Head-Mounted Display-Based Therapies for Adults Post-Stroke: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
Immersive vs. Non-Immersive VR
2. Methods
2.1. Eligibility Criteria
2.2. Search Procedure
2.3. Methodological Quality Assessment
2.4. Quantitative Analysis
2.5. Outcome Measures
3. Results
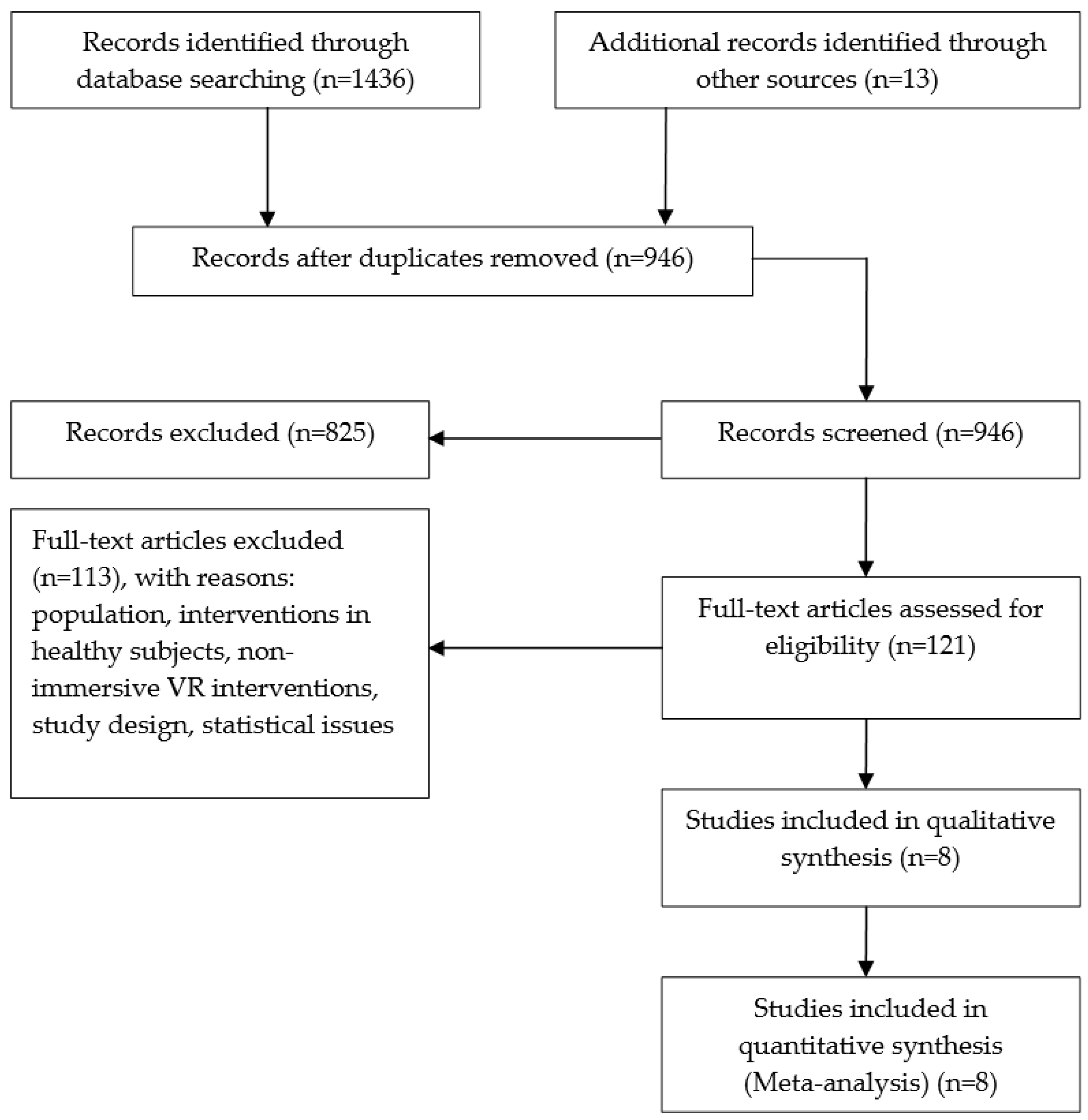
3.1. Search Results
3.2. Methodological Quality Assessment
3.3. Overview of Interventions
3.4. Outcomes Measures and Effect Sizes
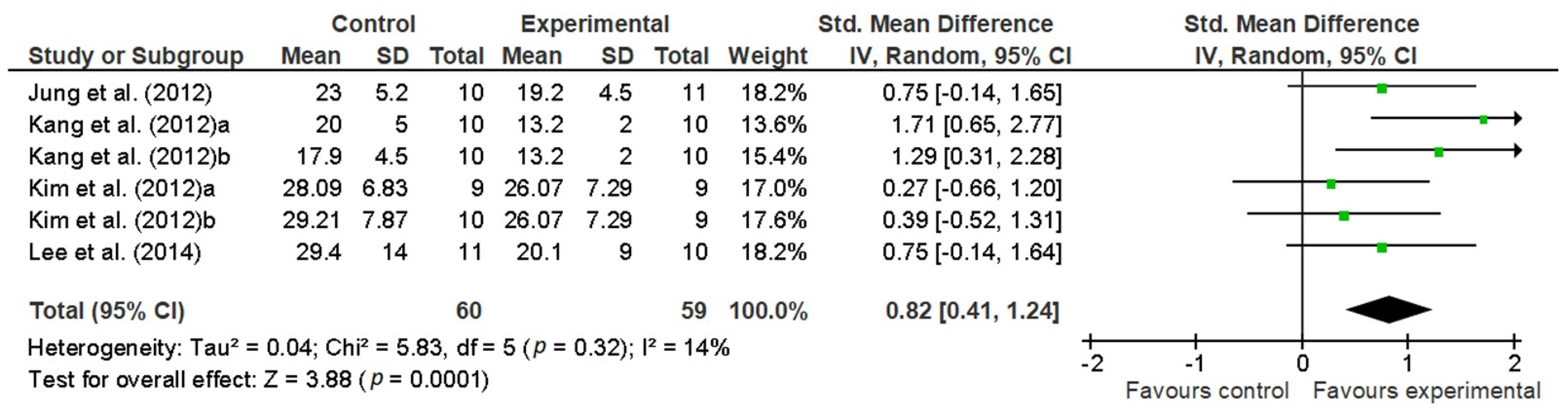
3.4.1. The Timed Up and Go (TUG) Test
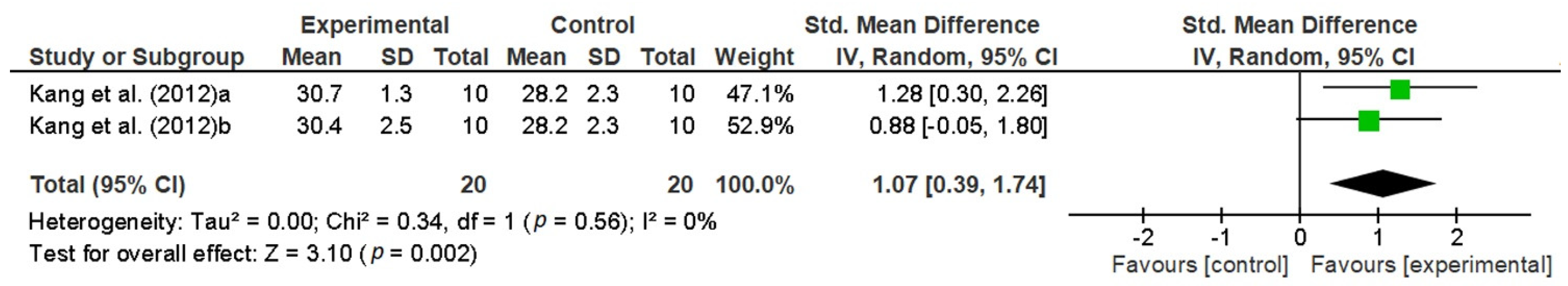
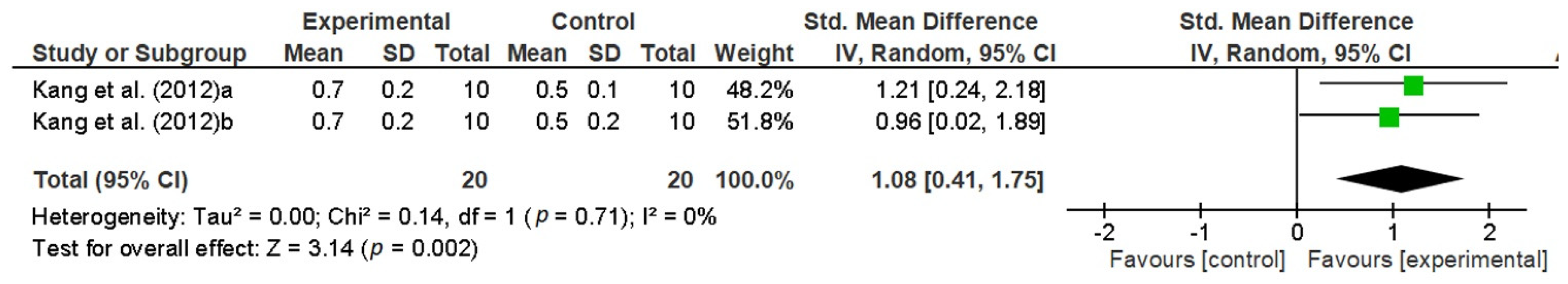
3.4.2. The Functional Reach Test (FRT)
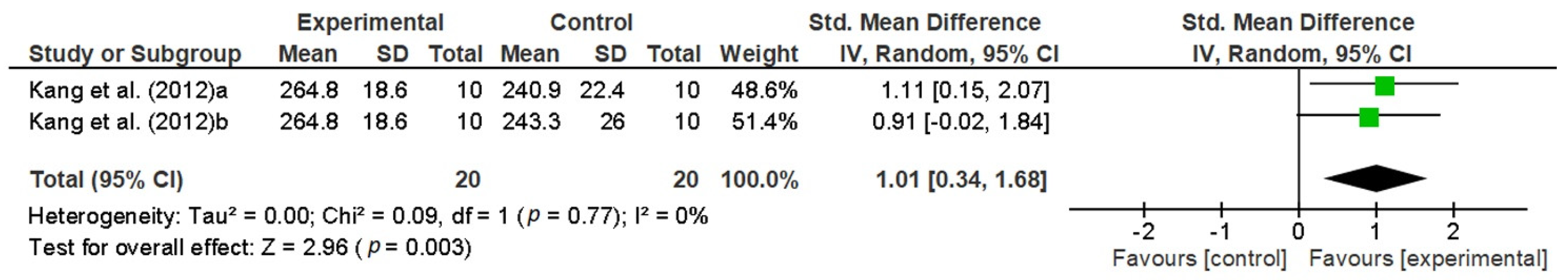
3.4.3. The Six-Minute Walk Test (6MWT)
3.4.4. The 10-Meter Walk Test (10MWT)
3.4.5. The Action Research Arm Test (ARAT)
3.4.6. The Fugl-Meyer Upper Extremity (FMUE)
3.4.7. Other Measures
4. Discussion
4.1. VR Treadmill and Feedback
4.2. Limitations
4.3. Implications for Research
4.4. Implications for Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rose, F.D.; Brooks, B.M.; Rizzo, A.A. Virtual Reality in Brain Damage Rehabilitation: Review. CyberPsychology Behav. 2005, 8, 241–262. [Google Scholar] [CrossRef]
- Holden, M.K. Virtual Environments for Motor Rehabilitation: Review. CyberPsychology Behav. 2005, 8, 187–211. [Google Scholar] [CrossRef]
- Iosa, M.; Morone, G.; Fusco, A.; Bragoni, M.; Coiro, P.; Multari, M.; Venturiero, V.; De Angelis, D.; Pratesi, L.; Paolucci, S. Seven Capital Devices for the Future of Stroke Rehabilitation. Stroke Res. Treat. 2012, 2012, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Crosbie, J.H.; Lennon, S.; McNeill, M.D.J.; McDonough, S.M. Virtual Reality in the Rehabilitation of the Upper Limb after Stroke: The User’s Perspective. CyberPsychology Behav. 2006, 9, 137–141. [Google Scholar] [CrossRef]
- Sveistrup, H. Motor Rehabilitation Using Virtual Reality. J. Neuroeng. Rehabil. 2004, 1, 10. [Google Scholar] [CrossRef]
- Langhorne, P.; Coupar, F.; Pollock, A. Motor Recovery after Stroke: A Systematic Review. Lancet Neurol. 2009, 8, 741–754. [Google Scholar] [CrossRef]
- Henderson, A.; Korner-Bitensky, N.; Levin, M. Virtual Reality in Stroke Rehabilitation: A Systematic Review of Its Effectiveness for Upper Limb Motor Recovery. Top. Stroke Rehabil. 2007, 14, 52–61. [Google Scholar] [CrossRef]
- Paolucci, S.; Di Vita, A.; Massicci, R.; Traballesi, M.; Bureca, I.; Matano, A.; Iosa, M.; Guariglia, C. Impact of Participation on Rehabilitation Results: A Multivariate Study. Eur. J. Phys. Rehabil. Med. 2012, 48, 455–466. [Google Scholar] [PubMed]
- Sisto, S.A.; Forrest, G.F.; Glendinning, D. Virtual Reality Applications for Motor Rehabilitation After Stroke. Top. Stroke Rehabil. 2002, 8, 11–23. [Google Scholar] [CrossRef]
- Broeren, J.; Claesson, L.; Goude, D.; Rydmark, M.; Sunnerhagen, K.S. Virtual Rehabilitation in an Activity Centre for Community-Dwelling Persons with Stroke. The Possibilities of 3-Dimensional Computer Games. Cereb. Dis. 2008, 26, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Housman, S.J.; Scott, K.M.; Reinkensmeyer, D.J. A Randomized Controlled Trial of Gravity-Supported, Computer-Enhanced Arm Exercise for Individuals with Severe Hemiparesis. Neurorehabil. Neural Repair 2009, 23, 505–514. [Google Scholar] [CrossRef]
- Yavuzer, G.; Senel, A.; Atay, M.B.; Stam, H.J. “Playstation Eyetoy Games” Improve Upper Extremity-Related Motor Functioning in Subacute Stroke: A Randomized Controlled Clinical Trial. Eur. J. Phys. Rehabil. Med. 2008, 44, 237–244. [Google Scholar]
- Yang, Y.-R.; Tsai, M.-P.; Chuang, T.-Y.; Sung, W.-H.; Wang, R.-Y. Virtual Reality-Based Training Improves Community Ambulation in Individuals with Stroke: A Randomized Controlled Trial. Gait Posture 2008, 28, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Walker, C.; Brouwer, B.J.; Culham, E.G. Use of Visual Feedback in Retraining Balance Following Acute Stroke. Phys. Ther. 2000, 80, 886–895. [Google Scholar] [CrossRef]
