Wearable Sensor Data to Track Subject-Specific Movement Patterns Related to Clinical Outcomes Using a Machine Learning Approach
Abstract
1. Introduction
2. Methods
2.1. Subjects
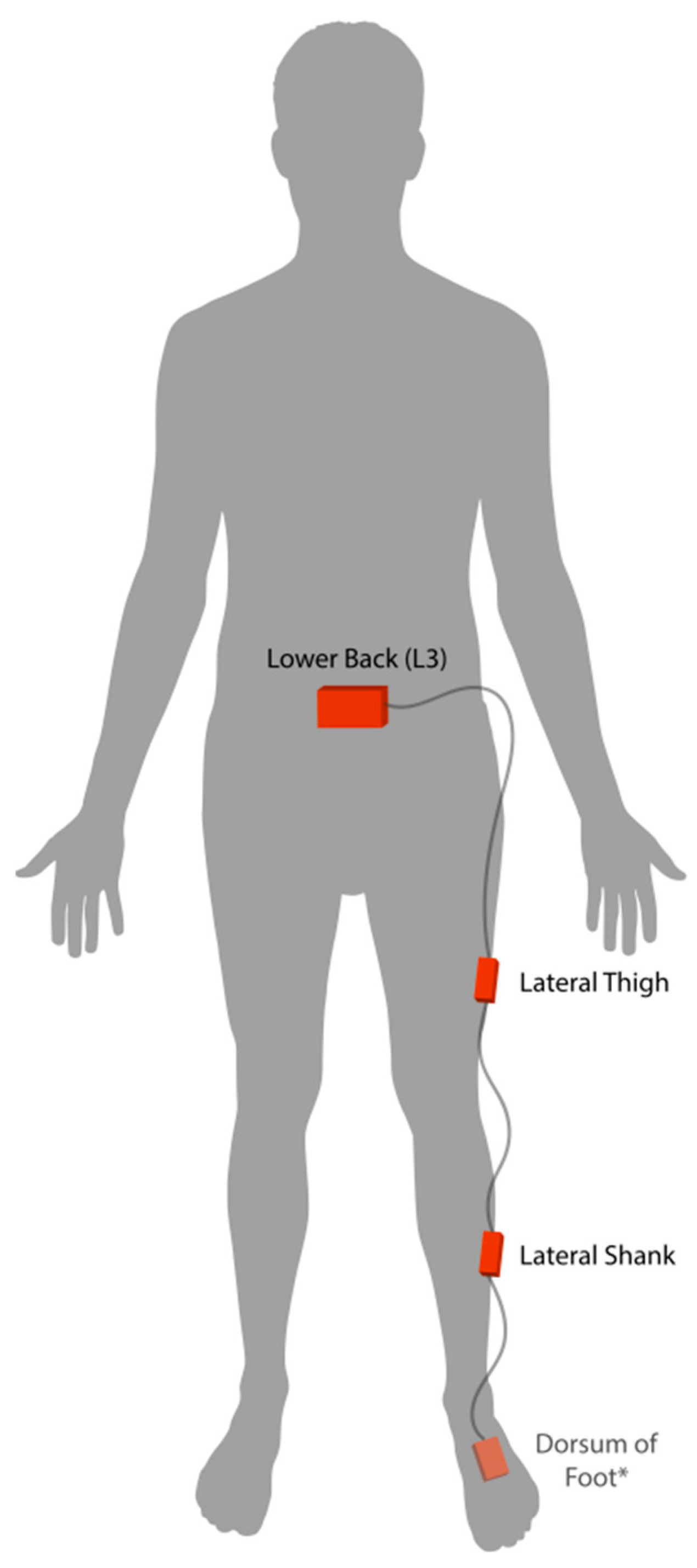
2.2. Protocol
2.3. Data Analysis
2.3.1. Pre-Processing
2.3.2. Data Reduction and Feature Selection
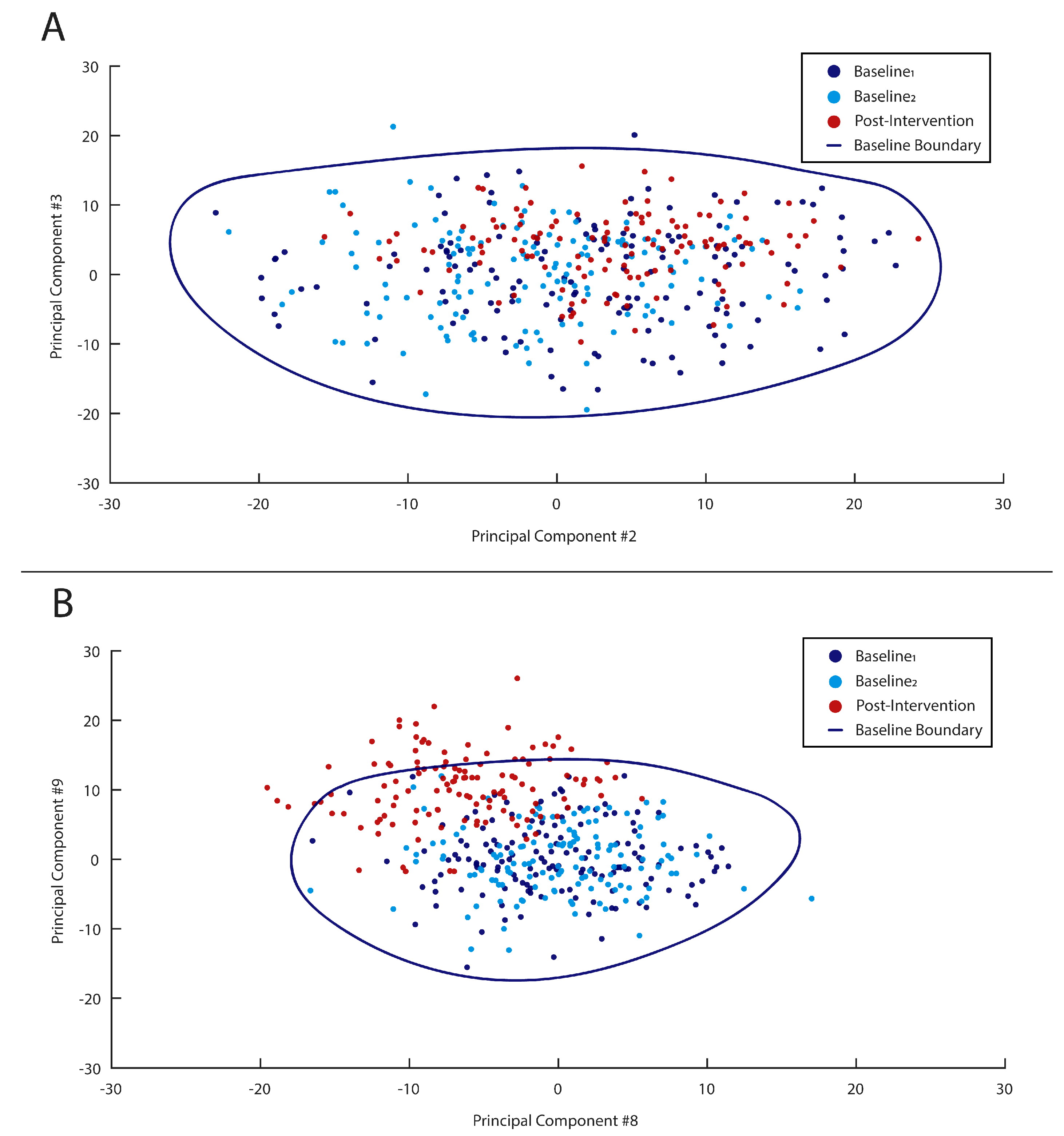
2.3.3. Defining Subject-Specific One-Class Models
2.3.4. Statistical Analysis
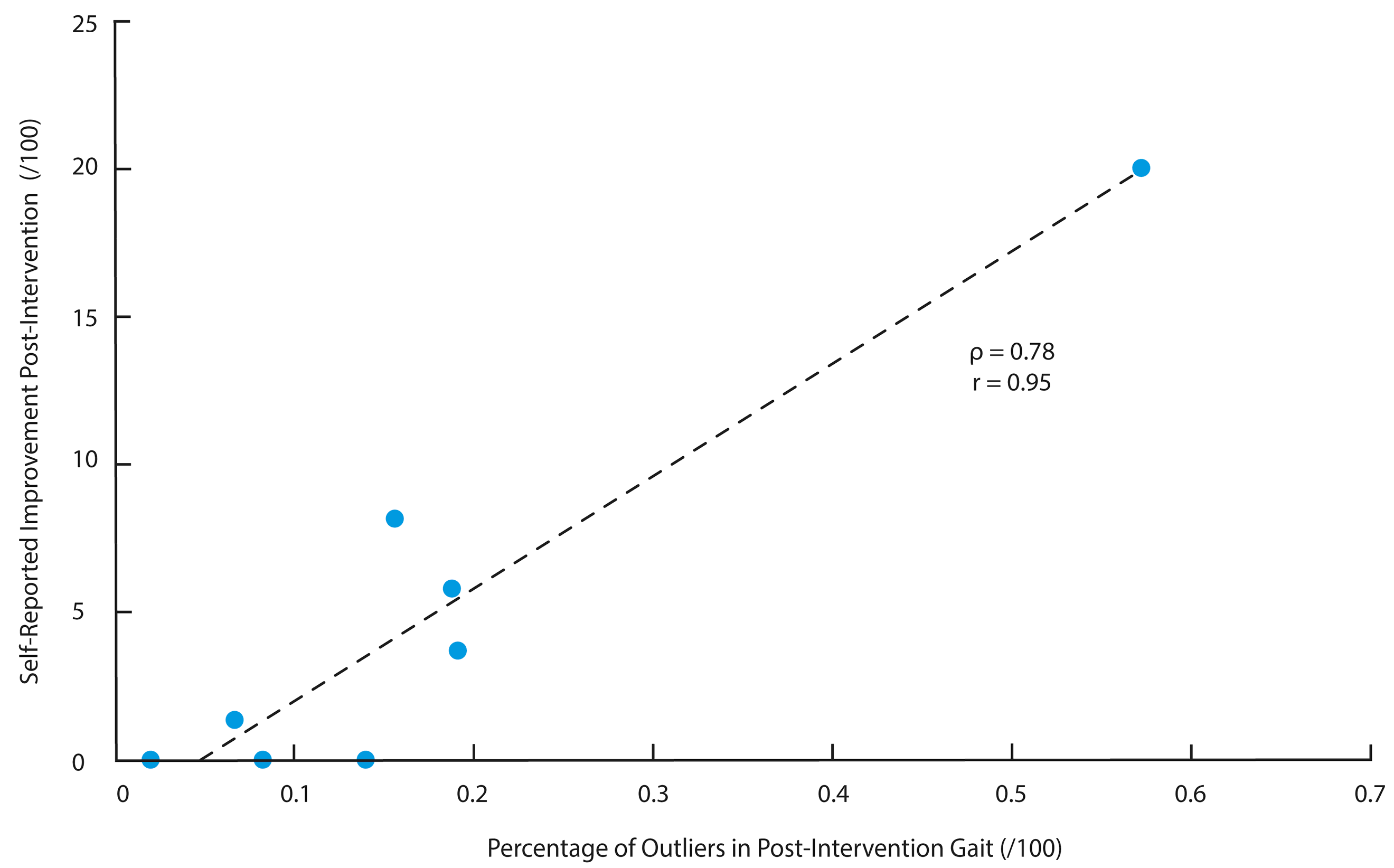
3. Results
4. Discussion
Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tao, W.; Liu, T.; Zheng, R.; Feng, H. Gait analysis using wearable sensors. Sensors 2012, 12, 2255–2283. [Google Scholar] [CrossRef] [PubMed]
- Shull, P.B.; Jirattigalachote, W.; Hunt, M.A.; Cutkosky, M.R.; Delp, S.L. Quantified self and human movement: A review on the clinical impact of wearable sensing and feedback for gait analysis and intervention. Gait Posture 2014, 40, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Yan, S.; Fang, C.; Guo, X.; Zhang, K. Clinical evaluation and gait characteristics before and after yotal knee arthroplasty based on a portable gait analyzer. Orthop. Surg. 2016, 8, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Barrois, R.; Gregory, T.; Oudre, L.; Moreau, T.; Truong, C.; Pulini, A.A.; Vienne, A.; Labourdette, C.; Vayatis, N.; Buffat, S.; et al. An automated recording method in clinical consultation to rate the limp in lower limb osteoarthritis. PLoS ONE 2016, 11, e0164975. [Google Scholar] [CrossRef] [PubMed]
- Pau, M.; Caggiari, S.; Mura, A.; Corona, F.; Leban, B.; Coghe, G.; Lorefice, L.; Marrosu, M.G.; Cocco, E. Clinical assessment of gait in individuals with multiple sclerosis using wearable inertial sensors: Comparison with patient-based measure. Mult. Scler. Relat. Disord. 2016, 10, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Ferber, R.; Osis, S.T.; Hicks, J.L.; Delp, S.L. Gait biomechanics in the era of data science. J. Biomech. 2016, 49, 3759–3761. [Google Scholar] [CrossRef] [PubMed]
