Synthetic Aperture Radar Imaging for Burn Wounds Diagnostics
Abstract
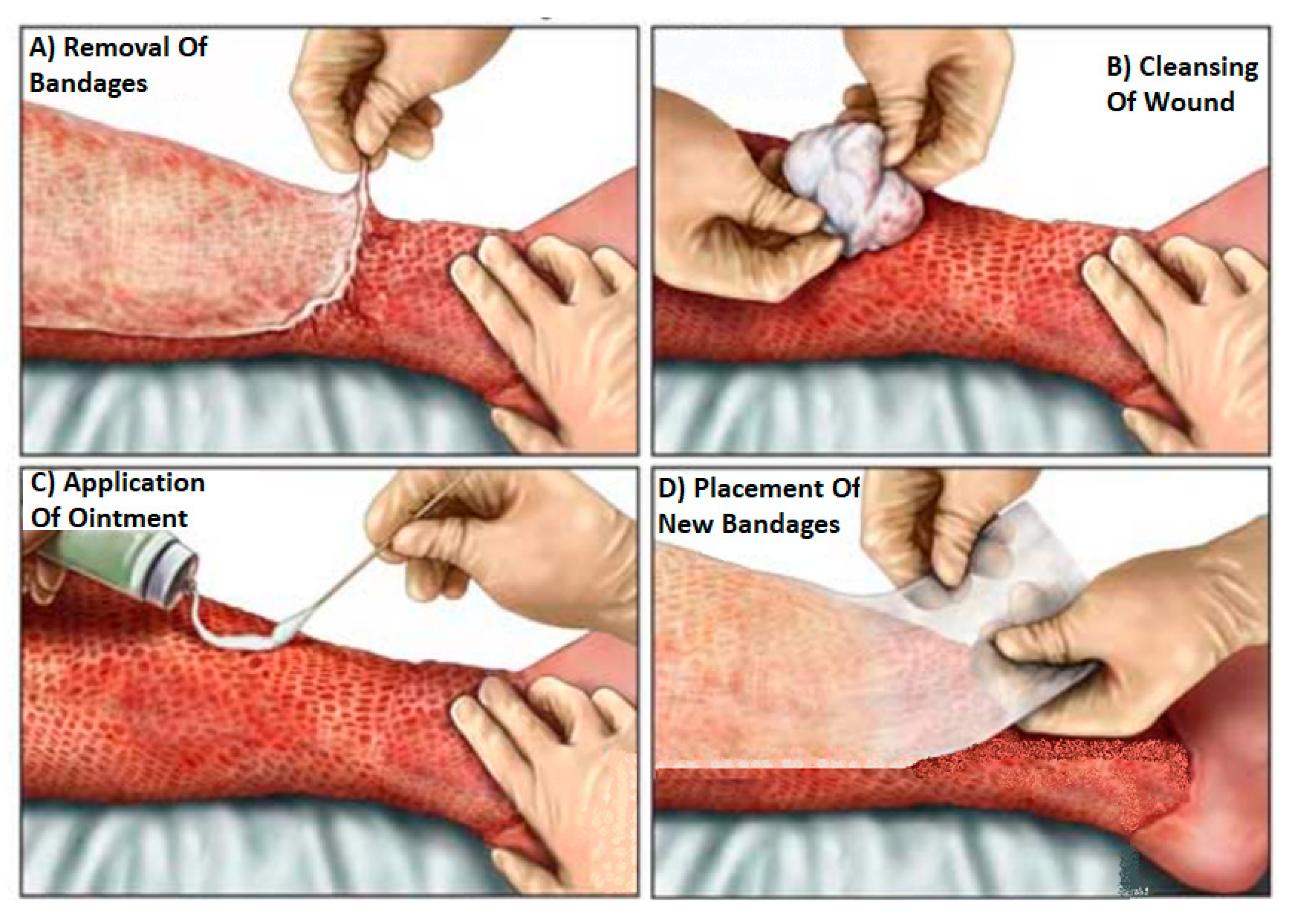
1. Introduction
2. Materials and Methods
2.1. Porcine Skin Samples
2.2. Selection of Frequency Band
2.3. Experimental Setup
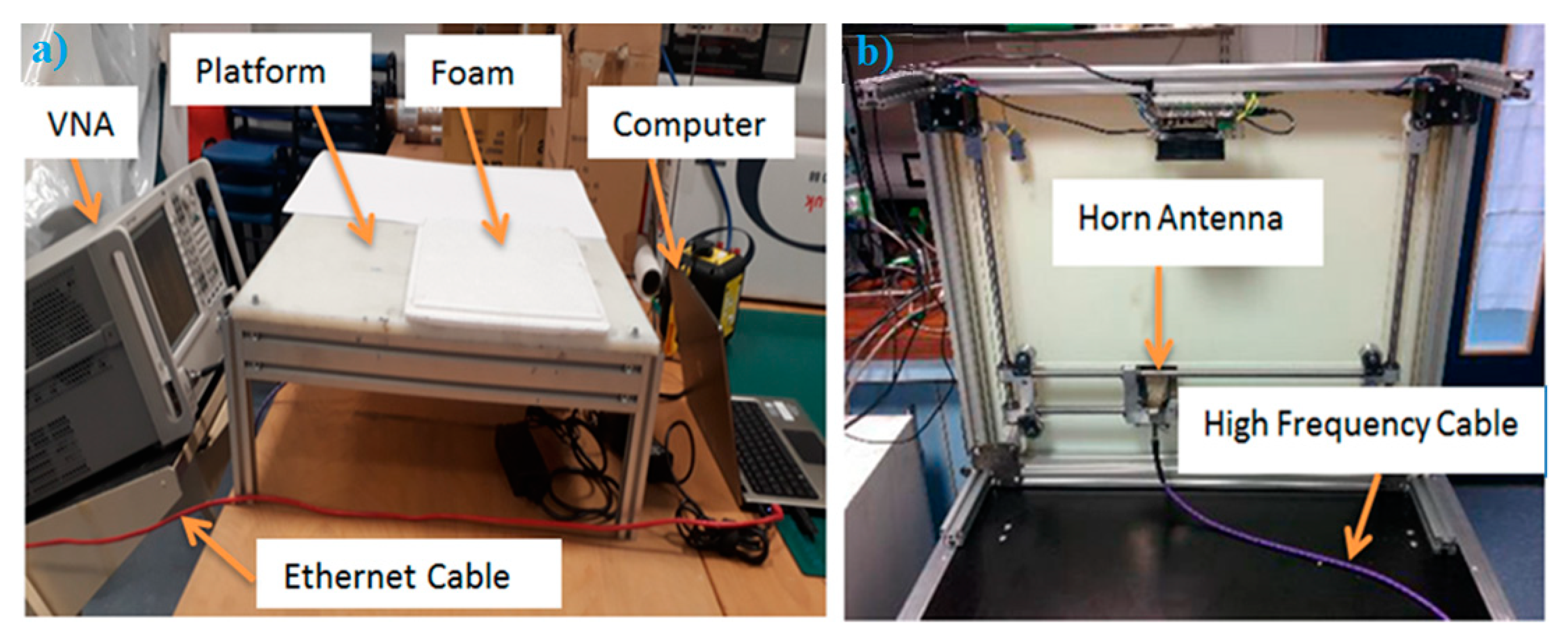
2.4. Methodology of Scanning Images
2.5. Synthetic Aperture Radar Algorithim
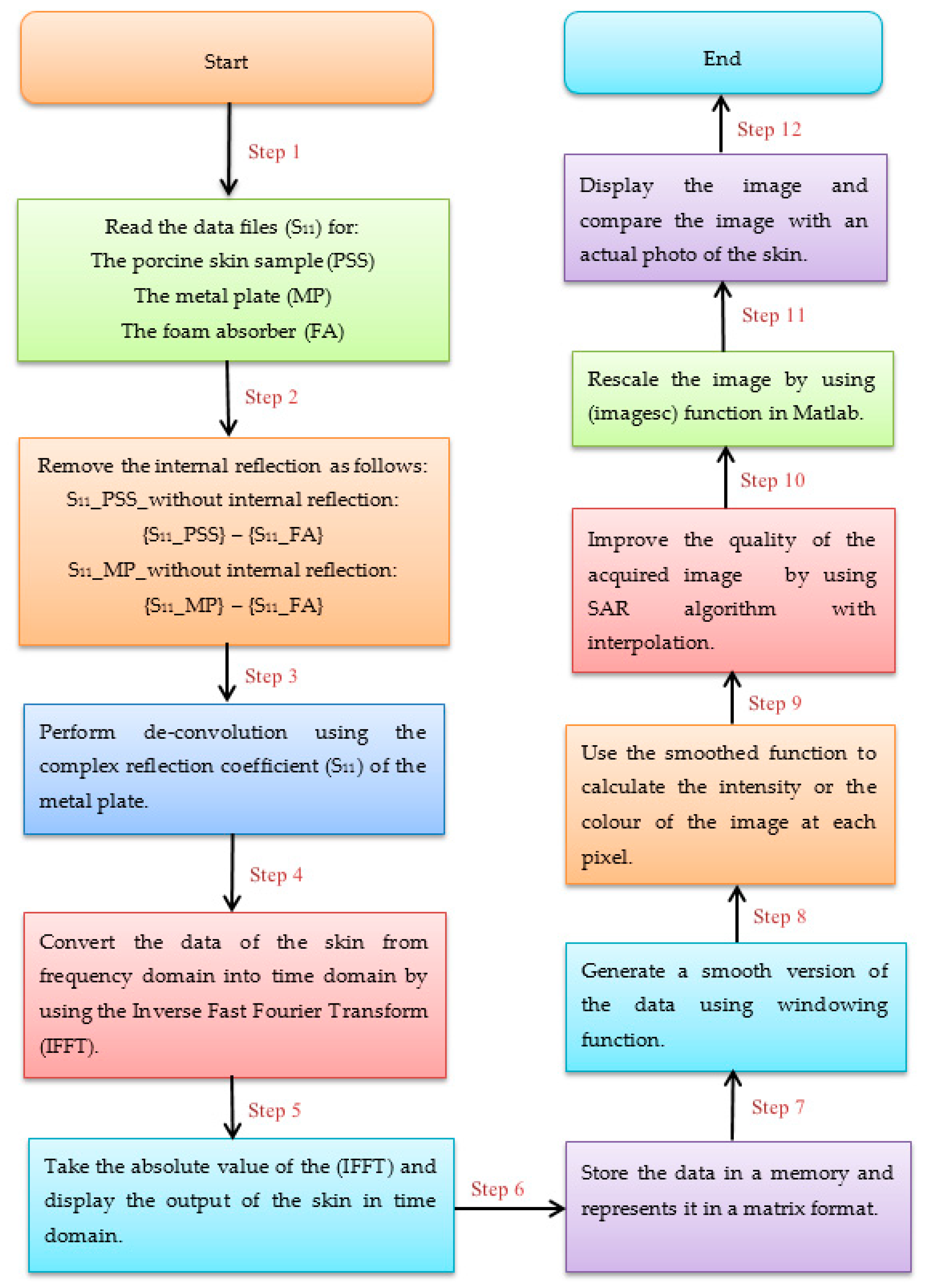
2.6. Methodology of Data Processing
2.7. Methodology of Identifying Artefacts
3. Experimental Results
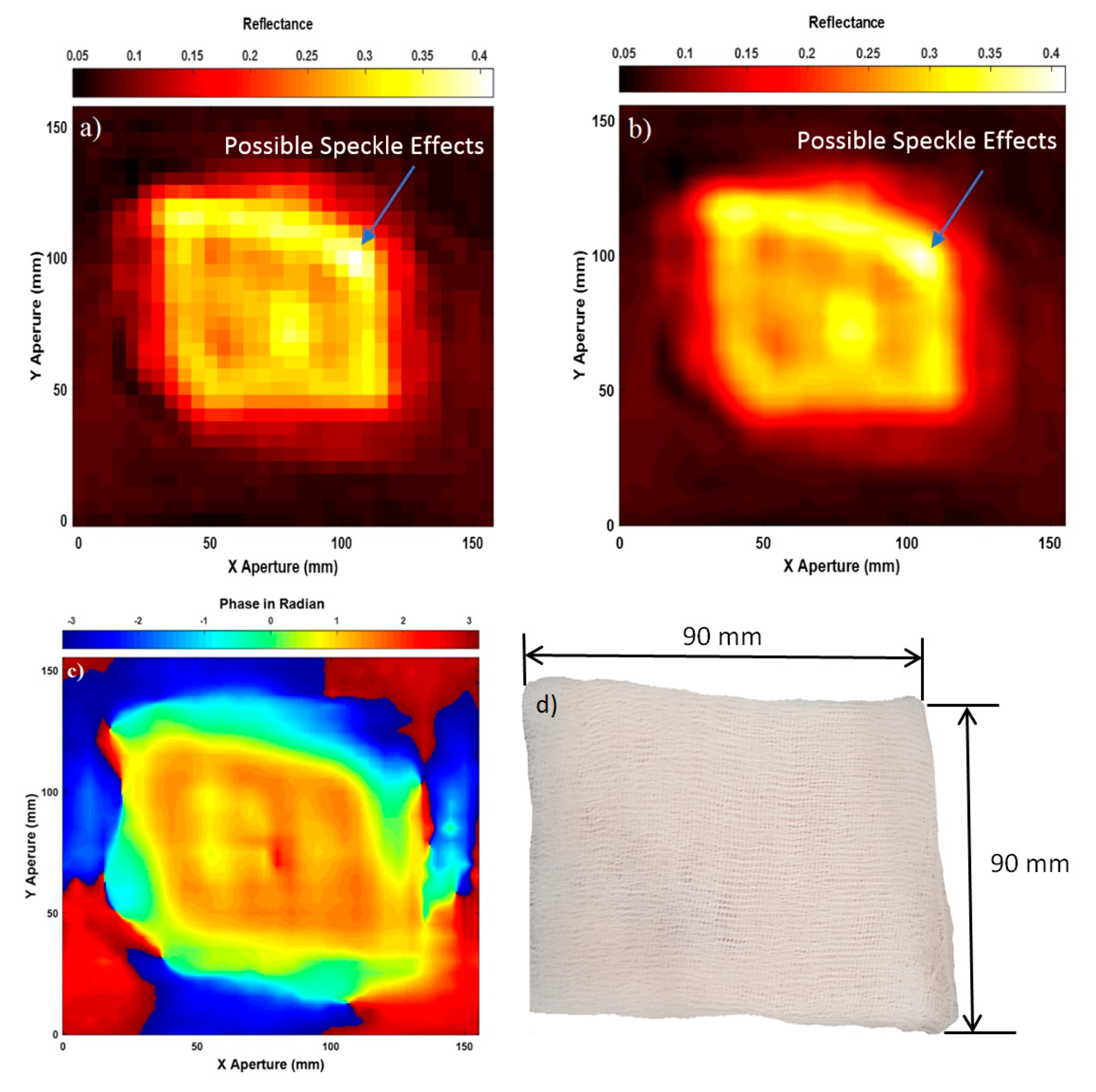
3.1. Images for the Skin without Burns
3.2. Images for the Skin with Dressing Materials
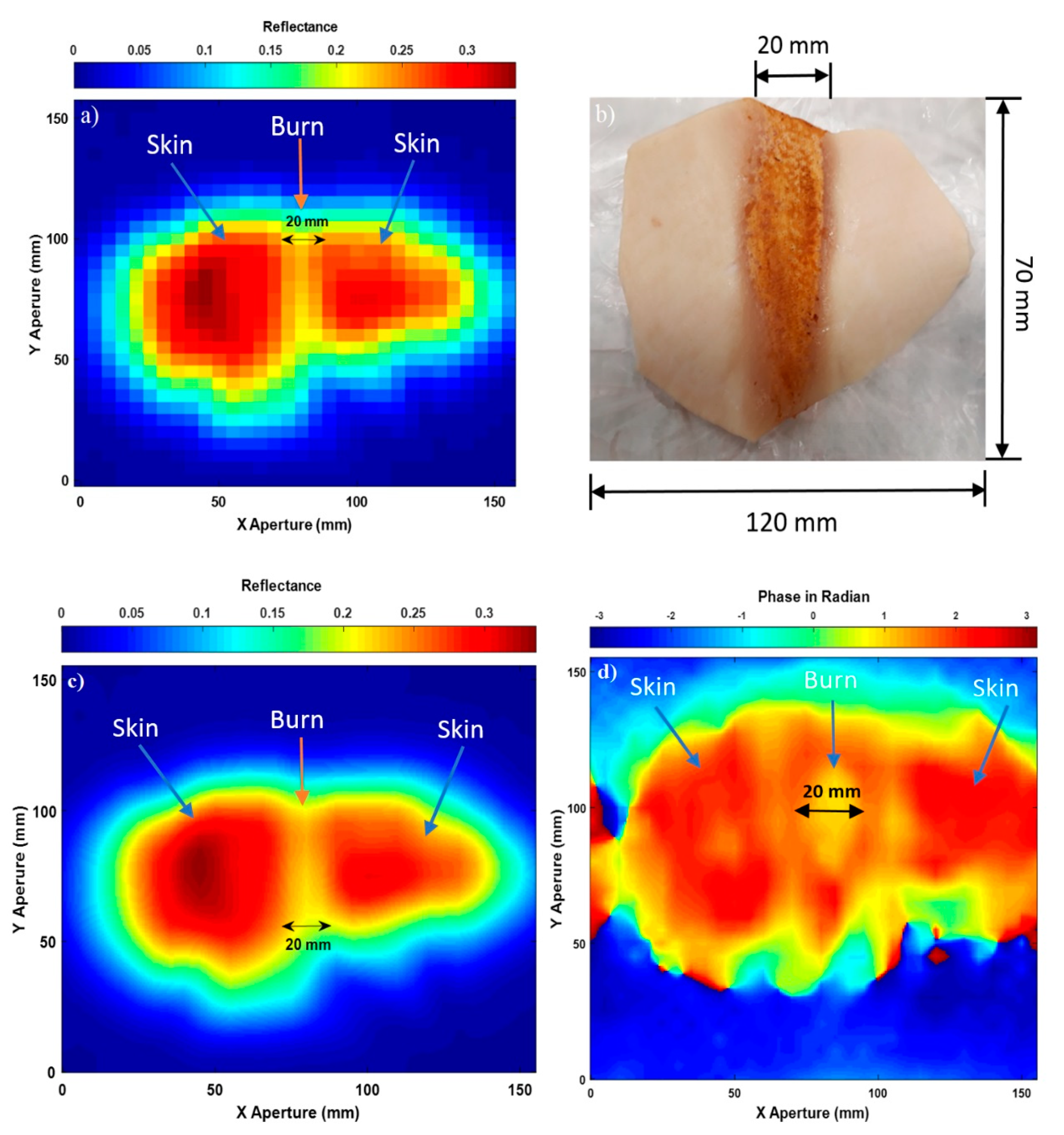
3.3. Images for the Skin with Burns
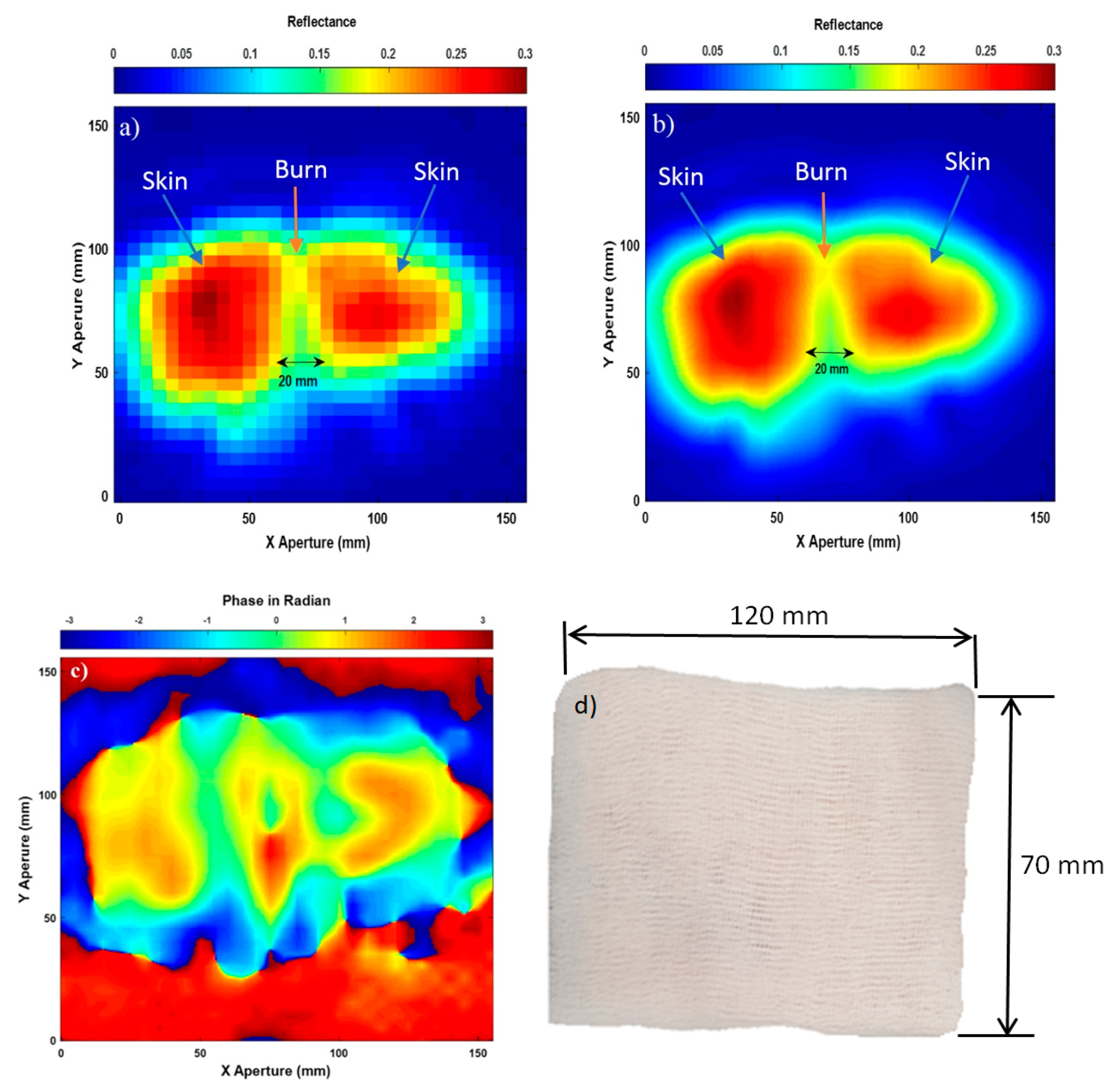
3.4. Images for the Skin with Burns and Dressing Materials
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- The Child Accident Prevention Trust. The Costs of Burns. August 2013. Available online: http://www.makingthelink.net/tools/costs-child-accidents/costs-burns. (accessed on 24 December 2019).
- Harmer, S.W.; Shylo, S.; Shah, M.; Bowring, N.J.; Owda, A.Y. On the feasibility of assessing burn wound healing without removal of dressings using radiometric millimetre-wave sensing. Prog. Electromagn. Res. M 2016, 45, 173–183. [Google Scholar] [CrossRef]
