Fully Convolutional Deep Neural Networks with Optimized Hyperparameters for Detection of Shockable and Non-Shockable Rhythms
Abstract
1. Introduction
2. ECG Databases
2.1. Public Holter Databases
- AHA fibrillation database (AHADB) [61], including 30 min ECG recordings from 10 patients (files A8001 to A8010); only the first out of the two available ECG channels is used;
- Massachusetts Institute of Technology – Beth Israel Hospital (MIT-BIH) malignant ventricular ectopy database (VFDB) [62,63,64], including 35 min ECG recordings from 22 patients (files 418 to 430; 602, 605, 607, 609, 610, 611, 612, 614, and 615); only the first out of the two available ECG channels is used;
2.2. OHCA Databases
- November 2010–December 2010 (OHCA1 from 226 patients);
- June 2011–September 2011 (OHCA2 from 733 patients).
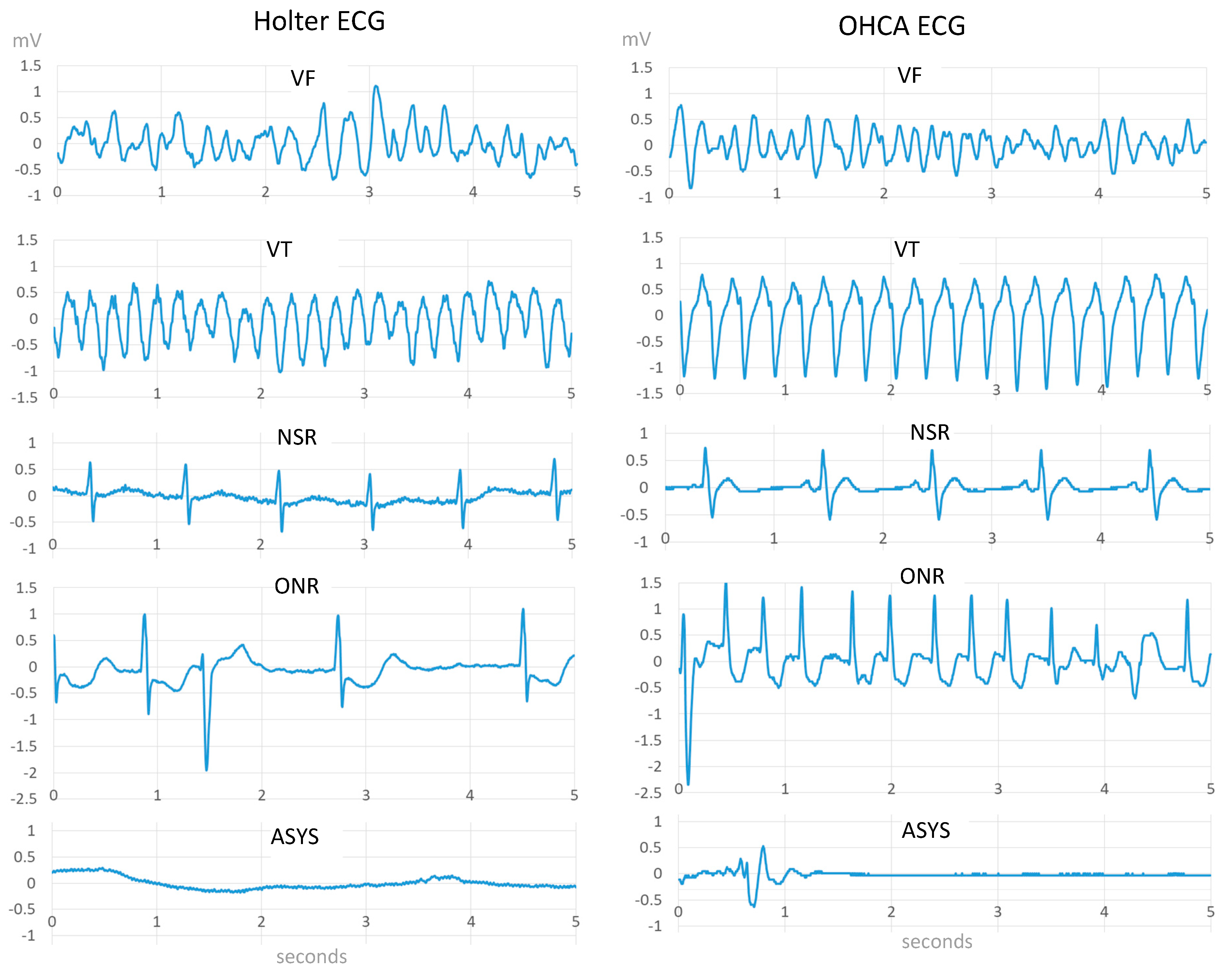
2.3. Rhythm Annotation
- Shockable rhythms, including:
- ○
- Coarse ventricular fibrillation (VF) with amplitude >200 µV;
- ○
- Rapid ventricular tachycardia (VT) with rate >150 bpm;
- Nonshockable rhythms, including:
- ○
- Normal sinus rhythm (NSR) with visible P-QRS-T waves,
- ○
- Other nonshockable rhythms (ONR), such as supraventricular tachycardia, sinus bradycardia, atrial fibrillation and flutter, heart block, idioventricular rhythms, and premature ventricular contractions;
- ○
- Asystole (ASYS), representing ECG signal with peak to peak amplitude <100 µV, lasting more than 4 s;
- Intermediate rhythms, consisting of fine ventricular fibrillations with amplitude in the range 100–200 µV (i.e., between ASYS and VF), and slow ventricular tachycardia with rate <150 bpm. AHA does not set any performance goal for such rhythms [4];
- Inconsistent rhythm (i.e., transition from NSh to Sh);
- Strips that contain extreme artifacts, significant baseline wander, electromyogram noise, pacemaker impulses.
2.4. Training/Validation Subsets
- A training dataset, including all Sh and NSh strips from AHA, CUDB and OHCA1 databases;
- A validation dataset, including all Sh and NSh strips from VFDB and OHCA2 databases.
3. Methods
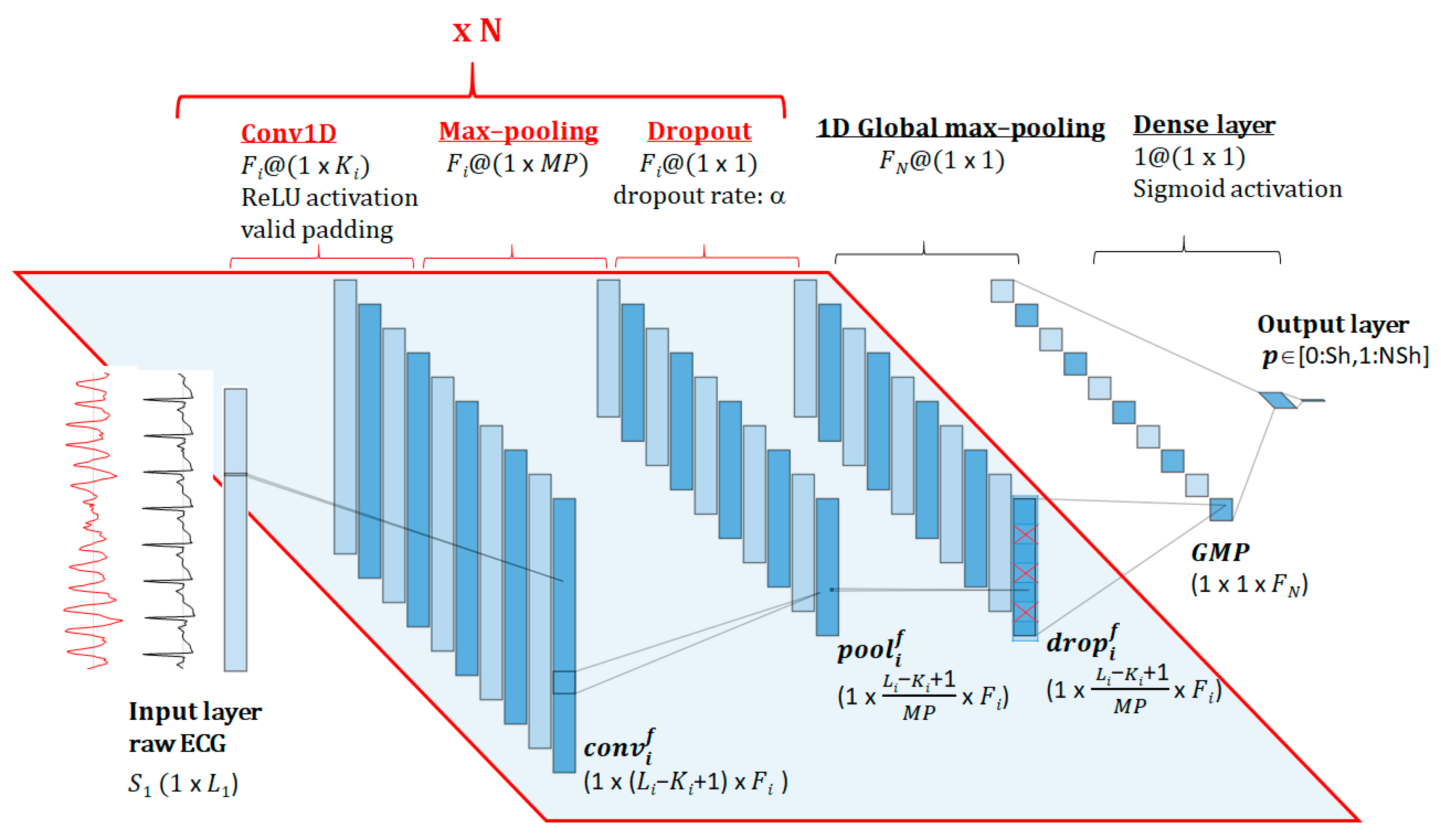
3.1. DNN Architecture
- -
- i = [1, 2, … N] identifies the sequential number of the convolutional layer.
