Spatial Distribution of Muscular Effects of Acute Whole-Body Electromyostimulation at the Mid-Thigh and Lower Leg—A Pilot Study Applying Magnetic Resonance Imaging
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Randomization and Blinding
2.3. Outcomes
- Intramuscular edema at the mid-thigh;
- Intramuscular edema at the lower leg.
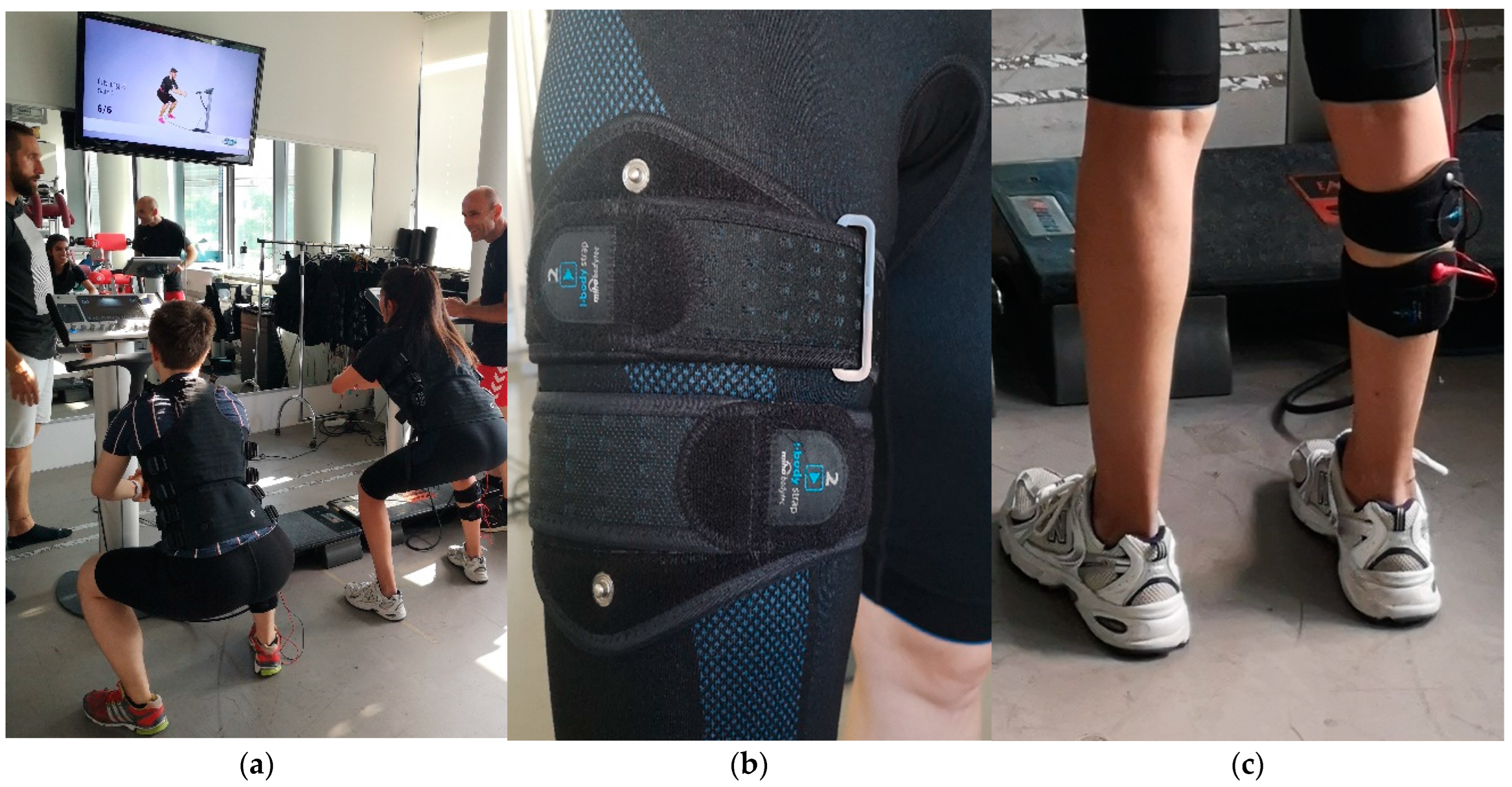
2.4. Intervention
2.5. WB-EMS Application
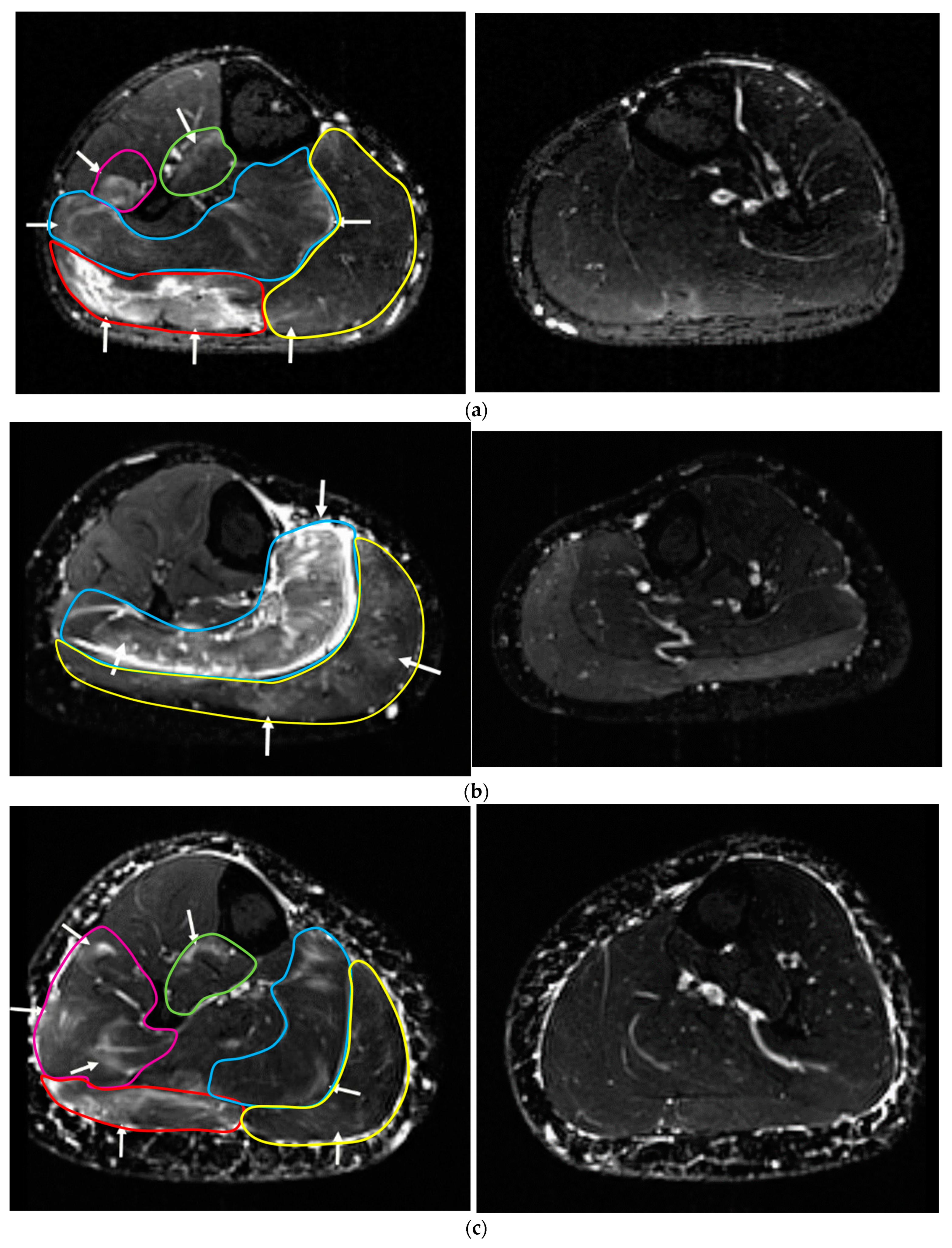
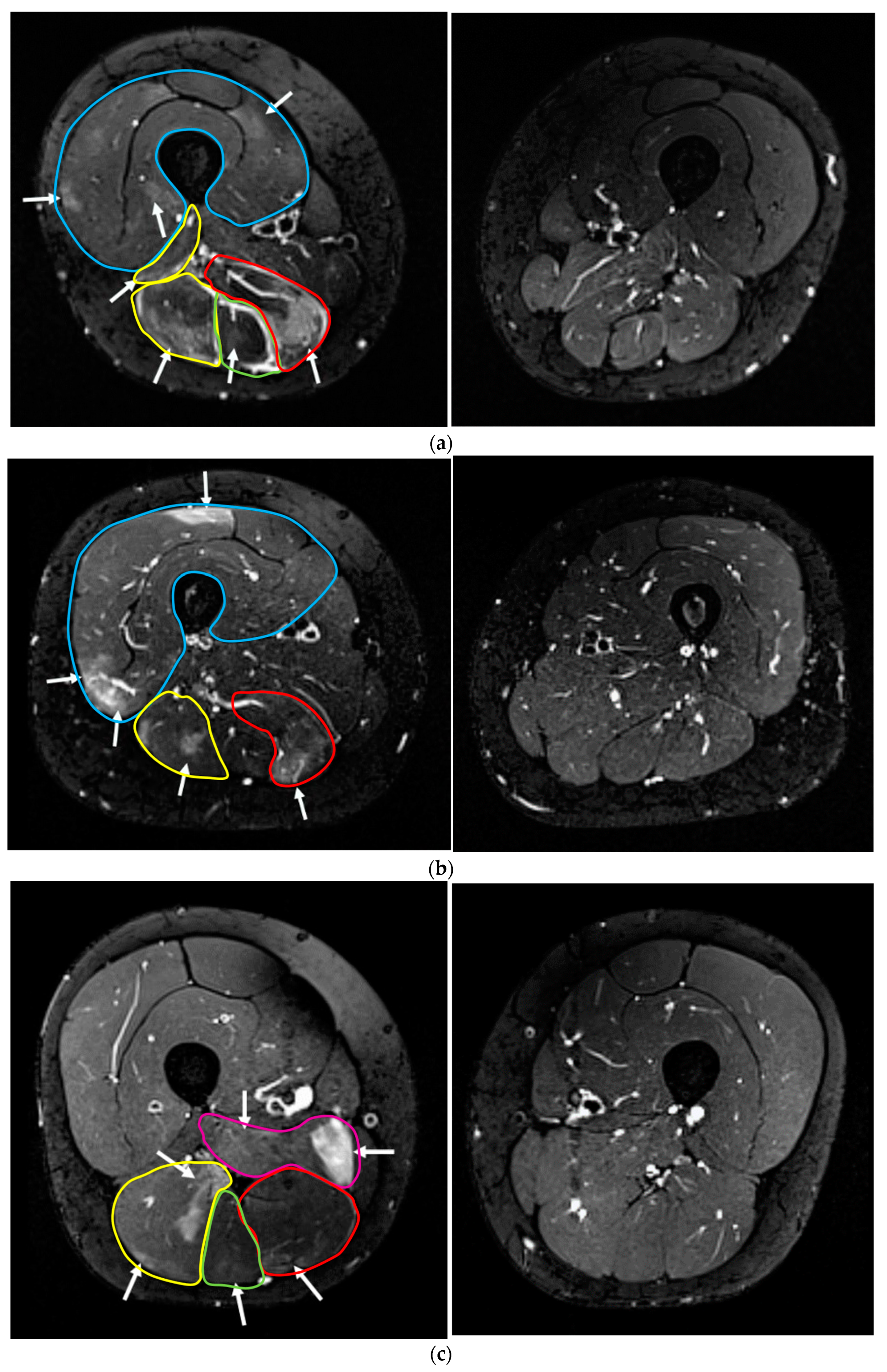
2.6. Semi-Quantitative MRI Analysis
2.7. Statistical Analysis
3. Results
3.1. Compliance with the WB-EMS Protocol
3.2. Baseline MRI Assessment
3.3. Follow-Up MRI Assessment after 72 h
3.3.1. Upper Leg
3.3.2. Lower Leg
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kemmler, W.; Shojaa, M.; Steele, J.; Berger, J.; Fröhlich, M.; Schoene, D.; von Stengel, S.; Kleinöder, H.; Kohl, M. Efficacy of Whole-Body Electromyostimulation (WB-EMS) on body composition and muscle strength in non-athletic adults. A systematic review and meta-analysis. Front. Physiol. 2021, 12, 640657. [Google Scholar] [CrossRef] [PubMed]
- Van Kerkhof, P. Evidenzbasierte Elektrotherapie [Evidence-Based Electrotherapy]; Springer: Berlin/Heidelberg, Germany, 2022. [Google Scholar]
- Kemmler, W.; Kleinoder, H.; Frohlich, M. Editorial: Whole-Body Electromyostimulation: A Training Technology to Improve Health and Performance in Humans? Front. Physiol. 2020, 11, 523. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; Eifler, C.; Fröhlich, M. Ganzkörper-Elektromyostimulation: Effekte, Limitationen, Perspektiven einer Innovativen Trainingsmethode; Springer-Spektrum: Berlin/Heidelberg, Germany, 2022. [Google Scholar]
- Milne, C.J. Rhabdomyolysis, myoglobinuria and exercise. Sport. Med. 1988, 6, 93–106. [Google Scholar] [CrossRef]
- Teschler, M.; Weissenfels, A.; Bebenek, M.; Frohlich, M.; Kohl, M.; von Stengel, S.; Kemmler, W. Very high creatine kinase CK levels after WB_EMS. Are there implications for health. Int. J. Clin. Exp. Med. 2016, 9, 22841–22850. [Google Scholar]
