Exploring Endothelial Expansion on a Chip
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Culture
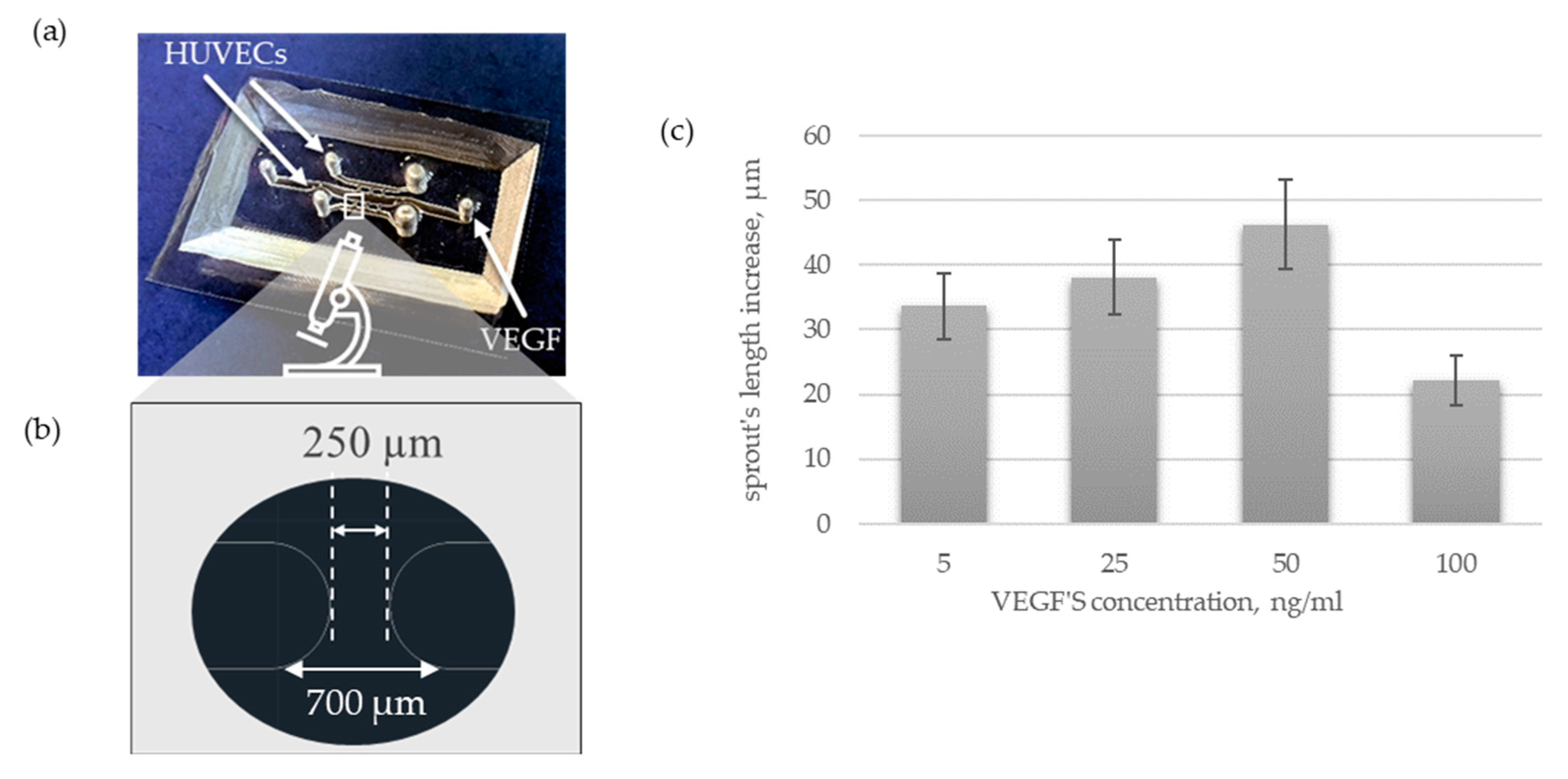
2.2. Manufacture of a Microplatform
2.3. Lumen’s Formation
2.4. HUVECs Loading and Its Culture within a Microfluidic Platform
2.5. Pro-Angiogenic Agent Loading
2.6. Analysis of Cell Behavior and Their Morphology
2.7. Statistical Analysis
3. Results
3.1. Vascularization under Microflow Conditions
3.1.1. Lumen Formation
3.1.2. HUVECs Loading
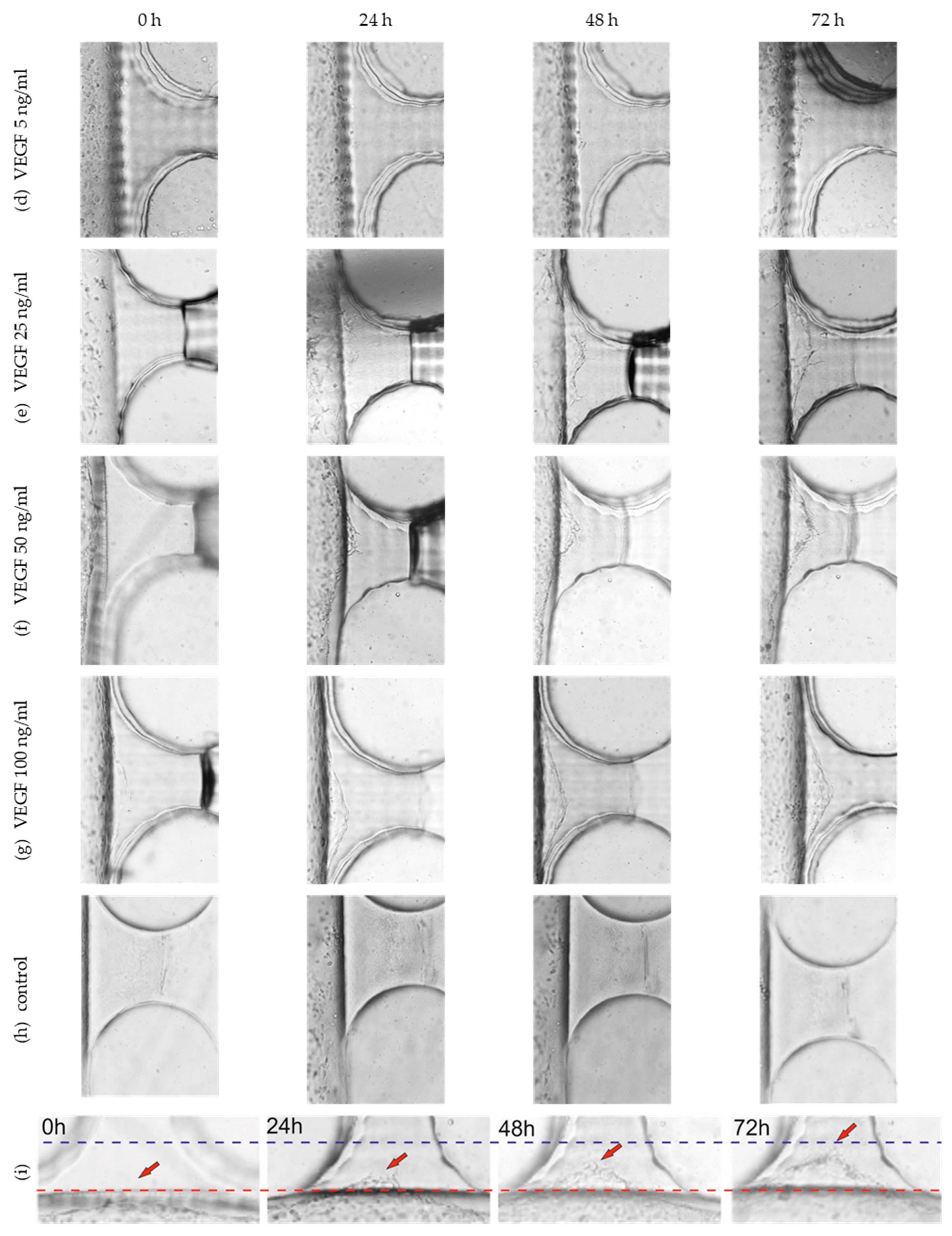
3.2. Angiogenesis under Microflow Conditions
3.2.1. Design and Manufacture of a Microplatform
3.2.2. Angiogenic Activation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Warmke, N.; Walker, A.M.N.; Cubbon, R.M.; Kingdom, U. Angiogenesis. Encycl. Cardiovasc. Res. Med. 2018, 85–96. [Google Scholar] [CrossRef]
- DiPietro, L.A. Angiogenesis and Wound Repair: When Enough Is Enough. J. Leukoc. Biol. 2016, 100, 979–984. [Google Scholar] [CrossRef] [PubMed]
- Chung, A.S.; Ferrara, N. Developmental and Pathological Angiogenesis. Annu. Rev. Cell Dev. Biol. 2011, 27, 563–584. [Google Scholar] [CrossRef] [PubMed]
- Colin-Pierre, C.; Berthélémy, N.; Belloy, N.; Danoux, L.; Bardey, V.; Rivet, R.; Mine, S.; Jeanmaire, C.; Maquart, F.X.; Ramont, L.; et al. The Glypican-1/HGF/C-Met and Glypican-1/VEGF/VEGFR2 Ternary Complexes Regulate Hair Follicle Angiogenesis. Front. Cell Dev. Biol. 2021, 9, 781172. [Google Scholar] [CrossRef]
- Nanas, S.; Philippou, A. Exercise Training Enhances Angiogenesis-Related Gene Heart Failure. Cells 2021, 10, 1915. [Google Scholar]
- Johnson, K.E.; Wilgus, T.A. Vascular Endothelial Growth Factor and Angiogenesis in the Regulation of Cutaneous Wound Repair. Adv. Wound Care 2014, 3, 647–661. [Google Scholar] [CrossRef]
- Felmeden, D.C.; Blann, A.D.; Lip, G.Y.H. Angiogenesis: Basic Pathophysiology and Implications for Disease. Eur. Heart J. 2003, 24, 586–603. [Google Scholar] [CrossRef]
- Lugano, R.; Ramachandran, M.; Dimberg, A. Tumor Angiogenesis: Causes, Consequences, Challenges and Opportunities. Cell. Mol. Life Sci. 2020, 77, 1745–1770. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2021. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef]
