Optimization and Validation of an Adjustable Activity Classification Algorithm for Assessment of Physical Behavior in Elderly
Abstract
1. Introduction
2. Materials and Methods
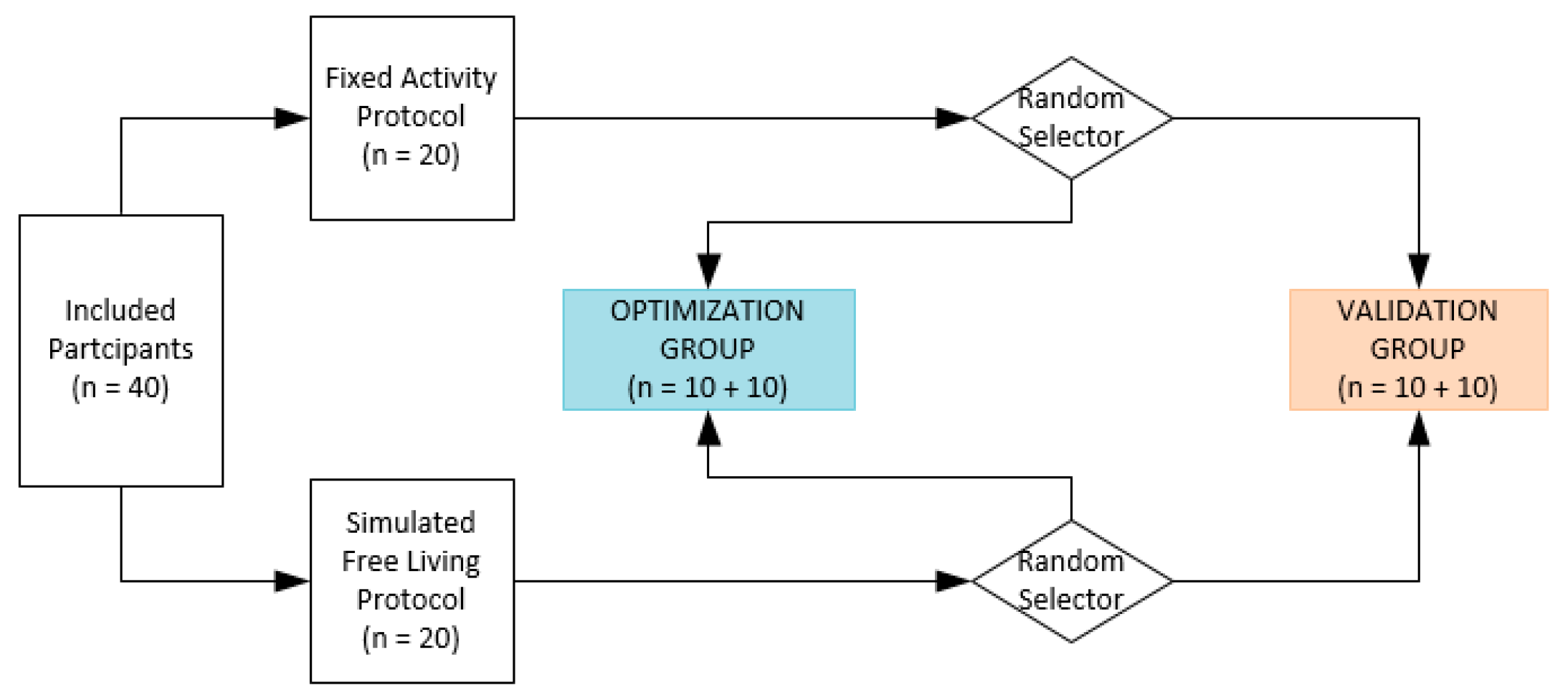
2.1. Study Design
2.2. Participants
2.3. Device Description
2.4. Data Collection
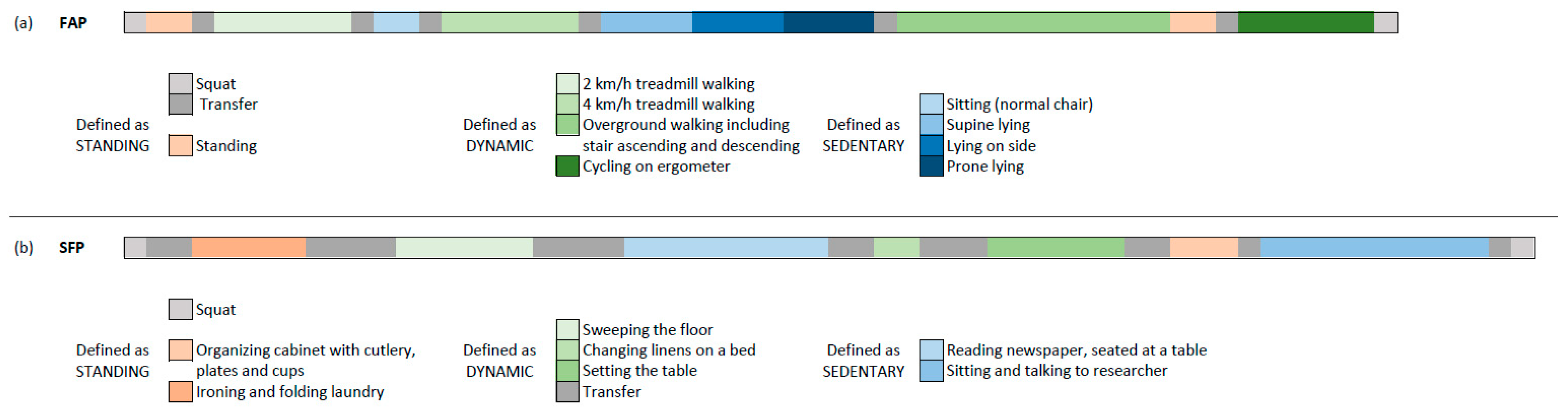
2.5. Activity Protocol
2.6. Algorithm Description
2.7. Data Analysis
2.7.1. Parameter Setting Optimization
2.7.2. Algorithm Validation
3. Results
3.1. Participant Characteristics
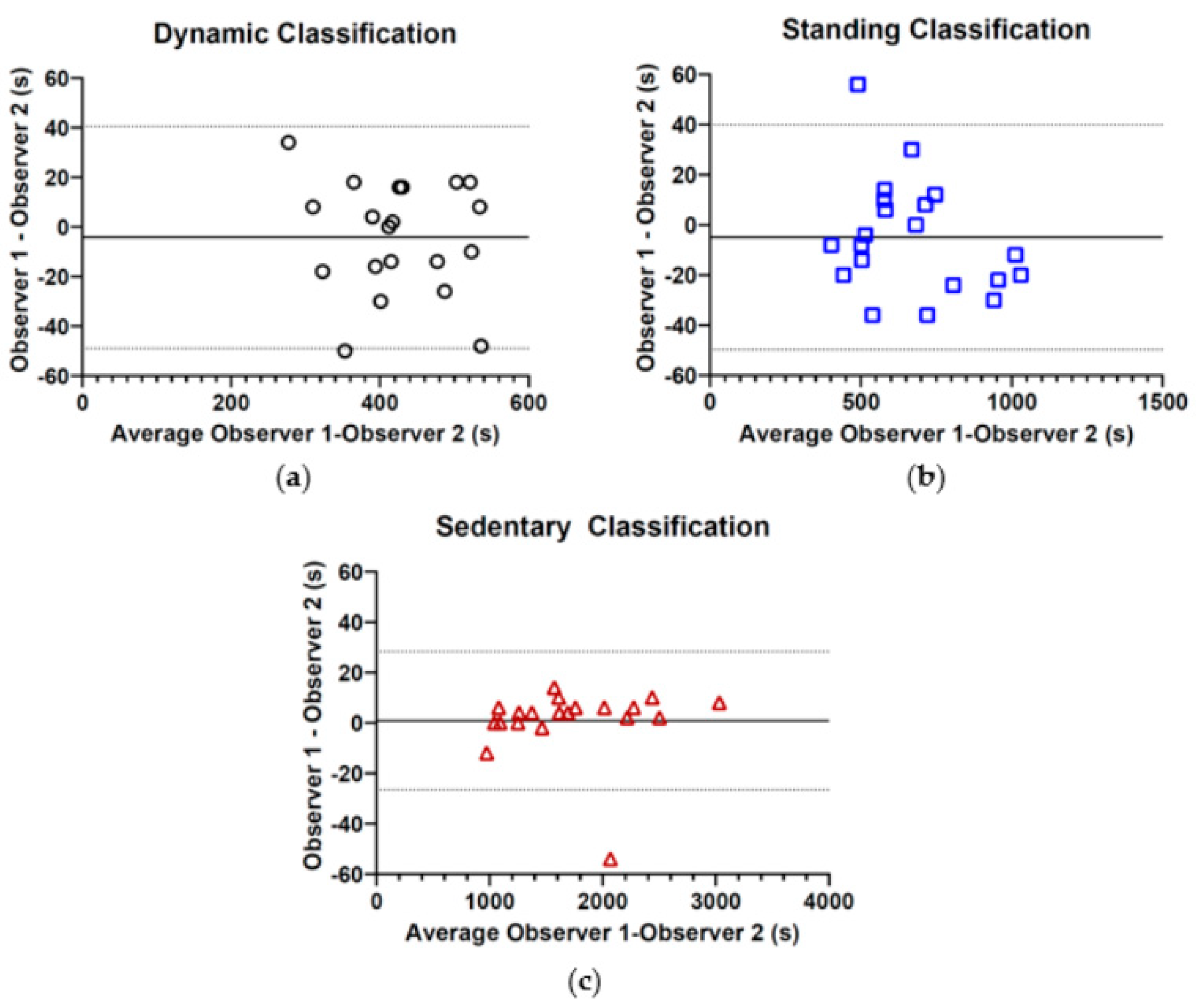
3.2. Inter-Observer Reliability Simulated Free-Living Protocol
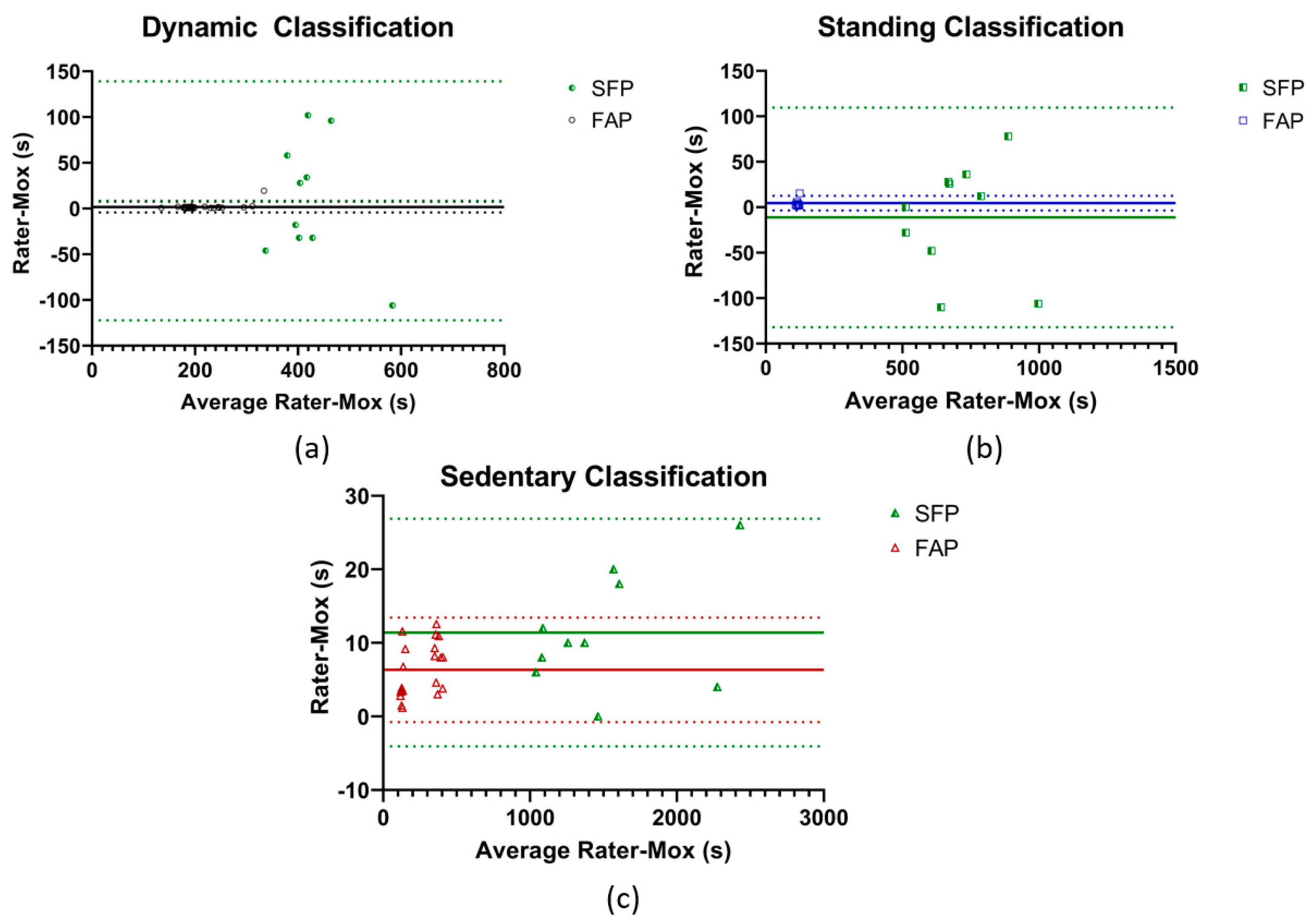
3.3. Parameter Setting Optimization
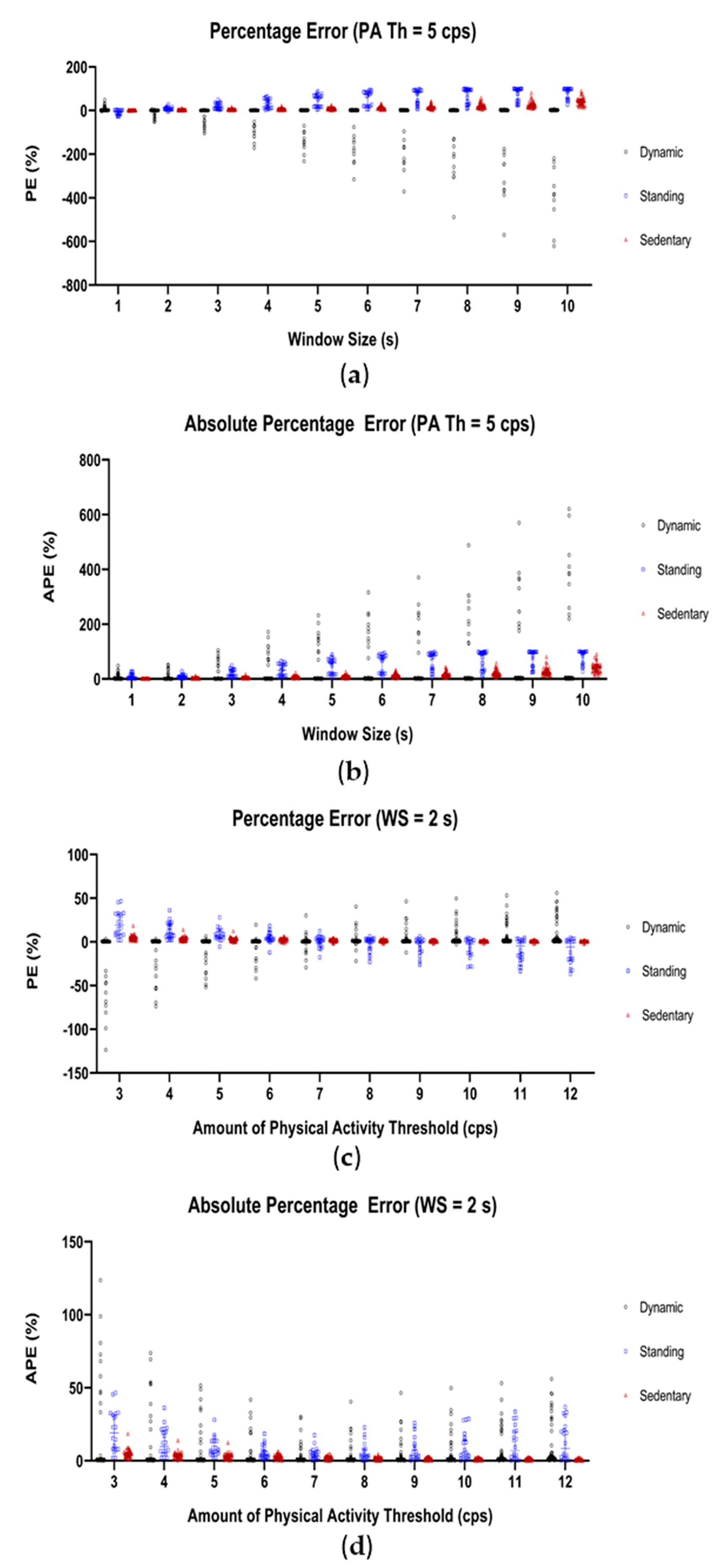
3.3.1. Data Segmentation Window Size
3.3.2. Amount of Physical Activity Threshold
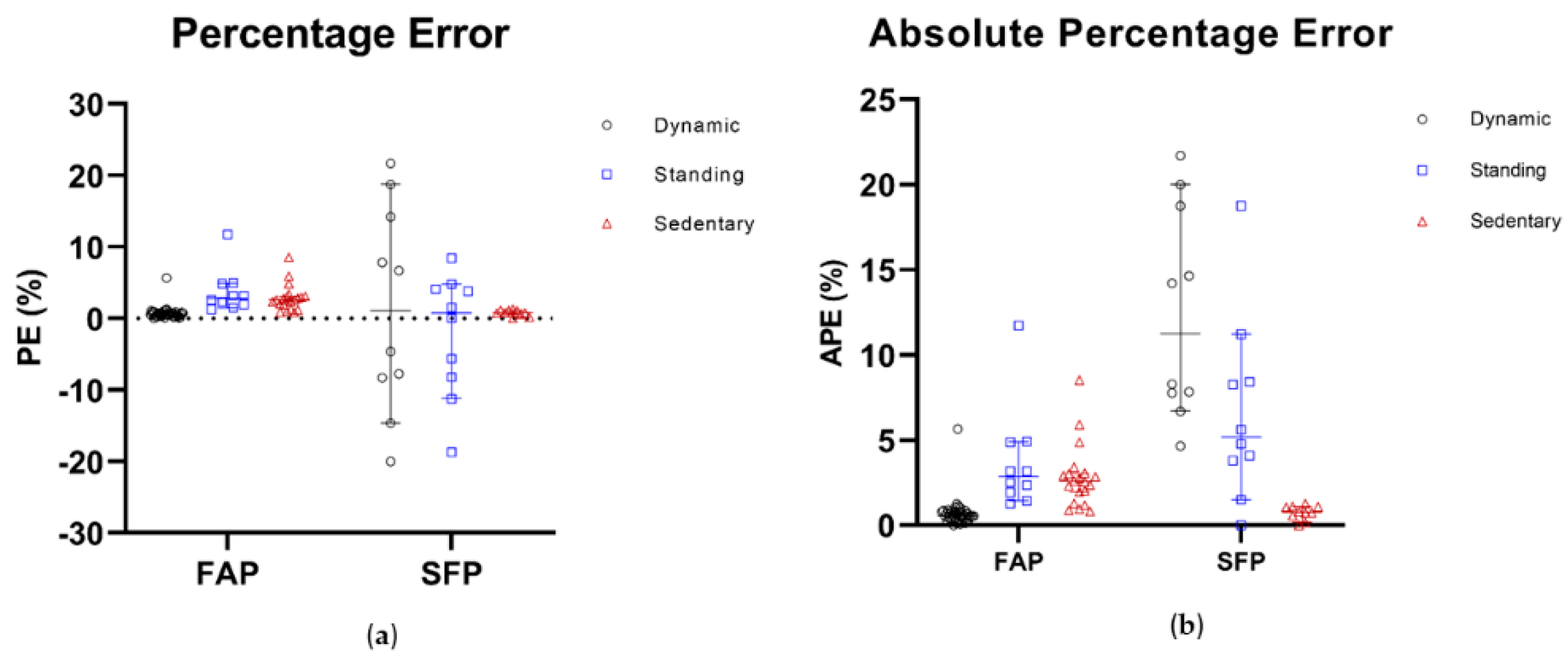
3.4. Algorithm Validation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| WHO | World Health Organization; |
| FAP | fixed activity protocol; |
| SFP | simulated free-living protocol; |
| MOX | MOX Activity Logger; |
| COPD | chronic obstructive pulmonary disease; |
| ADL | activities of daily living; |
| NA | noise acceleration; |
| BA | body acceleration; |
| GA | gravitational acceleration; |
| SMA | signal magnitude area; |
| cps | counts per second; |
| CI | confidence interval; |
