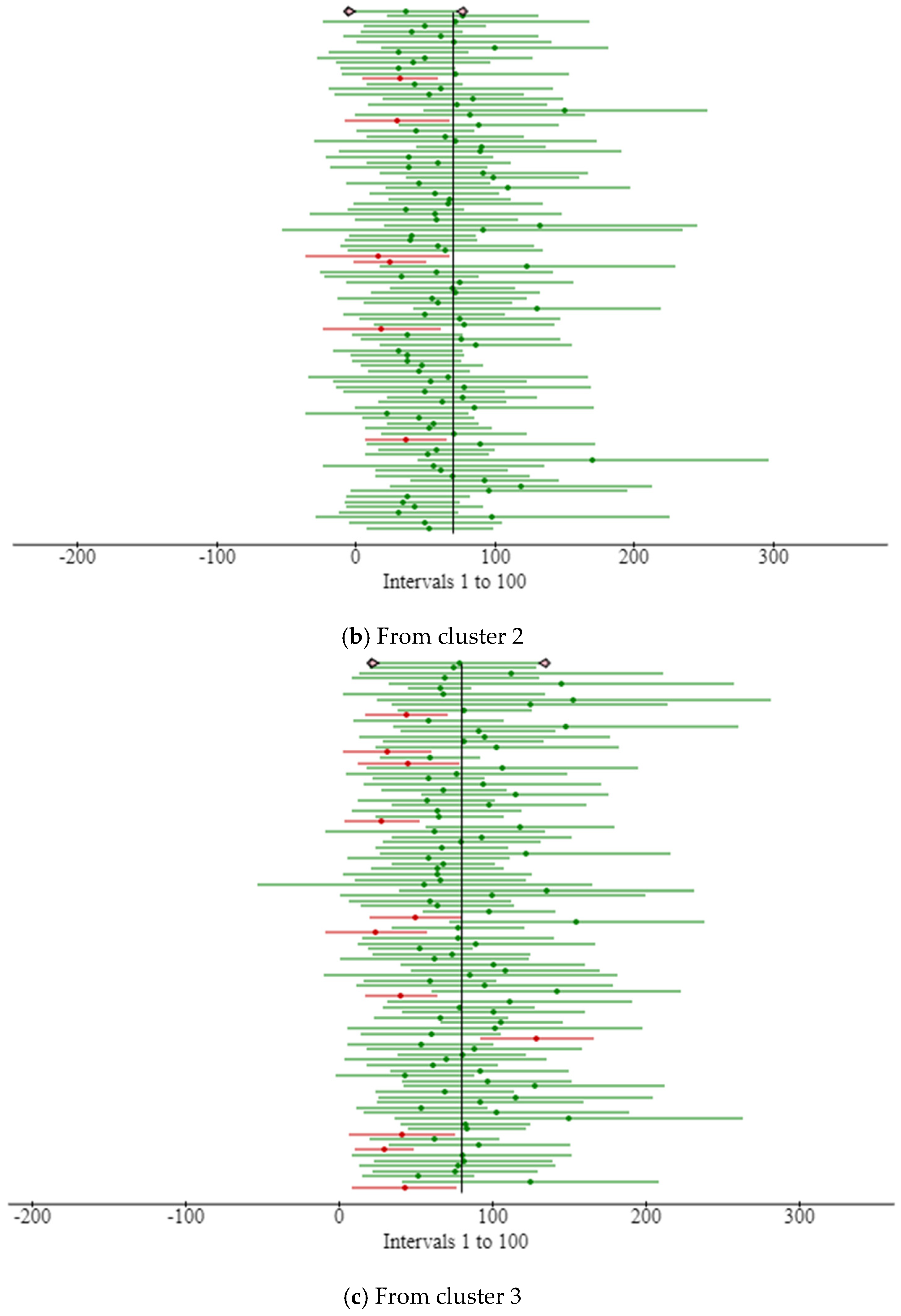
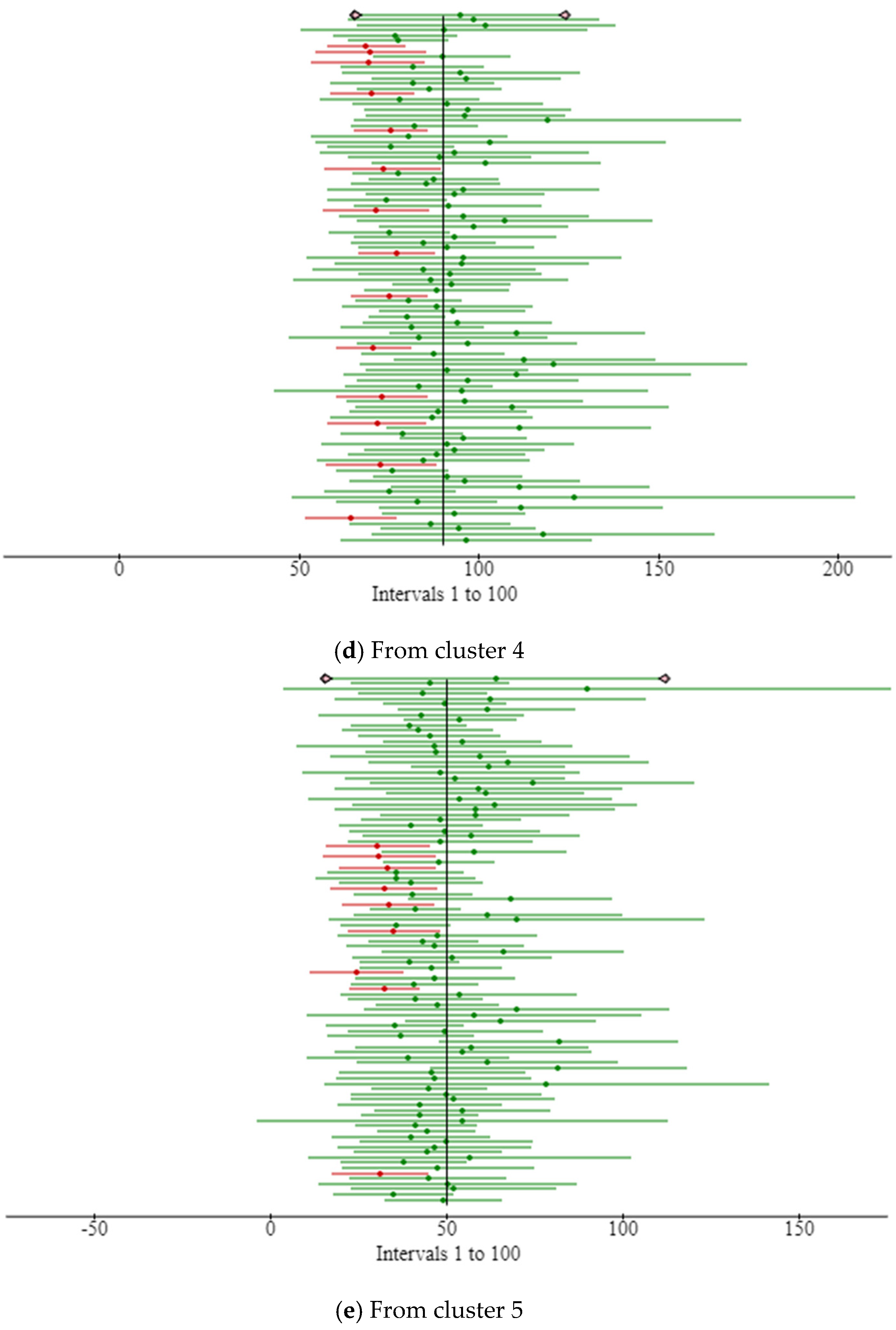
- Phase two Clustering
- ●
- : The graphs are made up of self-loops from and .
- ●
- : Graphs are mostly made of self-loops from
- ●
- Graphs in are mostly made up of self-loops from .
- ●
- : Self-loops from make up the majority of the graphs.
