Evaluation of Internal Fit and Marginal Adaptation of Provisional Crowns Fabricated with Three Different Techniques
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
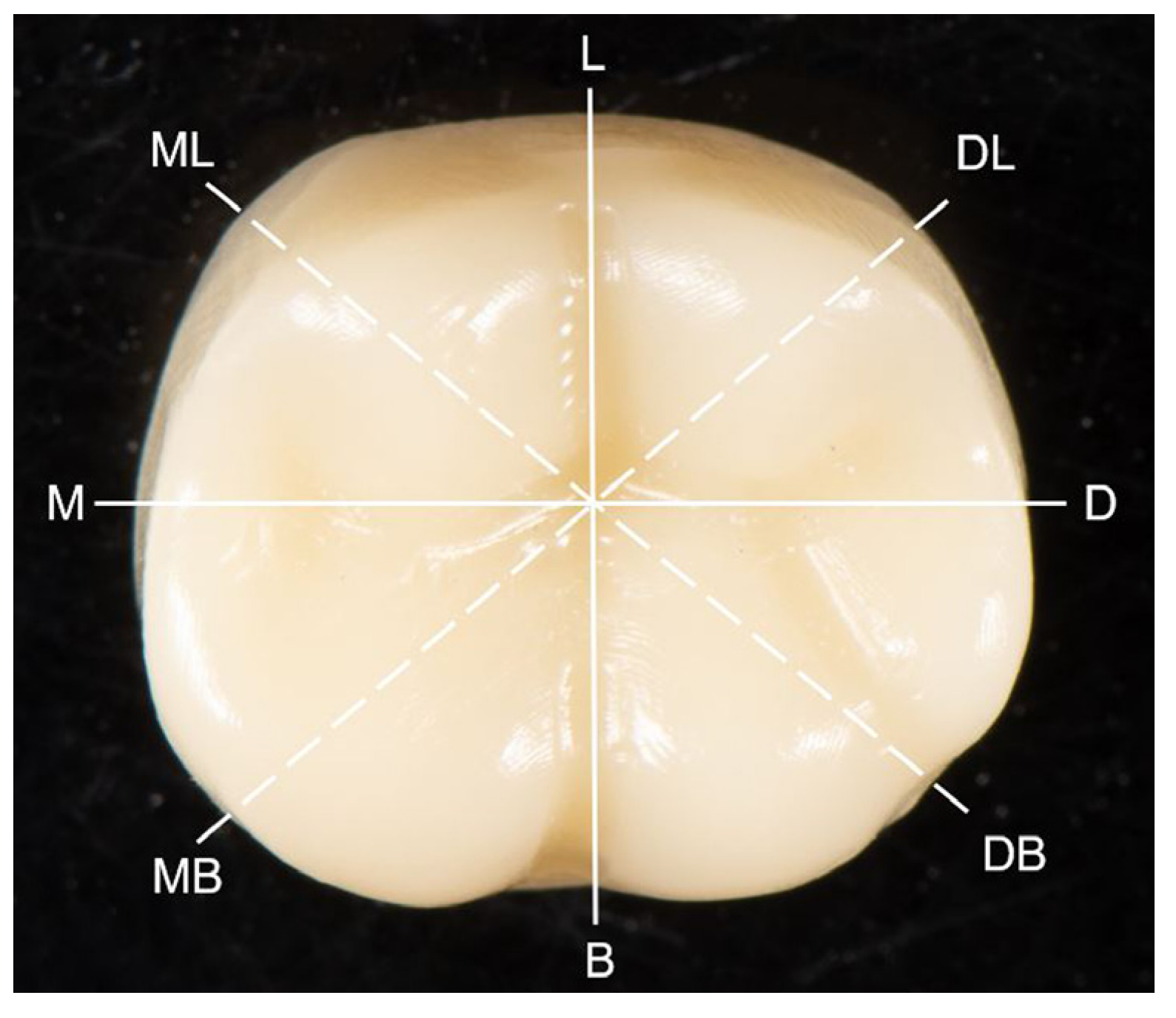
2.2. Measurement of Internal Fit
2.3. Measurement of Marginal Discrepancy
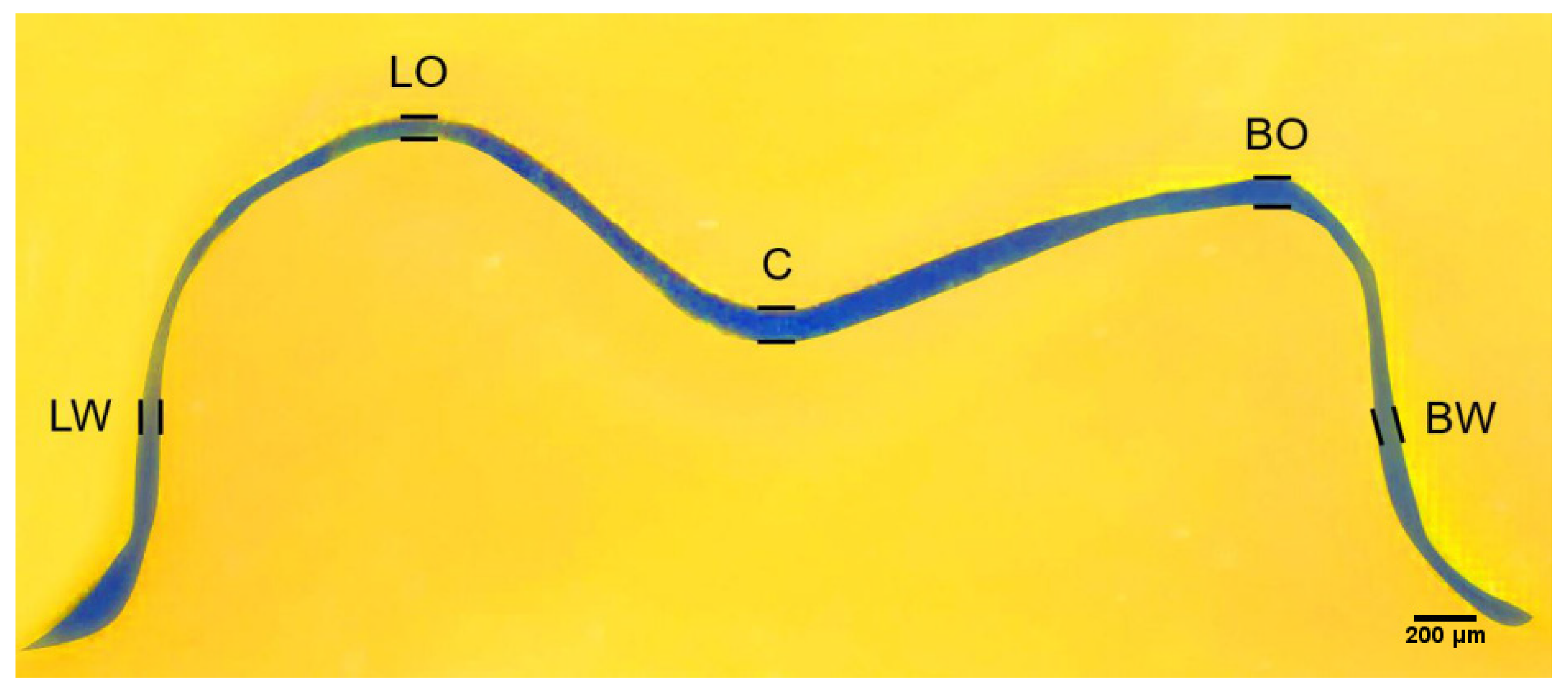
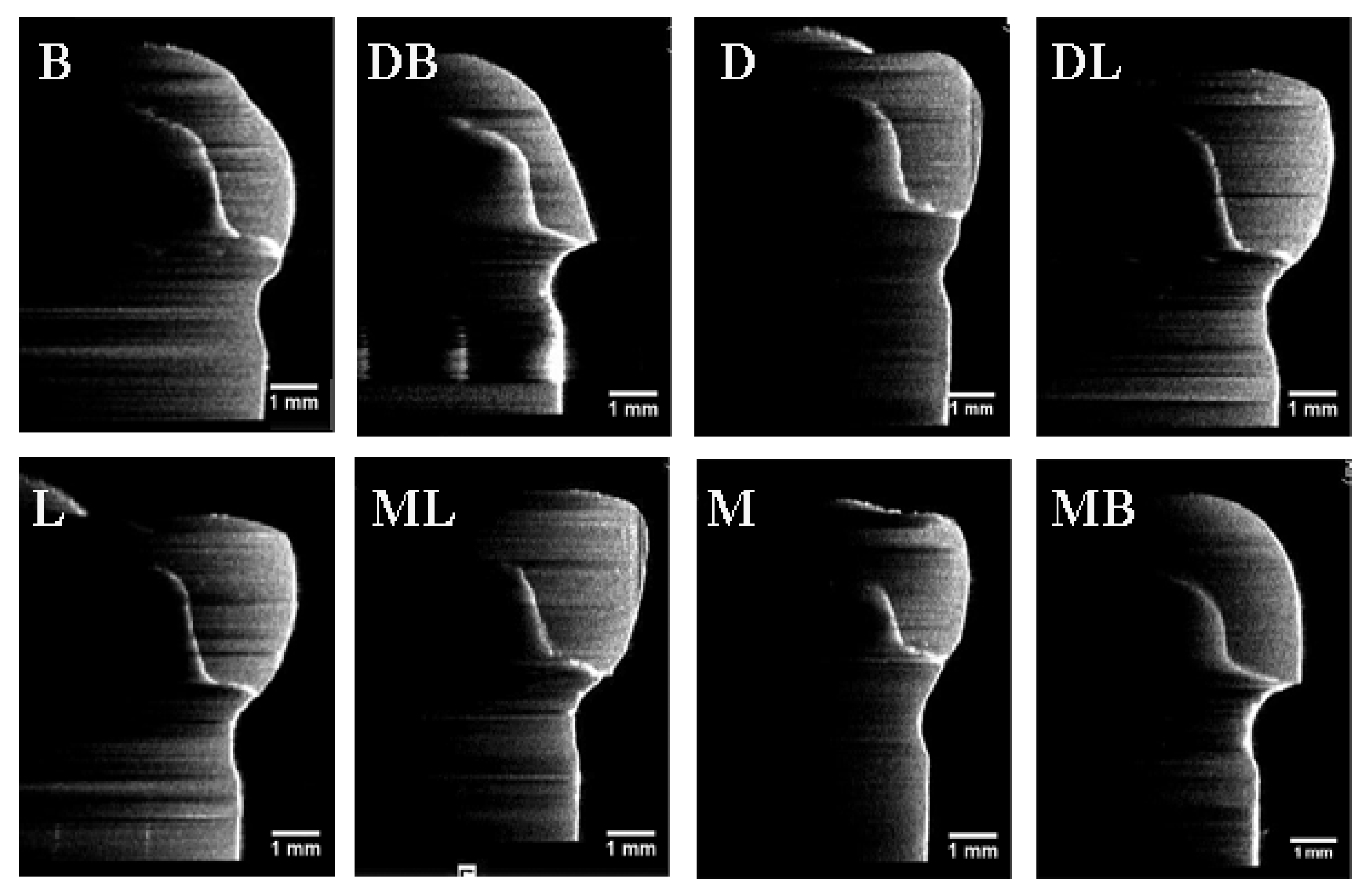
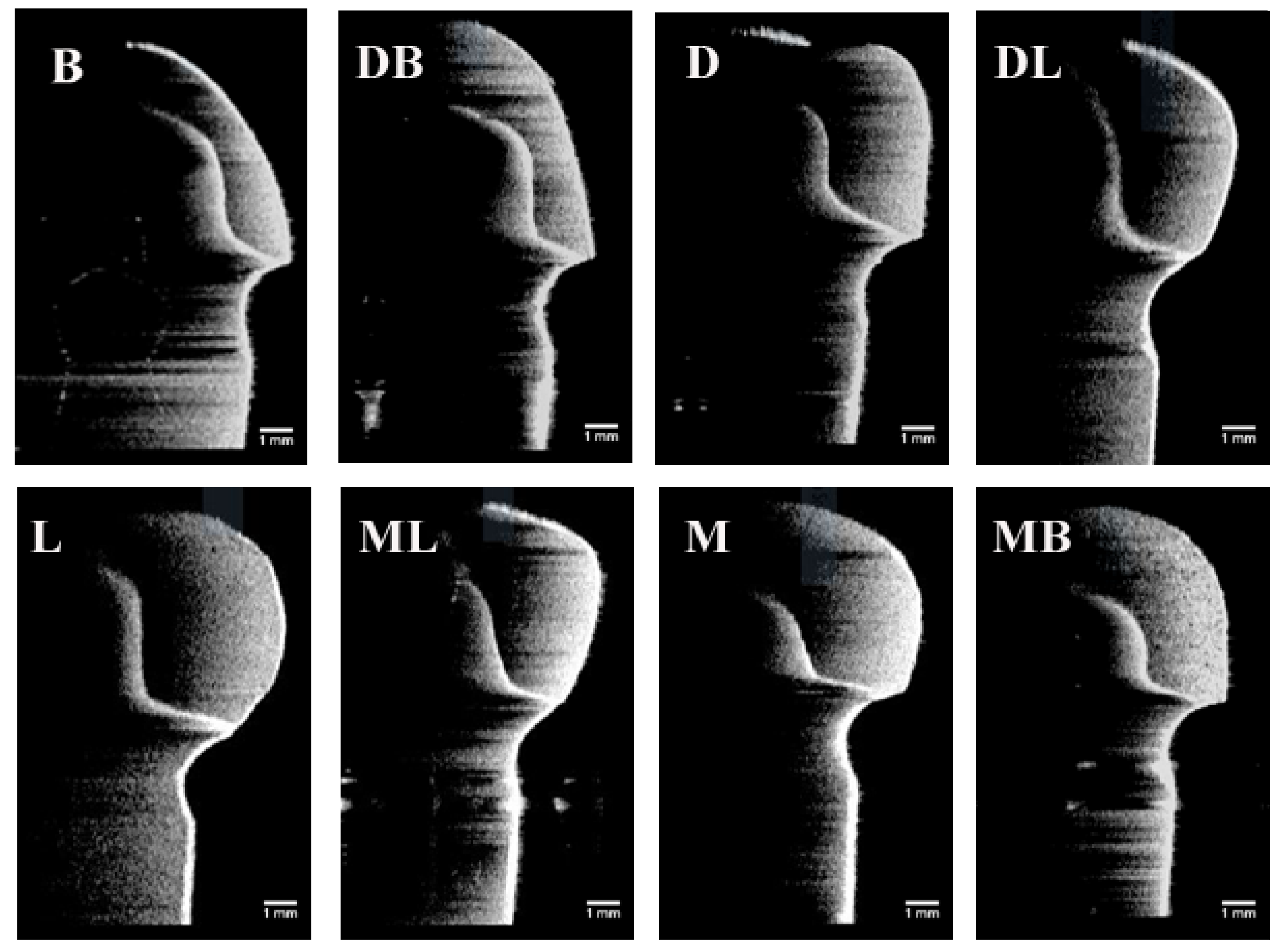
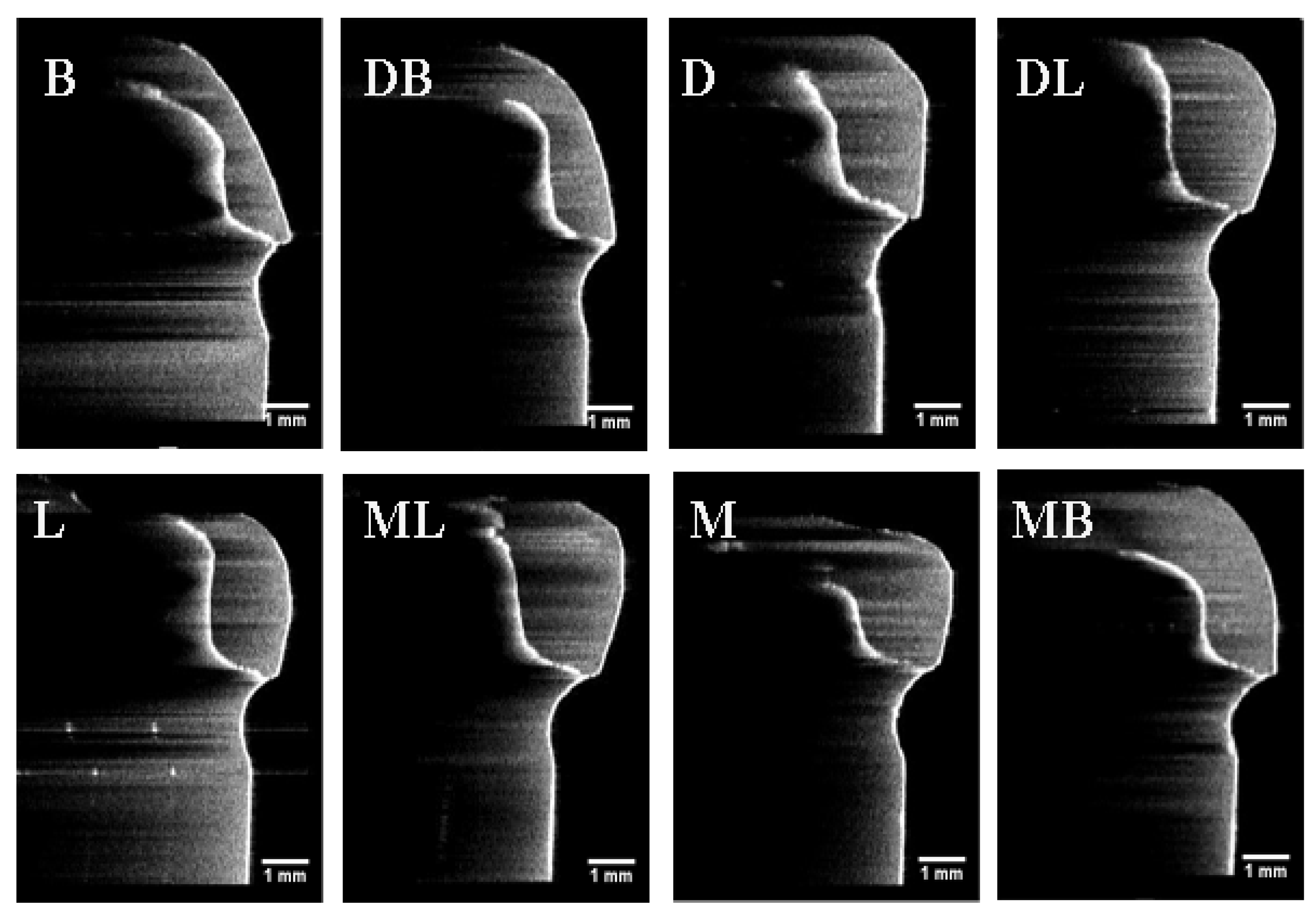
2.3.1. PVS-Replica Method
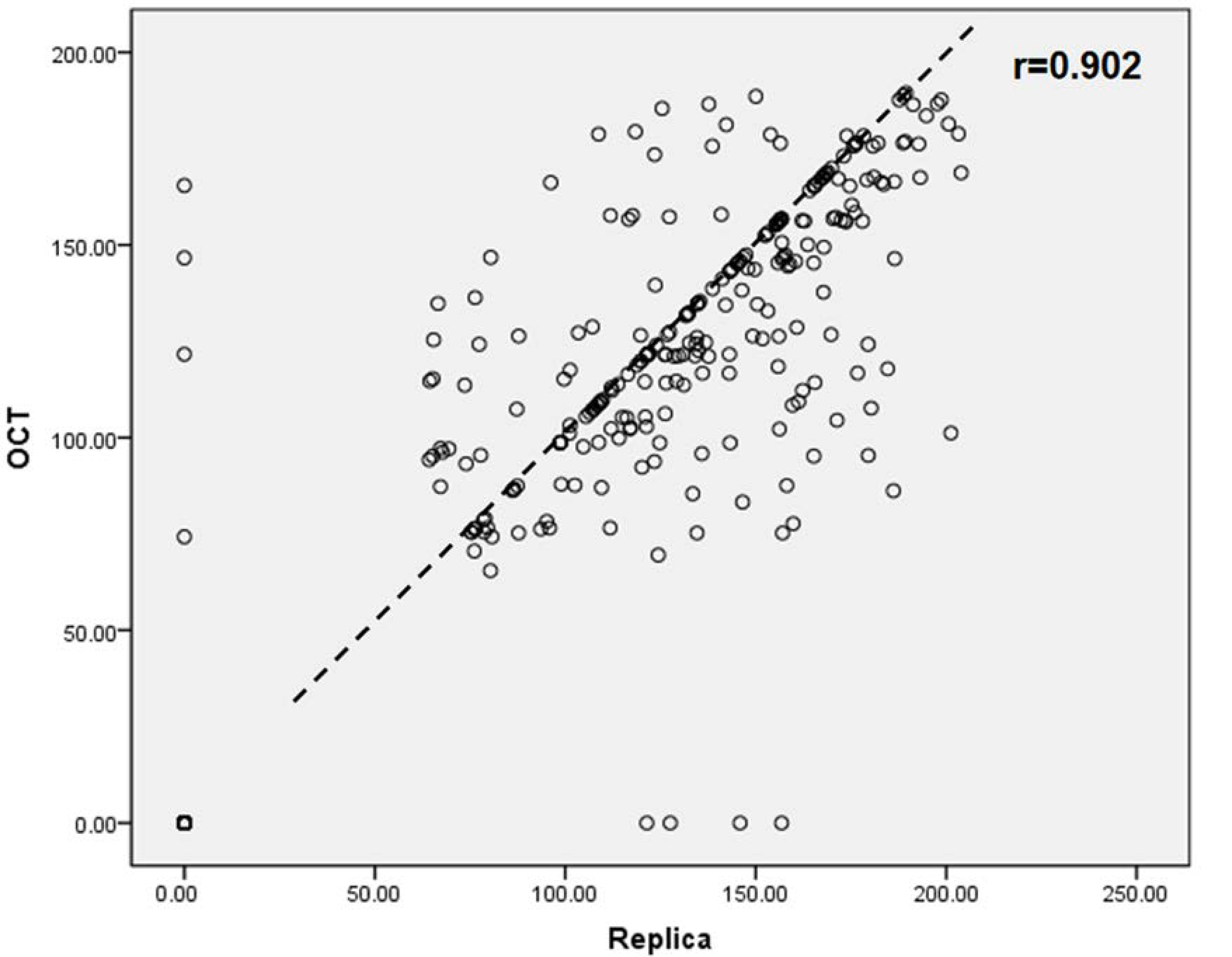
2.3.2. OCT Scanning Technique
2.4. Statistical Analysis
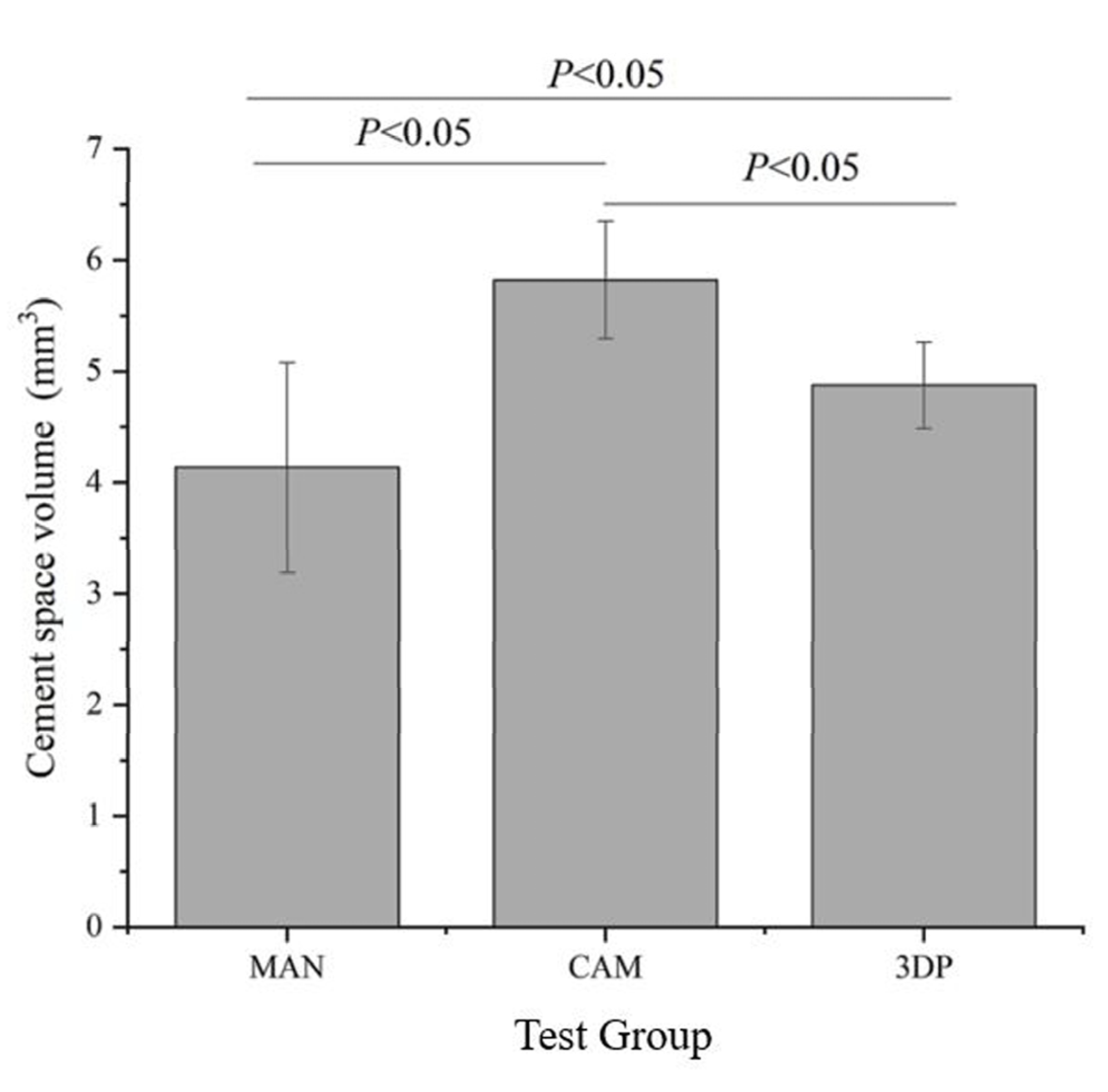
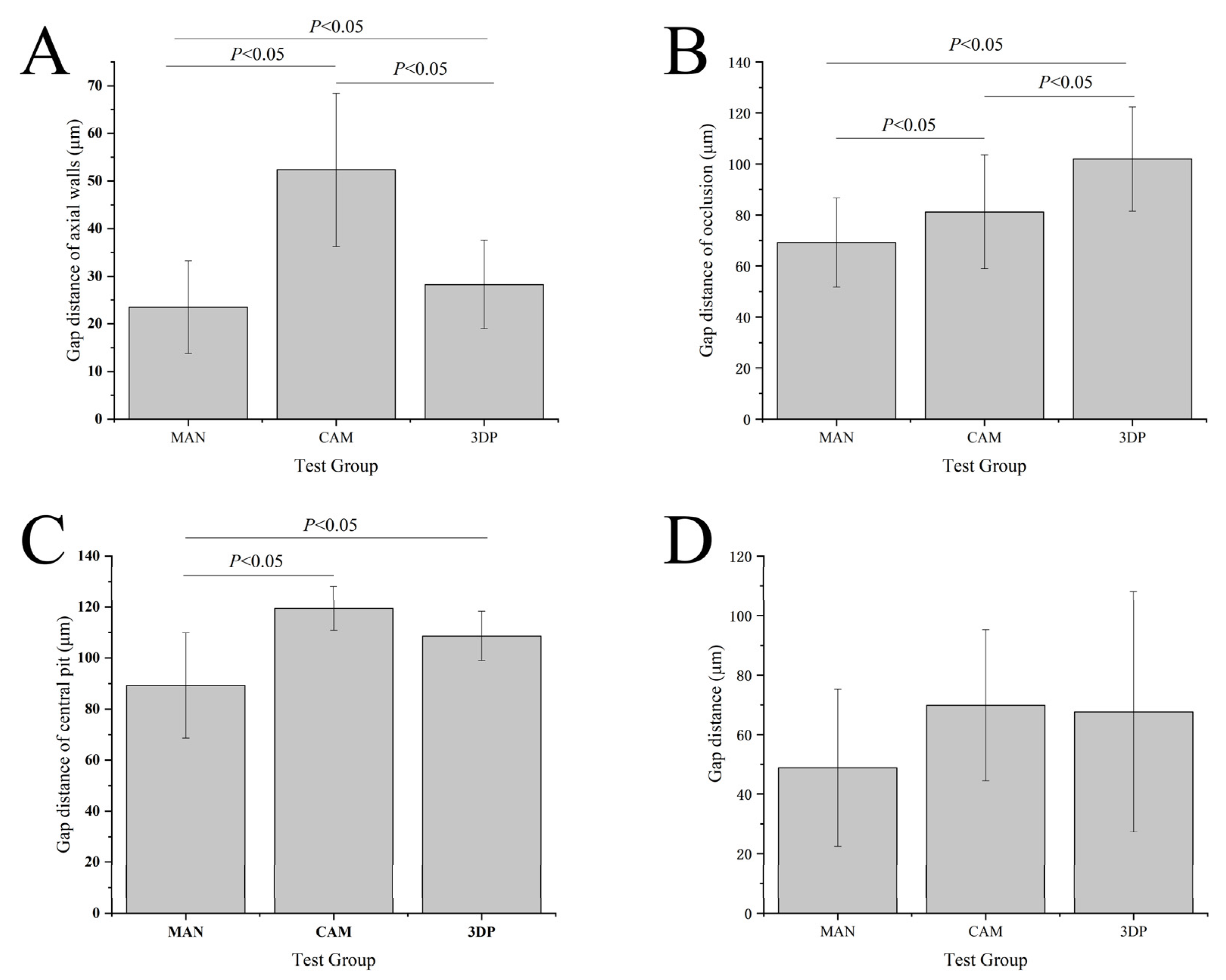
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Burns, D.R.; Beck, A.D.; Nelson, S.K. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: Report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J. Prosthet. Dent. 2003, 90, 474–497. [Google Scholar] [CrossRef]
- Lodding, D.W. Long-term esthetic provisional restorations in dentistry. Curr. Opin. Cosmet. Dent. 1997, 4, 16–21. [Google Scholar] [PubMed]
- Sakrana, A.A. In vitro evaluation of the marginal and internal discrepancies of different esthetic restorations. J. Appl. Oral Sci. 2013, 21, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Kokubo, Y.; Ohkubo, C.; Tsumita, M.; Miyashita, A.; Von Steyern, P.V.; Fukushima, S. Clinical marginal and internal gaps of Procera AllCeram crowns. J. Oral Rehabil. 2005, 32, 526–530. [Google Scholar] [CrossRef]
- Abduo, J.; Lyons, K.; Swain, M. Fit of zirconia fixed partial denture: A systematic review. J. Oral Rehabil. 2010, 37, 866–876. [Google Scholar] [CrossRef]
- Baig, M.R.; Tan, K.B.-C.; Nicholls, J.I. Evaluation of the marginal fit of a zirconia ceramic computer-aided machined (CAM) crown system. J. Prosthet. Dent. 2010, 104, 216–227. [Google Scholar] [CrossRef]