| PE | percentage error; |
| APE | absolute percentage error; |
| ICC | intraclass correlation; |
| WS | window size; |
| PA Th | physical activity threshold; |
| SO Th | sensor orientation threshold. |
Appendix A
References
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Hamari, L.; Kullberg, T.; Ruohonen, J.; Heinonen, O.J.; Díaz-Rodríguez, N.; Lilius, J.; Pakarinen, A.; Myllymäki, A.; Leppänen, V.; Salanterä, S.; et al. Physical activity among children: Objective measurements using Fitbit One((R)) and ActiGraph. BMC Res. Notes 2017, 10, 161. [Google Scholar] [CrossRef]
- Van Roekel, E.H.; Winkler, E.A.; Bours, M.J.; Lynch, B.M.; Willems, P.J.; Meijer, K.; Kant, I.; Beets, G.L.; Sanduleanu, S.; Healy, G.N.; et al. Associations of sedentary time and patterns of sedentary time accumulation with health-related quality of life in colorectal cancer survivors. Prev. Med. Rep. 2016, 4, 262–269. [Google Scholar] [CrossRef]
- Verlaan, L.; Bolink, S.A.A.N.; Van Laarhoven, S.N.; Lipperts, M.; Heyligers, I.C.; Grimm, B.; Senden, R. Accelerometer-based Physical Activity Monitoring in Patients with Knee Osteoarthritis: Objective and Ambulatory Assessment of Actual Physical Activity During Daily Life Circumstances. Open Biomed. Eng. J. 2015, 9, 157. [Google Scholar] [CrossRef]