- ●
- Graphs in are mostly made up of self-loops from .
- C.
- Cluster to Situation Mapping
- ●
- : This cluster often manifests around the start of the movement. Because this cluster incorporates four distinct clusters from the first phase of clustering, it may regularly relocate to new locations.
- ●
- : During morning and night, this cluster often manifests. Areas 7 and 8 are divided equally; however, region 8 has a larger population than area 7.
- ●
- : This cluster depicts a scenario where Area 8 has maximum movement.
- ●
- : The first part of the morning and night is when this cluster often manifests. Areas 7 and 8 are divided equally.
- ●
- : This cluster often manifests at the conclusion of the night.
4. Results and Discussion
Validation of Record Logs Behaviors
5. Conclusions and Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ahmed, E.; Yaqoob, I.; Hashem, I.A.T.; Khan, I.; Ahmed, A.I.A.; Imran, M.; Vasilakos, A.V. The role of big data analytics in Internet of Things. Comput. Networks 2017, 129, 459–471. [Google Scholar] [CrossRef]
- Khaleeq, H.; Abou-Elnour, A.; Tarique, M. A Reliable Wireless System for Water Quality Monitoring and Level Control. Netw. Protoc. Algorithms 2016, 8, 1–14. [Google Scholar] [CrossRef]
- Garcia, M.; Martinez, C.; Tomas, J.; Lloret, J. Wireless Sensors Self-Location in an Indoor WLAN Environment. In Proceedings of the 2007 International Conference on Sensor Technologies and Applications (SENSORCOMM 2007), Valencia, Spain, 14–20 October 2017; pp. 146–151. [Google Scholar] [CrossRef]
- Lloret, J.; Macías, E.; Suárez, A.; Lacuesta, R. Ubiquitous Monitoring of Electrical Household Appliances. Sensors 2012, 12, 15159–15191. [Google Scholar] [CrossRef]
- Mieronkoski, R.; Azimi, I.; Rahmani, A.M.; Aantaa, R.; Terävä, V.; Liljeberg, P.; Salanterä, S. The Internet of Things for basic nursing care—A scoping review. Int. J. Nurs. Stud. 2017, 69, 78–90. [Google Scholar] [CrossRef] [PubMed]
- Hossin, M.Z. From habitual sleep hours to morbidity and mortality: Existing evidence, potential mechanisms, and future agenda. Sleep Health 2016, 2, 146–153. [Google Scholar] [CrossRef]
