Abstract
Heart rate variability (HRV) measurements provide information on the autonomic nervous system and the balance between parasympathetic and sympathetic activity. A high HRV can be advantageous, reflecting the ability of the autonomic nervous system to adapt, whereas a low HRV can be indicative of fatigue, overtraining or health issues. There has been a surge in wearable devices that claim to measure HRV. Some of these include spot measurements, whilst others only record during periods of rest and/or sleep. Few are capable of continuously measuring HRV (≥24 h). We undertook a narrative review of the literature with the aim to determine which currently available wearable devices are capable of measuring continuous, precise HRV measures. The review also aims to evaluate which devices would be suitable in a field setting specific to military populations. The Polar H10 appears to be the most accurate wearable device when compared to criterion measures and even appears to supersede traditional methods during exercise. However, currently, the H10 must be paired with a watch to enable the raw data to be extracted for HRV analysis if users need to avoid using an app (for security or data ownership reasons) which incurs additional cost.
1. Introduction
Heart rate variability (HRV) is a measure of the variation in time between adjacent heartbeats, otherwise known as R-R intervals [1,2]. HRV is a powerful biomarker and is sensitive to the level of activity and work, of both physiological and psychological systems [3]. An overall high HRV reflects the capability of the autonomic nervous system (ANS) to adapt to stressors, is indicative of good health and linked to the performance of executive function [2]. Reduced HRV is disadvantageous as it signifies poor ANS adaptability and has been found to be associated with fatigue, stress and overtraining [4].
Traditional methods of measuring HRV include electrocardiography (ECG). Clinical multi-lead ECG systems (e.g., Holter ECGs) are expensive, involve considerable participant and researcher burden and are not practical for field base monitoring in active populations. Whilst multi-lead ECG devices are established as the gold standard, devices using single lead ECG or photoplethysmography (PPG) are practical and simple to use [3]. The use of PPG technology to detect HRV is a relatively new method that has been integrated into wearable wrist and finger-worn devices. Although motion artefact has been noted as a limitation with this method, the comfort and feasibility of such devices make them appealing alternatives to multi-lead ECG systems [5]. Chest straps that use ECG electrodes provide another wireless solution for measuring HRV.
HRV is predominately described using time-domain or frequency-domain measurements. Other novel techniques are being explored within the literature, however, the Joint Position Statement by the e-Cardiology European Society of Cardiology Working Group and the European Heart Rhythm Association reported that both time and frequency domain measures are traditionally chosen to assess ANS physiology. This review will focus on these traditional techniques as they are widely employed within the literature and validated, making them the most reliable tools for HRV [6].
Time domain indices measure the amount of variability (time) between successive heart beats (the inter-beat interval, or R-R interval) [2]. Of the time domain measures, standard deviation of the normal-to-normal R-R intervals (SDNN) is typically measured over 24 h and reported in milliseconds (ms). The SDNN is the ‘gold standard’ measure for medical stratification of cardiac risk when recorded over 24 h [7]. Both the parasympathetic nervous system (PNS) and sympathetic nervous system (SNS) contribute to SDNN however, SNS makes a substantial contribution to 24 h recordings [2,8]. SDNN also provides information on overall HRV. When HRV is large and irregular, greater SDNN values are recorded [9]. The square root of the mean squared difference of successive R-R intervals over 24 h (RMSSD) is a measure of vagal modulation as 24 h values correlate strongly with high frequency HRV, a known measure of vagal HRV [2]. The percentage of adjacent R-R intervals that differ from each other by more than 50 ms (pNN50) is also a measure of vagal modulation [2].
Frequency domain methods involve applying Fast Fourier Transformation to separate HRV into different rhythms that operate within different frequency ranges [2]. Frequency domain methods are preferred when investigating short-term recordings [10] but they can also be used to analyse an entire 24 h period using ultra-low frequency (ULF). The physiological basis of ULF has been debated and is not clear. A recent study reported strong, significant correlations between ULF (≤0.003 Hz) and vagal markers of HRV and no correlations between ULF and sympathetic markers of HRV [11]. High frequency (HF, 0.15–0.40 Hz) reflects parasympathetic activity and is highly correlated with RMSSD and pNN50, whereas low frequency (LF, 0.04–0.15 Hz) denotes both parasympathetic and sympathetic activity. The ratio of LF:HF was originally deemed to reflect the balance between parasympathetic and sympathetic activity with a low LF:HF reflecting parasympathetic dominance and a high LF:HF indicating sympathetic influence [12] more recently, however, this model has come under scrutiny [13].
HRV is very useful in understanding the cardiovascular response to stress on the body. It can be used to evaluate the stress of acute exercise, changes to the ANS due to exercise training, and be used as a marker of overtraining or overreaching [14]. Monitoring HRV may also assist in improving individualised training prescription as HRV can assist in determining the intensity of a training session based on the PNS activity of an individual compared to their previous measures [15]. HRV guided training has been shown to be a beneficial tool for improving endurance running performance [15]. In addition, HRV has been identified in previous studies as a measure that could provide an early indication of illness and infection [16,17], although this requires further investigation to identify which illnesses and infections are associated with reduced HRV. A reduction in HRV (vagal withdrawal) may occur when an individual is exposed to a physical stressor, as this reduction in parasympathetic activity enables a greater effect on HR via activation of sympathetic activity to support the demands of the exercise or activity [14]. In relation to cognitive performance, reduced vagal control (specifically HF) has been related to a reduced ability to respond dynamically to changing demands and environments. This response then reduces the range of possible options and limits an individual’s ability to produce suitable responses and prevent inappropriate ones [18]. Individuals with a low HRV have shown to demonstrate poorer performance in association with short and long-term verbal memory, but not visual memory [19]. Overall, reduced HRV (RMSSD, SDNN, HF, LF, LF:HF) is associated with weaker cognitive performance [18]. If a cognitive task requires executive functioning, then vagal withdrawal is deemed maladaptive [20]. In contrast, a reduction in vagal activity is advantageous when an individual is subjected to a mental stressor that does not involve executive function as this demonstrates an individual’s ability to successfully deal with the stimulus [21,22].
The European Society of Cardiology and the North American Society of Pacing and Electrophysiology created a Task Force responsible for developing appropriate standards for HRV. The Task Force Recommendations [10] for the standardised measurement of HRV are either long term (24 h) or short term recordings (5 min). Continuous 24 h HRV measurements represent the cardiovascular systems response to a wide range of environmental stimuli and workloads. Circadian rhythms, core body temperature, metabolism, sleep cycle and renin-angiotensin system contribute to the variability seen in 24 h HRV recordings [2]. Short-term recordings are easier to conduct and involve fewer investigators/less participant burden and as such, are most commonly used throughout the non-clinical literature. More recently, even shorter recordings have become common (≤1 min) [23], however, these are not currently endorsed by the Task Force. In addition, as 24 h HRV measurements encompass measurements across the circadian rhythm, short term values are not interchangeable with 24 h HRV values [2].
Methodological issues are associated with many existing studies, as true baseline HRV measures have not been collected. In some studies, measurement of “baseline” HRV has been conducted close to the stimulus and therefore, responses to the stimulus may have already started to occur and influence HRV [24]. Furthermore, if not standardised and strictly controlled, short-term recordings (5 min) can be greatly influenced by external and internal factors, leading to inaccurate baseline measures. As HRV is unique to each person, accuracy of baseline HRV values is fundamental to ensuring confidence in subsequent measures. Dobbs et al. [25] concluded that meaningful interpretations of longitudinal HRV data are improved through weekly averages of consecutive day-to-day recordings which have been shown to be superior to snap-shot measures of HRV [26]. As 24 h HRV monitoring encompasses daily and nocturnal activity, longitudinal 24 h HRV recordings may provide a more holistic measure of HRV.
