Machine Learning Approach to Model Physical Fatigue during Incremental Exercise among Firefighters
Abstract
1. Introduction
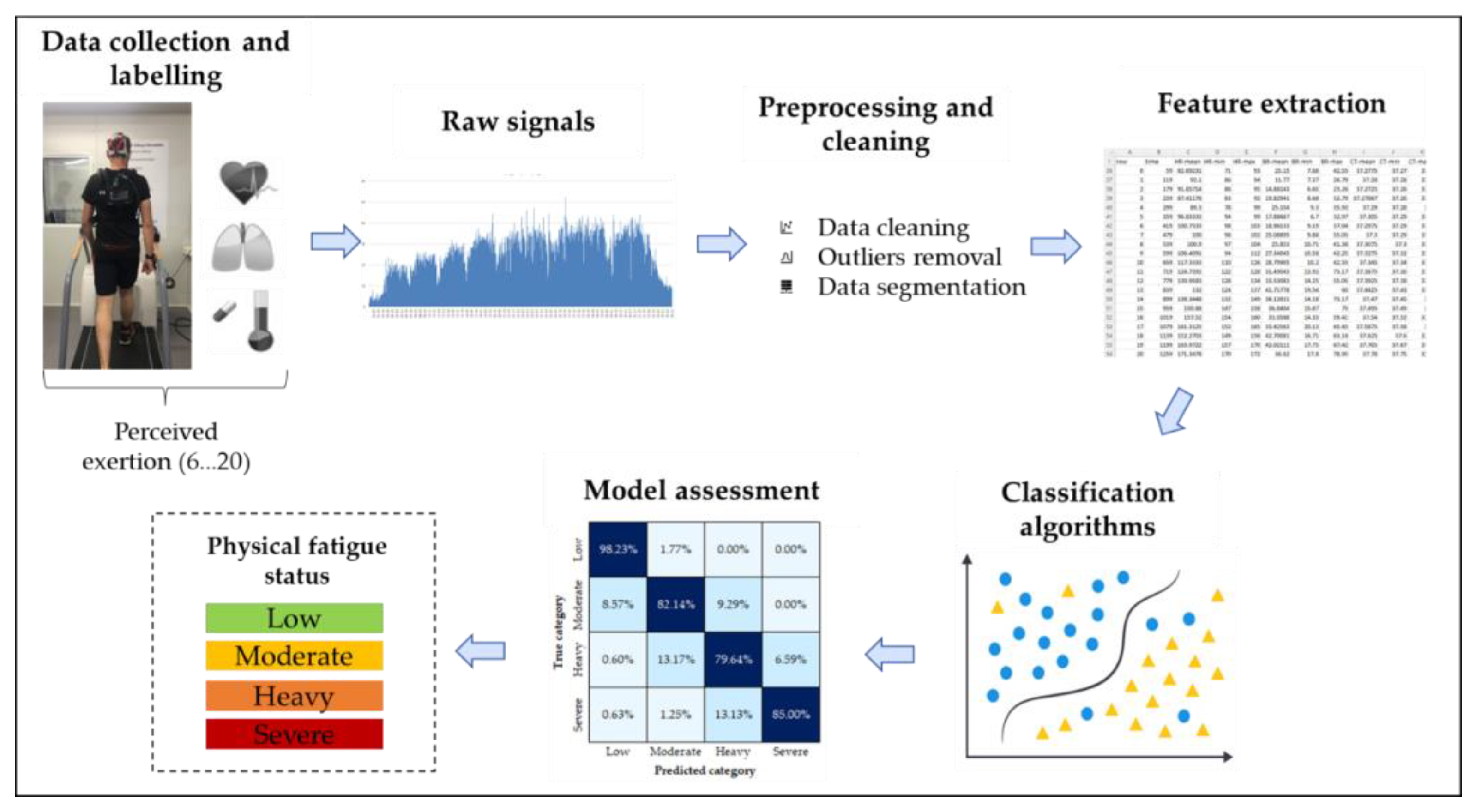
2. Materials and Methods
2.1. Participants
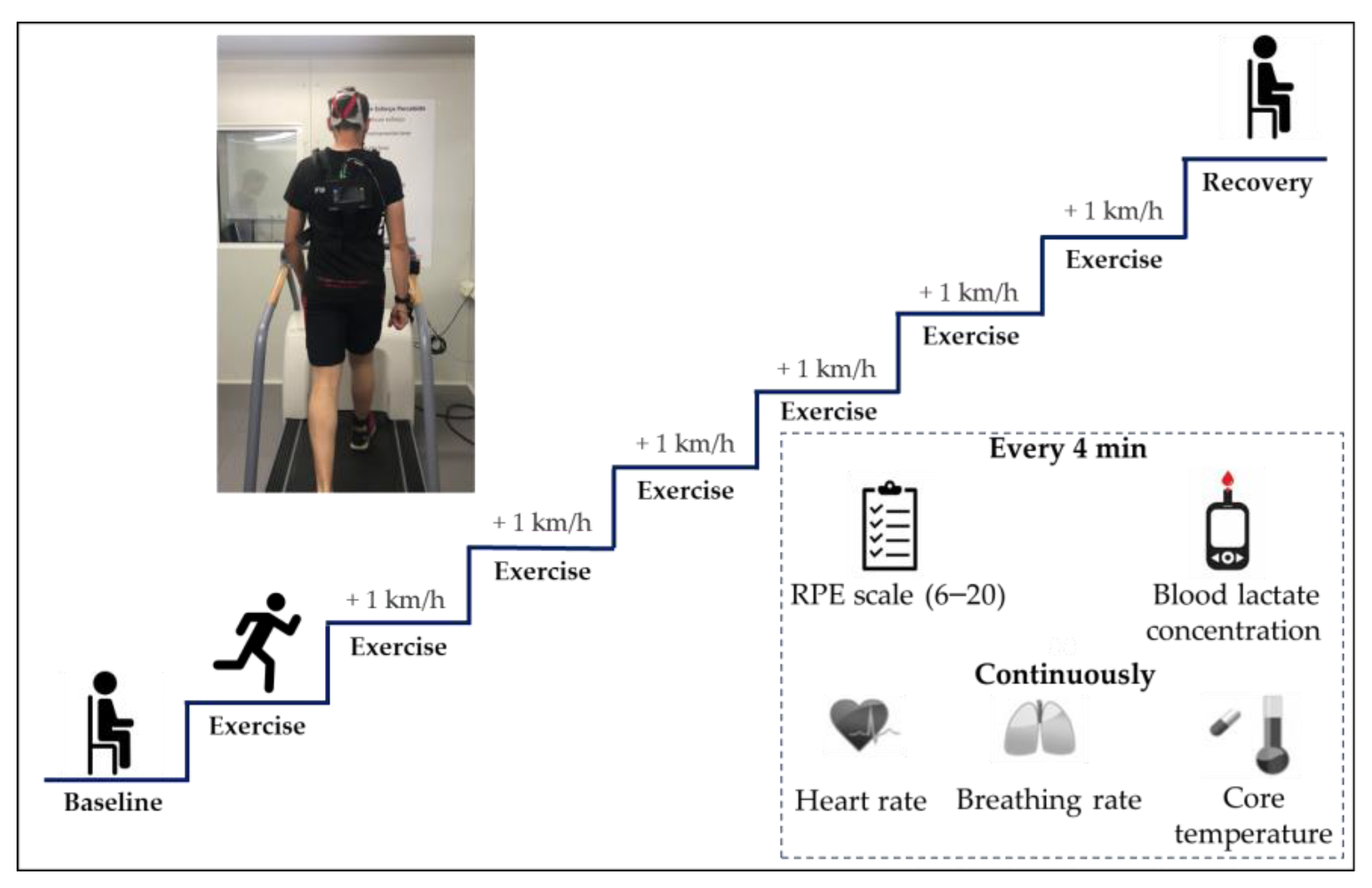
2.2. Data Collection and Labelling
2.3. Preprocessing and Cleaning
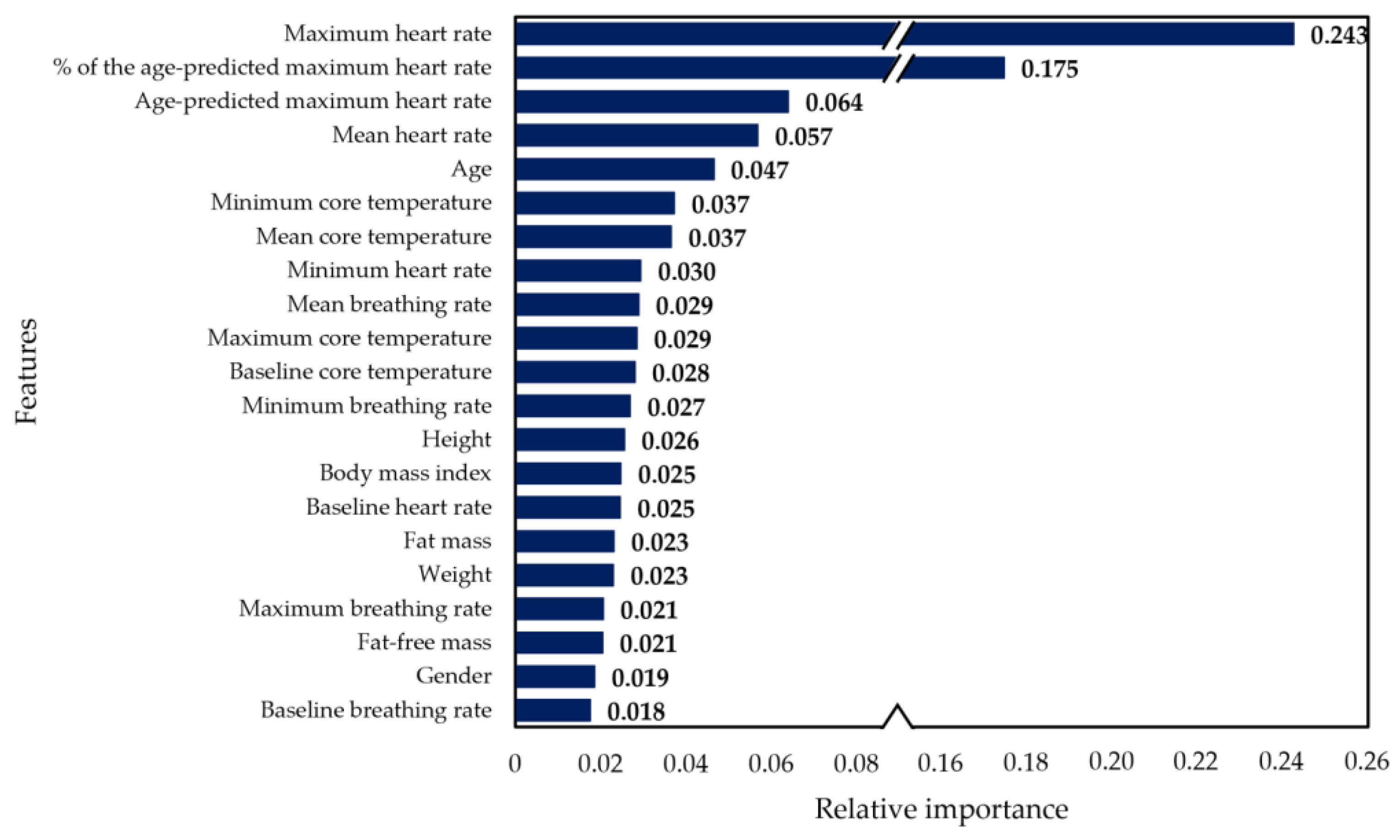
2.4. Feature Extraction
2.5. Classification Algorithms
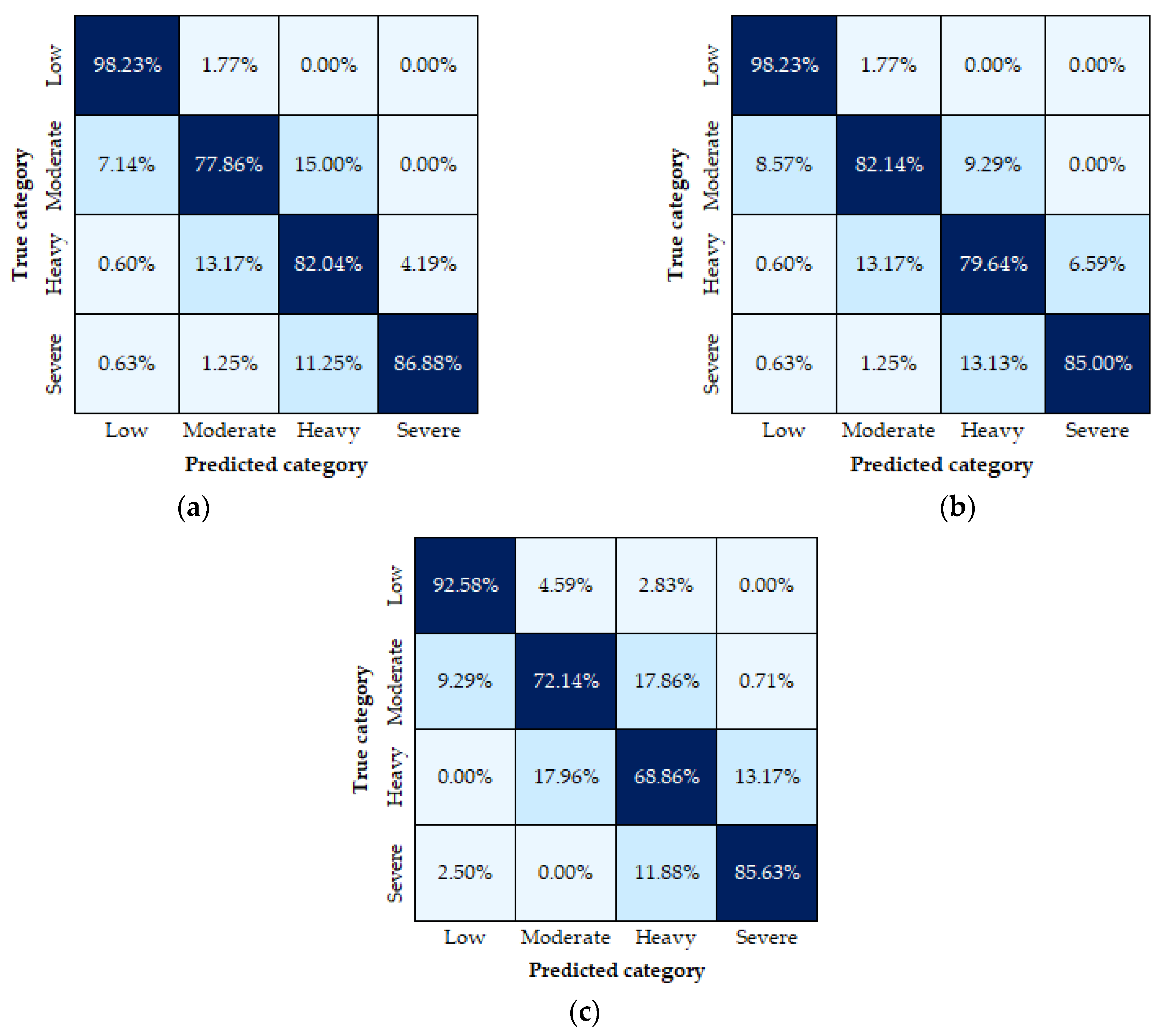
2.6. Model Assessment
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ream, E.; Richardson, A. Fatigue: A concept analysis. Int. J. Nurs. Stud. 1996, 33, 519–529. [Google Scholar] [CrossRef] [PubMed]
- Sadeghniiat-Haghighi, K.; Yazdi, Z. Fatigue management in the workplace. Ind. Psychiatry J. 2015, 24, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, J.A.; Caldwell, J.L.; Thompson, L.A.; Lieberman, H.R. Fatigue and its management in the workplace. Neurosci. Biobehav. Rev. 2019, 96, 272–289. [Google Scholar] [CrossRef] [PubMed]
- Hallowell, M.R. Worker Fatigue: Managing Concerns in Rapid Renewal Highway Construction Projects. Prof. Saf. 2010, 55, 18–26. [Google Scholar]
- Tran, Y.; Craig, A.; Craig, R.; Chai, R.; Nguyen, H. The influence of mental fatigue on brain activity: Evidence from a systematic review with meta-analyses. Psychophysiology 2020, 57, e13554. [Google Scholar] [CrossRef]
- Moshawrab, M.; Adda, M.; Bouzouane, A.; Ibrahim, H.; Raad, A. Smart Wearables for the Detection of Occupational Physical Fatigue: A Literature Review. Sensors 2022, 22, 7472. [Google Scholar] [CrossRef]