- Konrad, K.L.; Baeyens, J.-P.; Birkenmaier, C.; Ranker, A.H.; Widmann, J.; Leukert, J.; Wenisch, L.; Kraft, E.; Jansson, V.; Wegener, B. The effects of whole-body electromyostimulation (WB-EMS) in comparison to a multimodal treatment concept in patients with non-specific chronic back pain—A prospective clinical intervention study. PLoS ONE 2020, 15, e0236780. [Google Scholar] [CrossRef] [PubMed]
- Micke, F.; Weissenfels, A.; Wirtz, N.; Von Stengel, S.; Dörmann, U.; Kohl, M.; Kleinöder, H.; Donath, L.; Kemmler, W. Similar Pain Intensity Reductions and Trunk Strength Improvements following Whole-Body Electromyostimulation vs. Whole-Body Vibration vs. Conventional Back-Strengthening Training in Chronic Non-specific Low Back Pain Patients: A 3-armed randomized controlled trial. Front. Physiol. 2021, 13, 664991. [Google Scholar] [CrossRef]
- Weissenfels, A.; Teschler, M.; Willert, S.; Hettchen, M.; Frohlich, M.; Kleinoder, H.; Kohl, M.; von Stengel, S.; Kemmler, W. Effects of whole-body electromyostimulation on chronic nonspecific low back pain in adults: A randomized controlled study. J. Pain Res. 2018, 11, 1949–1957. [Google Scholar] [CrossRef]
- Hultman, E.; Sjoholm, H.; Jaderholm-Ek, I.; Krynicki, J. Evaluation of methods for electrical stimulation of human skeletal muscle in situ. Pflug. Arch. 1983, 398, 139–141. [Google Scholar] [CrossRef]
- Gobbo, M.; Gaffurini, P.; Bissolotti, L.; Esposito, F.; Orizio, C. Transcutaneous neuromuscular electrical stimulation: Influence of electrode positioning and stimulus amplitude settings on muscle response. Eur. J. Appl. Physiol. 2011, 111, 2451–2459. [Google Scholar] [CrossRef]
- Zink-Rückel, C.; Chaudry, O.; Engelke, K.; Ghasemikaram, M.; Kohl, M.; Uder, M.; Kemmler, W. Once weekly whole-body electromyostimulation enhance muscle-quality in men. Data of the randomized controlled Franconian EMS and Golf (FREMGO) study. Front. Physiol. 2021; submitted. [Google Scholar]