- Shin, D.-H.; Biocca, F. Health experience model of personal informatics: The case of a quantified self. Comput. Hum. Behav. 2017, 69, 62–74. [Google Scholar] [CrossRef]
- Liu, J.J.; Xu, W.; Huang, M.-C.; Alshurafa, N.; Sarrafzadeh, M.; Raut, N.; Yadegar, B. Sleep posture analysis using a dense pressure sensitive bedsheet. Pervasive Mob. Comput. 2014, 10, 34–50. [Google Scholar] [CrossRef]
- Wong, T.-S.; Wong, S.-K.; Leung, L.W.-C. Sleep-Posture Sensing and Monitoring System. U.S. Patent 8 803 682 B2, 12 August 2014. [Google Scholar]
- Royal, A.; John, D.; Bharti, O.; Tanwar, R.; Bhagat, D.K.; Padmawati, R.S.; Chaudhary, V.; Umapathi, R.; Bhadola, P.; Utarini, A. A Cost-Effectiveness Analysis of Pre-Exposure Prophylaxis to Avert Rabies Deaths in School-Aged Children in India. Vaccines 2023, 11, 88. [Google Scholar] [CrossRef] [PubMed]
- Shamayleh, A.; Awad, M.; Farhat, J. IoMT based predictive maintenance management of medical equipment. J. Med. Syst. 2020, 44, 1–12. [Google Scholar] [CrossRef]
- Cui, M.; Baek, S.S.; Crespo, R.G.; Premalatha, R. Internet of things-based cloud computing platform for analyzing the physical health condition. Technol. Health Care 2021, 29, 1233–1247. [Google Scholar] [CrossRef]
- Wang, Y.; Kung, L.; Wang, W.Y.C.; Cegielski, C.G. An integrated big data analytics-enabled transformation model: Application to health care. Inf. Manag. 2018, 55, 64–79. [Google Scholar] [CrossRef]
- Muthu, B.; Sivaparthipan, C.B.; Manogaran, G.; Sundarasekar, R.; Kadry, S.; Shanthini, A.; Dasel, A. IOT based wearable sensor for diseases prediction and symptom analysis in healthcare sector. Peer-to-Peer Netw. Appl. 2020, 13, 2123–2134. [Google Scholar] [CrossRef]
- Uchihira, N.; Choe, S.; Hiraishi, K.; Torii, K.; Chino, T.; Hirabayashi, Y.; Sugihara, T. Collaboration management by smart voice messaging for physical and adaptive intelligent services. In Proceedings of the 2013 PICMET’13: Technology Management in the IT-Driven Services (PICMET), San Jose, CA, USA, 28 July–1 August 2013; pp. 251–258. [Google Scholar]