- Seia, Z.; Musso, L.; Palazzini, S.; Bertero, M. Skin Biopsy Procedures: How and Where to Perform a Proper Biopsy, Skin Biopsy-Perspectives. In Skin Biopsy; Intech: Shanghai, China, 2011; pp. 1–18. [Google Scholar]
- Tewari, P.; Bajwa, N.; Singh, R.S.; Culjat, M.O.; Grundgest, W.S. In vivo terahertz imaging of rat skin burns. J. Biomed. Opt. 2012, 17, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Taylor, Z.D.; Singh, R.S.; Bennett, D.B.; Tewari, P.; Kealey, C.P.; Bajwa, N.; Culjat, M.O.; Stojadinovic, A.; Lee, H.; Hubschman, J.-P.; et al. THz Medical Imaging: In vivo Hydration Sensing. IEEE Trans. Terahertz Sci. Technol. 2011, 1, 201–219. [Google Scholar] [CrossRef] [PubMed]
- Arbab, M.H.; Winebrenner, D.P.; Dickey, T.C.; Chen, A.; Klein, M.B.; Mourad, P.D. Terahertz spectroscopy for the assessment of burn injuries in vivo. J. Biomed. Opt. 2013, 18, 1–7. [Google Scholar] [CrossRef]
- Arbab, M.H.; Dickey, T.C.; Winebrenner, D.P.; Chen, A.; Klein, M.B.; Mourad, P.D. Terahertz reflectometry of burn wounds in a rat model. Biomed. Opt. Express 2011, 2, 2339–2347. [Google Scholar] [CrossRef]