- Sedighi Maman, Z.; Alamdar Yazdi, M.A.; Cavuoto, L.A.; Megahed, F.M. A data-driven approach to modeling physical fatigue in the workplace using wearable sensors. Appl. Ergon. 2017, 65, 515–529. [Google Scholar] [CrossRef]
- Umer, W.; Li, H.; Yantao, Y.; Antwi-Afari, M.F.; Anwer, S.; Luo, X. Physical exertion modeling for construction tasks using combined cardiorespiratory and thermoregulatory measures. Autom. Constr. 2020, 112, 103079. [Google Scholar] [CrossRef]
- Barger, L.K.; Lockley, S.W.; Rajaratnam, S.M.; Landrigan, C.P. Neurobehavioral, health, and safety consequences associated with shift work in safety-sensitive professions. Curr. Neurol. Neurosci. Rep. 2009, 9, 155–164. [Google Scholar] [CrossRef]
- Lee, J.-Y.; Bakri, I.; Kim, J.-H.; Son, S.-Y.; Tochihara, Y. The impact of firefighter personal protective equipment and treadmill protocol on maximal oxygen uptake. J. Occup. Environ. Hyg. 2013, 10, 397–407. [Google Scholar] [CrossRef]
- Von Heimburg, E.; Sandsund, M.; Rangul, T.P.; Reinertsen, R.E. Physiological and perceptual strain of firefighters during graded exercise to exhaustion at 40 and 10 °C. Int. J. Occup. Saf. Ergon. 2017, 25, 412–422. [Google Scholar] [CrossRef]
- Aguirre, A.; Pinto, M.J.; Cifuentes, C.A.; Perdomo, O.; Díaz, C.A.R.; Múnera, M. Machine Learning Approach for Fatigue Estimation in Sit-to-Stand Exercise. Sensors 2021, 21, 5006. [Google Scholar] [CrossRef]