- Joshi, P.N. Cells and Organs on Chip—A Revolutionary Platform for Biomedicine. In Lab-on-a-Chip Fabrication and Application; InTech: London, UK, 2016. [Google Scholar]
- Pollet, A.; den Toonder, J. Recapitulating the Vasculature Using Organ-on-Chip Technology. Bioengineering 2020, 7, 17. [Google Scholar] [CrossRef] [PubMed]
- Tu, T.Y.; Wang, Z.; Bai, J.; Sun, W.; Peng, W.K.; Huang, R.Y.J.; Thiery, J.P.; Kamm, R.D. Rapid Prototyping of Concave Microwells for the Formation of 3D Multicellular Cancer Aggregates for Drug Screening. Adv. Healthc. Mater. 2014, 3, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.; Ho, L.; Moinuddin, S.M.; Sarkar, T.; Saha, D.; Ahsan, F. Multicellular Cell Seeding on a Chip: New Design and Optimization towards Commercialization. Biosensors 2022, 12, 587. [Google Scholar] [CrossRef]
- Jensen, C.; Teng, Y. Is It Time to Start Transitioning From 2D to 3D Cell Culture? Front. Mol. Biosci. 2020, 7, 33. [Google Scholar] [CrossRef]
- Baeriswyl, V.; Christofori, G. The Angiogenic Switch in Carcinogenesis. Semin. Cancer Biol. 2009, 19, 329–337. [Google Scholar] [CrossRef]
- Gordon, E.; Schimmel, L.; Frye, M. The Importance of Mechanical Forces for in Vitro Endothelial Cell Biology. Front. Physiol. 2020, 11, 684. [Google Scholar] [CrossRef] [PubMed]
- Song, J.W.; Munn, L.L. Fluid Forces Control Endothelial Sprouting. Proc. Natl. Acad. Sci. USA 2011, 108, 15342–15347. [Google Scholar] [CrossRef] [PubMed]
- Galie, P.A.; Nguyen, D.H.T.; Choi, C.K.; Cohen, D.M.; Janmey, P.A.; Chen, C.S. Fluid Shear Stress Threshold Regulates Angiogenic Sprouting. Proc. Natl. Acad. Sci. USA 2014, 111, 7968–7973. [Google Scholar] [CrossRef] [PubMed]
- Priyadarshani, J.; Awasthi, P.; Karan, P.; Das, S.; Chakraborty, S. Transport of Vascular Endothelial Growth Factor Dictates On-Chip Angiogenesis in Tumor Microenvironment. Phys. Fluids 2021, 33, 031910. [Google Scholar] [CrossRef]
- Madu, C.O.; Wang, S.; Madu, C.O.; Lu, Y. Angiogenesis in Breast Cancer Progression, Diagnosis, and Treatment. J. Cancer 2020, 11, 4474–4494. [Google Scholar] [CrossRef]