- -
- Si is the input vector of the ith convolutional layer, with size (1 × Li).
- -
- j = [0, 1, … Li – Ki + 1] indexes the output feature vector, applying convolutional operation with a valid padding [37].
- -
- are the weights and are the biases of the convolution kernel;
- -
- A is the applied nonlinear activation function ReLU (rectified linear unit);
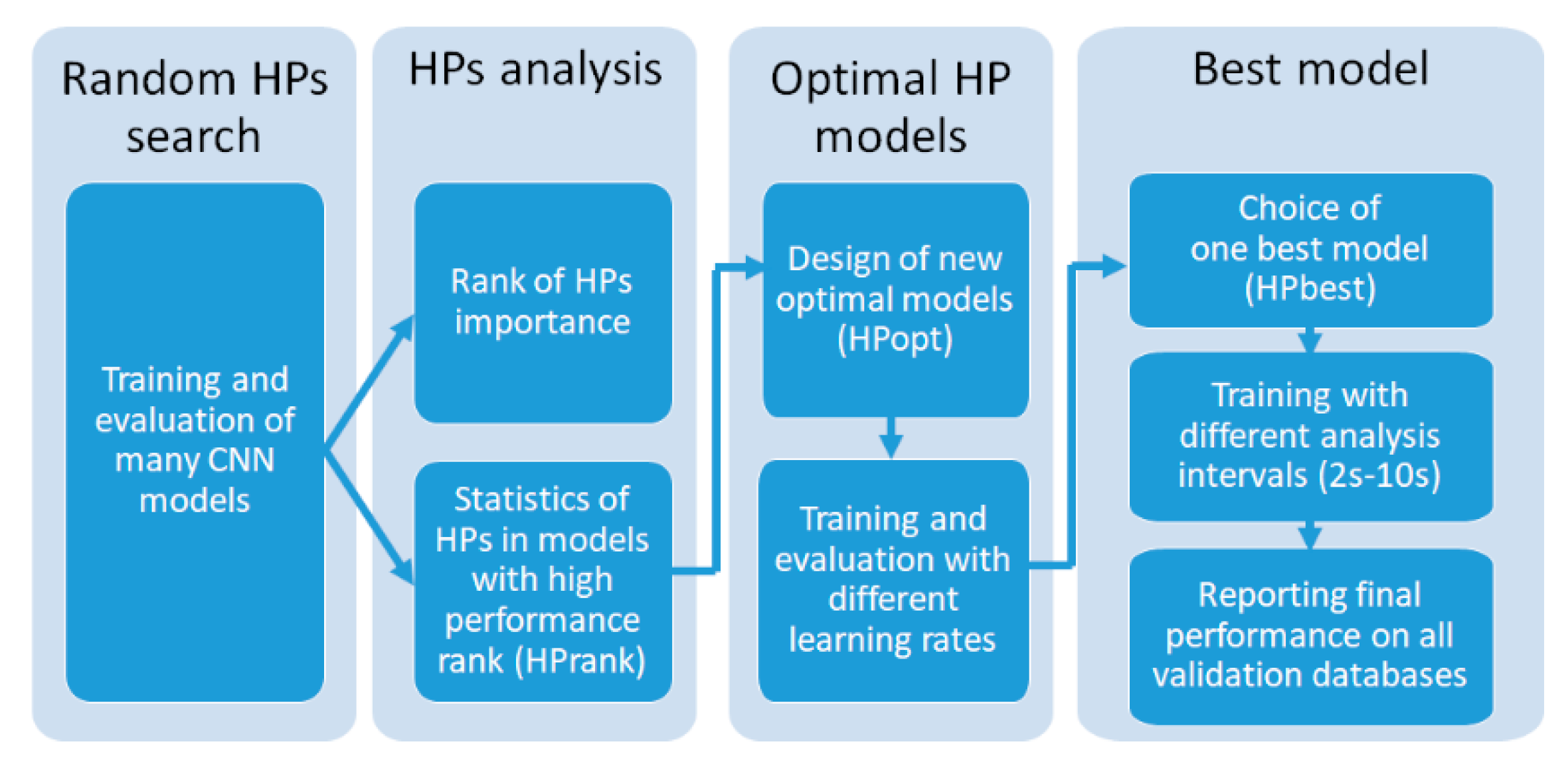
3.2. Hyperparameters Optimization
- Number of sequential CNN blocks (N), which virtually represents the depth of the network;
- Number of filters (Fi) and kernel size (Ki) of Conv1D in each sequential block (i = 1, 2, … N) that majorly influence the feature map representations of the ECG signal;
- Max-pooling size: A minimal fixed setting MP = 2 is used to gradually subsample the feature space at each sequential CNN block N, thus providing conditions to build deeper networks;
3.2.1. Random HP Search
- N = {1, 2, 3, 4, 5, 6, 7};
- Fi = {5, 10, 15, 20, 25, 30, 40, 50}; additional range F1 = {75, 100, 125, 150, 200} is included in the search space only for the shallowest CNN (N = 1), aiming to increase the number of trainable parameters to levels comparable to deeper CNNs (N > 1);
- Ki = {5, 10, 15, 20, 25, 30, 40, 50, 60, 70, 85, 100}; owing to the same reason as above, extra-large kernel sizes K1= {125, 150, 200} are included in the search space of CNN (N = 1);
- The vectors {Fi} and {Ki} are designed to follow a decreasing, increasing or constant trend from top to bottom layers (i = 1, 2, … N) in the same model.
3.2.2. HPs Analysis
3.2.3. Optimal HP Models
3.2.4. Best Model
3.3. Training of DNN Models
- Keep balanced training dataset by replicating the shockable cases four times, considering the ratio of total NSh/Sh cases in Table 1, i.e., after replication the number of Sh cases (4 × 720 = 2880) becomes roughly equal to the number of NSh cases (3170);
- Shuffle the training data for randomization before feeding it into batches;
- Split the training data into batches, because using small batch sizes achieves the best training stability and generalization performance;
- Normalization of the input data is not applied and the input signal resolution of 2.5 μV/LSB is maintained. We purposely keep the real ECG amplitude, since it is characteristic for some of the analyzed rhythms (e.g., ASYS peak-to-peak amplitude <100 µV).
- Training epochs: 400. Early stopping is applied if no improvement in performance is observed for more than 150 epochs;
- Batch size: 256;
- Kernel initializer: random uniform;
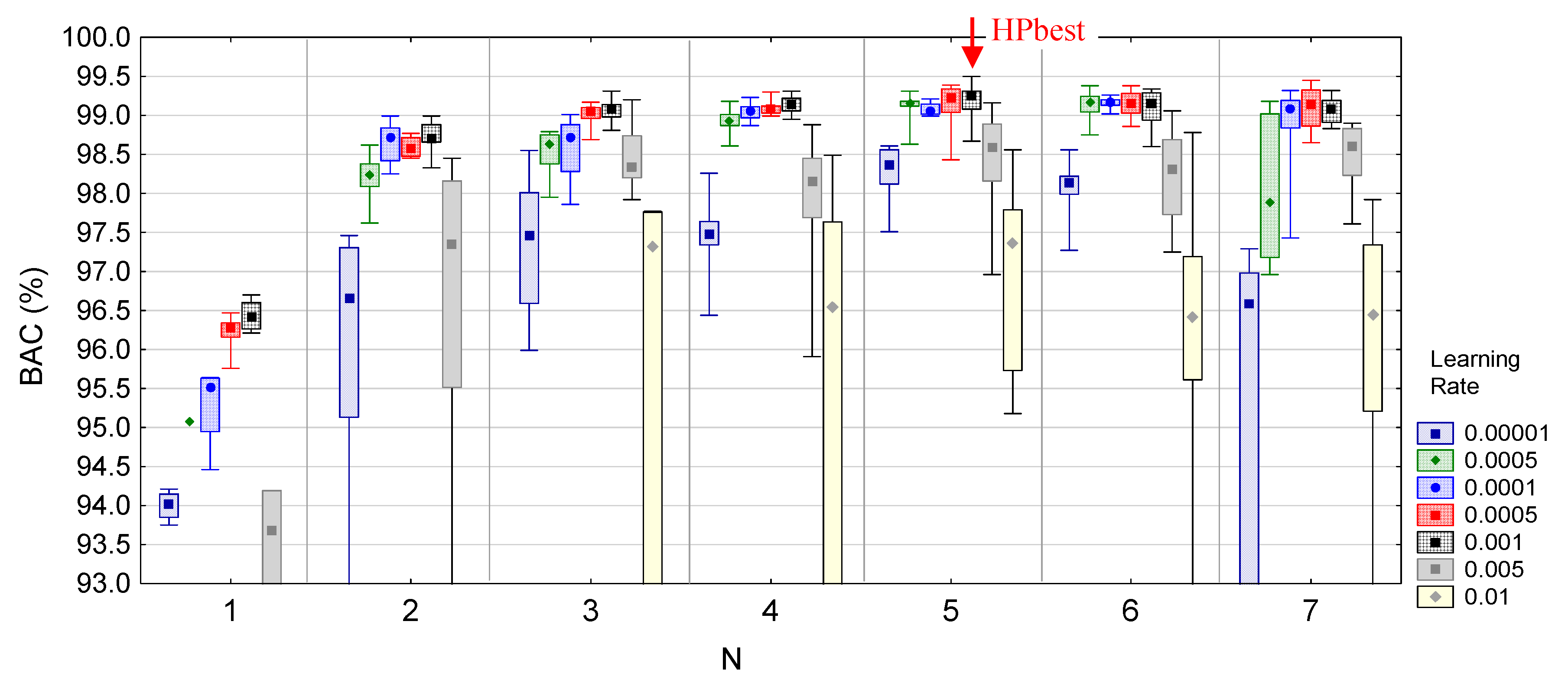
- Optimizer: ‘Adam’ with learning rate LR = 0.001, chosen as a good default setting [37], decay rate DR = LR/epochs, exponential decay rate for the first moment estimates β1 = 0.9 and exponential decay rate for the second moment estimates β2 = 0.999;
- Loss function: binary cross-entropy for 2 target classes (Sh/NSh);
- Metrics function: accuracy = (TP + TN)/(TP + TN + FP + FN). Owing to the concept for balanced training dataset during model fit, the metrics accuracy closely corresponds to BAC.