- Bustos, D.; Guedes, J.C.; Baptista, J.S.; Vaz, M.P.; Costa, J.T.; Fernandes, R.J. Applicability of Physiological Monitoring Systems within Occupational Groups: A Systematic Review. Sensors 2021, 21, 7249. [Google Scholar] [CrossRef]
- Adão Martins, N.R.; Annaheim, S.; Spengler, C.M.; Rossi, R.M. Fatigue Monitoring Through Wearables: A State-of-the-Art Review. Front. Physiol. 2021, 12, 790292. [Google Scholar] [CrossRef]
- Aryal, A.; Ghahramani, A.; Becerik-Gerber, B. Monitoring fatigue in construction workers using physiological measurements. Autom. Constr. 2017, 82, 154–165. [Google Scholar] [CrossRef]
- Bustos, D.; Guedes, J.C.; Vaz, M.P.; Pombo, E.; Fernandes, R.J.; Costa, J.T.; Baptista, J.S. Non-Invasive Physiological Monitoring for Physical Exertion and Fatigue Assessment in Military Personnel: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 8815. [Google Scholar] [CrossRef]
- Friedl, K.E. Military applications of soldier physiological monitoring. J. Sci. Med. Sport 2018, 21, 1147–1153. [Google Scholar] [CrossRef]
- Umer, W. Simultaneous monitoring of physical and mental stress for construction tasks using physiological measures. J. Build. Eng. 2022, 46, 103777. [Google Scholar] [CrossRef]
- Jebelli, H.; Choi, B.; Lee, S. Application of Wearable Biosensors to Construction Sites. II: Assessing Workers’ Physical Demand. J. Constr. Eng. Manag. 2019, 145, 04019080. [Google Scholar] [CrossRef]