Within Defence communities it is recognised that data collected from its people could provide a valuable resource to provide new insight into human health, behaviour and performance. As such, Defence is exploring how data collected from individuals could be exploited to improve health and wellbeing, efficiency of training and performance monitoring. As part of this initiative, there is a requirement to understand how measures made with wearable devices could be used to assess an individual’s physiological and psychological state and ultimately predict performance of military tasks. Given the applicability of HRV to quantify and monitor both physiological and cognitive stressors, the authors recognise the need to evaluate commercial off-the-shelf wearable devices regarding accuracy, reliability, feasibility and robustness in a military environment. Evaluation of devices capable of 24 h recording of HRV in free-living participants has currently, to the authors’ knowledge, not been conducted. In addition, devices that may be suitable for the general population and recreational sporting activities may not be appropriate for military populations. The physical robustness and unobtrusiveness of a device and its ability to handle and provide easy access to data from large populations is an important consideration for use with military studies. Therefore, the aim of this review was to investigate whether currently available wearable devices are capable of providing continuous, reliable and precise measurements of standard HRV parameters (as recommended by the European Society of Cardiology and the North American Society of Pacing and Electrophysiology) in a field setting.
2. Materials and Methods
Database searches (Web of Science™ and PubMed) were conducted to identify articles appropriate for the review using the search terms “heart rate variability”, “HRV”, “wearable device”, “wearable technology”, “reliability” and “validity”. Abstracts and titles were screened for relevance and inclusion criteria applied. These criteria required articles to: (i) use human participants only; (ii) be published between 2010–2020; (iii) be written in English; (iv) use healthy participants; (v) measure HRV and (vi) use commercially available devices. Articles had their reference list checked and any relevant publications not identified in the initial search were screened and if relevant, were used in this review. In addition, a Google search was conducted to search for wearable devices, which claimed to measure HRV and were available on the market at that time (February–April 2020). The list of devices was then used as an additional search tool for any relevant validation studies or white papers through the databases above and through manufacturers’ commercial websites.
As a more global measure of HRV is achieved through 24 h recordings, devices with a battery life <24 h and no/insufficient internal memory were deemed unsuitable for continuous HRV recording and were not discussed any further. A down-select criteria (see Table 1) was applied to the list of devices using information from the manufacturers, device manuals, small internal pilot studies and feedback from subject matter experts. Devices that qualified for further review were required as a minimum to: (i) have the capability of continuously measuring HRV; (ii) measure a range of HRV parameters; (iii) have undergone validation; (iv) have a battery life ≥24 h; (v) have an internal memory, and (vi) have access to the raw data. Devices were also ranked against their robustness and suitability for military populations, although this was not essential for down-select.

Table 1.
Criteria used to assess wearable devices based on the peer-reviewed literature and manufacturer’s websites.
3. Results
The searches performed found thirty two devices capable of measuring HRV. Each device was scored against the criteria listed in Table 1 and the results are shown in Table 2. From this, the devices down-selected for additional consideration were:

Table 2.
Scoring matrix for each wearable device based on down-select criteria from Table 1 (device names highlighted in bold were down-selected).
- Bittium FarosTM (Bittium, Oulu, Finland);
- Bodyguard 2 (Firstbeat Technologies Ltd., Jyväskylä, Finland);
- Actiheart (CamNtech Ltd., Cambridgeshire, UK);
- AidlabTM (AidlabTM, Gdańsk, Poland);
- Polar H10 (Polar Electro UK Ltd., Warwick, UK);
- Equivital EQ-02 (Equivital, Cambridge, UK);
- Empatica E4 (Empatica Inc, Boston, United States);
- Biovotion Everion® (Biofourmis, Boston, United States).
Discussed also in the review are a selection of wristwatches, which are currently not capable of directly measuring continuous HRV, but which are required by some sensors to act as a data logger and method of extraction. These watches/devices are:
- Garmin Fenix® 6X and 6S (Garmin Ltd., Southampton, UK);
- Garmin Tactix® Charlie/Delta (Garmin Ltd., Southampton, UK);
- Polar Vantage V (Polar Electro UK Ltd., Warwick, UK);
- Actigraph wGT3X-BT (Actigraph, Pensacola, United States).
Table S1 (supporting material) provides a summary of the HRV parameters available from each wearable device.
3.1. ECG Monitors
3.1.1. Bittium FarosTM 360
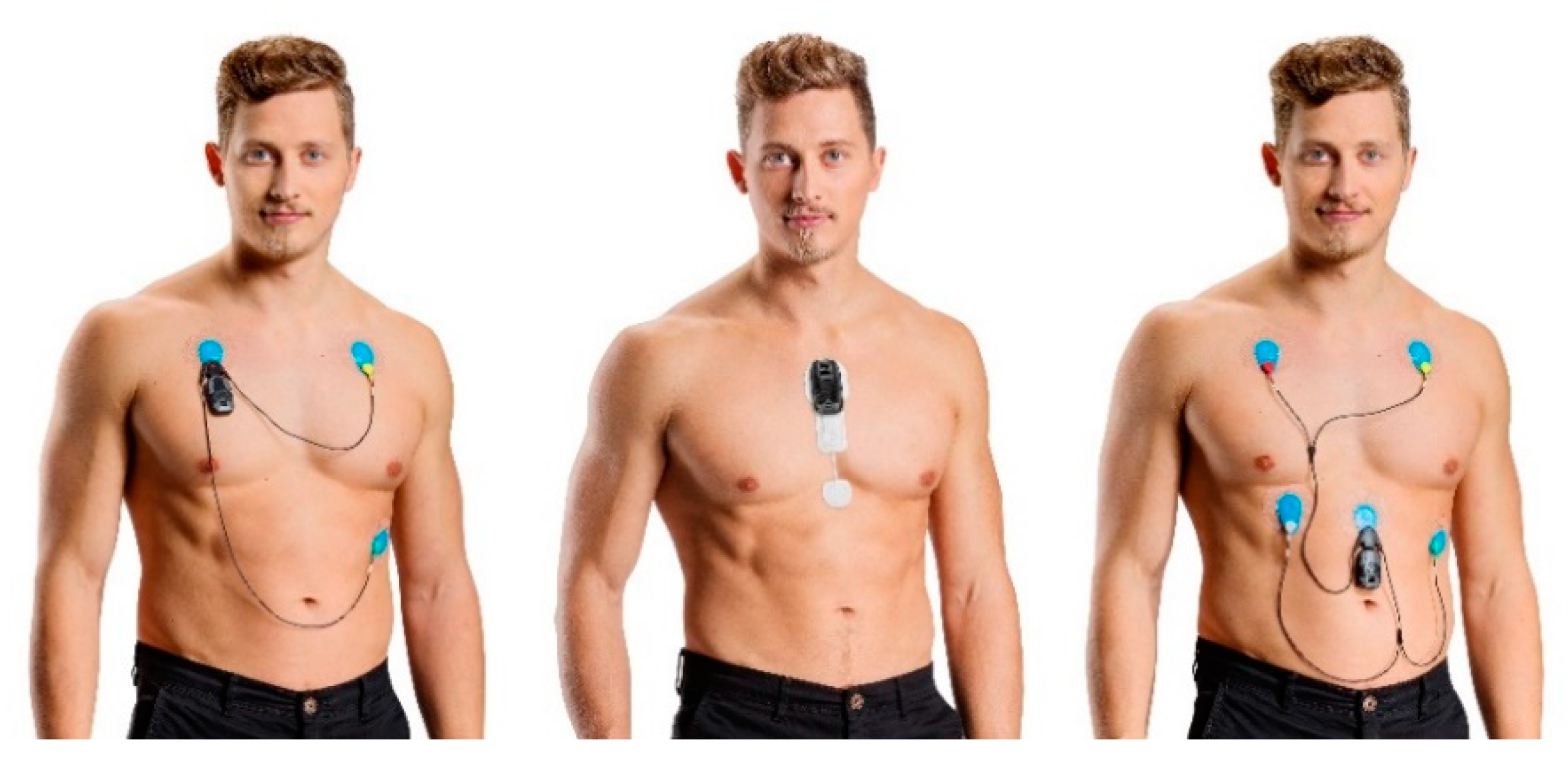
The Bittium FarosTM 360 can be used with a single or three-channel configuration. With a single channel configuration, the monitor fixes on the right superior pectoralis major at the midclavicular line with an electrode attached at the base of the ribs at the midclavicular line of the opposite side and an electrode fixed below the clavicle of the left side, symmetrical to the placement of the monitor (Figure 1). The devices are also able to attach onto a “FastFix waterproof patch” which enables wireless ECG measurement. The chest patch electrode can be used for three to seven days and replacement of the patch enables continuous recording.