- Saved model: the model with maximal accuracy after all training epochs.
4. Results
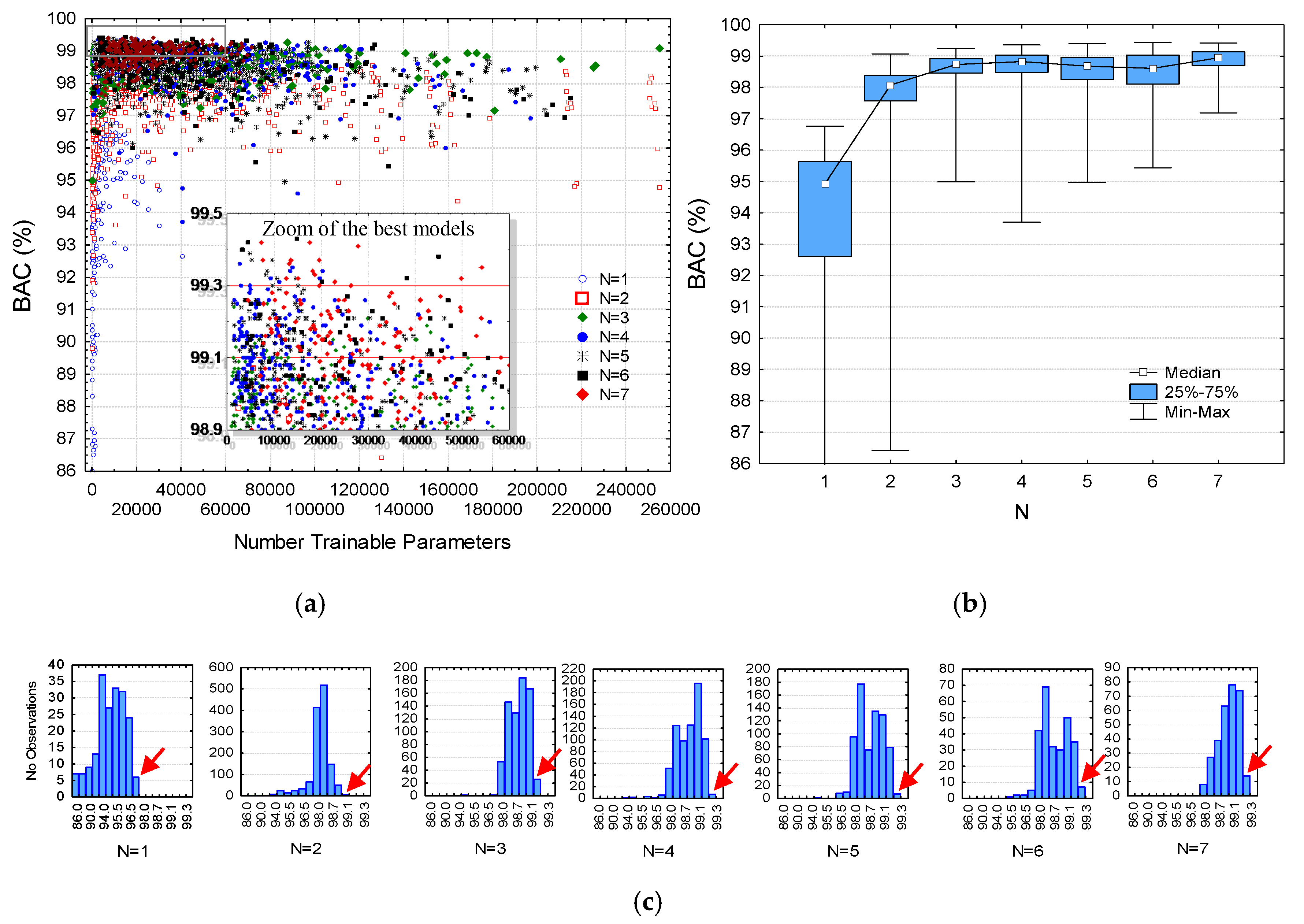
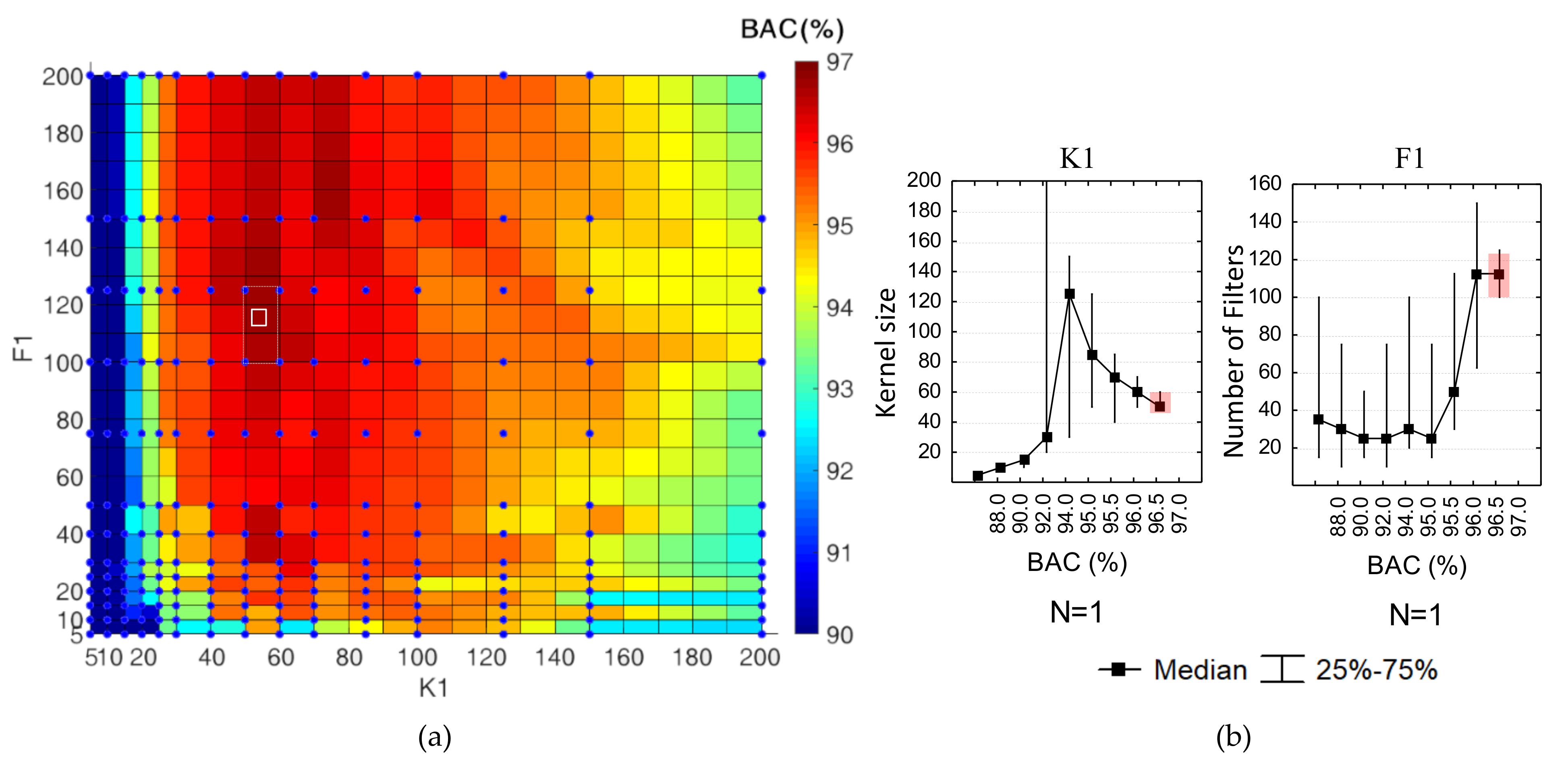
4.1. Random HPs Search
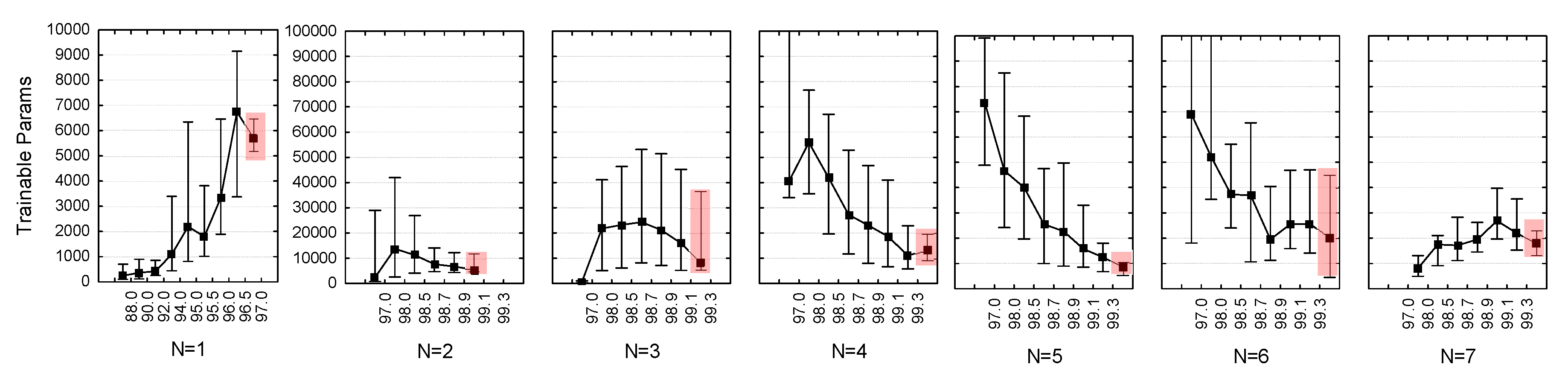
- (N = 1): 195 models, which cover the full search grid (13 filters × 15 kernel sizes). They are trained for 202 (120–298) epochs, reported as median value (quartile range). All models converged within 400 epochs.
