Validity of the Wrist-Worn Polar Vantage V2 to Measure Heart Rate and Heart Rate Variability at Rest
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
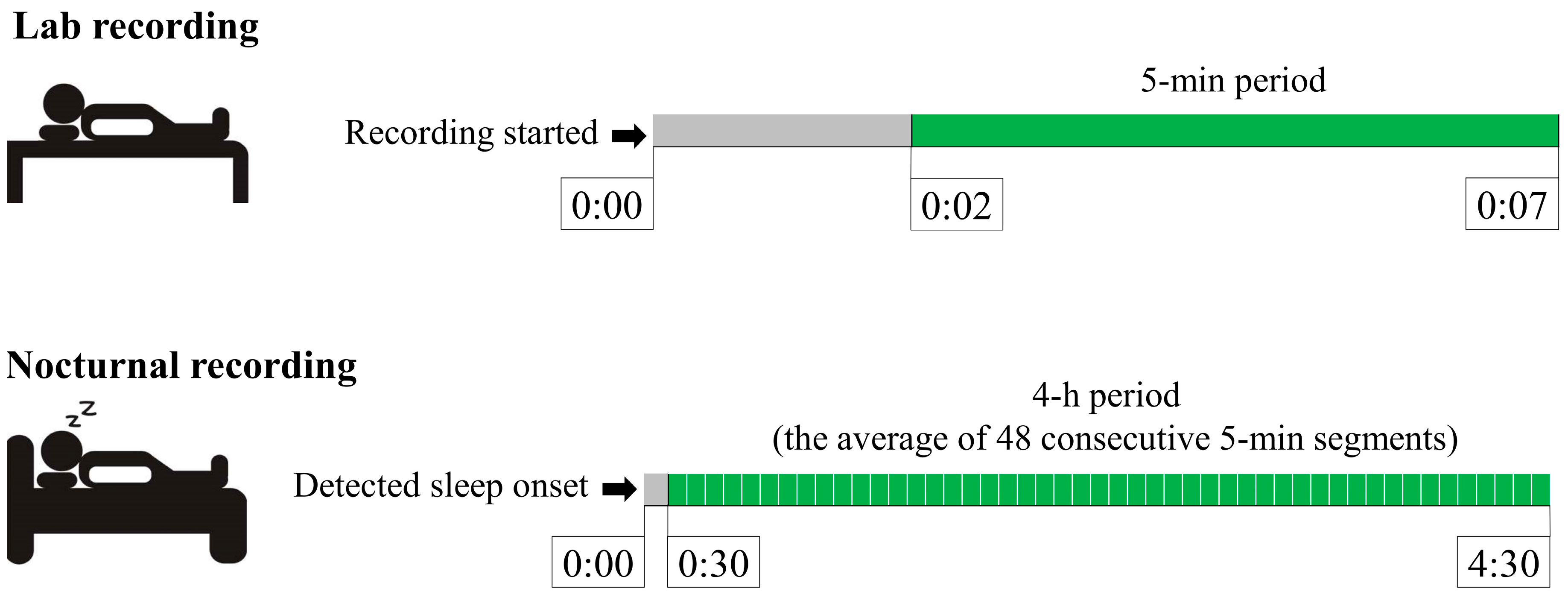
2.2. Experimental Overview
2.3. HRV Analysis
2.4. Statistical Analysis
3. Results
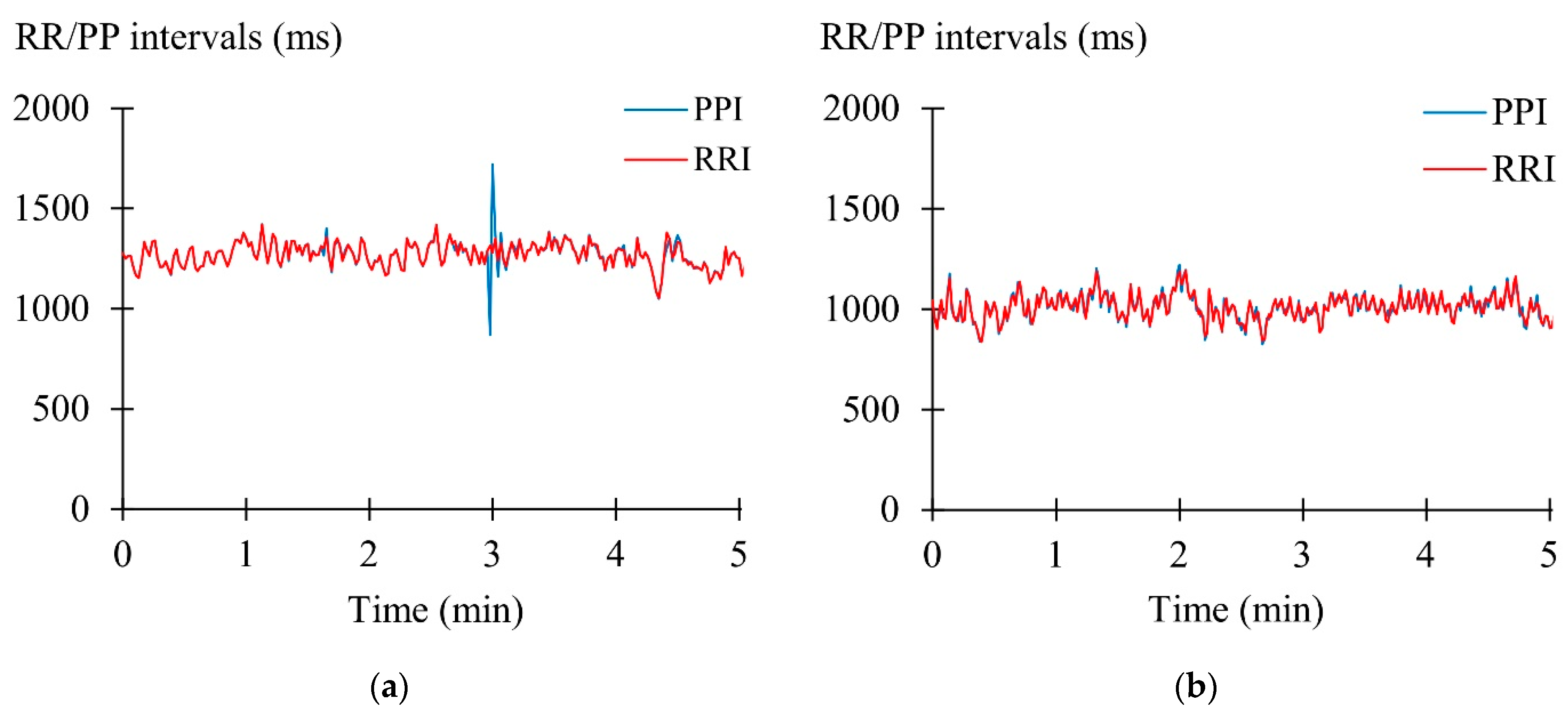
3.1. Laboratory Recordings
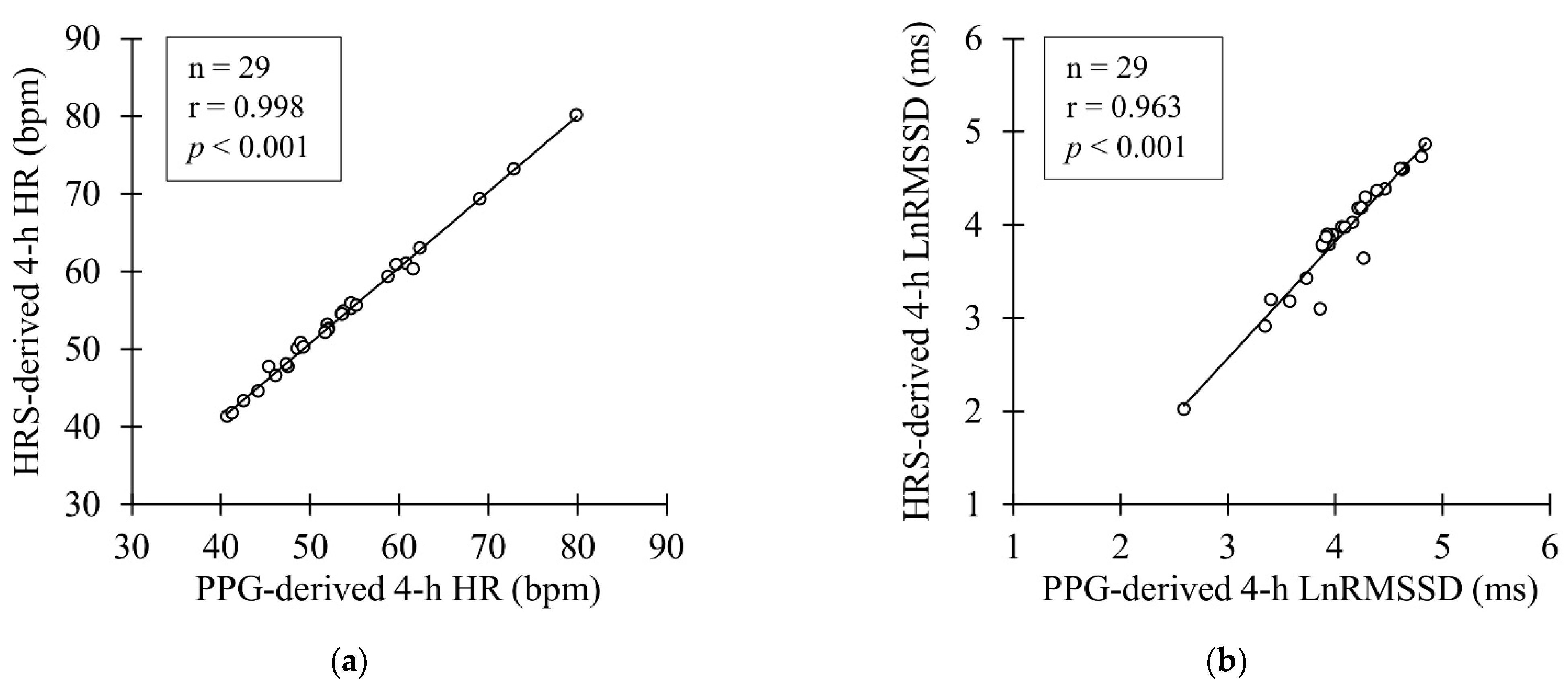
3.2. Nocturnal Recordings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thompson, W.R. FACSM worldwide survey of fitness trends for 2021. ACSMs Health Fit. J. 2021, 25, 10–19. [Google Scholar] [CrossRef]
- Fuller, D.; Colwell, E.; Low, J.; Orychock, K.; Tobin, M.A.; Simango, B.; Buote, R.; Van Heerden, D.; Luan, H.; Cullen, K.; et al. Reliability and validity of commercially available wearable devices for measuring steps, energy expenditure, and heart rate: Systematic review. JMIR Mhealth Uhealth 2020, 8, e18694. [Google Scholar] [CrossRef]
- Henriksen, A.; Mikalsen, M.H.; Woldaregay, A.Z.; Muzny, M.; Hartvigsen, G.; Hopstock, L.A.; Grimsgaard, S. Using fitness trackers and smartwatches to measure physical activity in research: Analysis of consumer wrist-worn wearables. J. Med. Internet Res. 2018, 20, e9157. [Google Scholar] [CrossRef] [PubMed]
- Martinmäki, K.; Rusko, H.; Kooistra, L.; Kettunen, J.; Saalasti, S. Intraindividual validation of heart rate variability indexes to measure vagal effects on hearts. Am. J. Physiol. Heart Circ. Physiol. 2006, 290, 640–647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altini, M.; Plews, D. What is behind changes in resting heart rate and heart rate variability? A large-scale analysis of longitudinal measurements acquired in free-living. Sensors 2021, 21, 7932. [Google Scholar] [CrossRef] [PubMed]
