Artificial Intelligence-Based Wearable Robotic Exoskeletons for Upper Limb Rehabilitation: A Review
Abstract
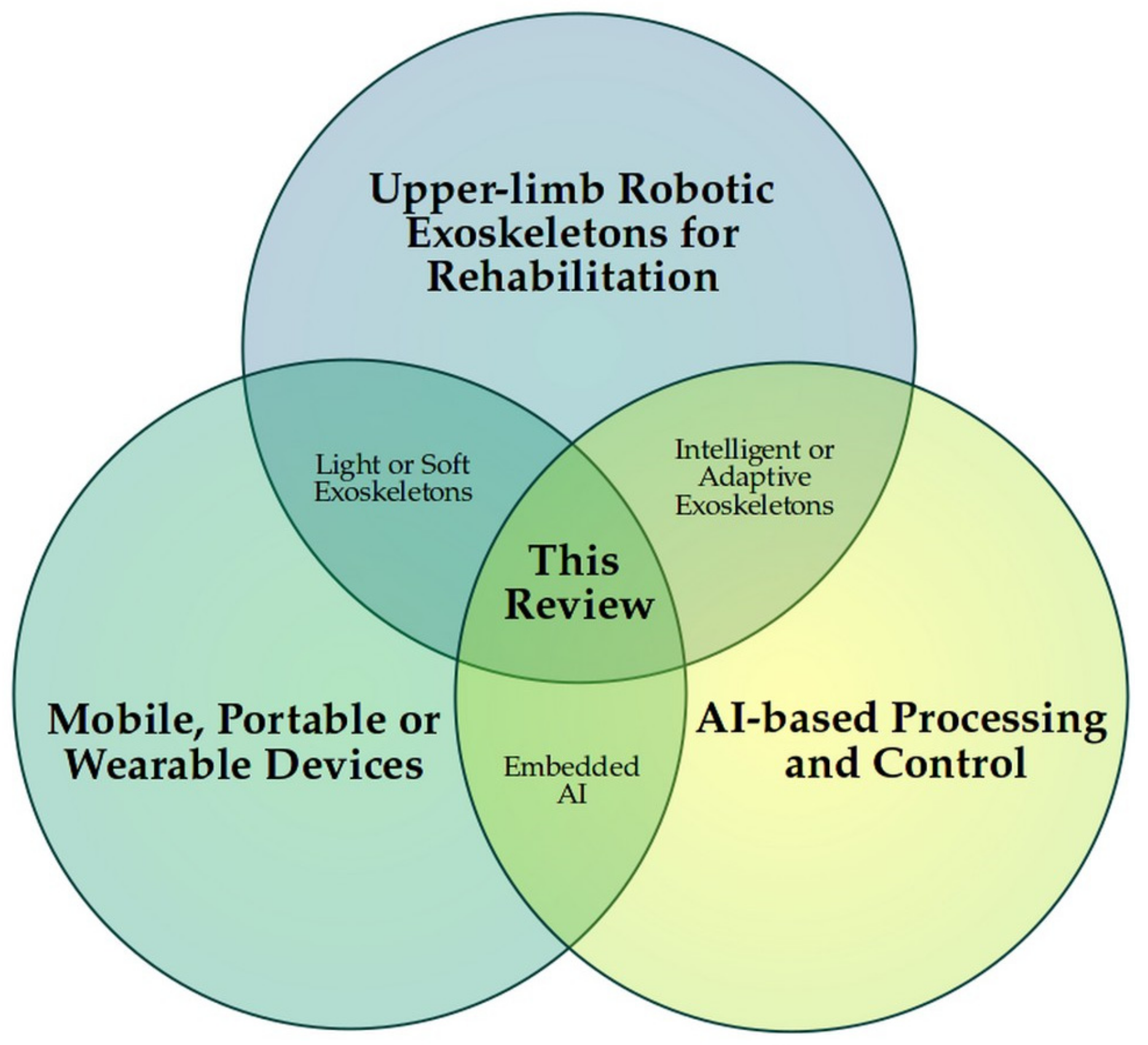
1. Introduction
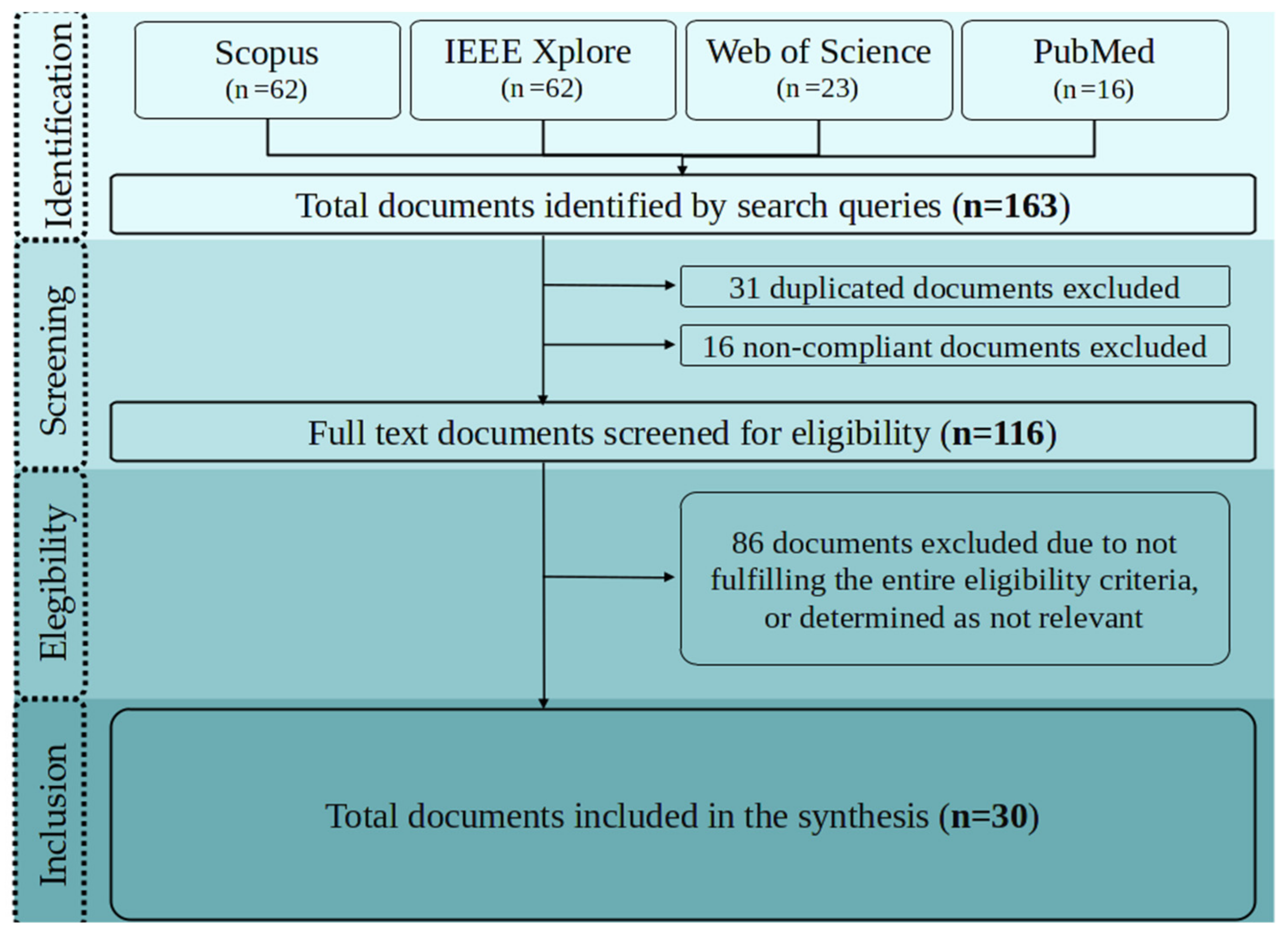
2. Methods
2.1. Eligibility Criteria
2.2. Search Methodology and Scope
2.3. Inclusion Criteria
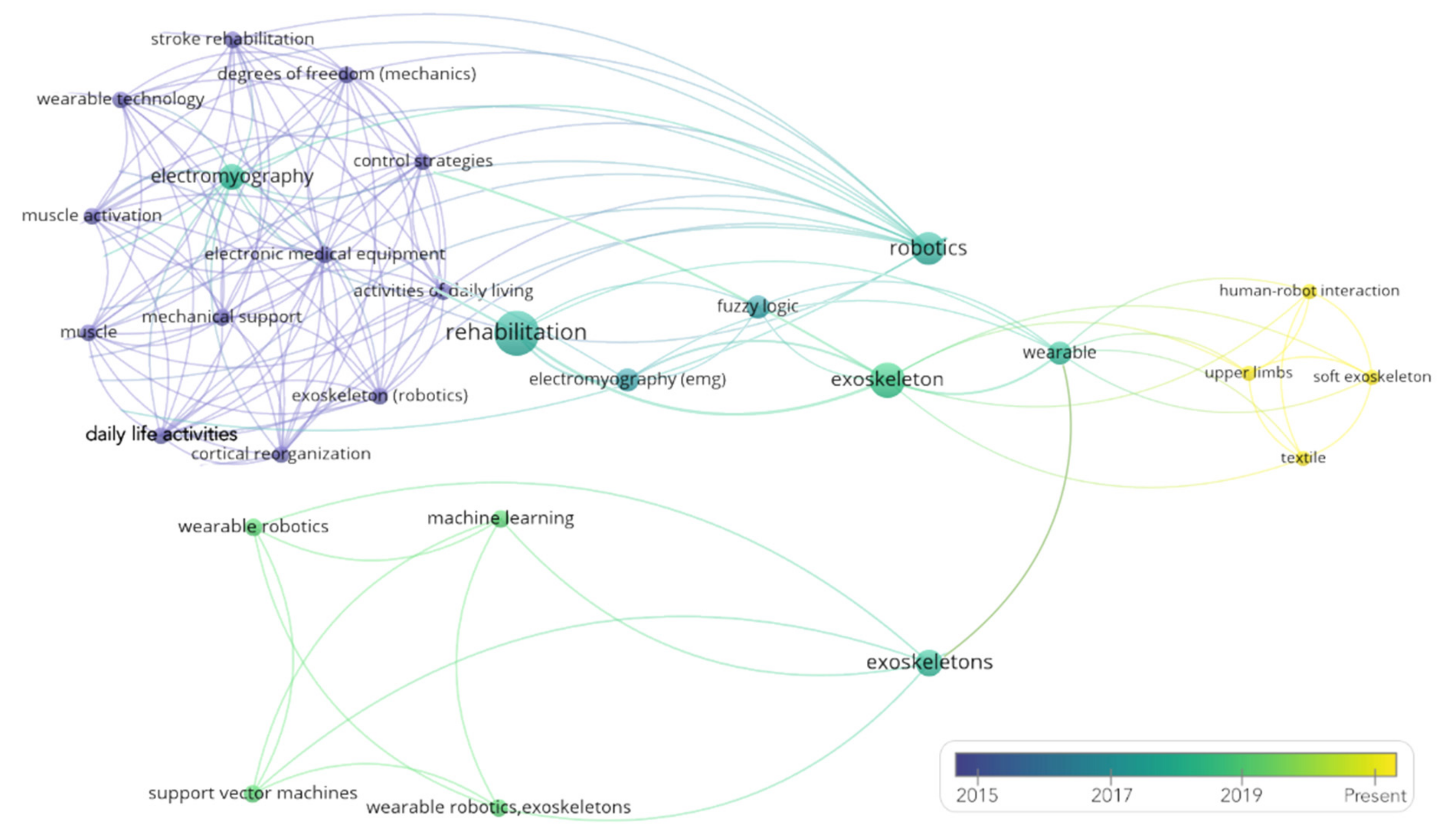
3. Results
3.1. Overview of Information Sources
3.2. Physical Characteristics and Operation Modes of the Robotic Exoskeletons
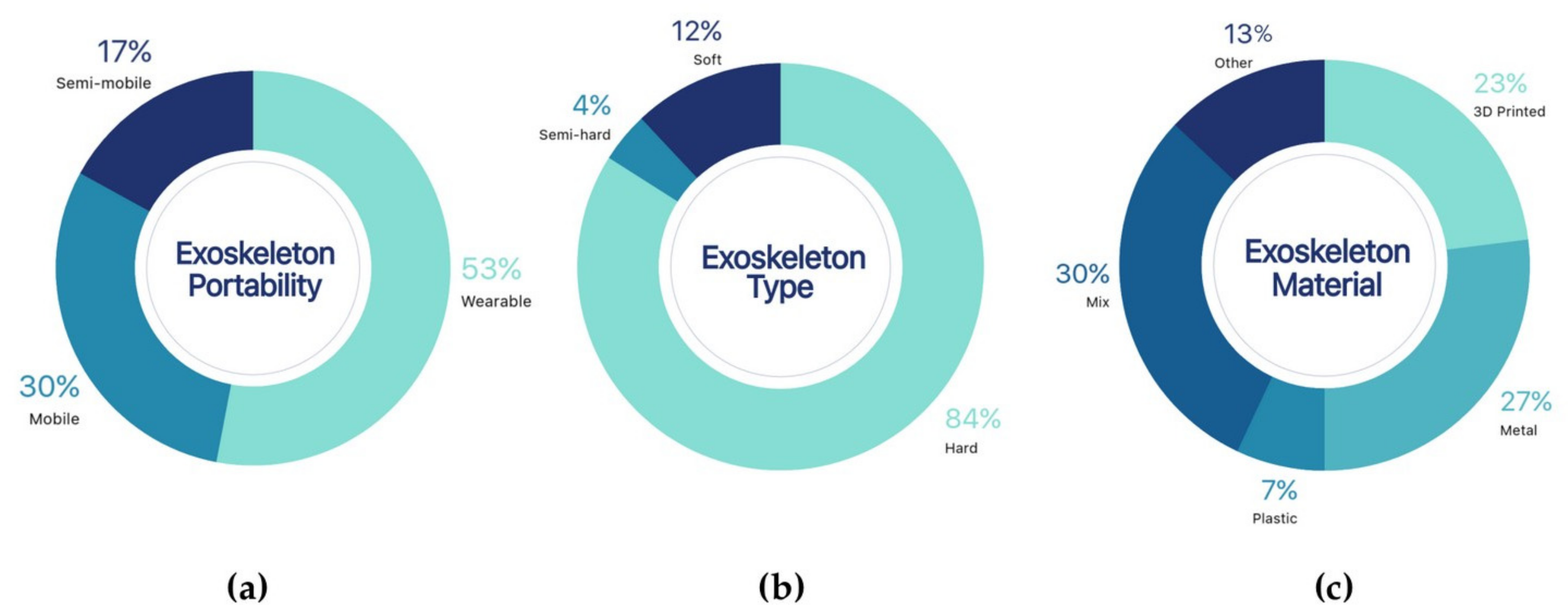
3.2.1. Physical Characteristics
Portability
Exoskeleton Type
Structural Materials
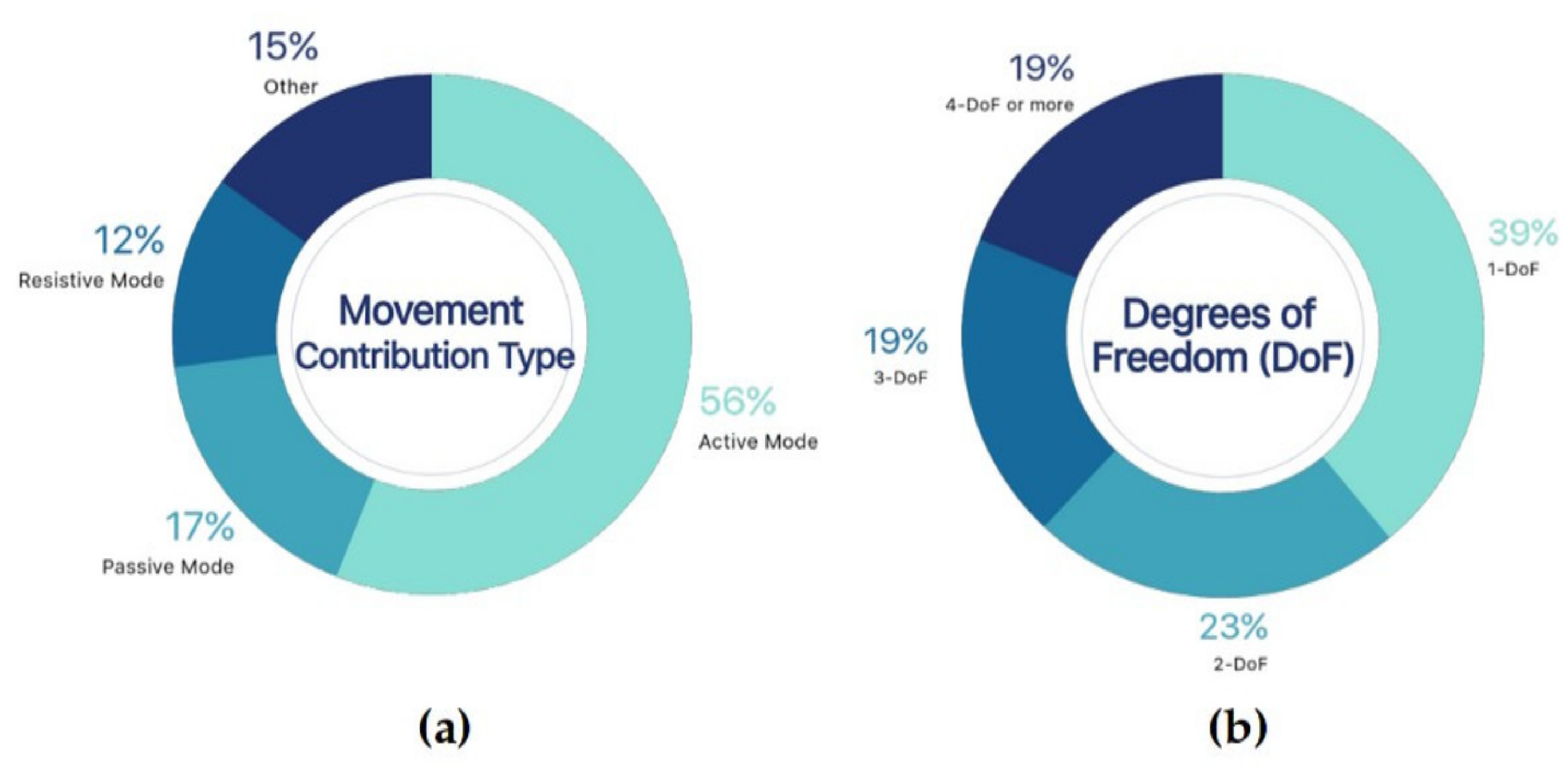
3.2.2. Operation Modes
Movement Contribution Type
- Multi-Mode
- Active Mode
- Passive Mode
Degrees of Freedom (DoFs)
- One DoF
- Two DoFs
- Three DoFs
- Four or more DoFs
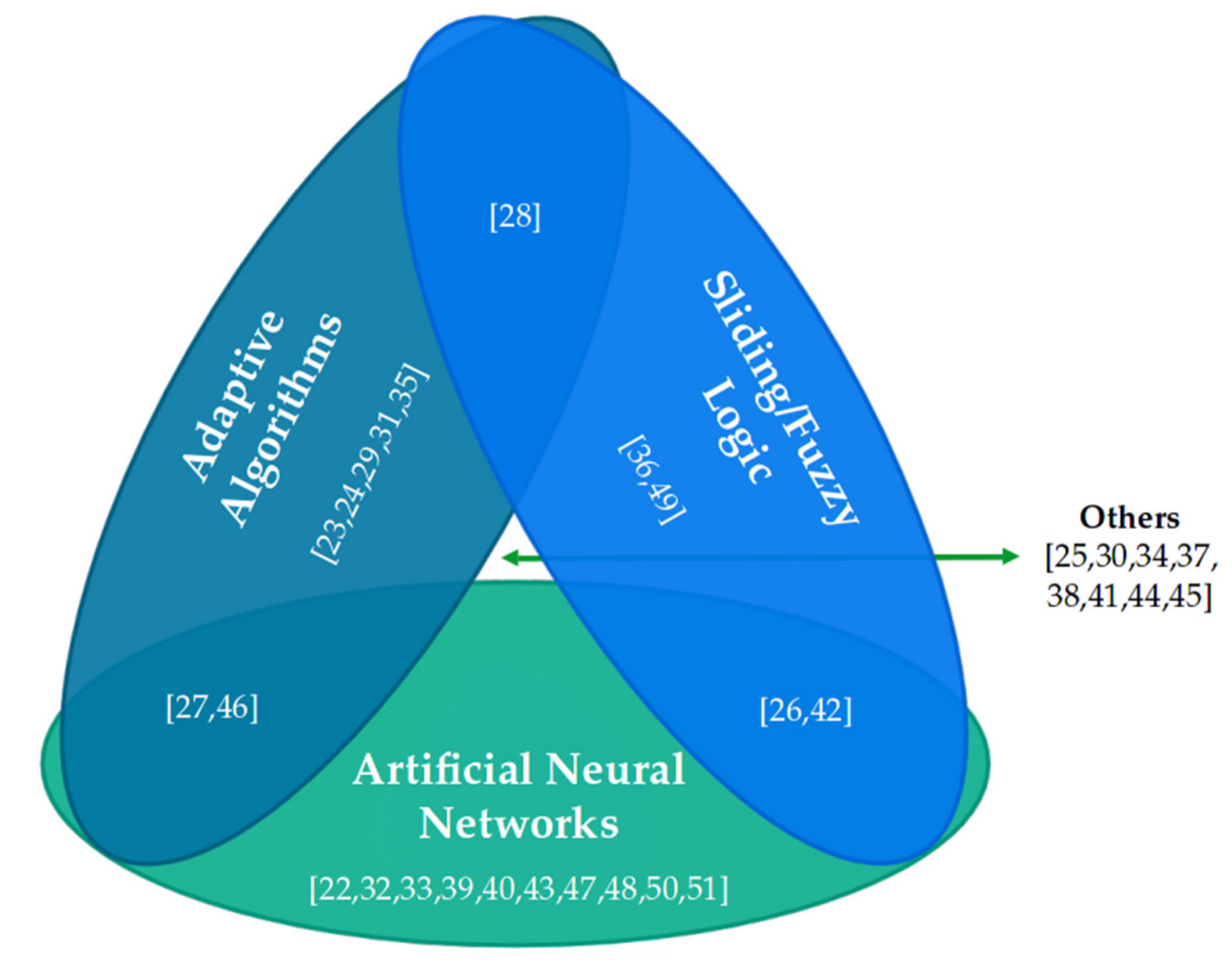
3.3. AI-Based Information Processing and Control Techniques
3.3.1. Artificial Neural Networks
3.3.2. Adaptive Algorithms
3.3.3. Sliding Modes and Fuzzy Logic
3.3.4. Mixed Techniques
Artificial Neural Networks and Adaptive Algorithms
Artificial Neural Networks and Fuzzy Logic
Fuzzy Logic and Adaptive Algorithms
