Home-Based Sleep Sensor Measurements in an Older Australian Population: Before and during a Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Approval and Consent to Participate
2.3. Participants and Recruitment
- aged 65 years and older;
- living at home—in the care of a designated aged care service provider; and
- English speaking, with proficiency in written English.
- people residing in long-term residential care;
- Individuals not able to give informed consent due to reasons such as severe cognitive impairment (must have been able to provide informed consent); and
- people who were unwilling to leave their electricity on overnight.
2.4. Sleep Monitoring Device
2.5. Sleep Measurements
2.6. Study Population and Period
2.7. Statistical Analysis
3. Results
3.1. Baseline Participant Characteristics
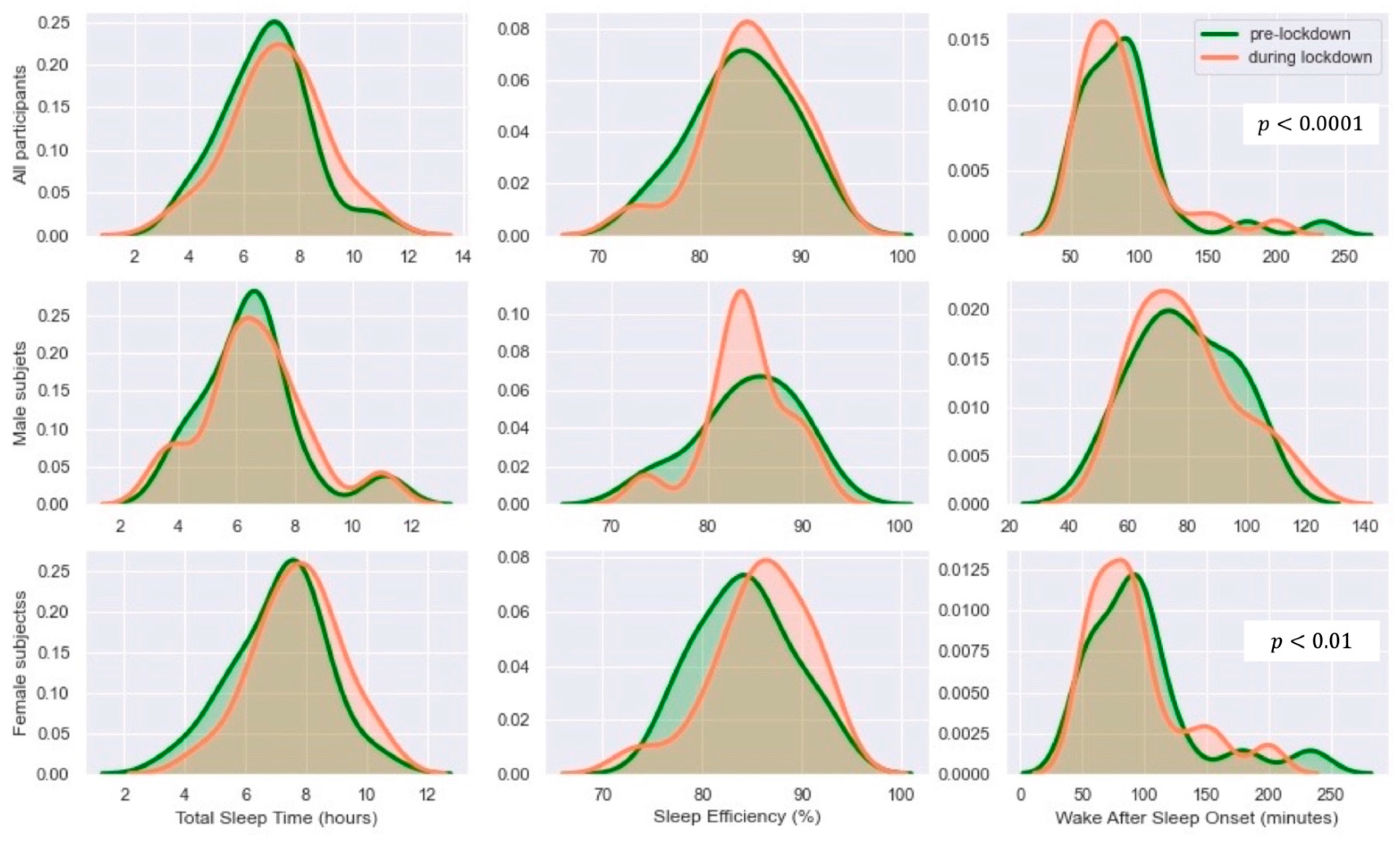
3.2. Distribution
3.3. Changes in Sleep Measures before and during Lockdown
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Long, L.; Zeng, X.; Zhang, X.; Xiao, W.; Guo, E.; Zhan, W.; Yang, X.; Li, C.; Wu, C.; Xu, T.; et al. Short-term outcomes of COVID-19 and risk factors for progression. Eur. Respir. J. 2020, 55, 2000990. [Google Scholar] [CrossRef] [Green Version]
- Parker, G.; Lie, D.; Siskind, D.J.; Martin-Khan, M.; Raphael, B.; Crompton, D.; Kisely, S. Mental health implications for older adults after natural disasters–a systematic review and meta-analysis. Int. Psychogeriatr. 2016, 28, 11–20. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef] [Green Version]
- Jia, G.; Yuan, P. The association between sleep quality and loneliness in rural older individuals: A cross-sectional study in Shandong Province, China. BMC Geriatr. 2020, 20, 180. [Google Scholar] [CrossRef]
- Parlapani, E.; Holeva, V.; Nikopoulou, V.A.; Sereslis, K.; Athanasiadou, M.; Godosidis, A.; Stephanou, T.; Diakogiannis, I. Intolerance of Uncertainty and Loneliness in Older Adults during the COVID-19 Pandemic. Front. Psychiatry 2020, 11, 842. [Google Scholar] [CrossRef] [PubMed]
- Grossman, E.S.; Hoffman, Y.S.G.; Palgi, Y.; Shrira, A. COVID-19 related loneliness and sleep problems in older adults: Worries and resilience as potential moderators. Personal. Individ. Differ. 2021, 168, 110371. [Google Scholar] [CrossRef] [PubMed]
- Casagrande, M.; Favieri, F.; Tambelli, R.; Forte, G. The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020, 75, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef]
- Lauderdale, D.S.; Knutson, K.L.; Yan, L.L.; Liu, K.; Rathouz, P.J. Self-reported and measured sleep duration: How similar are they? Epidemiology 2008, 19, 838–845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, H.; Lack, L.; Lovato, N. A systematic review of the accuracy of sleep wearable devices for estimating sleep onset. Sleep Med. Rev. 2020, 49, 101227. [Google Scholar] [CrossRef]
