PatientDataChain: A Blockchain-Based Approach to Integrate Personal Health Records
Abstract
1. Introduction
1.1. Context
1.1.1. Electronic Health Records
1.1.2. Personal Health Records
1.1.3. Interoperability Standards in Healthcare
1.1.4. Wearables
- AI-based wearable devices to monitor healthcare at home
- Gait analysis data from wearables to predict Alzheimer’s and Parkinson’s diseases
- Biomolecule recording
1.1.5. Blockchain
- Decentralization: unlike traditional database systems, which store information on a central server, blockchain removes this single point of failure issue through decentralization. Data is hosted and managed though consensus by all the parties involved in the business flow, without having a single point of control.
- Distributed and scalable: for a distributed ledger configuration, the backend is a network of computers, each storing applications and data. This distribution guarantees availability and fast access to the system.
- Security and transparency: the entire blockchain concept emerged from the need for a secure and stable framework, thus data protection, security, and cryptography are core features of this technology.
- Data immutability and integrity: the decentralized and distributed architecture ensure data immutability and integrity, given that data cannot be altered unless all parties in the blockchain reach consensus, increasing trust between users.
1.2. The Problem
- 1.
- Lack of interoperability and difficulties in healthcare data exchange [36]. An essential issue now is the fact that hospitals and medical service providers are not interoperable. Consequently, medical health records are disparate, fragmented, and difficult to exchange. Thus, a patient ends up having their medical records stored in different locations: medical investigations are stored in the providers’ databases, medication data is stored locally with various pharmacies, etc. This lack of interoperability makes patients and providers face significant hurdles in initiating data retrieval and sharing. Thus, it becomes mandatory in the current context, where the volume of medical data generated is rapidly increasing, to define a common standard to integrate the patients’ healthcare records from various sources and enhance data exchange across the entire value chain.
- 2.
- Difficulties in ensuring data confidentiality and privacy, while maintaining secure access to patient records. At present, confidential medical records lack a protected structure, leading to serious data breaches. The Office for Civil Rights (OCR) of the Department of Health and Human Services (USA) issued reports of several data breaches in 2018 that culminated in the disclosure of 13 million total health records [37]. To become fully interoperable, healthcare data needs to be shared between healthcare stakeholders, while also protecting sensitive information and securing access only to authorized users. Data sharing and exchange is a great opportunity for improving the healthcare ecosystem on the road to interoperability, but also one of the biggest privacy challenges.
