Stepping towards More Intuitive Physical Activity Metrics with Wrist-Worn Accelerometry: Validity of an Open-Source Step-Count Algorithm
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Participant Characteristics
2.3. Accelerometer Assessment
2.4. Deriving Steps from Wrist-Worn Accelerometer Data: Algorithm Conception and Development
2.5. Accelerometer Data Processing
2.6. Statistical Analysis
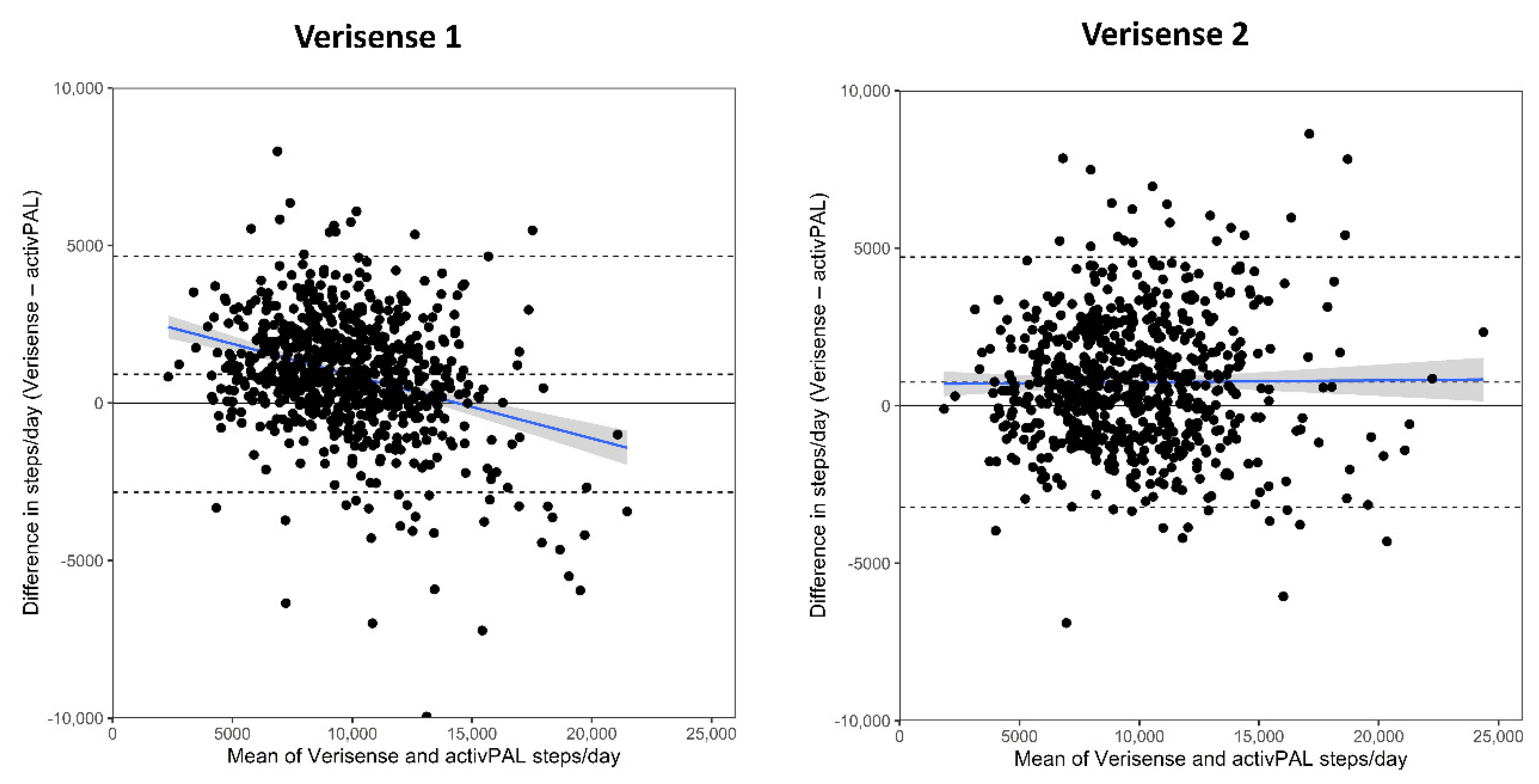
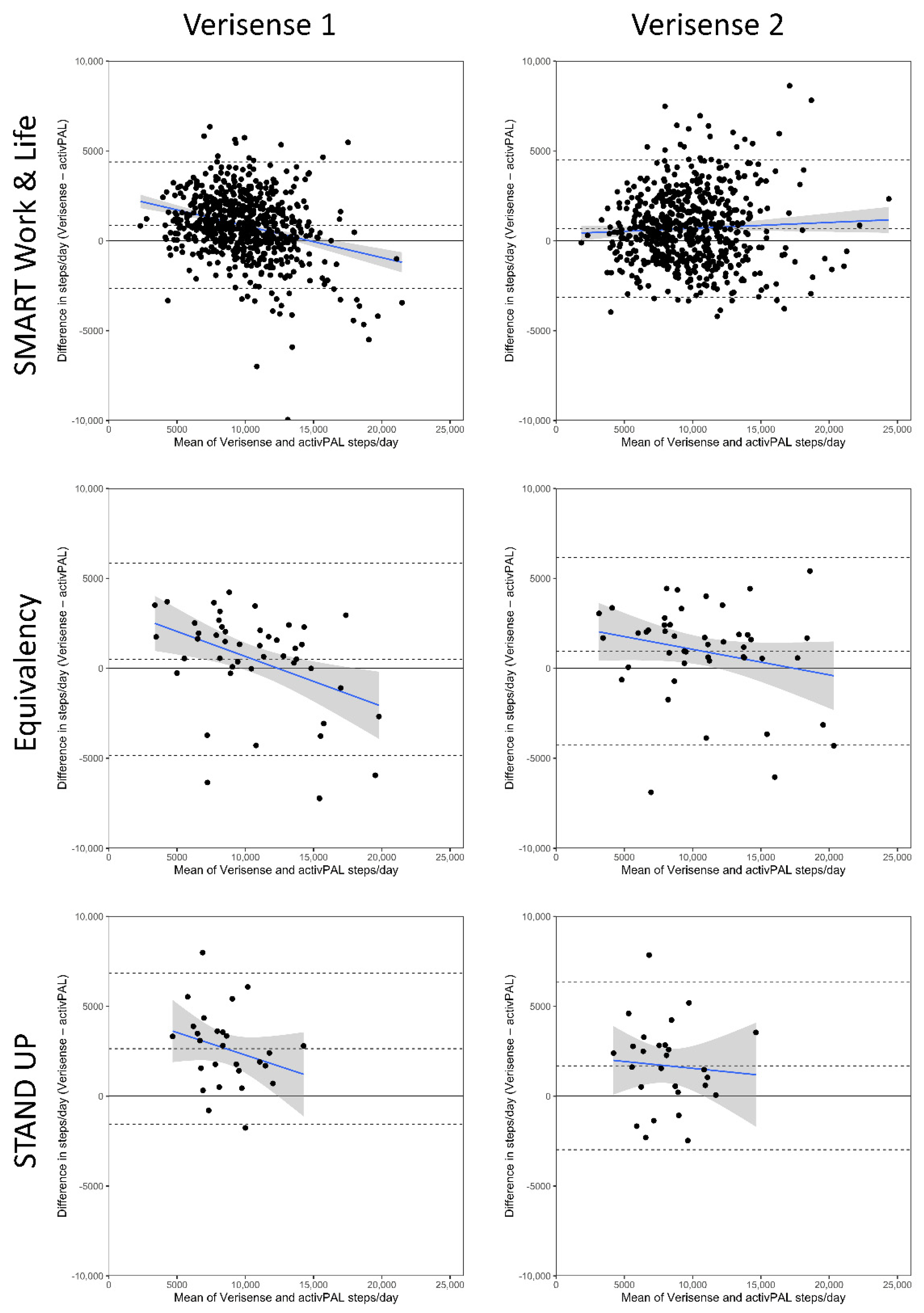
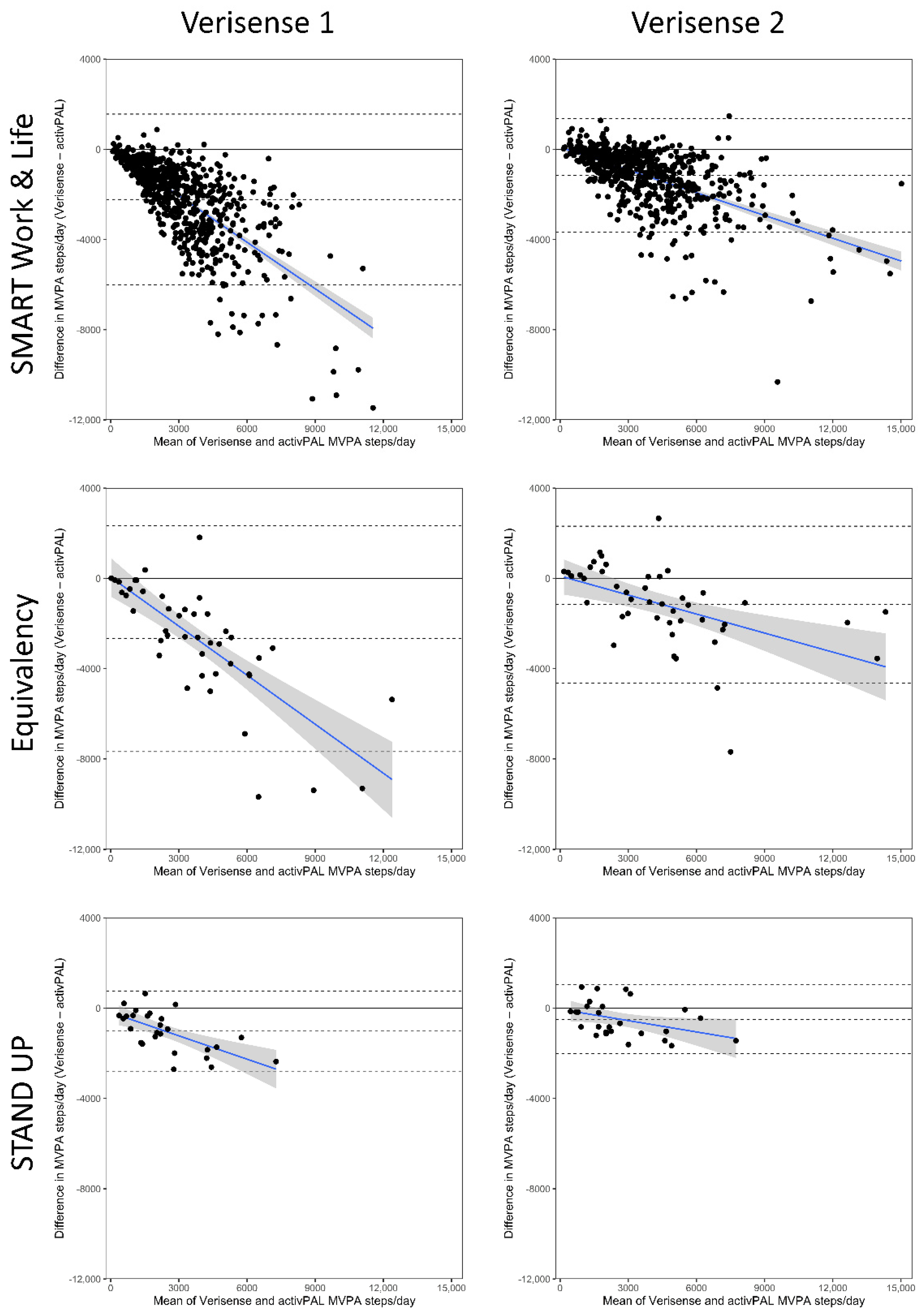
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ekelund, U.; Tarp, J.; Steene-Johannessen, J.; Hansen, B.H.; Jefferis, B.; Fagerland, M.W.; Whincup, P.; Diaz, K.M.; Hooker, S.P.; Chernofsky, A.; et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis. BMJ 2019, 366, l4570. [Google Scholar] [CrossRef] [PubMed]