- Nakamura, T.; Nonaka, M.; Maruyama, T. In vitro fitting accuracy of copy-milled alumina cores and all-ceramic crowns. Int. J. Prosthodont. 2001, 13, 189–193. [Google Scholar]
- Martins, L.M.; Lorenzoni, F.C.; de Melo, A.O.; da Silva, L.M.; de Oliveira, J.L.G.; de Oliveira, P.C.G.; Bonfante, G. Internal fit of two all-ceramic systems and metal-ceramic crowns. J. Appl. Oral Sci. 2012, 20, 235–240. [Google Scholar] [CrossRef]
- Goldman, M.; Laosonthorn, P.; White, R.R. Microleakage—Full crowns and the dental pulp. J. Endod. 1992, 18, 473–475. [Google Scholar] [CrossRef]
- Valderhaugw, J.; Birkeland, J. Periodontal conditions in patients 5 years following insertion of fixed prostheses. J. Oral Rehabilit. 1976, 3, 237–243. [Google Scholar] [CrossRef]
- Gratton, D.G.; Aquilino, S.A. Interim restorations. Dent. Clin. N. Am. 2004, 48, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Mai, H.-N.; Lee, K.-B.; Lee, D.-H. Fit of interim crowns fabricated using photopolymer-jetting 3D printing. J. Prosthet. Dent. 2017, 118, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Regish, K.M.; Sharma, D.; Prithviraj, D.R. Techniques of Fabrication of Provisional Restoration: An Overview. Int. J. Dent. 2011, 2011, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Shillingburg, H.T., Jr.; Sather, D.A.; Wilson, E.L., Jr.; Cain, J.R.; Mitchell, D.L.; Blanco, L.J.; Kesser, J.C. Fundamentals of Fixed Prosthodontics, 4th ed.; Quintessence Publishing: Chicago, IL, USA, 2012; pp. 241–268. [Google Scholar]
- Michalakis, K.X.; Pissiotis, A.; Hirayama, H.; Kang, K.; Kafantaris, N. Comparison of temperature increase in the pulp chamber during the polymerization of materials used for the direct fabrication of provisional restorations. J. Prosthet. Dent. 2006, 96, 418–423. [Google Scholar] [CrossRef]
- Kim, S.; Watts, D. Polymerization shrinkage-strain kinetics of temporary crown and bridge materials. Dent. Mater. 2004, 20, 88–95. [Google Scholar] [CrossRef]