- Zhao, Y.; Maher, J.R.; Kim, J.; Selim, M.A.; Levinson, H.; Wax, A. Evaluation of burn severity in vivo in a mouse model using spectroscopic optical coherence tomography. Biomed. Opt. Express 2015, 6, 3339–3345. [Google Scholar] [CrossRef]
- Srinivas, S.M.; de Boer, J.F.; Park, H.; Keikhanzadeh, K.; Huang, H.-E.L.; Zhang, J.; Jung, W.G.; Chen, Z.; Nelson, J.S. Determination of burn depth by polarization-sensitive optical coherence tomography. J. Biomed. Opt. 2004, 9, 207–212. [Google Scholar] [CrossRef]
- Park, B.H.; Saxer, C.; Srinivas, S.M.; Nelson, J.S.; de Boer, J.F. In vivo burn depth determination by high-speed fiber-based polarization sensitive optical coherence tomography. J. Biomed. Opt. 2001, 6, 474–479. [Google Scholar] [CrossRef]
- Kim, K.H.; Pierce, M.C.; Maguluri, G.; Park, B.H.; Yoon, S.J.; Lydon, M. In vivo imaging of human burn injuries with polarization-sensitive optical coherence tomography. J. Biomed. Opt. 2012, 17, 1–5. [Google Scholar] [CrossRef]
- Rollins, A.M.; Kulkarni, M.D.; Yazdanfar, S.; Ung-Arunyawee, R.; Izatt, J.A. In vivo video rate optical coherence tomography. Opt. Express 1998, 3, 219–229. [Google Scholar] [CrossRef]
