Computerized Assessment of Occlusion and Muscle Activity during Use of a Multilayer Clear Retainer: A Preliminary Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
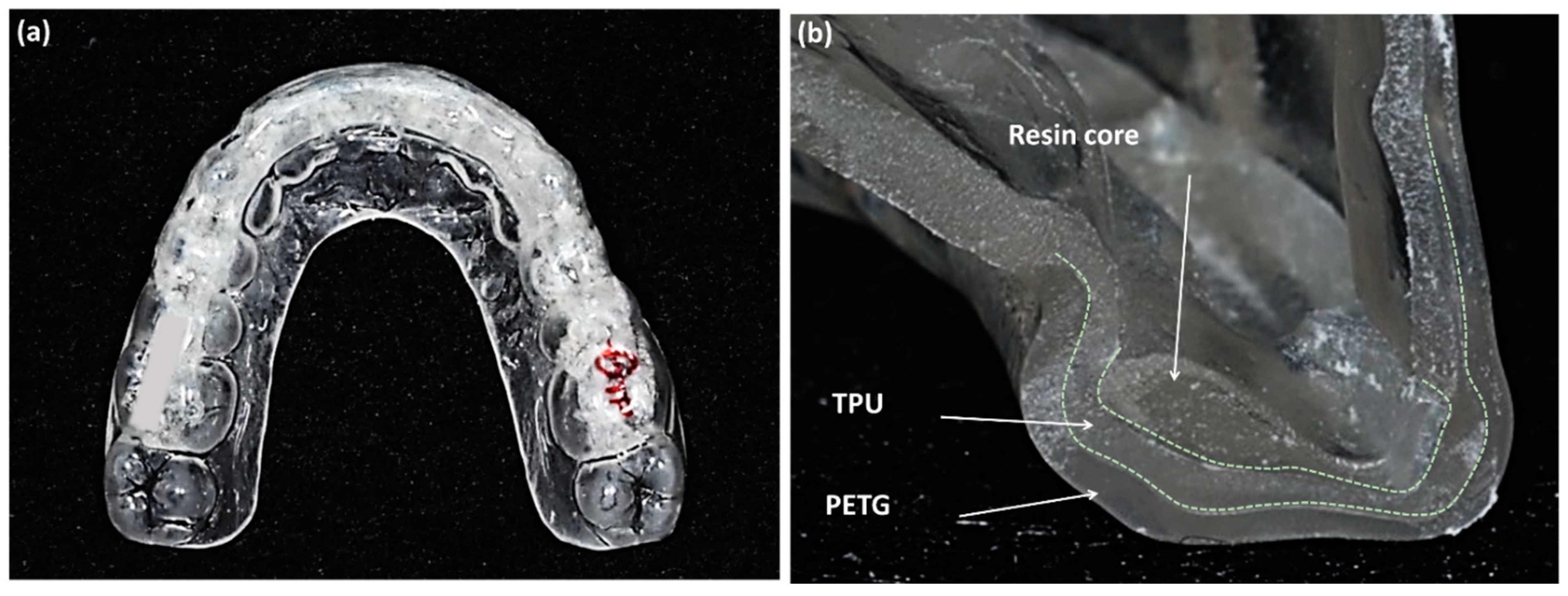
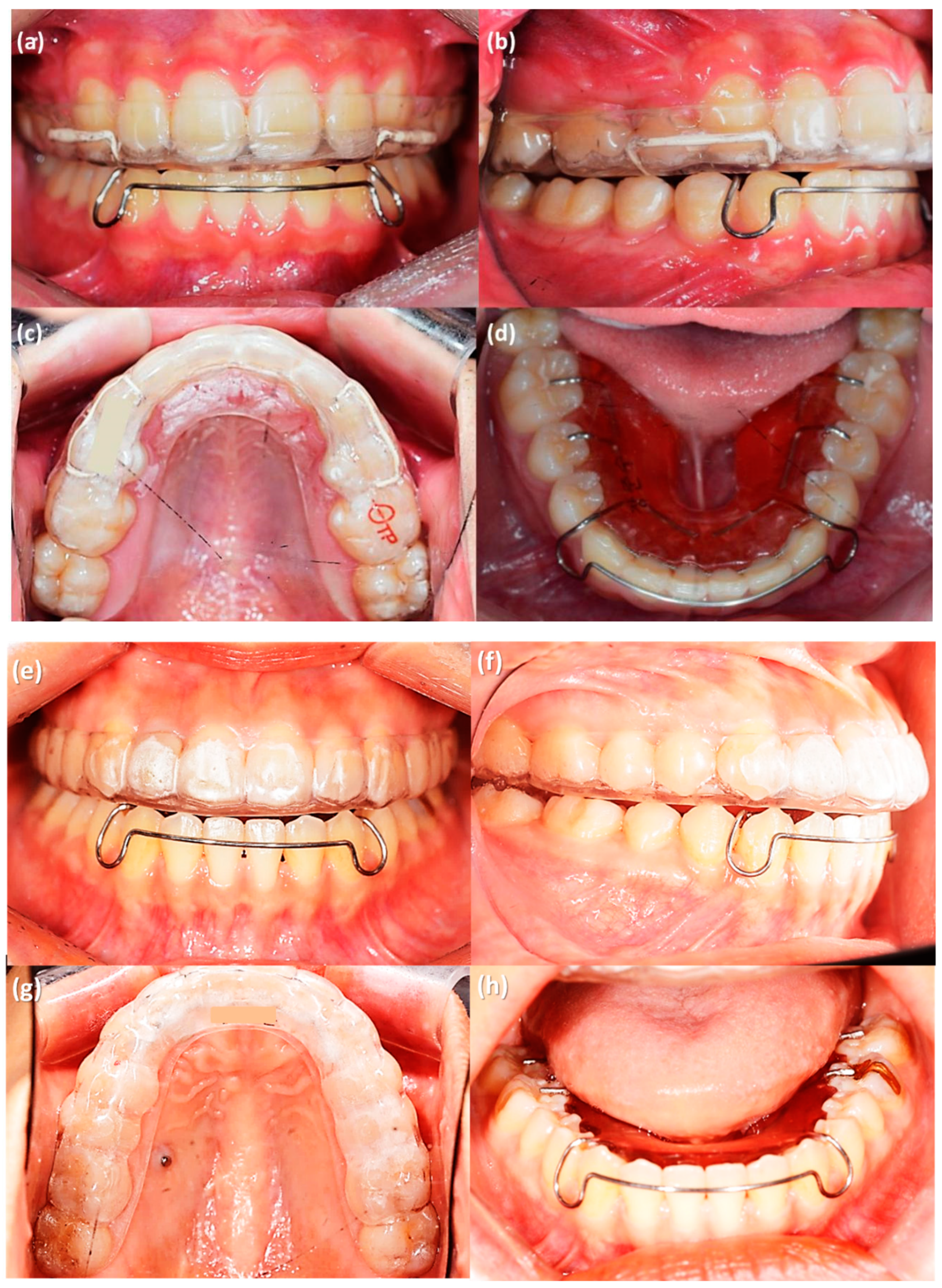
2.2. Retention Protocols
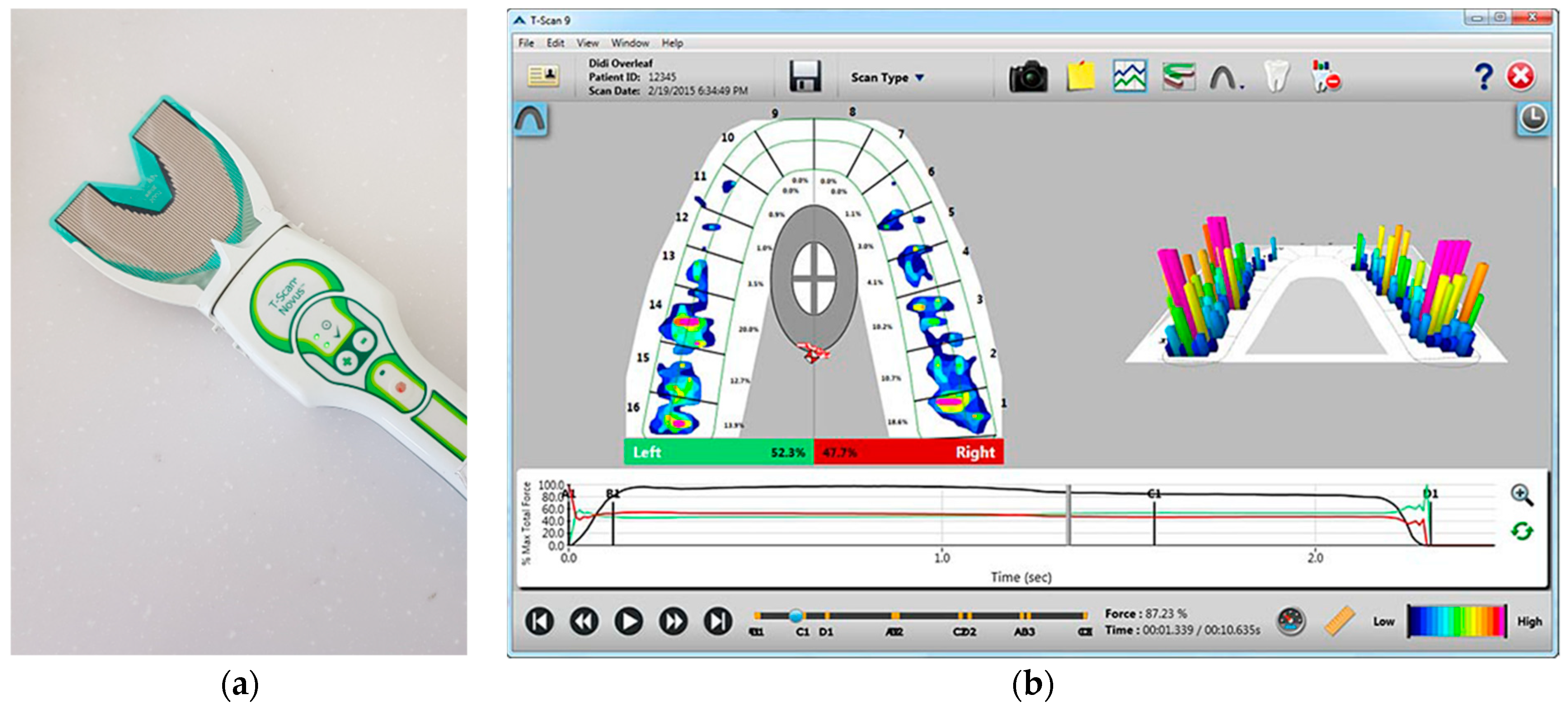
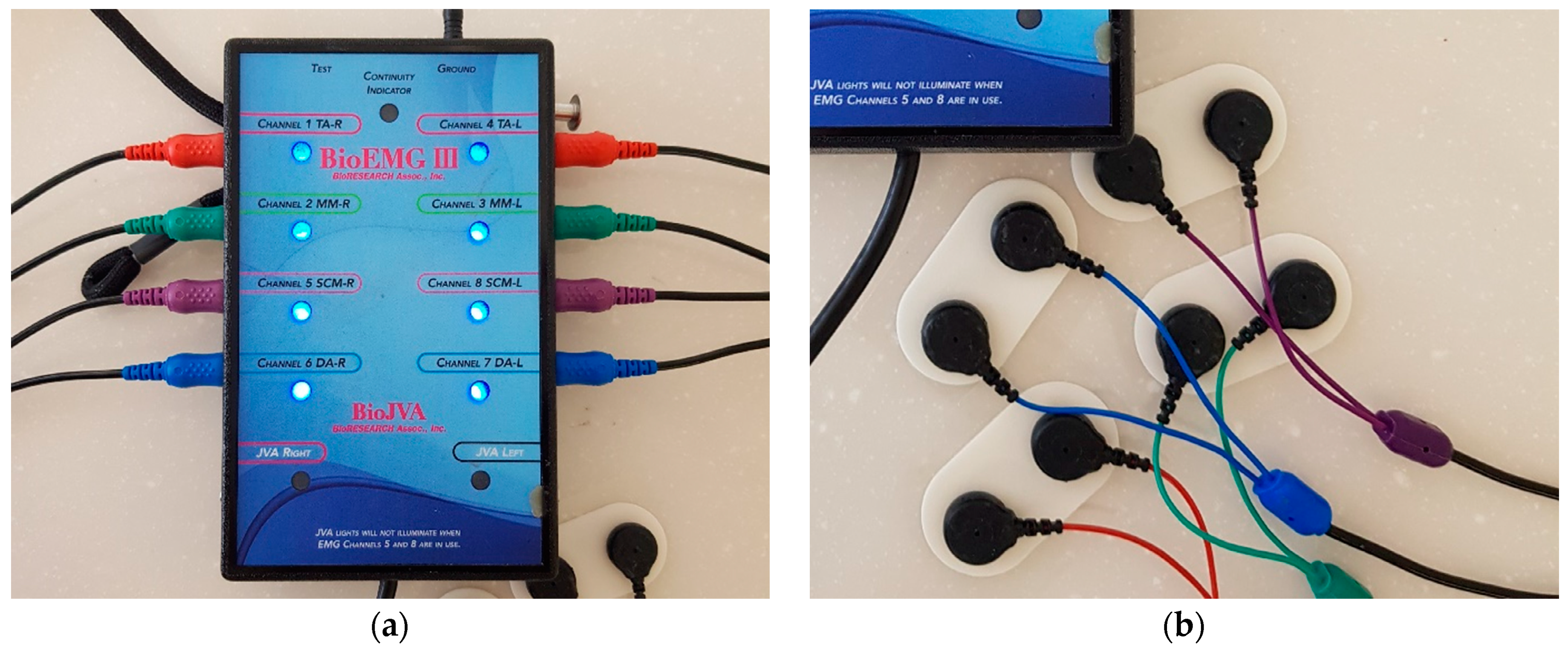
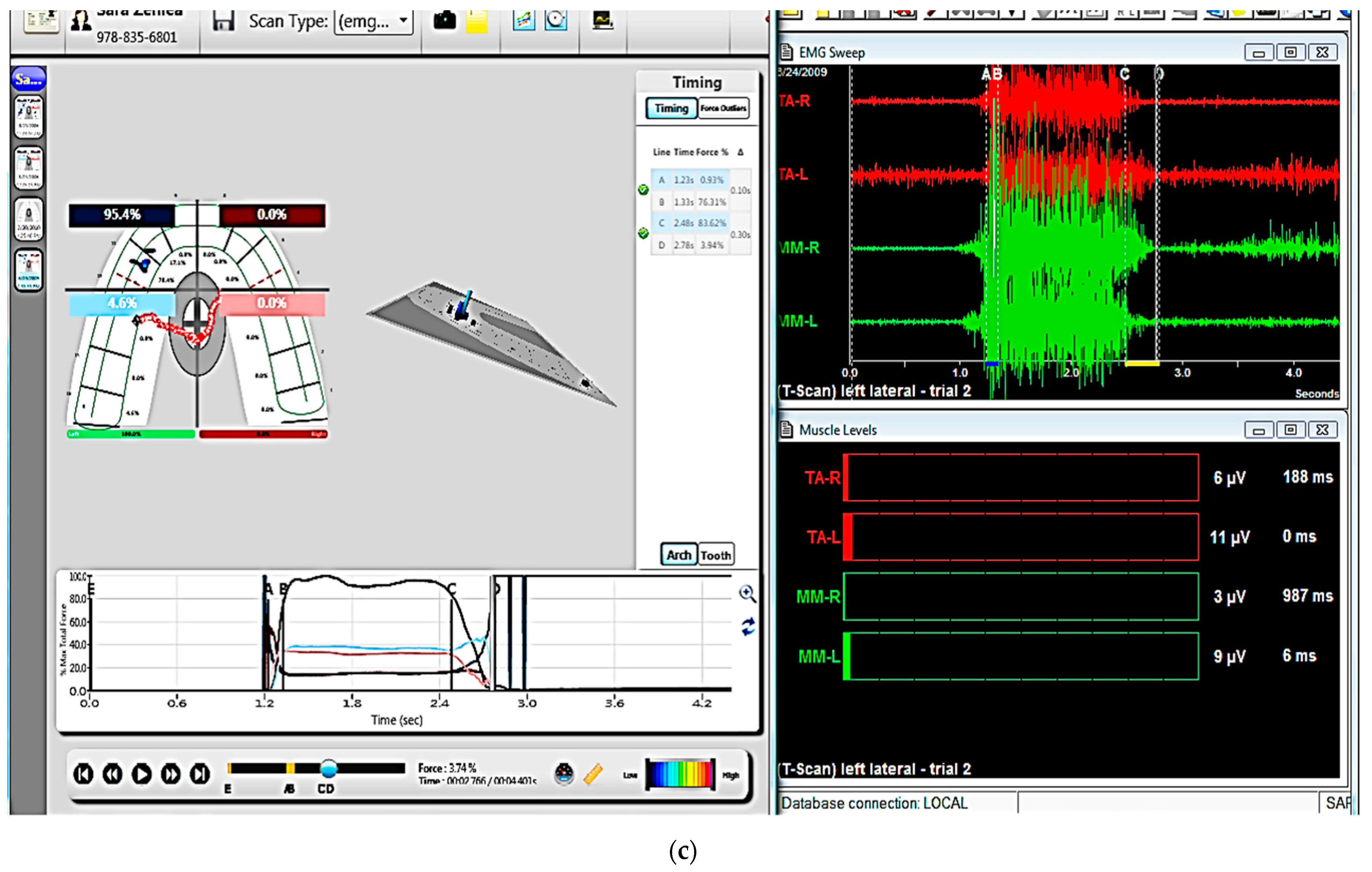
2.3. Occlusal and EMG Analysis
2.4. Statistical Analysis
3. Results
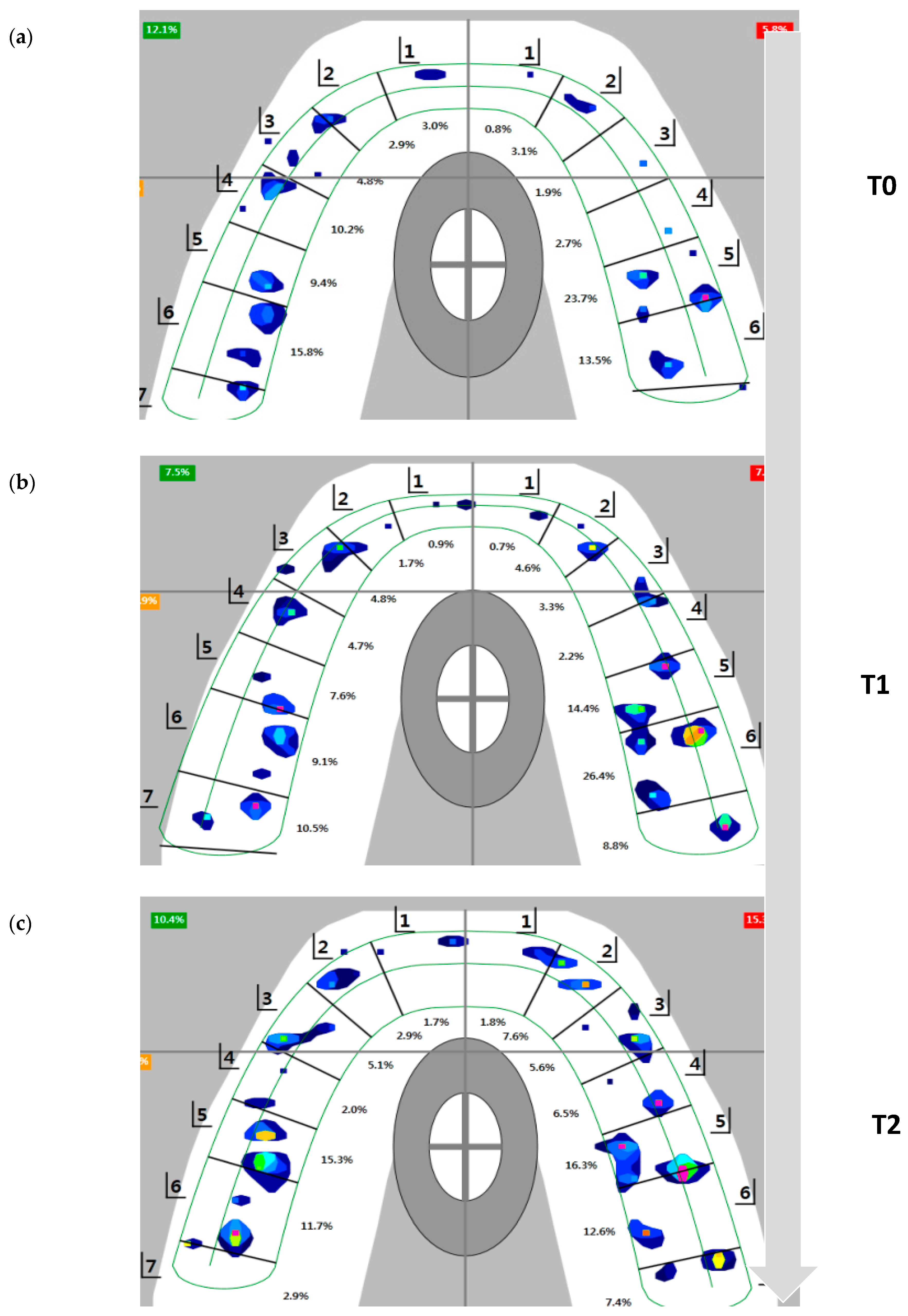
3.1. T-Scan Analysis
3.2. EMG Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Littlewood, S.J.; Millett, D.T.; Doubleday, B.; Bearn, D.R.; Worthington, H.V. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst. Rev. 2016, 2016, CD002283. [Google Scholar] [CrossRef] [PubMed]
- Aslan, B.I.; Dinçer, M.; Salmanli, O.; Qasem, M.A. Comparison of the effects of modified and full-coverage thermoplastic retainers on occlusal contacts. Orthodontics 2013, 14, e198–e208. [Google Scholar]
- Melrose, C.; Millett, D.T. Toward a perspective on orthodontic retention? Am. J. Orthod. Dentofac. Orthop. 1998, 113, 507–514. [Google Scholar] [CrossRef]
- Demir, A.; Babacan, H.; Nalcaci, R.; Topcuoglu, T. Comparison of retention characteristics of Essix and Hawley retainers. Korean J. Orthod. 2012, 42, 255–262. [Google Scholar] [CrossRef]
- Rowland, H.; Hichens, L.; Williams, A.; Hills, D.; Killingback, N.; Ewings, P.; Clark, S.; Ireland, A.J.; Sandy, J.R. The effectiveness of Hawley and and vacuum-formed retainers: A single-center randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 730–737. [Google Scholar] [CrossRef]