- Monday, J.; Blais, D. Marginal adaptation of provisional acrylic resin crowns. J. Prosthet. Dent. 1985, 54, 194–197. [Google Scholar] [CrossRef]
- Schwantz, J.K.; Oliveira-Ogliari, A.; Meereis, C.T.W.; Leal, F.B.; Ogliari, F.A.; Moraes, R.R. Characterization of Bis-Acryl Composite Resins for Provisional Restorations. Braz. Dent. J. 2017, 28, 354–361. [Google Scholar] [CrossRef]
- Van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Ng, J.; Ruse, D.; Wyatt, C. A comparison of the marginal fit of crowns fabricated with digital and conventional methods. J. Prosthet. Dent. 2014, 112, 555–560. [Google Scholar] [CrossRef]
- Ishida, Y.; Miyasaka, T. Dimensional accuracy of dental casting patterns created by 3D printers. Dent. Mater. J. 2016, 35, 250–256. [Google Scholar] [CrossRef]
- Koch, G.K.; Gallucci, G.O.; Lee, S.J. Accuracy in the digital workflow: From data acquisition to the digitally milled cast. J. Prosthet. Dent. 2016, 115, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage Provisional dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- Hoang, L.N.; Thompson, G.A.; Cho, S.-H.; Berzins, D.W.; Ahn, K.W. Die spacer thickness reproduction for central incisor crown fabrication with combined computer-aided design and 3D printing technology: An in vitro study. J. Prosthet. Dent. 2015, 113, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Beuer, F.; Naumann, M.; Gernet, W.; Sorensen, J.A. Precision of fit: Zirconia three-unit fixed dental prostheses. Clin. Oral Investig. 2008, 13, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Miranda, P.; Kim, D.K.; Lawn, B.R. Effect of an adhesive interlayer on the fracture of a brittle coating on a supporting substrate. J. Mater. Res. 2003, 18, 222–227. [Google Scholar] [CrossRef]
