A CBCT Evaluation of Midpalatal Bone Density in Various Skeletal Patterns
Abstract
:1. Introduction
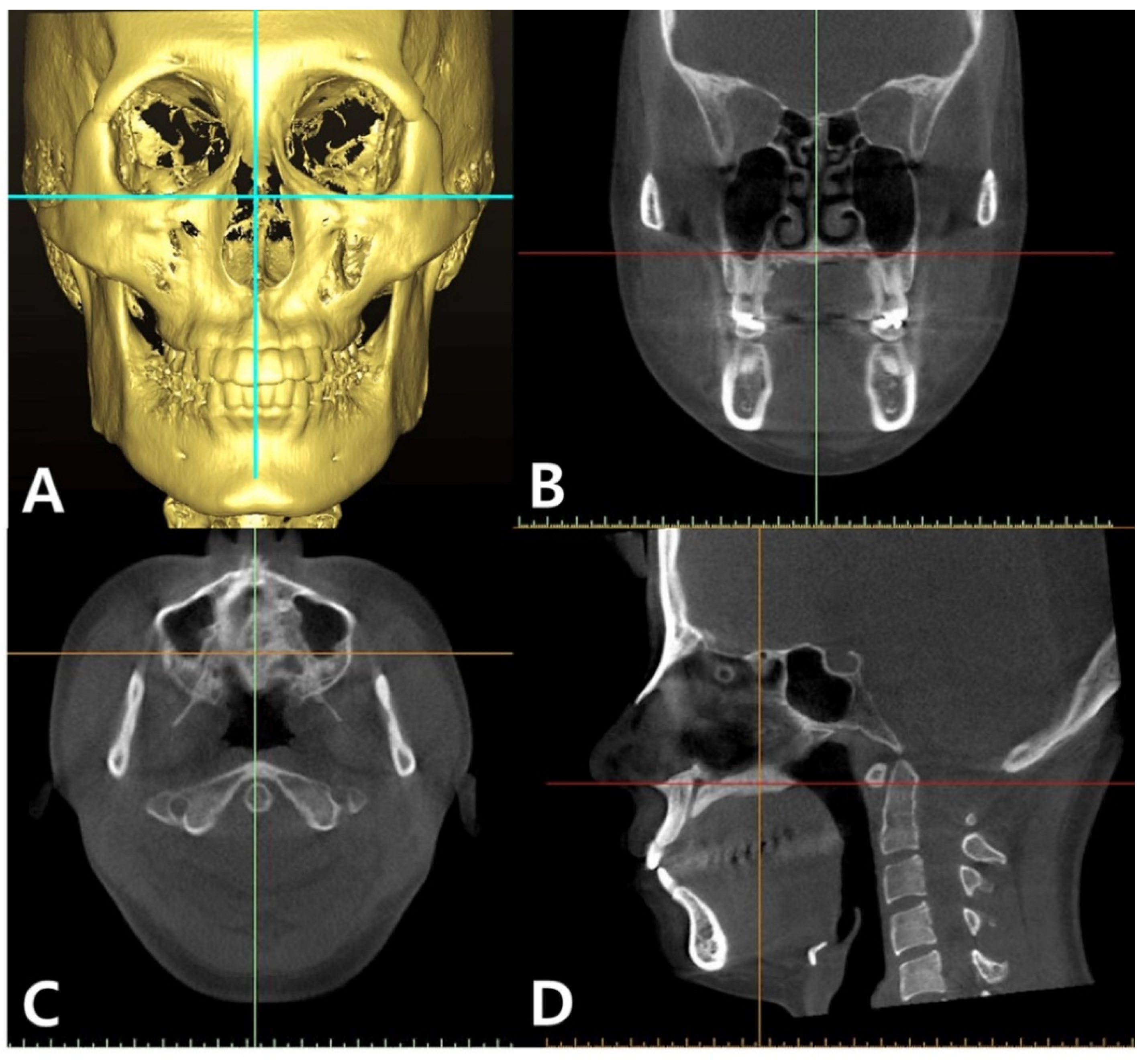
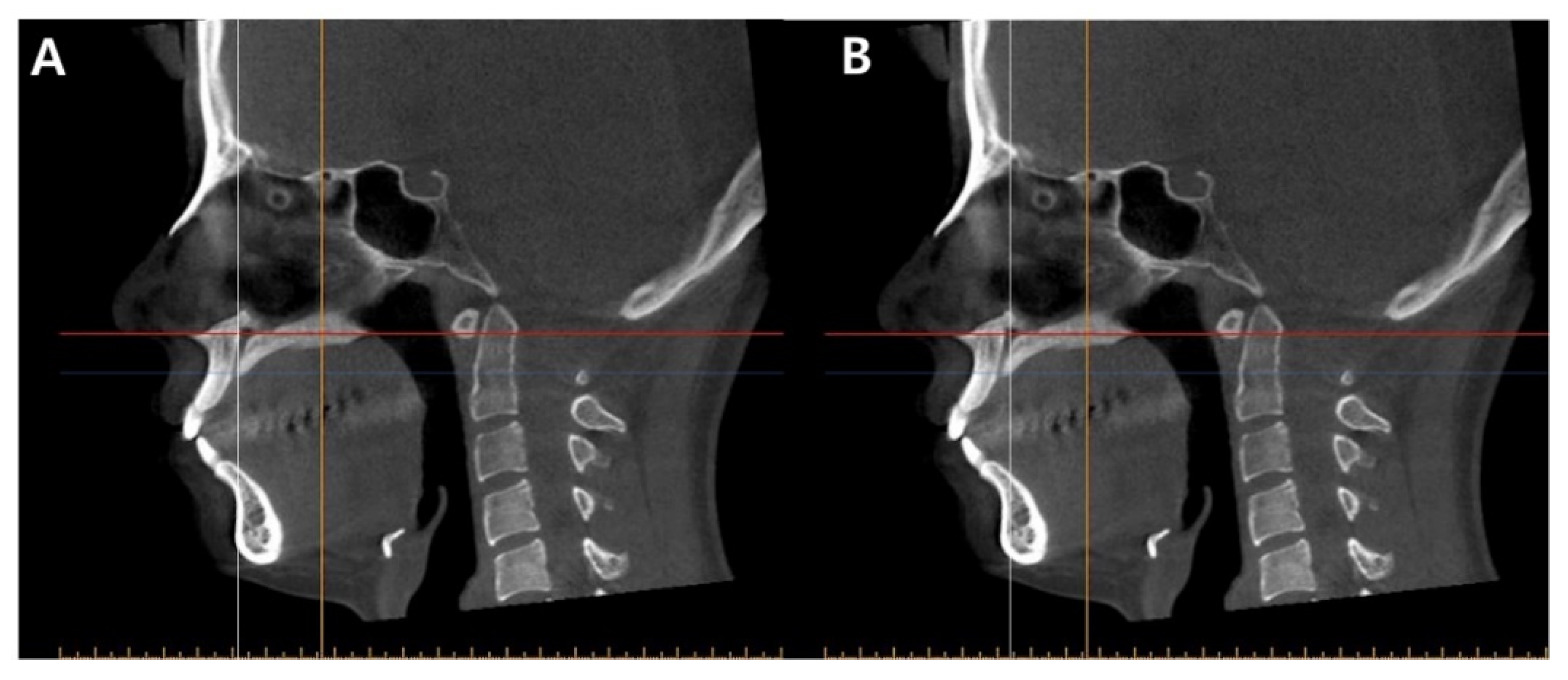
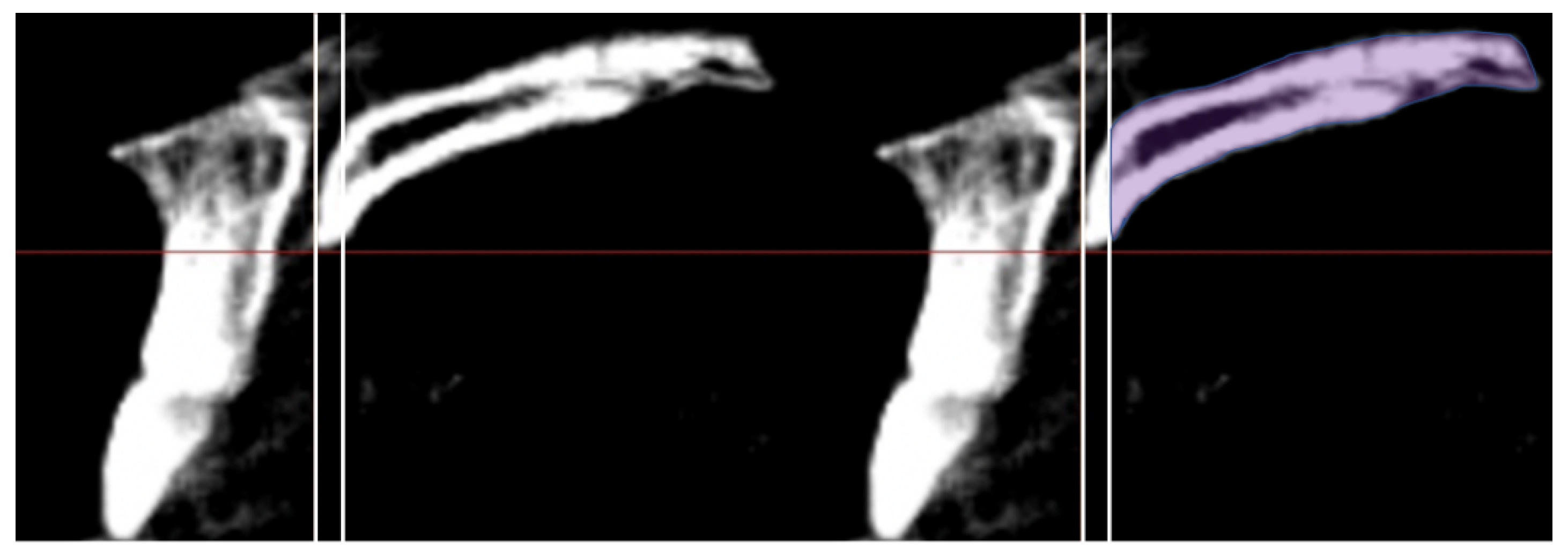
2. Materials and Methods
2.1. Subjects
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- Females showed significantly higher midpalatal BD than their male counterparts.
- Late adolescence individuals showed significantly less BD at the midpalatal suture than did individuals in early adolescence.
- Class II skeletal individuals showed significantly less midpalatal BD than Class III individuals.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Northway, W.M. Surgically assisted rapid maxillary expansion: A comparison of technique, response, and stability. Angle Orthod. 1997, 67, 309–320. [Google Scholar] [PubMed]
- Rungcharassaeng, K.; Caruso, J.M.; Kan, J.Y.K.; Kim, J.; Taylor, G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 428.e1–428.e8. [Google Scholar] [CrossRef] [PubMed]
- Suri, L.; Taneja, P. Surgically assisted rapid palatal expansion: A literature review. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 290–302. [Google Scholar] [CrossRef]
- Baysal, A.; Karadede, I.; Hekimoglu, S.; Ucar, F.; Ozer, T.; Veli, İ.; Uysal, T. TEvaluation of root resorption following rapid maxillary expansion using cone-beam computed tomography. Angle Orthod. 2012, 82, 488–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franchi, L.; Baccetti, T.; Lione, R.; Fanucci, E.; Cozza, P. Modifications of midpalatal sutural density induced by rapid maxillary expansion: A low-dose computed-tomography evaluation. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 486–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aranyarachkul, P.; Caruso, M.S.J.; Gantes, M.S.B.; Schulz, M.S.E. Bone density assessments of dental implant sites: Quantitative cone-beam computerized tomography. Int. J. Oral Maxillofac. Implant. 2005, 20, 416–424. [Google Scholar]