3.3.5. Other AI-Based Techniques
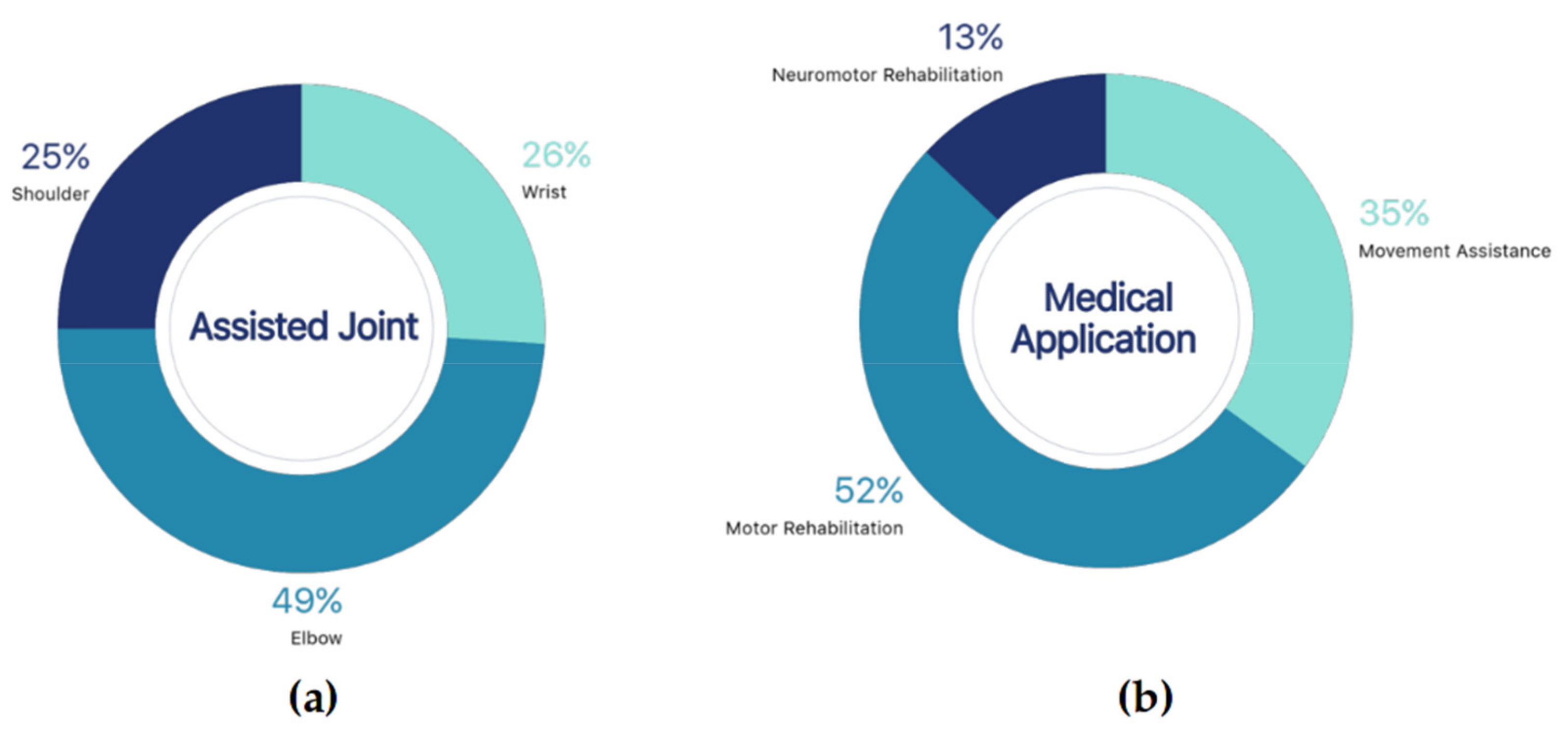
3.4. Type of Medical Application for the Upper Limb
3.4.1. Movement Assistance
3.4.2. Motor Rehabilitation
3.4.3. Neuromotor Rehabilitation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization; The World Bank. World Report on Disability; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Mathers, C.; Fat, D.M.; Boerma, J.T.; World Health Organization. The Global Burden of Disease: 2004 Update; World Health Organization: Geneva, Switzerland, 2008; ISBN 9789241563710. [Google Scholar]
- Mcfarlane, L.; Mclean, J. Education and training for direct care workers. Soc. Work Educ. 2003, 22, 385–399. [Google Scholar] [CrossRef]
- Young, J.; Forster, A. Review of stroke rehabilitation. BMJ 2007, 334, 86–90. [Google Scholar] [CrossRef]
- Adamson, J.; Beswick, A.; Ebrahim, S. Is stroke the most common cause of disability? J. Stroke Cerebrovasc. Dis. 2004, 13, 171–177. [Google Scholar] [CrossRef]
- Katan, M.; Luft, A. Global Burden of Stroke. Semin. Neurol. 2018, 38, 208–211. [Google Scholar] [CrossRef]