- Tulppo, M.P.; Kiviniemi, A.M.; Junttila, M.J.; Huikuri, H.V. Home monitoring of heart rate as a predictor of imminent cardiovascular events. Front. Physiol. 2019, 10, 341. [Google Scholar] [CrossRef] [PubMed]
- Binici, Z.; Mouridsen, M.R.; Køber, L.; Sajadieh, A. Decreased nighttime heart rate variability is associated with increased stroke risk. Stroke 2011, 42, 3196–3201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Wu, H.; Zhang, X.; Wei, X.; Hou, F.; Ma, Y. Sleep heart rate variability assists the automatic prediction of long-term cardiovascular outcomes. Sleep Med. 2020, 67, 217–224. [Google Scholar] [CrossRef]
- da Silva, D.F.; Ferraro, Z.M.; Adamo, K.B.; Machado, F.A. Endurance running training individually guided by HRV in untrained women. J. Strength Cond. Res. 2019, 33, 736–746. [Google Scholar] [CrossRef]
- Kiviniemi, A.M.; Hautala, A.J.; Kinnunen, H.; Tulppo, M.P. Endurance training guided individually by daily heart rate variability measurements. Eur. J. Appl. Physiol. 2007, 101, 743–751. [Google Scholar] [CrossRef]
- Javaloyes, A.; Sarabia, J.M.; Lamberts, R.P.; Moya-Ramon, M. Training prescription guided by heart-rate variability in cycling. Int J. Sports Physiol. Perform. 