Vital Signal Detection Using Multi-Radar for Reductions in Body Movement Effects
Abstract
:1. Introduction
2. Proposed Configuration Using Multi-Radars
2.1. Physiological Movement of the Heart and Lungs
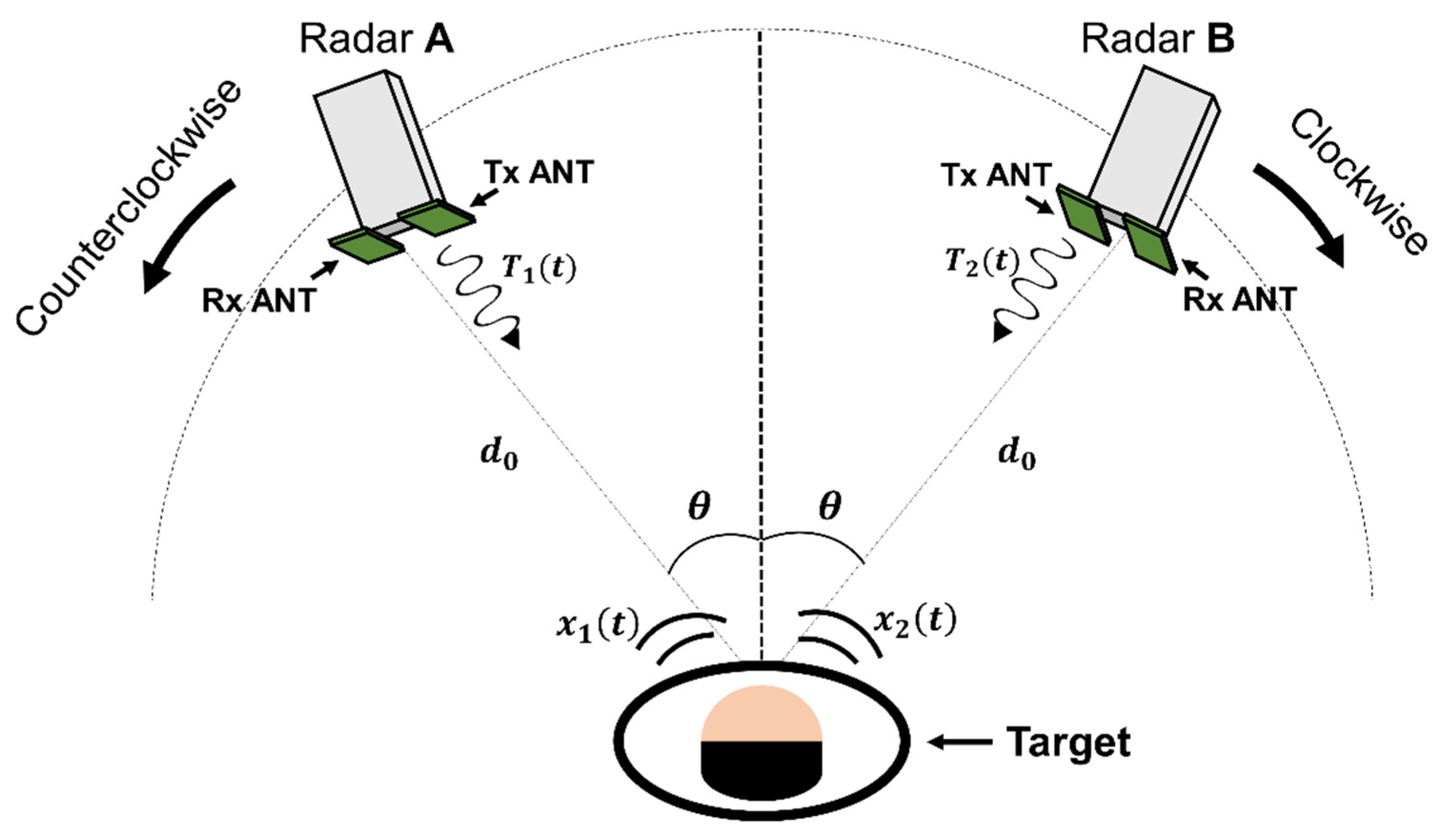
2.2. Proposed Configuration for Vital Signal Detection Using Multiple Radars
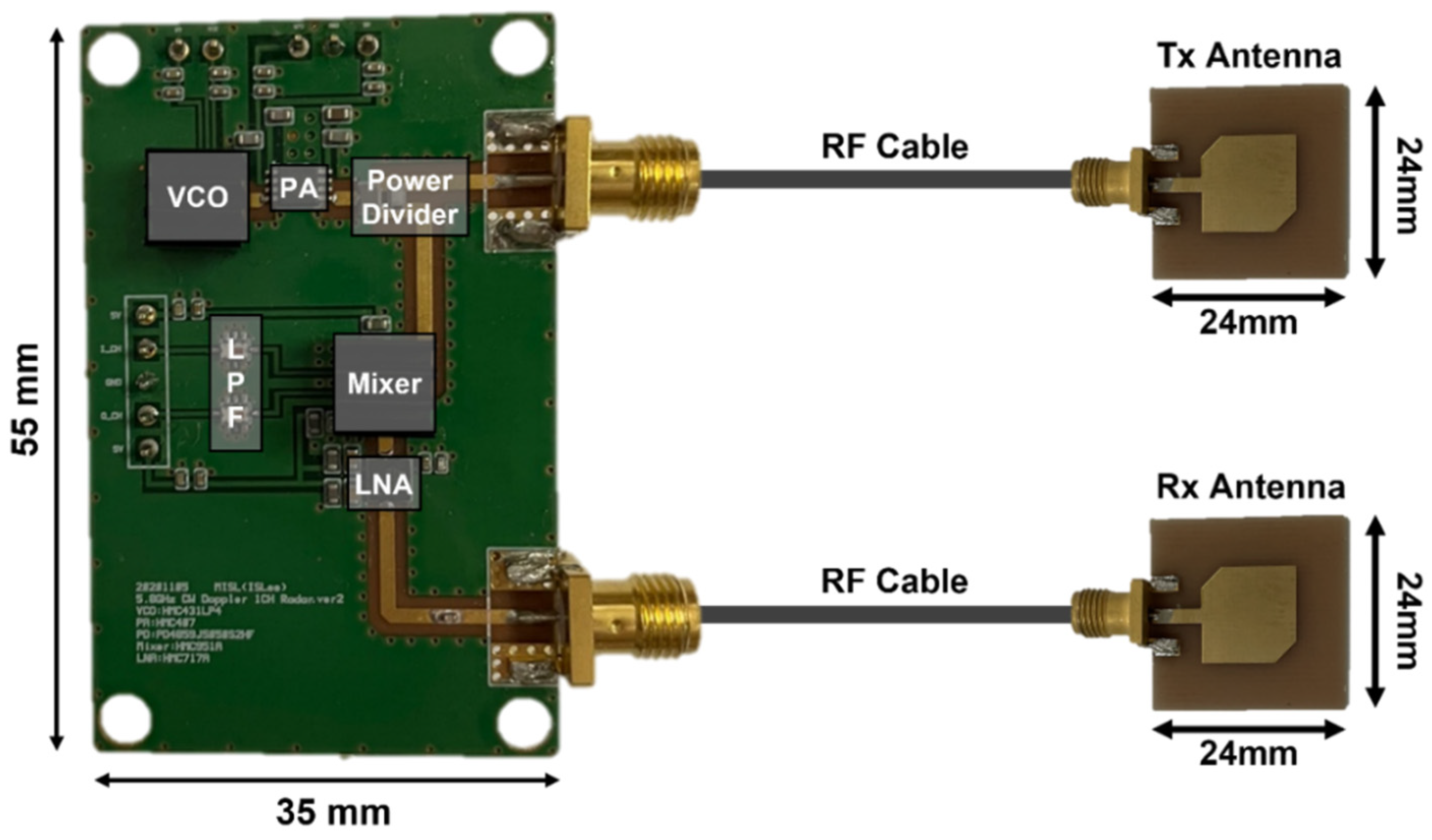
3. Measurement Environment
4. Results and Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baboli, M.; Singh, A.; Soll, B.; Boric-Lubecke, O.; Lubecke, V. Wireless sleep apnea detection using continuous wave quadrature Doppler radar. IEEE Sens. J. 2020, 20, 538–545. [Google Scholar] [CrossRef]
- Castro, I.D.; Mercuri, M.; Patel, A.; Puers, R.; Van Hoof, C.; Torfs, T. Physiological driver monitoring using capacitively coupled and radar sensors. Appl. Sci. 2019, 9, 3994. [Google Scholar] [CrossRef] [Green Version]
- Li, C.; Lubecke, V.; Boric-Lubecke, O.; Lin, J. A review on recent advances in Doppler radar sensors for noncontact healthcare monitoring. IEEE Trans. Microwave Theory Tech. 2013, 61, 2046–2060. [Google Scholar] [CrossRef]
- Kim, J.-Y.; Park, J.-H.; Jang, S.-Y.; Yang, J.-R. Peak detection algorithm for vital sign detection using Doppler radar sensors. Sensors 2019, 19, 1575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sim, J.Y.; Park, J.-H.; Yang, J.-R. Vital-signs detector based on frequency-shift keying radar. Sensors 2020, 20, 5516. [Google Scholar] [CrossRef]
- Droitcour, A.D.; Boric-Lubecke, O. Doppler Radar Physiological Sensing; Wiley: Hoboken, NJ, USA, 2016; pp. 39–68. [Google Scholar]
- Gouveia, C.; Vieira, J.; Pinho, P. A review on methods for random motion detection and compensation in bio-radar systems. Sensors 2019, 19, 604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, C.; Lin, J. Random body movement cancellation in doppler radar vital sign detection. IEEE Trans. Microwave Theory Tech. 2008, 56, 3143–3152. [Google Scholar]
