Remote Pain Monitoring Using Fog Computing for e-Healthcare: An Efficient Architecture
Abstract
1. Introduction
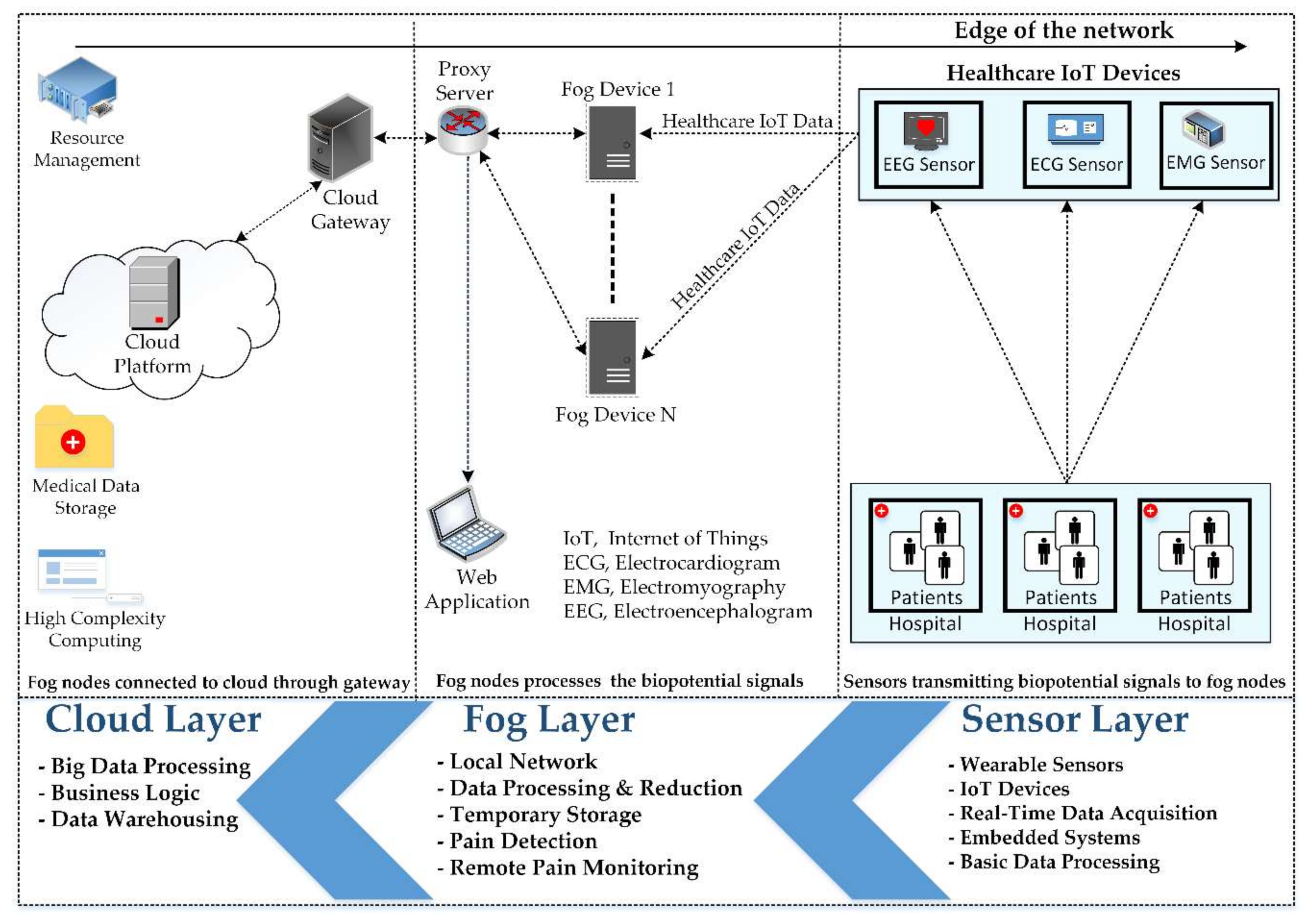
- An efficient fog-based remote pain monitoring system is proposed, consisting of a three-tier structure. Fog nodes reside in the middle tier, implementing the fog computing concept. Fog devices process the biopotential signals and transmit the pain information to the web servers via gateway devices.