- Paluch, A.E.; Bajpai, S.; Bassett, D.R.; Carnethon, M.R.; Ekelund, U.; Evenson, K.R.; Galuska, D.A.; Jefferis, B.J.; Kraus, W.E.; Lee, I.M.; et al. Daily steps and all-cause mortality: A meta-analysis of 15 international cohorts. Lancet Public Health 2022, 7, e219–e228. [Google Scholar] [CrossRef] [PubMed]
- Garduno, A.C.; LaCroix, A.Z.; LaMonte, M.J.; Dunstan, D.W.; Evenson, K.R.; Wang, G.; Di, C.; Schumacher, B.T.; Bellettiere, J. Associations of Daily Steps and Step Intensity With Incident Diabetes in a Prospective Cohort Study of Older Women: The OPACH Study. Diabetes Care 2022, 45, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.S.; Hyde, E.T.; Bassett, D.R.; Carlson, S.A.; Carnethon, M.R.; Ekelund, U.; Evenson, K.R.; Galuska, D.A.; Kraus, W.E.; Lee, I.M.; et al. Systematic review of the prospective association of daily step counts with risk of mortality, cardiovascular disease, and dysglycemia. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 78. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Kraus, W.E.; Janz, K.F.; Powell, K.E.; Campbell, W.W.; Jakicic, J.M.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L.; Physical Activity Guidelines Advisory Committee. Daily Step Counts for Measuring Physical Activity Exposure and Its Relation to Health. Med. Sci. Sports Exerc. 2019, 51, 1206–1212. [Google Scholar] [CrossRef]
- Bassett, D.R., Jr.; Toth, L.P.; LaMunion, S.R.; Crouter, S.E. Step Counting: A Review of Measurement Considerations and Health-Related Applications. Sports Med. 2017, 47, 1303–1315. [Google Scholar] [CrossRef]
- Hamer, M.; Blodgett, J.M.; Stamatakis, E. Dose-response association between step count and cardiovascular disease risk markers in middle-aged adults. Scand. J. Med. Sci. Sports 2022, 32, 1161–1165. [Google Scholar] [CrossRef]
- Dwyer, T.; Pezic, A.; Sun, C.; Cochrane, J.; Venn, A.; Srikanth, V.; Jones, G.; Shook, R.P.; Sui, X.; Ortaglia, A.; et al. Objectively Measured Daily Steps and Subsequent Long Term All-Cause Mortality: The Tasped Prospective Cohort Study. PLoS ONE 2015, 10, e0141274. [Google Scholar] [CrossRef]
- Ferguson, T.; Olds, T.; Curtis, R.; Blake, H.; Crozier, A.J.; Dankiw, K.; Dumuid, D.; Kasai, D.; O’Connor, E.; Virgara, R.; et al. Effectiveness of wearable activity trackers to increase physical activity and improve health: A systematic review of systematic reviews and meta-analyses. Lancet Digit Health 2022, 4, e615–e626. [Google Scholar] [CrossRef]
- Doherty, A.; Jackson, D.; Hammerla, N.; Plotz, T.; Olivier, P.; Granat, M.H.; White, T.; van Hees, V.T.; Trenell, M.I.; Owen, C.G.; et al. Large Scale Population Assessment of Physical Activity Using Wrist Worn Accelerometers: The UK Biobank Study. PLoS ONE 2017, 12, e0169649. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Available online: http://www.cdc.gov/nchs/nhanes.htm (accessed on 10 November 2022).