- Kemmler, W.; Grimm, A.; Bebenek, M.; Kohl, M.; von Stengel, S. Effects of Combined Whole-Body Electromyostimulation and Protein Supplementation on Local and Overall Muscle/Fat Distribution in Older Men with Sarcopenic Obesity: The Randomized Controlled Franconia Sarcopenic Obesity (FranSO) Study. Calcif. Tissue Int. 2018, 103, 266–277. [Google Scholar] [CrossRef]
- Berger, J.; Becker, S.; Ludwig, O.; Kemmler, W.; Frohlich, M. Whole-body electromyostimulation in physical therapy: Do gender, skinfold thickness or body composition influence maximum intensity tolerance? J. Phys. Ther. Sci. 2020, 32, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Guermazi, A.; Roemer, F.W.; Robinson, P.; Tol, J.L.; Regatte, R.R.; Crema, M.D. Imaging of Muscle Injuries in Sports Medicine: Sports Imaging Series. Radiology 2017, 285, 1063. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; Weissenfels, A.; Willert, S.; Fröhlich, M.; Ludwig, O.; Berger, J.; Zart, S.; Becker, S.; Backfisch, M.; Kleinöder, H.; et al. Recommended Contraindications for the Use of Non-Medical WB-Electromyostimulation. Dtsch. Z Sportmed. 2019, 70, 278–281. [Google Scholar] [CrossRef]
- Botter, A.; Oprandi, G.; Lanfranco, F.; Allasia, S.; Maffiuletti, N.A.; Minetto, M.A. Atlas of the muscle motor points for the lower limb: Implications for electrical stimulation procedures and electrode positioning. Eur. J. Appl. Physiol. 2011, 111, 2461–2471. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; Weissenfels, A.; Willert, S.; Shojaa, M.; von Stengel, S.; Filipovic, A.; Kleinöder, H.; Berger, J.; Fröhlich, M. Efficacy and safety of low frequency Whole-Body Electromyostimulation (WB-EMS) to improve health-related outcomes in non-athletic adults. A systematic review. Front. Physiol. 2018, 9, 573. [Google Scholar] [CrossRef]