- Rippon, M.G.; Springett, K.; Walmsley, R.; Patrick, K.; Millson, S. Ultrasound assessment of skin and wound tissue: Comparison with histology. Skin Res. Technol. 1998, 4, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Gnyawali, S.C.; Barki, K.G.; Mathew-Steiner, S.S.; Dixith, S.; Vanzant, D.; Kim, J.; Dickerson, J.L.; Datta, S.; Powell, H.; Roy, S.; et al. High-Resolution Harmonics Ultrasound Imaging for Non-Invasive Characterization of Wound Healing in a Pre-Clinical Swine Model. PLoS ONE 2015, 10, e0122327. [Google Scholar] [CrossRef] [PubMed]
- Brink, J.A.; Sheets, P.W.; Dines, K.A.; Etchison, M.R.; Hanke, C.W.; Sadove, A.M. Quantitative assessment of burn injury in porcine skin with high-frequency ultrasonic imaging. Investig. Radiol. 1986, 21, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Iraniha, S.; Cinat, M.E.; VanderKam, V.M.; Boyko, A.; Lee, D. Determination of Burn Depth with Noncontact Ultrasonography. J. Burn Care Rehabil. 2000, 21, 333–338. [Google Scholar] [CrossRef]
- Liddington, M.I.; Shakespeare, P.G. Timing of the thermographic assessment of burns. Burns 1996, 22, 26–28. [Google Scholar] [CrossRef]