- (N = 2): 1305 models trained for 140 (74–226) epochs. The relatively smaller number of trainable parameters than deeper networks resulted in a larger number of trained models generated during the training session;
- (N = 3): 707 models trained for 116 (57–204) epochs;
- (N = 4): 715 models trained for 69 (35–171) epochs;
- (N = 5): 716 models trained for 55 (25–143) epochs;
- (N = 6): 275 models trained for 44 (19–88) epochs;
- (N = 7): 303 models trained for 51 (20–62) epochs. Note the about 2.5-times smaller number of very deep models (N = 6, 7) than (N = 3, 4, 5), which is a consequence of the limited optional values for setting Ki in deeper CNN layers owing to the effect of reaching maximal model shrink with valid padding. In some iterations, the random search algorithm has spent abundant amount of time for finding a valid HPs setting.
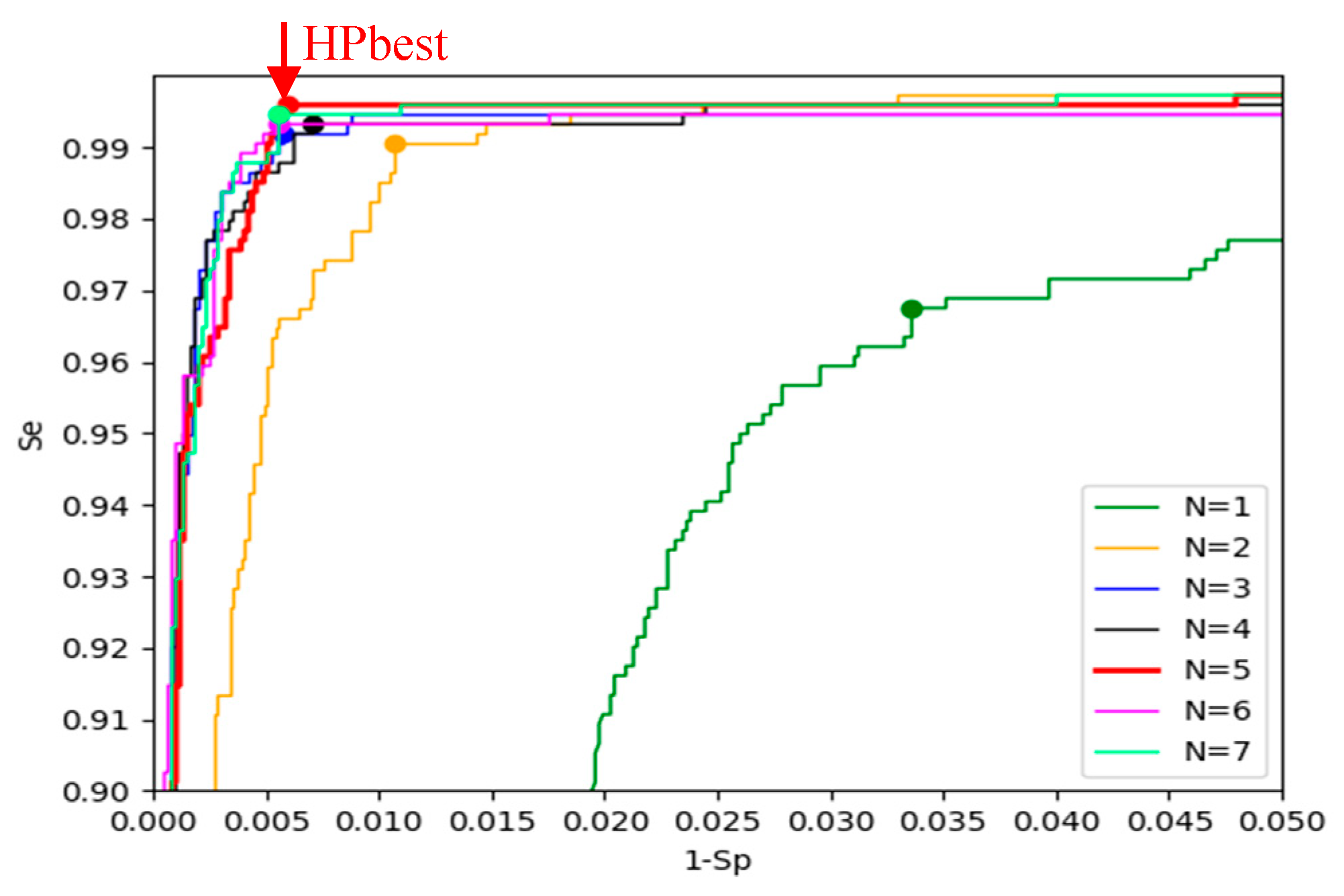
- BAC ≥ 96.5% applied for N = 1 (selecting six models);
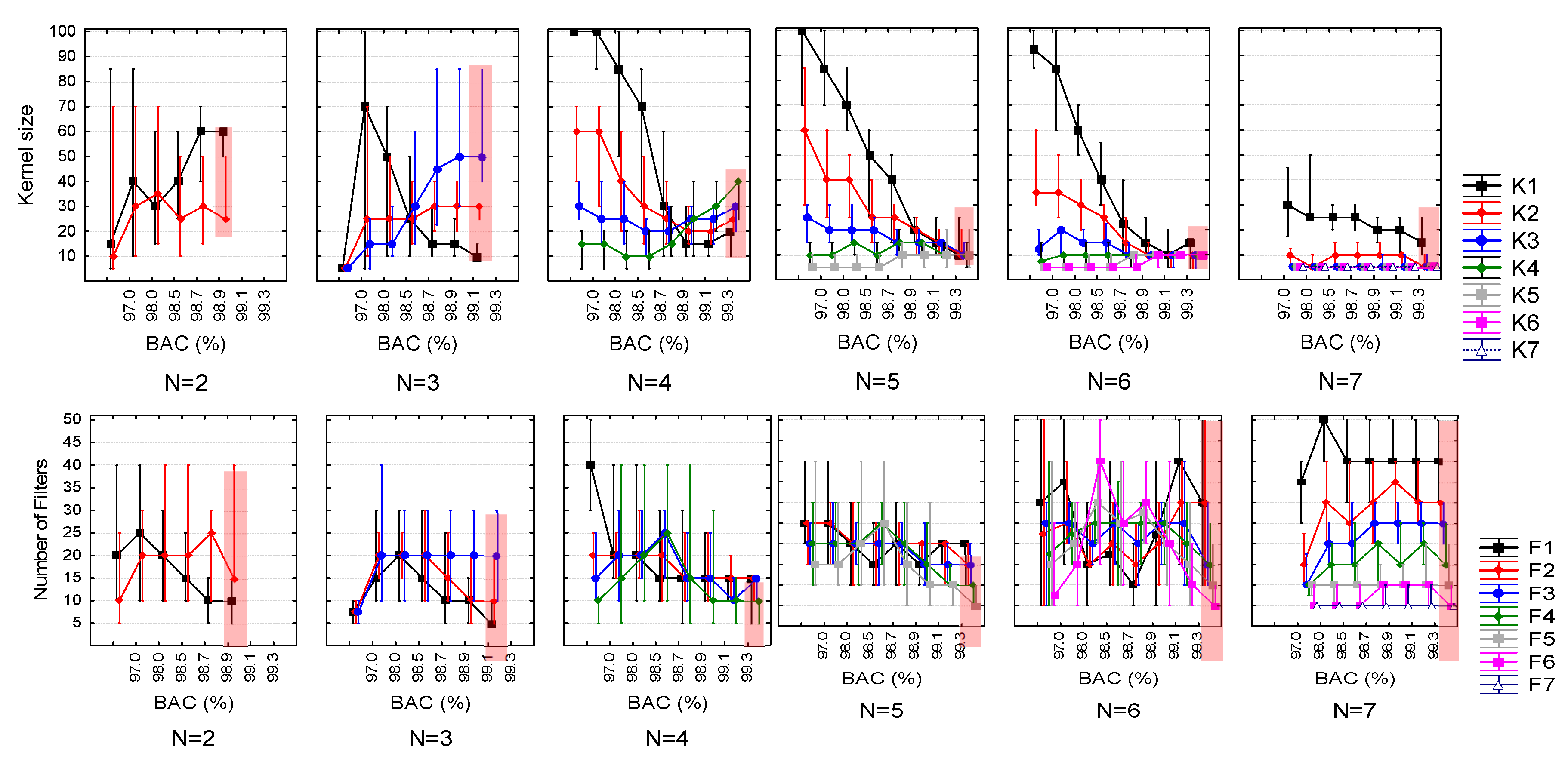
- BAC ≥ 98.9% for N = 2 (five models);
- BAC ≥ 99.1% for N = 3 (26 models);
- BAC ≥ 99.3% for N = 4 (seven models), N = 5 (seven models), N = 6 (seven models), N = 7 (14 models).