Figure 1.
Bittium FarosTM 360 different configurations (image used with permission from Bittium [31]).
As the FarosTM ECG is a certified medical device, it is frequently used as a criterion measure/substitute for ECG [27,28,29] highlighting its ability to generate high quality, reliable and valid HRV data. At present in its commercial off-the-shelf form, the single channel configuration may not be suitable for use in the field as leads may catch or be displaced during military activities. However, a study proposal has identified the FarosTM 360 will be employed to measure HRV in military populations [30] and study details indicate that adaptions to electrode configuration have occurred so that wired connections are not required. The research project by Laarni et al. [30] is still ongoing and so results cannot be provided about the feasibility of the FarosTM device in the field. The FastFix patch has not, to the authors’ knowledge, been trialed with the use of body armour. It is hypothesised that the FastFix configuration could be uncomfortable for individuals when using body armour, although without pilot testing, this cannot be confirmed. If monitoring individuals without body armour, this device would be suitable for long-term monitoring due to the long battery life (8 days) and 180 days of internal memory.
3.1.2. Actiheart
Using two ECG electrodes, the Actiheart is placed below the apex of the sternum with a wire, approximately 100 mm, running from the monitor to a second electrode located on the same level laterally (Figure 2). This placement is considered to reduce noise from movement artefacts [32]. The Actiheart has been used in a number of validation studies, but most have involved HR only [33]. To date, the only validation study for HRV measurements is by Kristiansen et al. [32] which utilised 24 h recording in females during free living conditions. When compared to a three-lead ECG Holter, there were no systematic differences between HRV parameters (R-R mean, HF, LF, LF:HF). The slopes, as estimated by Deming regression analysis, were all close to 1 and the deviations were ≤3%. Deviations of this size were considered to have no practical relevance as the within-subject standard deviations were greater. The study concluded that Actiheart was a suitable device for measuring HRV during occupational and recreational activities. The use of the Actiheart in research with free-living populations is increasing [34] as it has a large internal memory (14 days) and is also validated for energy expenditure and physical activity detection. The suitability of the device for use with military populations is yet to be determined, especially considering its wired connections, but exceeds the Bittium FarosTM in battery life (14 days).

Figure 2.
Actiheart 5 device (image used with permission from Actiheart [35]).
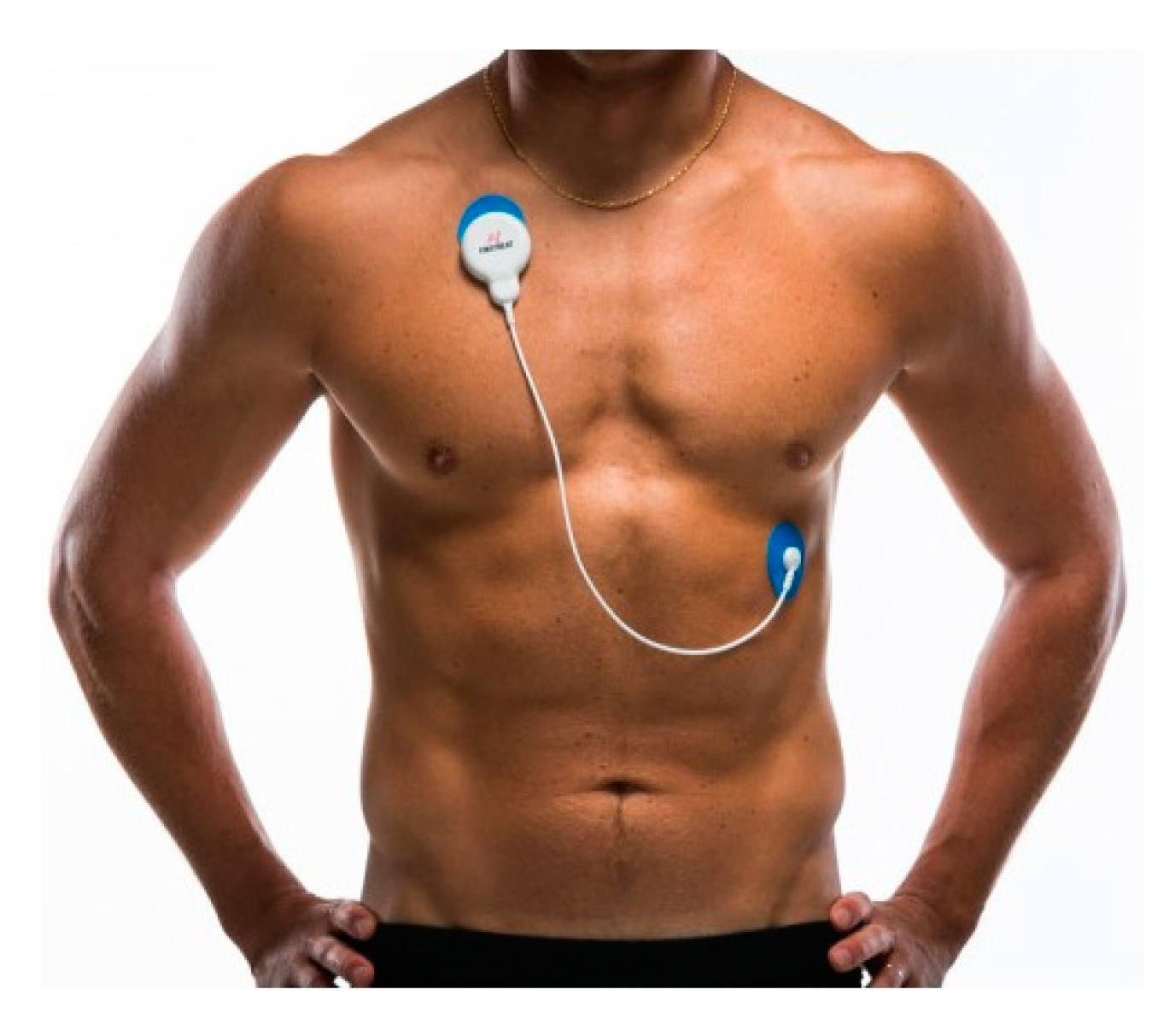
3.1.3. Firstbeat Bodyguard 2
Similar to the Actiheart, the Bodyguard 2 uses two electrodes (Figure 3), the first located under the right clavicle and the second on the left lower lateral side of the ribcage [36]. The device is lightweight, has a long battery life (6 days, 144 h) and has 20 days (480 h) of internal memory, making it suitable for long term monitoring. Furthermore, the data are readily available and easy to extract. Validation studies are limited, although Bogdány et al. [36] demonstrated very strong, significant correlations (r > 0.91, p <0.001) for SDNN, RMSSD and HF measurements when compared to a reference ECG (Nexus-10 MKII, Herten). Correlations for LF were significant, yet moderate (r = 0.55, p < 0.05). Bland and Altman plots showed acceptable levels of agreement between the reference values and values from the Bodyguard 2 but a t-test revealed significant differences for HF between devices (−1404.84 ± 1952.26, p = 0.018) indicating systematic measurement error. Given the relationship between HF and RMSSD (both representing vagal activity), the authors attributed this error to software issues. It was concluded that for long term HRV monitoring, the Bodyguard 2 was appropriate. Parak and Korhonen [37] explored the accuracy of the Bodyguard 2 by observing participants for 50 min, during which time they undertook various physical activities (walking and running at various speeds and gradients, and cycling at two different speeds). The Bodyguard 2 was compared to a two-channel ECG signal and was found to correctly detect 99.95% of all heartbeats which increased to 99.98% when an artefact correction was employed. Across all activities, mean absolute error was 4.45 and 2.27 ms before and after artefact correction respectively whilst the mean difference in RMSSD was 9.87 and 1.30 ms respectively. These results show that the Firstbeat Bodyguard 2 provides accurate data for HRV analysis during rest and exercise. Although data are promising, the limitations of this device include the risk of skin irritation with prolonged use, the device is considered by some users to be quite cumbersome and has a flashing light to show data transmission which can be seen through thin, light fabrics. Akin to other mobile ECG devices, the suitability for military populations is unclear due to wired connections which may not be appropriate when wearing body armour.