- Innocenti, T.; Ristori, D.; Miele, S.; Testa, M. The management of shoulder impingement and related disorders: A systematic review on diagnostic accuracy of physical tests and manual therapy efficacy. J. Bodyw. Mov. Ther. 2018, 23, 604–618. [Google Scholar] [CrossRef] [PubMed]
- Azma, K.; RezaSoltani, Z.; Rezaeimoghaddam, F.; Dadarkhah, A.; Mohsenolhosseini, S. Efficacy of tele-rehabilitation compared with office-based physical therapy in patients with knee osteoarthritis: A randomized clinical trial. J. Telemed. Telecare 2018, 24, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Longley, V.; Peters, S.; Swarbrick, C.; Bowen, A. What factors affect clinical decision-making about access to stroke rehabilitation? A systematic review. Clin. Rehabil. 2019, 33, 304–316. [Google Scholar] [CrossRef]
- Vukobratovic, M.K. When were acitve exoskeletons actually born? Int. J. Hum. Robot. 2007, 4, 459–486. [Google Scholar] [CrossRef]
- Dellon, B.; Matsuoka, Y. Prosthetics, exoskeletons, and rehabilitation [Grand Challenges of Robotics]. IEEE Robot. Autom. Mag. 2007, 14, 30–34. [Google Scholar] [CrossRef]
- Pons, J.L. Rehabilitation Exoskeletal Robotics. IEEE Eng. Med. Biol. Mag. 2010, 29, 57–63. [Google Scholar] [CrossRef]