- Tai, S. Clear Aligner Technique; Quintessence Publishing Co., Inc.: Hanover Park, IL, USA, 2018; pp. 74–76. [Google Scholar]
- Ahn, H.Y.; Kim, K.A.; Kim, S.H. A new type of clear orthodontic retainer incorporating multi-layer hybrid materials. Korean J. Orthod. 2015, 45, 268–272. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.Y.; Ahn, H.W.; Kim, S.H.; Nelson, G. Effects of a new type of clear overlay retainer on occlusal contacts. Korean J. Orthod. 2017, 47, 207–212. [Google Scholar] [CrossRef]
- Dupaix, R.B.; Boyce, M.C. Finite strain behavior of poly(ethylene terephthalate) (PET) and poly(ethylene terephthalate)-glycol (PETG). Polymer 2005, 46, 4827–4838. [Google Scholar] [CrossRef]
- Lu, Q.W.; Macosko, C.W. Comparing the compatibility of various functionalized polypropylenes with thermoplastic polyurethane (TPU). Polymer 2004, 45, 1981–1991. [Google Scholar] [CrossRef]
- Frick, A.; Rochman, A. Characterization of TPU-elastomers by thermal analysis (DSC). Polym. Test. 2004, 23, 413–417. [Google Scholar] [CrossRef]
- Afrashtehfar, K.I.; Qadeer, S. Computerized occlusal analysis as an alternative occlusal indicator. Cranio 2016, 34, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Kerstein, R.B. Combining technologies: A computerized occlusal analysis system synchronized with a computerized electromyography system. Cranio 2004, 22, 96–109. [Google Scholar] [CrossRef] [PubMed]