- Merians, A.S.; Jack, D.; Boian, R.; Tremaine, M.; Burdea, G.C.; Adamovich, S.V.; Recce, M.; Poizner, H. Virtual Reality-Augmented Rehabilitation for Patients Following Stroke. Phys. Ther. 2002, 82, 898–915. [Google Scholar] [CrossRef]
- Weiss, P.L.; Kizony, R.; Feintuch, U.; Katz, N. Virtual reality in neurorehabilitation. In Textbook of Neural Repair and Rehabilitation; Selzer, M., Clarke, S., Cohen, L., Duncan, P., Gage, F., Eds.; Cambridge University Press: Cambridge, UK, 2006; pp. 182–197. ISBN 978-0-511-54507-8. [Google Scholar]
- Schultheis, M.T.; Rizzo, A.A. The Application of Virtual Reality Technology in Rehabilitation. Rehabil. Psychol. 2001, 46, 296–311. [Google Scholar] [CrossRef]
- Schultheis, M.T.; Himelstein, J.; Rizzo, A.A. Virtual Reality and Neuropsychology: Upgrading the Current Tools. J. Head Trauma Rehabil. 2002, 17, 378–394. [Google Scholar] [CrossRef] [PubMed]
- Weiss, P.L.T.; Katz, N. The Potential of Virtual Reality for Rehabilitation. J. Rehabil. Res. Dev. 2004, 41, vii–x. [Google Scholar]
- Lange, B.; Koenig, S.; Chang, C.-Y.; McConnell, E.; Suma, E.; Bolas, M.; Rizzo, A. Designing Informed Game-Based Rehabilitation Tasks Leveraging Advances in Virtual Reality. Disabil. Rehabil. 2012, 34, 1863–1870. [Google Scholar] [CrossRef] [PubMed]
- Sherman, W.R.; Craig, A.B. Understanding Virtual Reality: Interface, Application, and Design; Morgan Kaufmann Series in Computer Graphics and Geometric Modeling; Morgan Kaufmann Publishers: Amsterdam, The Netherlands; Boston, MA, USA, 2003; ISBN 978-1-55860-353-0. [Google Scholar]
- Riva, G. Virtual environments in clinical psychology. Psychotherapy 2003, 40, 68–76. [Google Scholar] [CrossRef]
- Oujamaa, L.; Relave, I.; Froger, J.; Mottet, D.; Pelissier, J.-Y. Rehabilitation of arm function after stroke. Literature review. Ann. Phys. Rehabil. Med. 2009, 52, 269–293. [Google Scholar] [CrossRef]
- Crosbie, J.; McDonough, S.; Lennon, S.; McNeill, M. Development of a virtual reality system for the rehabilitation of the upper limb after stroke. Stud. Health Technol. Inform. 2005, 117, 218–222. [Google Scholar] [PubMed]
- Peñasco-Martín, B.; Reyes-Guzmán, A.D.L.; Gil-Agudo, Á.; Bernal-Sahún, A.; Pérez-Aguilar, B.; De La Peña-González, A.I. [Application of virtual reality in the motor aspects of neurorehabilitation]. Revista de Neurología 2010, 51, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Laver, K.E.; George, S.; Thomas, S.; Deutsch, J.E.; Crotty, M. Virtual reality for stroke rehabilitation. In Cochrane Database of Systematic Reviews; The Cochrane Collaboration, Ed.; John Wiley & Sons, Ltd.: Chichester, UK, 2011; p. CD008349.pub2. [Google Scholar]
- Rizzo, A.A.; Schultheis, M.; Kerns, K.A.; Mateer, C. Analysis of assets for virtual reality applications in neuropsychology. Neuropsychol. Rehabil. 2004, 14, 207–239. [Google Scholar] [CrossRef]
- Being There: Concepts, Effects and Measurements of User Presence in Synthetic Environments; Riva, G., Davide, F., IJsselsteijn, W.A., Eds.; Emerging Communication: Studies in New Technologies and Practices in Communication; IOS Press: Amsterdam, The Netherlands; Washington, DC, USA; Tokyo, Japan, 2003; ISBN 978-1-58603-301-9. [Google Scholar]
- Heeter, C. Being There: The Subjective Experience of Presence. Presence Teleoperators Virtual Environ. 1992, 1, 262–271. [Google Scholar] [CrossRef]
- Draper, J.V.; Kaber, D.B.; Usher, J.M. Telepresence. Hum. Factors 1998, 40, 354–375. [Google Scholar] [CrossRef] [PubMed]
- McNeill, M.; Pokluda, L.; McDonough, S.; Crosbie, J. Immersive Virtual Reality for Upper Limb Rehabilitation Following Stroke. In Proceedings of the IEEE International Conference on Systems, Man and Cybernetics, The Hague, The Netherlands, 10–13 October 2004; Volume 3, pp. 2783–2789. [Google Scholar]