- Liu, Y.; Li, J.; Zhou, J.; Liu, X.; Li, H.; Lu, Y.; Lin, B.; Li, X.; Liu, T. Angiogenesis and Functional Vessel Formation Induced by Interstitial Flow and Vascular Endothelial Growth Factor Using a Microfluidic Chip. Micromachines 2022, 13, 225. [Google Scholar] [CrossRef] [PubMed]
- Devadas, D.; Moore, T.A.; Walji, N.; Young, E.W.K. A Microfluidic Mammary Gland Coculture Model Using Parallel 3D Lumens for Studying Epithelial-Endothelial Migration in Breast Cancer. Biomicrofluidics 2019, 13, 064122. [Google Scholar] [CrossRef] [PubMed]
- Abe, Y.; Watanabe, M.; Chung, S.; Kamm, R.D.; Tanishita, K.; Sudo, R. Balance of Interstitial Flow Magnitude and Vascular Endothelial Growth Factor Concentration Modulates Three-Dimensional Microvascular Network Formation. APL Bioeng. 2019, 3, 036102. [Google Scholar] [CrossRef] [PubMed]
- Pauty, J.; Usuba, R.; Cheng, I.G.; Hespel, L.; Takahashi, H.; Kato, K.; Kobayashi, M.; Nakajima, H.; Lee, E.; Yger, F.; et al. A Vascular Endothelial Growth Factor-Dependent Sprouting Angiogenesis Assay Based on an In Vitro Human Blood Vessel Model for the Study of Anti-Angiogenic Drugs. eBioMedicine 2018, 27, 225–236. [Google Scholar] [CrossRef] [PubMed]
- Nakatsu, M.N.; Sainson, R.C.A.; Aoto, J.N.; Taylor, K.L.; Aitkenhead, M.; Pérez-del-Pulgar, S.; Carpenter, P.M.; Hughes, C.C.W. Angiogenic Sprouting and Capillary Lumen Formation Modeled by Human Umbilical Vein Endothelial Cells (HUVEC) in Fibrin Gels: The Role of Fibroblasts and Angiopoietin-1. Microvasc. Res. 2003, 66, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.C.; Sohn, H.A.; Park, Z.Y.; Oh, S.; Kang, Y.K.; Lee, K.M.; Kang, M.; Jang, Y.J.; Yang, S.J.; Hong, Y.K.; et al. A Lactate-Induced Response to Hypoxia. Cell 2015, 161, 595–609. [Google Scholar] [CrossRef]
- Krock, B.L.; Skuli, N.; Simon, M.C. Hypoxia-Induced Angiogenesis: Good and Evil. Genes Cancer 2011, 2, 1117–1133. [Google Scholar] [CrossRef]
- Polet, F.; Feron, O. Endothelial Cell Metabolism and Tumour Angiogenesis: Glucose and Glutamine as Essential Fuels and Lactate as the Driving Force. J. Intern. Med. 2013, 273, 156–165. [Google Scholar] [CrossRef]