- 3.
- Data ownership. Another problem in healthcare today is related to data ownership, namely the fact that patients are unable to have complete control of their own medical records. This aspect’s importance increases with the rise of personalized medicine and wearables [38]. In the data-sharing context, one aspect that becomes essential is the patient’s consent to make this a transparent process [39]. Thus, for reaching a fully integrated and interoperable healthcare system, an important requirement is to grant the patient ownership of their data, which will enable them to decide who has permission to access their data and with what privileges [13]. This would help create a flexible and secure health records management. As a matter of fact, a common problem with all the existing systems is insufficient security controls for users accessing or sharing files [40], as there are major considerations concerning user privacy and therefore limitations of dominant access to personal information [41].
- 4.
- Patient data overload. Health Information Technology (HIT) has evolved, but still lacks a unified viewpoint over the entire patient’s health history [42,43]. One of the new approaches on personal health records focus on integrating healthcare data collected from various sensors, trackers, and wearable devices, such as fitness trackers, smartwatches, or devices that monitor healthcare parameters (heart rate, glucose level etc.) [44]. A challenge that occurs in this context is the huge amount of data that is produced, that need to be processed, analyzed and stored. Thus, new storage and processing solutions must be found [45]. In addition, a strong user interface (UI) becomes relevant in presenting the information to healthcare providers in an attractive and easy-to-interpret manner. Consequently, there is an increasing trend within healthcare organizations to focus on user experience, and engage UI designers in the process to address this need [46].
2. Related Work
2.1. Distributed PHR Models
- The uPHR (Ubiquitous PHR framework) model [47] is an event-based distributed model. The model implements the standards HL7, CCR, and CEN 13606. Limitations: does not focus on security and data privacy.
- The HealthVault [48] is a web-based, client-server, PHR for keeping health and fitness records. It is compliant with HL7. Limitations: proprietary solution.
- The DEPR (Distributed Electronic Patient Records) model [49] is a distributed model based on the OpenEMR system, compliant with several standards. Limitations: does not focus on security or data privacy.
- My HealtheVet [50] is an online platform for sharing health information. It is designed on a distributed event-based model, and the interoperability model and security policies are based on the HL7 standard.