- The parameters under consideration are execution cost, latency, and network consumption. The proposed architecture reduces these factors, making the proposed system most suitable for health-related applications. Moreover, it ensures real-time monitoring of patients and rapid medical assistance provisioning by minimizing the time spent from pain detection to display in the web application. The proposed architecture not only reduces time but also reduces the data to be transmitted to the cloud by discarding the unwanted data at the fog nodes.
- Simulations are performed on different scales for appraising the proposed fog-based remote pain monitoring architecture. The results of the comparison performed between cloud architecture and proposed architecture validate the superiority of the proposed architecture in terms of execution cost, delay, and network consumption.
2. Background
3. Related Work
4. Proposed Architecture
4.1. The Sensor Layer
4.2. The Fog Layer
4.3. The Cloud Layer
4.4. Overview
5. Simulation Setup and Results
| Algorithm 1 Fog-based remote pain monitoring system with first come first served (FCFS) scheduling. |
 |
5.1. Execution Cost
5.2. Latency
5.3. Network Consumption
6. Results and Discussion
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Shukla, S.; Hassan, M.F.; Khan, M.K.; Jung, L.T.; Awang, A. An analytical model to minimize the latency in healthcare internet-of-things in fog computing environment. PLoS ONE 2019, 14, e0224934. [Google Scholar] [CrossRef] [PubMed]
- Naha, R.K.; Garg, S.; Georgakopoulos, D.; Jayaraman, P.P.; Gao, L.; Xiang, Y.; Ranjan, R. Fog Computing: Survey of trends, architectures, requirements, and research directions. IEEE Access 2018, 6, 47980–48009. [Google Scholar] [CrossRef]
- Nandyala, C.S.; Kim, H.-K. From cloud to fog and IoT-based real-time U-healthcare monitoring for smart homes and hospitals. Int. J. Smart Home 2016, 10, 187–196. [Google Scholar] [CrossRef]
- Gia, T.N.; Jiang, M.; Rahmani, A.-M.; Westerlund, T.; Liljeberg, P.; Tenhunen, H. Fog computing in healthcare internet of things: A case study on ecg feature extraction. In Proceedings of the 2015 IEEE International Conference on Computer and Information Technology, Ubiquitous Computing and Communications; Dependable, Autonomic and Secure Computing; Pervasive Intelligence and Computing, Liverpool, UK, 26–28 October 2015; pp. 356–363. [Google Scholar]
- Shi, Y.; Ding, G.; Wang, H.; Roman, H.E.; Lu, S. The fog computing service for healthcare. In Proceedings of the 2015 2nd International Symposium on Future Information and Communication Technologies for Ubiquitous HealthCare (Ubi-HealthTech), Beijing, China, 28–30 May 2015; pp. 1–5. [Google Scholar]
- Jonassaint, C.R.; Shah, N.; Jonassaint, J.; De Castro, L. Usability and feasibility of an mHealth intervention for monitoring and managing pain symptoms in sickle cell disease: The Sickle Cell Disease Mobile Application to Record Symptoms via Technology (SMART). Hemoglobin 2015, 39, 162–168. [Google Scholar] [CrossRef]
- Lucey, P.; Cohn, J.F.; Matthews, I.; Lucey, S.; Sridharan, S.; Howlett, J.; Prkachin, K.M. Automatically detecting pain in video through facial action units. IEEE Trans. Syst. Man Cybern. Part B 2010, 41, 664–674. [Google Scholar] [CrossRef]
- Kächele, M.; Werner, P.; Al-Hamadi, A.; Palm, G.; Walter, S.; Schwenker, F. Bio-visual fusion for person-independent recognition of pain intensity. In Proceedings of the International Workshop on Multiple Classifier Systems, Günzburg, Germany, 29 June–1 July 2015; Springer Science and Business Media LLC.: Berlin/Heidelberg, Germany, 2015; pp. 220–230. [Google Scholar]
- Hossain, M.S.; Muhammad, G. Cloud-assisted speech and face recognition framework for health monitoring. Mob. Netw. Appl. 2015, 20, 391–399. [Google Scholar] [CrossRef]