- Yu, X.; Li, C.; Lin, J. Two-dimensional noncontact vital sign detection using Doppler radar array approach. In Proceedings of the 2011 Conference on International Microwave Symposium, Baltimore, MD, USA, 5–10 June 2011. [Google Scholar]
- Li, C.; Xiao, Y.; Lin, J. Experiment and spectral analysis of a low-power Ka-band heartbeat detector measuring from four sides of a human body. IEEE Trans. Microwave Theory Tech. 2006, 54, 4464–4471. [Google Scholar] [CrossRef]
- Tang, M.-C.; Kuo, C.-Y.; Wun, D.-C.; Wang, F.-K.; Horng, T.-S. A self- and mutually injection-locked radar system for monitoring vital signs in real time with random body movement cancellation. IEEE Trans. Microwave Theory Tech. 2016, 64, 4812–4822. [Google Scholar] [CrossRef]
- Wang, F.-K.; Horng, T.; Peng, K.; Jau, J.; Li, J.-Y.; Chen, C. Single-antenna Doppler radars using self and mutual injection locking for vital sign detection with random body movement cancellation. IEEE Trans. Microwave Theory Tech. 2011, 59, 3577–3587. [Google Scholar] [CrossRef]
- Singh, A.; Lubecke, V. Respiratory monitoring and clutter rejection using a CW Doppler radar with passive RF tags. IEEE Sens. J. 2012, 12, 558–565. [Google Scholar] [CrossRef]
- Gu, C.; Wang, G.; Li, Y.; Inoue, T.; Li, C. A hybrid Radar-camera sensing system with phase compensation for random body movement cancellation in Doppler vital sign detection. IEEE Trans. Microwave Theory Tech. 2013, 61, 4678–4688. [Google Scholar] [CrossRef]
- Mostafanezhad, I.; Park, B.-K.; Boric-Lubecke, O.; Lubecke, V.; Host-Madsen, A. Sensor nodes for Doppler radar measurements of life signs. In Proceedings of the IEEE/MTT-S International Microwave Symposium, Honolulu, HI, USA, 3–8 June 2007. [Google Scholar]
- Gu, C.; Wang, G.; Inoue, T.; Li, C. Doppler radar vital sign detection with random body movement cancellation based on adaptive phase compensation. In Proceedings of the IEEE MTT-S International Microwave Symposium, Seattle, WA, USA, 2–7 June 2013. [Google Scholar]