- Bishara, S.E.; Staley, R.N. Maxillary expansion: Clinical Implications. Am. J. Orthod. Dentofac. Orthop. 1987, 91, 3–14. [Google Scholar] [CrossRef]
- Persson, M.; Thilander, B. Palatal suture closure in man from 15 to 35 years of age. Am. J. Orthod. 1977, 72, 42–52. [Google Scholar] [CrossRef]
- Knaup, B.; Yildizhan, F.; Wehrbei, H. Age-related changes in the midpalatal suture. J. Orofac. Orthop. 2004, 65, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Korbmacher, H.; Schilling, A.; Püschel, K.; Amling, M.; Kahl-Nieke, B. Age-dependent three-dimensional microcomputed tomography analysis of the human midpalatal suture. J. Orofac. Orthop. 2007, 68, 364–376. [Google Scholar] [CrossRef] [PubMed]
- Angelieri, F.; Cevidanes, L.H.S.; Franchi, L.; Gonçalves, J.R.; Benavides, E.; McNamara, J.A. Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 759–769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grünheid, T.; Larson, C.E.; Larson, B.E. Midpalatal suture density ratio: A novel predictor of skeletal response to rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Revelo, B.; Fishman, L.S. Maturational evaluation of ossification of the midpalatal suture. Am. J. Orthod. Dentofac. Orthop. 1994, 105, 288–292. [Google Scholar] [CrossRef]
- Fishman, L.S. Radiographic evaluation of skeletal maturation: A clinically oriented method based on hand-wrist films. Angle Orthod. 1982, 2, 88–112. [Google Scholar]
- Baccetti, T.; Franchi, L.; Cameron, C.G.; McNamara, J.A. Treatment timing for rapid maxillary expansion. Angle Orthod. 2001, 71, 343–350. [Google Scholar]
- Wehrbein, H.; Yildizhan, F. The mid-palatal suture in young adults. A radiological-histological investigation. Eur. J. Orthod. 2001, 23, 105–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Angelieri, F.; Franchi, L.; Cevidanes, L.H.S.; McNamara, J.A. Diagnostic performance of skeletal maturity for the assessment of midpalatal suture maturation. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 1010–1016. [Google Scholar] [CrossRef]
