Augmenting Clinical Outcome Measures of Gait and Balance with a Single Inertial Sensor in Age-Ranged Healthy Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Protocol and Data Collection
- The 10-m walk test (10MWT) of gait speed, with three trials each at a self-selected velocity (SSV) and fast velocity (FV). Increasing gait speed has been correlated with a higher quality of life [1] and community mobility [13]. The traditional clinical outcome of the 10MWT is average walking speed in the SSV and FV conditions. Participants walked over an instrumented walkway (GAITRite; CIR Systems, Inc., Franklin, NJ, USA) during this test, which was used as the gold standard for validating spatiotemporal gait characteristics computed from sensor data.
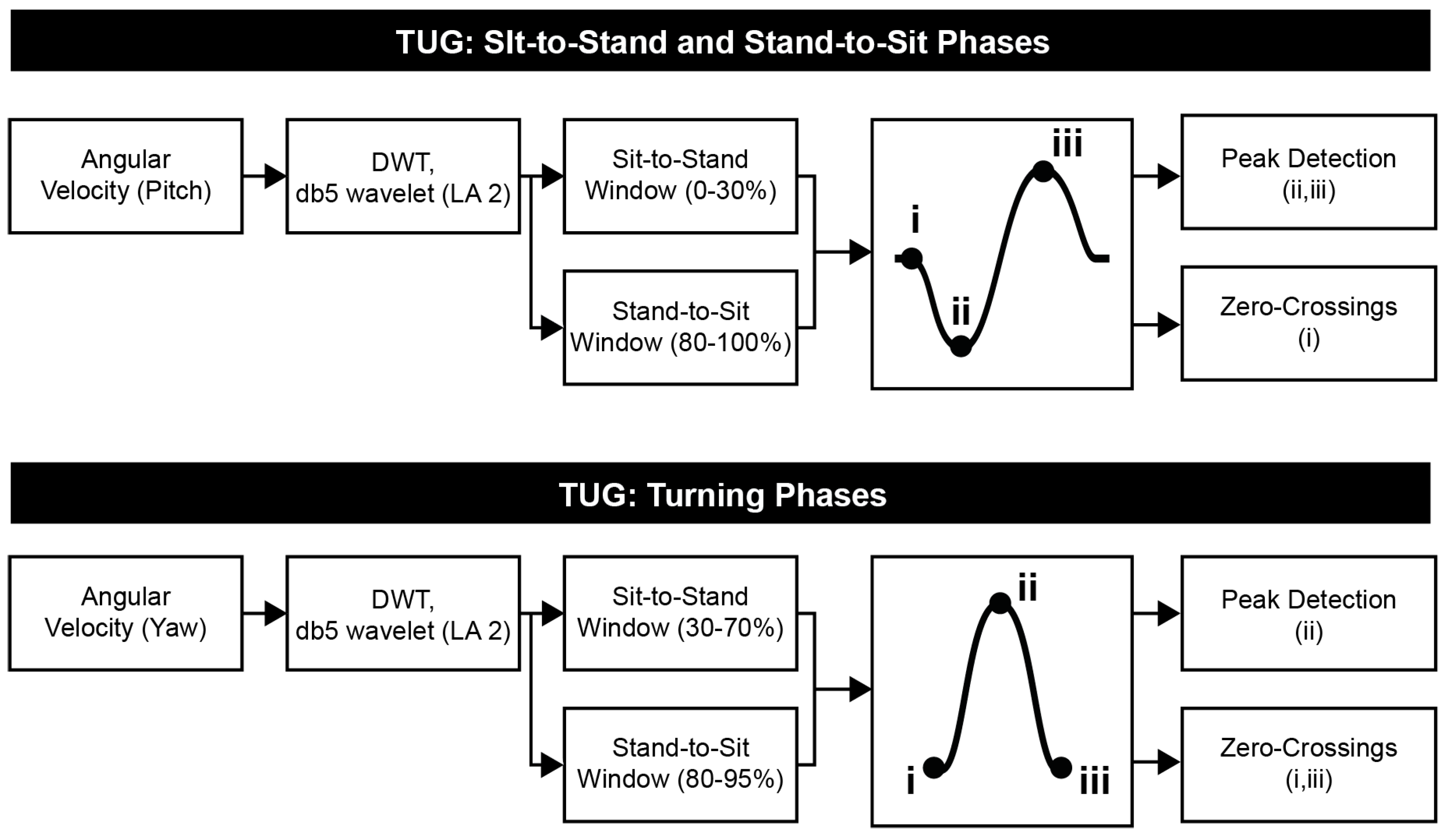
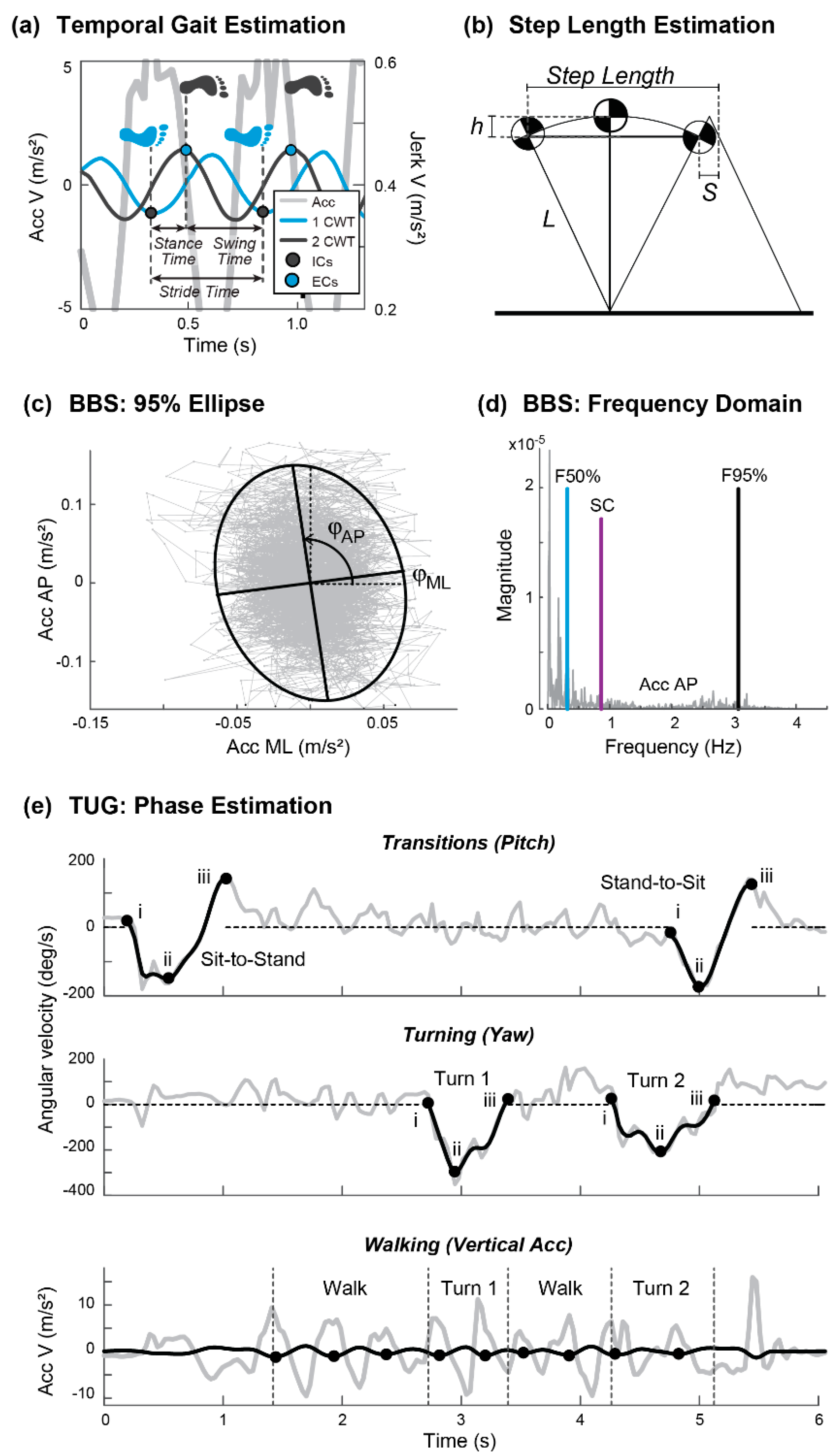
- Static postural stability condition of the Berg Balance Scale (BBS), including standing unsupported with feet apart (SU), standing with eyes closed (SEC), standing with feet together (SFT), (d) standing in tandem stance (ST) with their nondominant (or paretic) leg behind, and standing on one leg (SOL) on their nondominant (or paretic) leg. This test assesses functional balance and is associated with risk of falling [2]. A trained clinician scores each item on a 5-point ordinal scale, ranging from 0 (lowest function) to 4 (highest function). The traditional clinical outcome of the BBS is the total score.
- Timed Up and Go (TUG) test of functional mobility, with two trials collected. This test assesses functional mobility and is used to predict the risk of falls [14]. Participants began seated in a chair, rose to a standing position without use of their hands (Sit-to-Stand), walked 3 m (Walk), turned 180 degrees (Turn 1), walked 3 m back to the chair (Walk), turned 180° (Turn 2), and sat down in the chair without use of their hands (Stand-to-Sit). The traditional clinical outcome of the TUG is the total time required to complete the test.