Figure 3.
Firstbeat Bodyguard 2 (image used with permission from Firstbeat [38]).
3.2. Clothing Garments
3.2.1. AidlabTM
The AidlabTM device can be worn as a chest strap or attached to a special clothing garment (see the AidlabTM website for an image of this device). The device uses single-channel ECG signals to measure R-R intervals, although it is noted by the company that when using the clothing garments, the stability of the electrodes can be disrupted, which results in a slightly lower ECG quality compared to a measurement taken via a chest strap. AidlabTM has been validated using the chest strap only, Czekaj et al. [39] compared the AidlabTM to the Polar H7 HR monitor in participants exercising for a total of 15 min. Exercise intensity was increased every 5 min during cycle ergometer exercise (low, moderate and heavy). Significant, strong positive correlations for R-R intervals between the H7 and the AidlabTM were reported (r > 0.99, p < 0.05), whilst mean R-R intervals were very close between the devices indicating good agreement (mean difference = 3.12 ± 0.89 ms, 0.76 ± 0.21%). An average of 3.92% of measurements were outside the limits of agreement, which is deemed satisfactory. To the current authors’ knowledge, this is the only study (although a whitepaper) which compares this technology to criterion measures. Nevertheless, these data show promising results for the ability of AidlabTM to provide accurate HRV data during exercise. A comparison with gold standard methods such as a Holter ECG or the Bittium FarosTM would be useful, as would a more detailed analysis of HRV parameters using both time and frequency domain measures. In addition, as the most accurate data are obtained using the chest strap, users must consider what advantages it holds over the Polar H10 (see Section 3.3.1). The AidlabTM does claim to estimate respiration rate and temperature (via infrared signals) however, if HRV is the key variable to be measured, the AidlabTM is costed at USD 279 (GBP 227) compared to the Polar H10 (GBP 80) which has been deemed as the gold standard HR monitor.
3.3. Chest, Shoulder and Arm Straps/Bands
3.3.1. Polar H10 Heart Rate Monitor
While multi-lead ECG devices are deemed the “gold standard”, simple HR chest belts using ECG technology have become increasingly popular and claim to accurately measure R-R intervals. Such devices have the advantage of being feasible for use under field conditions for which traditional ECG devices are unsuitable [3]. The Polar H7 has for a number of years been used as the reference for wearable HR monitoring [40,41] but a newer model (H10) claims to offer even more accurate R-R data (Figure 4). A study by Gilgen-Ammann et al. [3] is the first and only investigation to validate the Polar H10 at rest and during exercise. The Polar H10 was compared to a three-lead ECG Holter monitor and a mean bias of 0.23 ± 26.8 ms was observed for R-R intervals. Good signal quality was observed in 99.6% of the Polar H10 data and a high correlation was reported (r = 0.997) between methods. In addition, there were no significant differences between the two systems (p = 0.208). The R-R interval signal quality was based on the number of the missing R-R intervals and detection errors. During low and moderate intensity activity, the Polar H10 reported similar signal quality to the Holter whereas, during high intensity activity, the Polar outperformed the Holter, detecting only 74 R-R interval errors (99.4% signal quality) compared to 1332 R-R interval errors from the Holter (89.9% signal quality). The authors conclude that Polar H10 could be recommended as the gold standard for R-R interval assessments in sport settings.

Figure 4.
Polar H10 chest strap.
The method of attaching the Polar H10 to the participant may also offer greater comfort, when compared to a Holter ECG device, and ease of use during prolonged wear and/or intense physical activity. ECG Holter monitors require preparation of the skin (shaving and light abrasion with an alcohol swab) prior to being fixed via adhesive, gel-conductive electrodes with a coverage of <60 mm. These electrodes will then typically be replaced at least once every 24 h and the skin will require cleaning at these intervals. In comparison, the Polar H10 requires minimal attention, with the ECG contacts held comfortably against the skin by an adjustable elastic-polymer strap. Although feedback stated that wearing a chest strap can be uncomfortable during military procedures [42], soldiers carry and wear many pieces of equipment that are uncomfortable or are “nuisances”. It was reported that if the utility of the device is properly understood by the solider then soldiers are likely to accept the piece of equipment. Therefore, an explanation to participants of the usefulness and the requirement in the use of any device is paramount to ensure optimal adherence.
The Polar H10 has the advantage of being able to be used in water and during activities such as swimming and its long battery life means data collection in the field is not typically limited. Furthermore, it can be paired with other wearable devices, allowing data to be recorded and displayed during wear. Unlike other chest-worn HR monitors, the Polar H10 benefits from an internal memory which allows for HR and accelerometry data for a single activity (up to 30 h) without the need for a paired wristwatch or smartphone. Although this method does not currently allow access to the R-R intervals, meaning users cannot currently analyse HRV data collected without a paired watch or access to an app. The Polar Sensor Logger app allows users to log their R-R intervals via Bluetooth and this app uses the Polar Software Development Kit, which enables access to raw data. The Software Development Kit may allow for the future development of specialised logger applications. This could, for example, allow for the development of bespoke hardware and software that could allow for direct pairing with multiple Polar H10 monitors and automated data transfer and analysis whenever these monitors are within range of an encrypted Bluetooth-enabled computer.
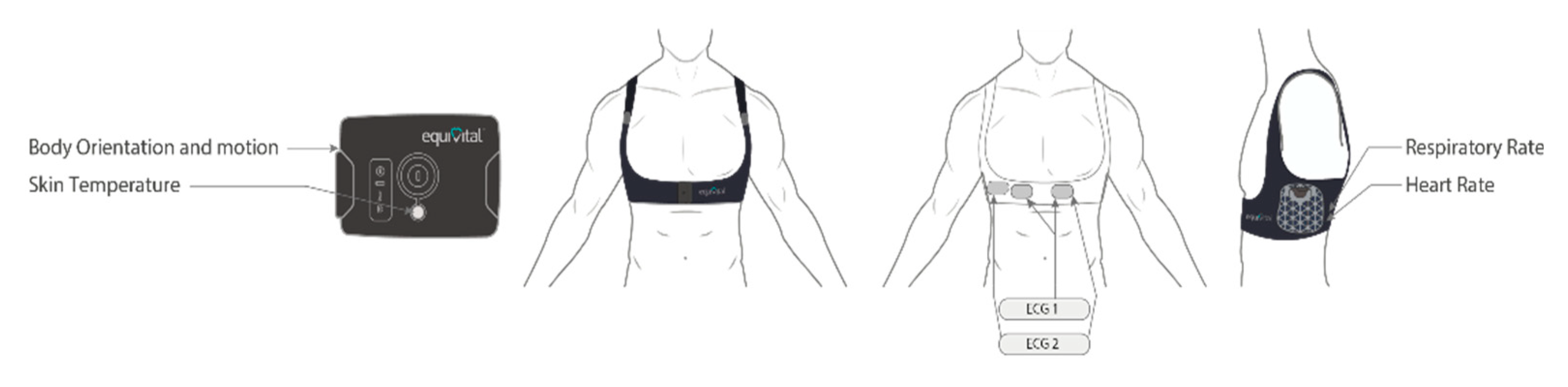
3.3.2. Equivital EQ-02
The Equivital EQ-01 has been used successfully in field studies to monitor HR [43] and HRV [44]. However, since then the system has been upgraded to the EQ-02 with improvements in design. The system consists of a sensor electronics module (SEM) that processes, stores and transmits the physiological data. The SEM (mass = 41.3 g) sits inside the sensor belt, on the left side, which incorporates two shoulder straps to provide more security (Figure 5). A two channel ECG incorporated into the chest belt measures R-R interval data.