- Hiraishi, K.; Kobayashi, K.; Choe, S.; Uchihira, N. Behavior modeling in physical and adaptive intelligent services. In Proceedings of the 2014 IEEE International Inter-Disciplinary Conference on Cognitive Methods in Situation Awareness and Decision Support (CogSIMA), San Antonio, TX, USA, 2–5 March 2014; pp. 244–249. [Google Scholar] [CrossRef]
- Wang, Y.; Kung, L.; Byrd, T.A. Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technol. Forecast. Soc. Chang. 2018, 126, 3–13. [Google Scholar] [CrossRef]
- Hirabayashi, Y.; Uchihira, N.; Torii, K.; Ikawa, Y. Verification of effectiveness of the nursing-care service space visualization and evaluation system: Field experiment aiming to improve nursing-care services. In Proceedings of the 2013 PICMET’13: Technology Management in the IT-Driven Services (PICMET), San Jose, CA, USA, 28 July–1 August 2013; pp. 1567–1571. [Google Scholar]
- Hiraishi, K.; Kobayashi, K. Detection of Unusual Human Activities Based on Behavior Modeling. IFAC Proc. Vol. 2014, 47, 182–187. [Google Scholar] [CrossRef]
- Gupta, M.; Gao, J.; Aggarwal, C.C.; Han, J. Outlier Detection for Temporal Data: A Survey. IEEE Trans. Knowl. Data Eng. 2013, 26, 2250–2267. [Google Scholar] [CrossRef]
- Chandola, V.; Banerjee, A.; Kumar, V. Anomaly detection: A survey. ACM Comput. Surv. 2009, 41, 1–22. [Google Scholar] [CrossRef]
- Mica, R. Endsley, Design for Situation Awareness: An Approach to User-Centered Design, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar]
- Sato, K.; Kobayashi, K.; Hiraishi, K. Situation recognition from behavior logs in caregiving services. In ITC-CSCC: International Technical Conference on Circuits Systems, Computers and Communications; 2015/6/29-7/2; ITC-CSCC: Seoul, Republic of Korea, 2015; pp. 721–724. [Google Scholar]
- Liao, T.W. Clustering of time series data—A survey. Pattern Recognit. 2005, 38, 1857–1874. [Google Scholar] [CrossRef]
- Fionn, M.; Pierre, L. Wardfs Hierarchical Clustering Method. arXiv 2011, arXiv:1111.6285v2. [Google Scholar]