2019, 14, 23–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stone, J.D.; Ulman, H.K.; Tran, K.; Thompson, A.G.; Halter, M.D.; Ramadan, J.H.; Stephenson, M.; Finomore, V.S., Jr.; Galster, S.M.; Rezai, A.R.; et al. Assessing the accuracy of popular commercial technologies that measure resting heart rate and heart rate variability. Front. Sports Act. Living 2021, 3, 585870. [Google Scholar] [CrossRef] [PubMed]
- Bent, B.; Goldstein, B.A.; Kibbe, W.A.; Dunn, J.P. Investigating sources of inaccuracy in wearable optical heart rate sensors. NPJ Digit. Med. 2020, 3, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuda, E.; Shibata, M.; Ogata, Y.; Ueda, N.; Yambe, T.; Yoshizawa, M.; Hayano, J. Pulse rate variability: A new biomarker, not a surrogate for heart rate variability. J. Physiol. Anthropol. 2020, 39, 21. [Google Scholar] [CrossRef] [PubMed]
- Plews, D.J.; Scott, B.; Altini, M.; Wood, M.; Kilding, A.E.; Laursen, P.B. Comparison of heart-rate-variability recording with smartphone photoplethysmography, polar H7 chest strap, and electrocardiography. Int. J. Sports Physiol. Perform. 2017, 12, 1324–1328. [Google Scholar] [CrossRef]
- Kinnunen, H.; Rantanen, A.; Kenttä, T.; Koskimäki, H. Feasible assessment of recovery and cardiovascular health: Accuracy of nocturnal HR and HRV assessed via ring PPG in comparison to medical grade ECG. Physiol. Meas. 2020, 41, 04NT01. [Google Scholar] [CrossRef] [PubMed]
- Hernando, D.; Roca, S.; Sancho, J.; Alesanco, Á.; Bailón, R. Validation of the apple watch for heart rate variability measurements during relax and mental stress in healthy subjects. Sensors 2018, 18, 2619. [Google Scholar] [CrossRef] [Green Version]