- Peng, C.-C.; Chung, K.-H.; Ramos, V., Jr. Assessment of the adaptation of interim crowns using different measurement technique. J. Prosthodont. 2020, 29, 87–93. [Google Scholar] [CrossRef]
- Peng, C.-C.; Chung, K.-H.; Yau, H.-T.; Ramos, V., Jr. Assessment of the internal fit and marginal integrity of Provisional crowns made by different manufacturing methods. J. Prosthet. Dent. 2020, 123, 514–522. [Google Scholar] [CrossRef]
- Luong, M.N.; Shimada, Y.; Araki, K.; Yoshiyama, M.; Tagami, J.; Sadr, A. Diagnosis of Occlusal Caries with Dynamic Slicing of 3D Optical Coherence Tomography Images. Sensors 2020, 20, 1659. [Google Scholar] [CrossRef]
- Kakizaki, S.; Aoki, A.; Tsubokawa, M.; Lin, T.; Mizutani, K.; Koshy, G.; Sadr, A.; Oda, S.; Sumi, Y.; Izumi, Y. Observation and determination of periodontal tissue profile using optical coherence tomography. J. Periodontal Res. 2017, 53, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Al-Imam, H.; Michou, S.; Benetti, A.R.; Gotfredsen, K. Evaluation of marginal and internal fit of acrylic bridges using optical coherence tomography. J. Oral Rehabil. 2018, 46, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Bakhsh, T. Optical comparison between micro-CT and OCT in imaging of marginal composite adaptation; Observational study. J. Microsc. 2020. [Google Scholar] [CrossRef]
- Holmes, J.R.; Bayne, S.C.; Holland, G.A.; Sulik, W.D. Considerations in measurement of marginal fit. J. Prosthet. Dent. 1989, 62, 405–408. [Google Scholar] [CrossRef]
- Huang, Z.; Zhang, L.; Zhu, J.; Zhao, Y.; Zhang, X. Clinical Marginal and Internal Fit of Crowns Fabricated Using Different CAD/CAM Technologies. J. Prosthodont. 2015, 24, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Brawek, P.K.; Wolfart, S.; Endres, L.; Kirsten, A.; Reich, S. The clinical accuracy of single crowns exclusively fabricated by digital workflow—the comparison of two systems. Clin. Oral Investig. 2013, 17, 2119–2125. [Google Scholar] [CrossRef]