- De Zambotti, M.; Cellini, N.; Goldstone, A.; Colrain, I.M.; Baker, F.C. Wearable Sleep Technology in Clinical and Research Settings. Med. Sci. Sports Exerc. 2019, 51, 1538–1557. [Google Scholar] [CrossRef]
- De Zambotti, M.; Baker, F.C.; Willoughby, A.R.; Godino, J.G.; Wing, D.; Patrick, K.; Colrain, I.M. Measures of sleep and cardiac functioning during sleep using a multi-sensory commercially-available wristband in adolescents. Physiol. Behav. 2016, 158, 143–149. [Google Scholar] [CrossRef] [Green Version]
- Kang, S.-G.; Kang, J.M.; Ko, K.-P.; Park, S.-C.; Mariani, S.; Weng, J. Validity of a commercial wearable sleep tracker in adult insomnia disorder patients and good sleepers. J. Psychosom. Res. 2017, 97, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Ranta, J.; Aittokoski, T.; Tenhunen, M.; Alasaukko-oja, M. EMFIT QS heart rate and respiration rate validation. Biomed. Phys. Eng. Express 2019, 5, 025016. [Google Scholar] [CrossRef]
- Zhang, Q.; Varnfield, M.; Higgins, L.; Smallbon, V.; Bomke, U.; O’Dwyer, J.; Byrnes, J.M.; Sum, M.; Hewitt, J.; Lu, W.; et al. Smarter Safer Homes Solution to Support Older People Living in Their Own Homes through Enhanced Care Models: Methodologies for a Stratified Randomized Controlled Trial. JMIR Prepr. 2021. [Google Scholar] [CrossRef]
- EMFIT Sleep Tracking and Monitoring. Available online: https://www.emfit.com/ (accessed on 24 May 2021).
- Lin, Y.; Liu, S.; Li, S.; Zuo, H.; Zhang, B. Relationships between the changes in sleep patterns and sleep quality among Chinese people during the 2019 coronavirus disease outbreak. Sleep Med. 2021. [Google Scholar] [CrossRef]
- Blume, C.; Schmidt, M.H.; Cajochen, C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr. Biol. 2020, 30, R795–R797. [Google Scholar] [CrossRef]
- Robbins, R.; Affouf, M.; Weaver, M.D.; Czeisler, M.É.; Barger, L.K.; Quan, S.F.; Czeisler, C.A. Estimated Sleep Duration before and during the COVID-19 Pandemic in Major Metropolitan Areas on Different Continents: Observational Study of Smartphone App Data. J. Med. Internet Res. 2021, 23, e20546. [Google Scholar] [CrossRef] [PubMed]
- Zitting, K.-M.; Lammers-van der Holst, H.M.; Yuan, R.K.; Wang, W.; Quan, S.F.; Duffy, J.F. Google Trends reveals increases in internet searches for insomnia during the 2019 coronavirus disease (COVID-19) global pandemic. J. Clin. Sleep Med. 2021, 17, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Buxton, O.M.; Hikichi, H.; Haneuse, S.; Aida, J.; Kondo, K.; Kawachi, I. Predictors of persistent sleep problems among older disaster survivors: A natural experiment from the 2011 Great East Japan earthquake and tsunami. Sleep 2018, 41, zsy084. [Google Scholar] [CrossRef]
- Dong, E.; Du, H.; Gardner, L. An Interactive Web-Based Dashboard to Track COVID-19 in Real Time. Available online: https://coronavirus.jhu.edu/map.html (accessed on 8 April 2021).