- Yehya, A.H.S.; Asif, M.; Petersen, S.H.; Subramaniam, A.V.; Kono, K.; Majid, A.M.S.A.; Oon, C.E. Angiogenesis: Managing the Culprits behind Tumorigenesis and Metastasis. Medicina 2018, 54, 8. [Google Scholar] [CrossRef]
- Hanahan, D.; Folkman, J. Patterns and Emerging Mechanisms of the Angiogenic Switch during Tumorigenesis. Cell 1996, 86, 353–364. [Google Scholar] [CrossRef]
- Nashimoto, Y.; Okada, R.; Hanada, S.; Arima, Y.; Nishiyama, K.; Miura, T.; Yokokawa, R. Vascularized Cancer on a Chip: The Effect of Perfusion on Growth and Drug Delivery of Tumor Spheroid. Biomaterials 2020, 229, 119547. [Google Scholar] [CrossRef] [PubMed]
- Bischel, L.L.; Lee, S.H.; Beebe, D.J. A Practical Method for Patterning Lumens through ECM Hydrogels via Viscous Finger Patterning. J. Lab. Autom. 2012, 17, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Myers, D.R.; Lam, W.A. Vascularized Microfluidics and Their Untapped Potential for Discovery in Diseases of the Microvasculature. Annu. Rev. Biomed. Eng. 2021, 23, 407–432. [Google Scholar] [CrossRef] [PubMed]
- Kwak, T.J.; Lee, E. In Vitro Modeling of Solid Tumor Interactions with Perfused Blood Vessels. Sci. Rep. 2020, 10, 20142. [Google Scholar] [CrossRef]
- Miller, C.P.; Tsuchida, C.; Zheng, Y.; Himmelfarb, J.; Akilesh, S. A 3D Human Renal Cell Carcinoma-on-a-Chip for the Study of Tumor Angiogenesis. Neoplasia 2018, 20, 610–620. [Google Scholar] [CrossRef]
- Gadde, M.; Phillips, C.; Ghousifam, N.; Sorace, A.G.; Wong, E.; Krishnamurthy, S.; Syed, A.; Rahal, O.; Yankeelov, T.E.; Woodward, W.A.; et al. In Vitro Vascularized Tumor Platform for Modeling Tumor-Vasculature Interactions of Inflammatory Breast Cancer. Biotechnol. Bioeng. 2020, 117, 3572–3590. [Google Scholar] [CrossRef]
- Park, S.; Kim, T.H.; Kim, S.H.; You, S.; Jung, Y. Three-Dimensional Vascularized Lung Cancer-on-a-Chip with Lung Extracellular Matrix Hydrogels for in Vitro Screening. Cancers 2021, 13, 3930. [Google Scholar] [CrossRef]
- Kim, D.; Hwang, K.S.; Seo, E.U.; Seo, S.; Lee, B.C.; Choi, N.; Choi, J.; Kim, H.N. Vascularized Lung Cancer Model for Evaluating the Promoted Transport of Anticancer Drugs and Immune Cells in an Engineered Tumor Microenvironment. Adv. Healthc. Mater. 2022, 11, 2102581. [Google Scholar] [CrossRef]