- Dziewonski, M. Planimetry of thermograms in diagnosis of burn wounds. Sci. Res. Inst. Math. Comput. Sci. 2009, 8, 33–38. [Google Scholar]
- Miccio, J.; Parikh, S.; Marinaro, X.; Prasad, A.; McClain, S.; Singer, A.J.; Clark, R.A.F. Forward-looking infrared imaging predicts ultimate burn depth in a porcine vertical injury progression model. Burns 2016, 42, 397–404. [Google Scholar] [CrossRef]
- Ruminski, J.; Kaczmarek, M.; Renkielska, A.; Nowakowski, A. Thermal parametric imaging in the evaluation of skin burn depth. IEEE Trans. Biomed. Eng. 2007, 54, 303–312. [Google Scholar] [CrossRef]
- Owda, A.Y.; Salmon, N.; Andrews, D.; Rezgui, N.-D. Active millimeter-wave radar for sensing and imaging through dressing materials. In Proceedings of the IEEE SENSORS, Glasgow, Scotland, 29 October–1 November 2017. [Google Scholar]
- Owda, A.Y.; Salmon, N.; Harmer, S.W.; Shylo, S.; Bowring, N.J.; Rezgu, N.D.; Shah, M. Millimeter-wave emissivity as a metric for the non-contact diagnosis of human skin conditions. Bioelectromagnetics 2017, 38, 559–569. [Google Scholar] [CrossRef]
- Owda, A.Y.; Salmon, N.; Rezgui, N.-D.; Shylo, S. Millimetre wave radiometers for medical diagnostics of human skin. In Proceedings of the IEEE SENSORS, Glasgow, Scotland, 29 October–1 November 2017. [Google Scholar]