- Bellenger, C.R.; Miller, D.; Halson, S.L.; Roach, G.; Sargent, C. Wrist-based photoplethysmography assessment of heart rate and heart rate variability: Validation of WHOOP. Sensors 2021, 21, 3571. [Google Scholar] [CrossRef]
- Vesterinen, V.; Rinkinen, N.; Nummela, A. A contact-free, ballistocardiography-based monitoring system (Emfit QS) for measuring nocturnal heart rate and heart rate variability: Validation study. JBME 2020, 5, e16620. [Google Scholar] [CrossRef]
- Schäfer, A.; Vagedes, J. How accurate is pulse rate variability as an estimate of heart rate variability? A review on studies comparing photoplethysmographic technology with an electrocardiogram. Int. J. Cardiol. 2013, 166, 15–29. [Google Scholar] [CrossRef]
- Wang, R.; Blackburn, G.; Desai, M.; Phelan, D.; Gillinov, L.; Houghtaling, P.; Gillinov, M. Accuracy of wrist-worn heart rate monitors. JAMA Cardiol. 2017, 2, 104–106. [Google Scholar] [CrossRef] [Green Version]
- Xie, J.; Wen, D.; Liang, L.; Jia, Y.; Gao, L.; Lei, J. Evaluating the validity of current mainstream wearable devices in fitness tracking under various physical activities: Comparative study. JMIR Mhealth Uhealth 2018, 6, e9754. [Google Scholar] [CrossRef] [Green Version]
- Ruiz-Malagon, E.J.; Ruiz-Alias, S.A.; García-Pinillos, F.; Delgado-Garcia, G.; Soto-Hermoso, V.M. Comparison between photoplethysmographic heart rate monitor from Polar Vantage M and Polar V800 with H10 chest strap while running on a treadmill: Validation of the Polar Precision PrimeTM photoplestimographic system. Proc. Inst. Mech. Eng. Part P J. Sports Eng. Technol. 2021, 235, 212–218. [Google Scholar] [CrossRef]