- Lee, W.-S.; Lee, D.-H.; Lee, K.-B. Evaluation of internal fit of provisional crown fabricated with CAD/CAM milling and 3D printing system. J. Adv. Prosthodont. 2017, 9, 265–270. [Google Scholar] [CrossRef] [PubMed]
- McLean, J.W.; Von Fraunhofer, J.A. The estimation of cement film thickness by an in vivo technique. Br. Dent. J. 1971, 131, 107–111. [Google Scholar] [CrossRef]
- Boening, K.W.; Wolf, B.H.; Schmidt, A.E.; Kästner, K.; Walter, M.H. Clinical fit of Procera AllCeram crowns. J. Prosthet. Dent. 2000, 84, 419–424. [Google Scholar] [CrossRef]
- Brain, M.; Jimbo, R.; Wennenberg, A. Production tolerance of additive manufactured polymeric objects for clinical applications. Dent. Mater. 2016, 32, 853–861. [Google Scholar] [CrossRef]
- Katheng, A.; Kanazawa, M.; Iwaki, M.; Minakuchi, S. Evaluation of dimensional accuracy and degree of polymerization of stereolithography photopolymer resin under different postpolymerization conditions: An in vitro study. J. Prosthet. Dent. 2020. [Google Scholar] [CrossRef]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef]
- Lang, N.P.; Kiel, R.A.; Anderhalden, K. Clinical and microbiological effects of subgingival restorations with overhanging or clinically perfect margins. J. Clin. Periodontol. 1983, 10, 563–578. [Google Scholar] [CrossRef] [PubMed]
- Brunsvold, M.A.; Lane, J.J. The prevalence of overhanging dental restorations and their relationship to periodontal disease. J. Clin. Periodontal. 1990, 17, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Nawafleh, N.A.; Mack, F.; Evans, J.; Mackay, J.; Hatamleh, M.M. Accuracy and Reliability of Methods to Measure Marginal Adaptation of Crowns and FDPs: A Literature Review. J. Prosthodont. 2013, 22, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Al Hamad, K.Q.; Al Rashdan, B.A.; Al Omari, W.M.; Baba, N.Z. Comparison of the Fit of Lithium Disilicate Crowns made from Conventional, Digital, or Conventional/Digital Techniques. J. Prosthodont. 2018, 28, e580–e586. [Google Scholar] [CrossRef]