- The CF (Conceptual Framework) model [51] is a framework implementing a distributed mechanism for wearable health systems. It is compliant with the HIPAA standard for security and privacy. Limitations: does not focus on interoperability.
- The SNOW project [52] is a decentralized medical data processing system, based on the openEHR standard.
2.2. Blockchain in Healthcare
3. Our Solution: PatientDataChain
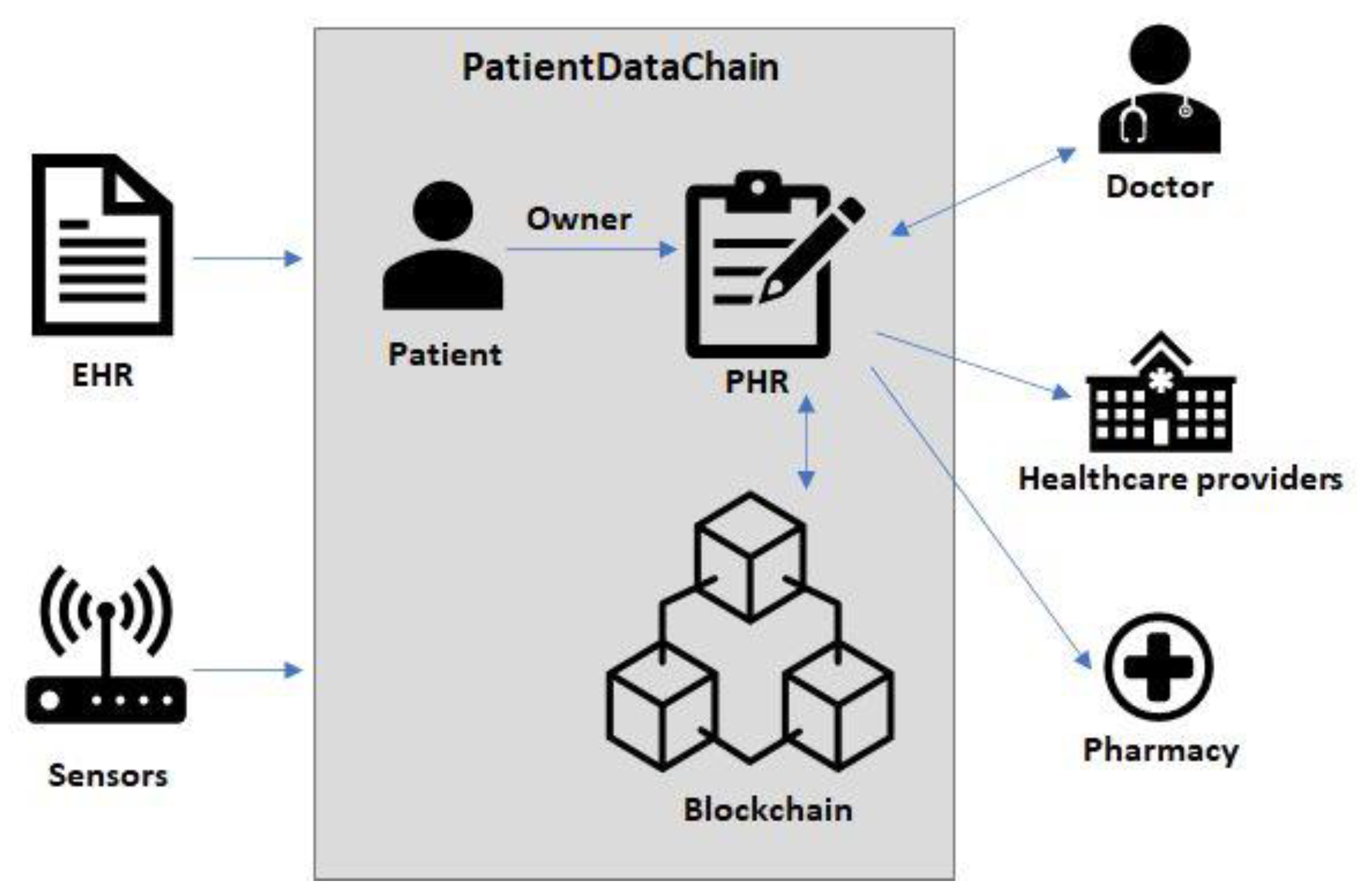
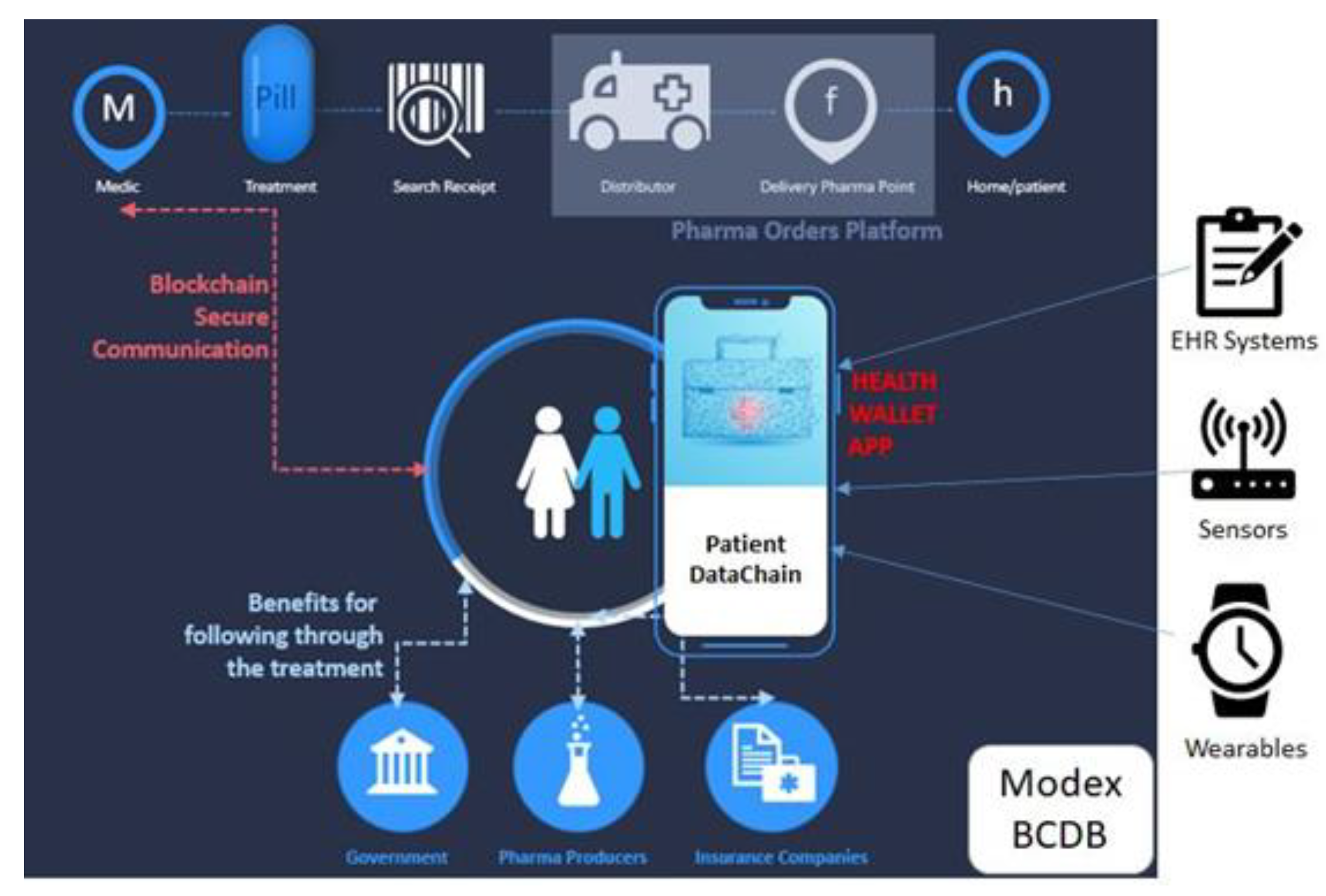
3.1. System Overview
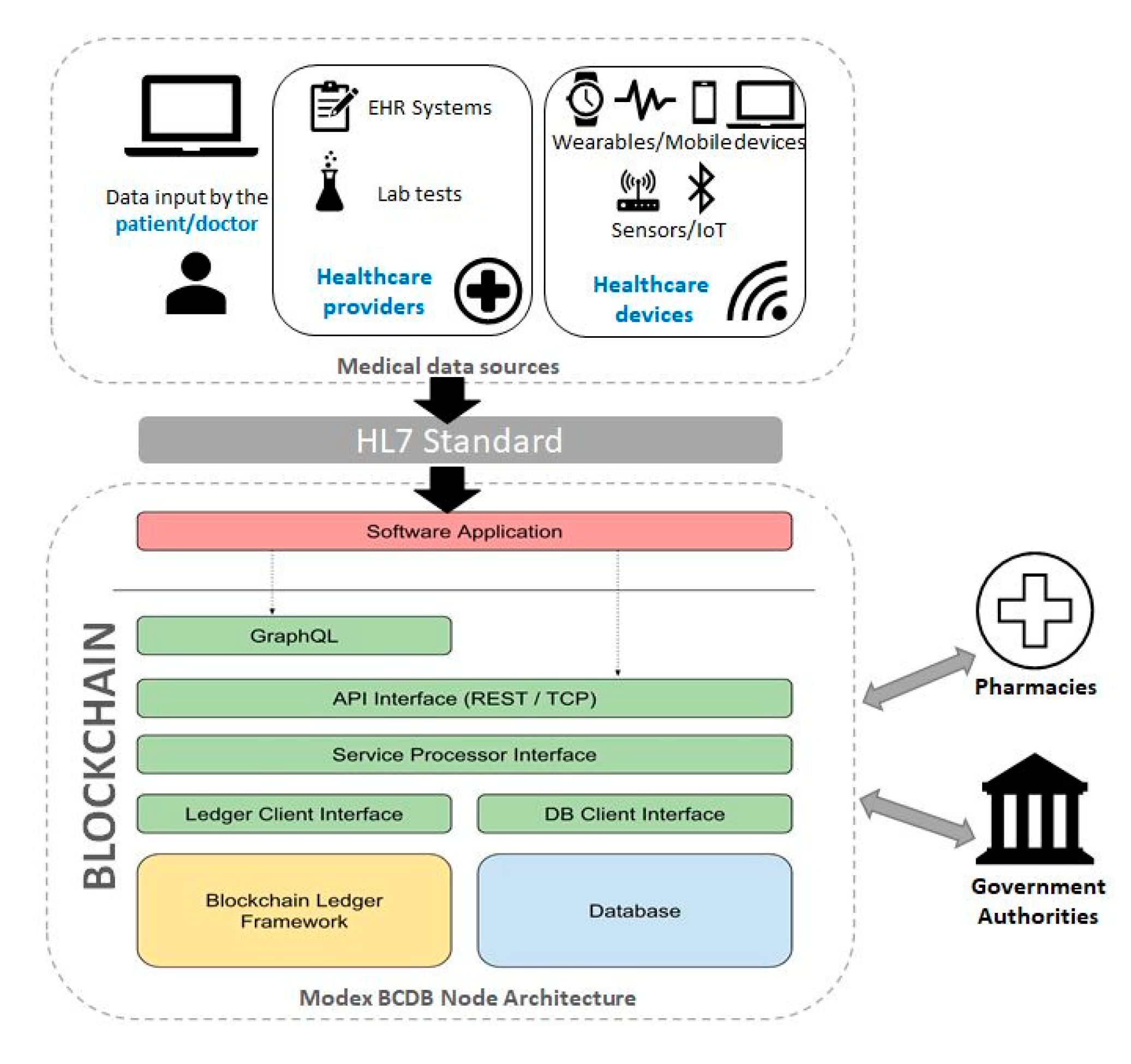
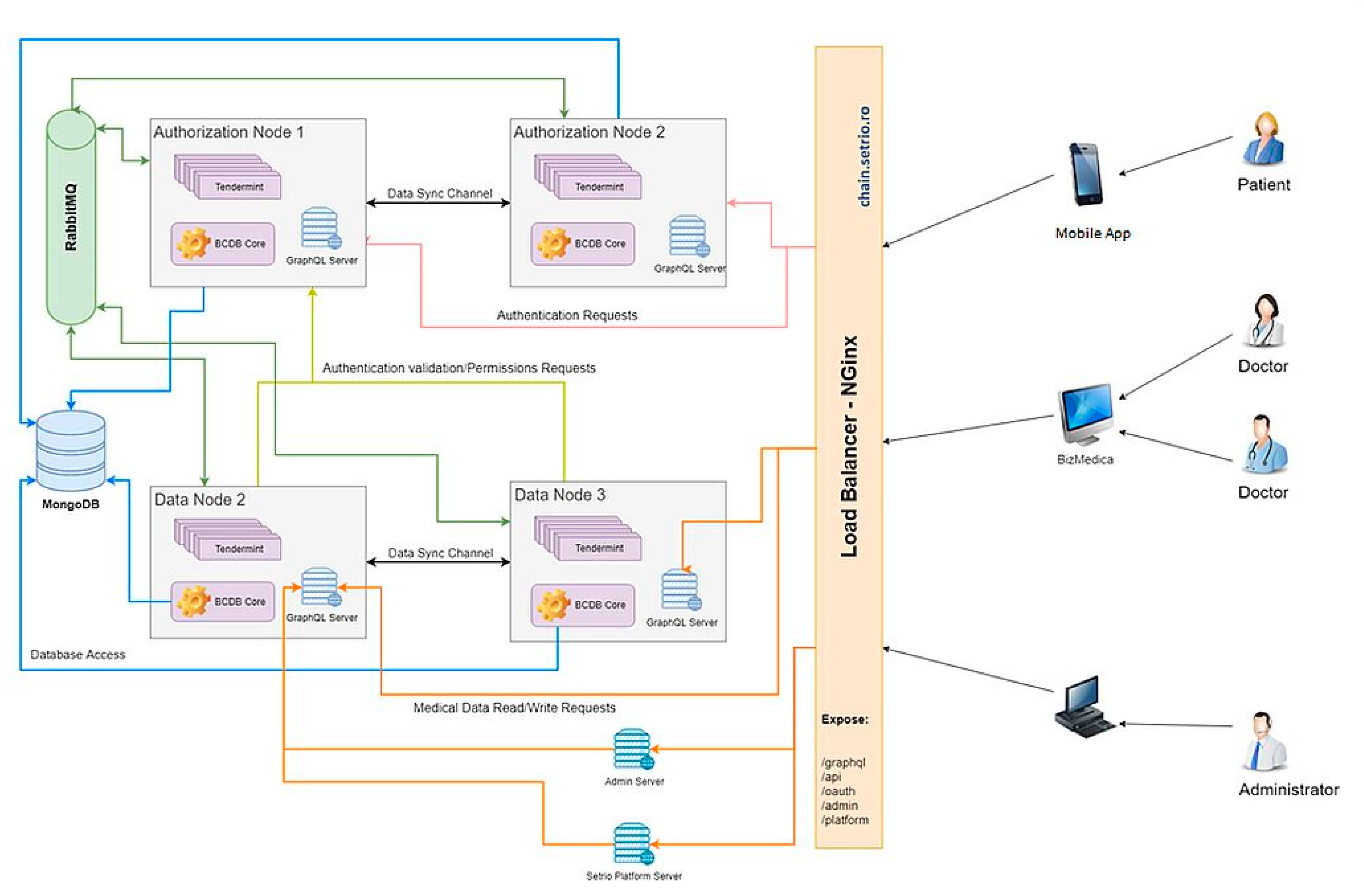
3.2. Modex Blockchain Database (BCDB)
3.3. System Architecture
- Data entered by the patient
- Data from existing EHR systems. PatientDataChain connects to EHR systems via APIs, and the middleware capabilities of Modex BCDB allow for the data in the database to be uploaded in the blockchain. Thus, the doctor will continue entering the medical data in his legacy EHR system, and the data will be automatically taken to the blockchain through the API connector.
- Data from various healthcare providers, such as laboratory exams.
- Data from wearables and healthcare tracking devices/sensors (such as fitness trackers or smartwatches).
3.4. System Development and Functionalities
- Registration. A patient is allowed to register through the mobile application into the PatientDataChain platform. The user is stored into the Modex BCDB network after the user will confirm the email provided at registration time. A doctor is allowed to register into the PatientDataChain platform after he receives an invitation by email. After registration, the doctor is redirected to the doctor web platform login page. At the first login, the doctor is prompted to complete his/her profile (title, specialties, medical clinics, contact details). The OAuth 2.0 protocol is used for authentication [65] and generates tokens for single sign-on. The token generation is based on the private key of the user.
- Data fusion. In order to ensure access to an integrated collection of medical data associated to each patient and provide a secure environment for storing personal health records, we developed a data fusion mechanism based on unique identifiers. The system tackles the challenge of data integration in the blockchain by assigning a unique identifier (ID) to each patient. The patient will own his data and can grant access to healthcare providers through a token mechanism, to view the data or to insert new records in his medical file. When a doctor must write on behalf of the patient, first they need to acquire the patient ownerId, generated from the patient identifier created after the first login into the mobile application. The blockchain provides the optimal context to track the unique patient identifier and solving the patient matching issues. In PatientDataChain, the pairing is done using the patientID and ownerID to integrate new data into the patient’s medical history.