- Shumate, T.; Link, M.; Furness, J.; Kemp-Smith, K.; Simas, V.; Climstein, M. Validity of the polar vantage M watch when measuring heart rate at different exercise intensities. PeerJ 2021, 9, e10893. [Google Scholar] [CrossRef]
- Gilgen-Ammann, R.; Schweizer, T.; Wyss, T. RR interval signal quality of a heart rate monitor and an ECG Holter at rest and during exercise. Eur. J. Appl. Physiol. 2019, 119, 1525–1532. [Google Scholar] [CrossRef]
- Buchheit, M. Monitoring training status with HR measures: Do all roads lead to Rome? Front. Physiol. 2014, 5, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plews, D.J.; Laursen, P.B.; Stanley, J.; Kilding, A.E.; Buchheit, M. Training adaptation and heart rate variability in elite endurance athletes: Opening the door to effective monitoring. Sports Med. 2013, 43, 773–781. [Google Scholar] [CrossRef]
- Pesonen, A.K.; Kuula, L. The validity of a new consumer-targeted wrist device in sleep measurement: An overnight comparison against polysomnography in children and adolescents. J. Clin. Sleep Med. 2018, 14, 585–591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polar Electro Oy. Polar Presicion Prime OHR [White Paper]. 2019. Available online: https://www.polar.com/sites/default/files/static/science/white-papers/polar-precision-prime-white-paper.pdf (accessed on 17 December 2021).