- Turani, Z.; Fatemizadeh, E.; Blumetti, T.; Daveluy, S.; Moraes, A.; Chen, W.; Mehregan, D.; Andersen, P.A.; Avanaki, K. Optical Radiomic Signatures Derived from Optical Coherence Tomography Images Improve Identification of Melanoma. Cancer Res. 2019, 79, 2021–2030. [Google Scholar] [CrossRef]
- Sumitani, Y.; Hamba, H.; Nakamura, K.; Sadr, A.; Nikaido, T.; Tagami, J. Micro-CT assessment of comparative radiopacity of adhesive/composite materials in a cylindrical cavity. Dent. Mater. J. 2018, 37, 634–641. [Google Scholar] [CrossRef]
| Material | Code | Fabricating Method | Manufacturer | Batch no. |
|---|---|---|---|---|
| LuxaCrown | MAN | Manual | DMG, Hamburg, Germany | 788811 |
| Lava Ultimate | CAM | CAD/CAM Technology | 3M ESPE, St. Paul, MN, USA | 2914B1-LT/14L |
| Dima Print Denture Teeth | 3DP | CAD/3D Printing | Kulzer North America South Bend, IN, USA | AC18124A2 |
| Fit Checker Advanced Blue | Automix | GC Corp., Tokyo, Japan | 1512021 | |
| Aquasil Ultra XLV | Automix | Dentsply Sirona, Charlotte, NC, USA | 170524 |
| Marginal Discrepancy (μm) | B Mean ± SD | DB Mean ± SD | D Mean ± SD | DL Mean ± SD | L Mean ± SD | ML Mean ± SD | M Mean ± SD | MB Mean ± SD | Total Mean ± SD |
|---|---|---|---|---|---|---|---|---|---|
| Polyvinyl siloxane-replica method | |||||||||
| MAN | 91.3 ± 64.1 | 65.6 ± 65.9 | 59.9 ± 50.2 | 90.0 ± 76.5 | 84.3 ± 70.8 | 38.9 ± 54.7 | 48.8 ± 54.9 | 91.7 ± 67.7 | 71.3 ± 64.9 a,b |
| CAM | 127.4 ± 33.9 | 134.7 ± 46.4 | 120.8 ± 44.2 | 69.7 ± 57.3 | 64.1 ± 76.3 | 65.9 ± 56.6 | 93.3 ± 60.9 | 109.8 ± 53.0 | 96.9 ± 60.2 b |
| 3DP | 129.9 ± 68.4 | 143.1 ± 45.6 | 151.5 ± 49.4 | 129.3 ± 78.5 | 123.1 ± 75.2 | 95.6 ± 80.3 | 78.4 ± 74.7 | 115.9 ± 71. 7 | 120.8 ± 70.9 c |