- Borg, E.; Kaijser, L. A comparison between three rating scales for perceived exertion and two different work tests. Scand. J. Med. Sci. Sport. 2006, 16, 57–69. [Google Scholar] [CrossRef]
- Gerhalter, T.; Marty, B.; Gast, L.V.; Porzelt, K.; Heiss, R.; Uder, M.; Schwab, S.; Carlier, P.G.; Nagel, A.M.; Turk, M. Quantitative (1)H and (23)Na muscle MRI in Facioscapulohumeral muscular dystrophy patients. J. Neurol. 2021, 268, 1076–1087. [Google Scholar] [CrossRef]
- Wang, L.H.; Friedman, S.D.; Shaw, D.; Snider, L.; Wong, C.J.; Budech, C.B.; Poliachik, S.L.; Gove, N.E.; Lewis, L.M.; Campbell, A.E.; et al. MRI-informed muscle biopsies correlate MRI with pathology and DUX4 target gene expression in FSHD. Hum. Mol. Genet. 2019, 28, 476–486. [Google Scholar] [CrossRef]
- Kemmler, W.; Weineck, J.; Kalender, W.A.; Engelke, K. The effect of habitual physical activity, non-athletic exercise, muscle strength, and VO2max on bone mineral density is rather low in early postmenopausal osteopenic women. J. Musculoskelet Neuronal. Interact. 2004, 4, 325–334. [Google Scholar]
- Bickel, C.S.; Gregory, C.M.; Dean, J.C. Motor unit recruitment during neuromuscular electrical stimulation: A critical appraisal. Eur. J. Appl. Physiol. 2011, 111, 2399–2407. [Google Scholar] [CrossRef]
- Coghlan, S.; Crowe, L.; McCarthypersson, U.; Minogue, C.; Caulfield, B. Neuromuscular electrical stimulation training results in enhanced activation of spinal stabilizing muscles during spinal loading and improvements in pain ratings. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2011, 2011, 7622–7625. [Google Scholar] [CrossRef] [PubMed]
- Ogino, M.; Shiba, N.; Maeda, T.; Iwasa, K.; Tagawa, Y.; Matsuo, S.; Nishimura, H.; Yamamoto, T.; Nagata, K.; Basford, J.R. MRI quantification of muscle activity after volitional exercise and neuromuscular electrical stimulation. Am. J. Phys. Med. Rehabil. 2002, 81, 446–451. [Google Scholar] [CrossRef] [PubMed]