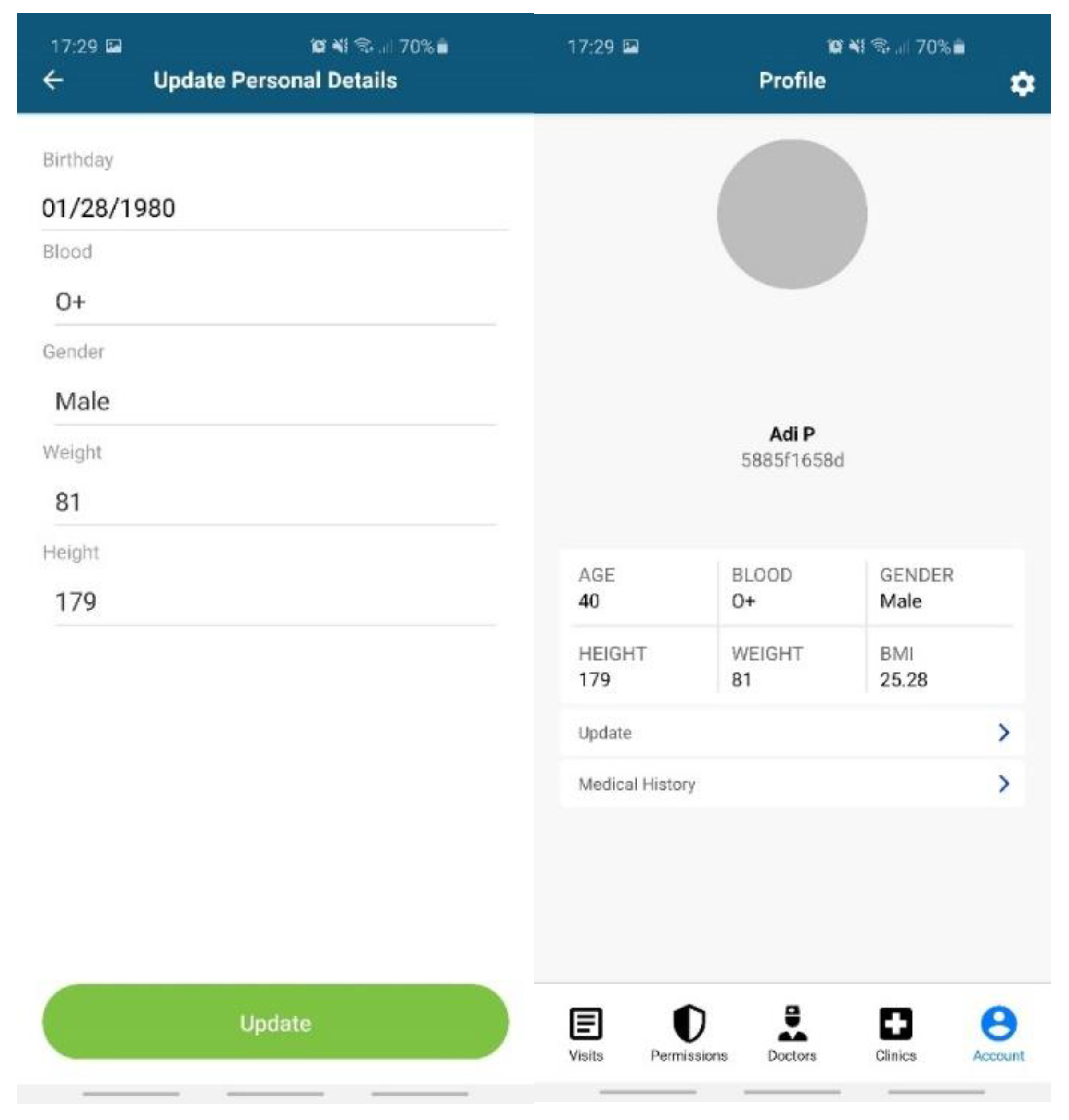
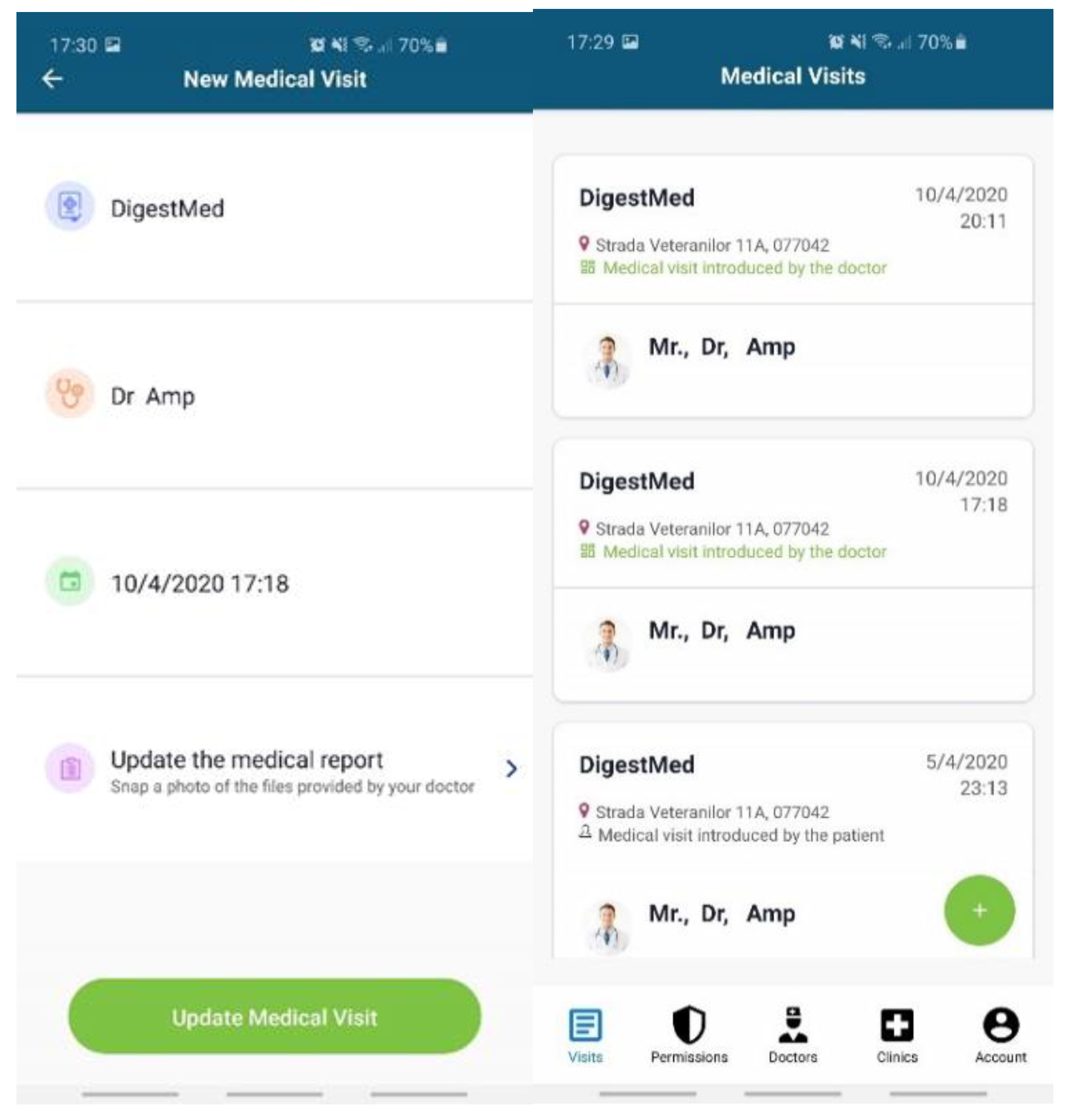
- Data entered by the patient (Figure 7): personal profile (name, age, blood type, gender, height, weight, body mass index (BMI)); allergies; medical history (chronic diseases, surgeries).
- Data from EHR systems. For the moment, we developed a dedicated API based on web services endpoints to connect to Setrio BizMedica [66]—a medical software for managing the activity of individual medical practices and clinics, integrated with the National Healthcare System in Romania. The API interface retrieves data from BizMedica and uses GraphQL queries to insert the data into the Modex BCDB architecture. The blockchain component will store the authenticity elements (timestamp, hash, and encryption key), while the encrypted medical health records will be stored in the MongoDB database, in correlation with the hash from the blockchain. The data from the MongoDB database can only be decrypted with a token generated based on the key in the blockchain. This mechanism enhances security and data protection.
- Doctors and healthcare institutions will continue using their legacy EHR systems, which will be integrated with PatientDataChain through the API interface. The API interface will identify each patient based on his unique ID in PatientDataChain. When a patient visits a doctor, they will grant access to the doctor to view their medical history and insert a new medical record (diagnosis, treatment, lab exams, MRIs, scans, etc.) in PatientDataChain (Figure 8) through a system token generated based on the ownerID field of the patient, which will be valid for a limited time.
- Data from wearables and healthcare tracking sensors, to keep the history of various health indicators as part of the medical history of the patient. Currently, PatientDataChain is integrated with Fitbit devices through the Fitbit web API [67] from Fitbit activity trackers. The data retrieved from the fitness tracker is fused with the medical history of the patient based on the unique ID of the patient. The Get Daily Activity Summary endpoint is used to retrieve a summary and list of a user’s activities and activity log entries for a given day. Other information retrieved from Fitbit devices and integrated into PatientDataChain are related to weight, fat, food logging, heart rate, and sleep.
- 3.
- Data ownership. When a user is created, the system generates a unique pair of private/public keys associated with the new user. The keys will be used with RSA 256 encryption to serve several purposes: user authentication, transaction signing, data encryption/decryption. The private/public keys sets are stored on the blockchain, in a dedicated authentication and licensing node. The data ownership is established through the following mechanism: when a patient is logged in and a new record of data needs to be inserted into his medical file, the private key of the patient will be used to encrypt the data. The hash of the data will be stored in the licensing node, whereas the encrypted medical data is stored in the MongoDB database. The private key is what grants a patient ownership of his medical health records.
- 4.