- Moses, S.R.; Adorno, J.J.; Palmer, A.F.; Song, J.W. Vessel-on-a-Chip Models for Studying Microvascular Physiology, Transport, and Function in Vitro. Am. J. Physiol. Cell Physiol. 2021, 320, C92–C105. [Google Scholar] [CrossRef]
- Apte, R.S.; Chen, D.S.; Ferrara, N. VEGF in Signaling and Disease: Beyond Discovery and Development. Cell 2019, 176, 1248–1264. [Google Scholar] [CrossRef]
- Ferrara, N. VEGF and the Quest for Tumour Angiogenesis Factors. Nat. Rev. Cancer 2002, 2, 795–803. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; Liu, X.; Zhang, X.; Wang, L.; Su, H.; Wang, L.; He, N.; Zhang, D.; Li, Z.; Kang, H.; et al. Flow Shear Stress Controls the Initiation of Neovascularization: Via Heparan Sulfate Proteoglycans within a Biomimetic Microfluidic Model. Lab Chip 2021, 21, 421–434. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-H.; Lei, K.F. Quantitative Study of Angiogenesis in Three-Dimensional Matrigel Barrier Using Electric Impedance Measurement Technique. SSRN Electron. J. 2022, 370, 132458. [Google Scholar] [CrossRef]
- Liu, L.; Xie, Z.; Zhang, W.; Fang, S.; Kong, J.; Jin, D.; Li, J.; Li, X.; Yang, X.; Luo, Y.; et al. Biomimetic Tumor-Induced Angiogenesis and Anti-Angiogenic Therapy in a Microfluidic Model. RSC Adv. 2016, 6, 35248–35256. [Google Scholar] [CrossRef]
- Chung, M.; Ahn, J.; Son, K.; Kim, S.; Jeon, N.L. Biomimetic Model of Tumor Microenvironment on Microfluidic Platform. Adv. Healthc. Mater. 2017, 6, 1700196. [Google Scholar] [CrossRef]
- Lee, S.; Kim, S.; Koo, D.J.; Yu, J.; Cho, H.; Lee, H.; Song, J.M.; Kim, S.Y.; Min, D.H.; Jeon, N.L. 3D Microfluidic Platform and Tumor Vascular Mapping for Evaluating Anti-Angiogenic RNAi-Based Nanomedicine. ACS Nano 2021, 15, 338–350. [Google Scholar] [CrossRef]
- Yeon, J.H.; Ryu, H.R.; Chung, M.; Hu, Q.P.; Jeon, N.L. In Vitro Formation and Characterization of a Perfusable Three-Dimensional Tubular Capillary Network in Microfluidic Devices. Lab Chip 2012, 12, 2815–2822. [Google Scholar] [CrossRef]