4.2. HP Statistical Analysis
4.3. Rank of HPs Importance
4.4. Optimal HP Models
4.5. Best Model
5. Discussion
5.1. HPs Optimization
- -
- Shallow and very deep DNNs (from five to 23 hidden layers), composed by three to 21 layers from one to seven CNN blocks × three layers (Conv1D, max-pooling, dropout) + one GMP + one dense layer for binary classification;
- -
- Different number of filters in each Conv1D layer: , i =1… N;
- -
- Different kernel sizes in each Conv1D layer: , i = 1 … N, valid for fs = 125 Hz.
5.2. Analysis of Our Best CNN Model
- The use of two ECG sources from the most famous public ventricular arrhythmia databases and private OHCA databases provides а robust setting for model optimization on a large scale of ECG rhythms that can be seen by Holters and defibrillators during treatment of cardiac arrest patients. This article uses the largest number of (Sh + NSh) samples for training (720 + 3170) and validation (739 + 5921), which is the important precondition for design of robust deep learning shock advisory systems;
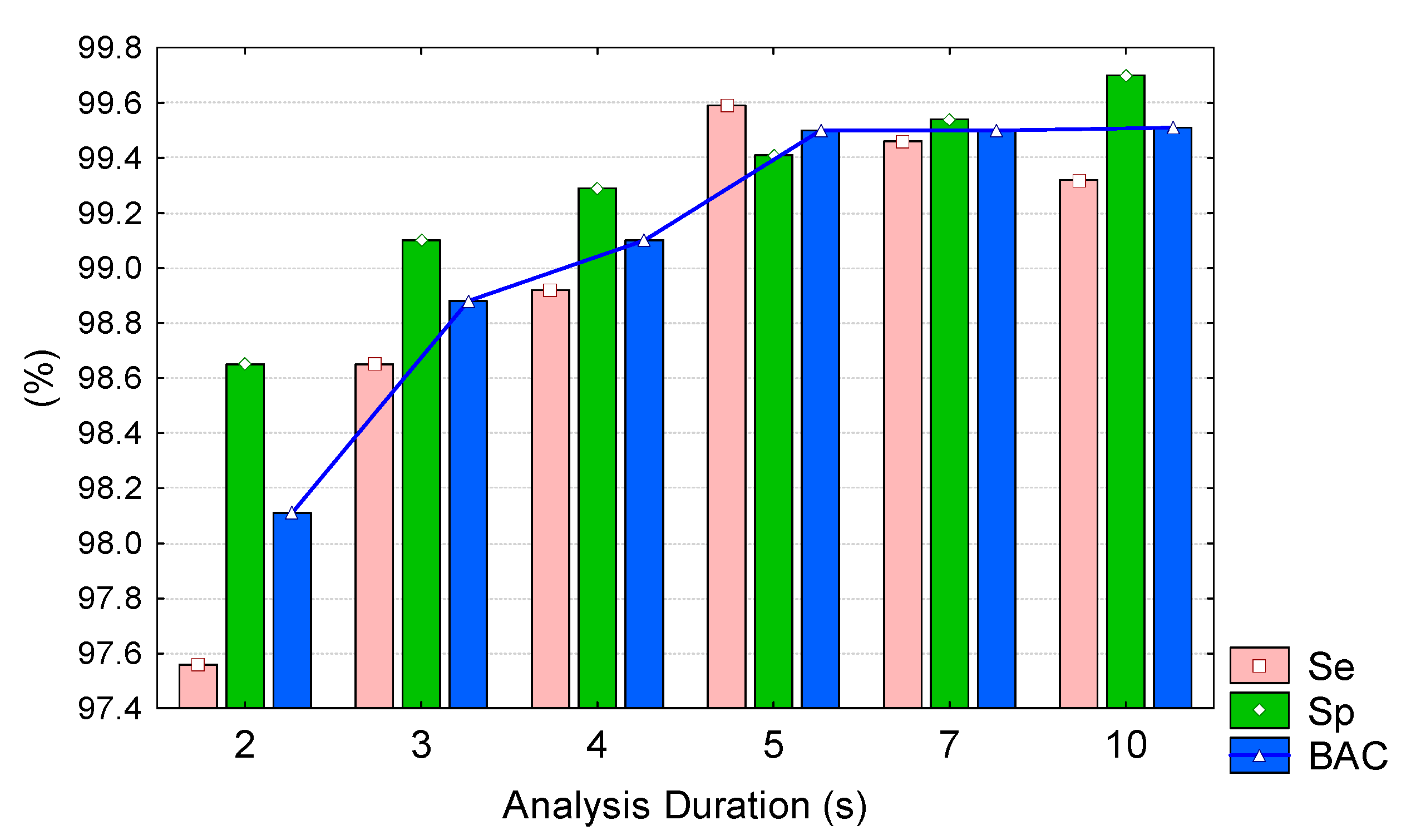
- The application of the model on ECG signals with short and long durations (2–10 s), with maximal performance for 5 s analysis (BAC = 99.5%, Se = 99.6%, Sp = 99.4%, Table 4) and tolerable drop in performance (<2% points) for very short 2 s analysis (BAC = 98.2%, Se = 97.6%, Sp = 98.7%, Table 4) can satisfy the crucial AED requirements for providing shock advisory decision with minimal hands-off delay after end of chest compressions.
5.3. Comparative Study to Other Published CNN Models for ECG Classification
- -
- Our best model outperforms all other models for both Public and OHCA databases. Its configuration can be distinguished as the deepest among others with five convolutional layers, while the number of filters and kernel sizes looks balanced within the middle range found in other studies. This result is a certain proof that HP optimization has an important role in accuracy and should always be carefully performed during DNN design for specific applications;
- -
- The models of Elola et al. [56] and Kiranyaz et al. [44] are the next best models with up to about −1% points and −1.5% points’ drop in BAC, respectively. These models are good examples for successful transfer learning of CNNs in ECG signal processing, where CNN designs optimized for detection of pulseless rhythm and heartbeat classification are here successfully relearned for detection of shockable rhythms. The model of Elola et al. [56] can be distinguished as a deep model (four convolutional layers) with a small number of trainable parameters (1441, owing to the small number of filters and kernels), while the model of Kiranyaz et al. [44] can be distinguished as the shallowest model (two convolutional layers), but with the largest number of trainable parameters (8389 resulting from the largest number of filters and kernel sizes). These models are good examples to show that both deep and shallow networks can almost perform equally if their HPs are optimized in a specific ECG diagnostic application;
- -
- The models of Picon et al. [60], Zubair et al. [48] and Acharya et al. [53] present the largest BAC drop (from −1% points to −5% points). The common HP setting observed in these models is the very small kernel size (three to five), which has been proven in our optimization study to have the most important impact to BAC (see Table 2);
- -
- We note that the additional LSTM layer in the model of Picon et al. [60] provides evidence for inferiority, observing the considerable BAC drop (−2.5% points to −5% points) for short-duration signals < 5 s in Holter databases. This demonstrates that fully convolutional networks are indeed enough powerful to extract features for superior Sh/NSh detection performance at minimal computational cost than other DNN architectures.
