A Game-Based Rehabilitation System for Upper-Limb Cerebral Palsy: A Feasibility Study
Abstract
1. Introduction
2. Materials and Methods
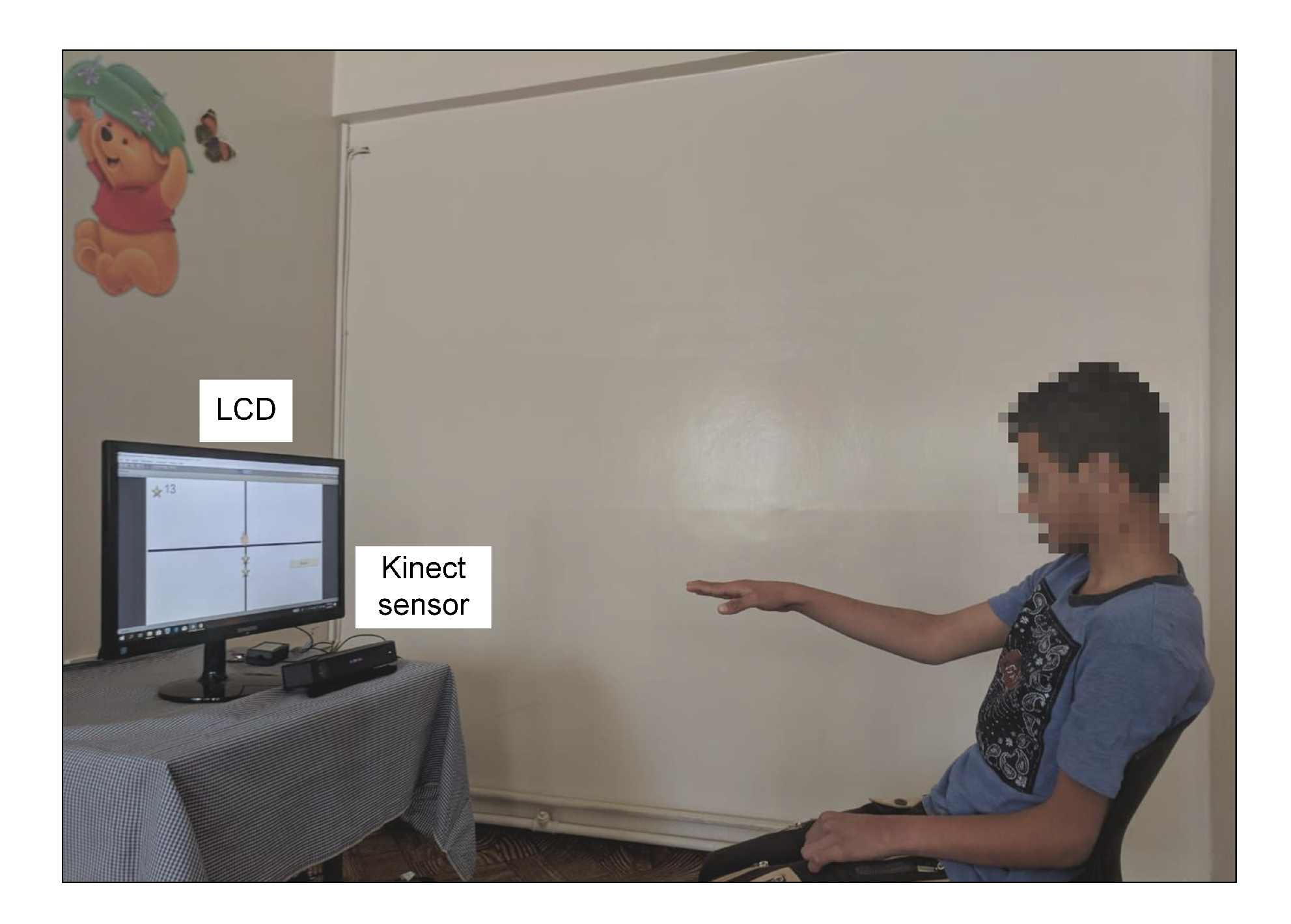
2.1. Overview of the Proposed Rehabilitation System
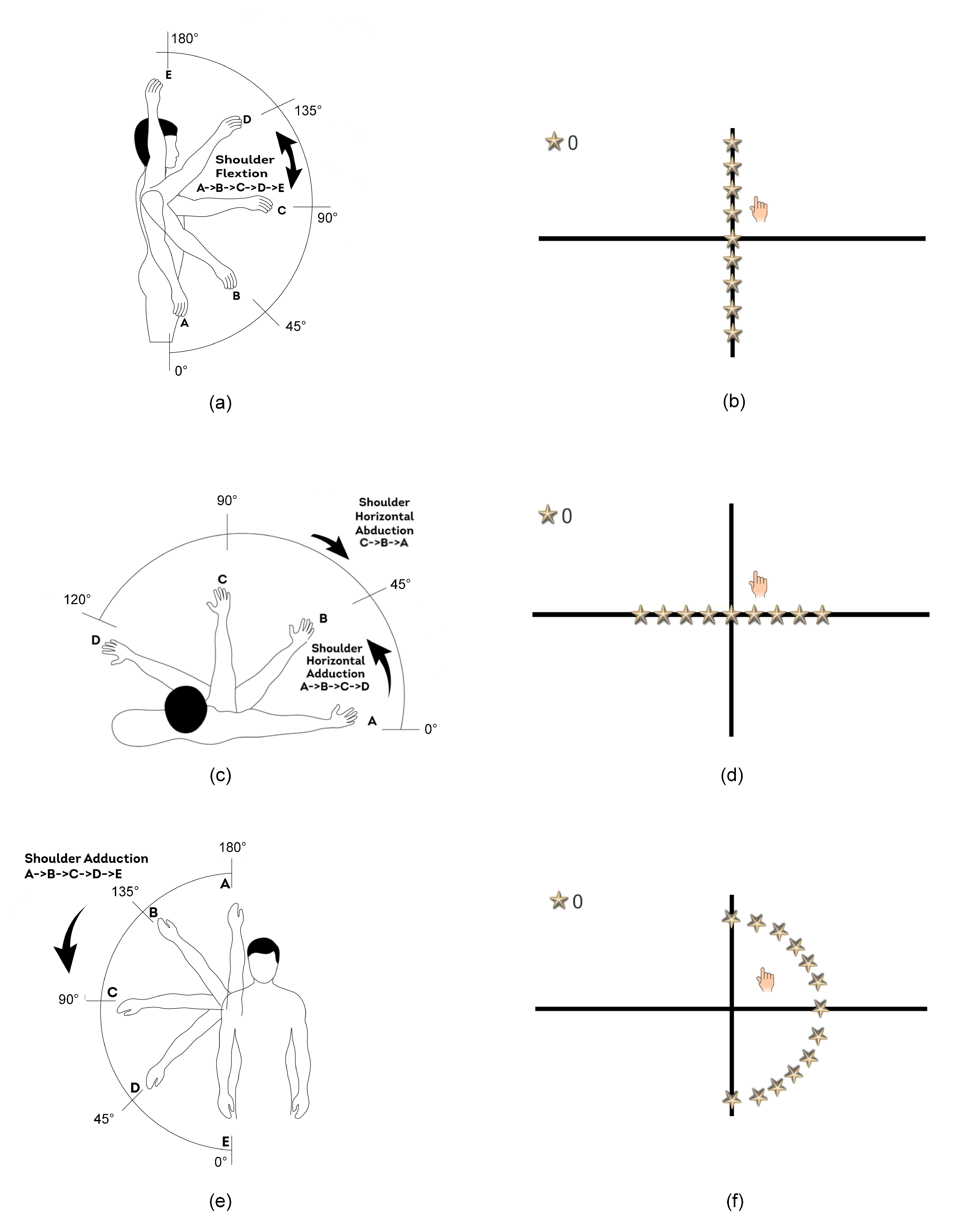
2.2. The Game-Based Rehabilitation Exercises
2.2.1. The Shoulder Flexion Game-Based Exercise