- Karel, J.M.; Senden, R.; Janssen, J.E.; Savelberg, H.H.; Grimm, B.; Heyligers, I.C.; Peeters, R.; Meijer, K. Towards unobtrusive in vivo monitoring of patients prone to falling. In Proceedings of the Annual International Conference of the IEEE on Engineering in Medicine and Biology Society (EMBC), Buenos Aires, Argentina, 31 August–4 September 2010; pp. 5018–5021. [Google Scholar]
- Koene, S.; Dirks, I.; Van Mierlo, E.; De Vries, P.R.; Janssen, A.J.; Smeitink, J.A.; Bergsma, A.; Essers, H.; Meijer, K.; De Groot, I.J.; et al. Domains of Daily Physical Activity in Children with Mitochondrial Disease: A 3D Accelerometry Approach. JIMD Rep. 2017, 36, 7–17. [Google Scholar]
- Meijer, K.; Annegarn, J.; Passos, V.L.; Savelberg, H.H.; Schols, A.M.; Wouters, E.F.; Spruit, M.A. Characteristics of daily arm activities in patients with COPD. Eur. Respir. J. 2014, 43, 1631–1641. [Google Scholar] [CrossRef]
- Verwey, R.; van der Weegen, S.; Spreeuwenberg, M.; Tange, H.; van der Weijden, T.; de Witte, L. A monitoring and feedback tool embedded in a counselling protocol to increase physical activity of patients with COPD or type 2 diabetes in primary care: Study protocol of a three-arm cluster randomised controlled trial. BMC Fam. Pract. 2014, 15, 93. [Google Scholar] [CrossRef]
- Welk, G.J.; Bai, Y.; Lee, J.M.; Godino, J.; Saint-Maurice, P.F.; Carr, L. Standardizing Analytic Methods and Reporting in Activity Monitor Validation Studies. Med. Sci. Sports Exerc. 2019, 51, 1767–1780. [Google Scholar] [CrossRef]