- Del Pozo Cruz, B.; Ahmadi, M.N.; Lee, I.M.; Stamatakis, E. Prospective Associations of Daily Step Counts and Intensity With Cancer and Cardiovascular Disease Incidence and Mortality and All-Cause Mortality. JAMA Intern Med. 2022, 182, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Sheng, M.; Yang, J.; Bao, M.; Chen, T.; Cai, R.; Zhang, N.; Chen, H.; Liu, M.; Wu, X.; Zhang, B.; et al. The relationships between step count and all-cause mortality and cardiovascular events: A dose-response meta-analysis. J. Sport Health Sci. 2021, 10, 620–628. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.M.; Shiroma, E.J.; Kamada, M.; Bassett, D.R.; Matthews, C.E.; Buring, J.E. Association of Step Volume and Intensity with All-Cause Mortality in Older Women. JAMA Intern Med. 2019, 179, 1105–1112. [Google Scholar] [CrossRef]
- Song, P.; Gupta, A.; Goon, I.Y.; Hasan, M.; Mahmood, S.; Pradeepa, R.; Siddiqui, S.; Frost, G.S.; Kusuma, D.; Miraldo, M.; et al. Data Resource Profile: Understanding the patterns and determinants of health in South Asians-the South Asia Biobank. Int. J. Epidemiol. 2021, 50, 717–718e. [Google Scholar] [CrossRef]
- Toth, L.P.; Park, S.; Springer, C.M.; Feyerabend, M.D.; Steeves, J.A.; Bassett, D.R. Video-Recorded Validation of Wearable Step Counters under Free-living Conditions. Med. Sci. Sports Exerc. 2018, 50, 1315–1322. [Google Scholar] [CrossRef]
- Ducharme, S.W.; Lim, J.; Busa, M.A.; Aguiar, E.J.; Moore, C.C.; Schuna, J.M.; Barreira, T.V.; Staudenmayer, J.; Chipkin, S.R.; Tudor-Locke, C. A Transparent Method for Step Detection Using an Acceleration Threshold. J. Meas. Phys. Behav. 2021, 4, 311–320. [Google Scholar] [CrossRef]
- Luu, L.; Pillai, A.; Lea, H.; Buendia, R.; Khan, F.M.; Dennis, G. Accurate Step Count with Generalized and Personalized Deep Learning on Accelerometer Data. Sensors 2022, 22, 3989. [Google Scholar] [CrossRef]
- Mattfeld, R.; Jesch, E.; Hoover, A. A new dataset for evaluating pedometer performance. In Proceedings of the 2017 IEEE International Conference on Bioinformatics and Biomedicine (BIBM), Kansas City, MO, USA, 13–16 November 2017; pp. 865–869. [Google Scholar]
- Patterson, M. Verisense Step Count Algorithm. Available online: https://github.com/ShimmerEngineering/Verisense-Toolbox/tree/master/Verisense_step_algorithm (accessed on 27 September 2022).
- Femiano, R.; Werner, C.; Wilhelm, M.; Eser, P. Validation of open-source step-counting algorithms for wrist-worn tri-axial accelerometers in cardiovascular patients. Gait Posture 2022, 92, 206–211. [Google Scholar] [CrossRef]
- Rowlands, A.V.; Maylor, B.D.; Dawkins, N.P.; Dempsey, P.; Edwardson, C.L.; Soczawa-Stronczyk, A.A.; Bocian, M.; Patterson, M.; Yates, T. Stepping up with GGIR: Validity of step cadence derived from wrist-worn research-grade accelerometers using the Verisense Step Count Algorithm. J. Sports Sci. 2022, 1–9. [Google Scholar] [CrossRef]
- Edwardson, C.L.; Biddle, S.J.H.; Clemes, S.A.; Davies, M.J.; Dunstan, D.W.; Eborall, H.; Granat, M.H.; Gray, L.J.; Healy, G.N.; Jaicim, N.B.; et al. Effectiveness of an intervention for reducing sitting time and improving health in office workers: Three arm cluster randomised controlled trial. BMJ 2022, 378, e069288. [Google Scholar] [CrossRef] [PubMed]