- Gorgey, A.S. Robotic exoskeletons: The current pros and cons. World J. Orthop. 2018, 9, 112–119. [Google Scholar] [CrossRef]
- Wang, Q.; Markopoulos, P.; Yu, B.; Chen, W.; Timmermans, A. Interactive wearable systems for upper body rehabilitation: A systematic review. J. Neuroeng. Rehabil. 2017, 14, 1–21. [Google Scholar] [CrossRef]
- Bouteraa, Y.; Ben Abdallah, I. Exoskeleton robots for upper-limb rehabilitation. In Proceedings of the 13th International Multi-Conference on Systems, Signals and Devices, SSD 2016, Leipzig, Germany, 21–24 March 2016. [Google Scholar]
- Balasubramanian, S.; Wei, R.; Perez, M.; Shepard, B.; Koeneman, E.; Koeneman, J.; He, J. RUPERT: An exoskeleton robot for assisting rehabilitation of arm functions. Virtual Rehabil. 2008, 1, 163–167. [Google Scholar] [CrossRef]
- Mekki, M.; Delgado, A.D.; Fry, A.; Putrino, D.; Huang, V. Robotic Rehabilitation and Spinal Cord Injury: A Narrative Review. Neurotherapeutics 2018, 15, 604–617. [Google Scholar] [CrossRef] [PubMed]
- Gilhooly, R. Exoskeletons Await in Work/Care Closet. Available online: http://www.japantimes.co.jp/life/2012/06/17/general/exoskeletons-await-in-workcare-closet (accessed on 30 November 2020).