- Bunn, J.A.; Navalta, J.W.; Fountaine, C.J.; Reece, J.D. Current State of Commercial Wearable Technology in Physical Activity Monitoring 2015–2017. Int. J. Exerc. Sci. 2018, 11, 503–515. [Google Scholar]
- Lindemann, U.; Zijlstra, W.; Aminian, K.; Chastin, S.; de Bruin, E.; Helbostad, J.; Bussmann, J. Recommendations for standardizing validation procedures assessing physical activity of older persons by monitoring body postures and movements. Sensors 2014, 14, 1267–1277. [Google Scholar] [CrossRef]
- Gorman, E.; Hanson, H.M.; Yang, P.H.; Khan, K.M.; Liu-Ambrose, T.; Ashe, M.C. Accelerometry analysis of physical activity and sedentary behavior in older adults: A systematic review and data analysis. Eur. Rev. Aging Phys. Act. 2014, 11, 35–49. [Google Scholar] [CrossRef]
- Hernando, C.; Collado, E.J.; Panizo, N.; Martinez-Navarro, I.; Hernando, B. Establishing cut-points for physical activity classification using triaxial accelerometer in middle-aged recreational marathoners. PLoS ONE 2018, 13, e0202815. [Google Scholar] [CrossRef]
- Howe, C.A.; Clevenger, K.; Leslie, R.; Ragan, M. Comparison of Accelerometer-Based Cut-Points for Children’s Physical Activity: Counts vs. Steps. Children 2018, 5, 105. [Google Scholar] [CrossRef]