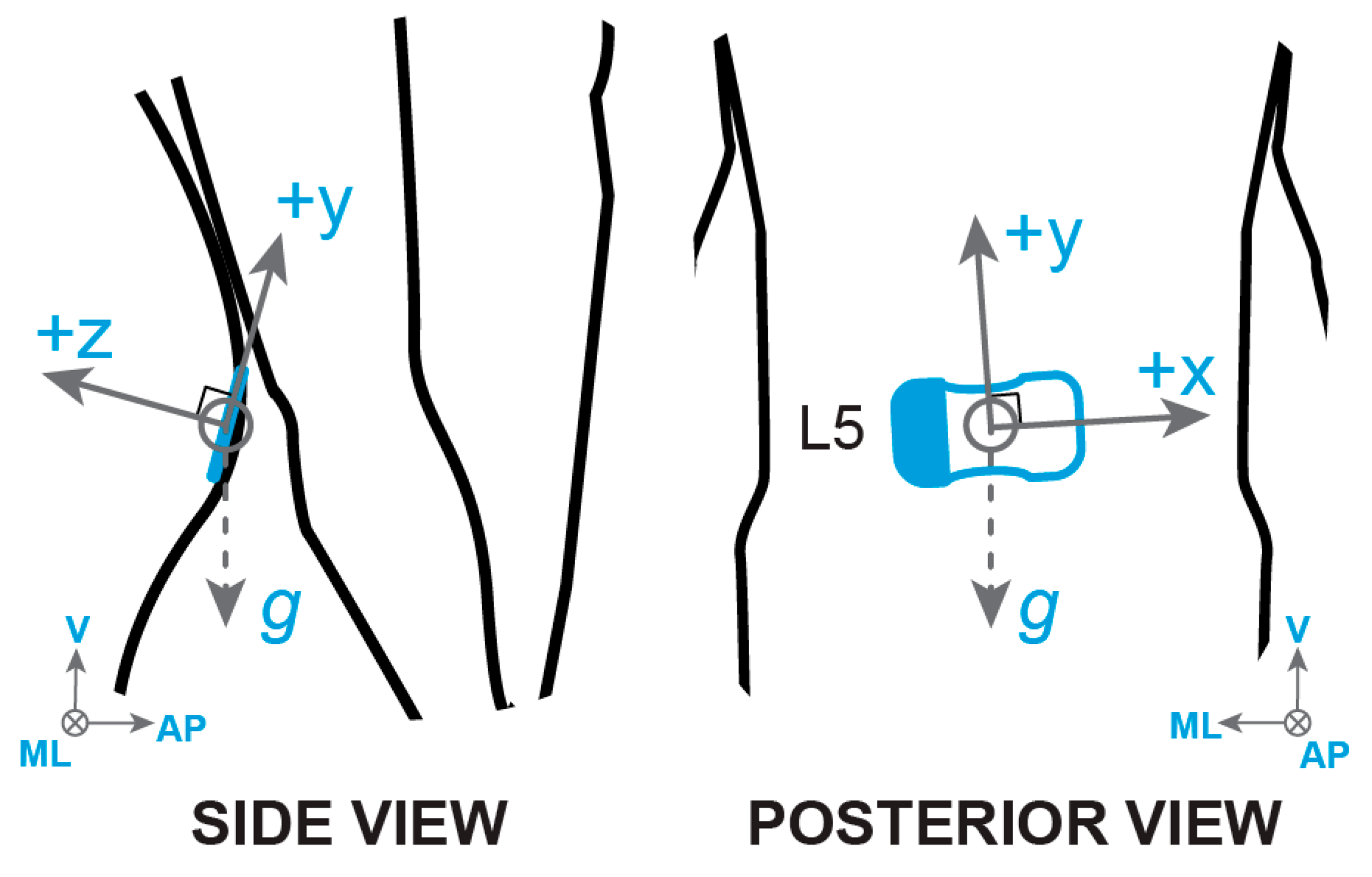
2.3. Sensor Technology
2.4. Data Exclusions
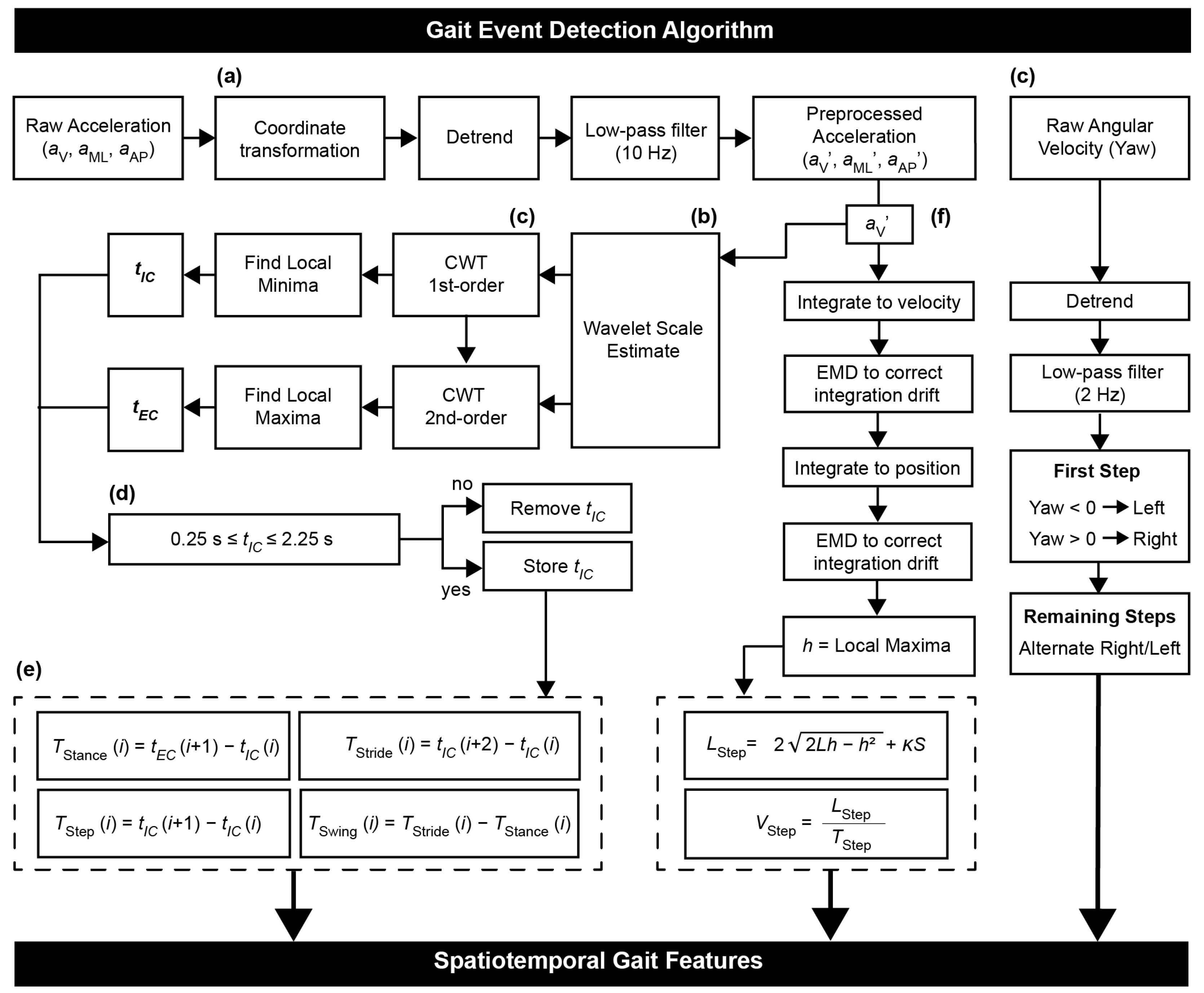
2.5. Data Analysis
2.5.1. Clinical Meta-Feature Extraction
2.5.2. Features Summary
2.6. Statistical Analysis
3. Results
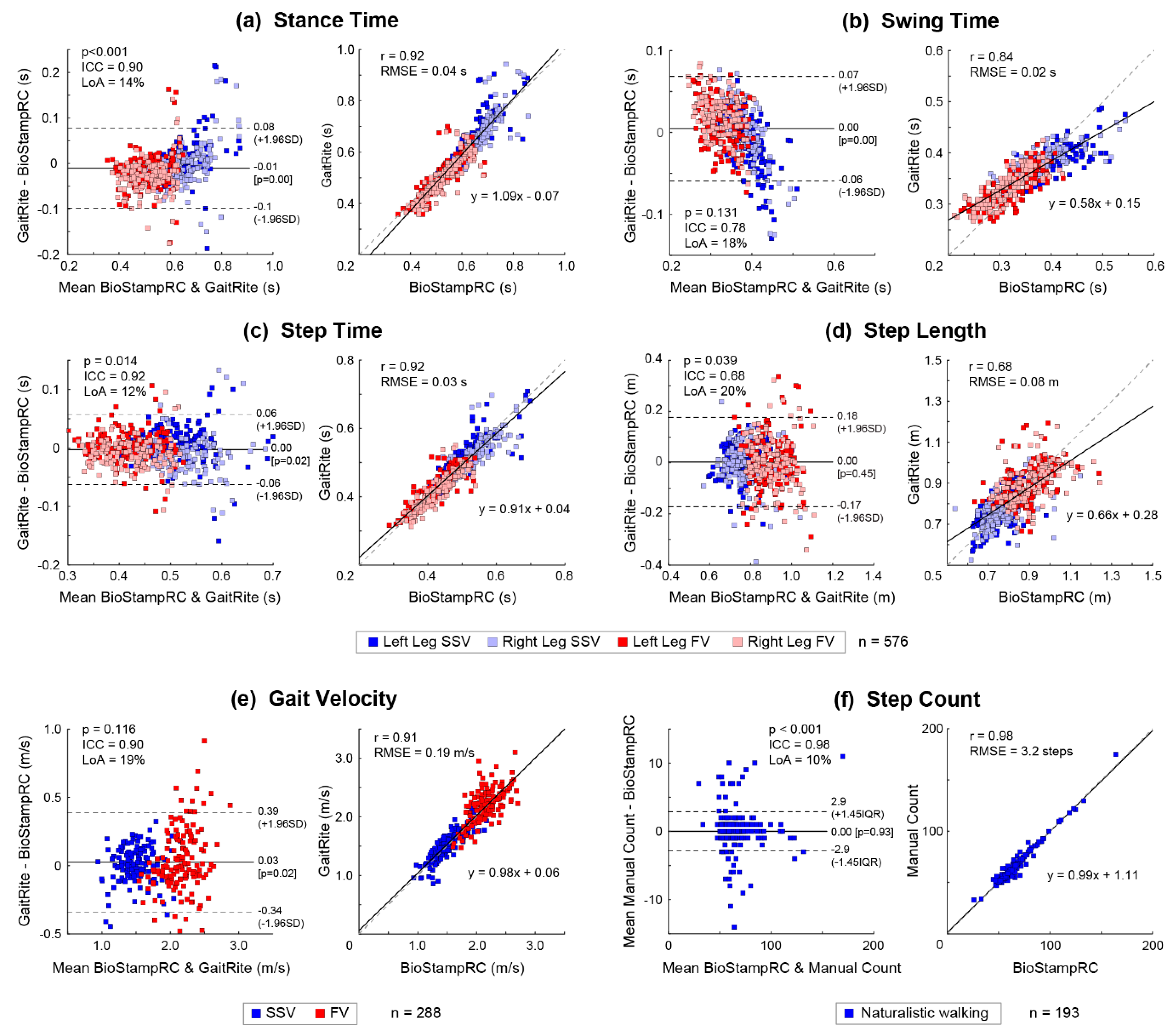
3.1. Validation of Spatiotemporal Gait Features
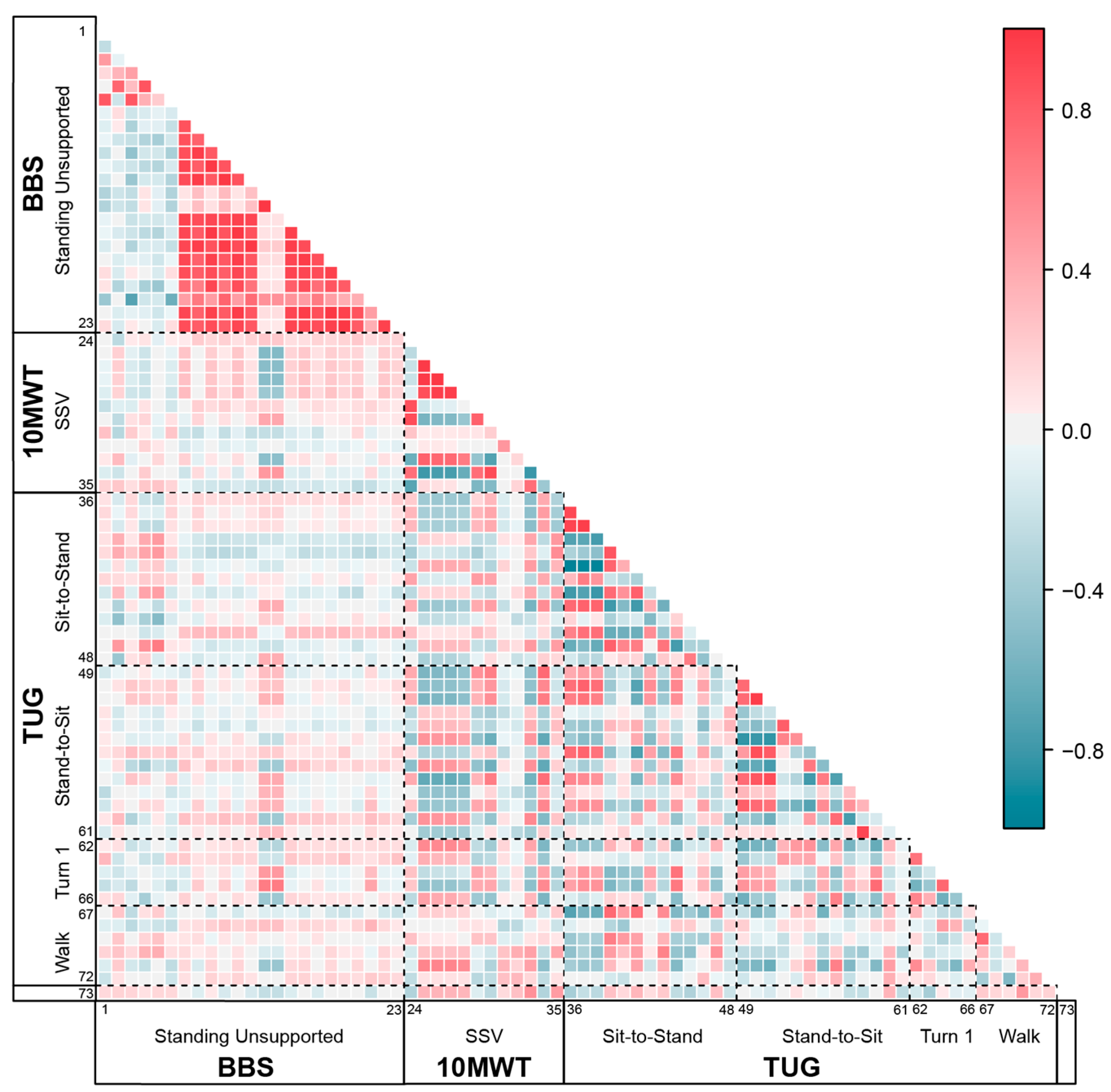
3.2. Feature Independence between Clinical Tests
3.3. Correlation between Age and Sensor-Derived Features
3.4. Hierarchical Multivariate Regression for Age Effects in Sensor-Derived Features
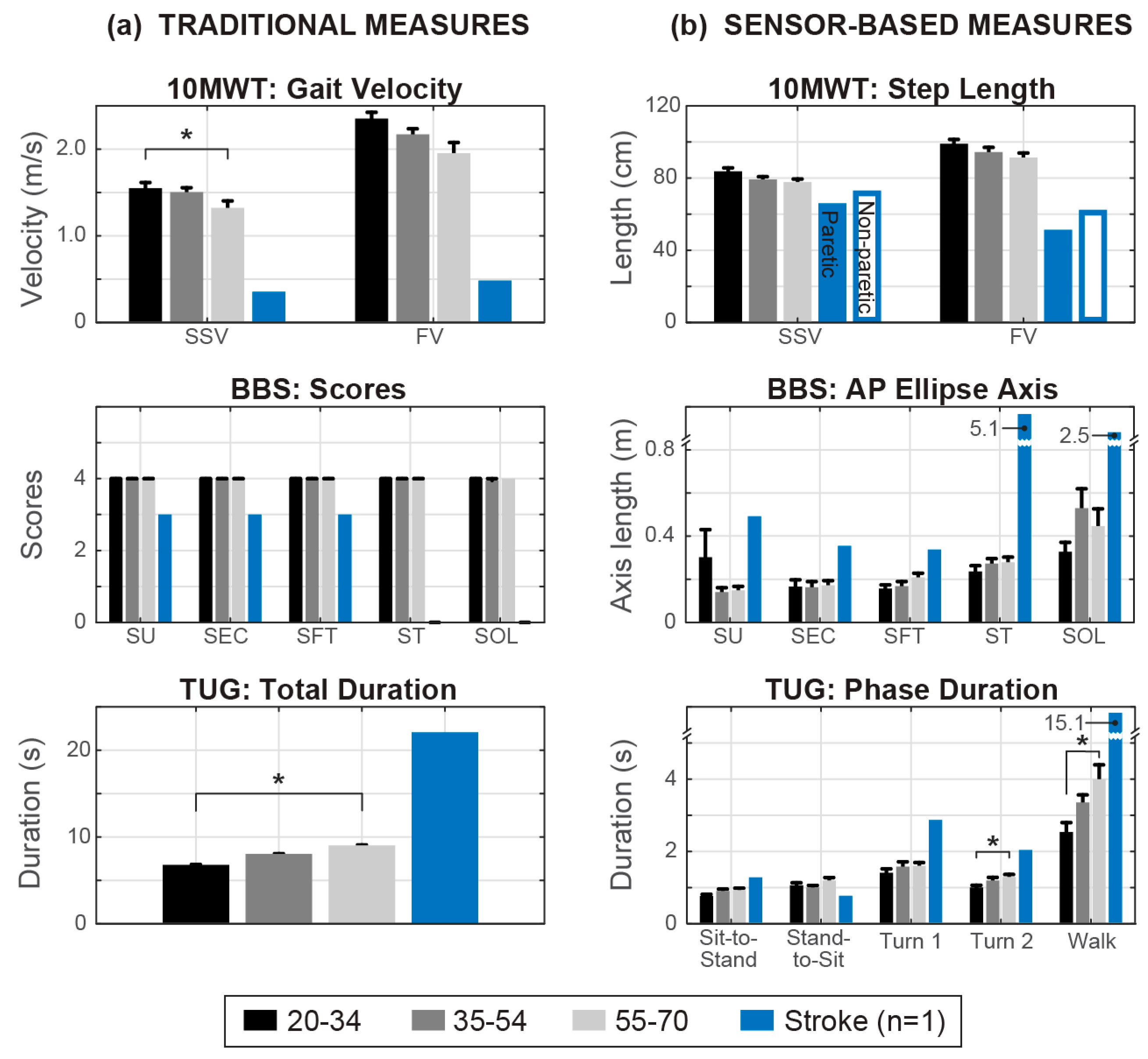
3.5. Differences between Age Groups and Stroke Rehabilitation Participant
4. Discussion
4.1. BBS Static Balance Performance
4.2. 10MWT Performance
4.3. TUG Performance
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Feature 1 | Normality | Correlation with Age | Controlled for Weight and Height | ||
|---|---|---|---|---|---|
| p | r | p | r * | p * | |
| F50% AP | 0.001 | −0.036 | 0.805 | −0.110 | 0.463 |
| F50% ML | <0.001 | −0.146 | 0.316 | 0.001 | 0.994 |
| F95% AP | 0.062 | −0.077 | 0.598 | −0.058 | 0.697 |
| F95% ML | 0.009 | −0.426 ** | 0.002 | −0.384 ** | 0.008 |
| SC AP | 0.266 | −0.134 | 0.359 | −0.120 | 0.421 |
| SC ML | 0.188 | −0.266 | 0.064 | −0.253 | 0.086 |
| Max Acc AP | <0.001 | −0.005 | 0.974 | 0.066 | 0.659 |
| Max Acc ML | <0.001 | 0.063 | 0.667 | 0.177 | 0.235 |
| Mean Acc AP | <0.001 | 0.123 | 0.399 | 0.088 | 0.558 |
| Mean Acc ML | <0.001 | 0.179 | 0.218 | 0.135 | 0.365 |
| RMS AP | <0.001 | 0.125 | 0.391 | 0.063 | 0.672 |
| RMS ML | <0.001 | 0.184 | 0.205 | 0.166 | 0.265 |
| Ellipse Angle AP | <0.001 | 0.103 | 0.483 | −0.187 | 0.209 |
| Ellipse Angle ML | <0.001 | 0.198 | 0.173 | 0.248 | 0.092 |
| 95% Ellipse Area | <0.001 | 0.141 | 0.333 | 0.038 | 0.798 |
| Ellipse Axis AP | <0.001 | 0.124 | 0.394 | 0.071 | 0.634 |
| Ellipse Axis ML | <0.001 | 0.110 | 0.454 | 0.095 | 0.526 |
| Jerk AP | <0.001 | −0.012 | 0.933 | −0.011 | 0.943 |
| Jerk ML | <0.001 | −0.105 | 0.473 | −0.120 | 0.423 |
| SwayV AP | <0.001 | 0.129 | 0.375 | 0.082 | 0.583 |
| SwayV ML | <0.001 | 0.171 | 0.240 | 0.182 | 0.222 |
| SPathA AP | <0.001 | −0.015 | 0.916 | −0.007 | 0.963 |
| SPathA ML | <0.001 | −0.099 | 0.496 | −0.117 | 0.435 |
| Feature 1 | Normality | Correlation with Age | Controlled for Weight and Height | ||
|---|---|---|---|---|---|
| p | r | p | r * | p * | |
| F50% AP | 0.010 | 0.023 | 0.899 | −0.076 | 0.678 |
| F50% ML | <0.001 | −0.233 | 0.185 | −0.308 | 0.087 |
| F95% AP | <0.001 | −0.214 | 0.255 | −0.217 | 0.234 |
| F95% ML | 0.008 | −0.145 | 0.412 | −0.168 | 0.358 |
| SC AP | <0.001 | −0.115 | 0.516 | −0.147 | 0.422 |
| SC ML | 0.305 | −0.378 ** | 0.007 | −0.369 * | 0.011 |
| Max Acc AP | <0.001 | 0.196 | 0.266 | 0.151 | 0.410 |
| Max Acc ML | <0.001 | 0.072 | 0.687 | 0.039 | 0.833 |
| Mean Acc AP | <0.001 | 0.107 | 0.548 | 0.174 | 0.341 |
| Mean Acc ML | <0.001 | 0.151 | 0.395 | 0.079 | 0.669 |
| RMS AP | <0.001 | 0.109 | 0.540 | 0.159 | 0.385 |
| RMS ML | <0.001 | 0.084 | 0.637 | 0.070 | 0.702 |
| Ellipse Angle AP | <0.001 | −0.061 | 0.733 | 0.080 | 0.665 |
| Ellipse Angle ML | <0.001 | −0.134 | 0.452 | −0.215 | 0.237 |
| 95% Ellipse Area | <0.001 | 0.049 | 0.782 | 0.092 | 0.617 |
| Ellipse Axis AP | <0.001 | 0.110 | 0.536 | 0.143 | 0.435 |
| Ellipse Axis ML | <0.001 | −0.004 | 0.981 | 0.042 | 0.819 |
| Jerk AP | <0.001 | 0.068 | 0.703 | 0.042 | 0.818 |
| Jerk ML | <0.001 | −0.125 | 0.481 | −0.089 | 0.628 |
| SwayV AP | <0.001 | 0.182 | 0.303 | 0.175 | 0.338 |
| SwayV ML | <0.001 | 0.180 | 0.308 | 0.105 | 0.569 |
| SPathA AP | <0.001 | −0.006 | 0.973 | −0.031 | 0.868 |
| SPathA ML | <0.001 | −0.209 | 0.236 | −0.128 | 0.486 |
| Feature 1 | Normality | Correlation with Age | Controlled for Weight and Height | ||
|---|---|---|---|---|---|
| p | r | p | r * | p * | |
| F50% AP | <0.001 | −0.070 | 0.635 | −0.133 | 0.374 |
| F50% ML | 0.101 | −0.101 | 0.489 | −0.097 | 0.517 |
| F95% AP | 0.001 | −0.116 | 0.426 | −0.188 | 0.207 |
| F95% ML | 0.162 | −0.312 * | 0.029 | −0.305 * | 0.037 |
| SC AP | 0.040 | −0.067 | 0.647 | −0.153 | 0.304 |
| SC ML | 0.121 | −0.269 | 0.062 | −0.261 | 0.076 |
| Max Acc AP | <0.001 | 0.188 | 0.195 | 0.110 | 0.463 |
| Max Acc ML | 0.004 | 0.134 | 0.360 | 0.106 | 0.477 |
| Mean Acc AP | 0.003 | 0.101 | 0.492 | 0.163 | 0.273 |
| Mean Acc ML | 0.001 | 0.154 | 0.292 | 0.187 | 0.209 |
| RMS AP | 0.006 | 0.119 | 0.415 | 0.166 | 0.266 |
| RMS ML | 0.009 | 0.145 | 0.319 | 0.186 | 0.211 |
| Ellipse Angle AP | <0.001 | −0.023 | 0.876 | −0.193 | 0.195 |
| Ellipse Angle ML | <0.001 | 0.140 | 0.339 | 0.099 | 0.508 |
| 95% Ellipse Area | <0.001 | 0.164 | 0.259 | 0.149 | 0.318 |
| Ellipse Axis AP | 0.035 | 0.164 | 0.260 | 0.192 | 0.197 |
| Ellipse Axis ML | <0.001 | 0.102 | 0.485 | 0.102 | 0.497 |
| Jerk AP | 0.025 | −0.055 | 0.708 | −0.108 | 0.469 |
| Jerk ML | 0.113 | −0.170 | 0.244 | −0.167 | 0.263 |
| SwayV AP | <0.001 | 0.056 | 0.704 | 0.144 | 0.333 |
| SwayV ML | <0.001 | 0.085 | 0.562 | 0.056 | 0.710 |
| SPathA AP | 0.029 | −0.064 | 0.660 | −0.110 | 0.461 |
| SPathA ML | 0.119 | −0.169 | 0.244 | −0.167 | 0.263 |
| Feature 1 | Normality | Correlation with Age | Controlled for Weight and Height | ||
|---|---|---|---|---|---|
| p | r | p | r * | p * | |
| F50% AP | <0.001 | −0.131 | 0.369 | −0.301 * | 0.040 |
| F50% ML | 0.033 | −0.045 | 0.760 | −0.076 | 0.610 |
| F95% AP | <0.001 | −0.017 | 0.907 | 0.038 | 0.800 |
| F95% ML | 0.055 | −0.050 | 0.733 | −0.055 | 0.712 |
| SC AP | 0.032 | −0.087 | 0.550 | −0.152 | 0.308 |
| SC ML | 0.133 | −0.076 | 0.605 | −0.077 | 0.608 |