- Wieczorek, A.; Loster, J.E. Activity of the masticatory muscles and occlusal contacts in young adults with and without orthodontic treatment. BMC Oral Health 2015, 15, 116. [Google Scholar] [CrossRef]
- Mahony, D. Refining occlusion with muscle balance to enhance long-term orthodontic stability. Malays. Dent. J. 2010, 31, 44–52. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Kim, Y.S.; Kwon, S.Y.; Park, Y.G.; Chung, K.R. Clinical application of the tongue elevator. J. Clin. Orthod. 2002, 36, 104–106. [Google Scholar]
- Naeije, M.; McCarroll, R.S.; Weijs, W.A. Electromyographic activity of the human masticatory muscles during submaximal clenching in the inter-cuspal position. J. Oral Rehabil. 1989, 16, 63–70. [Google Scholar] [CrossRef]
- Moss, J.P. The soft tissue environment of teeth and jaws: An experimental and clinical study: Part 1. Br. J. Orthod. 1980, 7, 127–137. [Google Scholar] [CrossRef]
- Moss, J.P. The soft tissue environment of teeth and jaws: Experimental malocclusion: Parts 2 and 3. Br. J. Orthod. 1980, 7, 205–216. [Google Scholar] [CrossRef]
- Kerstein, R.B. T-scan III applications in mixed arch and complete arch, implant -supported prosthodontics. Dent. Implant. Updat. 2008, 19, 49–53. [Google Scholar]