- Manna, S.K.; Dubey, V.N. Comparative study of actuation systems for portable upper limb exoskeletons. Med. Eng. Phys. 2018, 60, 1–13. [Google Scholar] [CrossRef]
- Smith, J.E. Self-adaptative and coevolving memetic algorithms. Stud. Comput. Intell. 2012, 379, 167–188. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6. [Google Scholar] [CrossRef] [PubMed]
- Sangha, S.; Elnady, A.M.; Menon, C. A compact robotic orthosis for wrist assistance. In Proceedings of the 2016 6th IEEE International Conference on Biomedical Robotics and Biomechatronics (BioRob), Singapore, 26–29 June 2016; pp. 1080–1085. [Google Scholar] [CrossRef]
- Chonnaparamutt, W.; Supsi, W. SEFRE: Semiexoskeleton Rehabilitation System. Appl. Bionics Biomech. 2016, 2016. [Google Scholar] [CrossRef]
- Sui, D.; Fan, J.; Jin, H.; Cai, X.; Zhao, J.; Zhu, Y. Design of a wearable upper-limb exoskeleton for activities assistance of daily living. In Proceedings of the 2017 IEEE International Conference on Advanced Intelligent Mechatronics (AIM), Munich, Germany, 3–7 July 2017; pp. 845–850. [Google Scholar] [CrossRef]
- Abdul Majeed, A.P.P.; Taha, Z.; Mohd Khairuddin, I.; Wong, M.Y.; Abdullah, M.A.; Mohd Razman, M.A. The control of an upper-limb exoskeleton by means of a particle swarm optimized active force control for motor recovery. IFMBE Proc. 2017, 58, 56–62. [Google Scholar] [CrossRef]
- Tageldeen, M.K.; Perumal, N.; Elamvazuthi, I.; Ganesan, T. Design and control of an upper arm exoskeleton using Fuzzy logic techniques. In Proceedings of the 2016 2nd IEEE International Symposium on Robotics and Manufacturing Automation (ROMA), Ipoh, Malaysia, 25–27 September 2016. [Google Scholar] [CrossRef]
- Seeland, A.; Tabie, M.; Kim, S.K.; Kirchner, F.; Kirchner, E.A. Adaptive multimodal biosignal control for exoskeleton supported stroke rehabilitation. In Proceedings of the 2017 IEEE International Conference on Systems, Man, and Cybernetics (SMC), Banff, AB, Canada, 5–8 October 2017; pp. 2431–2436. [Google Scholar] [CrossRef]
- Shamroukh, M.; Chacko, A.; Kalaichelvi, V.; Kalimullah, I.Q.; Barlingay, S.S.; Chattopadhyay, A.B. Evaluation of control strategies in semi-active orthosis for suppression of upper limb pathological tremors. In Proceedings of the 2017 International Conference on Innovations in Electrical, Electronics, Instrumentation and Media Technology (ICEEIMT), Coimbatore, India, 3–4 February 2017; pp. 75–80. [Google Scholar] [CrossRef]
- Lambelet, C.; Lyu, M.; Woolley, D.; Gassert, R.; Wenderoth, N. The eWrist—A wearable wrist exoskeleton with sEMG-based force control for stroke rehabilitation. In Proceedings of the 2017 International Conference on Rehabilitation Robotics, ICORR 2017, London, UK, 17–20 July 2017; pp. 726–733. [Google Scholar]
- Rehmat, N.; Zuo, J.; Meng, W.; Liu, Q.; Xie, S.Q.; Liang, H. Upper limb rehabilitation using robotic exoskeleton systems: A systematic review. Int. J. Intell. Robot. Appl. 2018, 2, 283–295. [Google Scholar] [CrossRef]
- Rosales Luengas, Y.; López-Gutiérrez, R.; Salazar, S.; Lozano, R. Robust controls for upper limb exoskeleton, real-time results. Proc. Inst. Mech. Eng. Part I J. Syst. Control Eng. 2018, 232, 797–806. [Google Scholar] [CrossRef]
- Siu, H.C.; Arenas, A.M.; Sun, T.; Stirling, L.A. Implementation of a surface electromyography-based upper extremity exoskeleton controller using learning from demonstration. Sensors 2018, 18, 467. [Google Scholar] [CrossRef] [PubMed]
- Di Febbo, D.; Ambrosini, E.; Pirotta, M.; Rojas, E.; Restelli, M.; Pedrocchi, A.L.G.; Ferrante, S. Does Reinforcement Learning outperform PID in the control of FES-induced elbow flex-extension? In Proceedings of the 2018 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Rome, Italy, 11–13 June 2018; Volume 3528725544, pp. 1–6. [Google Scholar] [CrossRef]
- Zhang, S.; Fu, Q.; Guo, S.; Fu, Y. Coordinative Motion-based Bilateral Rehabilitation Training System with Exoskeleton and Haptic Devices for Biomedical Application. Micromachines 2018, 10, 8. [Google Scholar] [CrossRef]
- Miao, Q.; Zhang, M.; Cao, J.; Xie, S.Q. Reviewing high-level control techniques on robot-assisted upper-limb rehabilitation. Adv. Robot. 2018, 32, 1253–1268. [Google Scholar] [CrossRef]
- Zhao, Z.; Li, X.; Hao, L. Research on the Control Method of a Rehabilitation Exoskeleton Robot for Passive Training on Upper-Limbs of Stroke Patients. In Proceedings of the 2018 IEEE 8th Annual International Conference on CYBER Technology in Automation, Control, and Intelligent Systems (CYBER), Tianjin, China, 19–23 July 2018; pp. 1106–1111. [Google Scholar] [CrossRef]
- Liu, Y.; Guo, S. Design of a Novel Wearable Power-assist Exoskeleton Device. In Proceedings of the 2018 13th World Congress on Intelligent Control and Automation (WCICA), Changsha, China, 4–8 July 2018; pp. 131–134. [Google Scholar] [CrossRef]
- Chen, L.; Zhang, C.; Liu, Z.; Zhang, T. Evaluation of Muscle Fatigue Based on CRP and RQA for Upper Limb Exoskeleton. In Proceedings of the 2018 Chinese Automation Congress (CAC), Xi’an, China, 30 November–2 December 2018; pp. 4210–4215. [Google Scholar] [CrossRef]
- Wang, W.; Qin, L.; Yuan, X.; Ming, X.; Sun, T.; Liu, Y. Bionic control of exoskeleton robot based on motion intention for rehabilitation training. Adv. Robot. 2019, 33, 590–601. [Google Scholar] [CrossRef]
- Guo, S.; Gao, W.; Bu, D. Radial Basis Function Neural Network-based Control Method for a Upper Limb Rehabilitation Robot. In Proceedings of the 2019 IEEE International Conference on Mechatronics and Automation (ICMA), Beijing, China, 2–5 August 2020; pp. 1327–1332. [Google Scholar] [CrossRef]
- Asokan, A.; Vigneshwar, M. Design and Control of an EMG-based Low-cost Exoskeleton for Stroke Rehabilitation. In Proceedings of the 2019 Fifth Indian Control Conference (ICC) 2019, Delhi, India, 9–11 January 2019; pp. 478–483. [Google Scholar] [CrossRef]
- Al Bakri, A.; Lezzar, M.Y.; Alzinati, M.; Mortazavi, K.; Shehieb, W.; Sharif, T. Intelligent Exoskeleton for Patients with Paralysis. In Proceedings of the 2018 IEEE 9th Annual Information Technology, Electronics and Mobile Communication Conference (IEMCON), Vancouver, BC, Canada, 1–3 November 2018; pp. 189–193. [Google Scholar] [CrossRef]
- Lei, Z. An upper limb movement estimation from electromyography by using BP neural network. Biomed. Signal Process. Control 2019, 49, 434–439. [Google Scholar] [CrossRef]
- Zaroug, A.; Proud, J.K.; Lai, D.T.H.; Mudie, K.; Billing, D.; Begg, R. Overview of Computational Intelligence (CI) Techniques for Powered Exoskeletons. In Computational Intelligence in Sensor Networks; Springer: Berlin/Heidelberg, Germany, 2019; Volume 776, pp. 353–383. ISBN 978-3-662-57275-7. [Google Scholar]