- Jiao, Y.; Sun, Z.; Fu, L.; Yu, X.; Jiang, C.; Zhang, X.; Liu, K.; Chen, X. Physiological responses and stress levels of high-speed rail train drivers under various operating conditions-a simulator study in China. Int. J. Rail Transp. 2022, 10, 1–16. [Google Scholar] [CrossRef]
- Baghdadi, A.; Megahed, F.M.; Esfahani, E.T.; Cavuoto, L.A. A machine learning approach to detect changes in gait parameters following a fatiguing occupational task. Ergonomics 2018, 61, 1116–1129. [Google Scholar] [CrossRef] [PubMed]
- Nasirzadeh, F.; Mir, M.; Hussain, S.; Tayarani Darbandy, M.; Khosravi, A.; Nahavandi, S.; Aisbett, B. Physical Fatigue Detection Using Entropy Analysis of Heart Rate Signals. Sustainability 2020, 12, 2714. [Google Scholar] [CrossRef]
- Lambay, A.; Liu, Y.; Morgan, P.; Ji, Z. A Data-Driven Fatigue Prediction using Recurrent Neural Networks. In Proceedings of the 2021 3rd International Congress on Human-Computer Interaction, Optimization and Robotic Applications (HORA), Ankara, Turkey, 11–13 June 2021; pp. 1–6. [Google Scholar]
- Hooda, R.; Joshi, V.; Shah, M. A comprehensive review of approaches to detect fatigue using machine learning techniques. Chronic Dis. Transl. Med. 2021, 8, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Pinto-Bernal, M.J.; Cifuentes, C.A.; Perdomo, O.; Rincón-Roncancio, M.; Múnera, M. A Data-Driven Approach to Physical Fatigue Management Using Wearable Sensors to Classify Four Diagnostic Fatigue States. Sensors 2021, 21, 6401. [Google Scholar] [CrossRef] [PubMed]