- Salfi, F.; Lauriola, M.; Amicucci, G.; Corigliano, D.; Viselli, L.; Tempesta, D.; Ferrara, M. Gender-related time course of sleep disturbances and psychological symptoms during the COVID-19 lockdown: A longitudinal study on the Italian population. Neurobiol. Stress 2020, 13, 100259. [Google Scholar] [CrossRef] [PubMed]
- Ee, N.; Maccora, J.; Hosking, D.; McCallum, J. Australian Grandparents Care; National Seniors Australia: Canberra, Australia, 2020. [Google Scholar]
- Mattingly, S.M.; Grover, T.; Martinez, G.J.; Aledavood, T.; Robles-Granda, P.; Nies, K.; Striegel, A.; Mark, G. The effects of seasons and weather on sleep patterns measured through longitudinal multimodal sensing. Npj Digit. Med. 2021, 4, 76. [Google Scholar] [CrossRef] [PubMed]
- Okamoto-Mizuno, K.; Tsuzuki, K. Effects of season on sleep and skin temperature in the elderly. Int. J. Biometeorol. 2010, 54, 401–409. [Google Scholar] [CrossRef] [PubMed]



| Daily Living Event | Sensor Type | Location |
|---|---|---|
| Meal preparation | Motion sensor Electrical power sensor Accelerometers | Dining room Kitchen |
| Dressing | Motion sensor Accelerometer | Wardrobe |
| Hygiene | Motion sensor Humidity sensor Temperature sensor | Bathroom |
| Indoor walking | Motion sensor | All rooms |
| Sit–stand transition times (out of a bed/chair) | Accelerometer Pressure sensor Sleep sensor | Bedroom Living room |
| Total, n = 31 | |
|---|---|
| Age, years, mean ± SD [range] | 84 ± 6.8 [70–94] |
| Female, n (%) | 17 (54.8%) |
| Body mass index, kg/m2, mean ± SD | 28.4 ± 6.1 |
| Pre-Lockdown | During Lockdown | p | |||||||
|---|---|---|---|---|---|---|---|---|---|
| All | Males | Females | All | Males | Females | All | Males | Females | |
| TST (h) | 6.9 ± 1.6 | 6.5 ± 1.8 | 7.1 ± 1.5 | 7.2 ± 1.7 | 6.7 ± 1.9 | 7.7 ± 1.4 | 0.06 | 0.7 | 0.014 * |
| SOL (min) | 25.8 ± 4.9 | 25.7 ± 4.6 | 25.8 ± 5.3 | 25.7 ± 6.6 | 25.8 ± 6.6 | 25.6 ± 6.7 | 0.94 | 0.9 | 0.88 |
| WASO (min) | 89.1 ± 37.3 | 78.7 ± 16 | 97.6 ± 47.2 | 86.8 ± 32.4 | 79.3 ± 17 | 93 ± 40.5 | 0.46 | 0.82 | 0.27 |
| SE (%) | 84.2 ± 4.8 | 84.2 ± 5.2 | 84.2 ± 4.7 | 85.1 ± 4.7 | 84.1 ± 4.5 | 85.9 ± 4.9 | 0.18 | 0.95 | 0.05 * |
| Time to bed | 20:11:25 ± 06:13:59 | 19:27:04 ± 07:58:38 | 20:47:56 ± 04:30:08 | 20:25:47 ± 05:00:48 | 20:44:06 ± 05:38:37 | 20:10:42 ± 04:35:37 | 0.76 | 0.47 | * |
| Time out of bed | 07:01:26 ± 01:32:25 | 06:54:57 ± 01:33:5 | 07:06:46 ± 01:33:41 | 06:51:18 ± 01:22:02 | 06:41:02 ± 01:30:09 | 06:59:45 ± 01:16:27 | 0.19 | 0.21 | 0.53 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kholghi, M.; Ellender, C.M.; Zhang, Q.; Gao, Y.; Higgins, L.; Karunanithi, M. Home-Based Sleep Sensor Measurements in an Older Australian Population: Before and during a Pandemic. Sensors 2021, 21, 5993. https://doi.org/10.3390/s21185993
Kholghi M, Ellender CM, Zhang Q, Gao Y, Higgins L, Karunanithi M. Home-Based Sleep Sensor Measurements in an Older Australian Population: Before and during a Pandemic. Sensors. 2021; 21(18):5993. https://doi.org/10.3390/s21185993
Chicago/Turabian StyleKholghi, Mahnoosh, Claire M. Ellender, Qing Zhang, Yang Gao, Liesel Higgins, and Mohanraj Karunanithi. 2021. "Home-Based Sleep Sensor Measurements in an Older Australian Population: Before and during a Pandemic" Sensors 21, no. 18: 5993. https://doi.org/10.3390/s21185993
APA StyleKholghi, M., Ellender, C. M., Zhang, Q., Gao, Y., Higgins, L., & Karunanithi, M. (2021). Home-Based Sleep Sensor Measurements in an Older Australian Population: Before and during a Pandemic. Sensors, 21(18), 5993. https://doi.org/10.3390/s21185993