- Taha, Z.; Abdul Majeed, A.P.P.; Abdullah, M.A.; Azmi, K.Z.M.; Bin Zakaria, M.A.; Ghani, A.S.A.; Hassan, M.H.A.; Razman, M.A.M. The control of an upper extremity exoskeleton for stroke rehabilitation by means of a hybrid active force control. In Proceedings of the Advances in Intelligent Systems and Computing, Lviv, Ukraine, 17–20 September 2019; Springer: Berlin, Germany, 2019; Volume 751, pp. 361–370. [Google Scholar]
- Vélez-Guerrero, M.A.; Callejas-Cuervo, M. Data Acquisition and Control Architecture for Intelligent Robotic Exoskeletons in Rehabilitation. In Proceedings of the 7th IEEE International Conference on E-Health and Bioengineering—EHB 2019, Iasi, Romania, 21–23 November 2019; pp. 1–4. [Google Scholar]
- Wang, W.; Li, H.; Xiao, M.; Chu, Y.; Yuan, X.; Ming, X.; Zhang, B. Design and verification of a human–robot interaction system for upper limb exoskeleton rehabilitation. Med. Eng. Phys. 2020, 79, 19–25. [Google Scholar] [CrossRef]
- Li, X.; Liu, S.; Chang, Y.; Li, S.; Fan, Y.; Yu, H. A Human Joint Torque Estimation Method for Elbow Exoskeleton Control. Int. J. Humanoid Robot. 2020, 17. [Google Scholar] [CrossRef]
- Chen, C.T.; Lien, W.Y.; Chen, C.T.; Twu, M.J.; Wu, Y.C. Dynamic Modeling and Motion Control of a Cable-Driven Robotic Exoskeleton with Pneumatic Artificial Muscle Actuators. IEEE Access 2020, 8, 149796–149807. [Google Scholar] [CrossRef]
- Samper-Escudero, J.L.; Gimenez-Fernandez, A.; Sanchez-Uran, M.A.; Ferre, M. A Cable-Driven Exosuit for Upper Limb Flexion Based on Fibres Compliance. IEEE Access 2020, 8, 153297–153310. [Google Scholar] [CrossRef]
- Varghese, R.J.; Lo, B.P.L.; Yang, G.Z. Design and Prototyping of a Bio-Inspired Kinematic Sensing Suit for the Shoulder Joint: Precursor to a Multi-DoF Shoulder Exosuit. IEEE Robot. Autom. Lett. 2020, 5, 540–547. [Google Scholar] [CrossRef]
- Kumar, S.; Simnofske, M.; Bongardt, B.; Müller, A.; Kirchner, F. Integrating mimic joints into dynamics algorithms: Exemplified by the hybrid recupera exoskeleton. In Proceedings of the Advances in Robotics, New Delhi, India, 28 June–2 July 2017; pp. 1–6. [Google Scholar] [CrossRef]
- Kumar, S.; Wöhrle, H.; Trampler, M.; Simnofske, M.; Peters, H.; Mallwitz, M.; Kirchner, E.; Kirchner, F. Modular Design and Decentralized Control of the Recupera Exoskeleton for Stroke Rehabilitation. Appl. Sci. 2019, 9, 626. [Google Scholar] [CrossRef]
- Christensen, S.; Bai, S.; Rafique, S.; Isaksson, M.; O’Sullivan, L.; Power, V.; Virk, G.S. AXO-SUIT—A Modular Full-Body Exoskeleton for Physical Assistance; Springer: Berlin, Germany, 2019; Volume 66, ISBN 9783030003654. [Google Scholar]
- Kim, B.; Deshpande, A.D. An upper-body rehabilitation exoskeleton Harmony with an anatomical shoulder mechanism: Design, modeling, control, and performance evaluation. Int. J. Rob. Res. 2017, 36, 414–435. [Google Scholar] [CrossRef]
- Van Eck, N.J.; Waltman, L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef]
- Reanaree, P.; Pintavirooj, C. Exoskeleton Suit Supports the Movement. In Proceedings of the 2018 11th Biomedical Engineering International Conference (BMEiCON), Chiang Mai, Thailand, 21–24 November 2018; pp. 1–4. [Google Scholar] [CrossRef]
- Dollar, A.M.; Herr, H. Lower Extremity Exoskeletons and Active Orthoses: Challenges and State-of-the-Art. IEEE Trans. Robot. 2008, 24, 144–158. [Google Scholar] [CrossRef]
- Abdul Majeed, A.P.P.; Taha, Z.; Abdullah, M.A.; Azmi, K.Z.M.; Bin Zakaria, M.A. The control of an upper extremity exoskeleton for stroke rehabilitation: An active force control scheme approach. Adv. Robot. Res. 2018, 2, 237–245. [Google Scholar] [CrossRef]
- Nag, P.K.; Mission, R.; Sinha, A.G.K.; Goswami, A. Introduction and Classification of Therapeutic Exercise; Shivaji College, University of Delhi: New Delhi, India, 2014. [Google Scholar]
- Gull, M.A.; Bai, S.; Bak, T. A review on design of upper limb exoskeletons. Robotics 2020, 9, 16. [Google Scholar] [CrossRef]
- De Vries, A.; De Looze, M. The Effect of Arm Support Exoskeletons in Realistic Work Activities: A Review Study. J. Ergon. 2019, 9, 1–9. [Google Scholar] [CrossRef]
- Lee, S.H.; Park, G.; Cho, D.Y.; Kim, H.Y.; Lee, J.Y.; Kim, S.; Park, S.B.; Shin, J.H. Comparisons between end-effector and exoskeleton rehabilitation robots regarding upper extremity function among chronic stroke patients with moderate-to-severe upper limb impairment. Sci. Rep. 2020, 10, 1–8. [Google Scholar] [CrossRef]
- Pang, Z.; Wang, T.; Wang, Z.; Yu, J.; Sun, Z.; Liu, S. Design and analysis of a wearable upper limb rehabilitation robot with characteristics of tension mechanism. Appl. Sci. 2020, 10, 2101. [Google Scholar] [CrossRef]
- Mallwitz, M.; Will, N.; Teiwes, J.; Kirchner, E.A. The CAPIO Active Upper Body Exoskeleton and Its Application for Teleoperation. In Proceedings of the 13th Symposium on Advanced Space Technologies in Robotics and Automation. ESA/Estec Symposium on Advanced Space Technologies in Robotics and Automation (ASTRA-2015), Noordwijk, The Netherlands, 11–13 May 2015; pp. 1–8. [Google Scholar]
- McPhee, J. Integration of Machine Learning with Dynamics and Control: From Autonomous Cars to Biomechatronics. CSME Bull. 2019, 151–152. [Google Scholar]
- Novak, D.; Riener, R. Control strategies and artificial intelligence in rehabilitation robotics. AI Mag. 2015, 36, 23–33. [Google Scholar] [CrossRef]
- Losey, D.P.; McDonald, C.G.; Battaglia, E.; O’Malley, M.K. A Review of Intent Detection, Arbitration, and Communication Aspects of Shared Control for Physical Human–Robot Interaction. Appl. Mech. Rev. 2018, 70, 010804. [Google Scholar] [CrossRef]
- Bonato, P. Advances in wearable technology and applications in physical medicine and rehabilitation. J. Neuroeng. Rehabil. 2005, 2, 2–5. [Google Scholar] [CrossRef] [PubMed]
- Nayak, S.; Kumar Das, R. Application of Artificial Intelligence (AI) in Prosthetic and Orthotic Rehabilitation. In Service Robotics; IntechOpen: London, UK, 2016; pp. 1–23. [Google Scholar] [CrossRef]
- Samper-Escudero, J.L.; Contreras-González, A.F.; Ferre, M.; Sánchez-Urán, M.A.; Pont-Esteban, D. Efficient Multiaxial Shoulder-Motion Tracking Based on Flexible Resistive Sensors Applied to Exosuits. Soft Robot. 2020, 7, 370–385. [Google Scholar] [CrossRef] [PubMed]
- Belda, K.; Böhm, J. Adaptive Predictive Control for Simple Mechatronic Systems. In Proceedings of the 10th WSEAS International Conference on Systems, Athens, Greece, 10–12 July 2006; World Scientific and Engineering Academy and Society (WSEAS): Stevens Point, WI, USA, 2006; pp. 309–314. [Google Scholar]
- Szuster, M.; Hendzel, Z. Intelligent Optimal Adaptive Control for Mechatronic Systems; Springer: Berlin, Germany, 2018. [Google Scholar]
- Marchal-Crespo, L.; Reinkensmeyer, D.J. Review of control strategies for robotic movement training after neurologic injury. J. Neuroeng. Rehabil. 2009, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Mounis, S.Y.A.; Azlan, N.Z.; Sado, F. Assist-as-needed control strategy for upper-limb rehabilitation based on subject’s functional ability. Meas. Control (UK) 2019, 52, 1354–1361. [Google Scholar] [CrossRef]