- Morton, S.; Pancherz, H. Changes in functional occlusion during the postorthodontic retention period: A prospective longitudinal clinical study. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Lustig, J.R.; Rossouw, P.E.; Buschang, P.H.; Behrents, R.G.; Woody, R.D. Assessment of post-orthodontic occlusal contacts with wrap-around and clear overlay retainers. Semin. Orthod. 2017, 23, 166–177. [Google Scholar] [CrossRef]
- Qadeer, S.; Yang, L.; Sarinnaphakorn, L.; Kerstein, R.B. Comparison of closure occlusal force parameters in post-orthodontic and non-orthodontic subjects using T-Scan® III DMD occlusal analysis. Cranio 2016, 34, 395–401. [Google Scholar] [CrossRef]
- Qadeer, S.; Abbas, A.A.; Sarinnaphakorn, L.; Kerstein, R.B. Comparison of excursive occlusal force parameters in post-orthodontic and non-orthodontic subjects using T-Scan® III. Cranio 2018, 36, 11–18. [Google Scholar] [CrossRef]
- Lee, S.M.; Lee, J.W. Computerized occlusal analysis: Correlation with occlusal indexes to assess the outcome of orthodontic treatment or the severity of malocculusion. Korean J. Orthod. 2016, 46, 27–35. [Google Scholar] [CrossRef]
- Lindauer, S.J.; Shoff, R.C. Comparison of Essix and Hawley retainers. J. Clin. Orthod. 1998, 32, 95–97. [Google Scholar]
- Seo, Y.J.; Kim, S.J.; Munkhshur, J.; Chung, K.R.; Ngan, P.; Kim, S.H. Treatment and retention of relapsed anterior open-bite with low tongue posture and tongue-tie: A 10-year follow-up. Korean J. Orthod. 2014, 44, 203–216. [Google Scholar] [CrossRef]
- Vaden, J.L. A century of the edgewise appliance. APOS Trends Orthod. 2015, 5, 239–249. [Google Scholar] [CrossRef]