- Essen, H.; Essen, J.M.; Nuessler, D.; Hommes, A.; Krebs, C.; Fatihi, N.; Buzug, T. Monitoring of wound healing by millimetre wave imaging. In Proceedings of the 35th International Conference on Infrared, Millimeter, and Terahertz Waves, Rome, Italy, 5–10 September 2010. [Google Scholar]
- Gao, Y.; Zoughi, R. Millimeter reflectometry as an effective diagnosis tool for skin burn injuries. In Proceedings of the IEEE International Instrumentation and Measurement Technology Conference Proceedings, Taipei, Taiwan, 23–26 May 2016. [Google Scholar]
- Gao, Y.; Zoughi, R. Millimeter Wave Reflectometry and Imaging for Noninvasive Diagnosis of Skin Burn Injuries. IEEE Trans. Instrum. Meas. 2017, 66, 77–84. [Google Scholar] [CrossRef]
- Owda, A.Y.; Salmon, N.; Shylo, S.; Owda, M. Assessment of Bandaged Burn Wounds Using Porcine Skin and Millimetric Radiometry. Sensors 2019, 19, 2950. [Google Scholar] [CrossRef] [PubMed]
- Jasa Pembuatan. EMP Enseval Medika Prima. 2016. Available online: http://www.emp.co.id/blog/Blog_1315_19/News_1315_20/Wound-pH.html (accessed on 23 December 2019).