- Zhong, Y.; Liu, L. Remote neonatal pain assessment system based on internet of things. In Proceedings of the 2011 International Conference on Internet of Things and 4th International Conference on Cyber, Physical and Social Computing, Dalian, China, 19–22 October 2011; pp. 629–633. [Google Scholar]
- Yang, G.; Jiang, M.; Ouyang, W.; Ji, G.; Xie, H.; Rahmani, A.M.; Liljeberg, P.; Tenhunen, H. IoT-Based Remote Pain Monitoring System: From Device to Cloud Platform. IEEE J. Biomed. Health Inform. 2018, 22, 1711–1719. [Google Scholar] [CrossRef]
- Da Fonseca, N.L.; Boutaba, R. Cloud Services, Networking, and Management; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Sarkar, S.; Misra, S. Theoretical modelling of fog computing: A green computing paradigm to support IoT applications. IET Netw. 2016, 5, 23–29. [Google Scholar] [CrossRef]
- Chang, Y.-C.P.; Chen, S.; Wang, T.-J.; Lee, Y. Fog computing node system software architecture and potential applications for NB-IoT industry. In Proceedings of the 2016 International Computer Symposium (ICS), Chiayi, Taiwan, 15–17 December 2016; pp. 727–730. [Google Scholar]
- Alrawais, A.; Alhothaily, A.; Hu, C.; Cheng, X. Fog computing for the internet of things: Security and privacy issues. IEEE Internet Comput. 2017, 21, 34–42. [Google Scholar] [CrossRef]
- Rahmani, A.M.; Gia, T.N.; Negash, B.; Anzanpour, A.; Azimi, I.; Jiang, M.; Liljeberg, P. Exploiting smart e-Health gateways at the edge of healthcare Internet-of-Things: A fog computing approach. Future Gener. Comput. Syst. 2018, 78, 641–658. [Google Scholar] [CrossRef]
- Lee, G.; Saad, W.; Bennis, M. An online optimization framework for distributed fog network formation with minimal latency. IEEE Trans. Wirel. Commun. 2019, 18, 2244–2258. [Google Scholar] [CrossRef]
- Skorin-Kapov, L.; Matijasevic, M. Analysis of QoS requirements for e-health services and mapping to evolved packet system QoS classes. Int. J. Telemed. Appl. 2010, 2010, 628086. [Google Scholar] [CrossRef] [PubMed]
- Gállego, J.R.; Hernández-Solana, Á.; Canales, M.; Lafuente, J.; Valdovinos, A.; Fernández-Navajas, J. Performance analysis of multiplexed medical data transmission for mobile emergency care over the UMTS channel. IEEE Trans. Inf. Technol. Biomed. 2005, 9, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Bonomi, F.; Milito, R.; Zhu, J.; Addepalli, S. Fog computing and its role in the internet of things. In Proceedings of the First Edition of the MCC Workshop on Mobile Cloud Computing, Helsinki, Finland, 17 August 2012; Association for Computing Machinery (ACM): New York, NY, USA, 2012; pp. 13–16. [Google Scholar]
- Liu, Y.; Fieldsend, J.E.; Min, G. A framework of fog computing: Architecture, challenges, and optimization. IEEE Access 2017, 5, 25445–25454. [Google Scholar] [CrossRef]
- Deng, R.; Lu, R.; Lai, C.; Luan, T.H.; Liang, H. Optimal workload allocation in fog-cloud computing toward balanced delay and power consumption. IEEE Internet Things J. 2016, 3, 1171–1181. [Google Scholar] [CrossRef]
- Nishtala, R.; Carpenter, P.; Petrucci, V.; Martorell, X. Hipster: Hybrid task manager for latency-critical cloud workloads. In Proceedings of the 2017 IEEE International Symposium on High Performance Computer Architecture (HPCA), Austin, TX, USA, 4–8 February 2017; pp. 409–420. [Google Scholar]
- Chen, N.; Yang, Y.; Li, J.; Zhang, T. A fog-based service enablement architecture for cross-domain IoT applications. In Proceedings of the 2017 IEEE Fog World Congress (FWC), Santa Clara, CA, USA, 30 October–1 November 2017; pp. 1–6. [Google Scholar]
- Wang, D.; Liu, Z.; Wang, X.; Lan, Y. Mobility-Aware Task Offloading and Migration Schemes in Fog Computing Networks. IEEE Access 2019, 7, 43356–43368. [Google Scholar] [CrossRef]