- Li, Z.; Han, X.-G.; Sheng, J.; Ma, S.-J. Virtual Reality for Improving Balance in Patients after Stroke: A Systematic Review and Meta-Analysis. Clin. Rehabil. 2016, 30, 432–440. [Google Scholar] [CrossRef]
- Corbetta, D.; Imeri, F.; Gatti, R. Rehabilitation That Incorporates Virtual Reality Is More Effective than Standard Rehabilitation for Improving Walking Speed, Balance and Mobility after Stroke: A Systematic Review. J. Physiother. 2015, 61, 117–124. [Google Scholar] [CrossRef]
- Iruthayarajah, J.; McIntyre, A.; Cotoi, A.; Macaluso, S.; Teasell, R. The Use of Virtual Reality for Balance among Individuals with Chronic Stroke: A Systematic Review and Meta-Analysis. Top. Stroke Rehabil. 2017, 24, 68–79. [Google Scholar] [CrossRef] [PubMed]
- Saposnik, G. Virtual Reality in Stroke Rehabilitation. In Ischemic Stroke Therapeutics: A Comprehensive Guide; Springer International Publishing: New York, NY, USA; pp. 225–233. ISBN 978-3-319-17749-6.
- Booth, V.; Masud, T.; Connell, L.; Bath-Hextall, F. The Effectiveness of Virtual Reality Interventions in Improving Balance in Adults with Impaired Balance Compared with Standard or No Treatment: A Systematic Review and Meta-Analysis. Clin. Rehabil. 2014, 28, 419–431. [Google Scholar] [CrossRef]
- Physiotherapy Evidence Database (PEDro). Available online: https://pedro.org.au/ (accessed on 28 December 2020).
- Moseley, A.M.; Herbert, R.D.; Sherrington, C.; Maher, C.G. Evidence for Physiotherapy Practice: A Survey of the Physiotherapy Evidence Database (PEDro). Aust. J. Physiother. 2002, 48, 43–49. [Google Scholar] [CrossRef]
- Hedges, L.V.; Olkin, I. Statistical Methods for Meta-Analysis; Academic Press: Orlando, FL, USA, 1985; ISBN 978-0-12-336380-0. [Google Scholar]
- Law, M.C.; MacDermid, J. Evidence-Based Rehabilitation: A Guide to Practice; SLACK Incorporated: Thorofare, NJ, USA, 2008; ISBN 978-1-55642-768-8. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988; ISBN 978-0-8058-0283-2. [Google Scholar]
- Sawilowsky, S.S. New Effect Size Rules of Thumb. J. Mod. App. Stat. Meth. 2009, 8, 597–599. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying Heterogeneity in a Meta-Analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Introduction to Meta-Analysis; Borenstein, M., Ed.; John Wiley & Sons: Chichester, UK, 2009; ISBN 978-0-470-05724-7. [Google Scholar]
- Ögün, M.N.; Kurul, R.; Yaşar, M.F.; Turkoglu, S.A.; Avci, Ş.; Yildiz, N. Effect of Leap Motion-Based 3D Immersive Virtual Reality Usage on Upper Extremity Function in Ischemic Stroke Patients. Arq. Neuro-Psiquiatr. 2019, 77, 681–688. [Google Scholar] [CrossRef]
- Lee, C.-H.; Kim, Y.; Lee, B.-H. Augmented Reality-Based Postural Control Training Improves Gait Function in Patients with Stroke: Randomized Controlled Trial. Hong Kong Physiother. J. 2014, 32, 51–57. [Google Scholar] [CrossRef]
- Crosbie, J.; Lennon, S.; McGoldrick, M.; McNeill, M.; McDonough, S. Virtual Reality in the Rehabilitation of the Arm after Hemiplegic Stroke: A Randomized Controlled Pilot Study. Clin. Rehabil. 2012, 26, 798–806. [Google Scholar] [CrossRef]
- Kang, H.-K.; Kim, Y.; Chung, Y.; Hwang, S. Effects of Treadmill Training with Optic Flow on Balance and Gait in Individuals Following Stroke: Randomized Controlled Trials. Clin. Rehabil. 2012, 26, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Foley, N.C.; Teasell, R.W.; Bhogal, S.K.; Speechley, M.R. Stroke Rehabilitation Evidence-Based Review: Methodology. Top. Stroke Rehabil. 2003, 10, 1–7. [Google Scholar] [CrossRef]
- Jung, J.; Yu, J.; Kang, H. Effects of Virtual Reality Treadmill Training on Balance and Balance Self-Efficacy in Stroke Patients with a History of Falling. J. Phys. Ther. Sci. 2012, 24, 1133–1136. [Google Scholar] [CrossRef]