- Sano, E.; Mori, C.; Nashimoto, Y.; Yokokawa, R.; Kotera, H.; Torisawa, Y.S. Engineering of Vascularized 3D Cell Constructs to Model Cellular Interactions through a Vascular Network. Biomicrofluidics 2018, 12, 042204. [Google Scholar] [CrossRef]




| Central | Lateral | Migrating Ports | |||
|---|---|---|---|---|---|
| microplatform 1 | lenghth | Designed | 1.8 cm | 1.6 cm | 300.00 µm |
| Patterned | not measured. | not measured. | 287.07 µm | ||
| height | Designed | 1000.00 µm | 1000.00 µm | 1000.00 µm | |
| Patterned | 998.33 µm | 998.33 µm | 998.33 µm | ||
| width | Designed | 1000.00 µm | 1000.00 µm | 50.00 µm | |
| Patterned | 1007.22 µm | 1025.13 µm | 49.12 µm | ||
| microplatform 2 | lenghth | Designed | 0.75 cm | 1 cm | 500.00 µm |
| Patterned | not measured. | not measured. | 494.05 µm | ||
| height | Designed | 500.00 µm | 500.00 µm | 500.00 µm | |
| patterned | 496.27 µm | 496.27 µm | 497.36 µm | ||
| width | Designed | 1000.00 µm | 500.00 µm | 500.00 µm | |
| patterned | 1014.67 µm | 503.23 µm | 487.64 µm | ||
| microplatform 3 | lenghth | Designed | 1.8 cm | 1 cm | 500.00 µm |
| Patterned | not meausred. | not meausred. | 496.72 µm | ||
| height | Designed | 1000.00 µm | 500.00 µm | 250.00 µm | |
| Patterned | 1033.47 µm | 505.93 µm | 243.30µm | ||
| width | Designed | 1000.00 µm | 500.00 µm | 250.00 µm | |
| Patterned | 979.05 µm | 507.26 µm | 273.20 µm |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Konopka, J.; Kołodziejek, D.; Flont, M.; Żuchowska, A.; Jastrzębska, E.; Brzózka, Z. Exploring Endothelial Expansion on a Chip. Sensors 2022, 22, 9414. https://doi.org/10.3390/s22239414
Konopka J, Kołodziejek D, Flont M, Żuchowska A, Jastrzębska E, Brzózka Z. Exploring Endothelial Expansion on a Chip. Sensors. 2022; 22(23):9414. https://doi.org/10.3390/s22239414
Chicago/Turabian StyleKonopka, Joanna, Dominik Kołodziejek, Magdalena Flont, Agnieszka Żuchowska, Elżbieta Jastrzębska, and Zbigniew Brzózka. 2022. "Exploring Endothelial Expansion on a Chip" Sensors 22, no. 23: 9414. https://doi.org/10.3390/s22239414
APA StyleKonopka, J., Kołodziejek, D., Flont, M., Żuchowska, A., Jastrzębska, E., & Brzózka, Z. (2022). Exploring Endothelial Expansion on a Chip. Sensors, 22(23), 9414. https://doi.org/10.3390/s22239414