- Rowlands, A.V.; Plekhanova, T.; Yates, T.; Mirkes, E.M.; Davies, M.; Khunti, K.; Edwardson, C.L. Providing a Basis for Harmonization of Accelerometer-Assessed Physical Activity Outcomes Across Epidemiological Datasets. J. Meas. Phys. Behav. 2019, 2, 131–142. [Google Scholar] [CrossRef]
- Ryan, C.G.; Grant, P.M.; Tigbe, W.W.; Granat, M.H. The validity and reliability of a novel activity monitor as a measure of walking. Br. J. Sports Med. 2006, 40, 779–784. [Google Scholar] [CrossRef] [PubMed]
- Steeves, J.A.; Bowles, H.R.; McClain, J.J.; Dodd, K.W.; Brychta, R.J.; Wang, J.; Chen, K.Y. Ability of thigh-worn ActiGraph and activPAL monitors to classify posture and motion. Med. Sci. Sports Exerc. 2015, 47, 952–959. [Google Scholar] [CrossRef]
- Edwardson, C.L.; Rowlands, A.V.; Bunnewell, S.; Sanders, J.; Esliger, D.W.; Gorely, T.; O’Connell, S.; Davies, M.J.; Khunti, K.; Yates, T. Accuracy of Posture Allocation Algorithms for Thigh- and Waist-Worn Accelerometers. Med. Sci. Sports Exerc. 2016, 48, 1085–1090. [Google Scholar] [CrossRef]
- Gu, F.; Khoshelham, K.; Shang, J.; Yu, F.; Wei, Z. Robust and Accurate Smartphone-Based Step Counting for Indoor Localization. IEEE Sens. J. 2017, 17, 3453–3460. [Google Scholar] [CrossRef]
- Maylor, B.D.; Edwardson, C.L.; Dempsey, P.; Patterson, M.; Yates, T.; Rowlands, A.V. A step towards more intuitive physical activity prescription: Validity of stepping-based metrics derived from wrist-worn accelerometry. The 9th International Conference on Ambulatory Monitoring of Physical Activity and Movement. J. Meas. Phys. Behav. 2022, 5, 1–101. [Google Scholar] [CrossRef]
- Migueles, J.H.; Rowlands, A.V.; Huber, F.; Sabia, S.; van Hees, V.T. GGIR: A Research Community–Driven Open Source R Package for Generating Physical Activity and Sleep Outcomes From Multi-Day Raw Accelerometer Data. J. Meas. Phys. Behav. 2019, 2, 188. [Google Scholar] [CrossRef]
- Van Hees, V.T.; Fang, Z.; Langford, J.; Assah, F.; Mohammad, A.; da Silva, I.C.; Trenell, M.I.; White, T.; Wareham, N.J.; Brage, S. Autocalibration of accelerometer data for free-living physical activity assessment using local gravity and temperature: An evaluation on four continents. J. Appl. Physiol. 2014, 117, 738–744. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Nelson, R.K.; Hasanaj, K.; Connolly, G.; Millen, L.; Muench, J.; Bidolli, N.S.C.; Preston, M.A.; Montoye, A.H.K. Comparison of Wrist- and Hip-Worn Activity Monitors When Meeting Step Guidelines. Prev. Chronic Dis. 2022, 19, E18. [Google Scholar] [CrossRef] [PubMed]
- Edwardson, C.L.; Davies, M.; Khunti, K.; Yates, T.; Rowlands, A.V. Steps per Day Measured by Consumer Activity Trackers Worn at the Non-Dominant and Dominant Wrist Relative to a Waist-Worn Pedometer. J. Meas. Phys. Behav. 2018, 1, 2–8. [Google Scholar] [CrossRef]