| Max Acc AP | <0.001 | 0.096 | 0.510 | −0.107 | 0.475 |
| Max Acc ML | <0.001 | 0.031 | 0.834 | −0.132 | 0.378 |
| Mean Acc AP | <0.001 | 0.238 | 0.099 | 0.089 | 0.550 |
| Mean Acc ML | <0.001 | 0.222 | 0.125 | 0.157 | 0.291 |
| RMS AP | <0.001 | 0.163 | 0.264 | 0.024 | 0.870 |
| RMS ML | <0.001 | 0.166 | 0.254 | 0.041 | 0.785 |
| Ellipse Angle AP | <0.001 | −0.070 | 0.634 | −0.064 | 0.668 |
| Ellipse Angle ML | 0.040 | 0.070 | 0.631 | 0.049 | 0.746 |
| 95% Ellipse Area | <0.001 | 0.179 | 0.219 | −0.042 | 0.779 |
| Ellipse Axis AP | <0.001 | 0.113 | 0.441 | −0.021 | 0.890 |
| Ellipse Axis ML | <0.001 | 0.231 | 0.110 | 0.068 | 0.651 |
| Jerk AP | 0.137 | 0.172 | 0.238 | 0.189 | 0.203 |
| Jerk ML | 0.176 | 0.114 | 0.434 | 0.126 | 0.399 |
| SwayV AP | <0.001 | 0.105 | 0.475 | −0.016 | 0.917 |
| SwayV ML | <0.001 | −0.032 | 0.825 | −0.071 | 0.635 |
| SPathA AP | 0.197 | 0.160 | 0.273 | 0.177 | 0.233 |
| SPathA ML | 0.323 | 0.106 | 0.471 | 0.118 | 0.430 |
| Feature 1 | Normality | Correlation with Age | Controlled for Weight and Height | ||
|---|---|---|---|---|---|
| p | r | p | r * | p * | |
| F50% AP | <0.001 | −0.015 | 0.98 | 0.084 | 0.577 |
| F50% ML | 0.106 | −0.169 | 0.274 | −0.155 | 0.299 |
| F95% AP | 0.100 | 0.014 | 0.922 | 0.029 | 0.848 |
| F95% ML | <0.001 | −0.103 | 0.479 | −0.143 | 0.337 |
| SC AP | 0.042 | 0.037 | 0.800 | 0.052 | 0.726 |
| SC ML | 0.500 | −0.175 | 0.228 | −0.171 | 0.250 |
| Max Acc AP | <0.001 | 0.185 | 0.202 | 0.139 | 0.353 |
| Max Acc ML | <0.001 | 0.432 ** | 0.002 | 0.348 * | 0.017 |
| Mean Acc AP | <0.001 | 0.226 | 0.118 | 0.173 | 0.245 |
| Mean Acc ML | <0.001 | 0.361 * | 0.011 | 0.377 ** | 0.009 |
| RMS AP | <0.001 | 0.226 | 0.118 | 0.166 | 0.264 |
| RMS ML | <0.001 | 0.356 * | 0.012 | 0.379 ** | 0.009 |
| Ellipse Angle AP | <0.001 | 0.184 | 0.206 | 0.177 | 0.235 |
| Ellipse Angle ML | 0.018 | −0.049 | 0.753 | −0.029 | 0.848 |
| 95% Ellipse Area | <0.001 | 0.292 * | 0.042 | 0.191 | 0.199 |
| Ellipse Axis AP | <0.001 | 0.354 * | 0.013 | 0.316 * | 0.031 |
| Ellipse Axis ML | <0.001 | 0.190 | 0.192 | 0.140 | 0.347 |
| Jerk AP | <0.001 | 0.234 | 0.105 | 0.152 | 0.306 |
| Jerk ML | <0.001 | 0.273 | 0.058 | 0.241 | 0.103 |
| SwayV AP | <0.001 | 0.182 | 0.210 | 0.205 | 0.167 |
| SwayV ML | <0.001 | 0.283 * | 0.049 | 0.324 * | 0.026 |
| SPathA AP | <0.001 | 0.257 | 0.074 | 0.178 | 0.232 |
| SPathA ML | <0.001 | 0.268 | 0.063 | 0.239 | 0.106 |
| Feature 1 | Normality | Correlation with Age | Controlled for Weight and Height | ||
|---|---|---|---|---|---|
| p | r | p | r * | p * | |
| Mean Vertical Displacement | <0.001 | −0.201 | 0.167 | −0.177 | 0.234 |
| Mean Stance Time | 0.163 | 0.219 | 0.133 | 0.313 * | 0.032 |
| Mean Step Time | 0.075 | 0.183 | 0.209 | 0.267 | 0.069 |
| Mean Stride Time | 0.073 | 0.179 | 0.219 | 0.541 | 0.264 |
| Mean Swing Time | 0.040 | 0.082 | 0.575 | 0.183 | 0.219 |
| Mean Step Length | 0.079 | −0.341 * | 0.017 | −0.367 * | 0.011 |
| Maximum Power Frequency | <0.001 | −0.221 | 0.127 | −0.216 | 0.144 |
| Stance Time Symmetry Ratio | 0.826 | −0.057 | 0.697 | −0.049 | 0.742 |
| Step Length Symmetry Ratio | <0.001 | −0.152 | 0.296 | −0.167 | 0.263 |
| Duration | <0.001 | 0.235 | 0.104 | 0.309 * | 0.034 |
| Mean Velocity | 0.116 | −0.658 ** | 0.008 | −0.387 ** | 0.007 |
| N Steps | 0.126 | 0.280 | 0.051 | 0.260 | 0.077 |
| Velocity Difference, FV – SSV | <0.001 | −0.013 | 0.931 | −0.004 | 0.979 |
| Feature 1 | Normality | Correlation with Age | Controlled for Weight and Height | ||
|---|---|---|---|---|---|
| p | r | p | r * | p * | |
| Mean Vertical Displacement | 0.383 | −0.251 | 0.086 | −0.272 | 0.067 |
| Mean Stance Time | 0.502 | 0.020 | 0.895 | 0.059 | 0.699 |
| Mean Step Time | 0.240 | 0.014 | 0.924 | 0.049 | 0.747 |
| Mean Stride Time | 0.248 | 0.012 | 0.936 | 0.048 | 0.753 |
| Mean Swing Time | 0.056 | 0.010 | 0.948 | 0.038 | 0.800 |
| Mean Step Length | 0.105 | −0.315 * | 0.029 | −0.370 * | 0.011 |
| Maximum Power Frequency | 0.003 | −0.355 * | 0.013 | −0.363 * | 0.013 |
| Stance Time Symmetry Ratio | 0.461 | −0.078 | 0.598 | −0.072 | 0.632 |
| Step Length Symmetry Ratio | 0.288 | 0.044 | 0.768 | 0.040 | 0.790 |
| Duration | 0.043 | 0.271 | 0.062 | 0.327 * | 0.026 |
| Mean Velocity | 0.383 | −0.364 * | 0.011 | 0.370 * | 0.011 |
| N Steps | 0.502 | 0.365 * | 0.011 | 0.367 * | 0.012 |
| Feature 1 | Normality | Correlation with Age | Controlled for Weight and Height | ||
|---|---|---|---|---|---|
| p | r | p | r * | p * | |
| SIT-TO-STAND | |||||
| Range Pitch Vel (i–ii) | 0.408 | −0.307 * | 0.037 | −0.290 | 0.051 |
| Range Pitch Vel (ii–iii) | 0.554 | −0.212 | 0.148 | −0.195 | 0.194 |
| SD Pitch Vel (i–iii) | 0.271 | −0.295 * | 0.042 | −0.279 | 0.060 |
| Mean Pitch Vel (i–iii) | 0.045 | 0.290 * | 0.046 | 0.309 * | 0.036 |
| Median Pitch Vel (i–iii) | 0.222 | 0.132 | 0.372 | 0.110 | 0.466 |
| Max Pitch Vel (i–ii) | 0.825 | 0.314 * | 0.030 | 0.301 * | 0.042 |
| Max Pitch Vel (ii–iii) | 0.152 | 0.093 | 0.528 | 0.104 | 0.493 |
| Mean Pitch Acc (i–ii) | <0.001 | 0.269 | 0.065 | 0.391 ** | 0.007 |
| Mean Pitch Acc (ii–iii) | 0.259 | −0.291 * | 0.045 | −0.289 | 0.052 |
| Mean Acc AP (i–iii) | 0.182 | −0.207 | 0.158 | −0.203 | 0.176 |
| SD Acc AP (i–iii) | 0.192 | −0.020 | 0.890 | 0.021 | 0.892 |
| Median Acc AP (i–iii) | 0.454 | −0.085 | 0.563 | −0.120 | 0.426 |
| Duration (i–iii) | 0.511 | 0.352 * | 0.014 | 0.344 * | 0.019 |
| WALK | |||||
| RMS Acc AP | 0.097 | 0.378 ** | 0.008 | 0.366 * | 0.012 |
| RMS Acc ML | 0.145 | 0.110 | 0.455 | 0.103 | 0.495 |
| RMS Acc V | 0.047 | 0.276 * | 0.058 | 0.299 * | 0.043 |
| Mean Step Time | 0.491 | 0.022 | 0.884 | 0.034 | 0.822 |
| SD Step Time | 0.025 | −0.120 | 0.418 | −0.110 | 0.466 |