2.2.2. The Shoulder Horizontal Abduction/Adduction Game-Based Exercise
2.2.3. The Shoulder Adduction Game-Based Exercise
2.3. The Computerized Assessment Method
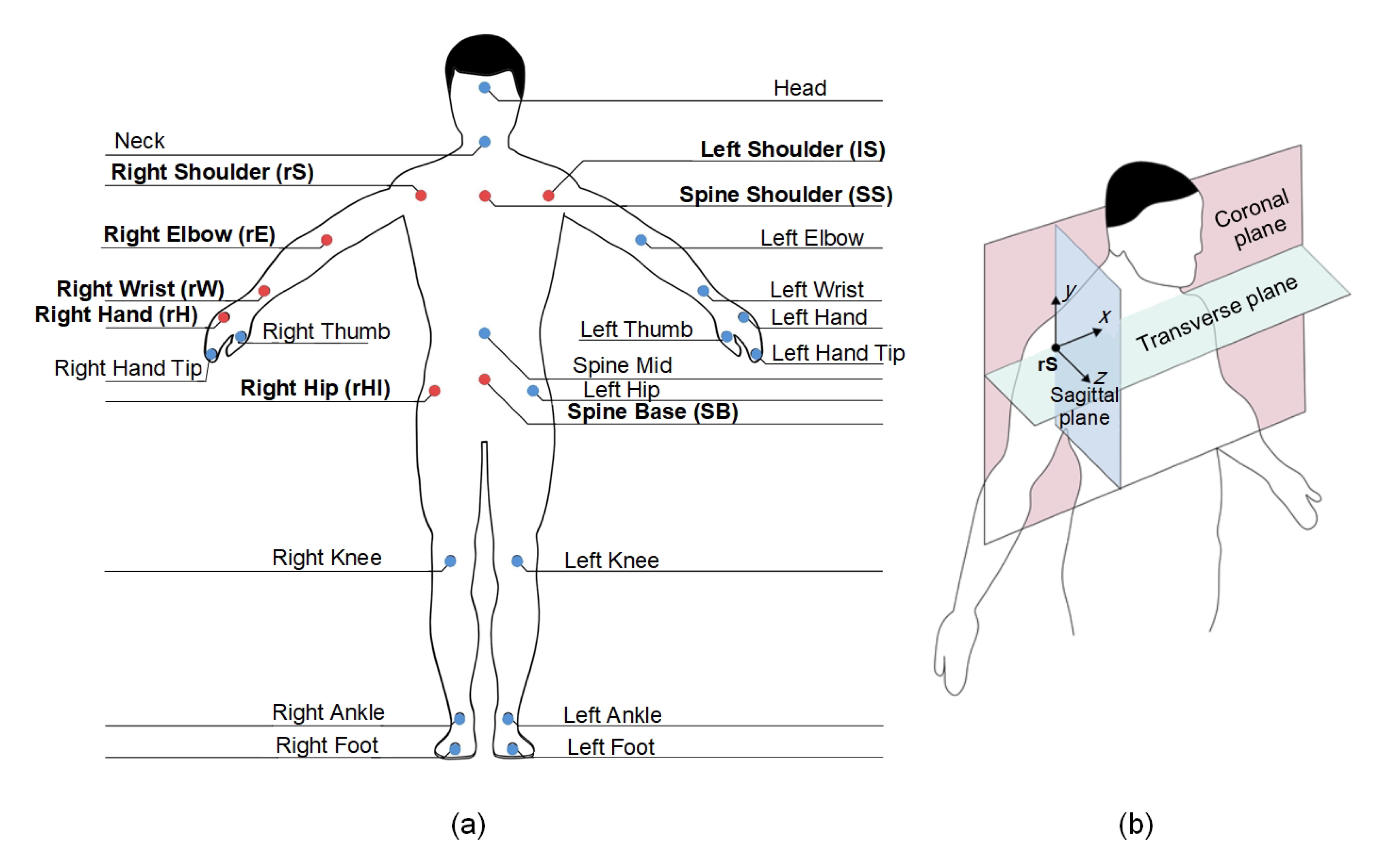
2.3.1. The Extended Motion-Pose Geometric Descriptor (E-MPGD)
E-MPGD: The Body-Attached Coordinate System
- The coronal plane (CP): This plane is defined using the rS, lS, and SB skeleton joints.