- Fuglevand, A.J.; Winter, D.A.; Patla, A.E.; Stashuk, D. Detection of motor unit action potentials with surface electrodes: Influence of electrode size and spacing. Biol. Cybern. 1992, 67, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Denegar, C.; Saliba, E.; Saliba, S.; Denegar, C.; Saliba, S. Therapeutic Modalities for Musculoskeletal Injuries; Human Kinetics: Champaign, IL, USA, 2009. [Google Scholar]
- Maffiuletti, N.A. Physiological and methodological considerations for the use of neuromuscular electrical stimulation. Eur. J. Appl. Physiol. 2010, 110, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Maffiuletti, N.A.; Morelli, A.; Martin, A.; Duclay, J.; Billot, M.; Jubeau, M.; Agosti, F.; Sartorio, A. Effect of gender and obesity on electrical current thresholds. Muscle Nerve 2011, 44, 202–207. [Google Scholar] [CrossRef]
- Bossert, F.P.; Jenrich, W.; Vogedes, K. Leitfaden Elektrotherapie; Urban und Fischer: München, Germany, 2006. [Google Scholar]
- Jubeau, M.; Gondin, J.; Martin, A.; Sartorio, A.; Maffiuletti, N.A. Random motor unit activation by electrostimulation. Int. J. Sport. Med. 2007, 28, 901–904. [Google Scholar] [CrossRef]
- Yadav, R.; Basista, R. Effect of Prolonged Sitting on Hamstring Muscle Flexibility and Lumbar Lordosis in Collegiate Student. Int. J. Health Res. 2020, 10, 280–289. [Google Scholar]
- Raichlen, D.A.; Pontzer, H.; Zdericd, T.W.; Harrise, J.W.; Mabulla, A.Z.; Hamilton, M.T.; Woo, B.A. Sitting, squatting, and the evolutionary biology of human inactivity. Proc. Natl. Acad. Sci. USA 2020, 117, 7115–7121. [Google Scholar] [CrossRef]
- Kemmler, W.; Kleinöder, H. Re: It’s time to regulate the use of whole body electrical stimulation. Whole body electromyostimulation application—The need for more common sense! BMJ 2016, 352, i693. [Google Scholar]
- Kemmler, W.; Teschler, M.; Bebenek, M.; von Stengel, S. (Very) high Creatinkinase concentration after exertional whole-body electromyostimulation application: Health risks and longitudinal adaptations. Wien. Med. Wochenschr. 2015, 165, 427–435. [Google Scholar] [CrossRef]