- ISO 9920:2007; Ergonomics of the Thermal Environment–Estimation of Thermal Insulation and Water Vapour Resistance of a Clothing Ensemble. International Organisation for Standardisation: Geneva, Switzerland, 2007.
- Cardoso, F.; Coelho, E.P.; Gay, A.; Vilas-Boas, J.P.; Pinho, J.C.; Pyne, D.B.; Fernandes, R.J. Case Study: A Jaw-Protruding Dental Splint Improves Running Physiology and Kinematics. Int. J. Sport. Physiol. Perform. 2022, 17, 791–795. [Google Scholar] [CrossRef]
- Cardoso, F.; Monteiro, A.S.; Vilas-Boas, J.P.; Pinho, J.C.; Pyne, D.B.; Fernandes, R.J. Effects of Wearing a 50% Lower Jaw Advancement Splint on Biophysical and Perceptual Responses at Low to Severe Running Intensities. Life 2022, 12, 253. [Google Scholar] [CrossRef]
- Sousa, A.N.A.; Figueiredo, P.; Zamparo, P.; Pyne, D.B.; Vilas-Boas, J.P.; Fernandes, R.J. Exercise Modality Effect on Bioenergetical Performance at VO2max Intensity. Med. Sci. Sport. Exerc. 2015, 47, 1705–1713. Available online: https://journals.lww.com/acsm-msse/Fulltext/2015/08000/Exercise_Modality_Effect_on_Bioenergetical.19.aspx (accessed on 13 October 2022). [CrossRef]
- Guedes, J.C.; Costa, E.Q.; Baptista, J.S. Using a Climatic Chamber to Measure the Human Psychophysiological Response under Different Combinations of Temperature and Humidity. Thermol. Int. 2012, 22, 49–54. Available online: http://ww.uhlen.at/thermology-international/archive/EAT2012_Book_of_Proceedings.pdf#page=50 (accessed on 13 September 2022).