- -
- Our best model outperforms a reference shock-advisory system of a commercial AED (Fred Easy, Schiller Médical, France) based on hand-crafted ECG morphology features and a decision tree classifier [7,19,25] by about (+0.5% points to +3% points) for analysis durations of 10 s and 2 s, respectively. Indeed, the AED shock advisory system does not show inferior performance to three DNNs [48,58,60], which is a clear indication that unoptimized deep networks have no benefit compared to traditional machine learning algorithms.
6. Conclusions
7. Limitations
Author Contributions
Funding
Conflicts of Interest
References
- Soar, J.; Nolan, J.; Böttiger, B.; Perkins, G.; Lott, C.; Carli, P.; Pellis, T.; Sandroni, C.; Skrifvars, M.; Smith, G.; et al. Adult advanced life support section Collaborators. Section 3. Adult advanced life support: European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation 2015, 95, 100–147. [Google Scholar] [CrossRef] [PubMed]
- Weisfeldt, M.L.; Sitlani, C.M.; Ornato, J.P.; Rea, T.; Aufderheide, T.P.; Davis, D.; Dreyer, J.; Hess, E.P.; Jui, J.; Maloney, J.; et al. Survival after application of automatic external defibrillators before arrival of the emergency medical system: Evaluation in the resuscitation outcomes consortium population of 21 million. J. Am. Coll. Cardiol. 2010, 55, 1713–1720. [Google Scholar] [CrossRef] [PubMed]
- Israelsson, J.; Wangenheim, B.V.; Årestedt, K.; Semark, B.; Schildmeijer, K.; Carlsson, J. Sensitivity and specificity of two different automated external defibrillators. Resuscitation 2017, 120, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Kerber, R.E.; Becker, L.B.; Bourland, J.D.; Cummins, R.O.; Hallstrom, A.P.; Michos, M.B.; Nichol, G.; Ornato, J.P.; Thies, W.H.; White, R.D.; et al. Automatic External Defibrillators for Public Access Defibrillation: Recommendations for Specifying and Reporting Arrhythmia Analysis Algorithm Performance, Incorporating New Waveforms, and Enhancing Safety. Circulation 1997, 95, 1677–1682. [Google Scholar] [CrossRef] [PubMed]
- Cheskes, S.; Schmicker, R.H.; Verbeek, P.R.; Salcido, D.D.; Brown, S.P.; Brooks, S.; Menegazzi, J.J.; Vaillancourt, C.; Powell, J.; May, S.; et al. Resuscitation Outcomes Consortium (ROC) investigators. The impact of peri-shock pause on survival from out-of-hospital shockable cardiac arrest during the Resuscitation Outcomes Consortium PRIMED trial. Resuscitation 2014, 85, 336–342. [Google Scholar] [CrossRef]
- Deakin, C.D.; Koster, R.W. Chest compression pauses during defibrillation attempts. Curr. Opin. Crit. Care 2016, 22, 206–211. [Google Scholar] [CrossRef]
- Didon, J.P.; Krasteva, V.; Ménétré, S.; Stoyanov, T.; Jekova, I. Shock advisory system with minimal delay triggering after end of chest compressions: Accuracy and gained hands-off time. Resuscitation 2011, 82, S8–S15. [Google Scholar] [CrossRef]
- Ayala, U.; Irusta, U.; Ruiz, J.; Ruiz de Gauna, S.; González-Otero, D.; Alonso, E.; Kramer-Johansen, J.; Naas, H.; Eftestøl, T. Fully automatic rhythm analysis during chest compression pauses. Resuscitation 2015, 89, 25–30. [Google Scholar] [CrossRef]
- Thakor, N.V.; Zhu, Y.S.; Pan, K.Y. Ventricular tachycardia and fibrillation detection by a sequential hypothesis testing algorithm. IEEE Trans. Biomed. Eng. 1990, 37, 837–843. [Google Scholar] [CrossRef]
- Clayton, R.H.; Murray, A.; Campbell, R.W. Comparison of four techniques for recognition of ventricular fibrillation from the surface ECG. Med. Biol. Eng. Comput. 1993, 31, 111–117. [Google Scholar] [CrossRef]
- Jekova, I. Comparison of five algorithms for the detection of ventricular fibrillation from the surface ECG. Physiol. Meas. 2000, 21, 429–439. [Google Scholar] [CrossRef] [PubMed]
- Jekova, I.; Dushanova, J.; Popivanov, D. Method for ventricular fibrillation detection in the external electrocardiogram using nonlinear prediction. Physiol. Meas. 2002, 23, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Jekova, I.; Krasteva, V. Real time detection of ventricular fibrillation and tachycardia. Physiol. Meas. 2004, 25, 1167–1178. [Google Scholar] [CrossRef] [PubMed]
- Amann, A.; Tratnig, R.; Unterkofler, K. Reliability of old and new ventricular fibrillation detection algorithms for automated external defibrillators. Biomed. Eng. Online 2005, 4. [Google Scholar] [CrossRef] [PubMed]
- Krasteva, V.; Jekova, I. Assessment of ECG frequency and morphology parameters for automatic classification of life-threatening cardiac arrhythmias. Physiol. Meas. 2005, 26, 707–723. [Google Scholar] [CrossRef] [PubMed]
- Jekova, I. Shock advisory tool: Detection of life-threatening cardiac arrhythmias and shock success prediction by means of a common parameter set. Biomed. Signal Process. Control 2007, 2, 25–33. [Google Scholar] [CrossRef]
- Amann, A.; Tratnig, R.; Unterkofler, K. Detecting ventricular fibrillation by time-delay methods. IEEE Trans. Biomed. Eng. 2007, 54, 174–177. [Google Scholar] [CrossRef]
- Jekova, I.; Krasteva, V.; Ménétré, S.; Stoyanov, T.; Christov, I.; Fleischhackl, R.; Schmid, J.J.; Didon, J.P. Bench study of the accuracy of a commercial AED arrhythmia analysis algorithm in the presence of electromagnetic interference. Physiol. Meas. 2009, 30, 695–705. [Google Scholar] [CrossRef]
- Krasteva, V.; Jekova, I.; Ménétré, S.; Stoyanov, T.; Didon, J.P. Influence of Analysis Duration on the Accuracy of a Shock Advisory System. Comput. Cardiol. 2011, 38, 537–540. [Google Scholar]
- Arafat, M.; Chowdhury, A.; Hasan, M. A simple time domain algorithm for the detection of ventricular fibrillation in electrocardiogram. Signal Image Video Process. 2011, 5, 1–10. [Google Scholar] [CrossRef]
- Irusta, U.; Ruiz, J.; Aramendi, E.; Ruiz de Gauna, S.; Ayala, U.; Alonso, E. A high-temporal resolution algorithm to discriminate shockable from nonshockable rhythms in adults and children. Resuscitation 2012, 83, 1090–1097. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Rajagopalan, C.; Clifford, G.D. Ventricular Fibrillation and Tachycardia Classification Using a Machine Learning Approach. IEEE Trans. Biomed. Eng. 2014, 61, 1607–1613. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Atienza, F.; Morgado, E.; Fernandez-Martinez, L.; Garcia-Alberola, A.; Rojo-Alvarez, J. Detection of life-threatening arrhythmias using feature selection and support vector machines. IEEE Trans. Biomed. Eng. 2014, 61, 832–840. [Google Scholar] [CrossRef] [PubMed]
- Figuera, C.; Irusta, U.; Morgado, E.; Aramendi, E.; Ayala, U.; Wik, L.; Kramer-Johansen, J.; Eftestøl, T.; Alonso-Atienza, F. Machine Learning Techniques for the Detection of Shockable Rhythms in Automated External Defibrillators. PLoS ONE 2016, 11, e0159654. [Google Scholar] [CrossRef]
- Krasteva, V.; Ménétré, S.; Jekova, I.; Stoyanov, T.; Jost, D.; Frattini, B.; Lemoine, S.; Lemoine, F.; Thomas, V.; Didon, J.P. Comparison of pediatric and adult ECG rhythm analysis by automated external defibrillators during out-of-hospital cardiac arrest. Comput. Cardiol. 2018, 45. [Google Scholar] [CrossRef]
- Plesinger, F.; Andrla, P.; Viscor, I.; Halamek, J.; Jurak, P. Fast Detection of Ventricular Tachycardia and Fibrillation in 1-Lead ECG from Three-Second Blocks. Comput. Cardiol. 2018, 45. [Google Scholar] [CrossRef]
- Manibardo, E.; Irusta, U.; Ser, J.D.; Aramendi, E.; Isasi, I.; Olabarria, M.; Corcuera, C.; Veintemillas, J.; Larrea, A. ECG-based Random Forest Classifier for Cardiac Arrest Rhythms. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 1504–1508. [Google Scholar]
- Fokkenrood, S.; Leijdekkers, P.; Gay, V. Ventricular Tachycardia/Fibrillation Detection Algorithm for 24/7 Personal Wireless Heart Monitoring. Lect. Notes Comput. Sci. 2007, 4541, 110–120. [Google Scholar] [CrossRef]