| Optical coherence tomographic scanning technique | |||||||||
| MAN | 110.4 ± 58.9 | 73.7 ± 67.9 | 97.0 ± 59.2 | 98.3 ± 71.1 | 52.8 ± 55.7 | 48.6 ± 65.7 | 77.8 ± 66.1 | 102.8 ± 64.7 | 82.7 ± 65.8 a,b |
| CAM | 111.6 ± 28.7 | 144.5 ± 30.2 | 130.4 ± 30.4 | 83.6 ± 70.5 | 30.3 ± 56.7 | 91.8 ± 44.5 | 100.0 ± 53.0 | 104.9 ± 28.9 | 99.6 ± 54.6 b |
| 3DP | 145.5 ± 37.4 | 147.3 ± 32.2 | 149.1 ± 44.1 | 158.0 ± 35.7 | 127.4 ± 47.5 | 148.2 ± 29.6 | 137.2 ± 47.5 | 132.4 ± 40.1 | 143.1 ± 39.9 c |
| Marginal Discrepancy (µm) | B Mean ± SD | DB Mean ± SD | D Mean ± SD | DL Mean ± SD | L Mean ± SD | ML Mean ± SD | M Mean ± SD | MB Mean ± SD | Total Mean ± SD |
|---|---|---|---|---|---|---|---|---|---|
| Polyvinyl siloxane-replica method | |||||||||
| MAN | 83.7 ± 55.5 | 62.2 ± 58.6 | 55.7 ± 48.0 | 68.6 ± 55.7 | 79.7 ± 67.1 | 33.0 ± 44.4 | 54.4 ± 52.5 | 69.00 ± 52.7 | 63.3 ± 55.2 a |
| CAM | 118.5 ± 27.9 | 136.4 ± 42.5 | 128.3 ± 42.4 | 69.7 ± 57.3 | 56.8 ± 76.6 | 59.2 ± 54.9 | 94.5 ± 61.0 | 95.1 ± 53.1 | 94.8 ± 59.8 b |
| 3DP | 116.1 ± 72. 5 | 139.3 ± 45.1 | 148.8 ± 47.7 | 127.9 ± 64.7 | 116.9 ± 72.6 | 94.5 ± 69.7 | 86.6 ± 81.6 | 117.7 ± 72.3 | 118.7 ± 67.7 c |
| Optical coherence tomographic scanning technique | |||||||||
| MAN | 93.3 ± 54.2 | 65.7 ± 61.9 | 94.0 ± 51.5 | 82.6 ± 61.1 | 57.1 ± 64.1 | 45.5 ± 61.2 | 67.0 ± 66.2 | 76.1 ± 49.2 | 72.7 ± 59.5 a |
| CAM | 115.6 ± 28.0 | 132.3 ± 36.2 | 128.5 ± 30.4 | 82.3 ± 69.8 | 33.8 ± 63.8 | 71.7 ± 44.1 | 101.6 ± 46.6 | 110.1 ± 27.6 | 97.0 ± 54.3 b |
| 3DP | 152.4 ± 27.3 | 140.6 ± 28.0 | 149.8 ± 40.7 | 152.7 ± 24.0 | 145.7 ± 45.5 | 150.0 ± 29.9 | 139.1 ± 50.0 | 140.6 ± 43.2 | 146.4 ± 36.6 c |
| Marginal Discrepancy (µm) | B Mean ± SD | DB Mean ± SD | D Mean ± SD | DL Mean ± SD | L Mean ± SD | ML Mean ± SD | M Mean ± SD | MB Mean ± SD | Total Mean ± SD |