- Benveniste, A.; Wilson, S.S.; Metivier, M.; Priouret, P. Adaptive Algorithms and Stochastic Approximations; Stochastic Modelling and Applied Probability; Springer: Berlin/Heidelberg, Germany, 2012; ISBN 9783642758942. [Google Scholar]
- Gambhire, S.J.; Kishore, D.R.; Londhe, P.S.; Pawar, S.N. Review of sliding mode based control techniques for control system applications. Int. J. Dyn. Control 2020. [Google Scholar] [CrossRef]
- Babaiasl, M.; Goldar, S.N.; Barhaghtalab, M.H.; Meigoli, V. Sliding mode control of an exoskeleton robot for use in upper-limb rehabilitation. In Proceedings of the 2015 3rd RSI International Conference on Robotics and Mechatronics (ICROM), Tehran, Iran, 7–9 October 2015; pp. 694–701. [Google Scholar] [CrossRef]
- Anam, K.; Al-Jumaily, A.A. Active exoskeleton control systems: State of the art. Procedia Eng. 2012, 41, 988–994. [Google Scholar] [CrossRef]
- Esmaeili, B.; Beyramzad, J.; Seyyedrasuli, M.; Noorani, M.R.S.; Ghanbari, A. Using fuzzy neural network sliding mode control for human-exoskeleton interaction forces minimization. In Proceedings of the 2018 IEEE International Conference on Mechatronics and Automation (ICMA), Changchun, China, 5–8 August 2018; pp. 403–410. [Google Scholar] [CrossRef]
- Rahmani, M.; Rahman, M.H. An upper-limb exoskeleton robot control using a novel fast fuzzy sliding mode control. J. Intell. Fuzzy Syst. 2019, 36, 2581–2592. [Google Scholar] [CrossRef]
- Widrow, B.; Lehr, M.A. Adaptive neural networks and their applications. Int. J. Intell. Syst. 1993, 8, 453–507. [Google Scholar] [CrossRef]
- Magoulas, G.D.; Vrahatis, M.N. Adaptive algorithms for neural network supervised learning: A deterministic optimization approach. Int. J. Bifurc. Chaos 2006, 16, 1929–1950. [Google Scholar] [CrossRef]
- Kar, S.; Das, S.; Ghosh, P.K. Applications of neuro fuzzy systems: A brief review and future outline. Appl. Soft Comput. J. 2014, 15, 243–259. [Google Scholar] [CrossRef]
- Xu, L.; Vu, Y.; Wu, Q. General Fuzzy Neural Network: Basic structure, algorithms and its applications. IFAC Proc. Vol. 1999, 32, 5255–5260. [Google Scholar] [CrossRef]
- Kiguchi, K.; Tanaka, T.; Fukuda, T. Neuro-fuzzy control of a robotic exoskeleton with EMG signals. IEEE Trans. Fuzzy Syst. 2004, 12, 481–490. [Google Scholar] [CrossRef]
- Stingu, P.E.; Lewis, F.L. Neuro-fuzzy Control of Autonomous Robotics. In Encyclopedia of Complexity and Systems Science; Meyers, R.A., Ed.; Springer: New York, NY, USA, 2009; pp. 6066–6086. ISBN 978-0-387-30440-3. [Google Scholar]
- Jiang, Y.; Yang, C.; Ma, H. A Review of Fuzzy Logic and Neural Network Based Intelligent Control Design for Discrete-Time Systems. Discret. Dyn. Nat. Soc. 2016, 2016. [Google Scholar] [CrossRef]
- Yang, S.; Han, J.; Xia, L.; Chen, Y.H. An optimal fuzzy-theoretic setting of adaptive robust control design for a lower limb exoskeleton robot system. Mech. Syst. Signal Process. 2020, 141, 106706. [Google Scholar] [CrossRef]
- Ou, Y.; Li, Z.; Li, G.; Su, C.Y. Adaptive fuzzy tracking control of a human lower limb with an exoskeleton. In Proceedings of the 2012 IEEE International Conference on Robotics and Biomimetics (ROBIO), Guangzhou, China, 11–14 December 2012; pp. 1937–1942. [Google Scholar] [CrossRef]
- Rahmani, M.; Rahman, M.H.; Ghommam, J. A 7-DoF Upper Limb Exoskeleton Robot Control Using a New Robust Hybrid Controller. Int. J. Control. Autom. Syst. 2019, 17, 1–9. [Google Scholar] [CrossRef]
- Bembli, S.; Haddad, N.K.; Belghith, S. Robustness Analysis of an Upper Limb Exoskeleton Controlled by Sliding Mode Algorithm. Mech. Mach. Sci. 2019, 58, 99–112. [Google Scholar] [CrossRef]
- Anirudh Sharma, C.; Sai, A.S.K.; Kumar, V.; Prasad, A.; Begum, R.; Sharvani, G.S.; Manjunath, A.E. Multifaceted Bio-medical applications of Exoskeleton: A review. In Proceedings of the 2018 2nd International Conference on Inventive Systems and Control (ICISC), Coimbatore, India, 19–20 January 2018; pp. 11–15. [Google Scholar]
- Kiguchi, K. Active exoskeletons for upper-limb motion assist. Int. J. Hum. Robot. 2007, 4, 607–624. [Google Scholar] [CrossRef]
- Ruiz, A.F.; Forner-Cordero, A.; Rocon, E.; Pons, J.L. Exoskeletons for rehabilitation and motor control. In Proceedings of the First IEEE/RAS-EMBS International Conference on Biomedical Robotics and Biomechatronics, Pisa, Italy, 20–22 February 2006; pp. 601–606. [Google Scholar] [CrossRef]
- Proietti, T.; Crocher, V.; Roby-Brami, A.; Jarrasse, N. Upper-limb robotic exoskeletons for neurorehabilitation: A review on control strategies. IEEE Rev. Biomed. Eng. 2016, 9, 4–14. [Google Scholar] [CrossRef]
- Onose, G.; Popescu, N.; Munteanu, C.; Ciobanu, V.; Sporea, C.; Mirea, M.D.; Daia, C.; Andone, I.; Spînu, A.; Mirea, A. Mobile mechatronic/robotic orthotic devices to assist-rehabilitate neuromotor impairments in the upper limb: A systematic and synthetic review. Front. Neurosci. 2018, 12, 577. [Google Scholar] [CrossRef] [PubMed]
- Iandolo, R.; Marini, F.; Semprini, M.; Laffranchi, M.; Mugnosso, M.; Cherif, A.; De Michieli, L.; Chiappalone, M.; Zenzeri, J. Perspectives and challenges in robotic neurorehabilitation. Appl. Sci. 2019, 9, 3183. [Google Scholar] [CrossRef]
- Morgenstern, J.D.; Rosella, L.C.; Daley, M.J.; Goel, V.; Schünemann, H.J.; Piggott, T. “AI’s gonna have an impact on everything in society, so it has to have an impact on public health”: A fundamental qualitative descriptive study of the implications of artificial intelligence for public health. BMC Public Health 2021, 21, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Keravnou-Papailiou, E.; Antoniou, G. Medical analytics for healthcare intelligence—Recent advances and future directions. Artif. Intell. Med. 2021, 112, 102009. [Google Scholar] [CrossRef] [PubMed]
- Sherratt, F.; Plummer, A. Understanding LSTM Network Behaviour of IMU-Based. Sensors 2021, 21, 1264. [Google Scholar] [CrossRef] [PubMed]
- Monardo, G.; Pavese, C.; Giorgi, I.; Godi, M.; Colombo, R. Evaluation of Patient Motivation and Satisfaction during Technology-Assisted Rehabilitation: An Experiential Review. Games Health J. 2021, 10, 13–27. [Google Scholar] [CrossRef]
- Alarcón-Aldana, A.C.; Callejas-Cuervo, M.; Bo, A.P.L. Upper limb physical rehabilitation using serious videogames and motion capture systems: A systematic review. Sensors 2020, 20, 5989. [Google Scholar] [CrossRef]
- De la Tejera, J.A.; Bustamante-Bello, R.; Ramirez-Mendoza, R.A.; Izquierdo-Reyes, J. Systematic review of exoskeletons towards a general categorization model proposal. Appl. Sci. 2021, 11, 76. [Google Scholar] [CrossRef]

| Database | Search Query |
|---|---|