- Medical Records Permission Control. Only the patient will be able to see his medical records and, on demand, the patient can give permission to a specific doctor or healthcare provider for a period of seven days. Once the patient has given permission to a doctor to see their medical history, the information will be available for the doctor on the web platform. This permission-granting mechanism is based on the private/public key of the patient. When the patient wants to grant access to a doctor to see the data, a token will be generated based on the public key of the patient, which will allow the doctor to access the medical files and also to insert a new medical visit.
4. Validation and Discussion
4.1. Methodology
- assess the main functionalities of the system and the data exchange features
- analyze the performance of a blockchain-based system and assess the scale-up possibilities
4.2. Validation of the System Functionalities
- Reading/writing functionalities for the patient/owner of the PHR
- Integration with the EHR system
- Acquiring a short-term user access token for granting access to data
- Getting logged-user details
- Getting doctor profile details
- Getting a patient ownerId based on the patient’s unique identifier
- Writing a medical report and visit on behalf of a patient
- Inserting a medical report
- Inserting a medical visit
- Attaching files to a medical report on behalf of a patient
- Acquiring healthcare data from a fitness tracker
4.2.1. Getting a Patient OwnerId Using the Patient Identifier
curl --location --request POST ‘https://chain.setrio.ro/api/data/filter/Identifier?skip=0&limit=1’ \
--header ‘Authorization: Bearer -sm0n18N7MJJzY_og88N95HX8pnndskzGGcw5GaNaU8’ \
--header ‘Content-Type: application/json’ \
--data-raw ‘{
“filter”: {
“patientId”: “fde53c5a11”
}
}’
{
“records”: [
{
“_id”:”59ea2347d6139195b183f5988b4d527710c385c6fed7119699129e94b3769c8f”,
“metadata”: {
“previousBlockId”: “2BBA75BB049B2A0D1F91709903219CB1FD1242178157B2EC6BC28F1CED4306EA”,
“blockId”: “49”,
“id”: “59ea2347d6139195b183f5988b4d527710c385c6fed7119699129e94b3769c8f”,
“blockNum”: “49”,
“version”: 2,
“previousRecordBlockId”: “c4db13e4424fe2865138c0145c7fdd111b728609f4b581cb61ab29a4e8837214”,
“recordId”: “386609bcadcfada54a0c26bdc8f408060d145abc19bff21c2e2f8e4e9d949f8f62bf20”,
“ownerId”: “3866093b83947ddbbf48ec39667fcb6ef2d235992caf5107f0f5e5337fa57810e869bd”,
“status”: “COMMITTED”,
“transactionId”: “59ea2347d6139195b183f5988b4d527710c385c6fed7119699129e94b3769c8f”,
“createdBy”: “3866093b83947ddbbf48ec39667fcb6ef2d235992caf5107f0f5e5337fa57810e869bd”,
“createdAt”: “2020-07-16 14:48:56”,
“modifiedBy”: “3866093b83947ddbbf48ec39667fcb6ef2d235992caf5107f0f5e5337fa57810e869bd”,
“modifiedAt”: “2020-07-16 14:49:06”,
“dataType”: “JSON”,
“nodeId”: “HF-data-01”,
“recordPermission”: “PERMISSIONED”,
“networkIdentifier”: “OPEN”,
“recordSignature”: “5ea3b0b94bd2b8c46f0c97e7fe5d85a4d6dde6f13b652f2173790d0620600d64cea5947839f9caa05ab450a1339a332723c00d668d93c83985f2a167d66b4119”
},
“ownerId”: “3866093b839439a92b368bbedc271cf663c125748982ea4a938096940dfa88e2f49013”,
“patientId”: “fde53c5a11”,
“validated”: “true”
}
]
}
-
Writing a medical report and visit on behalf of a patient
-
Inserting a medical report
curl --location --request POST ‘https://chain.setrio.ro/api/data/MedicalReport?ownerId=3866093b839439a92b368bbedc271cf663c125748982ea4a938096940dfa88e2f49013′ \
--header ‘Authorization: Bearer MNHx6lDQxvzEE-nKchhZmx74L9j2-Q4Z5I6Bh18k_kM’ \
--header ‘Content-Type: application/json’ \
--data-raw ‘{
“diagnosis”: “Hashimoto syndrome”,
“symptoms”: “thyroide is huge”,
“observations”: “take care of you”,
“documents”: [
{
“name”: “medical_report.pdf”,
“serialNo”: “12342r43fr544”,
“description”: “Lorem ipsum”,
“addByUser”: false
},
{
“name”: “reteta.pdf”,
“serialNo”: “xxxx79832793”,
“description”: “Lorem ipsum”,
“addByUser”: false
}
]
}’
{
“transactionId”: “cb2cf0a5e7bd96c706417349448904adc6b119becfc466b369bdd1cae80ca1f6”,
“recordId”: “3866099799650f037ea4694bc0b12c56ab9f5c77728bc3a50056ae865ce2d9d3773513”,
“version”: 1,
“ownerId”: “3866093b839439a92b368bbedc271cf663c125748982ea4a938096940dfa88e2f49013”,
“createdBy”: “3866093b8394889db747715de07b33c196a123ceeaf3fbbc2b94729f9fc2b00b70196e”,
“createdAt”: “2020-07-16 14:57:38”,
“recordPermission”: “PERMISSIONED”,
“nodeId”: “HF-data-01”,
“networkIdentifier”: “OPEN”,
“dataType”: “JSON”,
“systemEntity”: false
}
-
Inserting a medical visit
- Medical clinic record ID (metadata.recordId of the medical clinic record from the Practice entity)
- Doctor record ID (metadata.recordId of the doctor’s record from the Provider entity)
- Medical report record ID (metadata.recordId of the medical report record from the MedicalReport entity)
curl --location --request POST ‘https://chain.setrio.ro/api/data/MedicalVisit?ownerId=3866093b839439a92b368bbedc271cf663c125748982ea4a938096940dfa88e2f49013′ \
--header ‘Authorization: Bearer MNHx6lDQxvzEE-nKchhZmx74L9j2-Q4Z5I6Bh18k_kM’ \
--header ‘Content-Type: application/json’ \
--data-raw ‘{
“practice”: “386609295f8eb49e42aa726383076fe90dde29303dc344616d7e9dd3cab3e283ffe6ea”,
“provider”: “386609c5a8fdd3f99d3d2f6c26c8dbc09ffb1e1a66cf762e93aa02b6f3a9f6daeeb1e2”,
“startDate”: “2020-02-20T14:00:00”,
“addByUser”: false,
“medicalReport”: “38660997996588813eb31566aff65f7b274338c2f19189224ebc184114851bcb882b8e”
}’
{
“transactionId”: “ca510e0a4de3f1c777ca223f14270231ed8a250756cafbbf9bb04ac62f68653a”,
“recordId”: “3866098bedcf801d694fc2f5c490f0f05091dc78cd54a101f68ebc51dee0923808b373”,
“version”: 1,
“ownerId”: “3866093b839439a92b368bbedc271cf663c125748982ea4a938096940dfa88e2f49013”,
“createdBy”: “3866093b8394889db747715de07b33c196a123ceeaf3fbbc2b94729f9fc2b00b70196e”,
“createdAt”: “2020-07-16 14:58:07”,
“recordPermission”: “PERMISSIONED”,
“nodeId”: “HF-data-01”,
“networkIdentifier”: “OPEN”,
“dataType”: “JSON”,
“systemEntity”: false
}
4.2.2. Attaching Files to a Medical Report on Behalf of a Patient
curl --location --request POST ‘https://chain.setrio.ro/api/data/file/upload?ownerId=3866093b839439a92b368bbedc271cf663c125748982ea4a938096940dfa88e2f49013′ \ --header ‘Content-Type: application/json’ \ --header ‘Authorization: Bearer MNHx6lDQxvzEE-nKchhZmx74L9j2-Q4Z5I6Bh18k_kM’ \ --form ‘qqfile =@/home/user/doc.png’ \ --form ‘referenceId=38660997996588813eb31566aff65f7b274338c2f19189224ebc184114851bcb882b8e’ \ --form ‘referenceName=MedicalReport’ \ --form ‘mimeType=image/jpeg’ \ --form ‘qquuid=sdfsdfsdfsds’ \ --form ‘qqfilename=doc1.jpg’
{
“code”: 2000,
“success”: true,
“message”: “File uploaded successfully!”