- Prince, S.A.; Reed, J.L.; Mark, A.E.; Blanchard, C.; Grace, S.; Reid, R. An examination of accelerometer cut-points for quantifying physical activity in cardiac populations. Can. J. Cardiol. 2014, 30, S308. [Google Scholar] [CrossRef]
- Banos, O.; Galvez, J.M.; Damas, M.; Pomares, H.; Rojas, I. Window size impact in human activity recognition. Sensors 2014, 14, 6474–6499. [Google Scholar] [CrossRef]
- Bersch, S.; Azzi, D.; Khusainov, R.; Achumba, I.; Ries, J. Sensor data acquisition and processing parameters for human activity classification. Sensors 2014, 14, 4239–4270. [Google Scholar] [CrossRef]
- Bouten, C.V.C.; Westerterp, K.R.; Verduin, M.; Jansse, J.G. A triaxial accelerometer for the assessment of daily physical activity in relation to energy expenditure. In Proceedings of the 15th Annual International Conference of the IEEE Engineering in Medicine and Biology Societ, San Diego, CA, USA, 28–31 October 1993. [Google Scholar]
- Lipperts, M.; van Laarhoven, S.; Senden, R.; Heyligers, I.; Grimm, B. Clinical validation of a body-fixed 3D accelerometer and algorithm for activity monitoring in orthopaedic patients. J. Orthop. Transl. 2017, 11, 19–29. [Google Scholar] [CrossRef]
- Mathie, M.J.; Coster, A.C.F.; Lovell, N.H.; Celler, B.G. Detection of daily physical activities using a triaxial accelerometer. Med. Biol. Eng. Comput. 2003, 41, 296–301. [Google Scholar] [CrossRef]