- The transverse plane (TP): This plane is defined using the rS and lS skeleton joints as well as the virtual joint. The virtual joint is obtained by shifting the SS skeleton joint along the direction orthogonal to the coronal plane, denoted by the positive z direction, by a distance of 0.2 m to ensure that the z coordinate of the joint is different than the rS and lS joints.
- The sagittal plane (SP): This plane is defined using the rS skeleton joint as well as the and virtual joints. The virtual joint is obtained by shifting the rS skeleton joint along the positive z direction by a distance of 0.2 m. The virtual joints is obtained by shifting the rS skeleton joint along the direction orthogonal to the transverse plane, denoted by the negative y direction, to match the y coordinate of the rHI joint.
E-MPGD: The Time-Varying Features
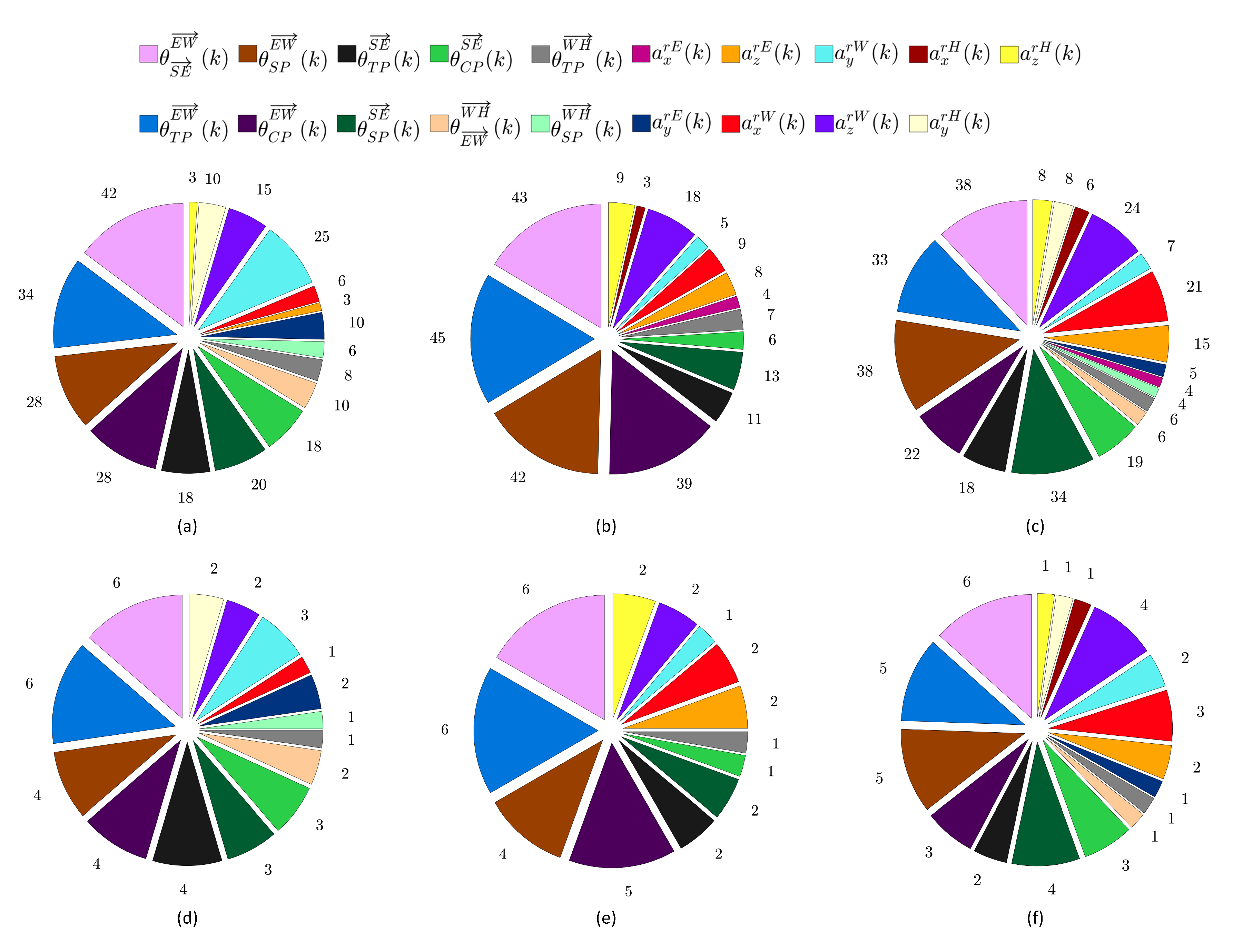
2.3.2. Features Extraction, Selection, and Classification
3. Experimental Evaluation and Results
3.1. Participants
3.2. Experimental Protocol
- •
- The participant should perform the movements associated with the game-based exercise, as described in Section 2.2 and illustrated in Figure 3, in a correct manner. In particular, compensatory movements should be avoided as much as possible.