- O’Connell, S.; Olaighin, G.; Quinlan, L.R. When a Step Is Not a Step! Specificity Analysis of Five Physical Activity Monitors. PLoS ONE 2017, 12, e0169616. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Barreira, T.V.; Schuna, J.M., Jr. Comparison of step outputs for waist and wrist accelerometer attachment sites. Med. Sci. Sports Exerc. 2015, 47, 839–842. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Schuna, J.M., Jr. Steps to preventing type 2 diabetes: Exercise, walk more, or sit less? Front. Endocrinol. 2012, 3, 142. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Petterson, J.L.; Bray, N.W.; Kimmerly, D.S.; O’Brien, M.W. Validity of the activPAL monitor to measure stepping activity and activity intensity: A systematic review. Gait Posture 2022, 97, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Stansfield, B.; Hajarnis, M.; Sudarshan, R. Characteristics of very slow stepping in healthy adults and validity of the activPAL3 activity monitor in detecting these steps. Med. Eng. Phys. 2015, 37, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Edwardson, C.L.; Henson, J.; Bodicoat, D.H.; Bakrania, K.; Khunti, K.; Davies, M.J.; Yates, T. Associations of reallocating sitting time into standing or stepping with glucose, insulin and insulin sensitivity: A cross-sectional analysis of adults at risk of type 2 diabetes. BMJ Open 2017, 7, e014267. [Google Scholar] [CrossRef]
- Healy, G.N.; Winkler, E.A.; Owen, N.; Anuradha, S.; Dunstan, D.W. Replacing sitting time with standing or stepping: Associations with cardio-metabolic risk biomarkers. Eur. Heart J. 2015, 36, 2643–2649. [Google Scholar] [CrossRef]

| Threshold Description | Parameter Unit | Verisense 1 | Verisense 2 |
|---|---|---|---|
| Peak detection threshold | Samples | 3 | 4 |
| Minimum periodicity threshold | Samples | 5 | 4 |
| Maximum periodicity threshold | Samples | 15 | 20 |
| Similarity threshold | G | −0.5 | −1.0 |
| Window size of continuity | Samples | 4 | 4 |
| Number threshold of continuity | Number of windows | 4 | 4 |
| Variance threshold for motion recognition | Variance of G | 0.001 | 0.01 |
| Magnitude threshold | G | 1.2 | 1.25 |
| Characteristic | SMART Work and Life | Wrist Equivalency | STAND UP | Overall |
|---|---|---|---|---|
| N | 640 | 46 | 27 | 713 |
| Age (years) | 44.8 (10.3) | 24.6 (4.5) | 73.3 (4.2) | 44.6 (9.7) |
| Sex, n female | 463 (72.3%) | 29 (63.0%) | 14 (51.9%) | 506 (71.0%) |
| Ethnicity, n White British | 455 (71.1%) | 39 (84.8%) | 14 (51.9%) | 508 (71.2%) |
| BMI (kg/m2) | 26.4 (6.1) | 23.2 (3.8) | 26.4 (3.9) | 26.2 (5.9) |
| Sitting time (min/day) | 603.6 (94.8) | 589.3 (130.0) | 557.2 (116.0) | 601.0 (98.5) |
| Standing time (min/day) | 233.6 (75.6) | 216.1 (76.1) | 300.0 (85.4) | 235.1 (77.1) |
| Stepping time (min/day) | 110.9 (34.0) | 117.8 (52.9) | 114.9 (34.7) | 111.5 (35.5) |
| Average acceleration (mg) | 27.6 (7.9) | 31.1 (9.6) | 25.1 (4.9) | 27.7 (8.0) |
| Intensity gradient | −2.54 (0.23) | −2.38 (0.33) | −2.75 (0.20) | −2.55 (0.24) |
| Outcome | SMART Work and Life | Equivalency | STAND UP | Overall |
|---|---|---|---|---|
| N | 640 | 46 | 27 | 713 |
| N valid days | 4.9 (4.7, 5.0) | 2.1 (1.8, 2.4) | 3.9 (3.2, 4.6) | 4.7 (4.5, 4.8) |