- Preece, S.J.; Goulermas, J.Y.; Kenney, L.P.; Howard, D.; Meijer, K.; Crompton, R. Activity identification using body-mounted sensors—A review of classification techniques. Physiol. Meas. 2009, 30, R1. [Google Scholar] [CrossRef]
- Annegarn, J.; Spruit, M.A.; Uszko-Lencer, N.H.; Vanbelle, S.; Savelberg, H.H.; Schols, A.M.; Wouters, E.F.; Meijer, K. Objective physical activity assessment in patients with chronic organ failure: A validation study of a new single-unit activity monitor. Arch. Phys. Med. Rehabil. 2011, 92, 1852–1857. [Google Scholar] [CrossRef]
- National Institute for Public Health and the Environment. Beweeggedrag Bij Personen Van 4 Jaar en Ouder in 2018. Available online: https://www.rivm.nl/leefstijlmonitor/bewegen (accessed on 10 May 2018).
- Senden, R.; Savelberg, H.H.C.M.; Grimm, B.; Heyligers, I.C.; Meijer, K. Accelerometry-based gait analysis, an additional objective approach to screen subjects at risk for falling. Gait Posture 2012, 36, 296–300. [Google Scholar] [CrossRef]
- Berendsen, B.A.; Hendriks, M.R.; Meijer, K.; Plasqui, G.; Schaper, N.C.; Savelberg, H.H. Which activity monitor to use? Validity, reproducibility and user friendliness of three activity monitors. BMC Public Health 2014, 14, 749. [Google Scholar] [CrossRef]
- Maastricht Instruments. MOX1. Available online: www.accelerometry.eu (accessed on 1 September 2019).