- Lv, Q.; Dong, Y.; Sun, Y.; Li, C.; Ran, L. Detection of bio-signals from body movement based on high-dynamic-range Doppler radar sensor (Invited). In Proceedings of the IEEE MTT-S International Microwave Workshop Series on RF and Wireless Technologies for Biomedical and Healthcare Applications, Taipei, Taiwan, 21–23 September 2015. [Google Scholar]
- Lee, I.-S.; Park, J.-H.; Yang, J.-R. Detrending technique for denoising in CW radar, Sensors 2021, 21, 6376. Sensors 2021, 21, 6376. [Google Scholar]
- Li, Y.; Wang, G.; Gu, C.; Li, C. Movement-immune respiration monitoring using automatic DC-correction algorithm for CW Doppler radar system. In Proceedings of the Topical Conference on Biomedical Wireless Technologies, Networks, and Sensing Systems, Newport Beach, CA, USA, 19–23 January 2014; pp. 7–9. [Google Scholar]
- Ramachandran, G.; Singh, M. Three-dimensional reconstruction of cardiac displacement patterns on the chest wall during the P, QRS and T-segments of the ECG by laser speckle inteferometry. Med. Biol. Eng. Comput. 2006, 27, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Laizzo, P.A. Handbook of Cardiac Anatomy, Physiology, and Devices; Springer International Publishing: Manhattan, NY, USA, 2015; pp. 51–79. [Google Scholar]
- Periasamy, A.; Singh, M. Reconstruction of cardiac displacement patterns on the chest wall by laser speckle interferometry. IEEE Trans. Med. Imaging 1985, 4, 52–57. [Google Scholar] [CrossRef] [PubMed]
- De Groote, A.; Wantier, M.; Cheron, G.; Estenne, M.; Paiva, M. Chest wall motion during tidal breathing. Eur. J. Appl. Physiol. 1997, 83, 1531–1537. [Google Scholar] [CrossRef] [Green Version]
- Plathow, C.; Ley, S.; Fink, C.; Puderbach, M.; Heilmann, M.; Zuna, I.; Kauczor, H. Evaluation of chest motion and volumetry during the breathing cycle by dynamic MRI in healthy subjects. Investigative Radiology 2004, 39, 202–209. [Google Scholar] [CrossRef]
- BruceBlaus. Medical Gallery of Blausen Medical 2014. Available online: https://commons.wikimedia.org/wiki/File:Systolevs_Diastole.png (accessed on 28 September 2021).