- Ma, M.; He, D.; Wang, H.; Kumar, N.; Choo, K.-K.R. An efficient and provably secure authenticated key agreement protocol for fog-based vehicular ad-hoc networks. IEEE Internet Things J. 2019, 6, 8065–8075. [Google Scholar] [CrossRef]
- Vilalta, R.; López, V.; Giorgetti, A.; Peng, S.; Orsini, V.; Velasco, L.; Serral-Gracia, R.; Morris, D.; De Fina, S.; Cugini, F. TelcoFog: A unified flexible fog and cloud computing architecture for 5G networks. IEEE Commun. Mag. 2017, 55, 36–43. [Google Scholar] [CrossRef]
- Dar, B.K.; Shah, M.A.; Shahid, H.; Naseem, A. Fog computing based automated accident detection and emergency response system using android smartphone. In Proceedings of the 2018 14th International Conference on Emerging Technologies (ICET), Islamabad, Pakistan, 21–22 November 2018; pp. 1–6. [Google Scholar]
- Saharan, K.; Kumar, A. Fog in comparison to cloud: A survey. Int. J. Comput. Appl. 2015, 122, 10–12. [Google Scholar]
- Atlam, H.F.; Walters, R.J.; Wills, G.B. Fog computing and the internet of things: A review. Big Data Cogn. Comput. 2018, 2, 10. [Google Scholar] [CrossRef]
- Dastjerdi, A.V.; Gupta, H.; Calheiros, R.N.; Ghosh, S.K.; Buyya, R. Fog computing: Principles, architectures, and applications. In Internet of Things; Elsevier: Amsterdam, The Netherlands, 2016; pp. 61–75. [Google Scholar]
- Dastjerdi, A.V.; Buyya, R. Fog computing: Helping the Internet of Things realize its potential. Computer 2016, 49, 112–116. [Google Scholar] [CrossRef]
- Jia, B.; Hu, H.; Zeng, Y.; Xu, T.; Yang, Y. Double-matching resource allocation strategy in fog computing networks based on cost efficiency. J. Commun. Netw. 2018, 20, 237–246. [Google Scholar] [CrossRef]
- Gao, X.; Huang, X.; Bian, S.; Shao, Z.; Yang, Y. PORA: Predictive offloading and resource allocation in dynamic fog computing systems. IEEE Internet Things J. 2019, 7, 72–87. [Google Scholar] [CrossRef]
- Mutlag, A.A.; Ghani, M.K.A.; Arunkumar, N.; Mohammed, M.A.; Mohd, O. Enabling technologies for fog computing in healthcare IoT systems. Future Gener. Comput. Syst. 2019, 90, 62–78. [Google Scholar] [CrossRef]
- Kumar, V.; Laghari, A.A.; Karim, S.; Shakir, M.; Brohi, A.A. Comparison of fog computing & cloud computing. Int. J. Math. Sci. Comput. 2019, 5, 31–41. [Google Scholar]
- Khattak, H.A.; Islam, S.U.; Din, I.U.; Guizani, M. Integrating fog computing with VANETs: A consumer perspective. IEEE Commun. Stand. Mag. 2019, 3, 19–25. [Google Scholar] [CrossRef]
- Muheidat, F.; Tawalbeh, L.A.; Tyrer, H. Context-aware, accurate, and real time fall detection system for elderly people. In Proceedings of the 2018 IEEE 12th International Conference on Semantic Computing (ICSC), Laguna Hills, CA, USA, 31 January–2 February 2018; pp. 329–333. [Google Scholar]
- Tejaswini, S.; Sriraam, N.; Pradeep, G. Cloud-Based Framework for Pain Scale Assessment in NICU-A Primitive Study with Infant Cries. In Proceedings of the 2018 3rd International Conference on Circuits, Control, Communication and Computing (I4C), Bengaluru, India, 3–5 October 2018; pp. 1–4. [Google Scholar]
- GJ, B.K. Internet of Things (IoT) and Cloud Computing based Persistent Vegetative State Patient Monitoring System: A remote Assessment and Management. In Proceedings of the 2018 International Conference on Computational Techniques, Electronics and Mechanical Systems (CTEMS), Belagavi, India, 21–23 December 2018; pp. 301–305. [Google Scholar]
- Muhammed, T.; Mehmood, R.; Albeshri, A.; Katib, I. UbeHealth: A personalized ubiquitous cloud and edge-enabled networked healthcare system for smart cities. IEEE Access 2018, 6, 32258–32285. [Google Scholar] [CrossRef]