-
Acquiring healthcare data from a fitness tracker
curl --location --request POST ‘https://chain.setrio.ro/api/data/FitbitCharge?ownerId=3866093b839439a92b368bbedc271cf663c125748982ea4a938096940dfa88e2f49013′ \ --header ‘Authorization: Bearer MNHx6lDQxvzEE-nKchhZmx74L9j2-Q4Z5I6Bh18k_kM’ \ --header ‘Content-Type: application/json’ \ -- GET https://api.fitbit.com/1/user/-/activities/heart/date/today/1d.json }’
{
“transactionId”: “cb2cf0a5e7bd96c706417349448904adc6b119becfc466b369bdd1cae80ca1f6”,
“recordId”: “3866099799650f037ea4694bc0b12c56ab9f5c77728bc3a50056ae865ce2d9d3773513”,
“version”: 1,
“ownerId”: “3866093b839439a92b368bbedc271cf663c125748982ea4a938096940dfa88e2f49013”,
“createdBy”: “3866093b8394889db747715de07b33c196a123ceeaf3fbbc2b94729f9fc2b00b70196e”,
“createdAt”: “2020-07-16 14:57:38”,
“recordPermission”: “PERMISSIONED”,
“nodeId”: “HF-data-01”,
“networkIdentifier”: “OPEN”,
“dataType”: “JSON”,
“systemEntity”: false
“activities-heart”: [
{
“dateTime”: “2020-08-04”,
“value”: {
“customHeartRateZones”: [],
“heartRateZones”: [
{
“caloriesOut”: 273.2109,
“max”: 135,
“min”: 89,
“minutes”: 40,
“name”: “Fat Burn”
},
{
“caloriesOut”: 315.6609,
“max”: 179,
“min”: 128,
“minutes”: 60,
“name”: “Cardio”
},
{
“caloriesOut”: 122,
“max”: 215,
“min”: 175,
“minutes”: 5,
“name”: “Peak”
}
],
“restingHeartRate”: 73
}
}
]
}
- -
- The creation of patient and doctor users;
- -
- The registration of medical history by the patient, through the mobile application;
- -
- Integration connector with EHR type applications that can send information in the patient’s digital medical file;
- -
- The web interface through which doctors can view the medical history of patients who grant them the necessary permissions;
- -
- Integration connector with fitness tracker devices from which we collect healthcare data and integrate it into the patients’ PHR;
- -
- Data exchange and immutability granted by the blockchain technology.
4.3. Analysis of the System Performance and Scalability
- Enhance the scalability of the system and the blockchain capabilities to support a larger number of users.
- Provide integration with pharmacies management software, to link the entire medical chain: doctor–patient–pharmacy. This includes the following functionalities:
- -
- Develop dedicated API interfaces to connect with specific pharmacy management systems.
- -
- Allow pharmacies registered in the system to display information about the availability of the stock of medicines and their selling prices.
- -
- Patients can search for the availability of some medicines at the pharmacies in the platform that are located on a certain selected radius.
- -
- Online reservation of the products found by the search described above and the patient can be notified by the pharmacy when the order is ready for pick-up.
- Automate management of the treatments prescribed to the patient by the doctor—by defining the treatment schemes in the patients’ application and then guiding the patient during the treatment by reminding them of the times when they must take the pills.
- Generate automatic refill orders to pharmacies, for medicines that are part of the treatments and are reaching the minimum stock amount where the refill must be done.
- Implement big data analytics for predictive functionalities.
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Allied Market Research. Healthcare IT Market or Healthcare Information Technology Market Overview. Available online: https://www.alliedmarketresearch.com/healthcare-information-technology-market (accessed on 5 August 2020).
- HealthIT.gov—Office of the National Coordinator for Health IT. What Is an Electronic Health Record? Available online: https://www.healthit.gov/faq/what-electronic-health-record-ehr (accessed on 24 July 2020).
- HealthIT.gov—Office of the National Coordinator for Health IT. What Is a Personal Health Record? Available online: https://www.healthit.gov/faq/what-personal-health-record-0 (accessed on 24 July 2020).
- ISO/TR 14639-2:2014 Health Informatics—Capacity-based eHealth Architecture Roadmap—Part 2: Architectural Components and Maturity Model. Available online: https://www.iso.org/standard/54903.html (accessed on 24 July 2020).
- ISO. Health Informatics—Capacity-Based eHealth Architecture Roadmap—Part 2: Architectural Components and Maturity Model, Technical Report (ISO/TRTR14639-2). Available online: https://www.iso.org/obp/ui/#iso:std:iso:tr:14639:-2:ed-1:v1:en (accessed on 24 July 2020).
- Heart, T.; Ben-Assuli, O.; Shabtai, I. A review of PHR, EMR and EHR integration: A more personalized healthcare and public health policy. Health Policy Technol. 2017, 6, 20–25, ISSN 2211-8837. [Google Scholar] [CrossRef]
- Menachemi, N.; Collum, T.H. Benefits and drawbacks of electronic health record systems. Risk Manag. Healthc. Policy 2011, 2011, 47–55. [Google Scholar] [CrossRef]
- Bhartiya, S.; Mehrotra, D.; Girdhar, A. Issues in achieving complete interoperability while sharing electronic health records. Procedia Comput. Sci. 2016, 78, 192–198. [Google Scholar] [CrossRef]
- Tang, P.; Ash, J.; Bates, D.; Overhage, J.; Sands, D. Personal health records: Definitions, benefits, and strategies for overcoming barriers to adoption. J. Am. Med. Informatics Assoc. 2006, 13, 121–126. [Google Scholar] [CrossRef]
- Roehrs, A.; Da Costa, C.A.; da Rosa Righi, R.; de Oliveira, K.S.F. Personal health records: A systematic literature review. J. Med. Internet Res. 2017, 19, e13. [Google Scholar] [CrossRef]
- George, T.P.; Hopla, D.L. Advantages of personal health records. Nurs. Crit. Care 2015, 10, 10–12. [Google Scholar] [CrossRef]
- HIMSS Guide. Interoperability in Healthcare. Available online: https://www.himss.org/resources/interoperability-healthcare (accessed on 10 October 2020).
- ICD-10. Available online: https://www.cms.gov/Medicare/Coding/ICD10/index?redirect=/icd10 (accessed on 10 October 2020).
- NCD. Available online: https://www.fda.gov/drugs/drug-approvals-and-databases/national-drug-code-directory (accessed on 10 October 2020).
- SNOMED. Available online: http://www.snomed.org/ (accessed on 10 October 2020).
- LOINC. Available online: https://loinc.org/ (accessed on 10 October 2020).
- HL7. Available online: https://www.hl7.org/ (accessed on 10 October 2020).
- DICOM. Available online: https://www.dicomstandard.org/ (accessed on 10 October 2020).
- FHIR. Available online: https://www.hl7.org/fhir/overview.html (accessed on 10 October 2020).
- HIPAA. Available online: https://www.hhs.gov/hipaa/index.html (accessed on 10 October 2020).
- CYBERSECURITY AND PRIVACY. GDPR Security and Privacy Need-to-Knows. Available online: https://www.himss.org/resources/gdpr-security-and-privacy-need-knows (accessed on 10 October 2020).