| N Steps | 0.003 | 0.403 ** | 0.005 | 0.483 ** | 0.001 |
| Duration | <0.001 | 0.432 ** | 0.002 | 0.488 ** | 0.001 |
| TURN 1 | |||||
| Max Yaw Vel | 0.397 | −0.225 | 0.125 | −0.213 | 0.154 |
| Mean Yaw Acc (i–ii) | <0.001 | −0.203 | 0.167 | −0.181 | 0.228 |
| Mean Yaw Acc (ii–iii) | <0.001 | 0.185 | 0.209 | 0.203 | 0.177 |
| N Steps | 0.460 | −0.169 | 0.251 | −0.187 | 0.212 |
| Duration | 0.217 | 0.100 | 0.500 | 0.094 | 0.535 |
| TURN 2 | |||||
| Max Yaw Vel | 0.829 | −0.457 ** | 0.001 | −0.455 ** | 0.001 |
| Mean Yaw Acc (i–ii) | <0.001 | −0.569 ** | <0.001 | −0.581 ** | <0.001 |
| Mean Yaw Acc (ii–iii) | 0.014 | 0.366 * | 0.010 | 0.315 * | 0.033 |
| N Steps | 0.947 | 0.297 * | 0.040 | 0.296 * | 0.046 |
| Duration | 0.246 | 0.365 * | 0.011 | 0.391 ** | 0.007 |
| STAND-TO-SIT | |||||
| Range Pitch Vel (i–ii) | 0.026 | −0.259 | 0.076 | −0.357 * | 0.015 |
| Range Pitch Vel (ii–iii) | 0.699 | −0.290 * | 0.045 | −0.303 * | 0.041 |
| SD Pitch Vel (i–iii) | 0.101 | −0.313 * | 0.030 | −0.335 * | 0.023 |
| Mean Pitch Vel (i–iii) | 0.362 | −0.066 | 0.654 | −0.084 | 0.581 |
| Median Pitch Vel (i–iii) | 0.761 | −0.066 | 0.657 | −0.097 | 0.521 |
| Max Pitch Vel (i–ii) | 0.002 | 0.213 | 0.146 | 0.315 * | 0.033 |
| Max Pitch Vel (ii–iii) | 0.995 | −0.223 | 0.127 | −0.234 | 0.117 |
| Mean Acc Pitch (i–ii) | 0.001 | 0.328 * | 0.023 | 0.291 * | 0.050 |
| Mean Acc Pitch (ii–iii) | 0.002 | −0.362 * | 0.012 | −0.422 ** | 0.004 |
| Mean Acc AP (i–iii) | 0.839 | −0.365 * | 0.011 | −0.398 ** | 0.006 |
| SD Acc AP (i–iii) | 0.005 | −0.315 * | 0.029 | −0.326 * | 0.027 |
| Median Acc AP (i–iii) | 0.520 | −0.259 | 0.076 | −0.279 | 0.060 |
| Duration (i–iii) | <0.001 | 0.226 | 0.122 | 0.238 | 0.112 |
References
- Perry, J.; Burnfield, J.M. Gait Analysis: Normal and Pathological Function, 2nd ed.; Slack Incorporated: Thorofare, NJ, USA, 2010; pp. 1–551. [Google Scholar]
- Lajoie, Y.; Gallagher, S.P. Predicting falls within the elderly community: Comparison of postural sway, reaction time, the Berg balance scale and the Activities-specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch. Gerontol. Geriatr. 2004, 38, 11–26. [Google Scholar] [CrossRef]
- Barker, S.; Craik, R.; Freedman, W.; Herrmann, N.; Hillstrom, H. Accuracy, reliability, and validity of a spatiotemporal gait analysis system. Med. Eng. Phys. 2006, 28, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Lach, J.; Lo, B.; Yang, G.Z. Toward Pervasive Gait Analysis with Wearable Sensors: A Systematic Review. IEEE J. Biomed. Health Inform. 2016, 20, 1521–1537. [Google Scholar] [CrossRef] [PubMed]
- Schull, P.B.; Jirattigalachote, W.; Hunt, M.A.; Cutkosky, M.R.; Delp, S.L. Quantified self and human movement: A review on the clinical impact of wearable sensing and feedback for gait analysis and intervention. Gait Posture 2014, 40, 11–19. [Google Scholar] [CrossRef]
- Panebianco, G.P.; Bisi, M.C.; Stagni, R.; Fantozzi, S. Analysis of the performance of 17 algorithms from a systematic review: Influence of sensor position, analysed variable and computational approach in gait timing estimation from IMU measurements. Gait Posture 2018, 66, 76–82. [Google Scholar] [CrossRef]
- Caldas, R.; Mundt, M.; Potthast, W.; Buarque de Lima Neto, F.; Markert, B. A systematic review of gait analysis methods based on inertial sensors and adaptive algorithms. Gait Posture 2017, 57, 204–210. [Google Scholar] [CrossRef]
- Hubble, R.P.; Naughton, G.A.; Silburn, P.A.; Cole, M.H. Wearable Sensor Use for Assessing Standing Balance and Walking Stability in People with Parkinson’s Disease: A Systematic Review. PLoS ONE 2015, 10, e0123705. [Google Scholar] [CrossRef]
- Bergamini, E.; Iosa, M.; Belluscio, V.; Morone, G.; Tramontano, M.; Vannozzi, G. Multi-sensor assessment of dynamic balance during gait in patients with subacute stroke. J. Biomech. 2017, 61, 208–215. [Google Scholar] [CrossRef]
- Park, J.H.; Mancini, M.; Carlson-Kuhta, P.; Nutt, J.G.; Horak, F.B. Quantifying effects of age on balance and gait with inertial sensors in community-dwelling healthy adults. Exp Gerontol. 2016, 85, 48–58. [Google Scholar] [CrossRef]
- Moon, Y.; McGinnis, R.S.; Seagers, K.; Motl, R.W.; Sheth, N.; Wright, J.A.; Ghaffari, R.; Sosnoff, J.J. Monitoring gait in multiple sclerosis with novel wearable motion sensors. PLoS ONE 2017, 12, e0171346. [Google Scholar] [CrossRef]
- Sun, R.; Moon, Y.; McGinnis, R.S.; Seagers, K.; Motl, R.W.; Sheth, N.; Wright, J.A.; Ghaffari, R.; Patel, S.; Sosnoff, J.J. Assessment of Postural Sway in Individuals with Multiple Sclerosis Using a Novel Wearable Inertial Sensor. Digit. Biomark. 2018, 2, 1–10. [Google Scholar] [CrossRef]
- Bowden, M.G.; Balasubramanian, C.K.; Behrman, A.L.; Kautz, S.A. Validation of a speed-based classification system using quantitative measures of walking performance poststroke. Neurorehabil. Neural Repair 2008, 22, 672–675. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [PubMed]
- Moe-Nilssen, R. A new method for evaluating motor control in gait under real-life environmental conditions. Part 1: The instrument. Clin. Biomech. 1998, 13, 320–327. [Google Scholar] [CrossRef]
- Del Din, S.; Godfrey, A.; Rochester, L. Validation of an Accelerometer to Quantify a Comprehensive Battery of Gait Characteristics in Healthy Older Adults and Parkinson’s Disease: Toward Clinical and at Home Use. IEEE J. Biomed. Health Inform. 2016, 20, 838–847. [Google Scholar] [CrossRef]
- McCamley, J.; Donati, M.; Grimpampi, E.; Mazza, C. An enhanced estimate of initial contact and final contact instants of time using lower trunk inertial sensor data. Gait Posture 2012, 36, 316–318. [Google Scholar] [CrossRef]