When comparing the EQ-01 to the EQ-02, the findings of a survey of 39 US Infantry dismounted soldiers suggested that the Equivital EQ-02 system provided a better fit (~51%), easier donning (~10%), more comfort (~45%), reduced impact on military performance (~45%), reduced impact on the body (~17%) and was generally more acceptable for dismounted soldiers (~32%) [45]. Furthermore, when the EQ-02 was tested as part of a human factors assessment in 28 military personnel during chemical, biological, radiological, nuclear, and explosive training [46], the EQ-02 was deemed comfortable by 82% of participants (n = 23), with 89% believing this system would be acceptable for extended wear (>8 h). When asked whether the system had any impact on military performance, in individuals who wore body armour, a mean (± SD) score of 4.9 ± 0.3 was reported, with 4 = slight negative impact and 5 = no negative impact.
Akintola et al. [47] conducted the first, and to the present authors’ knowledge, only validation of the Equivital EQ-02 system for HRV monitoring. During a 24 h period, participants wore both the EQ-02 and a Holter three-channel ECG monitor. When all data were included (24 h), correlations between the two methods were r = 0.393, r = 0.285 and 0.982 for SDNN, RMSSD and pNN50, respectively. The average artefact percentage from this period was 12.76% compared to 2.95% by the Holter. When a 3 h recording with minimal artefacts (1.15%) was analysed, the correlation for pNN50 was similar (r = 0.967) but all correlations improved (r = 0.786 for SDNN and r = 0.868 for RMSSD). Thus, it was concluded that although the EQ-02 can measure HRV accurately, its validity is highly dependent on artefact content. Akintola et al. [47] stated that the advantages of the EQ-02 including its non-invasive methods and its ability to measure a number of physiological parameters should be considered above the disadvantages of higher artefact percentage when planning to measure HRV with large sample sizes or during field studies.

Figure 5.
Equivital EQ-02 device (image supplied by Equivital [48]).
Figure 5.
Equivital EQ-02 device (image supplied by Equivital [48]).
3.3.3. Biovotion Everion®
The Biovotion Everion® armband is available as a health and fitness device or as a medical device (CE class IIa) (see Biofourmis website for an image of this device). It is capable of collecting continuous data across a number of physiological parameters in a non-invasive manner, has a 4 day internal memory and a battery life of 46 h. Barrios et al. [49] investigated the level of agreement between the Everion®, the Empatica E4 and a medical grade 5-lead ECG Holter. Data were collected during rest and exercise of varying modes and intensities. For HR, the Everion® provided data similar to the Holter as there was no significant differences in mean HR and ICC showed excellent agreement (ICC = 0.985). At rest, there was good to excellent agreement between the Everion® and Holter across all HRV parameters. Excellent agreement was shown for all time domain measures (ICC ≥ 0.914) and moderate to excellent agreement for frequency domain measures (ICC ≥ 0.614). When exercise was performed, only LF and SDNN showed moderate to good agreement (LF: 0.266–0.945, SDNN: 0.755–0.835). All other parameters demonstrated poor agreement. The authors concluded that the Everion® is a valid surrogate for HRV measurement during periods of rest or low intensity activity and therefore this device would be suitable for continuous monitoring in individuals with sedentary lifestyles only.
3.4. Wrist Watches
3.4.1. Empatica E4
The Empatica E4 is one of very few PPG devices able to measure HRV from the wrist (see the Empatica website for further details and an image of the device). It employs red and green infra-red lights to determine blood volume pulse. Investigations into the signal quality of the E4 were conducted by McCarthy et al. [50]. Using long term HRV monitoring (24 h and 48 h) and comparing against Holter data, PPG data had poor data quality twice as often (10%) as the ECG (5%). This was primarily believed to be due to the location of the device. Pietilä et al. [51] evaluated the E4 during every day activities such as sitting, standing and household activities and also during cycling. Data from the E4 were compared to an ECG device (Bodyguard 2 by Firstbeat) in 20 males. The proportion of correct beat-to-beat detection was 67.9 ± 11.8% for E4 during sitting, 47.7 ± 20.9% during cycling and only 9.1 ± 14.2% during household work. The authors attributed such a low percentage during household activities to missed beats and the location of the sensors on the wrist, i.e., the wrist experiences much more motion than the torso. Furthermore, the E4 overestimated RMSSD particularly during cycling. During sitting, the criterion measure averaged RMSSD values of 46.6 ± 30.9 ms compared to 56.8 ± 30.9 ms for the E4, with a mean error of 10.2 ± 6.7 ms. This level of accuracy was deemed sufficient. During exercise, error was much greater, RMSSD for the criterion and E4 during cycling was 13.4 ± 5.5 ms and 62.1 ± 20.5 ms respectively with an error of 48.7 ± 21.8 ms. As stated previously, Barrios et al. [49] investigated the level of agreement between the Everion®, the Empatica E4 and a medical grade 5-lead ECG Holter. For HR data, the Empatica showed the largest bias (~17 bpm) and the bias increased with increased levels of activity. The location of the device was attributed to this large difference, as the activity was cycling during which the wrist is bent creating poor contact between the device and skin. For HRV data, the Empatica E4 suffered from significant amounts of missing data, so much so that HRV parameters were unable to be calculated for this study. The evidence collected concludes that HRV using the Empatica E4 can only be measured reliably and accurately during resting conditions. Empatica have developed a new device, the “Embrace Plus”, due to be launched soon. To date, no white papers or validation studies exist for this device, but it may be in the future that this new device has an improved capacity over the E4 for measuring HRV.
3.4.2. Polar Vantage V
Although the Polar Vantage V is capable of measuring HR through PPG technology, it can only provide HRV data during a 4 h period during sleep and there is currently no method to export R-R interval data for further analysis. For measurements during the day, or longer than 4 h, this device must be paired with a HR monitor (Polar H10 or H7 is recommended) to collect this information. The watch therefore acts as a means of extracting the data from the HR monitor. Nevertheless, the Polar Vantage V has received the prestigious iF and Red Dot design awards and its durability has been proven in several military standard tests (MIL-STD-810G). It can provide the user with a number of other measures including estimated energy expenditure and sleep indices. The long battery life (40 h) and ability to import data from a Polar device into commercial HRV analysis software, e.g., Kubios, makes this device attractive to researchers. Kubios has a function to import files directly from a Polar device when Kubios is paired to an associated cloud based Polar Flow account (although this still requires a Polar H10 paired to the device). This is suitable for individuals likely importing one file at a time, but it is not ideal for large scale research projects, especially those that wish to avoid uploading data to Polar Flow.
3.4.3. Garmin Watches
There are a number of Garmin watches available on the market. Each one comes with its own unique selling point, for example, the Garmin Tactix® Charlie and Delta were built with military users in mind. Both watches are similar to the Polar Vantage V are robust and have been tested to military standards (MIL-STD-810). They also contain features such as night-vision goggle compatibility and stealth mode, meaning users can stop sharing and storing GPS location should security be an issue. Furthermore, if security does become a problem, these devices contain a kill switch that wipes the device of all user memory. The primary difference between these two models is Delta has a larger internal memory capacity (32 GB vs. 16 GB) and greater battery life. The Fenix® 6X and 6S are both simpler versions of the Tactix® Delta watch (the Tactix® Charlie is a modified version of the Fenix® 5x). They are durable watches, having been tested to U.S. military standards for thermal, shock and water resistance, but have less technology associated with them and the main difference between the two models is the 6X has almost twice the battery life of the 6S. For monitoring HRV, they all perform the same role and act as a data logger. Similar to the Polar Vantage V, the watch uses HR via PPG technology to generate its own HRV score (stress/recovery score), but for accurate R-R interval data, a compatible chest strap is required. Currently, the only way for commercial software to import data from an ECG HR monitor, is for a watch to have been worn, although Kubios are currently creating an app (was due early 2020) which will be able to read live data from Polar sensors, including ECG and R-R data from Polar H10 sensors. Therefore, in regard to the accuracy and reliability of the watches for HRV, it is not applicable, as they do not directly measure HRV.