- Kim, I.-C.; Lee, B.-H. Effects of Augmented Reality with Functional Electric Stimulation on Muscle Strength, Balance and Gait of Stroke Patients. J. Phys. Ther. Sci. 2012, 24, 755–762. [Google Scholar] [CrossRef]
- Jaffe, D.L.; Brown, D.A.; Pierson-Carey, C.D.; Buckley, E.L.; Lew, H.L. Stepping over Obstacles to Improve Walking in Individuals with Poststroke Hemiplegia. JRRD 2004, 41, 283. [Google Scholar] [CrossRef]
- Park, Y.-H.; Lee, C.; Lee, B.-H. Clinical Usefulness of the Virtual Reality-Based Postural Control Training on the Gait Ability in Patients with Stroke. J. Exerc. Rehabil. 2013, 9, 489–494. [Google Scholar] [CrossRef]
- Crosbie, J.H.; McNeill, M.D.J.; Burke, J.; McDonough, S. Utilising Technology for Rehabilitation of the Upper Limb Following Stroke: The Ulster Experience. Phys. Ther. Rev. 2009, 14, 336–347. [Google Scholar] [CrossRef]
- Duncan, P.W.; Weiner, D.K.; Chandler, J.; Studenski, S. Functional Reach: A New Clinical Measure of Balance. J. Gerontol. 1990, 45, M192–M197. [Google Scholar] [CrossRef]
- Harris-Love, M.L.; Macko, R.F.; Whitall, J.; Forrester, L.W. Improved Hemiparetic Muscle Activation in Treadmill versus Overground Walking. Neurorehabil. Neural Repair 2004, 18, 154–160. [Google Scholar] [CrossRef]
- Bayat, R.; Barbeau, H.; Lamontagne, A. Speed and Temporal-Distance Adaptations during Treadmill and Overground Walking Following Stroke. Neurorehabil. Neural Repair 2005, 19, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Harvey, R.L. Improving Poststroke Recovery: Neuroplasticity and Task-Oriented Training. Curr. Treat. Options Cardiovasc. Med. 2009, 11, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Hwang, W.-H.; Tsai, Y.-C.; Liu, F.-K.; Hsieh, L.-F.; Chern, J.-S. Improving Balance Skills in Patients Who Had Stroke through Virtual Reality Treadmill Training. Am. J. Phys. Med. Rehabil. 2011, 90, 969–978. [Google Scholar] [CrossRef] [PubMed]
- Pailhous, J.; Ferrandez, A.M.; Flückiger, M.; Baumberger, B. Unintentional Modulations of Human Gait by Optical Flow. Behav. Brain Res. 1990, 38, 275–281. [Google Scholar] [CrossRef]
- Prokop, T.; Schubert, M.; Berger, W. Visual Influence on Human Locomotion. Modulation to Changes in Optic Flow. Exp. Brain Res. 1997, 114, 63–70. [Google Scholar] [CrossRef]
- Varraine, E.; Bonnard, M.; Pailhous, J. Interaction between Different Sensory Cues in the Control of Human Gait. Exp. Brain Res. 2002, 142, 374–384. [Google Scholar] [CrossRef]
- Pickhinke, J.; Chien, J.H.; Mukherjee, M. Varying the Speed of Perceived Self-Motion Affects Postural Control during Locomotion. Stud. Health Technol. Inf. 2014, 196, 319–324. [Google Scholar]
- Hollman, J.H.; Brey, R.H.; Bang, T.J.; Kaufman, K.R. Does Walking in a Virtual Environment Induce Unstable Gait? Gait Posture 2007, 26, 289–294. [Google Scholar] [CrossRef]
- Katsavelis, D.; Mukherjee, M.; Decker, L.; Stergiou, N. The Effect of Virtual Reality on Gait Variability. Nonlinear Dyn. Psychol. Life Sci. 2010, 14, 239–256. [Google Scholar]
- Mukherjee, M.; Siu, K.-C.; Katsavelis, D.; Fayad, P.; Stergiou, N. The Influence of Visual Perception of Self-Motion on Locomotor Adaptation to Unilateral Limb Loading. J. Mot. Behav. 2011, 43, 101–111. [Google Scholar] [CrossRef]
- Mendelson, D.N.; Redfern, M.S.; Nebes, R.D.; Richard Jennings, J. Inhibitory Processes Relate Differently to Balance/Reaction Time Dual Tasks in Young and Older Adults. Aging Neuropsychol. Cogn. 2009, 17, 1–18. [Google Scholar] [CrossRef]
- Lamontagne, A.; Fung, J.; McFadyen, B.J.; Faubert, J. Modulation of Walking Speed by Changing Optic Flow in Persons with Stroke. J. Neuroeng. Rehabil. 2007, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- Powell, W.A.; Hand, S.; Stevens, B.; Simmonds, M. Optic Flow with a Stereoscopic Display: Sustained Influence on Speed of Locomotion. Annu. Rev. CyberTherapy Telemed. 2006, 4, 65–70. [Google Scholar]