- Farahani, B.; Firouzi, F.; Chang, V.; Badaroglu, M.; Constant, N.; Mankodiya, K. Towards fog-driven IoT eHealth: Promises and challenges of IoT in medicine and healthcare. Future Gener. Comput. Syst. 2018, 78, 659–676. [Google Scholar] [CrossRef]
- Negash, B.; Gia, T.N.; Anzanpour, A.; Azimi, I.; Jiang, M.; Westerlund, T.; Rahmani, A.M.; Liljeberg, P.; Tenhunen, H. Leveraging fog computing for healthcare IoT. In Fog Computing in the Internet of Things; Springer: Berlin/Heidelberg, Germany, 2018; pp. 145–169. [Google Scholar]
- Gaigawali, M.N.; Chaskar, U. Cloud Based ECG Monitoring and Fibrillation Detection for Healthcare System. In Proceedings of the 2018 Second International Conference on Intelligent Computing and Control Systems (ICICCS), Madurai, India, 14–15 June 2018; pp. 287–291. [Google Scholar]
- Idoga, P.E.; Toycan, M.; Nadiri, H.; Çelebi, E. Factors affecting the successful adoption of e-health cloud based health system from healthcare consumers’ perspective. IEEE Access 2018, 6, 71216–71228. [Google Scholar] [CrossRef]
- Sood, S.K.; Mahajan, I. A fog-based healthcare framework for chikungunya. IEEE Internet Things J. 2017, 5, 794–801. [Google Scholar] [CrossRef]
- Gupta, H.; Vahid Dastjerdi, A.; Ghosh, S.K.; Buyya, R. iFogSim: A toolkit for modeling and simulation of resource management techniques in the Internet of Things, Edge and Fog computing environments. Softw. Pract. Exp. 2017, 47, 1275–1296. [Google Scholar] [CrossRef]
- Qaddoura, R.; Manaseer, S. Comparative Study for the Effect of CPU Speed in Fog Networks. In Proceedings of the 2018 Fifth International Symposium on Innovation in Information and Communication Technology (ISIICT), Philadelphia, PA, USA, 31 October–1 November 2018; pp. 1–5. [Google Scholar]
- Jayasena, K.N.; Thisarasinghe, B. Optimized task scheduling on fog computing environment using meta heuristic algorithms. In Proceedings of the 2019 IEEE International Conference on Smart Cloud (SmartCloud), Tokyo, Japan, 10–12 December 2019; pp. 53–58. [Google Scholar]
- Awaisi, K.S.; Abbas, A.; Zareei, M.; Khattak, H.A.; Khan, M.U.S.; Ali, M.; Din, I.U.; Shah, S. Towards a Fog Enabled Efficient Car Parking Architecture. IEEE Access 2019, 7, 159100–159111. [Google Scholar] [CrossRef]
- Mahmud, R.; Kotagiri, R.; Buyya, R. Fog computing: A taxonomy, survey and future directions. In Internet of Everything; Springer: Berlin/Heidelberg, Germany, 2018; pp. 103–130. [Google Scholar]
- Fang, J.; Ma, A. IoT Application Modules Placement and Dynamic Task Processing in Edge-Cloud Computing. IEEE Internet Things J. 2020, 1. [Google Scholar] [CrossRef]
- Mukherjee, M.; Shu, L.; Wang, D. Survey of fog computing: Fundamental, network applications, and research challenges. IEEE Commun. Surv. Tutor. 2018, 20, 1826–1857. [Google Scholar] [CrossRef]
- Friesen, E.; Ekman, P. Facial action coding system: A technique for the measurement of facial movement. Palo Alto 1978, 3. [Google Scholar] [CrossRef]
- Maaten, L.V.d.; Hinton, G. Visualizing data using t-SNE. J. Mach. Learn. Res. 2008, 9, 2579–2605. [Google Scholar]
- Sadiq, M.T.; Yu, X.; Yuan, Z.; Fan, Z.; Rehman, A.U.; Li, G.; Xiao, G. Motor imagery EEG signals classification based on mode amplitude and frequency components using empirical wavelet transform. IEEE Access 2019, 7, 127678–127692. [Google Scholar] [CrossRef]
- Rahbari, D.; Nickray, M. Scheduling of fog networks with optimized knapsack by symbiotic organisms search. In Proceedings of the 2017 21st Conference of Open Innovations Association (FRUCT), Helsinki, Finland, 6–10 November 2017; pp. 278–283. [Google Scholar]
- Martin, J.P.; Kandasamy, A.; Chandrasekaran, K. Mobility aware autonomic approach for the migration of application modules in fog computing environment. J. Ambient Intell. Humaniz. Comput. 2020, 11, 5259–5278. [Google Scholar] [CrossRef]