- Bongers, C.C.W.G.; Daanen, H.A.M.; Bogerd, C.P.; Hopman, M.T.E.; Eijsvogels, T.M.H. Validity, Reliability, and Inertia of Four Different Temperature Capsule Systems. Med. Sci. Sport. Exerc. 2018, 50, 169–175. Available online: https://journals.lww.com/acsm-msse/Fulltext/2018/01000/Validity,_Reliability,_and_Inertia_of_Four.21.aspx (accessed on 20 October 2022). [CrossRef]
- Sousa, A.C.; Fernandes, R.J.; Boas, J.P.V.; Figueiredo, P. High-intensity Interval Training in Different Exercise Modes: Lessons from Time to Exhaustion. Int. J. Sport. Med. 2018, 39, 668–673. [Google Scholar] [CrossRef]
- Pratas, P.; Bustos, D.; Guedes, J.C.; Mendes, J.; Baptista, J.S.; Vaz, M. Physiological Monitoring Systems for Fatigue Detection Within Firefighters: A Brief Systematic Review. In Occupational and Environmental Safety and Health IV; Arezes, P.M., Baptista, J.S., Melo, R.B., Castelo Branco, J., Carneiro, P., Colim, A., Costa, N., Costa, S., Duarte, J., Guedes, J.C., et al., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 469–486. [Google Scholar]
- Shakerian, S.; Habibnezhad, M.; Ojha, A.; Lee, G.; Liu, Y.; Jebelli, H.; Lee, S. Assessing occupational risk of heat stress at construction: A worker-centric wearable sensor-based approach. Saf. Sci. 2021, 142, 105395. [Google Scholar] [CrossRef]
- Umer, W.; Yu, Y.; Antwi-Afari, M.F.; Jue, L.; Siddiqui, M.K.; Li, H. Heart rate variability based physical exertion monitoring for manual material handling tasks. Int. J. Ind. Ergon. 2022, 89, 103301. [Google Scholar] [CrossRef]
- Li, S.; Zhang, X. Research on orthopedic auxiliary classification and prediction model based on XGBoost algorithm. Neural Comput. Appl. 2020, 32, 1971–1979. [Google Scholar] [CrossRef]
- Uddin, S.; Khan, A.; Hossain, M.E.; Moni, M.A. Comparing different supervised machine learning algorithms for disease prediction. BMC Med. Inform. Decis. Mak. 2019, 19, 281. [Google Scholar] [CrossRef]
- Abu Alfeilat, H.A.; Hassanat, A.B.A.; Lasassmeh, O.; Tarawneh, A.S.; Alhasanat, M.B.; Eyal Salman, H.S.; Prasath, V.B.S. Effects of Distance Measure Choice on K-Nearest Neighbor Classifier Performance: A Review. Big Data 2019, 7, 221–248. [Google Scholar] [CrossRef]
- Friedman, J.H. Greedy function approximation: A gradient boosting machine. Ann. Stat. 2001, 29, 1189–1232. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. XGBoost: A Scalable Tree Boosting System. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Ogunleye, A.; Wang, Q.-G. XGBoost model for chronic kidney disease diagnosis. IEEE/ACM Trans. Comput. Biol. Bioinform. 2019, 17, 2131–2140. [Google Scholar] [CrossRef]
- Seiffert, C.; Khoshgoftaar, T.M.; Van Hulse, J.; Napolitano, A. RUSBoost: A hybrid approach to alleviating class imbalance. IEEE Trans. Syst. Man Cybern.-Part A Syst. Hum. 2009, 40, 185–197. [Google Scholar] [CrossRef]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Kang, M.; Jameson, N.J. Machine Learning: Fundamentals. In Prognostics and Health Management of Electronics; John Wiley & Sons: Hoboken, NJ, USA, 2018; pp. 85–109. [Google Scholar]