3.4.4. Actigraph wGT3X-BT
The Actigraph wGT3X-BT uses a 3-axis accelerometer to capture and record a variety of objective activity and sleep parameters (Figure 6). These data are then converted using publicly available algorithms to calculate a variety of measures including energy expenditure, activity counts, sleep indices and acceleration. The device is also capable of recording HRV but, similar to the watches above, it requires a Polar H10 or H7 chest strap to capture the R-R intervals. Real time data are not available, however depending on the situation in which data are being collected, this may be beneficial. When using military personnel as participants for research, this feature is advantageous as it means that no data on performance or health are fed back directly to the individual wearing their watch or their chain of command, the data are purely used for research purposes. For individual consumers, this would not be an attractive feature. The device benefits from an internal memory and longer battery life than the other watches (6.9 days with HR monitoring). This device has been successfully used by military populations to measure sleep activity during basic training, for which the research is due to be published.

Figure 6.
Actigraph wGT3X-BT.
4. Discussion
Monitoring and measuring HRV in military populations could be useful for tailoring individualised training programmes, indicating the onset of illness or infection, identifying risk of overreaching and overtraining, quantifying cognitive performance and as an overall measure of health. A number of currently available wearable devices may be incompatible with military users due to the placement of sensors and/ or wires, short battery life meaning monitoring over 24 h is not possible, insufficient or no internal memory and/or the technology not capable of dealing with harsh field conditions. There has been a large increase in the number of new wearable devices on the market claiming to measure HRV which require further investigation to determine their accuracy and feasibility in military field conditions.
Although significant improvements have been made in wearable technology for HRV, many of the commercially available off-the-shelf devices simply do not have the battery life, internal memory capacity to allow 24 h recordings, or are unable to take measurements during activity and therefore, are unsuitable for use in field settings. Clinical devices such as the Bittium FarosTM, Bodyguard 2 and Actiheart allow multi-day measurements, however, their practicality in defence research and long term individual monitoring is unclear as the devices are bulkier than other technologies.
Clothing garments with integrated sensors are unobtrusive and usually offer other physiological parameters alongside HRV. Evidence shows that such devices suffer from a lack of validation studies specifically for HRV parameters. Chest straps offer an easy and accurate alternative to ECG measurements and currently are the most accurate when compared to the more traditional methods. Although the advancement in technology design has reduced the bulkiness of the sensor on the strap, the acceptance and practicality of such a device within a military setting is still in its initial stages.
Devices using PPG have vastly improved in recent years but are still limited by inconsistencies in data attributed to location of the device (if on the wrist, subject to motion artefacts, if on the finger, the fit of the device can influence results), skin characteristics (e.g., pigmentation, tattoos), temperature, microcirculation and the pressure placed on the sensor [52]. In addition, due to the nature of PPG being susceptible to motion noise, there is also greater inaccuracy during periods of activity [49]. Georgiou et al. [4] compiled a systematic review comparing ECG derived R-R data with those produced by commercially available wearable PPG devices for accuracy and reliability. The authors reviewed 18 articles in total. All studies examined HRV at rest and, overall, the correlation between R-R interval (as measured by the Holter) and wearable devices (using PPG) was excellent (r = 0.91 to 0.99). Only eight of the studies examined HRV during exercise and all reported a reduction in the level of agreement as the intensity of exercise increased. It was concluded that due to the reduced accuracy in PPG devices during exercise, they should only be recommended as a surrogate for HRV during resting conditions, or very mild exercise, which is unfortunate given that during stressful situations such as vigorous exercise, this technology would be most useful [4].
PPG devices offer a less intrusive way to measure HRV as technology can be worn on the wrist or finger. A number of well-known commercial companies such as Oura ring, AVA bracelet, and Sosche Rhythm 24TM (listed in Table 2) are capable of measuring and storing R-R intervals, however, some only measure one HRV parameter and furthermore, these devices are only able to measure R-R intervals during rest/sleep and therefore not suitable for 24 h monitoring or during periods of activity. Regular HRV monitoring from either an overnight recording or a measurement upon awakening are becoming increasingly popular in both sporting and general populations and using algorithms, some devices can provide an individual with a proprietary “status” or “recovery score” which is easy for users to understand. As these algorithms are proprietary, they are not suitable for research purposes. Most devices provide individuals with perturbations from baseline. If establishing single, acute baseline values, these measurements should be standardised and controlled as the influence of both external (temperature, noise, and lighting) and internal factors (emotional behaviours) can affect HRV and the ability to collect a ‘true’ baseline value.
Longer duration recordings offer a more holistic measure of HRV as they encompass both nocturnal and daily activities. A study by Morrin et al. [53] compared 24 h HRV recordings to resting 5 min measurements and found significantly lower coefficient of variation (CV) with 24 h measures in all HRV parameters and showed superior reproducibility. When conducting intervention studies, it is recommended that 24 h HRV be measured [2,53]. Furthermore, when assessing the response to different stressors, measures from long duration recordings can offer more granularity in regard to the response of the ANS to a range of stimuli (e.g., magnitude of the reduction of parasympathetic activity on increasing exercise intensity or prior to a cognitive task).
Most recently, Dobbs et al. [25] performed a meta-analysis on studies measuring HRV obtained in a clinical or laboratory setting via an ECG, against HRV data collected from wearable devices (including Polar or Suunto HR monitors, ithlete). A small, yet significant amount of absolute error was detected when comparing the portable devices to ECG measures although error levels did not differ between postures. SDNN, when compared to all other HRV parameters, was the metric associated with the greatest amount of error (medium effect). However, RMSSD and HF (both reflective of the PNS) did not significantly differ in terms of error rates between methodologies. Although the wearable devices reported error rates when compared to ECG, these errors were small and the practicality and accessibility of the wearable devices outweigh the negligible error reported. Therefore, it is suggested that for performance and overall health research (not clinical research), the utility and cost-benefit of wearable technology to detect R-R intervals should be considered when designing HRV studies [25].
The Polar H10 strap appears to be a very strong contender for the most practical and accurate device used to collect HRV data, especially during exercise. Gilgen-Ammann et al. [3] concluded that the greater R-R interval detection during high intensity exercise could be attributed to the nature of the activity when compared to resting conditions. Excessive movements could create more noise in the electrical signal of the Holter due to wired connections whereas, electrodes are contained in a compact chest belt for the Polar H10. The major limitation with the H10 currently is that it must be paired with a watch such as the Polar Vantage, Actigraph or Garmin or a smartphone to enable the raw data to be extracted for HRV analysis. Polar have released a Software Developer Kit to bypass the requirement of a watch but currently (April 2020) no commercially available software solution has been marketed.
5. Conclusions
The aim of this review was to investigate whether currently available wearable devices are capable of providing continuous, reliable and precise measurements of standard HRV parameters for use in studies on military personnel. Apart from portable ECG monitors such as Bittium FarosTM, Bodyguard 2 and Actiheart, most other reviewed devices suffered from either poor validity, large amounts of missing data or artefacts, or were only reliable at rest or during low intensity exercise. The three named devices above, although shown as valid and accurate, are not suitable for use with military populations due to wired connections. The Polar H10 emerges as the most accurate wearable device when compared to criterion measures and reports less R-R interval error detection when compared to a Holter ECG device during exercise. Nevertheless, the H10 must be paired with a watch to enable the raw data to be extracted for HRV analysis if users need to avoid using an app (for security or data ownership reasons).
It must be noted that the battery life of the devices reviewed varies considerably and researchers should acknowledge that battery life values provided by the manufacturer must be taken with caution and are likely to be reduced in field study conditions. Therefore, prior to any field study, a pilot of the proposed technology and/or devices is recommended for information regarding accuracy, practicality, battery life testing, and data retrieval processes. Additionally, the sampling rate of a wearable device should be considered to ensure accuracy is not compromised. To ensure optimal adherence from participants, an explanation of the usefulness and the requirements of the device is crucial.