- •
- The participant should cover the range of motion targeted by the game-based exercise, which is illustrated in Figure 3, as much as possible.
- •
- The participant should perform the movements associated with the game-based exercise slowly and in a controllable and stable manner in which the right arm is kept straight as much as possible.
3.3. Performance Evaluation
3.4. Results of the Cerebral Palsy Children
3.5. Results of the Typically Developing Subjects
4. Discussion and Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The Definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. 2007, 49, 8–14. [Google Scholar]
- Aisen, M.L.; Kerkovich, D.; Mast, J.; Mulroy, S.; Wren, T.A.; Kay, R.M.; Rethlefsen, S.A. Cerebral palsy: Clinical care and neurological rehabilitation. Lancet Neurol. 2011, 10, 844–852. [Google Scholar] [CrossRef]
- Cerebral Palsy Foundation. Key Facts. Available online: http://www.yourcpf.org/statistics/ (accessed on 23 January 2020).
- Eunson, P. Aetiology and epidemiology of cerebral palsy. Paediatr. Child Health 2016, 26, 367–372. [Google Scholar] [CrossRef]
- Cadwgan, J.; Goodwin, J.; Fairhurst, C. Fifteen-minute consultation: Modern-day art and science of managing cerebral palsy. Arch. Dis. Childhood Educ. Pract. 2019, 104, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Papavasiliou, A.S. Management of motor problems in cerebral palsy: A critical update for the clinician. Eur. J. Paediatr. Neurol. 2009, 13, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Lewis, G.N.; Rosie, J.A. Virtual reality games for movement rehabilitation in neurological conditions: How do we meet the needs and expectations of the users? Disabil. Rehabil. 2012, 34, 1880–1886. [Google Scholar] [CrossRef]
- Novak, I. Evidence-Based Diagnosis, Health Care, and Rehabilitation for Children With Cerebral Palsy. J. Child Neurol. 2014, 29, 1141–1156. [Google Scholar] [CrossRef]
- Green, D.; Wilson, P.H. Use of virtual reality in rehabilitation of movement in children with hemiplegia—A multiple case study evaluation. Disabil. Rehabil. 2012, 34, 593–604. [Google Scholar] [CrossRef]
- Zoccolillo, L.; Morelli, D.; Cincotti, F.; Muzzioli, L.; Gobbetti, T.; Paolucci, S.; Iosa, M. Video-game based therapy performed by children with cerebral palsy: A cross-over randomized controlled trial and a cross-sectional quantitative measure of physical activity. Eur. J. Phys. Rehabil. Med. 2015, 51, 669–676. [Google Scholar]
- Gordon, C.; Roopchand-Martin, S.; Gregg, A. Potential of the Nintendo WiiTM as a rehabilitation tool for children with cerebral palsy in a developing country: A pilot study. Physiotherapy 2012, 98, 238–242. [Google Scholar] [CrossRef]
- Chen, Y.; Fanchiang, H.D.; Howard, A. Effectiveness of virtual reality in children with cerebral palsy: A systematic review and meta-analysis of randomized controlled trials. Phys. Ther. 2018, 98, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Daoud, M.I.; Alazrai, R.; Alhusseini, A.; Shihan, D.; Alhwayan, E.; Abou-Tair, D.I.; Qadoummi, T. ICTs for Improving Patients Rehabilitation Research Techniques. In Communications in Computer and Information Science; Chapter Interactive Kinect-Based Rehabilitation Framework for Assisting Children with Upper Limb Cerebral Palsy; Springer: Cham, Switzerland, 2017. [Google Scholar]
- Daoud, M.I.; Qadoummi, T.; Abou-Tair, D.I. An interactive rehabilitation framework for assisting people with cerebral palsy. In Proceedings of the 3rd Workshop on ICTs for Improving Patients Rehabilitation Research Techniques (REHAB 15), Lisbon, Portugal, 1–2 October 2015; pp. 46–49. [Google Scholar]
- Chang, Y.J.; Han, W.Y.; Tsai, Y.C. A Kinect-based upper limb rehabilitation system to assist people with cerebral palsy. Res. Dev. Disabil. 2013, 34, 3654–3659. [Google Scholar] [CrossRef]