- Najafi, B.; Aminian, K.; Paraschiv-Ionescu, A.; Loew, F.; Bula, C.J.; Robert, P. Ambulatory system for human motion analysis using a kinematic sensor: Monitoring of daily physical activity in the elderly. IEEE Trans. Biomed. Eng. 2003, 50, 711–723. [Google Scholar] [CrossRef]
- Zijlstra, W.; Hof, A.L. Assessment of spatio-temporal gait parameters from trunk accelerations during human walking. Gait Posture 2003, 18, 1–10. [Google Scholar] [CrossRef]
- Zhao, Q.; Zhang, B.; Wang, J.; Feng, W.; Jia, W.; Sun, M. Improved method of step length estimation based on inverted pendulum model. Int. J. Distrib. Sens. Netw. 2017, 13, 1–13. [Google Scholar] [CrossRef]
- Huang, N.E.; Shen, Z.; Long, S.R.; Wu, M.L.; Shih, H.H.; Zheng, Q.; Yen, N.-C.; Tung, C.C.; Liu, H.H. The empirical mode decomposition and Hilbert spectrum for nonlinear and non-stationary time series analysis. Proc. R. Soc. Lond. Ser. A Math. Phys. Eng. Sci. 1998, 454, 903–995. [Google Scholar] [CrossRef]
- Namazi, H.; Kulish, V.V.; Hussaini, J.; Hussaini, J.; Delaviz, A.; Delaviz, F.; Habibi, S.; Ramezanpoor, S. A signal processing based analysis and prediction of seizure onset in patients with epilepsy. Oncotarget 2016, 7, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Pham, M.H.; Elshehabi, M.; Haertner, L.; Del Din, S.; Srulijes, K.; Heger, T.; Synofzik, M.; Hobert, M.A.; Faber, G.S.; Hansen, C.; et al. Validation of a Step Detection Algorithm during Straight Walking and Turning in Patients with Parkinson’s Disease and Older Adults Using an Inertial Measurement Unit at the Lower Back. Front. Neurol. 2017, 8, 457. [Google Scholar] [CrossRef] [PubMed]
- Schubert, P.; Kirchner, M. Ellipse area calculations and their applicability in posturography. Gait Posture 2014, 39, 518–522. [Google Scholar] [CrossRef] [PubMed]
- Vervoort, D.; Vuillerme, N.; Kosse, N.; Hortobágyi, T.; Lamoth, C.J.C. Multivariate analyses and classification of inertial sensor data to identify aging effects on the Timed-Up-and-Go Test. PLoS ONE 2016, 11, e0155984. [Google Scholar] [CrossRef]
- Weiss, A.; Mirelman, A.; Buchman, A.S.; Bennett, D.S.; Hausdorff, J.M. Using a Body-Fixed Sensor to Identify Subclinical Gait Difficulties in Older Adults with IADL Disability: Maximizing the Output of the Timed Up and Go. PLoS ONE 2013, 8, e68885. [Google Scholar] [CrossRef]
- Weiss, A.; Herman, R.; Plotnik, M.; Brozgol, M.; Giladi, N.; Hausdorff, J.M. An instrumented timed up and go: The added value of an accelerometer for identifying fall risk in idiopathic fallers. Physiol. Meas. 2011, 32, 2003–2018. [Google Scholar] [CrossRef]
- Mancini, M.; Salarian, A.; Carlson-Kuhta, P.; Zampieri, C.; King, L.; Chiari, L.; Horak, F.B. ISway: A sensitive, valid and reliable measure of postural control. J. Neuroeng. Rehabil. 2012, 9, 59. [Google Scholar] [CrossRef]
- Palmerini, L.; Rocchi, L.; Mellone, S.; Valzania, F.; Chiari, L. Feature selection for accelerometer-based posture analysis in Parkinson’s disease. IEEE Trans. Inf. Technol. Biomed. 2011, 15, 481–490. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Mukaka, M. A guide to appropriate use of Correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar]
- Lee, C.R.; Farley, C.T. Determinants of the center of mass trajectory in human walking and running. J. Exp. Biol. 1998, 201, 2935–2944. [Google Scholar] [PubMed]
- Takada, R.; Lisco, G.; Fujisawa, T.; Gastaldi, L.; Tohyma, H.; Tadano, S. Drift removal for improving the accuracy of gait parameters using wearable sensor systems. Sensors 2014, 14, 23230–23247. [Google Scholar] [CrossRef] [PubMed]
- Bergamini, E.; Ligorio, G.; Summa, A.; Vannozzi, G.; Cappozzo, A.; Sabatini, A.M. Estimating Orientation Using Magnetic and Inertial Sensors and Different Sensor Fusion Approaches: Accuracy Assessment in Manual and Locomotion Tasks. Sensors 2014, 14, 18625–18649. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.; Clark, R.D.; Webster, I. Postural stability and associated physiological factors in a population of aged persons. J. Gerontol. 1991, 46, M69–M76. [Google Scholar] [CrossRef] [PubMed]
- Steffen, T.M.; Hacker, T.A.; Mollinger, L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys. Ther. 2002, 82, 128–137. [Google Scholar] [PubMed]
- Greve, C.; Zijlstra, W.; Hortobagyi, T.; Bongers, R.M. Not all is lost: Old adults retain flexibility in motor behaviour during sit-to-stand. PLoS ONE 2013, 8, e77760. [Google Scholar] [CrossRef] [PubMed]
- Riley, P.O.; Schenkman, M.L.; Mann, R.W.; Hodge, W.A. Mechanics of a constrained chair-rise. J. Biomech. 1991, 24, 77–85. [Google Scholar] [CrossRef]
- Lummel, R.V. Assessing Sit-to-Stand for Clinical Use. Ph.D. Thesis, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands, 2017. [Google Scholar]
- Della Croce, U.; Cereatti, A.; Mancini, M. Gait Parameters Estimated Using Inertial Measurement Units. In Handbook of Human Motion; Müller, B., Wolf, S., Eds.; Springer: Cham, Switzerland, 2018; pp. 245–265. [Google Scholar]
- Anwary, A.R.; Yu, H.; Vassallo, M. An automatic gait feature extraction method for identifying gait asymmetry using wearable sensors. Sensors 2008, 18, 676. [Google Scholar] [CrossRef]
- Lau, H.; Tong, K. The reliability of using accelerometer and gyroscope for gait event identification on persons with dropped foot. Gait Posture 2008, 27, 248–257. [Google Scholar] [CrossRef]
- Trojaniello, D.; Cereatti, A.; Pelosin, E.; Avanzino, L.; Mirelman, A.; Hausdorff, J.M.; Della Croce, U. Estimation of step-by-step spatio-temporal parameters of normal and impaired gait using shank-mounted magneto-inertial sensors: Application to elderly, hemiparetic, parkinsonian and choreic gait. J. Neuroeng. Rehabil. 2014, 11, 152. [Google Scholar] [CrossRef]