- Rustwick, B.; Atkins, D. Comparison of electrocardiographic characteristics of adults and children for automated external defibrillator algorithms. Pediatr. Emerg. Care 2014, 30, 851–855. [Google Scholar] [CrossRef]
- Kuo, S.; Dillman, R. Computer detection of ventricular fibrillation. In Proceedings of the Computers in Cardiology; IEEE Computer Society: Long beach, CA, USA, 1978; pp. 347–349. [Google Scholar]
- Barro, S.; Ruiz, R.; Cabello, D.; Mira, J. Algorithmic sequential decision-making in the frequency domain for life threatening ventricular arrhythmias and imitative artefacts: A diagnostic system. J. Biomed. Eng. 1989, 11, 320–328. [Google Scholar] [CrossRef]
- Requena-Carrión, J.; Alonso-Atienza, F.; Everss, E.; Sánchez-Muñoz, J.J.; Ortiz, M.; García-Alberola, A.; Rojo-Álvarez, J.L. Analysis of the robustness of spectral indices during ventricular fibrillation. Biomed. Signal Process. Control 2013, 8, 733–739. [Google Scholar] [CrossRef]
- Mjahad, A.; Rosado-Muñoz, A.; Bataller-Mompeán, M.; Francés-Víllora, J.V.; Guerrero-Martínez, J.F. Ventricular Fibrillation and Tachycardia detection from surface ECG using time-frequency representation images as input dataset for machine learning. Comput. Methods Programs Biomed. 2017, 141, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.S.; Zhu, Y.S.; Thakor, N.V.; Wang, Z.Z. Detecting ventricular tachycardia and fibrillation by complexity measure. IEEE Trans. Biomed. Eng. 1999, 46, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Tripathy, R.K.; Sharma, L.N.; Dandapat, S. Detection of shockable ventricular arrhythmia using variational mode decomposition. J. Med. Syst. 2016, 40, 79. [Google Scholar] [CrossRef]
- Heaton, J. Deep learning and neural networks. In Artificial Intelligence of Humans; Heaton Research Inc.: Chesterfield, UK, 2015; Volume 3. [Google Scholar]
- Géron, A. Hands-On Machine Learning with Scikit-Learn, Keras, TensorFlow: Concepts, Tools, Techniques to Build Intelligent Systems, 2nd ed.; O’Reilly Media Inc.: Sebastopol, CA, USA, 2019; pp. 1–856. [Google Scholar]
- Goodfellow, I.; Bengio, Y.; Courville, A. Deep Learning; MIT press: London, UK, 2016. [Google Scholar]
- Chiang, H.T.; Hsieh, Y.Y.; Fu, S.W.; Hung, K.H.; Tsao, Y.; Chien, S.Y. Noise Reduction in ECG Signals Using Fully Convolutional Denoising Autoencoders. IEEE Access 2019, 7, 60806–60813. [Google Scholar] [CrossRef]
- Zhong, W.; Guo, X.; Wang, G. Non-invasive Fetal Electrocardiography Denoising Using Deep Convolutional Encoder-Decoder Networks. Lect. Notes Electr. Eng. 2020, 592, 1–10. [Google Scholar] [CrossRef]
- Lee, J.S.; Lee, S.J.; Choi, M.; Seo, M.; Kim, S.W. QRS detection method based on fully convolutional networks for capacitive electrocardiogram. Expert Syst. Appl. 2019, 134, 66–78. [Google Scholar] [CrossRef]
- Silva, P.; Luz, E.; Wanner, E.; Menotti, D.; Moreira, G. QRS detection in ECG signal with convolutional network. Lect. Notes Comput. Sci. 2019, 11401, 802–809. [Google Scholar] [CrossRef]
- Sereda, I.; Alekseev, S.; Koneva, A.; Kataev, R.; Osipov, G. ECG segmentation by neural networks: Errors and correction. In Proceedings of the 2019 International Joint Conference on Neural Networks, Budapest, Hungary, 14–19 July 2019. [Google Scholar]
- Kiranyaz, S.; Ince, T.; Gabbouj, M. Real-time patient-specific ECG classification by 1-D convolutional neural networks. IEEE Trans. Biomed. Eng. 2016, 63, 664–675. [Google Scholar] [CrossRef]
- Acharya, U.R.; Oh, S.L.; Hagiwara, Y.; Tan, J.H.; Adam, M.; Gertych, A.; Tan, R.S. A deep convolutional neural network model to classify heartbeats. Comput. Biol. Med. 2017, 89, 389–396. [Google Scholar] [CrossRef]
- Xu, X.; Liu, H. ECG heartbeat classification using convolutional neural networks. IEEE Access 2020, 8, 8614–8619. [Google Scholar] [CrossRef]
- Shaker, A.M.; Tantawi, M.; Shedeed, H.A.; Tolba, M.F. Heartbeat Classification Using 1D Convolutional Neural Networks. Adv. Intell. Syst. Comput. 2020, 1058, 502–511. [Google Scholar] [CrossRef]
- Zubair, M.; Kim, J.; Yoon, C. An automated ECG beat classification system using convolutional neural networks. In Proceedings of the 2016 IEEE Conference on IT Convergence and Security (ICITCS), Prague, Czech Republic, 26 September 2016; pp. 1–5. [Google Scholar]
- Fan, X.; Yao, Q.; Cai, Y.; Miao, F.; Sun, F.; Li, Y. Multiscaled Fusion of Deep Convolutional Neural Networks for Screening Atrial Fibrillation from Single Lead Short ECG Recordings. IEEE J. Biomed. Health Inf. 2018, 22, 1744–1753. [Google Scholar] [CrossRef] [PubMed]
- Rubin, J.; Parvaneh, S.; Rahman, A.; Conroy, B.; Babaeizadeh, S. Densely connected convolutional networks for detection of atrial fibrillation from short single-lead ECG recordings. J. Electrocardiol. 2018, 51, S18–S21. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Sǎrkkǎ, S.; Rad, A.B. Spectro-temporal ECG analysis for atrial fibrillation detection. In Proceedings of the 28th IEEE International Workshop on Machine Learning for Signal Processing (MLSP), Aalborg, Denmark, 17–20 September 2018. [Google Scholar]
- Parvaneh, S.; Rubin, J.; Rahman, A.; Conroy, B.; Babaeizadeh, S. Analyzing single-lead short ECG recordings using dense convolutional neural networks and feature-based post-processing to detect atrial fibrillation. Physiol. Meas. 2018, 39, 084003. [Google Scholar] [CrossRef]
- Acharya, U.R.; Fujita, H.; Oh, S.L.; Hagiwara, Y.; Tan, J.H.; Adam, M. Automated detection of arrhythmias using different intervals of tachycardia ECG segments with convolutional neural network. Inf. Sci. 2017, 405, 81–90. [Google Scholar] [CrossRef]
- Fujita, H.; Cimr, D. Decision support system for arrhythmia prediction using convolutional neural network structure without preprocessing. Appl. Intell. 2019, 49, 3383–3391. [Google Scholar] [CrossRef]
- Hannun, A.Y.; Rajpurkar, P.; Haghpanahi, M.; Tison, G.H.; Bourn, C.; Turakhia, M.P.; Ng, A.Y. Cardiologist-level arrhythmia detection and classification in ambulatory electrocardiograms using a deep neural network. Nat. Med. 2019, 25, 65–69. [Google Scholar] [CrossRef]
- Elola, A.; Aramendi, E.; Irusta, U.; Picón, A.; Alonso, E.; Owens, P.; Idris, A. Deep Neural Networks for ECG-Based Pulse Detection during Out-of-Hospital Cardiac Arrest. Entropy 2019, 21, 305. [Google Scholar] [CrossRef]
- Nguyen, M.T.; Kiseon, K. Feature learning using convolutional neural network for cardiac arrest detection. In Proceedings of the 2018 International Conference on Smart Green Technology in Electrical and Information Systems (ICSGTEIS), Bali, Indonesia, 25–27 October 2018; pp. 39–42. [Google Scholar]
- Acharya, U.R.; Fujita, H.; Oh, S.L.; Raghavendra, U.; Tan, J.H.; Adam, M.; Gertych, A.; Hagiwara, Y. Automated identification of shockable and nonshockable life-threatening ventricular arrhythmias using convolutional neural network. Future Gener. Comput. Syst. 2018, 79, 952–959. [Google Scholar] [CrossRef]
- Irusta, U.; Aramendi, E.; Chicote, B.; Alonso, D.; Corcuera, C.; Veintemillas, J.; Larrea, A.; Olabarria, M. Deep learning approach for a shock advise algorithm using short electrocardiogram analysis intervals. Resuscitation 2019, 142, e28–e114. [Google Scholar] [CrossRef]
- Picon, A.; Irusta, U.; Álvarez-Gila, A.; Aramendi, E.; Alonso-Atienza, F.; Figuera, C.; Ayala, U.; Garrote, E.; Wik, L.; Kramer-Johansen, J.; et al. Mixed convolutional and long short-term memory network for the detection of lethal ventricular arrhythmia. PLoS ONE 2019, 14, e0216756. [Google Scholar] [CrossRef] [PubMed]
- American Heart Association (AHA). 1985 Ventricular Arrhythmia ECG Database; Emergency Care Research Institute: Plymouth Township, PA, USA, 1985. [Google Scholar]
- MIT-BIH Malignant Ventricular Ectopy Database. Available online: https://www.physionet.org/content/vfdb/1.0.0/ (accessed on 18 April 2020).