- Isfeld, D.; Lagravere, M.; Leon-Salazar, V.; Flores-Mir, C. Novel methodologies and technologies to assess mid-palatal suture maturation: A systematic review. Head Face Med. 2017, 13, 13. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.Y.; Xu, T.M.; Zou, W. Effects of rapid maxillary expansion on the midpalatal suture: A systematic review. Eur. J. Orthod. 2015, 37, 651–655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samra, D.A.; Hadad, R. Midpalatal suture: Evaluation of the morphological maturation stages via bone density. Prog. Orthod. 2018, 19, 1–7. [Google Scholar]
- Pauwels, R.; Jacobs, R.; Singer, S.R.; Mupparapu, M. CBCT-based bone quality assessment: Are hounsfield units applicable? Dentomaxillofacial Radiol. 2015, 44, 20140238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, S.; Bayome, M.; Lee, J.; Lee, Y.J.; Song, H.H.; Kook, Y.A. Evaluation of palatal bone density in adults and adolescents for application of skeletal anchorage devices. Angle Orthod. 2012, 82, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.H.; Park, S.H.; Lim, W.H.; Chun, Y.S. Palatal bone density in adult subjects: Implications for mini-implant placement. Angle Orthod. 2010, 80, 137–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryu, J.H.; Park, J.H.; Vu, T.T.T.; Bayome, M.; Kim, Y.; Kook, Y.A. Palatal bone thickness compared with cone-beam computed tomography in adolescents and adults for mini-implant placement. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Park, J.H.; Bayome, M.; Kim, H.S.; Mo, S.S.; Kook, Y.A. Palatal soft tissue thickness at different ages using an ultrasonic device. J. Clin. Pediatr. Dent. 2012, 36, 403–408. [Google Scholar] [CrossRef] [PubMed]