Future systems for measuring continuous HRV in a military field environment should have: a battery life >24 h, internal memory capacity that supports the storage of data >24 h, direct access to raw (R-R interval) data, low participant burden, and the ability to be used during movement. Furthermore, many of these new wearable devices have not been compared to criterion measures (Holter ECG or Bittium FarosTM) and therefore the level of agreement with validated, reliable tools during rest and exercise should be determined prior to use.
Supplementary Materials
The following are available online at https://www.mdpi.com/1424-8220/21/4/1061/s1, Table S1: HRV analysis known to be possible for each wearable device.
Author Contributions
Conceptualization, K.H. and N.A.; methodology, K.H.; Project Management, N.A. and G.W.; writing—original draft preparation, K.H.; writing—review and editing, K.H., N.A. and G.W.; supervision, N.A. and G.W. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the UK Ministry of Defence.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable.
Acknowledgments
The authors would like to thank Sue Tattersall and Katherine Cornes for reviewing this manuscript for internal approval prior to submission.
Conflicts of Interest
The authors declare no conflict of interest.
References
- The, A.F.; Reijmerink, I.; van der Laan, M.; Cnossen, F. Heart rate variability as a measure of mental stress in surgery: A systematic review. Int. Arch. Occup. Environ. Health 2020. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.; Ginsberg, J.P. An overview of heart rate variability metrics and norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed]
- Gilgen-Ammann, R.; Schweizer, T.; Wyss, T. RR interval signal quality of a heart rate monitor and an ECG Holter at rest and during exercise. Eur. J. Appl. Physiol. 2019, 119, 1525–1532. [Google Scholar] [CrossRef] [PubMed]
- Georgiou, K.; Larentzakis, A.V.; Khamis, N.N.; Alsuhaibani, G.I.; Alaska, Y.A.; Giallafos, E.J. Can wearable devices accurately measure heart rate variability? A systematic review. Folia Med. 2018, 60, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Moneghetti, K.J.; Christle, J.W.; Hadley, D.; Froelicher, V.; Plews, D. Heart rate variability: An old metric with new meaning in the era of using health technologies for health and exercise training guidance. Part two: Prognosis and training. Arrhythm Electrophysiol. Rev. 2018, 7, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Sassi, R.; Cerutti, S.; Lombardi, F.; Malik, M.; Huikuri, H.V.; Peng, C.K.; Schmidt, G.; Yamamoto, Y. Advances in heart rate variability signal analysis: Joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Europace 2015, 17, 1341–1353. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.; Hnatkova, K.; Huikuri, H.; Lombardi, F.; Schmidt, G.; Zabel, M. CrossTalk proposal: Heart rate variability is a valid measure of cardiac autonomic responsiveness. J. Physiol. 2019, 597, 2595–2598. [Google Scholar] [CrossRef] [PubMed]
- Grant, C.C.; van Rensburg, D.C.; Strydom, N.; Viljoen, M. Importance of tachogram length and period of recording during noninvasive investigation of the autonomic nervous system. Ann. Noninvasive Electrocardiol. 2011, 16, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.G.; Cheon, E.J.; Bai, D.S.; Lee, Y.H.; Koo, B.H. Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig. 2018, 15, 235–245. [Google Scholar] [CrossRef] [PubMed]
- Camm, A.J.; Malik, M.; Bigger, J.T.; Breithardt, G.; Cerutti, S.; Cohen, R.J.; Coumel, P.; Fallen, E.L.; Kennedy, H.L.; Kleiger, R.E.; et al. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur. Heart J. 1996, 17, 354–381. [Google Scholar]
- Lazzeroni, D.; Ziloli, C.; Colio, F.; Catellani, G.; Paglialonga, L.; Marazzi, P.; Moderato, L.; Bini, M.; Camaiora, U.; Geroldi, S.; et al. Relationship between ultra-low frequency of heart rate variability and autonomic function assessed by both 24H Holter ECG monitoring and cardiopulmonary exercise testing. Eur. Heart J. Suppl. 2019, 21, 197. [Google Scholar]
- Pagani, M.; Lombardi, F.; Guzzetti, S.; Rimoldi, O.; Furlan, R.; Pizzinelli, P.; Sandrone, G.; Malfatto, G.; Dell’Orto, S.; Piccaluga, E. Power spectral analysis of heart rate and arterial pressure variabilities as a marker of sympatho-vagal interaction in man and conscious dog. Circ. Res. 1986, 59, 178–193. [Google Scholar] [CrossRef]
- Billman, G.E. The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance. Front. Physiol. 2013, 4, 26. [Google Scholar] [CrossRef] [PubMed]
- Hernando, D.; Hernando, A.; Casajus, J.A.; Laguna, P.; Garatachea, N.; Bailon, R. Methodological framework for heart rate variability analysis during exercise: Application to running and cycling stress testing. Med. Biol. Eng. Comput. 2018, 56, 781–794. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, D.F.; Ferraro, Z.M.; Adamo, K.B.; Machado, F.A. Endurance Running Training Individually Guided by HRV in Untrained Women. J. Strength Cond. Res. 2019, 33, 736–746. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Ramsay, T.; Huebsch, L.; Flanagan, S.; McDiarmid, S.; Batkin, I.; McIntyre, L.; Sundaresan, S.R.; Maziak, D.E.; Shamji, F.M.; et al. Continuous multi-parameter heart rate variability analysis heralds onset of sepsis in adults. PLoS ONE 2009, 4, e6642. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Alamili, M.; Rosenberg, J.; Gogenur, I. Heart rate variability is reduced during acute uncomplicated diverticulitis. J. Crit. Care 2016, 32, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Forte, G.; Favieri, F.; Casagrande, M. Heart Rate Variability and Cognitive Function: A Systematic Review. Front. Neurosci. 2019, 13. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.J.; Su, S.; Veledar, E.; Bremner, J.D.; Goldstein, F.C.; Lampert, R.; Goldberg, J.; Vaccarino, V. Is heart rate variability related to memory performance in middle-aged men? Psychosom. Med. 2011, 73, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Hansen, A.L.; Johnsen, B.H.; Thayer, J.F. Vagal influence on working memory and attention. Int. J. Psychophysiol. 2003, 48, 263–274. [Google Scholar] [CrossRef]
- Lewis, M.J.; Kingsley, M.; Short, A.L.; Simpson, K. Rate of reduction of heart rate variability during exercise as an index of physcal work capacity. Scand. J. Med. Sci. Sports 2007, 17, 696–702. [Google Scholar] [CrossRef]
- Messerotti Benvenuti, S.; Mennella, R.; Buodo, G.; Palomba, D. Dysphoria is associated with reduced cardiac vagal withdrawal duringthe imagery of pleasant scripts: Evidence for the positive attenuation hypothesis. Biol. Psychol. 2015, 106, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Flatt, A.A.; Esco, M.R. Heart rate variability stabilization in athletes: Towards more convenient data acquisition. Clin. Physiol. Funct. Imaging 2016, 36, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.A., 3rd; Aikins, D.E.; Steffian, G.; Coric, V.; Southwick, S. Relation between cardiac vagal tone and performance in male military personnel exposed to high stress: Three prospective studies. Psychophysiology 2007, 44, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Dobbs, W.C.; Fedewa, M.V.; MacDonald, H.V.; Holmes, C.J.; Cicone, Z.S.; Plews, D.J.; Esco, M.R. The Accuracy of Acquiring Heart Rate Variability from Portable Devices: A Systematic Review and Meta-Analysis. Sports Med. 2019, 49, 417–435. [Google Scholar] [CrossRef] [PubMed]
- Plews, D.J.; Laursen, P.B.; Kilding, A.E.; Buchheit, M. Evaluating Training Adaptation with Heart-Rate Measures: A Methodological Comparison. Int. J. Sports Physiol. Perform. 2013, 8, 688–691. [Google Scholar] [CrossRef] [PubMed]
- Kinnunen, H.; Rantanen, A.; Kentta, T.; Koskimaki, H. Feasible assessment of recovery and cardiovascular health: Accuracy of nocturnal HR and HRV assessed via ring PPG in comparison to medical grade ECG. Physiol. Meas. 2020, 41, 04NT01. [Google Scholar] [CrossRef] [PubMed]
- Bent, B.; Goldstein, B.A.; Kibbe, W.A.; Dunn, J.P. Investigating sources of inaccuracy in wearable optical heart rate sensors. NPJ Digit. Med. 2020, 3, 18. [Google Scholar] [CrossRef] [PubMed]
- Vescio, B.; Salsone, M.; Gambardella, A.; Quattrone, A. Comparison between Electrocardiographic and Earlobe Pulse Photoplethysmographic Detection for Evaluating Heart Rate Variability in Healthy Subjects in Short- and Long-Term Recordings. Sensors 2018, 18, 844. [Google Scholar] [CrossRef] [PubMed]
- Laarni, J.; Pakarinen, S.; Bordi, M.; Kallinen, K.; Narvainen, J.; Kortelainen, H.; Lukander, K.; Pettersson, K.; Havola, J.; Pihlainen, K. Promoting Soldier Cognitive Readiness for Battle Tank Operations Through Bio-signal Measurements. In International Conference in Applied Human Factors and Ergonomics; Springer: Cham, Switzerland, 2019; pp. 142–154. [Google Scholar]
- Bittium. Bittium FarosTM—Cardiac Monitoring. Available online: https://www.bittium.com/medical/bittium-faros (accessed on 28 January 2021).