- Bajwa, N.; Sung, S.; Ennis, D.B.; Fishbein, M.C.; Nowroozi, B.N. Terahertz Imaging of Cutaneous Edema: Correlation With Magnetic Resonance Imaging in Burn Wounds. IEEE Trans. Biomed. Eng. 2017, 64, 2682–2694. [Google Scholar] [PubMed]
- Bajwa, N.; Nowroozi, B.; Garritano, J.; Sung, S.; Tewari, P. An investigation of THz burn wound edema imaging using MRI. In Proceedings of the 39th International Conference on Infrared, Millimeter, and Terahertz Waves, Tucson, AZ, USA, 14–19 September 2014. [Google Scholar]
- Lohmann, G.; Bohn, S.; Müller, K.; Trampel, R.; Turner, R. Image Restoration and Spatial Resolution in 7-Tesla Magnetic Resonance Imaging. Magn. Reson. Med. 2010, 64, 15–22. [Google Scholar] [CrossRef]
- Strutt, H.J.W., LVIII. On the scattering of light by small particles. Lond. Edinb. Dublin Philos. Mag. J. Sci. 2009, 41, 447–454. [Google Scholar] [CrossRef]
- Carovac, A.; Smajlovic, F.; Junuzovic, D. Application of Ultrasound in Medicine. Acta Inf. Med. 2011, 19, 168–171. [Google Scholar] [CrossRef]
- Monstrey, S.; Hoeksema, H.; Verbelen, J.; Pirayesh, A.; Blondeel, P. Assessment of burn depth and burn wound healing potential. Burns 2008, 34, 761–769. [Google Scholar] [CrossRef]
- Lubecke, O.B.; Nikawa, Y.; Snyder, W.; Lin, J.; Mizuno, K. Novel microwave and millimeter-wave biomedical applications. In Proceedings of the 4th International Conference, In Telecommunications in Modern Satellite, Cable and Broadcasting Services, Nis, Yugoslavia, 13–15 October 1999. [Google Scholar]
- Owda, A.Y.; Salmon, N.; Rezgui, N.-D. Electromagnetic Signatures of Human Skin in the Millimeter Wave Band 80–100 GHz. Prog. Electromagn. Res. B 2018, 80, 79–99. [Google Scholar] [CrossRef][Green Version]
- Owda, A.; Rezgui, N.-D.; Salmon, N. Signatures of human skin in the millimeter wave band (80–100) GHz. In Proceedings of the SPIE Europe Security+Defence, Millimetre Wave and Terahertz Sensors and Technology X, Warsaw, Poland, 11 – 14 September 2017. [Google Scholar]
- Owda, A.Y.; Salmon, N.A. Variation in the electromagnetic signatures of the human skin with physical activity and hydration level of the skin. In Proceedings of the Millimetre Wave and Terahertz Sensors and Technology XII, Strasbourg, France, 9–10 September 2019. [Google Scholar]
- Branski, L.K.; Mittermayr, R.; Herndon, D.N.; Norbury, W.B.; Masters, O.E.; Hofmann, M.; Traber, D.L.; Redl, H.; Jeschke, M.G. A porcine model of full-thickness burn, excision and skin autografting. Burns 2008, 34, 1119–1127. [Google Scholar] [CrossRef]
- Andrews, C.J.; Kempf, M.; Kimble, R.; Cuttle, L. Development of a Consistent and Reproducible Porcine Scald Burn Model. PLoS ONE 2016, 11, e0162888. [Google Scholar] [CrossRef]
- Wu, T.; Rappaport, T.S.; Collins, C.M. The Human Body and Millimeter-Wave Wireless Communication Systems: Interactions and Implications. In Proceedings of the IEEE International Conference on Communication (ICC), London, UK, 8–12 June 2015. [Google Scholar]