- Mesquita, R.; Meijer, K.; Pitta, F.; Azcuna, H.; Goërtz, Y.M.; Essers, J.M.; Wouters, E.F.; Spruit, M.A. Changes in physical activity and sedentary behaviour following pulmonary rehabilitation in patients with COPD. Respir. Med. 2017, 126, 122–129. [Google Scholar] [CrossRef]
- Peters, D.M.; Fritz, S.L.; Krotish, D.E. Assessing the reliability and validity of a shorter walk test compared with the 10-Meter Walk Test for measurements of gait speed in healthy, older adults. J. Geriatr. Phys. Ther. 2013, 36, 24–30. [Google Scholar] [CrossRef]
- Godfrey, A.; Conway, R.; Meagher, D.; ÓLaighin, G. Direct measurement of human movement by accelerometry. Med. Eng. Phys. 2008, 30, 1364–1386. [Google Scholar] [CrossRef]
- Dartfish Ltd. Dartfish EasyTag-Note. Available online: https://play.google.com/store/apps/details?id=com.dartfish.android.tag&hl=nl (accessed on 21 December 2017).
- Sasaki, J.E.; Hickey, A.; Staudenmayer, J.; John, D.; Kent, J.A.; Freedson, P.S. Performance of Activity Classification Algorithms in Free-Living Older Adults. Med. Sci. Sports. Exerc. 2016, 48, 941. [Google Scholar] [CrossRef]
- Fida, B.; Bernabucci, I.; Bibbo, D.; Conforto, S.; Schmid, M. Varying behavior of different window sizes on the classification of static and dynamic physical activities from a single accelerometer. Med. Eng. Phys. 2015, 37, 705–711. [Google Scholar] [CrossRef]
- Herssens, N.; Verbecque, E.; Hallemans, A.; Vereeck, L.; Van Rompaey, V.; Saeys, W. Do spatiotemporal parameters and gait variability differ across the lifespan of healthy adults? A systematic review. Gait Posture 2018, 64, 181–190. [Google Scholar] [CrossRef]
- Allahbakhshi, H.; Hinrichs, T.; Huang, H.; Weibel, R. The Key Factors in Physical Activity Type Detection Using Real-Life Data: A Systematic Review. Front. Physiol. 2019, 10, 75. [Google Scholar] [CrossRef]
- Farrahi, V.; Niemelä, M.; Kangas, M.; Korpelainen, R.; Jämsä, T. Calibration and validation of accelerometer-based activity monitors: A systematic review of machine-learning approaches. Gait Posture 2019, 68, 285–299. [Google Scholar] [CrossRef]
- Liu, L.; Wang, S.; Hu, B.; Qiong, Q.; Wen, J.; Rosenblum, D.S. Learning Structures of Interval-Based Bayesian networks in Probabilistic Generative Model for Human Complex Activity Recognition. Pattern Recognit. 2018, 81, 545–561. [Google Scholar] [CrossRef]
- Hildebrandt, V.H.; Bernaards, C.; Hofstetter, H. Trendrapport Bewegen en Gezondheid 2000/2014. 2014. Available online: http://publications.tno.nl/publication/34618420/2tVTmk/hilberhof-2015-trendrapport.pdf (accessed on 14 November 2019).
- Bourke, A.; Ihlen, E.; Helbostad, J. Development of a gold-standard method for the identification of sedentary, light and moderate physical activities in older adults: Definitions for video annotation. J. Sci. Med. Sport 2018, 22, 557–561. [Google Scholar] [CrossRef]
- Bourke, A.K.; Ihlen, E.A.; Van de Ven, P.; Nelson, J.; Helbostad, J.L. Video analysis validation of a real-time physical activity detection algorithm based on a single waist mounted tri-axial accelerometer sensor. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016. [Google Scholar]
- Burton, E.; Hill, K.D.; Lautenschlager, N.T.; Thøgersen-Ntoumani, C.; Lewin, G.; Boyle, E.; Howie, E. Reliability and validity of two fitness tracker devices in the laboratory and home environment for older community-dwelling people. BMC Geriatr. 2018, 18, 103. [Google Scholar] [CrossRef]
- Ferguson, T.; Rowlands, A.V.; Olds, T.; Maher, C. The validity of consumer-level, activity monitors in healthy adults worn in free-living conditions: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 42. [Google Scholar] [CrossRef]