- Tartaglia, G.M.; Moreira Rodrigues da Silva, M.A.; Sforza, C.; Ferrario, V.F. Masticatory muscle activity during maximum voluntary clench in different research diagnostic criteria for temporomandibular disorders (RDC/TMD) groups. Man. Ther. 2008, 13, 434–440. [Google Scholar] [CrossRef]
- Woźniak, K.; Piątkowska, D.; Lipski, M.; Mehr, K. Surface electromyography in orthodontics—A literature review. Med. Sci. Monit. 2013, 19, 416–423. [Google Scholar] [PubMed]
- Botelho, A.L.; Melchior Mde, O.; da Silva, A.M.; da Silva, M.A. Electromyographic evaluation of neuromuscular coordination of subject after orthodontic intervention. Cranio 2009, 27, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Ferrario, V.F.; Marciandi, P.V.; Tartaglia, G.M.; Dellavia, C.; Sforza, C. Neuromuscular evaluation of post-orthodontic stability: An experimental protocol. Int. J. Adult Orthod. Orthognath. Surg. 2002, 17, 307–313. [Google Scholar]
- Kerstein, R.B.; Radke, J. Masseter and temporalis excursive hyperactivity decreased by measured anterior guidance development. Cranio 2012, 30, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Wieczorek, A.; Loster, J.; Loster, B.W. Relationship between occlusal force distribution and the activity of masseter and anterior temporalis muscles in asymptomatic young adults. Biomed Res. Int. 2013, 2013, 354017. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Sforza, C.; Miani, A., Jr.; D’Addona, A.; Barbini, E. Electromyographic activity of human masticatory muscles in normal young people. Statistical evaluation of reference values for clinical applications. J. Oral Rehabil. 1993, 20, 271–280. [Google Scholar] [CrossRef]