- Zhou, Y.; Cheng, H.; Yu, J.X. Graph clustering based on structural/attribute similarities. Proc. VLDB Endow. 2009, 2, 718–729. [Google Scholar] [CrossRef]
- Koutra, D.; Vogelstein, J.T.; Faloutsos, C. Deltacon: A principled massive-graph similarity function. In Proceedings of the 2013 SIAM International Conference on Data Mining, Austin, TX, USA, 2–4 May 2013; Society for Industrial and Applied Mathematics: Philadelphia, PA, USA, 2013; pp. 162–170. [Google Scholar] [CrossRef]
- Soundarajan, S. A Guide to Selecting a Network Similarity Method. In Proceedings of the 2014 SIAM International Conference on Data Mining, Philadelphia, PA, USA, 24–26 April 2014; pp. 1037–1045. [Google Scholar]
- Murase, H.; Sakai, R. Moving object recognition in eigenspace representation: Gait analysis and lip reading. Pattern Recognit. Lett. 1996, 17, 155–162. [Google Scholar] [CrossRef]
- Ke, Y.; Sukthankar, R.; Hebert, M. Efficient visual event detection using volumetric features. In Proceedings of the Tenth IEEE International Conference on Computer Vision (ICCV’05), Beijing, China, 17–21 October 2005; Volume 1, pp. 166–173. [Google Scholar] [CrossRef]
- Hiraishi, K.; Choe, S.; Torii, K.; Uchihira, N.; Tanaka, T. Modeling of complex processes in nursing and caregiving services. In Proceedings of the 2012 IEEE International Conference on Systems, Man, and Cybernetics (SMC), Seoul, Republic of Korea, 14–17 October 2012; pp. 1449–1454. [Google Scholar] [CrossRef]
- García-Magariño, I.; Lacuesta, R.; Lloret, J. Agent-based simulation of smart beds with internet-of-things for exploring big data analytics. IEEE Access 2017, 6, 366–379. [Google Scholar] [CrossRef]
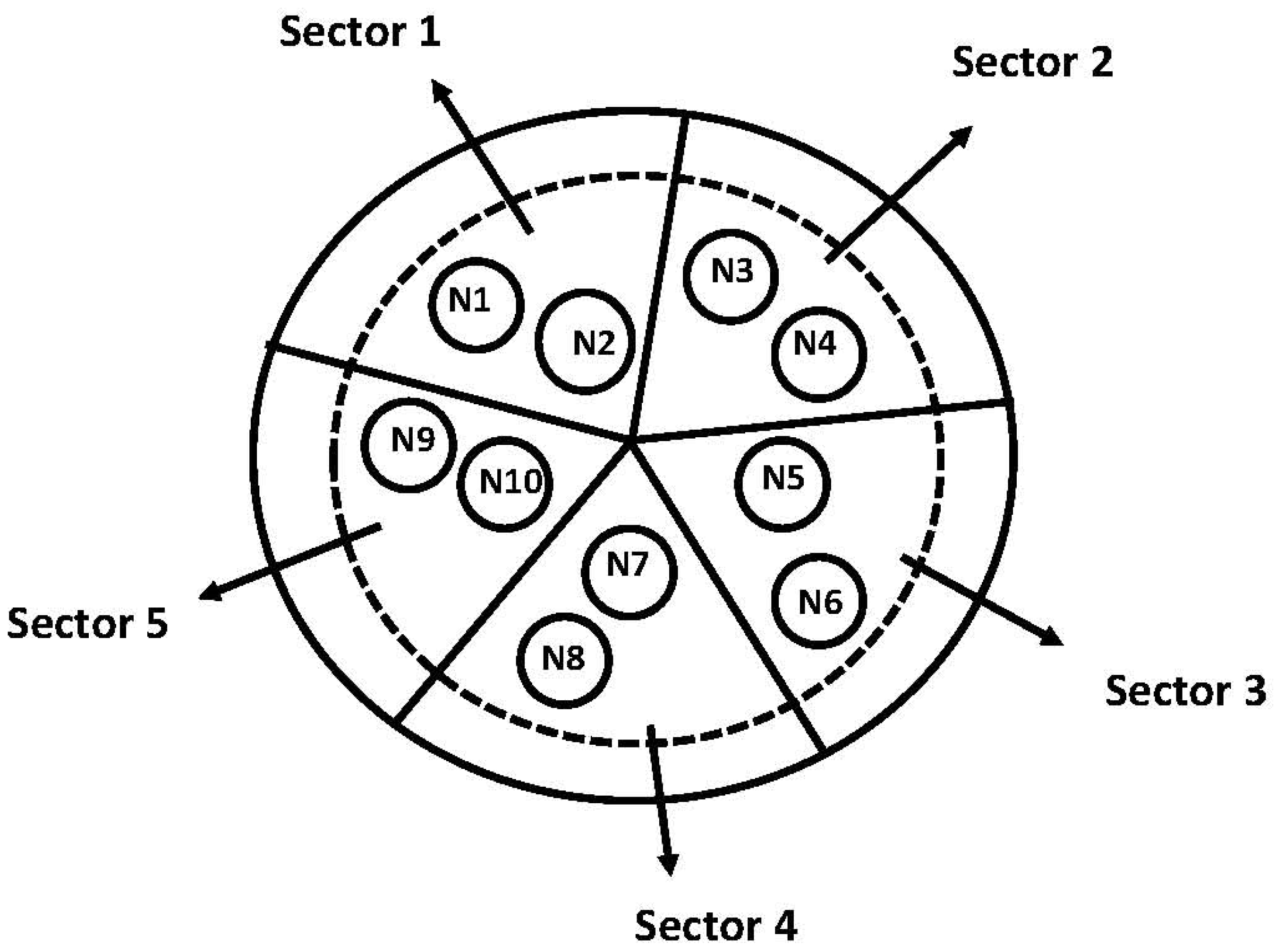

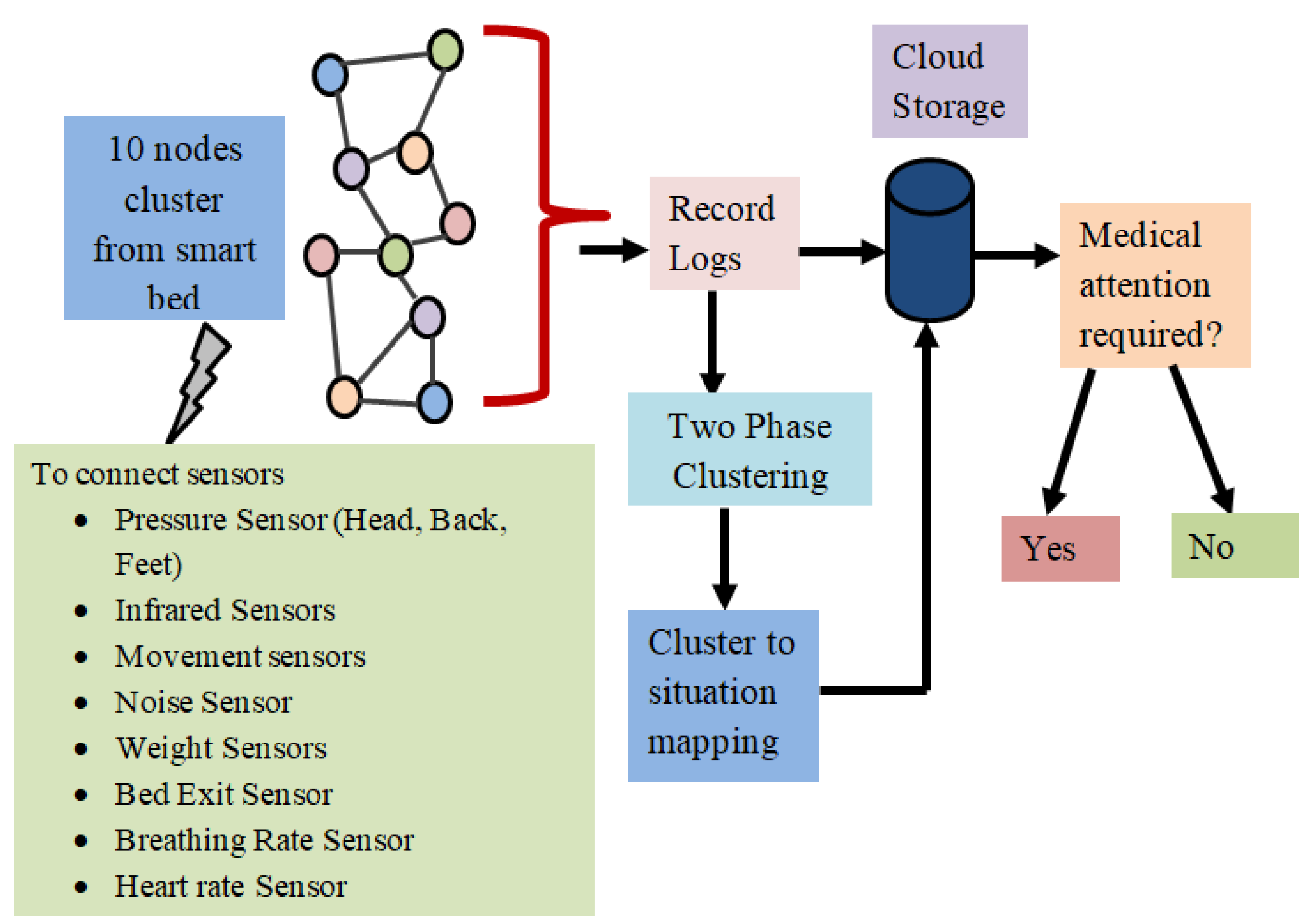

| S. No. | Connection to Sensor Node | Type of Sensor | Description about Sensor |
|---|---|---|---|
| 1 | Node 1 | Pressure sensors (head) | Pressure sensors are used to monitor the patient’s pressure points, such as their head. |
| 2 | Node 2 | Infrared sensors | Infrared sensors are used to detect changes in the patient’s body temperature. |