- Lee, B.G.; Choi, B.; Jebelli, H.; Lee, S. Assessment of construction workers’ perceived risk using physiological data from wearable sensors: A machine learning approach. J. Build. Eng. 2021, 42, 102824. [Google Scholar] [CrossRef]
- Bzdok, D.; Altman, N.; Krzywinski, M. Statistics versus machine learning. Nat. Methods 2018, 15, 233–234. [Google Scholar] [CrossRef] [PubMed]
- Rajula, H.S.R.; Verlato, G.; Manchia, M.; Antonucci, N.; Fanos, V. Comparison of Conventional Statistical Methods with Machine Learning in Medicine: Diagnosis, Drug Development, and Treatment. Medicina 2020, 56, 455. [Google Scholar] [CrossRef] [PubMed]
- Mamoshina, P.; Vieira, A.; Putin, E.; Zhavoronkov, A. Applications of Deep Learning in Biomedicine. Mol. Pharm. 2016, 13, 1445–1454. [Google Scholar] [CrossRef] [PubMed]
- Shookster, D.; Lindsey, B.; Cortes, N.; Martin, J.R. Accuracy of Commonly Used Age-Predicted Maximal Heart Rate Equations. Int. J. Exerc. Sci. 2020, 13, 1242–1250. [Google Scholar]
- Pluntke, U.; Gerke, S.; Sridhar, A.; Weiss, J.; Michel, B. Evaluation and Classification of Physical and Psychological Stress in Firefighters using Heart Rate Variability. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 2207–2212. [Google Scholar]
- Kupschick, S.; Pendzich, M.; Gardas, D.; Jürgensohn, T.; Wischniewski, S.; Adolph, L. Predicting Firefighters’ Exertion Based on Machine Learning Techniques; Federal Institute for Occupational Safety and Health: Dortmund, Germany, 2016. [Google Scholar] [CrossRef]
- Arias-Torres, D.; José; Hernández-Nolasco, A.; Wister, M.A. Detection of fatigue on gait using accelerometer data and supervised machine learning. Int. J. Grid Util. Comput. 2020, 11, 474–485. [Google Scholar] [CrossRef]
| RPE | Level of Exertion | Physical Fatigue Levels |
|---|---|---|
| 6 | No exertion | Low |
| 7 | ||
| 7.5 | Extremely light | |
| 8 | ||
| 9 | Very light | |
| 10 | ||
| 11 | Light | |
| 12 | Moderate | |
| 13 | Somewhat hard | |
| 14 | ||
| 15 | Hard | Heavy |
| 16 | ||
| 17 | Very Hard | Severe |
| 18 | ||
| 19 | Extremely hard | |
| 20 | Maximal exertion |
| Stage No.: | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| Treadmill velocity (km/h) | 5.4 ± 1.8 | 6.2 ± 1.9 | 7.0 ± 2.1 | 8.0 ± 2.1 | 9.0 ± 2.1 | 10.0 ± 2.1 | 11.0 ± 2.1 |
| Oxygen uptake (mL/min/kg) | 18.7 ± 7.2 2–7 | 22.5 ± 8.3 3–7 | 25.5 ± 9.2 4–7 | 29.5 ± 9.4 5–7 | 34.5 ± 9.1 6–7 | 39.1 ± 8.6 | 40.5 ± 8.6 |
| Oxygen uptake (mL/min) | 1418.5 ± 571.9 2–7 | 1688.3 ± 630.3 3–7 | 1919.3 ± 706.5 4–7 | 2228.0 ± 731.9 5–7 | 2611.2 ± 709.4 6–7 | 2964.5 ± 684.9 | 3065.2 ± 698.1 |
| Respiratory frequency (1/min) | 26 ± 7 2–7 | 28 ± 8 4–7 | 31 ± 7 4–7 | 35 ± 7 5–7 | 40 ± 8 6–7 | 47 ± 8 7 | 52 ± 8 |
| Tidal volume (L) | 1.25 ± 0.38 2–7 | 1.47 ± 0.48 5–7 | 1.50 ± 0.46 4–7 | 1.65 ± 0.40 5–7 | 1.86 ± 0.39 6–7 | 2.03 ± 0.43 | 1.99 ± 0.34 |
| Ventilation (L/min) | 33 ± 14 2–7 | 42 ± 16 3–7 | 47 ± 18 4–7 | 58 ± 18 5–7 | 75 ± 20 6–7 | 94 ± 19 7 | 105 ± 20 |
| Carbon dioxide production (mL/min) | 1260.2 ± 533.5 2–7 | 1601.3 ± 609.4 3–7 | 1802.1 ± 689.9 4–7 | 2170.0 ± 708.7 5–7 | 2641.8 ± 689.9 6–7 | 3091.8 ± 609.3 | 3236.2 ± 691.7 |
| Respiratory quotient | 0.89 ± 0.13 2–7 | 0.95 ± 0.15 5–7 | 0.95 ± 0.17 6–7 | 0.99 ± 0.20 5–7 | 1.03 ± 0.207 | 1.06 ± 0.19 | 1.07 ± 0.20 |