- Gregory, C.M.; Embry, A.; Perry, L.; Bowden, M.G. Quantifying human movement across the continuum of care: From lab to clinic to community. J. Neurosci. Methods 2014, 231, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Bataille, L.R.; Martig, A.K. Enabling breakthroughs in Parkinson’s disease with wearable technologies and big data analytics. Mhealth 2016, 2, 20. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Lach, J.; Lo, B.; Yang, G.Z. Toward pervasive gait analysis with wearable sensors: A systematic review. IEEE J. Biomed. Health Inform. 2016, 20, 1521–1537. [Google Scholar] [CrossRef] [PubMed]
- Deo, R.C. Machine learning in medicine. Circulation 2015, 132, 1920–1930. [Google Scholar] [CrossRef] [PubMed]
- Kobsar, D.; Osis, S.T.; Boyd, J.E.; Hettinga, B.A.; Ferber, R. Wearable sensors to predict improvement following an exercise intervention in patients with knee osteoarthritis. J. Neuroeng. Rehabil. 2017, 14, 94. [Google Scholar] [CrossRef] [PubMed]
- Mannini, A.; Trojaniello, D.; Cereatti, A.; Sabatini, A.M. A machine learning framework for gait classification using inertial sensors: Application to elderly, post-stroke and huntington’s disease patients. Sensors 2016, 16, 134. [Google Scholar] [CrossRef] [PubMed]
- Palmerini, L.; Rocchi, L.; Mazilu, S.; Gazit, E.; Hausdorff, J.M.; Chiari, L. Identification of characteristic motor patterns preceding freezing of gait in Parkinson’s disease using wearable sensors. Front. Neurol. 2017, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Drover, D.; Howcroft, J.; Kofman, J.; Lemaire, E.D. Faller classification in older adults using wearable sensors based on turn and straight-walking accelerometer-based features. Sensors 2017, 17, 321. [Google Scholar] [CrossRef] [PubMed]
- Riaz, Q.; Vögele, A.; Krüger, B.; Weber, A. One small step for a man: Estimation of gender, age and height from recordings of one step by a single inertial sensor. Sensors 2015, 15, 31999–32019. [Google Scholar] [CrossRef] [PubMed]
- Lubetzky-Vilnai, A.; Ciol, M.; McCoy, S.W. Statistical analysis of clinical prediction rules for rehabilitation interventions: Current state of the literature. Arch. Phys. Med. Rehabil. 2014, 95, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Mills, K.; Hunt, M.A.; Ferber, R. Biomechanical deviations during level walking associated with knee osteoarthritis: A systematic review and meta-analysis. Arthritis Care Res. (Hoboken) 2013, 65, 1643–1665. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Martín, D.; Samà, A.; Pérez-López, C.; Català, A.; Arostegui, J.M.M.; Cabestany, J.; Bayés, À.; Alcaine, S.; Mestre, B.; Prats, A.; et al. Home detection of freezing of gait using Support Vector Machines through a single waist-worn triaxial accelerometer. PLoS ONE 2017, 12, e0171764. [Google Scholar] [CrossRef] [PubMed]
- Benson, L.C.; Clermont, C.A.; Bošnjak, E.; Ferber, R. The use of wearable devices for walking and running gait analysis outside of the lab: A systematic review. Gait Posture 2018, 63, 124–138. [Google Scholar] [CrossRef] [PubMed]
- Mourão-Miranda, J.; Hardoon, D.R.; Hahn, T.; Marquand, A.F.; Williams, S.C.R.; Shawe-Taylor, J.; Brammer, M. Patient classification as an outlier detection problem: An application of the One-Class Support Vector Machine. Neuroimage 2011, 58, 793–804. [Google Scholar] [CrossRef] [PubMed]
- Haladjian, J.; Haug, J.; Nüske, S.; Bruegge, B. A wearable sensor system for lameness detection in dairy cattle. Multimodal Technol. Interact. 2018, 2, 27. [Google Scholar] [CrossRef]
- Cola, G.; Avvenuti, M.; Vecchio, A.; Yang, G.Z.; Lo, B. An on-node processing approach for anomaly detection in gait. IEEE Sens. J. 2015, 15, 6640–6649. [Google Scholar] [CrossRef]
- Mundfrom, D.J.; Shaw, D.G.; Ke, T.L. Minimum Sample Size Recommendations for Conducting Factor Analyses. Int. J. Test. 2005, 5, 159–168. [Google Scholar] [CrossRef]
- Roos, E.M.; Roos, H.P.; Lohmander, L.S.; Ekdahl, C.; Beynnon, B.D. Knee Injury and Osteoarthritis Outcome Score (KOOS)—Development of a self-administered outcome measure. J. Orthop. Sports Phys. Ther. 1998, 28, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Tundo, M.D.; Lemaire, E.; Baddour, N. Correcting Smartphone orientation for accelerometer-based analysis. In Proceedings of the 2013 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Gatineau, QC, Canada, 4–5 May 2013; pp. 58–62. [Google Scholar] [CrossRef]
- Kobsar, D.; Osis, S.T.; Phinyomark, A.; Boyd, J.E.; Ferber, R. Reliability of gait analysis using wearable sensors in patients with knee osteoarthritis. J. Biomech. 2016, 49, 3977–3982. [Google Scholar] [CrossRef] [PubMed]