- Memmler, R.L.; Cohen, B.J.; Wood, D.L.; Ravielli, A. Memmler’s The Human Body in Health and Disease, 11th ed.; Lippincott Williams & Wilkins: Burlington, MA, USA, 2009. [Google Scholar]
- Park, B.-K.; Boric-Lubecke, O.; Lubecke, V. Arctangent demodulation with DC offset compensation in quadrature Doppler radar receiver systems. IEEE Trans. Microwave Theory Tech. 2007, 55, 1073–1079. [Google Scholar] [CrossRef]
- Fan, T.; Ma, C.; Gu, Z.; Lv, Q.; Chen, J.; Ye, D.; Huangfu, J.; Sun, Y.; Li, C.; Ran, L. Wireless hand gesture recognition based on continuous-wave Doppler radar sensors. IEEE Trans. Microwave Theory Tech. 2016, 64, 4012–4020. [Google Scholar] [CrossRef]
- Park, J.-H.; Yang, J.-R. Multiphase continuous-wave Doppler radar with multiarc circle fitting algorithm for small periodic displacement measurement. IEEE Trans. Microwave Theory Tech. 2021, 69, 5135–5144. [Google Scholar] [CrossRef]
- Tang, M.-C.; Wang, F.-K.; Horng, T.-S. Single self-injection-locked radar with two antennas for monitoring vital signs with large body movement cancellation. IEEE Trans. Microwave Theory Tech. 2017, 65, 5324–5333. [Google Scholar] [CrossRef]
- Lv, Q.; Chen, L.; An, K.; Wang, J.; Li, H.; Ye, D.; Huangfu, J.; Li, C.; Ran, L. Doppler vital signs detection in the presence of large-scale random body movements. IEEE Trans. Microwave Theory Tech. 2018, 66, 4261–4270. [Google Scholar] [CrossRef]
- Yang, Z.-K.; Shi, H.; Zhao, S.; Huang, X.-D. Vital sign detection during large-scale and fast body movements based on an adaptive noise cancellation algorithm using a single Doppler radar sensor. Sensors 2020, 20, 4183. [Google Scholar] [CrossRef] [PubMed]














| Ref. | Techniques | Maximum Body Movement [mm] | Maximum Body Velocity [mm/s] | Detection Accuracy [%] | |
|---|---|---|---|---|---|
| Respiration | Heartbeat | ||||
| [8] | CSD method using two antennas around the subject | Not mentioned | 4 | Not mentioned | Not mentioned |
| [30] | SIL 1 radar using two antennas | 200 | 7.7 | Not mentioned | 96.5 |
| [31] | Polynomial fitting algorithm | 150 | 0 | Not mentioned | Not mentioned |
| [32] | Adaptive noise cancelation algorithm | 155 | 47.6 | 97.9 | 99.1 |
| This work | Correlation method using multiple radars | 80 | 53.4 | 97.8 2 | 97.9 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jang, A.-J.; Lee, I.-S.; Yang, J.-R. Vital Signal Detection Using Multi-Radar for Reductions in Body Movement Effects. Sensors 2021, 21, 7398. https://doi.org/10.3390/s21217398
Jang A-J, Lee I-S, Yang J-R. Vital Signal Detection Using Multi-Radar for Reductions in Body Movement Effects. Sensors. 2021; 21(21):7398. https://doi.org/10.3390/s21217398
Chicago/Turabian StyleJang, Ah-Jung, In-Seong Lee, and Jong-Ryul Yang. 2021. "Vital Signal Detection Using Multi-Radar for Reductions in Body Movement Effects" Sensors 21, no. 21: 7398. https://doi.org/10.3390/s21217398