| Heart rate (bpm) | 110 ± 17 2–7 | 127 ± 20 3–7 | 139 ± 22 4–7 | 153 ± 20 5–7 | 168 ± 13 6–7 | 179 ± 11 | 183 ± 20 |
| Core temperature (°C) | 37.36 ± 0.36 3–7 | 37.47 ± 0.40 3–7 | 37.56 ± 0.40 4–7 | 37.71 ± 0.45 5–7 | 37.81 ± 0.40 6–7 | 38.01 ± 0.40 7 | 38.19 ± 0.44 |
| Lactate concentration (mmol/L) | 2.4 ± 1.0 4–7 | 2.6 ± 1.0 3–7 | 3.1 ± 1.4 4–7 | 4.3 ± 1.5 5–7 | 6.0 ± 3.0 6–7 | 10.3 ± 3.4 7 | 14.4 ± 4.0 |
| RPE (6–20) | 9 ± 2 2–7 | 11 ± 2 3–7 | 12 ± 2 4–7 | 14 ± 2 5–7 | 16 ± 2 6–7 | 17 ± 1 7 | 19 ± 1 |
| Classifier | Accuracy | Precision | Recall | F1 score | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (a) | (b) | (c) | (a) | (b) | (c) | (a) | (b) | (c) | (a) | (b) | (c) | |
| XGBoosted Tree | 0.88 | 0.88 | 0.82 | 0.89 | 0.88 | 0.82 | 0.88 | 0.88 | 0.82 | 0.88 | 0.88 | 0.82 |
| Gradient-Boosted Tree | 0.87 | 0.87 | 0.81 | 0.87 | 0.88 | 0.81 | 0.87 | 0.87 | 0.81 | 0.87 | 0.87 | 0.81 |
| Bagged Tree | 0.85 | 0.84 | 0.81 | 0.85 | 0.84 | 0.81 | 0.85 | 0.84 | 0.81 | 0.85 | 0.84 | 0.81 |
| Random Forest | 0.84 | 0.84 | 0.81 | 0.85 | 0.85 | 0.82 | 0.84 | 0.84 | 0.81 | 0.84 | 0.84 | 0.81 |
| Linear Support Vector Machine | 0.83 | 0.84 | 0.77 | 0.83 | 0.84 | 0.77 | 0.83 | 0.84 | 0.77 | 0.83 | 0.84 | 0.77 |
| K-nearest Neighbours | 0.80 | 0.80 | 0.64 | 0.80 | 0.80 | 0.66 | 0.80 | 0.80 | 0.64 | 0.80 | 0.80 | 0.65 |
| RUSBoosted Trees | 0.79 | 0.79 | 0.71 | 0.79 | 0.80 | 0.72 | 0.79 | 0.79 | 0.71 | 0.79 | 0.79 | 0.72 |
| Artificial Neural Network | 0.73 | 0.72 | 0.73 | 0.72 | 0.71 | 0.73 | 0.73 | 0.73 | 0.73 | 0.72 | 0.71 | 0.73 |
| Quadratic Support Vector Machine | 0.41 | 0.42 | 0.42 | 0.38 | 0.43 | 0.47 | 0.41 | 0.42 | 0.42 | 0.31 | 0.31 | 0.31 |
| Cubic Support Vector Machine | 0.45 | 0.46 | 0.44 | 0.46 | 0.49 | 0.44 | 0.45 | 0.46 | 0.44 | 0.36 | 0.37 | 0.34 |
| Gaussian Support Vector Machine | 0.36 | 0.38 | 0.36 | 0.35 | 0.46 | 0.37 | 0.37 | 0.38 | 0.36 | 0.28 | 0.29 | 0.27 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bustos, D.; Cardoso, F.; Rios, M.; Vaz, M.; Guedes, J.; Torres Costa, J.; Santos Baptista, J.; Fernandes, R.J. Machine Learning Approach to Model Physical Fatigue during Incremental Exercise among Firefighters. Sensors 2023, 23, 194. https://doi.org/10.3390/s23010194
Bustos D, Cardoso F, Rios M, Vaz M, Guedes J, Torres Costa J, Santos Baptista J, Fernandes RJ. Machine Learning Approach to Model Physical Fatigue during Incremental Exercise among Firefighters. Sensors. 2023; 23(1):194. https://doi.org/10.3390/s23010194
Chicago/Turabian StyleBustos, Denisse, Filipa Cardoso, Manoel Rios, Mário Vaz, Joana Guedes, José Torres Costa, João Santos Baptista, and Ricardo J. Fernandes. 2023. "Machine Learning Approach to Model Physical Fatigue during Incremental Exercise among Firefighters" Sensors 23, no. 1: 194. https://doi.org/10.3390/s23010194
APA StyleBustos, D., Cardoso, F., Rios, M., Vaz, M., Guedes, J., Torres Costa, J., Santos Baptista, J., & Fernandes, R. J. (2023). Machine Learning Approach to Model Physical Fatigue during Incremental Exercise among Firefighters. Sensors, 23(1), 194. https://doi.org/10.3390/s23010194