|---|---|---|---|---|---|---|---|---|---|
| Polyvinyl siloxane-replica method | |||||||||
| MAN | 40.7 ± 45.3 | 28.5 ± 33.0 | 14.8 ± 21.5 | 18.2 ± 26.0 | 15.1 ± 24.5 | 10.5 ± 18.7 | 14.4 ± 23.2 | 21.9 ± 32.0 | 21.5 ± 30.3 a |
| CAM | 6.3 ± 17.9 | 19.1 ± 32.9 | 3.7 ± 14.3 | 0 | 2.3 ± 8.8 | 0 | 7.2 ± 19.9 | 18.7 ± 32.2 | 7.0 ± 20.1 b |
| 3DP | 25.0 ± 26.5 | 8.3 ± 17.9 | 11.0 ± 24.0 | 11.8 ± 25.5 | 9.7 ± 21.1 | 11.1 ± 24.3 | 5.3 ± 14.4 | 23.8 ± 33.2 | 13.3 ± 24.2 b,c |
| Optical coherence tomographic scanning technique | |||||||||
| MAN | 41.4 ± 52.4 | 25.5 ± 42.3 | 22.4 ± 47.0 | 8.4 ± 26.1 | 3.6 ± 14.5 | 0 | 21.5 ± 46.4 | 39.7 ± 55.4 | 20.3 ± 41.5 a |
| CAM | 2.8 ± 11.3 | 18.5 ± 28.8 | 5.7 ± 15.5 | 0 | 2.8 ± 11.1 | 2.8 ± 11.1 | 0 | 2.9 ± 11.4 | 4.5 ± 14.8 b |
| 3DP | 18.8 ± 25.2 | 6.7 ± 18.4 | 3.6 ± 14.5 | 11.5 ± 25.2 | 6.4 ± 17.6 | 3.5 ± 14.2 | 0 | 4.2 ± 16.6 | 6.8 ± 18.4 b,c |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, J.; Xie, H.; Sadr, A.; Chung, K.-H. Evaluation of Internal Fit and Marginal Adaptation of Provisional Crowns Fabricated with Three Different Techniques. Sensors 2021, 21, 740. https://doi.org/10.3390/s21030740
Wu J, Xie H, Sadr A, Chung K-H. Evaluation of Internal Fit and Marginal Adaptation of Provisional Crowns Fabricated with Three Different Techniques. Sensors. 2021; 21(3):740. https://doi.org/10.3390/s21030740
Chicago/Turabian StyleWu, Jie, Hongjun Xie, Alireza Sadr, and Kwok-Hung Chung. 2021. "Evaluation of Internal Fit and Marginal Adaptation of Provisional Crowns Fabricated with Three Different Techniques" Sensors 21, no. 3: 740. https://doi.org/10.3390/s21030740
APA StyleWu, J., Xie, H., Sadr, A., & Chung, K.-H. (2021). Evaluation of Internal Fit and Marginal Adaptation of Provisional Crowns Fabricated with Three Different Techniques. Sensors, 21(3), 740. https://doi.org/10.3390/s21030740