| Variables | Gender | Age (y) | Mandibular Plane Angle (MPA) | ANB Angle | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | Adolescence | Adult | Hypodivergent | Normover-gent | Hyperdivergent | Class III | Class I | Class II | |||||
| Early | Middle | Late | ||||||||||||
| 10 ≤ y < 14 | 14 ≤ y ≤ 17 | 17 < y ≤ 21 | y > 21 | MPA < 22° | 22° ≤ MPA ≤ 28° | MPA > 28° | ANB < 0° | 0° ≤ ANB ≤ 4° | ANB > 4° | |||||
| Gender | Male | 62 | 13 | 21 | 13 | 15 | 19 | 23 | 20 | 23 | 24 | 15 | ||
| Female | 64 | 18 | 13 | 19 | 14 | 22 | 20 | 22 | 15 | 32 | 17 | |||
| Age | Early | 13 | 18 | 9 | 11 | 11 | 4 | 15 | 12 | |||||
| Adolescence | Middle | 21 | 13 | 11 | 12 | 11 | 7 | 16 | 11 | |||||
| Late | 13 | 19 | 10 | 11 | 11 | 16 | 12 | 4 | ||||||
| Adult | 15 | 14 | 11 | 9 | 9 | 11 | 13 | 5 | ||||||
| MPA | Hypodivergent | 19 | 22 | 9 | 11 | 10 | 11 | 14 | 19 | 8 | ||||
| Normovergent | 23 | 20 | 11 | 12 | 11 | 9 | 15 | 18 | 10 | |||||
| Hyperdivergent | 20 | 22 | 11 | 11 | 11 | 9 | 9 | 19 | 14 | |||||
| ANB | Class III | 23 | 15 | 4 | 7 | 16 | 11 | 14 | 15 | 9 | ||||
| Class I | 24 | 32 | 15 | 16 | 12 | 13 | 19 | 18 | 19 | |||||
| Class II | 15 | 17 | 12 | 11 | 4 | 5 | 8 | 10 | 14 | |||||
| Total (each) | 126 | 31 | 34 | 32 | 29 | 41 | 43 | 42 | 38 | 56 | 32 | |||
| Means (Standard Deviations) | ||||||
|---|---|---|---|---|---|---|
| Variables | Gender | Age (y) | ||||
| Male (n = 62) | Female (n = 64) | Early: 10 ≤ y < 14 (n = 31) | Middle: 14 ≤ y ≤ 17 (n = 34) | Late: 17 < y ≤ 21 (n = 32) | Adult: y > 21 (n = 29) | |
| BD | 549.33 (113.06) | 657.25 (110.93) | 529.05 (96.45) | 561.13 (124.57) | 662.09 (112.58) | 679.90 (96.99) |
| Means (Standard Deviations) | ||||||
|---|---|---|---|---|---|---|
| Variables | Mandibular Plane Angle (MPA) | ANB Angle | ||||
| Hypodivergent MPA < 22° (n = 41) | Normovergent 22° ≤ MPA ≤ 28° (n = 43) | Hyperdivergent MPA > 28° (n = 42) | Class III ANB < 0° (n = 38) | Class I 0° ≤ ANB ≤ 4° (n = 56) | Class II ANB > 4° (n = 32) | |