- Jang, S.H.; You, S.H.; Hallett, M.; Cho, Y.W.; Park, C.-M.; Cho, S.-H.; Lee, H.-Y.; Kim, T.-H. Cortical Reorganization and Associated Functional Motor Recovery After Virtual Reality in Patients with Chronic Stroke: An Experimenter-Blind Preliminary Study. Arch. Phys. Med. Rehabil. 2005, 86, 2218–2223. [Google Scholar] [CrossRef]
- You, S.H.; Jang, S.H.; Kim, Y.-H.; Hallett, M.; Ahn, S.H.; Kwon, Y.-H.; Kim, J.H.; Lee, M.Y. Virtual Reality-Induced Cortical Reorganization and Associated Locomotor Recovery in Chronic Stroke: An Experimenter-Blind Randomized Study. Stroke 2005, 36, 1166–1171. [Google Scholar] [CrossRef]
- Banz, R.; Bolliger, M.; Colombo, G.; Dietz, V.; Lünenburger, L. Computerized Visual Feedback: An Adjunct to Robotic-Assisted Gait Training. Phys. Ther. 2008, 88, 1135–1145. [Google Scholar] [CrossRef] [PubMed]
- Horlings, C.G.C.; Carpenter, M.G.; Küng, U.M.; Honegger, F.; Wiederhold, B.; Allum, J.H.J. Influence of Virtual Reality on Postural Stability during Movements of Quiet Stance. Neurosci. Lett. 2009, 451, 227–231. [Google Scholar] [CrossRef]
- Keshner, E.A.; Kenyon, R.V. Postural and Spatial Orientation Driven by Virtual Reality. Stud. Health Technol. Inf. 2009, 145, 209–228. [Google Scholar] [CrossRef]
- Van Peppen, R.P.S.; Kortsmit, M.; Lindeman, E.; Kwakkel, G. Effects of Visual Feedback Therapy on Postural Control in Bilateral Standing after Stroke: A Systematic Review. J. Rehabil. Med. 2006, 38, 3–9. [Google Scholar] [CrossRef]
- Crosbie, J.H.; Lennon, S.; Basford, J.R.; McDonough, S.M. Virtual Reality in Stroke Rehabilitation: Still More Virtual than Real. Disabil. Rehabil. 2007, 29, 1139–1146. [Google Scholar] [CrossRef]
- Durgin, F.H.; Li, Z. Controlled Interaction: Strategies for Using Virtual Reality to Study Perception. Behav. Res. Methods 2010, 42, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Knapp, J.; Loomis, J. Visual Perception of Egocentric Distance in Real and Virtual Environments. In Virtual and Adaptive Environments; Hettinger, L., Haas, M., Eds.; CRC Press: Boca Raton, FL, USA, 2003; pp. 21–46. ISBN 978-0-8058-3107-8. [Google Scholar]
- Mon-Williams, M.; Bingham, G.P. Ontological Issues in Distance Perception: Cue Use under Full Cue Conditions Cannot Be Inferred from Use under Controlled Conditions. Percept. Psychophys. 2008, 70, 551–561. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liebermann, D.G.; Berman, S.; Weiss, P.L.; Levin, M.F. Kinematics of Reaching Movements in a 2-D Virtual Environment in Adults with and Without Stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2012, 20, 778–787. [Google Scholar] [CrossRef]
- Piggott, L.; Wagner, S.; Ziat, M. Haptic Neurorehabilitation and Virtual Reality for Upper Limb Paralysis: A Review. Crit. Rev. Biomed. Eng. 2016, 44, 1–32. [Google Scholar] [CrossRef]
- Schultheis, M.T.; Rebimbas, J.; Mourant, R.; Millis, S.R. Examining the Usability of a Virtual Reality Driving Simulator. Assist. Technol. 2007, 19, 1–10. [Google Scholar] [CrossRef]
- Turolla, A.; Dam, M.; Ventura, L.; Tonin, P.; Agostini, M.; Zucconi, C.; Kiper, P.; Cagnin, A.; Piron, L. Virtual Reality for the Rehabilitation of the Upper Limb Motor Function after Stroke: A Prospective Controlled Trial. J. Neuroeng. Rehabil. 2013, 10, 85. [Google Scholar] [CrossRef]
- Tsoupikova, D.; Stoykov, N.S.; Corrigan, M.; Thielbar, K.; Vick, R.; Li, Y.; Triandafilou, K.; Preuss, F.; Kamper, D. Virtual Immersion for Post-Stroke Hand Rehabilitation Therapy. Ann. Biomed. Eng. 2015, 43, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, S.K.; Levin, M.F. Viewing Medium Affects Arm Motor Performance in 3D Virtual Environments. J. Neuroeng. Rehabil. 2011, 8, 36. [Google Scholar] [CrossRef]