- Fraccaro, P.; Walsh, L.; Doyle, J.; O’Sullivan, D. Real-world gyroscope-based gait event detection and gait feature extraction. In Proceedings of the eTELEMED—The Sixth International Conference on eHealth, Telemedicine, and Social Medicine, Barcelona, Spain, 24–27 March 2014. [Google Scholar]
- Rampp, A.; Barth, J.; Schuelein, S.; Gassmann, K.-G.; Klucken, J.; Eskofier, B.M. Inertial Sensor-Based Stride Parameter Calculation From Gait Sequences in Geriatric Patients. IEEE Trans. Biomed. Eng. 2015, 62, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
- Deluzio, K.J.; Astephen, J.L. Biomechanical features of gait waveform data associated with knee osteoarthritis: An application of principal component analysis. Gait Posture 2007, 25, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Nigg, B.M.; Baltich, J.; Maurer, C.; Federolf, P. Shoe midsole hardness, sex and age effects on lower extremity kinematics during running. J. Biomech. 2012, 45, 1692–1697. [Google Scholar] [CrossRef] [PubMed]
- Schölkopf, B.; Platt, J.C.; Shawe-Taylor, J.; Smola, A.J.; Williamson, R.C. Estimating the Support of a High-Dimensional Distribution. Neural Comput. 2001, 13, 1443–1471. [Google Scholar] [CrossRef] [PubMed]
- Schölkopf, B.; Williamson, R.; Smola, A.; Shawe-Taylor, J.; Platt, J. Support vector method for novelty detection. In Proceedings of the 12th International Conference on Neural Information Processing Systems (NIPS’99), Cambridge, MA, USA, 29 November–4 December 1999. [Google Scholar]
- Zhang, X.; Gu, C.; Lin, J. Support vector machines for anomaly detection. In Proceedings of the 2006 6th World Congress on Intelligent Control and Automation, Dalian, China, 21–23 June 2006. [Google Scholar]
- Lukashevich, H.; Nowak, S.; Dunker, P. Using one-class SVM outliers detection for verification of collaboratively tagged image training sets. In Proceedings of the 2009 IEEE International Conference on Multimedia and Expo, New York, NY, USA, 28 June–3 July 2009. [Google Scholar]
- Guerbai, Y.; Chibani, Y.; Hadjadji, B. The effective use of the one-class SVM classifier for handwritten signature verification based on writer-independent parameters. Pattern Recognit. 2015, 48, 103–113. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum: New Jersey, NJ, USA, 1988; ISBN 978-0-12-179060-8. [Google Scholar]