- Rahbari, D.; Nickray, M. Low-latency and energy-efficient scheduling in fog-based IoT applications. Turk. J. Electr. Eng. Comput. Sci. 2019, 27, 1406–1427. [Google Scholar] [CrossRef]
- Siam, A.I.; Abou Elazm, A.; El-Bahnasawy, N.A.; El Banby, G.; Abd El-Samie, F.E.; Abd El-Samie, F.E. Smart Health Monitoring System based on IoT and Cloud Computing. Menoufia J. Electron. Eng. Res. 2019, 28, 37–42. [Google Scholar] [CrossRef]
- Casti, P.; Mencattini, A.; Filippi, J.; D’Orazio, M.; Comes, M.C.; Di Giuseppe, D.; Martinelli, E. A Personalized Assessment Platform for Non-invasive Monitoring of Pain. In Proceedings of the 2020 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Bari, Italy, 1 June–1 July 2020; pp. 1–5. [Google Scholar]
- Al-Khafajiy, M.; Baker, T.; Chalmers, C.; Asim, M.; Kolivand, H.; Fahim, M.; Waraich, A.J.M.T.; Applications. Remote health monitoring of elderly through wearable sensors. Multimed. Tools Appl. 2019, 78, 24681–24706. [Google Scholar] [CrossRef]









| Real-Time E-Healthcare Services | Healthcare Applications | Type of Media | Maximum Delay |
|---|---|---|---|
| Audio communication | Audio conversation between patients and doctors | Audio | <150 milliseconds one-way |
| Video communication | Video conferencing between patients and doctors | Video | <250 milliseconds one-way |
| Robotic services | Tele-ultrasonography | Control signals related to robotics | <300 milliseconds round-trip time |
| Monitoring services | Remote pain monitoring | Biosignal of patients gathered by sensors | <300 milliseconds for real-time ECG |
| CPU Length | Network Length (bytes) | Sensor Detecting Interval |
|---|---|---|
| 1200 million instructions | 22,000 bytes | 25 milliseconds |
| Parameter | Cloud | Proxy Server | Web Server | Fog Node | Sensor Node |
|---|---|---|---|---|---|
| Level | 0 | 1 | 2 | 2 | 3 |
| Rate per MIPS | 0.01 | 0.0 | 0.0 | 0.0 | 0.0 |
| RAM (MB) | 40,000 | 4000 | 4000 | 4000 | 1000 |
| Idle power | 16 × 83.25 | 83.43 | 83.43 | 83.43 | 82.44 |
| Downlink bandwidth (MB) | 10,000 | 10,000 | 10,000 | 10,000 | - |
| CPU length (MIPS) | 44,800 | 2800 | 2800 | 2800 | 500 |
| Uplink bandwidth (MB) | 100 | 10,000 | 10,000 | 10,000 | 10,000 |
| Busy power (Watt) | 16 × 103 | 107.339 | 107.339 | 107.339 | 87.53 |
| Reference | Paradigm | Remote Monitoring | Response Time | Cost of Execution in Cloud | Network Consumption |
|---|---|---|---|---|---|
| [61] | Cloud | Pain | Moderate | High | High |
| [39] | Cloud | Pain | Moderate | High | High |
| [62] | Cloud | Health | Moderate | High | High |
| [40] | Cloud | Patient | Moderate | High | High |
| [11] | Cloud | Pain | Moderate | High | High |
| Proposed System | Fog | Pain | Minimum | Low | Low |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hassan, S.R.; Ahmad, I.; Ahmad, S.; Alfaify, A.; Shafiq, M. Remote Pain Monitoring Using Fog Computing for e-Healthcare: An Efficient Architecture. Sensors 2020, 20, 6574. https://doi.org/10.3390/s20226574
Hassan SR, Ahmad I, Ahmad S, Alfaify A, Shafiq M. Remote Pain Monitoring Using Fog Computing for e-Healthcare: An Efficient Architecture. Sensors. 2020; 20(22):6574. https://doi.org/10.3390/s20226574
Chicago/Turabian StyleHassan, Syed Rizwan, Ishtiaq Ahmad, Shafiq Ahmad, Abdullah Alfaify, and Muhammad Shafiq. 2020. "Remote Pain Monitoring Using Fog Computing for e-Healthcare: An Efficient Architecture" Sensors 20, no. 22: 6574. https://doi.org/10.3390/s20226574
APA StyleHassan, S. R., Ahmad, I., Ahmad, S., Alfaify, A., & Shafiq, M. (2020). Remote Pain Monitoring Using Fog Computing for e-Healthcare: An Efficient Architecture. Sensors, 20(22), 6574. https://doi.org/10.3390/s20226574