| BD | 606.93 (105.57) | 586.34 (136.06) | 619.65 (128.25) | 633.82 (117.43) | 613.90 (123.99) | 551.83 (119.10) |
| Variables | Mean BD Difference (HU) | 95% Wald Confidence Interval | p-Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Gender | ||||
| Male vs. Female | −108.75 | −140.25 | −77.25 | <0.001 *** |
| Age | ||||
| Early vs. Middle | −47.35 | −96.48 | 1.80 | 0.062 |
| Early vs. Late | −104.04 | −163.76 | −44.32 | <0.001 *** |
| Early vs. adult | −121.22 | −182.35 | −60.09 | <0.001 *** |
| Middle vs. Late | −56.69 | −110.93 | −2.46 | 0.037 * |
| Middle vs. Adult | −73.87 | −129.97 | −17.78 | 0.004 ** |
| Late vs. Adult | −17.18 | −61.50 | 27.14 | 0.447 |
| Vertical skeletal pattern | ||||
| Hypo vs. Normo | 15.74 | −21.74 | 53.22 | 0.410 |
| Hypo vs. Hyper | −28.14 | −71.63 | 15.35 | 0.294 |
| Normo vs. Hyper | −43.88 | −89.67 | 1.90 | 0.065 |
| Horizontal skeletal pattern | ||||
| Class I vs. Class II | 42.92 | −1.07 | 86.90 | 0.057 |
| Class I vs. Class III | −17.39 | −55.28 | 20.50 | 0.368 |
| Class II vs. Class III | −60.31 | −114.70 | −5.92 | 0.024 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chae, J.-M.; Rogowski, L.; Mandair, S.; Bay, R.C.; Park, J.H. A CBCT Evaluation of Midpalatal Bone Density in Various Skeletal Patterns. Sensors 2021, 21, 7812. https://doi.org/10.3390/s21237812
Chae J-M, Rogowski L, Mandair S, Bay RC, Park JH. A CBCT Evaluation of Midpalatal Bone Density in Various Skeletal Patterns. Sensors. 2021; 21(23):7812. https://doi.org/10.3390/s21237812
Chicago/Turabian StyleChae, Jong-Moon, Leah Rogowski, Suchita Mandair, R. Curtis Bay, and Jae Hyun Park. 2021. "A CBCT Evaluation of Midpalatal Bone Density in Various Skeletal Patterns" Sensors 21, no. 23: 7812. https://doi.org/10.3390/s21237812
APA StyleChae, J.-M., Rogowski, L., Mandair, S., Bay, R. C., & Park, J. H. (2021). A CBCT Evaluation of Midpalatal Bone Density in Various Skeletal Patterns. Sensors, 21(23), 7812. https://doi.org/10.3390/s21237812