| Fixed Activity Protocol | ||
| Optimization Group (n = 10) | Validation Group (n = 10) | |
| Gender (male) | 5 (50%) | 3 (30%) |
| Age (years) | 69 (67–77) | 68 (66–73) |
| Body weight (kg) | 81.0 (63.0–90.0) | 69.4 (59–86.5) |
| Body length (cm) | 170 (159–175) | 160 (157–169) |
| Average Walking Speed (m/s) | 1.22 (0.88–1.60) | 1.37 (1.06–1.48) |
| Simulated Free-Living Protocol | ||
| Optimization Group (n = 10) | Validation Group (n = 10) | |
| Gender (male) | 6 (60%) | 4 (40%) |
| Age (years) | 73 (70–77) | 75 (69–88) |
| Body weight (kg) | 88.1 (75.1–114.0) | 70.0 (48.8–101.6) |
| Body length (cm) | 174 (165–184) | 169 (158–182) |
| Average Walking Speed (m/s) | 1.16 (0.79–1.29) | 1.15 (0.85–1.38) |
| Optimal Window Size | Optimal Amount of Physical Activity Threshold | ||||||
| Percentage Error (%) | Percentage Error (%) | ||||||
| WS (s) | Dynamic | Standing | Sedentary | PA Th (cps) | Dynamic | Standing | Sedentary |
|---|---|---|---|---|---|---|---|
| 1 | 1.5 (0.7–2.5) | −3 (−15.1–1.7) | 1.3 (0.7–1.4) | 6 | 0.7 (0.4–0.9) | 3.5 (2.0–6.5) | 2.4 (1.8–3.4) |
| 2 | 0.6 (0.4–0.7) | 6.8 (4.4–13.4) | 2.9 (1.8–4.2) | 7 | 0.7 (0.6–0.9) | 1.9 (−2.3–4.0) | 2.0 (0.5–2.5) |
| 3 | 0.7 (0.4–0.9) | 16.9 (8.2–31.8) | 4.6 (2.9–5.8) | 8 | 0.9 (0.6–1.0) | 1.2 (−7.7–2.7) | 1.4 (0.4–1.8) |
| Absolute Percentage Error (%) | Absolute Percentage Error (%) | ||||||
| WS (s) | Dynamic | Standing | Sedentary | PA Th (cps) | Dynamic | Standing | Sedentary |
| 1 | 1.6 (0.9–2.6) | 4.7 (1.9–15.1) | 1.4 (0.8–1.6) | 6 | 0.9 (0.7–1.0) | 4.0 (2.4–7.2) | 2.4 (1.8–3.4) |
| 2 | 0.9 (0.6–1.0) | 6.8 (5.1–13.4) | 2.9 (1.8–4.2) | 7 | 0.9 (0.7–1.0) | 3.9 (2.2–6.2) | 2.0 (1.4–2.5) |
| 3 | 1.0 (0.7–1.3) | 16.9 (8.2–31.8) | 4.6 (2.9–5.8) | 8 | 0.9 (0.7–1.0) | 3.6 (2.0–7.7) | 1.7 (0.6–2.0) |
| Optimized Algorithm Settings (WS = 2 s, PA Th = 7 cps, SO Th = 0.8 g) | ||||||
| Dynamic | Standing | Sedentary | ||||
| FAP | SFP | FAP | SFP | FAP | SFP | |
| PE (%) | 0.6 (0.4–0.8) | 1.0 (−14.6–18.6) | 2.9 (1.5–4.9) | 0.8 (−11.2–4.8) | 2.6 (2.0–3.0) | 0.8 (0.2–1.1) |
| APE (%) | 0.6 (0.4–0.8) | 11.3 (6.7–20.0) | 2.9 (1.5–4.9) | 5.2 (1.5–11.2) | 2.6 (2.0–3.1) | 0.8 (0.2–1.1) |
| Algorithm Settings Used by Annegarn et al. (WS = 1 s, PA Th = 5 cps, SO Th = 0.8 g) | ||||||
| Dynamic | Standing | Sedentary | ||||
| FAP | SFP | FAP | SFP | FAP | SFP | |
| PE (%) | 1.1 (0.6–2.9) | 27.9 (11.6–40.0) | 1.6 (1.5–2.4) | −12.6 (− 27.2–7.9) | 1.7 (1.2–2.0) | 0.3 (−0.1–1.0) |
| APE (%) | 1.1 (0.6–2.9) | 27.9 (11.7–40.0) | 1.6 (1.5–2.4) | 12.6 (7.9–27.2) | 1.7 (1.2–2.0) | 0.4 (0.1–1.0) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bijnens, W.; Aarts, J.; Stevens, A.; Ummels, D.; Meijer, K. Optimization and Validation of an Adjustable Activity Classification Algorithm for Assessment of Physical Behavior in Elderly. Sensors 2019, 19, 5344. https://doi.org/10.3390/s19245344
Bijnens W, Aarts J, Stevens A, Ummels D, Meijer K. Optimization and Validation of an Adjustable Activity Classification Algorithm for Assessment of Physical Behavior in Elderly. Sensors. 2019; 19(24):5344. https://doi.org/10.3390/s19245344
Chicago/Turabian StyleBijnens, Wouter, Jos Aarts, An Stevens, Darcy Ummels, and Kenneth Meijer. 2019. "Optimization and Validation of an Adjustable Activity Classification Algorithm for Assessment of Physical Behavior in Elderly" Sensors 19, no. 24: 5344. https://doi.org/10.3390/s19245344
APA StyleBijnens, W., Aarts, J., Stevens, A., Ummels, D., & Meijer, K. (2019). Optimization and Validation of an Adjustable Activity Classification Algorithm for Assessment of Physical Behavior in Elderly. Sensors, 19(24), 5344. https://doi.org/10.3390/s19245344