- Hettchen, M.; Glockler, K.; von Stengel, S.; Piechele, A.; Lotzerich, H.; Kohl, M.; Kemmler, W. Effects of Compression Tights on Recovery Parameters after Exercise Induced Muscle Damage: A Randomized Controlled Crossover Study. Evid.–Based Complement. Altern. Med. 2019, 2019, 5698460. [Google Scholar] [CrossRef] [PubMed]
| MRI-Scan I | WB-EMS Application | Rest Period | MRI-Scan II |
|---|---|---|---|
| Baseline | Immediately after MRT | After WB-EMS—72 h | 72 h post |
| Variable | Women | Men | ||
|---|---|---|---|---|
| MV ± SD, Number | Range | MV ± SD, Number | Range | |
| Gender | 5 | --------- | 3 | ---------- |
| Age [years] | 26.4 ± 2.8 | 24–31 | 24.0 ± 1.0 | 23–25 |
| Body height [cm] 1 | 166.5 ± 3.5 | 163–171 | 178.7 ± 12.2 | 168–192 |
| Body mass [kg] 2 | 59.2 ± 7.0 | 50.7–69.9 | 77.0 ± 12.9 | 67.2–91.6 |
| Total body-fat [%] 1 | 21.5 ± 2.6 | 19.4–25.8 | 20.2 ± 5.5 | 13.8–26.8 |
| Physical activity 3 | 4.4 ± 0.5 | 4–5 | 3.3 ± 1.5 | 2–5 |
| Physical fitness 3 | 4.4 ± 0.6 | 4–5 | 4.7 ± 0.6 | 4–5 |
| Exercise [sessions/w] 4 | 2.1 ± 1.9 | 0–5 | 2.2 ± 1.3 | 1–4 |
| Diseases [n] 4 | 0 | ------------ | 0 | ------------ |
| Medication [n] 4 | 0 | ------------ | 0 | ------------ |
| Smokers [n] 4 | 0 | ------------ | 0 | ------------ |
| Compartment of the Edema | Participants with Edema (Total: n = 8) | Maximum Depth of the Edema from Skin (mm) MV ± SD, (Range) | Intramuscular Edema Volume (Grading) MV (Range) |
|---|---|---|---|
| m. vastus lateralis | 4 | 29 ± 9; 19–39 | 1 (1) |
| m. vastus medialis | 2 | 25; 47 | 1 (1) |
| m. vastus intermedialis | 1 | 61 | 1 |
| m. rectus femoris | 0 | ------- | -------- |
| m. biceps femoris | 6 | 50 ± 12; 39–72 | 1 (1) |
| m. semimembranosus | 5 | 31 ± 6; 23–37 | 1 (1) |
| m. semitendinosus | 3 | 37 ± 6; 32–44 | 1 (1) |