| Group | N | Age (years) | Height (cm) | Weight (kg) | Female | Male |
|---|---|---|---|---|---|---|
| Ages 20–34 | 14 | 26.4 (3.9) | 173.0 (11.4) | 71.5 (13.8) | 6 | 8 |
| Ages 35–54 | 19 | 43.7 (5.8) | 169.9 (12.8) | 79.2 (23.7) | 11 | 8 |
| Ages 55–70 | 16 | 61.8 (5.1) | 169.7 (7.5) | 73.1 (15.9) | 8 | 8 |
| Stroke | 1 | 57 | 185.4 | 82.8 | 0 | 1 |
| Test | Feature | Reference | Units | Definition |
|---|---|---|---|---|
| BBS | F50% (AP, ML) | [28,29] | Hz | Frequency accounting for 50% of total power of the signal |
| F95% (AP, ML) | [28,29] | Hz | Frequency accounting for 95% of total power of the signal | |
| SC (AP, ML) | [28,29] | Hz | Spectral centroid (indicates center of mass of the spectrum) | |
| Max Acc (AP, ML) | m/s2 | Maximum acceleration | ||
| Mean Acc (AP, ML) | m/s2 | Mean acceleration | ||
| RMS (AP, ML) | [12,28] | m/s2 | Root mean square of acceleration | |
| Ellipse Angles (AP, ML) | [12,29] | m/s2 | Angles of 95% of ellipse orientation | |
| 95% Ellipse Area | m2/s4 | Area of 95% ellipse | ||
| Ellipse Axis (AP, ML) | [29] | m/s2 | Length of 95% ellipse axis | |
| Jerk (AP, ML) | [12] | m/s3 | Smoothness of sway (time derivative of acceleration) | |
| SwayV (AP, ML) | [12,28] | m/s | Mean sway velocity | |
| SPathA (AP, ML) | [28] | m/s2 | Total acceleration path | |
| 10MWT | Mean Vertical Displacement | m | Vertical displacement of the body Center of Mass (CoM) | |
| Mean Stance Time (SSV, FV) | [16] | s | Length of time for which the foot is in contact with the ground | |
| Mean Step Time (SSV, FV) | [16] | s | Length of time between successive ICs of opposite feet | |
| Mean Stride Time (SSV, FV) | [16] | s | Length of time between successive ICs of the same foot | |
| Mean Swing Time (SSV, FV) | [16] | s | Length of time for which the foot is not in contact with the ground | |
| Mean Step Length (SSV, FV) | [16] | cm | Distance between successive ICs of opposite feet | |
| Maximum Power Frequency (SSV, FV) | (m/s2)2/Hz | Maximum power from the power spectral density of vertical acceleration | ||
| Stance Time Symmetry Ratio (SSV, FV) | unitless | Stance time ratio of right and left leg (temporal symmetry) | ||
| Step Length Symmetry Ratio (SSV, FV) | unitless | Step length ratio of right and left leg (spatial symmetry) | ||
| Duration (SSV, FV) | s | Time required to complete the test, averaged over three trials | ||
| Mean Velocity (SSV, FV) | [16] | m/s | Mean step velocity | |
| N Steps (SSV, FV) | unitless | Number of steps taken | ||
| Velocity Difference, FV–SSV | m/s | Difference in average walking velocity between SSV and FV modes | ||
| TUG—Sit to Stand, Stand to Sit | Range Pitch Vel (i–ii, ii–iii)2 | [25] | °/s | Difference between the minimum and maximum values of angular velocity (pitch axis) |
| SD Pitch Vel (i–iii) | [25] | °/s | Standard deviation of angular velocity (pitch axis) | |
| Mean Pitch Vel (i–iii) | [25] | °/s | Mean value of angular velocity (pitch axis) | |
| Median Pitch Vel (i–iii) | [25] | °/s | Median value of angular velocity (pitch axis) | |
| Max Pitch Vel (i–ii, ii–iii) | [25] | °/s | Maximum value of angular velocity (pitch axis) | |
| Mean Pitch Acc (i–ii, ii–iii) | [25] | °/s2 | Average rate of change of angular velocity (angular acceleration, pitch axis) | |
| Mean Acc AP (i–iii) | [25] | m/s2 | Mean phase value of AP acceleration | |
| SD Acc AP (i–iii) | [25] | m/s2 | Standard deviation of AP acceleration | |
| Median Acc AP (i–iii) | [25] | m/s2 | Median value of AP acceleration | |
| Duration (i–iii) | [25] | s | Time required to complete the phase | |
| TUG—Turn 1, Turn 2 | N Steps | [25] | unitless | Number of steps taken |
| Max Yaw Vel | [25] | °/s | Maximum value of angular velocity magnitude (yaw axis) | |
| Mean Yaw Acc (i–ii, ii–iii) | [25] | °/s2 | Average rate of change of angular velocity (angular acceleration, yaw axis) | |
| Duration | [25] | s | Time required to complete the turn phase | |
| TUG—Walk 1 + Walk 2 | RMS Acc (AP, ML, V) | [25] | m/s2 | Root mean square of acceleration |
| Mean Step Time | [25] | s | Mean step time over the two walking phases | |
| SD Step Time | [25] | s | Standard deviation of step time | |
| N Steps | [25] | unitless | Number of steps taken | |
| Duration | [25] | s | Time required to complete the walking phase | |
| Naturalistic Walking | N Steps | unitless | Number of steps taken |
| Feature | Model no. | Standardized Beta Coefficients | R2 | R2 Change | F Change | df | p | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Weight | Height | Sex | Age | |||||||
| BBS-SU | ||||||||||
| F95% ML | 1 | −0.246 | 0.061 | 0.061 | 3.03 | 1, 47 | 0.088 | |||
| 2 | −0.429 | 0.295 | 0.114 | 0.054 | 2.78 | 1, 46 | 0.10 | |||
| 3 | −0.416 | 0.347 | −0.076 | 0.116 | 0.002 | 0.10 | 1, 45 | 0.75 | ||
| 4 | −0.374 | 0.305 | −0.074 | −0.363 | 0.247 | 0.131 | 7.62 | 1, 44 | 0.008 | |
| BBS-SEC | ||||||||||
| SC ML | 1 | −0.100 | 0.010 | 0.010 | 0.48 | 1, 47 | 0.49 | |||
| 2 | −0.206 | 0.170 | 0.028 | 0.018 | 0.84 | 1, 46 | 0.37 | |||
| 3 | −0.184 | 0.251 | −0.119 | 0.033 | 0.005 | 0.23 | 1, 45 | 0.63 | ||
| 4 | −0.143 | 0.209 | −0.117 | −0.365 | 0.165 | 0.132 | 6.95 | 1, 44 | 0.012 | |
| BBS-SFT | ||||||||||
| F95% ML | 1 | −0.165 | 0.027 | 0.027 | 1.31 | 1, 47 | 0.26 | |||
| 2 | −0.212 | 0.077 | 0.031 | 0.004 | 0.17 | 1, 46 | 0.68 | |||
| 3 | −0.162 | 0.268 | −0.281 | 0.058 | 0.028 | 1.31 | 1, 45 | 0.26 | ||
| 4 | −0.127 | 0.234 | −0.279 | −0.301 | 0.148 | 0.090 | 4.65 | 1, 44 | 0.037 | |