- Masci, C.; Ciarrocchi, I.; Spadaro, A.; Necozione, S.; Marci, M.C.; Monaco, A. Does orthodontic treatment provide a real functional improvement? a case control study. BMC Oral Health 2013, 13, 57. [Google Scholar] [CrossRef]
- Suvinen, T.I.; Kemppainen, P. Review of clinical EMG studies related to muscle and occlusal factors in healthy and TMD subjects. J. Oral Rehabil. 2007, 34, 631–644. [Google Scholar] [CrossRef]
- Scopel, V.; Alves da Costa, G.S.; Urias, D. An electromyographic study of masseter and anterior temporalis muscles in extra-articular myogenous TMJ pain patients compared to an asymptomatic and normal population. Cranio 2005, 23, 194–203. [Google Scholar] [CrossRef]
- Kim, K.A.; Park, H.S.; Lee, S.Y.; Kim, S.J.; Baek, S.H.; Ahn, H.W. Short-term changes in muscle activity and jaw movement patterns after orthognathic surgery in skeletal Class III patients with facial asymmetry. Korean J. Orthod. 2019, 49, 254–264. [Google Scholar] [CrossRef]
- Kerstein, R. Computerized Occlusal Analysis Technology Applications in Dental Medicine; IGI Global: Hershey, PA, USA, 2015; Volume 2, pp. 35–61. [Google Scholar]


| Subjects | |
|---|---|
| Number (n) | 18 |
| Age (years) | 20.3 ± 6.0 1 |
| Gender (n) | |
| Male | 8 |
| Female | 10 |
| Sagittal pattern (n) | |
| Class I | 8 |
| Class II | 6 |
| Class III | 4 |
| Vertical pattern (n) | |
| Hyperdivergent | 3 |