- Luna-Oliva, L.; Ortiz-Gutierrez, R.M.; Cano-de la Cuerda, R.; Piedrola, R.M.; Alguacil-Diego, I.M.; Sanchez-Camarero, C.; Martinez Culebras, M. Kinect Xbox 360 as a therapeutic modality for children with cerebral palsy in a school environment: A preliminary study. NeuroRehabilitation 2013, 33, 513–521. [Google Scholar] [CrossRef]
- Bryanton, C.; Bosse, J.; Brien, M.; Mclean, J.; McCormick, A.; Sveistrup, H. Feasibility, motivation, and selective motor control: Virtual reality compared to conventional home exercise in children with cerebral palsy. Cyberpsychol. Behav. 2006, 9, 123–128. [Google Scholar] [CrossRef]
- Bonnechere, B.; Jansen, B.; Omelina, L.; Da Silva, L.; Mougeat, J.; Heymans, V.; Vandeuren, A.; Rooze, M.; Van Sint Jan, S. Use of serious gaming to increase motivation of cerebral palsy children during rehabilitation. Eur. J. Paediatr. Neurol. 2013, 17, S12. [Google Scholar] [CrossRef]
- Hung, J.; Chang, Y.; Chou, C.; Wu, W.; Howell, S.; Lu, W. Developing a suite of motion-controlled games for upper extremity training in children with cerebral palsy: A proof-of-concept study. Games Health J. 2018, 7, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Jelsma, J.; Pronk, M.; Ferguson, G.; Jelsma-Smit, D. The effect of the Nintendo Wii Fit on balance control and gross motor function of children with spastic hemiplegic cerebral palsy. Dev. Neurorehabil. 2013, 16, 27–37. [Google Scholar] [CrossRef]
- Winkels, D.G.M.; Kottink, A.I.R.; Temmink, R.A.J.; Nijlant, J.M.M.; Buurke, J.H. WiiTM-habilitation of upper extremity function in children with cerebral palsy. An explorative study. Dev. Neurorehabil. 2013, 16, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Sevick, M.; Eklund, E.; Mensch, A.; Foreman, M.; Standeven, J.; Engsberg, J. Using free internet videogames in upper extremity motor training for children with cerebral palsy. Behav. Sci. 2016, 6, 10. [Google Scholar] [CrossRef]
- Machado, F.R.C.; Antunes, P.P.; Souza, J.; Dos Santos, A.C.; Levandowski, D.C.; De Oliveira, A.A. Motor improvement using motion sensing game devices for cerebral palsy rehabilitation. J. Motor Behav. 2017, 49, 273–280. [Google Scholar] [CrossRef]
- Sandlund, M.; Domellof, E.; Grip, H.; Ronnqvist, L.; Hager, C.K. Training of goal directed arm movements with motion interactive video games in children with cerebral palsy—A kinematic evaluation. Dev. Neurorehabil. 2014, 17, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Ayed, I.; Ghazel, A.; Jaume-I-Capo, A.; Moyà-Alcover, G.; Varona, J.; Martínez-Bueso, O. Vision-based serious games and virtual reality systems for motor rehabilitation: A review geared toward a research methodology. Int. J. Med. Inform. 2019, 131, 103909. [Google Scholar] [CrossRef] [PubMed]
- Huber, M.; Rabin, B.; Docan, C.; Burdea, G.; Nwosu, M.E.; Abdelbaky, M.; Golomb, M.R. PlayStation 3-based tele-rehabilitation for children with hemiplegia. In Proceedings of the 2008 Virtual Rehabilitation Conference, Vancouver, BC, Canada, 25–27 August 2008; pp. 105–112. [Google Scholar]
- Roy, A.K.; Soni, Y.; Dubey, S. Enhancing effectiveness of motor rehabilitation using kinect motion sensing technology. In Proceedings of the IEEE Global Humanitarian Technology Conference: South Asia Satellite (GHTC-SAS), Trivandrum, India, 23–24 August 2013; pp. 298–304. [Google Scholar]
- Sinpithakkul, C.; Kusakunniran, W.; Bovonsunthonchai, S.; Wattananon, P. Game-based enhancement for rehabilitation based on action recognition using kinect. In Proceedings of the IEEE Region 10 Conference (TENCON 2018), Jeju, Korea, 28–31 Octorber 2018; pp. 303–308. [Google Scholar]