| BBS-ST | ||||||||||
| F50% AP | 1 | 0.022 | <0.001 | <0.001 | 0.02 | 1, 47 | 0.88 | |||
| 2 | −0.073 | 0.152 | 0.015 | 0.015 | 0.68 | 1, 46 | 0.42 | |||
| 3 | -0.071 | 0.158 | −0.008 | 0.015 | <0.001 | 0.001 | 1, 45 | 0.98 | ||
| 4 | −0.037 | 0.123 | −0.006 | −0.300 | 0.104 | 0.089 | 4.39 | 1, 44 | 0.042 | |
| BBS-SOL | ||||||||||
| Max Acc ML | 1 | −0.059 | 0.003 | 0.003 | 0.16 | 1, 47 | 0.69 | |||
| 2 | −0.157 | 0.158 | 0.019 | 0.015 | 0.72 | 1, 46 | 0.40 | |||
| 3 | −0.092 | 0.405 | −0.362 | 0.065 | 0.046 | 2.20 | 1, 45 | 0.15 | ||
| 4 | −0.131 | 0.445 | −0.364 | 0.347 | 0.184 | 0.119 | 6.42 | 1, 44 | 0.015 | |
| Mean Acc ML | 1 | −0.120 | 0.014 | 0.014 | 0.69 | 1, 47 | 0.41 | |||
| 2 | −0.164 | 0.070 | 0.017 | 0.003 | 0.14 | 1, 46 | 0.71 | |||
| 3 | −0.098 | 0.321 | −0.368 | 0.065 | 0.047 | 2.27 | 1, 45 | 0.14 | ||
| 4 | −0.140 | 0.363 | −0.370 | 0.376 | 0.205 | 0.140 | 7.74 | 1, 44 | 0.008 | |
| RMS ML | 1 | −0.091 | 0.008 | 0.008 | 0.40 | 1, 47 | 0.53 | |||
| 2 | −0.159 | 0.109 | 0.016 | 0.007 | 0.34 | 1, 46 | 0.56 | |||
| 3 | −0.098 | 0.342 | −0.341 | 0.056 | 0.041 | 1.94 | 1, 45 | 0.17 | ||
| 4 | −0.140 | 0.385 | −0.343 | 0.378 | 0.198 | 0.142 | 7.78 | 1, 44 | 0.008 | |
| Ellipse Axis AP | 1 | −0.030 | 0.001 | 0.001 | 0.04 | 1, 47 | 0.84 | |||
| 2 | −0.110 | 0.128 | 0.011 | 0.010 | 0.47 | 1, 46 | 0.50 | |||
| 3 | −0.042 | 0.386 | −0.377 | 0.061 | 0.050 | 2.38 | 1, 45 | 0.13 | ||
| 4 | −0.078 | 0.422 | −0.379 | 0.316 | 0.160 | 0.099 | 5.19 | 1, 44 | 0.028 | |
| SwayV ML | 1 | −0.187 | 0.035 | 0.035 | 1.70 | 1, 47 | 0.20 | |||
| 2 | −0.192 | 0.009 | 0.035 | <0.001 | 0.002 | 1, 46 | 0.96 | |||
| 3 | −0.109 | 0.322 | −0.460 | 0.109 | 0.074 | 3.725 | 1, 45 | 0.060 | ||
| 4 | −0.146 | 0.359 | −0.462 | 0.321 | 0.211 | 0.102 | 5.678 | 1, 44 | 0.022 | |
| 10MWT-SSV | ||||||||||
| Mean Stance Time | 1 | 0.373 | 0.139 | 0.139 | 7.59 | 1, 47 | 0.008 | |||
| 2 | 0.051 | 0.521 | 0.307 | 0.168 | 11.14 | 1, 46 | 0.002 | |||
| 3 | 0.016 | 0.384 | 0.200 | 0.321 | 0.014 | 0.91 | 1, 45 | 0.35 | ||
| 4 | −0.022 | 0.423 | 0.206 | 0.265 | 0.390 | 0.069 | 4.97 | 1, 44 | 0.031 | |
| Mean Step Length | 1 | 0.388 | 0.151 | 0.151 | 8.34 | 1, 47 | 0.006 | |||
| 2 | 0.076 | 0.506 | 0.309 | 0.158 | 10.53 | 1, 46 | 0.002 | |||
| 3 | 0.026 | 0.313 | 0.280 | 0.336 | 0.027 | 1.84 | 1, 45 | 0.18 | ||
| 4 | 0.069 | 0.268 | 0.272 | −0.305 | 0.427 | 0.092 | 7.03 | 1, 44 | 0.011 | |
| Duration | 1 | 0.186 | 0.035 | 0.035 | 1.69 | 1, 47 | 0.20 | |||
| 2 | 0.100 | 0.139 | 0.047 | 0.012 | 0.58 | 1, 46 | 0.45 | |||
| 3 | 0.087 | 0.089 | 0.074 | 0.049 | 0.002 | 0.09 | 1, 45 | 0.77 | ||
| 4 | 0.044 | 0.134 | 0.082 | 0.306 | 0.140 | 0.092 | 4.69 | 1, 44 | 0.036 | |
| Mean Velocity | 1 | −0.044 | 0.002 | 0.002 | 0.09 | 1, 47 | 0.77 | |||
| 2 | −0.009 | −0.057 | 0.004 | 0.002 | 0.09 | 1, 46 | 0.76 | |||
| 3 | −0.010 | −0.063 | 0.009 | 0.004 | <0.001 | 0.001 | 1, 45 | 0.97 | ||
| 4 | 0.044 | −0.121 | −0.001 | −0.388 | 0.152 | 0.148 | 7.68 | 1, 44 | 0.008 | |
| 10MWT-FV | ||||||||||
| Mean Step Length | 1 | 0.516 | 0.266 | 0.266 | 16.67 | 1, 47 | <0.001 | |||
| 2 | 0.221 | 0.485 | 0.414 | 0.148 | 11.38 | 1, 46 | 0.002 | |||
| 3 | 0.122 | 0.097 | 0.566 | 0.527 | 0.113 | 10.50 | 1, 45 | 0.002 | ||
| 4 | 0.160 | 0.055 | 0.559 | −0.281 | 0.604 | 0.077 | 8.41 | 1, 44 | 0.006 | |
| Maximum Power Frequency | 1 | 0.138 | 0.019 | 0.019 | 0.89 | 1, 47 | 0.35 | |||
| 2 | 0.140 | −0.004 | 0.019 | <0.001 | 0.001 | 1, 46 | 0.98 | |||
| 3 | 0.095 | −0.179 | 0.255 | 0.042 | 0.023 | 1.05 | 1, 45 | 0.31 | ||
| 4 | 0.145 | −0.233 | 0.246 | −0.361 | 0.170 | 0.128 | 6.61 | 1, 44 | 0.014 | |
| Duration | 1 | 0.104 | 0.011 | 0.011 | 0.51 | 1, 47 | 0.48 | |||
| 2 | 0.145 | −0.067 | 0.014 | 0.003 | 0.13 | 1, 46 | 0.72 | |||
| 3 | 0.152 | −0.041 | −0.038 | 0.014 | 0.001 | 0.02 | 1, 45 | 0.88 | ||
| 4 | 0.107 | 0.008 | −0.030 | 0.328 | 0.120 | 0.106 | 5.16 | 1, 44 | 0.028 | |
| Mean Velocity | 1 | 0.155 | 0.024 | 0.024 | 1.14 | 1, 47 | 0.29 | |||
| 2 | 0.110 | 0.074 | 0.028 | 0.003 | 0.16 | 1, 46 | 0.69 | |||
| 3 | 0.083 | −0.032 | 0.155 | 0.036 | 0.008 | 0.39 | 1, 45 | 0.54 | ||
| 4 | 0.133 | −0.086 | 0.146 | −0.367 | 0.168 | 0.132 | 6.81 | 1, 44 | 0.012 | |
| N Steps | 1 | −0.259 | 0.067 | 0.067 | 3.31 | 1, 47 | 0.075 | |||
| 2 | 0.022 | −0.463 | 0.202 | 0.135 | 7.63 | 1, 46 | 0.008 | |||
| 3 | 0.100 | −0.162 | −0.439 | 0.270 | 0.068 | 4.10 | 1, 45 | 0.049 | ||
| 4 | 0.055 | −0.114 | −0.431 | 0.327 | 0.375 | 0.105 | 7.21 | 1, 44 | 0.010 | |
| TUG- SIT-TO-STAND | ||||||||||
| Mean Pitch Vel (i–iii) | 1 | 0.101 | 0.010 | 0.010 | 0.47 | 1, 47 | 0.50 | |||
| 2 | 0.338 | −0.383 | 0.100 | 0.090 | 4.51 | 1, 46 | 0.039 | |||
| 3 | 0.240 | −0.378 | −0.007 | 0.100 | <0.001 | 0.001 | 1, 45 | 0.98 | ||
| 4 | 0.304 | −0.344 | −0.005 | 0.295 | 0.186 | 0.086 | 4.55 | 1, 44 | 0.039 | |
| Max Pitch Vel (i–ii) | 1 | 0.227 | 0.052 | 0.052 | 2.51 | 1, 47 | 0.12 | |||
| 2 | 0.373 | −0.235 | 0.086 | 0.034 | 1.67 | 1, 46 | 0.20 | |||
| 3 | 0.371 | −0.243 | 0.012 | 0.086 | <0.001 | 0.002 | 1, 45 | 0.961 | ||
| 4 | 0.336 | −0.210 | 0.014 | 0.290 | 0.169 | 0.083 | 4.29 | 1, 44 | 0.044 | |
| Mean Pitch Acc (i–ii) | 1 | 0.036 | 0.001 | 0.001 | 0.06 | 1, 47 | 0.81 | |||
| 2 | 0.201 | −0.266 | 0.045 | 0.043 | 2.05 | 1, 46 | 0.16 | |||
| 3 | 0.162 | −0.411 | 0.214 | 0.061 | 0.016 | 0.75 | 1, 45 | 0.39 | ||
| 4 | 0.116 | −0.366 | 0.217 | 0.385 | 0.207 | 0.146 | 7.94 | 1, 44 | 0.007 | |
| Duration (i–iii) | 1 | 0.091 | 0.008 | 0.008 | 0.39 | 1, 47 | 0.54 | |||
| 2 | 0.165 | −0.119 | 0.017 | 0.009 | 0.40 | 1, 46 | 0.53 | |||
| 3 | 0.144 | −0.197 | 0.115 | 0.022 | 0.005 | 0.21 | 1, 45 | 0.649 | ||