| Normodivergent | 10 |
| Hypodivergent | 5 |
| Treatment option (n) | |
| Premolars extraction | 6 |
| Non-extraction | 12 |
| T0 | T1 | T2 | p-Value 5 | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Time (s) | |||||||
| OT 1 | 0.23 | 0.12 | 0.27 | 0.13 | 0.24 | 0.15 | 0.494 |
| Pro-DT 2 | 0.52 | 0.29 | 0.44 | 0.17 | 0.56 | 0.27 | 0.279 |
| Left-DT 3 | 0.95 | 0.49 | 0.72 | 0.29 | 0.81 | 0.43 | 0.070 |
| Right-DT 4 | 0.88 | 0.61 | 0.75 | 0.60 | 0.58 | 0.25 | 0.135 |
| Force (%) | |||||||
| Left Anterior | 7.68 | 8.04 | 6.01 | 6.60 | 4.88 | 5.30 | 0.226 |
| Right Anterior | 7.57 | 7.56 | 5.77 | 4.69 | 5.07 | 5.48 | 0.269 |
| Anterior | 15.24 | 14.73 | 11.78 | 10.41 | 9.95 | 9.78 | 0.213 |
| Left Posterior | 49.68 | 9.60 | 47.08 | 10.03 | 49.66 | 12.55 | 0.488 |
| Right Posterior | 35.07 | 10.36 | 41.13 | 9.81 | 40.38 | 9.49 | 0.010 * T1 > T0 (0.020), T2 > T0 (0.042) 6 |
| Posterior | 84.76 | 14.73 | 88.21 | 10.40 | 90.04 | 9.76 | 0.215 |
| Larger side | 57.47 | 6.83 | 56.86 | 6.01 | 59.09 | 6.30 | 0.234 |
| Smaller side | 42.53 | 6.85 | 43.16 | 6.02 | 40.90 | 6.31 | 0.233 |
| T0 | T1 | T2 | p-Value 8 | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Potentials (μV) | |||||||
| TA_L 1 | 79.00 | 39.31 | 71.33 | 27.32 | 90.89 | 42.91 | 0.202 |
| TA_R 2 | 85.59 | 44.53 | 88.56 | 37.68 | 87.61 | 41.71 | 0.934 |
| MM_L 3 | 74.53 | 61.08 | 67.17 | 65.74 | 72.44 | 47.94 | 0.613 |
| MM_R 4 | 61.24 | 51.25 | 62.00 | 55.35 | 56.94 | 29.47 | 0.983 |
| Asymmetry index (%) | |||||||