- Vilas-Boas, M.D.C.; Choupina, H.M.P.; Rocha, A.P.; Fernandes, J.M.; Cunha, J.P.S. Full-body motion assessment: Concurrent validation of two body tracking depth sensors versus a gold standard system during gait. J. Biomech. 2019, 87, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Alazrai, R.; Mowafi, Y.; Lee, G. Anatomical-plane-based representation for human-human interactions analysis. Pattern Recognit. 2015, 48, 2346–2363. [Google Scholar] [CrossRef]
- Alazrai, R.; Momani, M.; Daoud, M.I. Fall detection for elderly from partially observed depth-map video sequences based on view-invariant human activity representation. Appl. Sci. 2017, 7, 316. [Google Scholar] [CrossRef]
- Alazrai, R.; Mowafi, Y.; Hamad, E. A fall prediction methodology for elderly based on a depth camera. In Proceedings of the 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 4990–4993. [Google Scholar]
- Snell, R.S. Clinical Anatomy by Regions, 9th ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2011. [Google Scholar]
- Wöllmer, M.; Al-Hames, M.; Eyben, F.; Schuller, B.; Rigoll, G. A multidimensional dynamic time warping algorithm for efficient multimodal fusion of asynchronous data streams. Neurocomputing 2009, 73, 366–380. [Google Scholar] [CrossRef]
- Guyon, I.; Weston, J.; Barnhill, S.; Vapnik, V. Gene selection for cancer classification using support vector machines. Mach. Learn. 2002, 46, 389–422. [Google Scholar] [CrossRef]
- Han, J.; Kamber, M.; Pei, J. Data Mining: Concepts and Techniques, 3rd ed.; Elsevier: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Sim, J.; Wright, C.C. The kappa statistic in reliability studies: Use, interpretation, and sample size requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef]
- Cohen, J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960, 20, 37–46. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Cameron, M.H.; Monroe, L. Physical Rehabilitation for the Physical Therapist Assistant; Elsevier: Amsterdam, The Netherlands, 2011. [Google Scholar]
- DeMatteo, C.; Law, M.; Russell, D.; Pollock, N.; Rosenbaum, P.; Walter, S. The reliability and validity of the quality of upper extremity skills test. Phys. Occup. Ther. Pediatr. 1993, 13, 1–18. [Google Scholar] [CrossRef]
- Mathiowetz, V.; Federman, S.; Wiemer, D. Box and block test of manual dexterity: Norms for 6–19 year olds. Can. J. Occup. Ther. 1985, 52, 241–245. [Google Scholar] [CrossRef]
- Randall, M.; Johnson, L.; Reddihough, D. The Melbourne Assessment of Unilateral Upper Limb Function: Test Administration Manual; Royal Children’s Hospital: Melbourne, Australia, 1999. [Google Scholar]
- Arnould, C.; Penta, M.; Renders, A.; Thonnard, J. ABILHAND-Kids: A measure of manual ability in children with cerebral palsy. Neurology 2004, 63, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Acar, G.; Altun, G.P.; Yurdalan, S.; Polat, M.G. Efficacy of neurodevelopmental treatment combined with the Nintendo© Wii in patients with cerebral palsy. J. Phys. Ther. Sci. 2016, 28, 774–780. [Google Scholar] [CrossRef]
- Jebsen, R.H.; Taylor, N.; Trieschmann, R.B.; Trotter, M.J.; Howard, L.A. An objective and standardized test of hand function. Arch. Phys. Med. Rehabil. 1969, 50, 311–319. [Google Scholar]
- Msall, M.E.; DiGaudio, K.; Duffy, L.C.; LaForest, S.; Braun, S.; Granger, C.V. WeeFIM: Normative sample of an instrument for tracking functional independence in children. Clin. Pediatr. 1994, 33, 431–438. [Google Scholar] [CrossRef]
- Ding, W.L.; Zheng, Y.Z.; Su, Y.P.; Li, X.L. Kinect-based virtual rehabilitation and evaluation system for upper limb disorders: A case study. J. Back Musculoskel. Rehabil. 2018, 31, 611–621. [Google Scholar] [CrossRef]
- Gaillard, F.; Cacioppo, M.; Bouvier, B.; Bouzille, G.; Newman, C.J.; Pasquet, T.; Cretual, A.; Rauscent, H.; Bonan, I. Assessment of bimanual performance in 3-D movement analysis: Validation of a new clinical protocol in children with unilateral cerebral palsy. Ann. Phys. Rehabil. Med. in Press. [CrossRef]


| Type | Features | Description | Mathematical Formulation |