- Kristiansen, J.; Korshøj, M.; Skotte, J.H.; Jespersen, T.; Søgaard, K.; Mortensen, O.S.; Holtermann, A. Comparison of two systems for long-term heart rate variability monitoring in free-living conditions- a pilot study. Biomed. Eng. Online 2011, 10, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Brage, S.; Westgate, K.; Franks, P.W.; Stegle, O.; Wright, A.; Ekelund, U.; Wareham, N.J. Estimation of Free-Living Energy Expenditure by Heart Rate and Movement Sensing: A Doubly-Labelled Water Study. PLoS ONE 2015, 10. [Google Scholar] [CrossRef]
- Hallman, D.M.; Sato, T.; Kristiansen, J.; Gupta, N.; Skotte, J.; Holtermann, A. Prolonged Sitting is Associated with Attenuated Heart Rate Variability during Sleep in Blue-Collar Workers. Int. J. Environ. Res. Public Health 2015, 12, 14811–14827. [Google Scholar] [CrossRef] [PubMed]
- CamNtech. Actiheart 5. Available online: https://www.camntech.com/actiheart-5/ (accessed on 28 January 2021).
- Bogdány, T.; Boros, S.; Szemerszky, R.; Köteles, F. Validation of the Firstbeat TeamBelt and BodyGuard2 systems. Magy. Sporttudományi Szle. 2016, 17, 5–12. [Google Scholar]
- Parak, J.; Korhonen, I. Accuracy of Firstbeat Bodyguard 2 Beat-to-Beat Heart Rate Monitor; White Paper; Firstbeat Technology Ltd.: Tampere, Finland, 2013. [Google Scholar]
- Firstbeat Ltd. Bodyguard 2. Available online: https://shop.firstbeat.com/product/bodyguard-2/ (accessed on 28 January 2021).
- Czekaj, L.; Daniszewski, M.; Domaszewicz, J. Validation of the Aidlab solution for measuring Heart Rate Variability; Aidlab: Gdańsk, Poland, 2019. [Google Scholar]
- Cheatham, S.W.; Kolber, M.J.; Ernst, M.P. Concurrent validity of resting pulse-rate measurements: A comparison of 2 smartphone applications, the polar H7 belt monitor, and a pulse oximeter with bluetooth. J. Sport Rehabil. 2015, 24, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Giles, D.; Draper, N.; Neil, W. Validity of the Polar V800 heart rate monitor to measure RR intervals at rest. Eur. J. Appl. Physiol. 2016, 116, 563–571. [Google Scholar] [CrossRef] [PubMed]
- Tharion, W.J.; Hoyt, R.W. Form Factor Evaluation of Open Body Area Network (OBAN) Physiological Status Monitoring (PSM) System Prototype Designs; U.S. Army Research Insititue of Environmental Medicine: Natick, MA, USA, 2018. [Google Scholar]
- Teien, H.K.; Castellani, J.; Martini, S.; Pasiakos, S.M. Physiological monitoring during multi-day Norwegian ski patrols in the artic. J. Sci. Med. Sport 2017, 20, S134–S135. [Google Scholar] [CrossRef]
- Reiger, A.; Stoll, R.; Kreuzfeld, S.; Behrens, K.; Weippert, M. Heart rate and heart rate variability as indirect markers of surgeons’ intraoperative stress. Int. Arch. Occup. Environ. Health 2014, 87, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Tharion, W.J.; Buller, M.J.; Potter, A.W.; Karis, A.J.; Goetz, V.; Hoyt, R. Acceptability and usability of an ambulatory health monitoring system for use by military personnel. IIE Trans. Occup. Ergon. Human Factors 2013, 1, 203–214. [Google Scholar] [CrossRef]
- Tharion, W.J.; Buller, M.J.; Clements, C.M.; Dominguez, D.; Sampsonis, C.; Mullen, S.P.; Karis, A.J.; Potter, A.W. Human Factors Evaluation of Equvital EQ-02 Physiological Status Monitoring System; Army Research Institute of Environmental Medicine: Natick, MA, USA, 2013. [Google Scholar]
- Akintola, A.A.; van de Pol, V.; Bimmel, D.; Maan, A.C.; van Heemst, D. Comparative Analysis of the Equivital EQ02 Lifemonitor with Holter Ambulatory ECG Device for Continuous Measurement of ECG, Heart Rate, and Heart Rate Variability: A Validation Study for Precision and Accuracy. Front. Physiol. 2016, 7, 391. [Google Scholar] [CrossRef] [PubMed]
- Equivital. eq lifemonitor. Available online: https://www.equivital.com/products/eq02-lifemonitor (accessed on 28 January 2021).
- Barrios, L.; Oldrati, P.; Santini, S.; Lutterotti, A. Evaluating the accuracy of heart rate sensors based on photoplethysmography for in-the-wild analysis. In Proceedings of the 13th EAI International Conference on Pervasive Computing Technologies for Healthcare, Trento, Italy, 20–23 May 2019; pp. 251–261. [Google Scholar]
- McCarthy, C.; Pradhan, N.; Redpath, C.; Adler, A. Validation of the Empatica E4 wristband. In Proceedings of the IEEE EMBS International Student Conference, Ottawa, ON, Canada, 29–31 May 2016; pp. 1–4. [Google Scholar]
- Pietilä, J.; Mehrang, S.; Tolonen, J.; Helander, E.; Jimison, H.; Pavel, M.; Korhonen, I. Evaluation of the accuracy and reliability for photoplethysmography based heart rate and beat-to-beat detection during daily activities. In Proceedings of the 37th Annual International Conference IEEE Engineering Medicine Biology Society, Milano, Italy, 25–29 August 2015; pp. 145–148. [Google Scholar] [CrossRef]
- Speer, K.E.; Semple, S.; Naumovski, N.; McKune, A.J. Measuring heart rate variability using commercially available devices in healthy children: A validity and reliability study. Eur. J. Investig. Health Psychol. Educ. 2020, 10, 390–404. [Google Scholar] [CrossRef]
- Morrin, N.M.; Stone, M.R.; Henderson, K.J. Reproducability of 24-h ambulatory blood pressure and measures of autonomic function. Blood Press. Monit. 2017, 22, 169. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© Crown copyright (2020), Defence Science and Technology Laborato-ry (Dstl). This materialis licensed under the terms of the Open Gov-ernment Licence except where otherwise stated.To view this li-cence, visit: http://www.nationalarchives.gov.uk/doc/open-government-licence/version/3).