| Asym_MM 5 | 4.83 | 28.03 | −1.73 | 32.73 | 2.79 | 25.75 | 0.891 |
| Asym_TA 6 | −3.04 | 20.26 | −2.17 | 22.04 | 12.06 | 21.37 | 0.089 |
| Asym index 7 | 0.31 | 19.32 | −0.93 | 21.38 | 9.84 | 14.92 | 0.248 |
| Activity index | −18.21 | 29.07 | −19.92 | 27.76 | −17.59 | 27.25 | 0.939 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, K.Y.; Choi, J.-Y.; Oh, S.H.; Moon, H.-W.; Kim, S.-H.; Ahn, H.-W.; Kim, K.A.; Nelson, G. Computerized Assessment of Occlusion and Muscle Activity during Use of a Multilayer Clear Retainer: A Preliminary Study. Sensors 2021, 21, 541. https://doi.org/10.3390/s21020541
Kim KY, Choi J-Y, Oh SH, Moon H-W, Kim S-H, Ahn H-W, Kim KA, Nelson G. Computerized Assessment of Occlusion and Muscle Activity during Use of a Multilayer Clear Retainer: A Preliminary Study. Sensors. 2021; 21(2):541. https://doi.org/10.3390/s21020541
Chicago/Turabian StyleKim, Kyoung Yeon, Jin-Young Choi, Song Hee Oh, Hyung-Wook Moon, Seong-Hun Kim, Hyo-Won Ahn, Kyung A Kim, and Gerald Nelson. 2021. "Computerized Assessment of Occlusion and Muscle Activity during Use of a Multilayer Clear Retainer: A Preliminary Study" Sensors 21, no. 2: 541. https://doi.org/10.3390/s21020541
APA StyleKim, K. Y., Choi, J.-Y., Oh, S. H., Moon, H.-W., Kim, S.-H., Ahn, H.-W., Kim, K. A., & Nelson, G. (2021). Computerized Assessment of Occlusion and Muscle Activity during Use of a Multilayer Clear Retainer: A Preliminary Study. Sensors, 21(2), 541. https://doi.org/10.3390/s21020541