- Borrego, A.; Latorre, J.; Llorens, R.; Alcañiz, M.; Noé, E. Feasibility of a Walking Virtual Reality System for Rehabilitation: Objective and Subjective Parameters. J. Neuroeng. Rehabil. 2016, 13, 68. [Google Scholar] [CrossRef] [PubMed]
- Slater, M.; Steed, A. A Virtual Presence Counter. Presence Teleoperators Virtual Environ. 2000, 9, 413–434. [Google Scholar] [CrossRef]
- Witmer, B.G.; Singer, M.F. Measuring presence in virtual environments. Meas. Presence Virtual Environ. 1994, 53. [Google Scholar] [CrossRef]
- Palacios-Navarro, G.; Albiol-Pérez, S.; García-Magariño García, I. Effects of Sensory Cueing in Virtual Motor Rehabilitation. A Review. J. Biomed. Inform. 2016, 60, 49–57. [Google Scholar] [CrossRef]
- Viau, A.; Feldman, A.G.; McFadyen, B.J.; Levin, M.F. Reaching in Reality and Virtual Reality: A Comparison of Movement Kinematics in Healthy Subjects and in Adults with Hemiparesis. J. Neuroeng. Rehabil. 2004, 1, 11. [Google Scholar] [CrossRef]
- Lam, Y.S.; Man, D.W.K.; Tam, S.F.; Weiss, P.L. Virtual Reality Training for Stroke Rehabilitation. Neurorehabilitation 2006, 21, 245–253. [Google Scholar] [CrossRef]
- Lee, G. Effects of Training using video games on the muscle strength, muscle tone, and activities of daily living of chronic stroke patients. J. Phys. Ther. Sci. 2013, 25, 595–597. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.-S.; Park, M.-J.; Yoon, I.-J.; Park, S.-H. Effects of virtual reality on upper extremity function and activities of daily living performance in acute stroke: A double-blind randomized clinical trial. Neurorehabilitation 2012, 31, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Jang, S.H.; Kim, C.S.; Jung, J.H.; You, J.H. Use of virtual reality to enhance balance and ambulation in chronic stroke: A double-blind, randomized controlled study. Am. J. Phys. Med. Rehabil. 2009, 88, 693–701. [Google Scholar] [CrossRef]
- Reid, D. The use of virtual reality to improve upper-extremity efficiency skills in children with cerebral palsy: A pilot study. Technol. Disabil. 2002, 14, 53–61. [Google Scholar] [CrossRef]
- Azulay, J.-P.; Mesure, S.; Blin, O. Influence of visual cues on gait in Parkinson’s disease: Contribution to attention or sensory dependence? J. Neurol. Sci. 2006, 248, 192–195. [Google Scholar] [CrossRef] [PubMed]
- Nieuwboer, A.; Kwakkel, G.; Rochester, L.; Jones, D.; Van Wegen, E.; Willems, A.M.; Chavret, F.; Hetherington, V.; Baker, K.; Lim, I. Cueing training in the home improves gait-related mobility in Parkinson’s disease: The RESCUE trial. J. Neurol. Neurosurg. Psychiatry 2007, 78, 134–140. [Google Scholar] [CrossRef]
- Griffin, H.J.; Greenlaw, R.; Limousin, P.; Bhatia, K.P.; Quinn, N.P.; Jahanshahi, M. The effect of real and virtual visual cues on walking in Parkinson’s disease. J. Neurol. 2011, 258, 991–1000. [Google Scholar] [CrossRef]
- Viirre, E.; Sitarz, R. Vestibular rehabilitation using visual displays: Preliminary study. Laryngoscope 2002, 112, 500–503. [Google Scholar] [CrossRef] [PubMed]
- Suárez, H.; Suarez, A.; Lavinsky, L. Postural adaptation in elderly patients with instability and risk of falling after balance training using a virtual-reality system. Int. Tinnitus J. 2006, 12, 41–44. [Google Scholar]
- Fischer, H.C.; Stubblefield, K.; Kline, T.; Luo, X.; Kenyon, R.V.; Kamper, D.G. Hand rehabilitation following stroke: A pilot study of assisted finger extension training in a virtual environment. Top. Stroke Rehabil. 2007, 14, 1–12. [Google Scholar] [CrossRef]
- Willemsen, P.; Colton, M.B.; Creem-Regehr, S.H.; Thompson, W.B. The effects of head-mounted display mechanical properties and field of view on distance judgments in virtual environments. ACM Trans. Appl. Percept. 2009, 6, 8. [Google Scholar] [CrossRef]




| Author(s)/Year of Publication/ PEDro Score | Participants | Stroke Onset (Months) | Study Design | Control/Experimental Group Interventions | Outcome Measures | Conclusions |