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Hayano, J.; Barros, A.K.; Kamiya, A.; Ohte, N.; Yasuma, F. Assessment of pulse rate variability by the method of pulse frequency demodulation. Biomed. Eng. Online 2005, 4, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plews, D.J.; Laursen, P.B.; Le Meur, Y.; Hausswirth, C.; Kilding, A.E.; Buchheit, M. Monitoring training with heart-rate variability: How much compliance is needed for valid assessment? Int. J. Sports Physiol. Perform. 2014, 9, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Hynynen, E.; Vesterinen, V.; Rusko, H.; Nummela, A. Effects of moderate and heavy endurance exercise on nocturnal HRV. Int. J. Sports Med. 2010, 31, 428–432. [Google Scholar] [CrossRef]
- Nuuttila, O.P.; Nummela, A.; Häkkinen, K.; Seipäjärvi, S.; Kyröläinen, H. Monitoring training and recovery during a period of increased intensity or volume in recreational endurance athletes. Int. J. Environ. Res. Public Health 2021, 18, 2401. [Google Scholar] [CrossRef] [PubMed]
- Brandenberger, G.; Buchheit, M.; Ehrhart, J.; Simon, C.; Piquard, F. Is slow wave sleep an appropriate recording condition for heart rate variability analysis. Auton. Neurosci. 2005, 121, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Rincon Soler, A.I.; Silva, L.E.V.; Fazan, R., Jr.; Murta, L.O., Jr. The impact of artifact correction methods of RR series on heart rate variability parameters. J. Appl. Physiol. 2018, 124, 646–652. [Google Scholar] [CrossRef]
- Mejía-Mejía, E.; Budidha, K.; Abay, T.Y.; May, J.M.; Kyriacou, P.A. Heart rate variability (HRV) and pulse rate variability (PRV) for the assessment of autonomic responses. Front. Physiol. 2020, 11, 779. [Google Scholar] [CrossRef]
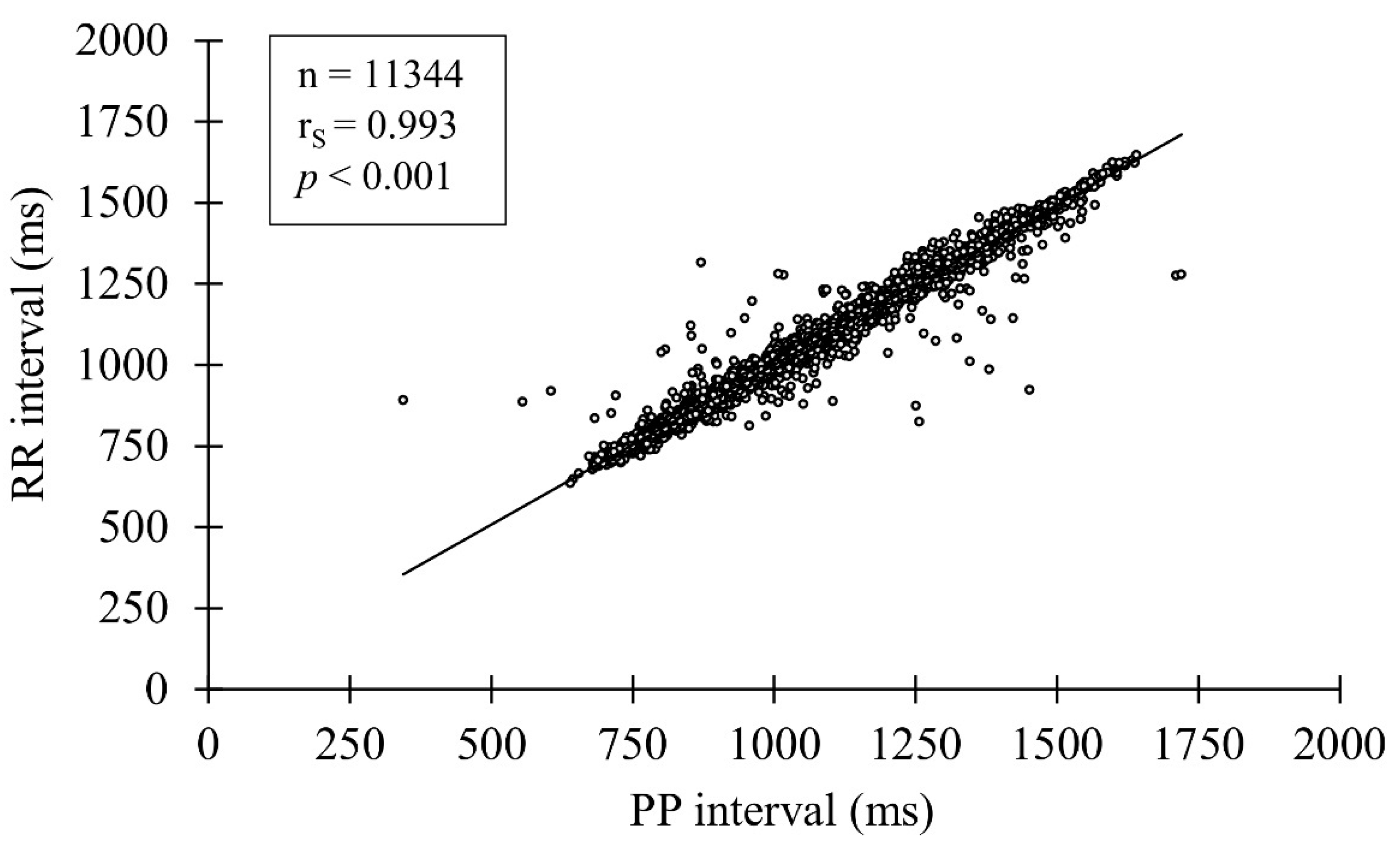