- Dunn, J.; Runge, R.; Snyder, M. Wearables and the medical revolution. Pers. Med. 2018, 15, 429–448. [Google Scholar] [CrossRef]
- Lobelo, F.; Kelli, H.M.; Tejedor, S.C.; Pratt, M.; McConnell, M.V.; Martin, S.S.; Welk, G.J. The wild Wild West: A framework to integrate mHealth software applications and wearables to support physical activity assessment, counseling and interventions for cardiovascular disease risk reduction. Prog. Cardiovasc. Dis. 2016, 58, 584–594. [Google Scholar] [CrossRef]
- Channa, A.; Popescu, N.; Ciobanu, V. Wearable solutions for patients with Parkinson’s disease and neurocognitive disorder: A systematic review. Sensors 2020, 20, 2713. [Google Scholar] [CrossRef]
- Voicu, R.-A.; Dobre, C.; Bajenaru, L.; Ciobanu, R.-I. Human physical activity recognition using smartphone sensors. Sensors 2019, 19, 458. [Google Scholar] [CrossRef]
- Research and Markets. Global Wearable Technology in Healthcare (Medical, Healthcare and Wellness) Market 2020–2027. Available online: https://www.globenewswire.com/news-release/2020/09/09/2090913/0/en/Global-Wearable-Technology-in-Healthcare-Medical-Healthcare-and-Wellness-Market-2020-2027.html (accessed on 11 October 2020).
- Carfagno, J. 5 New and Emerging Wearable Medical Devices, Online Review, 2019. Available online: https://www.docwirenews.com/docwire-pick/future-of-medicine-picks/top-5-wearable-medical-devices/ (accessed on 10 August 2020).
- Green, E.M.; van Mourik, R.; Wolfus, C.; Heitner, S.B.; Dur, O.; Semigran, M.J. Machine learning detection of obstructive hypertrophic cardiomyopathy using a wearable biosensor. NPJ Digit. Med. 2019, 2, 57. [Google Scholar] [CrossRef]
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable sensors for remote health monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef]
- Chung, P.-C.; Hsu, Y.-L.; Wang, C.-Y.; Lin, C.-W.; Wang, J.-S.; Pai, M.-C. Gait analysis for patients with Alzheimer’s disease using a triaxial accelerometer. In Proceedings of the IEEE International Symposium on Circuits and Systems (ISCAS), Seoul, Korea, 20–23 May 2012; pp. 1323–1326. [Google Scholar] [CrossRef]
- Reches, T.; Dagan, M.; Herman, T.; Gazit, E.; Gouskova, N.A.; Giladi, N.; Manor, B.; Hausdorff, J.M. Using wearable sensors and machine learning to automatically detect freezing of gait during a FOG-provoking test. Sensors 2020, 20, 4474. [Google Scholar] [CrossRef]
- Wang, L.; Lou, Z.; Jiang, K.; Shen, G. Bio-multifunctional smart wearable sensors for medical devices. Adv. Intell. Syst. 2019, 1. [Google Scholar] [CrossRef]
- GlobalData Report. Wearable Technology in Healthcare. Available online: http://www.tauli.cat/institut/wp-content/uploads/2020/06/wearables-GlobalData_WearableTechnologyinHealthcare_220819.pdf (accessed on 10 August 2020).
- Gupta, M. Blockchain for Dummies, IBM Limited ed.; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2017. [Google Scholar]
- Muzny, M.; Henriksen, A.; Giordanengo, A.; Muzik, J.; Grottland, A.; Blixgard, H.; Hartvigsen, G.; Arsand, E. Wearable sensors with possibilities for data exchange: Analyzing status and needs of different actors in mobile health monitoring systems. Int. J. Med. Inform. 2020, 133, 104017. [Google Scholar] [CrossRef]
- Wachter, R.M. Making IT Work: Harnessing the Power of Health Information Technology to Improve Care in England, Report of the National Advisory Group on Health Information Technology in England. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/550866/Wachter_Review_Accessible.pdf (accessed on 10 October 2020).
- HIPAA Journal. Largest Healthcare Data Breaches of 2018. Available online: https://www.hipaajournal.com/largest-healthcare-data-breaches-of-2018/ (accessed on 25 August 2020).
- Chen, H.S.; Jarrell, J.T.; Carpenter, K.A.; Cohen, D.S.; Hunag, X. Blockchain in healthcare: A patient-centered model. Biomed. J. Sci. Tech. Res. 2019, 20, 15017–15022. [Google Scholar]
- Powles, J.; Hodson, H. Google DeepMind and healthcare in an age of algorithms. Health Technol. 2017, 7, 351–367. [Google Scholar] [CrossRef]
- Mandl, K.D.; Markwell, D.; MacDonald, R.; Szolovits, P.; Kohane, I.S. Public standards and patients’ control: How to keep electronic medical records accessible but private medical information: Access and privacy doctrines for developing electronic medical records desirable characteristics of electronic medical records challenges and limitations for electronic medical records conclusions commentary: Open approaches to electronic patient records commentary: A patient’s viewpoint. BMJ Clin. Res. 2001, 322, 283–287. [Google Scholar]
- Linn, L.A.; Koo, M.B. Blockchain for Health Data and Its Potential Use in Health It and Health Care Related Research. Available online: https://www.healthit.gov/sites/default/files/11-74-ablockchainforhealthcare.pdf (accessed on 10 October 2020).
- Dinh-Le, C.; Chuang, R.; Chokshi, S.; Mann, D. Wearable health technology and electronic health record integration: Scoping review and future directions. JMIR mHealth uHealth 2019, 7, e12861. [Google Scholar] [CrossRef]
- Roehrs, A.; Da Costa, C.A.; da Rosa Righi, R. OmniPHR: A distributed architecture model to integrate personal health records. J. Biomed. Inform. 2017, 71, 70–81. [Google Scholar] [CrossRef]
- Reeder, B.; David, A. Health at hand: A systematic review of smart watch uses for health and wellness. J. Biomed. Inform. 2016, 63, 269–276. [Google Scholar] [CrossRef]
- Latest Trends in Medical Monitoring Devices and Wearable Health Technology. Available online: https://www.businessinsider.com/wearable-technology-healthcare-medical-devices (accessed on 10 October 2020).
- Flach, J.M.; Schanely, P.; Kuenneke, L.; Chidoro, B.; Mubaslat, J.; Howard, B. Electronic health records and evidence-based practice: Solving the little-data problem. Proc. Int. Symp. Hum. Factors Ergon. Health Care 2018, 7, 30–35. [Google Scholar] [CrossRef]
- Simon, S.K.; Anbananthen, K.S.M.; Lee, S. A ubiquitous personal health record (uPHR) framework. In Proceedings of the International Conference on Advanced Computer Science and Electronics Information (ICACSEI 2013), Beijing, China, 25–26 July 2013. [Google Scholar]
- Spil, T.; Klein, R. Personal health records success: Why Google Health failed and what does that mean for Microsoft Health Vault? In Proceedings of the 47th Hawaii International Conference on System Sciences, Waikoloa, HI, USA, 6–9 January 2014; pp. 2818–2827. [Google Scholar]
- Kemkar, O.S.; Kalode, P. Formulation of distributed electronic patient record system using OpenEMR concept. Int. J. Eng. Innov. Res. 2015, 4, 85–89. [Google Scholar]
- Klein, D.M.; Fix, G.M.; Hogan, T.P.; Simon, S.R.; Nazi, K.M.; Turvey, C.L. Use of the blue button online tool for sharing health information: Qualitative interviews with patients and providers. J. Med Internet Res. 2015, 17, e199. [Google Scholar] [CrossRef]
- Safavi, S.; Shukur, Z. Conceptual privacy framework for health information on wearable device. PLoS ONE 2014, 9, e114306. [Google Scholar] [CrossRef]
- Hailemichael, M.A.; Marco-Ruiz, L.; Bellika, J.G. Privacy-preserving statistical query and processing on distributed OpenEHR data. Stud. Health Technol. Inform. 2015, 210, 766–770. [Google Scholar]
- Yoon, H.J. Blockchain technology and healthcare. Healthc. Inform. Res. 2019, 25, 59–60. [Google Scholar] [CrossRef]
- Stan, O.; Miclea, L. New era for technology in healthcare powered by GDPR and blockchain. In Proceedings of the 6th International Conference on Advancements of Medicine and Health Care through Technology, Cluj-Napoca, Romania, 17–20 October 2018; pp. 311–317. [Google Scholar] [CrossRef]
- Tiganoaia, B.; Cernian, A. Computer Systems for Business and Data Management, Transaction and Security; University Publishing House: Bucharest, Romania, 2019; p. 170. ISBN 978-606-28-0955-3. [Google Scholar]
- MedBlocks. Available online: https://medblocks.org/ (accessed on 10 October 2020).