| m. adductor magnus | 2 | 46; 68 | 1 (1) |
| Compartment of the Edema | Participants with Edema (Total: n = 8) | Maximum Depth of the Edema from Skin (mm) MV ± SD, (Range) | Intramuscular Edema Volume Grading MV (Range) |
|---|---|---|---|
| m. gastrocnemius medialis | 8 | 24 ± 5; (18–33) | 1 (1) |
| m. gastrocnemius lateralis | 7 | 26 ± 4; (21–31) | 1.3 (1–2) |
| m. soleus | 6 | 35 ± 14; (19–51) | 1.2 (1–2) |
| m. peroneus longus | 4 | 31 ± 4; (25–35) | 1 (1) |
| m. extensor digitorum | 1 | 25 | 1 (1) |
| m. tibialis posterior | 2 | 42; 56 | 1 (1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Götz, M.; Heiss, R.; von Stengel, S.; Roemer, F.; Berger, J.; Nagel, A.; Uder, M.; Kemmler, W. Spatial Distribution of Muscular Effects of Acute Whole-Body Electromyostimulation at the Mid-Thigh and Lower Leg—A Pilot Study Applying Magnetic Resonance Imaging. Sensors 2022, 22, 10017. https://doi.org/10.3390/s222410017
Götz M, Heiss R, von Stengel S, Roemer F, Berger J, Nagel A, Uder M, Kemmler W. Spatial Distribution of Muscular Effects of Acute Whole-Body Electromyostimulation at the Mid-Thigh and Lower Leg—A Pilot Study Applying Magnetic Resonance Imaging. Sensors. 2022; 22(24):10017. https://doi.org/10.3390/s222410017
Chicago/Turabian StyleGötz, Marina, Rafael Heiss, Simon von Stengel, Frank Roemer, Joshua Berger, Armin Nagel, Michael Uder, and Wolfgang Kemmler. 2022. "Spatial Distribution of Muscular Effects of Acute Whole-Body Electromyostimulation at the Mid-Thigh and Lower Leg—A Pilot Study Applying Magnetic Resonance Imaging" Sensors 22, no. 24: 10017. https://doi.org/10.3390/s222410017
APA StyleGötz, M., Heiss, R., von Stengel, S., Roemer, F., Berger, J., Nagel, A., Uder, M., & Kemmler, W. (2022). Spatial Distribution of Muscular Effects of Acute Whole-Body Electromyostimulation at the Mid-Thigh and Lower Leg—A Pilot Study Applying Magnetic Resonance Imaging. Sensors, 22(24), 10017. https://doi.org/10.3390/s222410017