| ActivPAL steps | 9369 (9117, 9622) | 10,345.3 (8924, 11,767) | 7282.7 (6214, 8352) | 9352.2 (9103, 9601) |
| Verisense original algorithm (1) | ||||
| Verisense steps | 10,239 (10,025, 10,454) | 10,829 (9723, 11,935) | 9922 (9052, 10,792) | 10,265 (10,058, 10,472) |
| Mean difference to activPAL | +870 (730, 1009) | +501 (−311, 1313) | +2639 (1789, 3490) | +913 (772, 1054) |
| 95% LoA’s | −2648, 4388 | −4860, 5861 | −1573, 6852 | −2837, 4663 |
| Verisense refined algorithm (2) | ||||
| Verisense steps | 10,056 (99,796, 10,316) | 11,269 (10,017, 12,521) | 8975 (7969, 9981) | 10,093 (9844, 10,344) |
| Mean difference to activPAL | +687 (535, 839) | +942 (150, 1733) | +1692 (749, 2635) | +742 (592, 891) |
| 95% LoA’s | −3139, 4513 | −4280, 6164 | −2982, 6366 | −3235, 4718 |
| Outcome | SMART Work and Life | Equivalency | STAND UP | Overall |
|---|---|---|---|---|
| N | 640 | 46 | 27 | 713 |
| N valid days | 4.9 (4.7, 5.0) | 2.1 (1.8, 2.4) | 3.9 (3.2, 4.6) | 4.7 (4.5, 4.8) |
| ActivPAL MVPA steps | 4309 (4102, 4516) | 5214 (4092, 6336) | 2913 (2110, 3716) | 4306 (4104, 4508) |
| Verisense original algorithm (1) | ||||
| Verisense MVPA steps | 2085 (1979, 2192) | 2426 (1851, 3001) | 1893 (1345, 2442) | 2099 (1995, 2204) |
| Mean difference to activPAL | −2224 (−2074, −2374) | −2788 (−2055, −3521) | −1019 (−662, −1377) | −2207 (−2062, −2351) |
| 95% LoA’s | −6010, +1562 | −7571, +1995 | −2791, +752 | −6055, +1641 |
| Verisense refined algorithm (2) | ||||
| Verisense MVPA steps | 3149 (2999, 3299) | 3935 (3065, 4805) | 2418 (1767, 3070) | 3098 (2954, 3243) |
| Mean difference to activPAL | −1160 (−1061, −1260) | −1279 (−785, −1773) | −494 (−186, −803) | −1204 (−1101, −1307) |
| 95% LoA’s | −3684, +1363 | −4503, +1945 | −2022, +1033 | −3954, +1547 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maylor, B.D.; Edwardson, C.L.; Dempsey, P.C.; Patterson, M.R.; Plekhanova, T.; Yates, T.; Rowlands, A.V. Stepping towards More Intuitive Physical Activity Metrics with Wrist-Worn Accelerometry: Validity of an Open-Source Step-Count Algorithm. Sensors 2022, 22, 9984. https://doi.org/10.3390/s22249984
Maylor BD, Edwardson CL, Dempsey PC, Patterson MR, Plekhanova T, Yates T, Rowlands AV. Stepping towards More Intuitive Physical Activity Metrics with Wrist-Worn Accelerometry: Validity of an Open-Source Step-Count Algorithm. Sensors. 2022; 22(24):9984. https://doi.org/10.3390/s22249984
Chicago/Turabian StyleMaylor, Benjamin D., Charlotte L. Edwardson, Paddy C. Dempsey, Matthew R. Patterson, Tatiana Plekhanova, Tom Yates, and Alex V. Rowlands. 2022. "Stepping towards More Intuitive Physical Activity Metrics with Wrist-Worn Accelerometry: Validity of an Open-Source Step-Count Algorithm" Sensors 22, no. 24: 9984. https://doi.org/10.3390/s22249984
APA StyleMaylor, B. D., Edwardson, C. L., Dempsey, P. C., Patterson, M. R., Plekhanova, T., Yates, T., & Rowlands, A. V. (2022). Stepping towards More Intuitive Physical Activity Metrics with Wrist-Worn Accelerometry: Validity of an Open-Source Step-Count Algorithm. Sensors, 22(24), 9984. https://doi.org/10.3390/s22249984