- Secure Health Chain. Available online: https://secure.health/ (accessed on 10 October 2020).
- MedicalChain. Available online: https://medicalchain.com/en/ (accessed on 10 October 2020).
- Doc.AI. Available online: https://doc.ai/ (accessed on 10 October 2020).
- OmniPHR. Available online: https://www.sciencedirect.com/science/article/pii/S1532046417301089 (accessed on 10 October 2020).
- MIStore. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6028902/ (accessed on 10 October 2020).
- Modex BCDB. Available online: https://modex.tech/blockchain-database-product/ (accessed on 18 August 2020).
- Modex BCDB Architecture. Available online: https://bcdb.modex.tech/docs/?_ga=2.18520113.945759058.1597697725-746203822.1592299666#/intro/architecture (accessed on 20 September 2020).
- GraphQL. Available online: https://graphql.org/ (accessed on 10 October 2020).
- Auth0 2.0 Protocol. Available online: https://auth0.com/docs/flows/authorization-code-flow (accessed on 10 October 2020).
- BizMedica. Available online: https://setrio.ro/bizmedica/?gclid=Cj0KCQjwuL_8BRCXARIsAGiC51AyUrkDoVrqvEucQea1wAX-5c9YB0DMogkxqD7cyQsHBjR2P21pVDAaAmmHEALw_wcB (accessed on 12 October 2020).
- Fitbit Web API. Available online: https://dev.fitbit.com/ (accessed on 30 September 2020).
- McCoy, A.B.; Wright, A.; Kahn, M.G.; Shapiro, J.S.; Bernstam, E.V.; Sittig, D.F. Matching identifiers in electronic health records: Implications for duplicate records and patient safety. BMJ Qual. Saf. 2013, 22, 219–224. [Google Scholar] [CrossRef]


| Category | Standard | Short Description |
|---|---|---|
| Vocabulary/terminology standards | ICD-10 and ICD-11 [13] | Medical classification list of diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases by the World Health Organization (WHO). |
| NDC [14] | List of all drugs manufactured | |
| SNOMED-CT [15] | Clinical health terminology | |
| LOINC [16] | A universal code system for identifying health measurements, observations and documents. | |
| Content standards | HL7 [17] | Messaging standard that allows the exchange of clinical data between systems |
| Transport standards | DICOM [18] | The standard for the communication and management of medical imaging information. |
| FHIR [19] | An HL7 standard for electronic exchange of healthcare information | |
| Privacy and security standards | HIPAA [20] | Privacy and security of protected health information (US) |
| GDPR [21] | Privacy and security of protected information (Europe) |
| Name | Type of System | Description |
|---|---|---|
| MedBlocks [56] | Electronic medical records (EMR) | P2P filesystem made immutable using distributed ledger technology, for storing medical records. Strength: improved consensus mechanism to ensure the network is not overloaded |
| Secure Health Chain [57] | EMR | Stores electronic personal medical records on a blockchain and ensures that only authorized parties, who have been granted permission, can access data. |
| MedicalChain [58] | EMR | Decentralized platform that enables storage, exchange and use of medical data. It enables the user to give healthcare professionals access to their personal health data. |
| Doc.AI [59] | Generate insights from medical data | Enterprise AI platform that uses natural language processing, computer vision and blockchain to generate insights from medical data. |
| OmniPHR [60] | PHR | Distributed system for storing patient health data. It stores different patient datasets into different blocks on the chain |
| MIStore [61] | Medical Insurance Storage System | A blockchain-based medical insurance storage system |
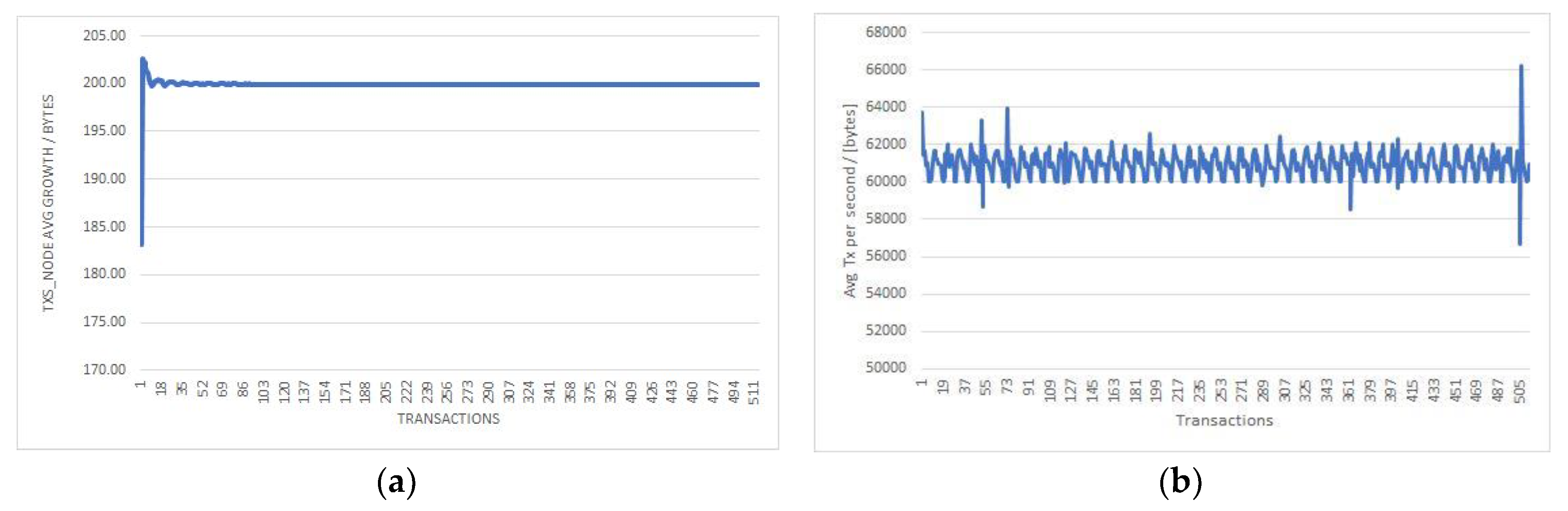
| Number of Transactions | TXs_Node Average Growth/Transaction (Bytes) | Total Logs Growth/Transaction (Bytes) | Average Disk Used Growth/Transaction (Gigabytes) | Average TX Per Second (Bytes) | |
|---|---|---|---|---|---|
| Node 1 | 514 | 60937 | 60934 | 0.22 | 199.90 |
| Node 2 | 523 | 60939 | 60936 | 0.21 | 198.80 |
| Node 3 | 568 | 60934 | 60932 | 0.19 | 200.10 |
| Node 4 | 547 | 60925 | 60929 | 0.17 | 196.90 |
| Node 5 | 507 | 60936 | 60933 | 0.21 | 199.40 |
| Node 6 | 530 | 60937 | 60934 | 0.22 | 199.90 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cernian, A.; Tiganoaia, B.; Sacala, I.; Pavel, A.; Iftemi, A. PatientDataChain: A Blockchain-Based Approach to Integrate Personal Health Records. Sensors 2020, 20, 6538. https://doi.org/10.3390/s20226538
Cernian A, Tiganoaia B, Sacala I, Pavel A, Iftemi A. PatientDataChain: A Blockchain-Based Approach to Integrate Personal Health Records. Sensors. 2020; 20(22):6538. https://doi.org/10.3390/s20226538
Chicago/Turabian StyleCernian, Alexandra, Bogdan Tiganoaia, Ioan Sacala, Adrian Pavel, and Alin Iftemi. 2020. "PatientDataChain: A Blockchain-Based Approach to Integrate Personal Health Records" Sensors 20, no. 22: 6538. https://doi.org/10.3390/s20226538
APA StyleCernian, A., Tiganoaia, B., Sacala, I., Pavel, A., & Iftemi, A. (2020). PatientDataChain: A Blockchain-Based Approach to Integrate Personal Health Records. Sensors, 20(22), 6538. https://doi.org/10.3390/s20226538