- Rezgui, N.D.; Bowring, N.J.; Andrews, D.A.; Harmer, S.W.; Southgate, M.J.; O’Reilly, D. Development of an ultra wide band microwave radar based footwear scanning system. In Proceedings of the SPIE Millimetre Wave and Terahertz Sensors and Technology VI, Dresden, Germany, 24–25 September 2013. [Google Scholar]
- Rezgui, N.D.; Bowring, N.; Andrews, D.; Harmer, S.; Southgate, M.J.; O’Reilly, D. Scanning Apparatus. U.S. Patent 2015/0369756 A1, 24 December 2015. [Google Scholar]
- Rezgui, N.-D.; Andrews, D.A.; Bowring, N. Ultra-wide-band 3D microwave imaging scanner for the detection of concealed weapons. In Proceedings of the SPIE Millimetre Wave and Terahertz Sensors and Technology VIII, Toulouse, France, 21–24 September 2015. [Google Scholar]
- Chou, C.-K.; Andrea, J.D.; Petersen, R. IEEE Standard for Safety Levels with Respect to Human Exposure to Radio Frequency Electromagnetic Fields, 3KHz to 300GHz; U.S.A: IEEE Std C 95.1; IEEE: New York, NY, USA, 2006. [Google Scholar]
- Sheen, D.M.; McMakin, D.L.; Hall, T.E. Three-dimensional millimeter-wave imaging for concealed weapon detection. IEEE Trans. Microw. Theory Tech. 2001, 49, 1581–1592. [Google Scholar] [CrossRef]
- Skolnik, M. Radar Handbook, 3rd ed.; McGraw Hill: New York, NY, USA, 2008. [Google Scholar]
- Skolnik, M.I. Introduction to Radar Systems; McGraw Hill: Singapore, 2001. [Google Scholar]
- Rees, W.G. Physical Principles of Remote Sensing, 3rd ed.; Cambridge University Press: New York, NY, USA, 2013. [Google Scholar]
- Nezry, E. Adaptive Speckle Filtering in Radar Imagery. In Land Applications of Radar Remote Sensing; IntechOpen: London, UK, 2014; pp. 1–55. [Google Scholar]
- Dhillon, S.S.; Vitiello, M.S.; Linfield, E.H.; Davies, A.G.; Hoffmann, M.C.; Booske, J.; Paoloni, C.; Gensch, M.; Weightman, P.; Williams, G.P. The 2017 terahertz science and technology roadmap. J. Phys. D Appl. Phys. 2017, 50, 1–49. [Google Scholar] [CrossRef]
- Born, M.; Wolf, E. Principles of Optics, 7th ed.; Cambridge University Press: Cambridge, UK, 1999. [Google Scholar]
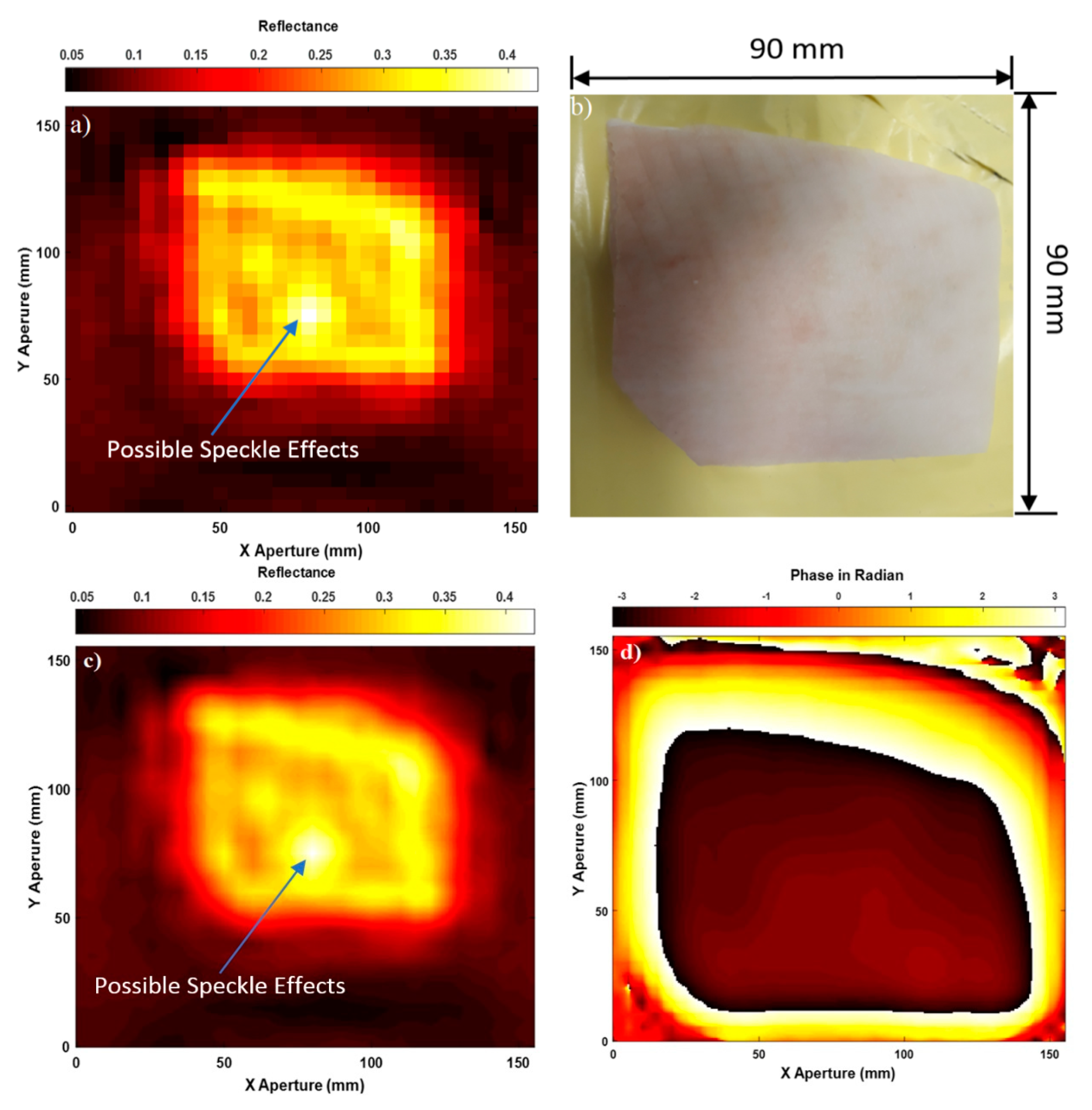
| Sample Description | Mean Reflectance of the Skin | Mean Reflectance of the Burn |
|---|---|---|
| Sample 1: Skin without Dressing Materials; Figure 4 | 0.32 | - |
| Sample 1: Skin with Dressing Materials; Figure 5 | 0.30 | - |
| Sample 2: Skin with Burns and without Dressing Materials; Figure 6 | 0.28 | 0.20 |
| Sample 2: Skin with Burns and Dressing Materials; Figure 7 | 0.26 | 0.18 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Owda, A.Y.; Owda, M.; Rezgui, N.-D. Synthetic Aperture Radar Imaging for Burn Wounds Diagnostics. Sensors 2020, 20, 847. https://doi.org/10.3390/s20030847
Owda AY, Owda M, Rezgui N-D. Synthetic Aperture Radar Imaging for Burn Wounds Diagnostics. Sensors. 2020; 20(3):847. https://doi.org/10.3390/s20030847
Chicago/Turabian StyleOwda, Amani Yousef, Majdi Owda, and Nacer-Ddine Rezgui. 2020. "Synthetic Aperture Radar Imaging for Burn Wounds Diagnostics" Sensors 20, no. 3: 847. https://doi.org/10.3390/s20030847
APA StyleOwda, A. Y., Owda, M., & Rezgui, N.-D. (2020). Synthetic Aperture Radar Imaging for Burn Wounds Diagnostics. Sensors, 20(3), 847. https://doi.org/10.3390/s20030847