- Bokaeian, H.R.; Bakhtiary, A.H.; Mirmohammadkhani, M.; Moghimi, J. Quadriceps strengthening exercises may not change pain and function in knee osteoarthritis. J. Bodyw. Mov. Ther. 2018, 22, 528–533. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, M.; Klokker, L.; Graven-Nielsen, T.; Bartholdy, C.; Schjødt Jørgensen, T.; Bandak, E.; Danneskiold-Samsøe, B.; Christensen, R.; Bliddal, H. Association of exercise therapy and reduction of pain sensitivity in patients with knee osteoarthritis: A randomized controlled trial. Arthritis Care Res. (Hoboken) 2014, 66, 1836–1843. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, M.; Klokker, L.; Bartholdy, C.; Schjoedt-Jorgensen, T.; Bandak, E.; Bliddal, H. No effects of functional exercise therapy on walking biomechanics in patients with knee osteoarthritis: Exploratory outcome analyses from a randomised trial. BMJ Open Sport Exerc. Med. 2017, 2. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.L.; Kyriakides, M.; Metcalf, B.; Egerton, T.; Wrigley, T.V.; Hodges, P.W.; Hunt, M.A.; Roos, E.M.; Forbes, A.; Ageberg, E.; et al. Neuromuscular versus quadriceps strengthening exercise in patients with medial knee osteoarthritis and varus malalignment: A randomized controlled trial. Arthritis Rheumatol. 2014, 66, 950–959. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.L.; Hunt, M.A.; Wrigley, T.V.; Hunter, D.J.; McManus, F.J.; Hodges, P.W.; Li, L.; Hinman, R.S. Hip strengthening reduces symptoms but not knee load in people with medial knee osteoarthritis and varus malalignment: A randomised controlled trial. Osteoarthr. Cartil. 2010, 18, 621–628. [Google Scholar] [CrossRef] [PubMed]
- Sled, E.A.; Khoja, L.; Deluzio, K.J.; Olney, S.J.; Culham, E.G. Effect of a home program of hip abductor exercises on knee joint loading, strength, function, and pain in people with knee osteoarthritis: A clinical trial. Phys. Ther. 2010, 90, 895–904. [Google Scholar] [CrossRef] [PubMed]