| Scopus | TITLE-ABS-KEY ((“powered exoskeleton” OR “robotic exoskeleton” OR “active exoskeleton” OR exosuit OR “powered ortho*” OR “robotic ortho*” OR “active ortho*”) AND ((up* OR “upper limb” OR arm OR forearm OR shoulder OR elbow) AND NOT (low* OR hip OR gait OR vision OR theoretical OR walk*)) AND (rehabilitation OR “physical therapy” OR impair* OR health)) AND (intellig* OR adaptiv* OR netw* OR “artificial neur*” OR ANN OR learn*) AND (wearable OR mobile OR portable) AND (LIMIT-TO (SUBJAREA, “ENGI”) OR LIMIT-TO (SUBJAREA, “COMP”) OR LIMIT-TO (SUBJAREA, “MEDI”)) AND (LIMIT-TO (PUBYEAR, 2020) OR LIMIT-TO (PUBYEAR, 2019) OR LIMIT-TO (PUBYEAR, 2018) OR LIMIT-TO (PUBYEAR, 2017) OR LIMIT-TO (PUBYEAR, 2016)) |
| IEEE Xplore | ((exoskeleton OR exosuit OR ortho*) AND (upper OR arm OR forearm OR shoulder OR elbow) AND (rehabilitation OR “physical therapy” OR impairment OR health) AND (intellig* OR adaptive OR netw* OR “artificial neur*” OR ANN OR learn*) AND (wearable OR mobile OR portable) NOT (low* OR hip OR gait OR walk*)) |
| Web of Science | TS=((exoskeleton OR exosuit OR ortho*) AND (upper OR arm OR forearm OR shoulder OR elbow) AND (rehabilitation OR “physical therapy” OR impair* OR health) AND (intellig* OR adaptiv* OR netw* OR “artificial neur*” OR ANN OR learn*) AND (wearable OR mobile OR portable) NOT (low* OR hip OR gait OR walk* OR vision OR theoretical)) AND PY=(2020 OR 2019 OR 2018 OR 2017 OR 2016) |
| PubMed | ((exoskeleton OR exosuit OR ortho*) AND (upper OR arm OR forearm OR shoulder OR elbow) AND (rehabilitation OR “physical therapy” OR impair* OR health) AND (intellig* OR adaptiv* OR netw* OR “artificial neur*” OR ANN OR learn*) AND (wearable OR mobile OR portable) NOT (low* OR hip OR gait OR walk*)) AND ((“2016”[Date—Publication]: “2020”[Date—Publication])) |
| No. | Ref. | Year | MF | Exoskeleton Type | Portability | Used AI Techniques | Operation Modes | Medical App. | DoF-Joint |
|---|---|---|---|---|---|---|---|---|---|
| 1 | [22] | 2016 | Dev. | Hard: 3DPL/ME | Wearable | Artificial Neural Networks | AC/PA/RE | NMR | (1)-Wrist |
| 2 | [23] | 2016 | Dev. | Hard: PL/ME | Semi-mobile | Adaptive Finite State Machines | AC/RE /OT | MR | (2)-Shoulder (1)-Elbow |
| 3 | [24] | 2017 | Dev. | Hard: ME | Wearable | Adaptive Torque Compensation | AC/PA | AA/MR | (3)-Shoulder (2)-Elbow |
| 4 | [25] | 2017 | Dev. | Not Shown | Mobile | PD + Intelligent Active Force (AFC) + Particle Swarm Optimization | AC | MR | (1)-Shoulder (1)-Elbow |
| 5 | [26] | 2017 | Dev. | Hard: 3DPL/ME | Wearable | Fuzzy Logic via Artificial Neural Networks | AC | MR | (1)-Elbow |
| 6 | [27] | 2017 | Dev. | Dual Arm Hard: ME | Wearable | Adaptive Algorithms + Artificial Neural Networks | AC | NMR | (4)-Back (3)-Shoulder (1)-Elbow (2)-Wrist |
| 7 | [28] | 2017 | Com. | Semi-hard: PL | Wearable | Adaptive Fuzzy PID Controller | AC/OT | AA | (1)-Wrist/Elbow |
| 8 | [29] | 2017 | Dev. | Hard: 3DPL | Wearable | Adaptive Admittance and Proportional Derivative Cont. | AC | MR | (1)-Wrist |
| 9 | [30] | 2018 | Mix. | Mixed | Mixed | Mixed | AC/RE /OT | Mixed | Mixed |
| 10 | [31] | 2018 | Dev. | Hard: ME | Mobile | Adaptive Sliding Modes + Adaptive Proportional Derivative | AC | MR | (3)-Shoulder (2)-Elbow |
| 11 | [32] | 2018 | Dev. | Hard: PL | Wearable | Active Learning Mapping via KNN classifier | AC | AA | (1)-Wrist |
| 12 | [33] | 2018 | Dev. | Hard: 3DPL | Mobile | Reinforcement Learning via Artificial Neural Networks and Proximal Policy Optimization | PA | NMR | (2)-Shoulder (1)-Elbow |
| 13 | [34] | 2018 | Dev. | Dual Arm Hard: PL/ME | Semi-mobile | Impedance control via cascaded loop | AC | AA/NMR | (1)-Elbow (1)-Wrist |
| 14 | [35] | 2018 | Dev. | Mixed | Mixed | Adaptive controllers via mixed techniques. | AC/RE /OT | Mixed | Mixed |
| 15 | [36] | 2019 | Dev. | Hard: 3DPL/ME | Wearable | Sliding Mode anti-interference controller | PA | AA/MR | (1)-Elbow (1)-Wrist |
| 16 | [37] | 2019 | Dev. | Hard: PL/ME | Wearable | Adaptive Algorithms + Artificial Neural Networks | AC/PA | AA/MR | (1)-Elbow (5)-Passive |
| 17 | [38] | 2019 | Dev. | Not Shown | Mobile | Recurrence Quantification Analysis (RQA) | PA | AA | Not Shown |
| 18 | [39] | 2019 | Dev. | Hard: ME | Wearable | Hierarchical Support Vector Machines | AC | MR | (2)-Elbow (1)-Wrist |
| 19 | [40] | 2019 | Dev. | Hard: PL/ME | Wearable | Radial Basis Function Artificial Neural Network | AC | MR | (1)-Shoulder (1)-Elbow (1)-Wrist |
| 20 | [41] | 2019 | Dev. | Hard: ME | Wearable | Adaptive Feedforward control scheme | AC/PA | AA/MR | (1)-Elbow |
| 21 | [42] | 2019 | Dev. | Hard: 3DPL | Wearable | Fuzzy Logic via Artificial Neural Networks | AC | AA | (2)-Elbow (1)-Wrist |
| 22 | [43] | 2019 | Dev. | Hard: ME | Wearable | Backpropagated Neural Network | AC | MR | (2)-Elbow (1)-Wrist |
| 23 | [44] | 2019 | Mix. | Mixed | Mixed | Mixed | AC/RE /OT | Mixed | Mixed |
| 24 | [45] | 2019 | Dev. | Hard: ME | Semi-mobile | Heuristically-tuned Proportional Derivative cont. | AC | MR | (1)-Elbow |
| 25 | [46] | 2019 | Dev. | Hard: 3DPL/ME | Wearable | Adaptive Algorithms + Artificial Neural Networks | AC/RE /OT | AA/MR/NMR | (1)-Elbow |
| 26 | [47] | 2020 | Dev. | Hard: ME | Wearable | Artificial Neural Networks | AC | MR | (2)-Elbow (1)-Wrist |
| 27 | [48] | 2020 | Dev. | Hard: 3DPL | Semi-mobile | Backpropagated Neural Network | AC | AA/MR | (1)-Elbow |
| 28 | [49] | 2020 | Dev. | Dual Arm Hard: ME | Semi-mobile | Fuzzy Sliding Mode controller | AC/OT | AA/MR | (3)-Shoulder (1)-Elbow |
| 29 | [50] | 2020 | Dev. | Soft | Wearable | Artificial Neural Networks + Sliding Mode controller | AC | MR | (1)-Shoulder (1)-Elbow |
| 30 | [51] | 2020 | Dev. | Soft | Wearable | Multivariate Multiple Regression via Artificial Neural Networks | AC | MR | (1)-Shoulder (1)-Elbow |
| 31 32 | [52] * [53] * | 2017 2019 | Dev. | Full-Body Hard: ME | Semi-mobile | Impedance control via cascaded loop + mixed | AC/RE /OT | AA/MR | (10)-Upper Body (30)-Full Body |
| 33 | [54] * | 2019 | Dev. | Full-Body Hard: 3DPL/ME | Semi-mobile | Mixed | AC/PA/RE | MR | (12)-Full Body |
| 34 | [55] * | 2017 | Dev. | Dual Arm Hard: 3DPL/ME | Mobile | Impedance control via cascaded loop + mixed | AC/RE /OT | MR | (14)-Upper Body |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vélez-Guerrero, M.A.; Callejas-Cuervo, M.; Mazzoleni, S. Artificial Intelligence-Based Wearable Robotic Exoskeletons for Upper Limb Rehabilitation: A Review. Sensors 2021, 21, 2146. https://doi.org/10.3390/s21062146
Vélez-Guerrero MA, Callejas-Cuervo M, Mazzoleni S. Artificial Intelligence-Based Wearable Robotic Exoskeletons for Upper Limb Rehabilitation: A Review. Sensors. 2021; 21(6):2146. https://doi.org/10.3390/s21062146
Chicago/Turabian StyleVélez-Guerrero, Manuel Andrés, Mauro Callejas-Cuervo, and Stefano Mazzoleni. 2021. "Artificial Intelligence-Based Wearable Robotic Exoskeletons for Upper Limb Rehabilitation: A Review" Sensors 21, no. 6: 2146. https://doi.org/10.3390/s21062146
APA StyleVélez-Guerrero, M. A., Callejas-Cuervo, M., & Mazzoleni, S. (2021). Artificial Intelligence-Based Wearable Robotic Exoskeletons for Upper Limb Rehabilitation: A Review. Sensors, 21(6), 2146. https://doi.org/10.3390/s21062146