| 3 | Node 3 | Movement sensors | Movement sensors measure the amount of movement in the bed, to alert the user if they are tossing and turning too much. |
| 4 | Node 4 | Noise sensor | Detects loud noises in the bedroom and can be used to alert caregivers or trigger alarms if necessary. |
| 5 | Node 5 | Weight sensors | Monitors the weight of the bed, allowing for weight distribution and improved comfort. |
| 6 | Node 6 | Bed exit sensor | This sensor detects when a patient is getting out of bed and triggers an alarm to alert nurses and caregivers |
| 7 | Node 7 | Pressure sensors (back) | Pressure sensors are used to monitor the patient’s pressure points, such as their back. |
| 8 | Node 8 | Pressure sensors (feet) | Pressure sensors are used to monitor the patient’s pressure points, such as their feet. |
| 9 | Node 9 | Breathing rate sensors | These sensors measure the patient’s breathing rate and can alert staff if the patient’s breathing rate changes significantly. |
| 10 | Node 10 | Heart rate sensors | Heart rate sensors monitor the patient’s heart rate and can alert staff to changes in heart rate. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maddeh, M.; Hajjej, F.; Alazzam, M.B.; Otaibi, S.A.; Turki, N.A.; Ayouni, S. Spatio-Temporal Cluster Mapping System in Smart Beds for Patient Monitoring. Sensors 2023, 23, 4614. https://doi.org/10.3390/s23104614
Maddeh M, Hajjej F, Alazzam MB, Otaibi SA, Turki NA, Ayouni S. Spatio-Temporal Cluster Mapping System in Smart Beds for Patient Monitoring. Sensors. 2023; 23(10):4614. https://doi.org/10.3390/s23104614
Chicago/Turabian StyleMaddeh, Mohamed, Fahima Hajjej, Malik Bader Alazzam, Shaha Al Otaibi, Nazek Al Turki, and Sarra Ayouni. 2023. "Spatio-Temporal Cluster Mapping System in Smart Beds for Patient Monitoring" Sensors 23, no. 10: 4614. https://doi.org/10.3390/s23104614
APA StyleMaddeh, M., Hajjej, F., Alazzam, M. B., Otaibi, S. A., Turki, N. A., & Ayouni, S. (2023). Spatio-Temporal Cluster Mapping System in Smart Beds for Patient Monitoring. Sensors, 23(10), 4614. https://doi.org/10.3390/s23104614