|---|---|---|---|
| Angle-based features | , , | The angles between the vector and the CP, TP, and SP at frame k. | , where is the angle between the vector and the plane P at frame k, and is the normal vector to the plane P. |
| , , | The angles between the vector and the CP, TP, and SP at frame k. | ||
| , , | The angles between the vector and the CP, TP, and SP at frame k. | ||
| The angle between the vectors and at frame k. | , where is the angle between the vectors and at frame k. | ||
| The angle between the vectors and at frame k. | |||
| Joint-based features | , , | The x, y, and z components of the rE joint velocity at frame k. | The locations of the rE. rW, and rH skeleton joints at frame k are provided by the Kinect sensor and transformed to the body-attached coordinate system. |
| , , | The x, y, and z components of the rW joint location at frame k. | ||
| , , | The x, y, and z components of the rH joint location at frame k. | ||
| , , | The x, y, and z components of the rE joint velocity at frame k. | , where is the velocity of skeleton joint p along direction d at frame k, and are the locations of p along direction d at frames k and , respectively, and is the time step between frames k and . | |
| , , | The x, y, and z components of the rW joint velocity at frame k. | ||
| , , | The x, y, and z components of the rH joint velocity at frame k. | ||
| , , | The x, y, and z components of the rE joint acceleration at frame k. | , where is the acceleration of skeleton joint p along direction d at frame k, and are the velocities of p along direction d at frames k and , respectively, and is the time step between frames k and . | |
| , , | The x, y, and z components of the rW joint acceleration at frame k. | ||
| , , | The x, y, and z components of the rH joint acceleration at frame k. |
| Participant | Gender | Cerebral Palsy | Cerebral Palsy |
|---|---|---|---|
| Category | Severity | ||
| Child 1 | Male | Spastic diplegic | Mild |
| Child 2 | Male | Spastic diplegic | Mild |
| Child 3 | Female | Spastic diplegic | Moderate |
| Child 4 | Male | Spastic himiplegic | Moderate |
| Child 5 | Female | Ataxia | Moderate |
| Child 6 | Male | Ataxia | Moderate |
| Participant | Shoulder Flexion | Shoulder Horizontal Abduction/Adduction | Shoulder Adduction | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Accuracy | Specificity | Sensitivity | Kappa | Accuracy | Specificity | Sensitivity | Kappa | Accuracy | Specificity | Sensitivity | Kappa | |
| (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | ||||
| Child 1 | 93 ± 3 | 91 ± 4 | 95 ± 3 | 0.86 ± 0.06 | 92 ± 4 | 91 ± 4 | 92 ± 5 | 0.83 ± 0.07 | 90 ± 4 | 89 ± 6 | 90 ± 4 | 0.80 ± 0.09 |
| Child 2 | 91 ± 3 | 90 ± 4 | 91 ± 5 | 0.81 ± 0.05 | 92 ± 3 | 93 ± 3 | 91 ± 4 | 0.84 ± 0.05 | 90 ± 3 | 88 ± 4 | 92 ± 6 | 0.81 ± 0.07 |
| Child 3 | 87 ± 4 | 87 ± 6 | 88 ± 3 | 0.74 ± 0.07 | 86 ± 3 | 85 ± 5 | 87 ± 5 | 0.72 ± 0.06 | 86 ± 2 | 87 ± 3 | 84 ± 4 | 0.72 ± 0.05 |
| Child 4 | 85 ± 3 | 86 ± 5 | 84 ± 4 | 0.70 ± 0.06 | 87 ± 4 | 88 ± 5 | 85 ± 4 | 0.73 ± 0.07 | 85 ± 4 | 85 ± 5 | 86 ± 6 | 0.71 ± 0.09 |
| Child 5 | 78 ± 4 | 80 ± 6 | 76 ± 5 | 0.57 ± 0.08 | 77 ± 4 | 79 ± 5 | 75 ± 5 | 0.54 ± 0.08 | 72 ± 4 | 73 ± 5 | 71 ± 6 | 0.45 ± 0.07 |
| Child 6 | 75 ± 3 | 78 ± 4 | 73 ± 4 | 0.51 ± 0.06 | 76 ± 3 | 80 ± 4 | 73 ± 4 | 0.53 ± 0.06 | 73 ± 2 | 73 ± 4 | 72 ± 3 | 0.46 ± 0.05 |
| All children | 85 ± 7 | 85 ± 7 | 84 ± 9 | 0.70 ± 0.14 | 85 ± 7 | 86 ± 7 | 84 ± 9 | 0.70 ± 0.14 | 83 ± 8 | 83 ± 8 | 83 ± 10 | 0.66 ± 0.16 |
| Participant | Shoulder Flexion | Shoulder Horizontal Abduction/Adduction | Shoulder Adduction | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Accuracy | Specificity | Sensitivity | Kappa | Accuracy | Specificity | Sensitivity | Kappa | Accuracy | Specificity | Sensitivity | Kappa | |