|---|---|---|---|---|---|---|
| Age (yrs ± SD) | ||||||
| Gender (M, F) | ||||||
| Jaffe et al. (2004) [52]/ PEDro: 4/10 | N = 20 | Control: 42.9 ± 30.1 | RCT | Control: stepping over real foam objects in a hallway (60 min, 3/week × 2 weeks) | Gait endurance: 6MWT | The VR training achieved higher improvements in velocity compared to control training |
| OG group (N = 10) | Subjects showed clinically meaningful changes in stride length, velocity, obstacle clearance capacity, and walking endurance | |||||
| Age: 63.6 ± 8.3 | ||||||
| Gender: (7 M, 3 F) | ||||||
| VR group (N = 10) | ||||||
| Age: 58.2 ± 11.2 | Gait kinematics: spatiotemporal gait parameters (walking velocity, cadence, and stride length) | |||||
| Gender: (5 M, 5 F) | Exp: 47 ± 27.5 | Experimental: stepping over virtual objects on a treadmill (60 min, 3/week × 2 weeks) | Obstacle clearance test, balance test | |||
| Jung et al. (2012) [50]/ PEDro: 5/10 | N = 21 | Control: 15.4 ± 4.7 | RCT | Control: treadmill walking training (30 min, 5/week × 3 weeks) | Balance (TUG) | There were significantly higher improvements in TUG and ABC in the VR treadmill-training group compared to the control group. |
| Control group (N = 10) | Significant increases in TUG and ABC in both groups after training. | |||||
| Age: 63.6 ± 5.1 | Improvements seen in the experimental group were significantly larger than the control group. | |||||
| Gender: (6 M, 4F) | ||||||
| Exp. group (N = 11) | ||||||
| Age: 60.5 ± 8.6 | ||||||
| Gender: (7 M, 4 F) | Exp: 12.6 ± 3.3 | Experimental: treadmill walking in a virtual outdoor environment (30 min, 5/week × 3 weeks) | Balance self-efficacy (ABC scale) | |||
| Park et al. (2013) [53]/ PEDro: 5/10 | N = 16 | Control: 135 ± 54.4 | RCT with follow-up | Control: two administrations of conventional rehabilitation (60 min, 5/week × 4 weeks) + (30 PT min, 3/week × 4 weeks) | Functional gait ability (10MWT) | Subjects in the VR group showed a significant improvement (except for cadence) after training and at the follow-up (compared to the control group). |
| Control group (N = 8) | Within groups, the VR group demonstrated greater improvements in stride length (only) compared to the control group | |||||
| Age: 48.75± 8.81 | No significant differences found in other parameters | |||||
| Gender: (5 M, 3 F) | ||||||
| Exp. group (N = 8) | ||||||
| Age: 46.25 ± 6.84 | ||||||
| Gender: (6 M, 2 F) | Exp: 139.5 ± 53.3 | Experimental: conventional rehabilitation (60 min, 5/week × 4 weeks) + VR-based postural control exercises (30 min, 3/week × 4 weeks) | Spatiotemporal gait ability (velocity, cadence, step length, and stride length) | |||
| Kang et al. (2012) [48]/ PEDro: 7/10 | N = 30 | TOF group: 14.1 ± 4.4 | RCT | Control: Conventional rehabilitation (30 min × 5/week × 4 weeks) + stretching added ROM exercises (30 min, 3/week × 4 weeks) | Balance (TUG, FRT) | Treadmill using optic flow speed modulation improved the balance and gait significantly compared to the control group |
| TOF group (N = 10) | Treadmill group: 13.5 ± 4.0 | Gait (6MWT, 10MWT) | ||||
| Age: 55.9 ± 6.5 | ||||||
| Gender: (6 M, 4 F) | Control group: 15.1 ± 7.4 | |||||
| Treadmill group (N = 10) | ||||||
| Age: 56.3 ± 7.6 | ||||||
| Gender: (4 M, 6 F) | ||||||
| Control group (N = 10) | ||||||
| Age: 56.1 ± 7.8 | Treadmill group = Conventional rehabilitation (30 min × 5/week × 4 weeks) + treadmill training (30 min, 3/week × 4 weeks) | |||||
| Gender: 6 M, 4 F | TOF group (Exp.): Conventional rehabilitation (30 min × 5/week × 4 week) + treadmill walking with optic flow (30 min, 3/week × 4 weeks) | |||||
| Crosbie et al. (2012) [47]/ PEDro: 8/10 | N = 18 | Control: 11.7 ± 7.8 | RCT with follow-up | Control: conventional therapy (30–45 min, 3/week × 3 weeks) | ARAT, upper limb motricity index | Neither small nor moderate changes were detected by measures |