- Gaudreault, N.; Mezghani, N.; Turcot, K.; Hagemeister, N.; Boivin, K.; De Guise, J.A. Effects of physiotherapy treatment on knee osteoarthritis gait data using principal component analysis. Clin. Biomech. 2011, 26, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Brenneman, E.C.; Maly, M.R. Identifying changes in gait waveforms following a strengthening intervention for women with knee osteoarthritis using principal components analysis. Gait Posture 2018, 59, 286–291. [Google Scholar] [CrossRef] [PubMed]
- Buford, T.W.; Pahor, M. Making preventive medicine more personalized: Implications for exercise-related research. Prev. Med. 2012, 55, 34–36. [Google Scholar] [CrossRef] [PubMed]
- Karsdal, M.A.; Christiansen, C.; Ladel, C.; Henriksen, K.; Kraus, V.B.; Bay-Jensen, A.C. Osteoarthritis—A case for personalized health care? Osteoarthr. Cartil. 2014, 22, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Phinyomark, A.; Hettinga, B.A.; Osis, S.; Ferber, R. Do intermediate- and higher-order principal components contain useful information to detect subtle changes in lower extremity biomechanics during running? Hum. Mov. Sci. 2015, 44, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Benson, L.C.; Clermont, C.A.; Osis, S.T.; Kobsar, D.; Ferber, R. Classifying running speed conditions using a single wearable sensor: Optimal segmentation and feature extraction methods. J. Biomech. 2018, 71, 94–99. [Google Scholar] [CrossRef] [PubMed]

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kobsar, D.; Ferber, R. Wearable Sensor Data to Track Subject-Specific Movement Patterns Related to Clinical Outcomes Using a Machine Learning Approach. Sensors 2018, 18, 2828. https://doi.org/10.3390/s18092828
Kobsar D, Ferber R. Wearable Sensor Data to Track Subject-Specific Movement Patterns Related to Clinical Outcomes Using a Machine Learning Approach. Sensors. 2018; 18(9):2828. https://doi.org/10.3390/s18092828
Chicago/Turabian StyleKobsar, Dylan, and Reed Ferber. 2018. "Wearable Sensor Data to Track Subject-Specific Movement Patterns Related to Clinical Outcomes Using a Machine Learning Approach" Sensors 18, no. 9: 2828. https://doi.org/10.3390/s18092828
APA StyleKobsar, D., & Ferber, R. (2018). Wearable Sensor Data to Track Subject-Specific Movement Patterns Related to Clinical Outcomes Using a Machine Learning Approach. Sensors, 18(9), 2828. https://doi.org/10.3390/s18092828