- Greenwald, S.D. Development and Analysis of a Ventricular Fibrillation Detector. Master’s Thesis, Department of Electrical Engineering and Computer Science, MIT, Cambridge, MA, USA, 1986. [Google Scholar]
- Goldberger, A.L.; Amaral, L.A.N.; Glass, L.; Hausdorff, J.M.; Ivanov, P.C.; Mark, R.G.; Mietus, J.E.; Moody, G.B.; Peng, C.K.; Stanley, H.E. PhysioBank, PhysioToolkit, and PhysioNet: Components of a New Research Resource for Complex Physiologic Signals. Circulation 2003, 101, e215–e220. [Google Scholar] [CrossRef] [PubMed]
- CU Ventricular Tachyarrhythmia Database. Available online: https://physionet.org/content/cudb/1.0.0/ (accessed on 18 April 2020).
- Nolle, F.M.; Badura, F.K.; Catlett, J.M.; Bowser, R.W.; Sketch, M.H. CREI-GARD, a new concept in computerized arrhythmia monitoring systems. Comput. Cardiol. 1986, 13, 515–518. [Google Scholar]
- Breiman, L.; Friedman, J.H.; Olshen, R.A.; Stone, C.J. Classification Regression Trees, 1st ed.; Wadsworth, Inc.: Monterey, CA, USA, 1984; pp. 146–148. [Google Scholar]
- Pham, H.; Guan, M.; Zoph, B.; Le, Q.; Dean, J. Efficient Neural Architecture Search via Parameters Sharing. Proc. Mach. Learn. Res. 2018, 80, 4095–4104. [Google Scholar]
- Liu, H.; Simonyan, K.; Yang, J. DARTS: Differentiable architecture search. In Proceedings of the International Conference on Learning Representations, New Orleans, LA, USA, 23 April 2019; pp. 1–13. [Google Scholar]

| Training Dataset | Validation Dataset | ||||||
|---|---|---|---|---|---|---|---|
| Rhythm | AHADB | CUDB | OHCA1 | Total | VFDB | OHCA2 | Total |
| VF | 430 | 93 | 66 | 589 | 308 | 221 | 529 |
| VT | 20 | 93 | 18 | 131 | 202 | 8 | 210 |
| NSR | 499 | 304 | 42 | 845 | 1023 | 154 | 1177 |
| ONR | 550 | 776 | 334 | 1660 | 1425 | 1063 | 2488 |
| ASYS | 6 | 4 | 655 | 665 | 4 | 2252 | 2256 |
| All Sh | 450 | 186 | 84 | 720 | 510 | 229 | 739 |
| All NSh | 1055 | 1084 | 1031 | 3170 | 2452 | 3469 | 5921 |
| N | F1 | F2 | F3 | F4 | F5 | F6 | F7 | K1 | K2 | K3 | K4 | K5 | K6 | K7 | Param |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 0.15 | 1.00 | 0.56 | ||||||||||||
| 2 | 0.36 | 0.35 | 0.80 | 1.00 | 1.00 | ||||||||||
| 3 | 0.28 | 0.29 | 0.05 | 1.00 | 0.64 | 0.44 | 0.58 | ||||||||
| 4 | 0.32 | 0.20 | 0.21 | 0.16 | 1.00 | 0.62 | 0.39 | 0.33 | 0.56 | ||||||
| 5 | 0.37 | 0.27 | 0.17 | 0.18 | 0.23 | 1.00 | 0.73 | 0.30 | 0.06 | 0.19 | 0.61 | ||||
| 6 | 0.27 | 0.22 | 0.18 | 0.17 | 0.17 | 0.24 | 1.00 | 0.72 | 0.40 | 0.18 | 0.46 | 0.55 | 0.63 | ||
| 7 | 0.18 | 0.68 | 0.75 | 0.68 | 0.41 | 0.18 | 0.09 | 0.73 | 0.27 | 0.23 | 0.00 | 0.00 | 0.00 | 0.00 | 1.00 |
| N | F1 | F2 | F3 | F4 | F5 | F6 | F7 | K1 | K2 | K3 | K4 | K5 | K6 | K7 | Param | LR | Max BAC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 113 | 50 | 5877 | 0.001 | 96.70% | ||||||||||||
| 2 | 10 | 15 | 60 | 25 | 4391 | 0.001 | 98.99% | ||||||||||
| 3 | 5 | 10 | 20 | 10 | 30 | 50 | 11606 | 0.001 | 99.31% | ||||||||
| 4 | 15 | 15 | 15 | 10 | 20 | 25 | 30 | 40 | 18741 | 0.001 | 99.31% | ||||||
| 5 * | 20 | 15 | 15 | 10 | 5 | 10 | 10 | 10 | 10 | 10 | 7521 | 0.001 | 99.50% | ||||
| 6 | 30 | 30 | 15 | 15 | 10 | 5 | 15 | 10 | 10 | 10 | 10 | 10 | 18311 | 0.0005 | 99.38% | ||
| 7 | 40 | 30 | 25 | 15 | 10 | 5 | 5 | 15 | 5 | 5 | 5 | 5 | 5 | 5 | 13486 | 0.0005 | 99.45% |
| Se/Sp (rhythm) | Analysis Duration | |||||
|---|---|---|---|---|---|---|
| 2 s | 3 s | 4 s | 5 s | 7 s | 10 s | |
| Validation dataset: Total | ||||||
| Se (all Sh), % | 97.6 | 98.7 | 98.9 | 99.6 | 99.5 | 99.3 |
| Sp (all NSh), % | 98.7 | 99.1 | 99.3 | 99.4 | 99.5 | 99.7 |
| BAC, % | 98.2 | 98.9 | 99.1 | 99.5 | 99.5 | 99.5 |
| Validation dataset: Holter (VFDB) | ||||||
| Se (all Sh), % | 98.6 | 99.4 | 99.8 | 100 | 99.8 | 100 |
| Sp (all NSh), % | 98.6 | 99.5 | 99.4 | 99.8 | 99.5 | 99.4 |
| BAC, % | 98.6 | 99.5 | 99.6 | 99.9 | 99.7 | 99.7 |
| Validation dataset: OHCA2 | ||||||
| Se (all Sh), % | 95.2 | 96.9 | 96.9 | 98.7 | 98.7 | 97.8 |
| Sp (all NSh), % | 98.7 | 98.8 | 99.2 | 99.2 | 99.6 | 99.1 |
| BAC, % | 97.0 | 97.9 | 98.1 | 99.0 | 99.2 | 99.2 |
| CNN Layers | LSTM Layer | Dense Layers | ||||||
|---|---|---|---|---|---|---|---|---|
| Methods | Original Application | N | Filters | Kernel Size | Max-Pool | Kernel Size | N (Kernel Size) | Trainable Params |
| This study | Sh/NSh detection | 5 | 20, 15, 15, 10, 5 | 10, 10, 10, 10, 10 | 2 | - | 1 (2) | 7521 |
| Picon et al. [60] | Sh/NSh detection | 2 | 32, 32 | 3, 3 | 7 | 20 | 1 (2) | 7493 |
| Acharya et al. [53] | Sh/NSh detection | 4 | 3, 5, 10, 10 | 5, 5, 5, 4 | 2 | - | 3 (10, 5, 2) | 939 |
| Elola et al. [56] 1 | Pulseless rhythm detection | 4 | 8, 8, 8, 8 | 7, 7, 7, 7 | 2 | - | 1 (2) | 1441 |
| Kiranyaz et al. [44] 1,2 | Heartbeat classification | 2 | 32, 16 | 15, 15 | 6 | - | 2 (10, 2) | 8389 |
| Zubair et al. [48] 1,2 | Heartbeat classification | 3 | 32, 16, 8 | 5, 5, 5 | 2 | - | 1 (2) | 3425 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krasteva, V.; Ménétré, S.; Didon, J.-P.; Jekova, I. Fully Convolutional Deep Neural Networks with Optimized Hyperparameters for Detection of Shockable and Non-Shockable Rhythms. Sensors 2020, 20, 2875. https://doi.org/10.3390/s20102875
Krasteva V, Ménétré S, Didon J-P, Jekova I. Fully Convolutional Deep Neural Networks with Optimized Hyperparameters for Detection of Shockable and Non-Shockable Rhythms. Sensors. 2020; 20(10):2875. https://doi.org/10.3390/s20102875
Chicago/Turabian StyleKrasteva, Vessela, Sarah Ménétré, Jean-Philippe Didon, and Irena Jekova. 2020. "Fully Convolutional Deep Neural Networks with Optimized Hyperparameters for Detection of Shockable and Non-Shockable Rhythms" Sensors 20, no. 10: 2875. https://doi.org/10.3390/s20102875
APA StyleKrasteva, V., Ménétré, S., Didon, J.-P., & Jekova, I. (2020). Fully Convolutional Deep Neural Networks with Optimized Hyperparameters for Detection of Shockable and Non-Shockable Rhythms. Sensors, 20(10), 2875. https://doi.org/10.3390/s20102875