| Control group (N = 9) | No significant improvement in either the control or intervention groups | |||||
| Age: 66.4 ± 7.4 | Transient dizziness and headache experienced by two participants in the VR group | |||||
| Gender: (5 M, 4 F) | ||||||
| VR group (N = 9) Age: 56.1 ± 14.5 | ||||||
| Gender: (5 M, 4 F) | VR group: 10 ± 6.4 | Experimental: specific upper limb VR tasks (reach to target, reach and grasp) (30–45 min, 3/week × 3 weeks) | ||||
| Lee et al. (2014) [46]/ PEDro: 7/10 | N = 21 | Exp: 11.7 ± 4.5 | RCT | Control: general physical therapy focused on postural control training (30 min, 5/week, 4 weeks) | BBS, TUG, gait velocity, stride length, cadence, and step length | The addition of VR-based training conveyed to significant improvement in the following gait variables (step length, stride length, and gait velocity) compared to general physical therapy treatment only (control group) |
| Control Group (N = 11) | ||||||
| Age: 54.0 ± 11.9 Gender: (6 M, 5 F) | No significant time × group effect in both TUG and BBS. | |||||
| AR group (N = 10) Age: 47.9 ± 12 | ||||||
| Gender: (8 M, 2 F) | Control: 11 ± 4.7 | Experimental: general physical therapy (30 min, 5/week × 4 week) + VR-based postural control training (30 min, 3/week × 4 weeks) | ||||
| Kim et al. (2012 [51])/ PEDro: 4/10 | N = 28 | Control: 10.4 ± 3.1 | RCT | Control: general physical therapy (30 min, 5/week, 8 weeks) + treadmill gait training (20 min, 3/week, 8 weeks). | TUG, BBS, muscle strength | VR-FES and FES groups showed greater improvements in muscle strength than control group |
| Control group (N = 9) | FES group: general physical therapy (30 min, 5/week, 8 weeks) + treadmill gait training + FES (20 min, 3/week, 8 weeks) | Greater improvements in gait speed (assessed by TUG) in VR-FES group than control group | ||||
| Age: 49.11 ± 11 Gender: (6 M, 3 F) | VR + FES group: general physical therapy (30 min, 5/week, 8 weeks) + treadmill gait training + VR + FES (20 min, 3/week, 8 weeks) | Significant improvements in BBS in all groups | ||||
| FES group (N = 10) Age: 51.5 ± 12.9 Gender: (5 M, 5 F) | ||||||
| VR-FES group (N = 9) | ||||||
| Age: 47.4 ±8.4 | FES group: 9.2 ± 2.7 | |||||
| Gender: (6 M, 3 F) | VR-FES group: 9.7 ± 4.2 | |||||
| Ögün et al. (2019) [45]/ PEDro: 6/10 * | N = 65 | Control: 15.37 ± 9.77 | RCT | Control: conventional upper extremity active exercises focused on gripping and handling (45 min, 3/week, 6 weeks) + passive VR therapy (15 min, 3/week, 6 weeks) | FMUE, ARAT, FIM, PASS-IADL, PASS-BADL | Significant improvements in FMUE, ARAT, FIM, and PASS scores (compared to baseline) |
| Control group (N = 32) | ||||||
| Age: 59.75 ± 8.07 Gender: (23 M, 9 F) | ||||||
| VR group (N = 33) Age: 61.48 ± 10.92 Gender: (28 M, 5 F) | VR group: 14.72 ± 7.38 | Experimental: task-oriented games focused on gripping and handling (60 min, 3/week, 6 weeks) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palacios-Navarro, G.; Hogan, N. Head-Mounted Display-Based Therapies for Adults Post-Stroke: A Systematic Review and Meta-Analysis. Sensors 2021, 21, 1111. https://doi.org/10.3390/s21041111
Palacios-Navarro G, Hogan N. Head-Mounted Display-Based Therapies for Adults Post-Stroke: A Systematic Review and Meta-Analysis. Sensors. 2021; 21(4):1111. https://doi.org/10.3390/s21041111
Chicago/Turabian StylePalacios-Navarro, Guillermo, and Neville Hogan. 2021. "Head-Mounted Display-Based Therapies for Adults Post-Stroke: A Systematic Review and Meta-Analysis" Sensors 21, no. 4: 1111. https://doi.org/10.3390/s21041111
APA StylePalacios-Navarro, G., & Hogan, N. (2021). Head-Mounted Display-Based Therapies for Adults Post-Stroke: A Systematic Review and Meta-Analysis. Sensors, 21(4), 1111. https://doi.org/10.3390/s21041111