| Pooled 5-min Results (n = 11344) | |
|---|---|
| PPG, PP interval (ms) | 1022.9 ± 181.1 |
| HRS, RR interval (ms) | 1022.7 ± 179.8 |
| Bias (ms) | 0.2 ± 22.8 |
| MAE (ms) | 10.7 ± 20.2 |
| MAPE (%) | 1.1 ± 2.0 |
| PPG Mean | HRS Mean | Bias | MAE | MAPE | ICC | CCC | |
|---|---|---|---|---|---|---|---|
| 5-min segment (n = 39) | |||||||
| HR (bpm) | 58.6 ± 9.5 | 58.6 ± 9.5 | 0.0 ± 0.1 | 0.0 ± 0.1 | 0.04 ± 0.08 | 1.000 *** | 1.000 |
| LnRMSSD (ms) | 4.01 ± 0.48 | 3.82 ± 0.51 | 0.19 ± 0.21 *** | 0.20 ± 0.20 | 5.57 ± 6.14 | 0.913 *** | 0.849 |
| 4-h segment (n = 29) | |||||||
| HR (bpm) | 53.8 ± 9.2 | 54.5 ± 9.0 | −0.7 ± 0.6 *** | 0.8 ± 0.5 | 1.49 ± 1.01 | 0.998 *** | 0.995 |
| LnRMSSD (ms) | 4.06 ± 0.47 | 3.90 ± 0.61 | 0.17 ± 0.20 *** | 0.17 ± 0.20 | 5.23 ± 7.36 | 0.931 *** | 0.890 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nuuttila, O.-P.; Korhonen, E.; Laukkanen, J.; Kyröläinen, H. Validity of the Wrist-Worn Polar Vantage V2 to Measure Heart Rate and Heart Rate Variability at Rest. Sensors 2022, 22, 137. https://doi.org/10.3390/s22010137
Nuuttila O-P, Korhonen E, Laukkanen J, Kyröläinen H. Validity of the Wrist-Worn Polar Vantage V2 to Measure Heart Rate and Heart Rate Variability at Rest. Sensors. 2022; 22(1):137. https://doi.org/10.3390/s22010137
Chicago/Turabian StyleNuuttila, Olli-Pekka, Elisa Korhonen, Jari Laukkanen, and Heikki Kyröläinen. 2022. "Validity of the Wrist-Worn Polar Vantage V2 to Measure Heart Rate and Heart Rate Variability at Rest" Sensors 22, no. 1: 137. https://doi.org/10.3390/s22010137
APA StyleNuuttila, O.-P., Korhonen, E., Laukkanen, J., & Kyröläinen, H. (2022). Validity of the Wrist-Worn Polar Vantage V2 to Measure Heart Rate and Heart Rate Variability at Rest. Sensors, 22(1), 137. https://doi.org/10.3390/s22010137