| (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | ||||
| Subject 1 | 98 ± 2 | 98 ± 2 | 98 ± 2 | 0.96 ± 0.03 | 98 ± 2 | 99 ± 2 | 98 ± 2 | 0.97 ± 0.03 | 97 ± 2 | 98 ± 2 | 97 ± 3 | 0.95 ± 0.04 |
| Subject 2 | 98 ± 2 | 98 ± 2 | 97 ± 3 | 0.96 ± 0.04 | 99 ± 1 | 99 ± 1 | 99 ± 1 | 0.99 ± 0.03 | 98 ± 2 | 97 ± 2 | 99 ± 2 | 0.96 ± 0.03 |
| Subject 3 | 99 ± 1 | 99 ± 1 | 99 ± 2 | 0.98 ± 0.03 | 99 ± 1 | 99 ± 1 | 99 ± 2 | 0.98 ± 0.03 | 99 ± 1 | 99 ± 1 | 99 ± 1 | 0.99 ± 0.02 |
| Subject 4 | 98 ± 2 | 98 ± 2 | 98 ± 2 | 0.97 ± 0.04 | 99 ± 1 | 99 ± 2 | 99 ± 1 | 0.98 ± 0.03 | 98 ± 2 | 97 ± 3 | 98 ± 3 | 0.95 ± 0.04 |
| Subject 5 | 98 ± 2 | 97 ± 3 | 99 ± 2 | 0.96 ± 0.05 | 98 ± 1 | 98 ± 2 | 98 ± 3 | 0.95 ± 0.03 | 97 ± 2 | 97 ± 2 | 97 ± 2 | 0.94 ± 0.03 |
| Subject 6 | 98 ± 2 | 99 ± 2 | 98 ± 3 | 0.96 ± 0.05 | 98 ± 2 | 98 ± 2 | 98 ± 2 | 0.96 ± 0.04 | 97 ± 1 | 97 ± 2 | 98 ± 2 | 0.95 ± 0.03 |
| Subject 7 | 99 ± 2 | 98 ± 3 | 99 ± 2 | 0.97 ± 0.04 | 99 ± 2 | 99 ± 2 | 99 ± 2 | 0.98 ± 0.03 | 98 ± 2 | 98 ± 2 | 97 ± 3 | 0.95 ± 0.05 |
| Subject 8 | 99 ± 1 | 99 ± 1 | 99 ± 1 | 0.99 ± 0.03 | 99 ± 2 | 99 ± 2 | 98 ± 2 | 0.97 ± 0.04 | 97 ± 3 | 97 ± 3 | 98 ± 3 | 0.95 ± 0.06 |
| Subject 9 | 98 ± 3 | 97 ± 3 | 98 ± 2 | 0.95 ± 0.05 | 97 ± 2 | 97 ± 3 | 97 ± 2 | 0.94 ± 0.04 | 97 ± 3 | 96 ± 3 | 97 ± 3 | 0.94 ±0.06 |
| Subject 10 | 97 ± 3 | 98 ± 2 | 97 ± 3 | 0.95 ± 0.05 | 97 ± 3 | 97 ± 2 | 97 ± 3 | 0.94 ± 0.05 | 97 ± 1 | 96 ± 2 | 97 ± 2 | 0.93 ± 0.02 |
| Subject 11 | 98 ± 2 | 99 ± 2 | 97 ± 3 | 0.96 ± 0.04 | 98 ± 1 | 97 ± 2 | 98 ± 2 | 0.95 ± 0.03 | 97 ± 2 | 97 ± 2 | 97 ± 3 | 0.94 ± 0.04 |
| Subject 12 | 99 ± 2 | 99 ± 1 | 98 ± 2 | 0.98 ± 0.04 | 99 ± 2 | 98 ± 3 | 99 ± 1 | 0.97 ± 0.04 | 98 ± 2 | 97 ± 3 | 98 ± 2 | 0.95 ± 0.04 |
| Subject 13 | 98 ± 3 | 97 ± 3 | 98 ± 3 | 0.95 ± 0.05 | 98 ± 2 | 98 ± 2 | 97 ± 2 | 0.95 ± 0.04 | 97 ± 2 | 97 ± 3 | 97 ± 3 | 0.94 ± 0.05 |
| Subject 14 | 98 ± 1 | 98 ± 2 | 99 ± 2 | 0.96 ± 0.02 | 98 ± 2 | 99 ± 2 | 98 ± 2 | 0.97 ± 0.03 | 98 ± 2 | 98 ± 2 | 98 ± 3 | 0.96 ± 0.04 |
| Subject 15 | 97 ± 2 | 97 ± 3 | 97 ± 2 | 0.95 ± 0.04 | 98 ± 2 | 98 ± 2 | 98 ± 3 | 0.96 ± 0.05 | 98± 2 | 97 ± 3 | 98 ± 2 | 0.95 ± 0.05 |
| Subject 16 | 99 ± 1 | 99 ± 2 | 98 ± 2 | 0.97 ± 0.03 | 98 ± 1 | 99 ± 2 | 98 ± 2 | 0.96 ± 0.02 | 98 ± 1 | 98 ± 2 | 98 ± 2 | 0.96 ± 0.03 |
| Subject 17 | 98 ± 2 | 99 ± 2 | 98 ± 3 | 0.97 ± 0.04 | 99 ± 1 | 99 ± 2 | 99 ± 1 | 0.98 ± 0.02 | 98 ± 2 | 97 ± 2 | 98 ± 3 | 0.95 ± 0.04 |
| Subject 18 | 96 ± 2 | 97 ±3 | 96 ± 3 | 0.93 ± 0.05 | 98 ± 2 | 97 ± 3 | 98 ± 2 | 0.95 ± 0.05 | 96 ± 2 | 97 ± 3 | 96 ± 3 | 0.93 ± 0.05 |
| Subject 19 | 97 ± 3 | 97 ± 3 | 96 ± 3 | 0.94 ± 0.06 | 97 ± 2 | 97 ± 3 | 97± 3 | 0.94 ± 0.05 | 96 ± 2 | 97 ± 2 | 96 ± 3 | 0.93 ± 0.03 |
| Subject 20 | 98 ± 1 | 98 ± 2 | 97 ± 2 | 0.95 ± 0.03 | 98 ± 3 | 98 ± 3 | 97 ± 4 | 0.95 ± 0.06 | 97 ± 2 | 97 ± 2 | 97 ± 3 | 0.93 ± 0.04 |
| All subjects | 98 ± 2 | 98 ± 2 | 98 ± 3 | 0.96 ± 0.04 | 98 ± 2 | 98 ± 2 | 98 ± 2 | 0.96 ± 0.04 | 97 ± 2 | 97 ± 2 | 97 ± 3 | 0.95 ± 0.04 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Daoud, M.I.; Alhusseini, A.; Ali, M.Z.; Alazrai, R. A Game-Based Rehabilitation System for Upper-Limb Cerebral Palsy: A Feasibility Study. Sensors 2020, 20, 2416. https://doi.org/10.3390/s20082416
Daoud MI, Alhusseini A, Ali MZ, Alazrai R. A Game-Based Rehabilitation System for Upper-Limb Cerebral Palsy: A Feasibility Study. Sensors. 2020; 20(8):2416. https://doi.org/10.3390/s20082416
Chicago/Turabian StyleDaoud, Mohammad I., Abdullah Alhusseini, Mostafa Z. Ali, and Rami Alazrai. 2020. "A Game-Based Rehabilitation System for Upper-Limb Cerebral Palsy: A Feasibility Study" Sensors 20, no. 8: 2416. https://doi.org/10.3390/s20082416
APA StyleDaoud, M. I., Alhusseini, A., Ali, M. Z., & Alazrai, R. (2020). A Game-Based Rehabilitation System for Upper-Limb Cerebral Palsy: A Feasibility Study. Sensors, 20(8), 2416. https://doi.org/10.3390/s20082416