| 4 | 0.103 | −0.157 | 0.118 | 0.344 | 0.138 | 0.117 | 5.83 | 1, 44 | 0.020 | |
| TUG-WALK | ||||||||||
| RMS Acc AP | 1 | 0.118 | 0.014 | 0.014 | 0.65 | 1, 47 | 0.43 | |||
| 2 | 0.272 | −0.248 | 0.052 | 0.038 | 1.80 | 1, 46 | 0.19 | |||
| 3 | 0.333 | −0.023 | −0.332 | 0.091 | 0.039 | 1.87 | 1, 45 | 0.18 | ||
| 4 | 0.290 | 0.018 | −0.329 | 0.357 | 0.217 | 0.126 | 6.94 | 1, 44 | 0.012 | |
| N Steps | 1 | 0.024 | 0.001 | 0.001 | 0.03 | 1, 47 | 0.87 | |||
| 2 | −0.060 | 0.136 | 0.012 | 0.011 | 0.52 | 1, 46 | 0.48 | |||
| 3 | −0.057 | 0.148 | −0.017 | 0.012 | <0.001 | 0.005 | 1, 45 | 0.95 | ||
| 4 | −0.115 | 0.203 | −0.013 | 0.483 | 0.243 | 0.231 | 13.10 | 1, 44 | 0.001 | |
| Duration | 1 | 0.124 | 0.015 | 0.015 | 0.71 | 1, 47 | 0.40 | |||
| 2 | 0.027 | 0.155 | 0.030 | 0.015 | 0.69 | 1, 46 | 0.41 | |||
| 3 | 0.018 | 0.120 | 0.051 | 0.031 | 0.001 | 0.04 | 1, 45 | 0.84 | ||
| 4 | −0.040 | 0.176 | 0.055 | 0.483 | 0.262 | 0.231 | 13.48 | 1, 44 | 0.001 | |
| TUG-TURN 2 | ||||||||||
| Max Yaw Vel | 1 | −0.136 | 0.019 | 0.019 | 0.87 | 1, 47 | 0.36 | |||
| 2 | −0.167 | 0.049 | 0.020 | 0.001 | 0.07 | 1, 46 | 0.80 | |||
| 3 | −0.178 | 0.007 | 0.062 | 0.021 | 0.001 | 0.06 | 1, 45 | 0.80 | ||
| 4 | −0.124 | −0.045 | 0.058 | −0.453 | 0.224 | 0.203 | 11.23 | 1, 44 | 0.002 | |
| Mean Yaw Acc (i–ii) | 1 | −0.145 | 0.021 | 0.021 | 0.99 | 1, 47 | 0.33 | |||
| 2 | −0.051 | −0.153 | 0.035 | 0.014 | 0.67 | 1, 46 | 0.42 | |||
| 3 | −0.061 | −0.193 | 0.059 | 0.037 | 0.001 | 0.06 | 1, 45 | 0.81 | ||
| 4 | 0.007 | −0.259 | 0.055 | −0.573 | 0.362 | 0.325 | 21.88 | 1, 44 | <0.001 | |
| Mean Yaw Acc (ii–iii) | 1 | 0.300 | 0.090 | 0.090 | 4.55 | 1, 47 | 0.038 | |||
| 2 | 0.353 | −0.086 | 0.094 | 0.005 | 0.23 | 1, 46 | 0.64 | |||
| 3 | 0.331 | −0.169 | 0.123 | 0.100 | 0.005 | 0.26 | 1, 45 | 0.61 | ||
| 4 | 0.294 | −0.135 | 0.126 | 0.302 | 0.190 | 0.090 | 4.79 | 1, 44 | 0.034 | |
| Duration | 1 | 0.459 | 0.210 | 0.210 | 12.26 | 1, 47 | 0.001 | |||
| 2 | 0.460 | −0.001 | 0.210 | <0.001 | <0.001 | 1, 46 | 0.99 | |||
| 3 | 0.453 | −0.026 | 0.036 | 0.211 | <0.001 | 0.03 | 1, 45 | 0.87 | ||
| 4 | 0.411 | 0.014 | 0.039 | 0.349 | 0.331 | 0.121 | 7.75 | 1, 44 | 0.008 | |
| TUG-STAND-TO-SIT | ||||||||||
| Range Pitch Vel (i–ii) | 1 | −0.331 | 0.109 | 0.109 | 5.64 | 1, 47 | 0.022 | |||
| 2 | −0.297 | −0.054 | 0.111 | 0.002 | 0.09 | 1, 46 | 0.76 | |||
| 3 | −0.259 | 0.084 | −0.204 | 0.126 | 0.015 | 0.74 | 1, 45 | 0.40 | ||
| 4 | −0.219 | 0.045 | −0.207 | −0.339 | 0.239 | 0.113 | 6.41 | 1, 44 | 0.015 | |
| Range Pitch Vel (ii–iii) | 1 | −0.408 | 0.166 | 0.166 | 9.16 | 1, 47 | 0.004 | |||
| 2 | −0.388 | −0.031 | 0.167 | 0.001 | 0.03 | 1, 46 | 0.86 | |||
| 3 | −0.314 | 0.244 | −0.406 | 0.225 | 0.058 | 3.30 | 1, 45 | 0.076 | ||
| 4 | −0.280 | 0.212 | −0.408 | −0.279 | 0.302 | 0.077 | 4.74 | 1, 44 | 0.035 | |
| SD Pitch Vel (i–iii) | 1 | −0.401 | 0.161 | 0.161 | 8.83 | 1, 47 | 0.005 | |||
| 2 | −0.333 | −0.109 | 0.168 | 0.007 | 0.40 | 1, 46 | 0.53 | |||
| 3 | −0.272 | 0.119 | −0.337 | 0.208 | 0.040 | 2.22 | 1, 45 | 0.14 | ||
| 4 | −0.235 | 0.083 | −0.339 | −0.308 | 0.302 | 0.094 | 5.80 | 1, 44 | 0.020 | |
| Mean Pitch Acc (i–ii) | 1 | 0.196 | 0.038 | 0.038 | 1.84 | 1, 47 | 0.18 | |||
| 2 | 0.101 | 0.154 | 0.053 | 0.015 | 0.69 | 1, 46 | 0.41 | |||
| 3 | 0.038 | −0.076 | 0.339 | 0.094 | 0.041 | 1.97 | 1, 45 | 0.17 | ||
| 4 | 0.004 | −0.043 | 0.341 | 0.286 | 0.174 | 0.081 | 4.21 | 1, 44 | 0.046 | |
| Mean Pitch Acc (ii–iii) | 1 | −0.440 | 0.194 | 0.194 | 11.04 | 1, 47 | 0.002 | |||
| 2 | −0.319 | −0.195 | 0.217 | 0.023 | 1.35 | 1, 46 | 0.25 | |||
| 3 | −0.290 | −0.088 | −0.158 | 0.226 | 0.009 | 0.50 | 1, 45 | 0.48 | ||
| 4 | −0.245 | −0.132 | −0.161 | −0.376 | 0.365 | 0.140 | 9.46 | 1, 44 | 0.004 | |
| Mean Acc AP (i–iii) | 1 | −0.320 | 0.102 | 0.102 | 5.25 | 1, 47 | 0.027 | |||
| 2 | −0.176 | −0.233 | 0.136 | 0.033 | 1.74 | 1, 46 | 0.19 | |||
| 3 | −0.142 | −0.109 | −0.183 | 0.148 | 0.012 | 0.61 | 1, 45 | 0.44 | ||
| 4 | −0.097 | −0.152 | −0.186 | −0.372 | 0.285 | 0.137 | 8.25 | 1, 44 | 0.006 | |
| SD Acc AP (i–iii) | 1 | −0.279 | 0.078 | 0.078 | 3.89 | 1, 47 | 0.055 | |||
| 2 | −0.233 | −0.075 | 0.081 | 0.003 | 0.17 | 1, 46 | 0.68 | |||
| 3 | −0.174 | 0.143 | −0.322 | 0.118 | 0.036 | 1.82 | 1, 45 | 0.19 | ||
| 4 | −0.136 | 0.107 | −0.324 | −0.315 | 0.216 | 0.098 | 5.39 | 1, 44 | 0.025 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Brien, M.K.; Hidalgo-Araya, M.D.; Mummidisetty, C.K.; Vallery, H.; Ghaffari, R.; Rogers, J.A.; Lieber, R.; Jayaraman, A. Augmenting Clinical Outcome Measures of Gait and Balance with a Single Inertial Sensor in Age-Ranged Healthy Adults. Sensors 2019, 19, 4537. https://doi.org/10.3390/s19204537
O’Brien MK, Hidalgo-Araya MD, Mummidisetty CK, Vallery H, Ghaffari R, Rogers JA, Lieber R, Jayaraman A. Augmenting Clinical Outcome Measures of Gait and Balance with a Single Inertial Sensor in Age-Ranged Healthy Adults. Sensors. 2019; 19(20):4537. https://doi.org/10.3390/s19204537
Chicago/Turabian StyleO’Brien, Megan K., Marco D. Hidalgo-Araya, Chaithanya K. Mummidisetty, Heike Vallery, Roozbeh Ghaffari, John A. Rogers, Richard Lieber, and Arun Jayaraman. 2019. "Augmenting Clinical Outcome Measures of Gait and Balance with a Single Inertial Sensor in Age-Ranged Healthy Adults" Sensors 19, no. 20: 4537. https://doi.org/10.3390/s19204537
APA StyleO’Brien, M. K., Hidalgo-Araya, M. D., Mummidisetty, C. K., Vallery, H., Ghaffari, R., Rogers, J. A., Lieber, R., & Jayaraman, A. (2019). Augmenting Clinical Outcome Measures of Gait and Balance with a Single Inertial Sensor in Age-Ranged Healthy Adults. Sensors, 19(20), 4537. https://doi.org/10.3390/s19204537








