Defining Requirements and Related Methods for Designing Sensorized Garments
Abstract
:1. Introduction
2. Materials and Methods
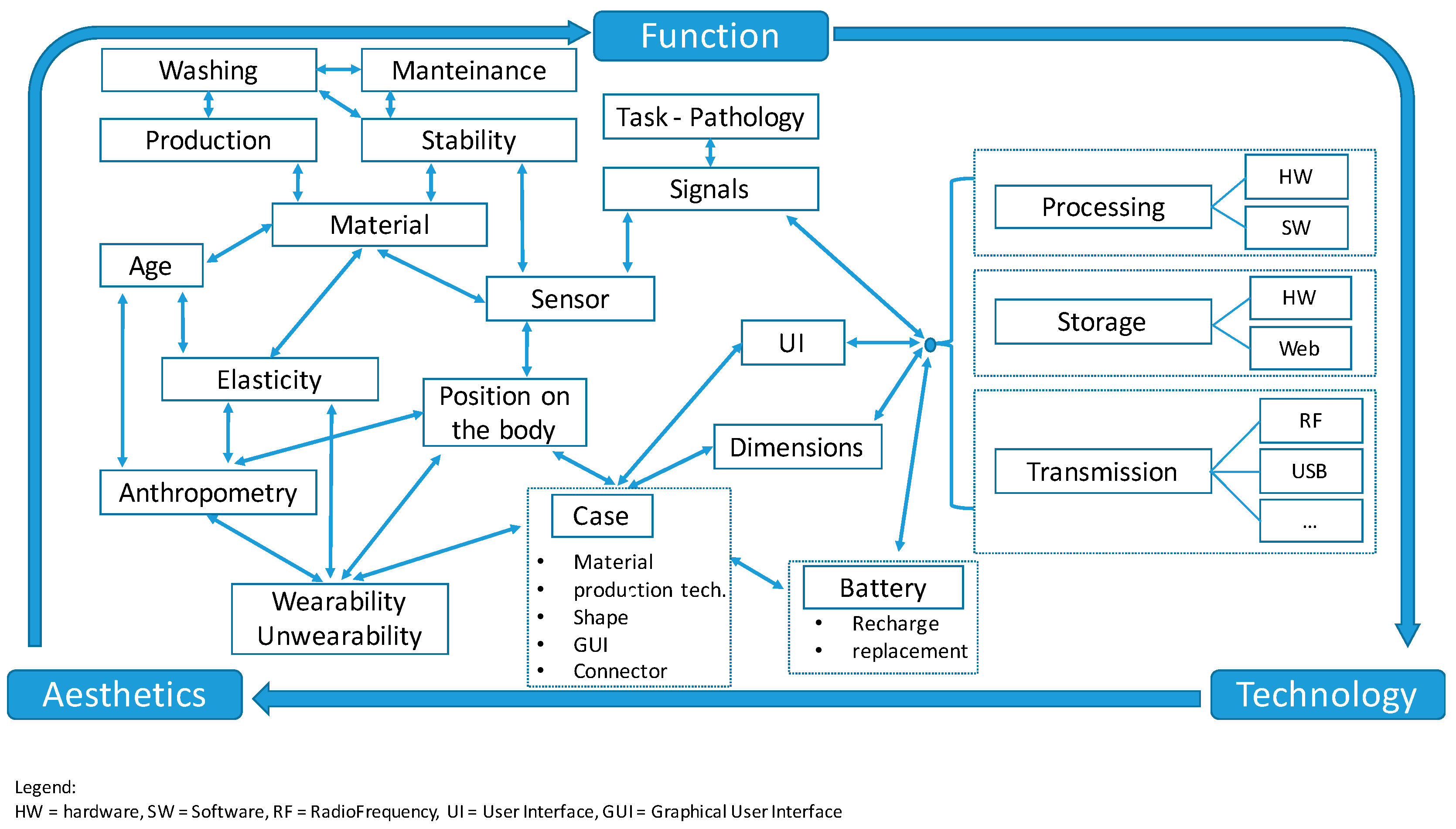
2.1. Technological Specifications of Wearable Systems
- bioelectric signals, such as Electro-Cardio-Gram (ECG), Electro-Myo-Gram (EMG), Electro-Encephalo-Gram (EEG), Electro-Oculo-Gram (EOG), Electro-Neuro-Gram (ENG), and others;
- thermal parameters, such as body temperature in specific points and its map on a specific portion of the body surface;
- mechanical measurements, such as the kinematics of body segments and the pressure at the human/object interface (e.g., the human back and a mattress);
- optical signals, such as the SpO2 assessment and other NIRS measurements;
- chemical analyses, such as the determination of the composition of the sweat and that of the inhaled/exhaled air.
- (a)
- metal yarns, i.e., yarns containing conductive fibers such as stainless steel, copper, and silver mixed with natural or synthetic fibers;
- (b)
- yarns containing electro-conductive fibers such as polymeric or carbon-coated threads.
2.2. Design Specifications of Wearable Systems
3. Discussion
- -
- human parameters to be monitored and related signals for the application or pathology, identifying the main signal and computed parameters;
- -
- typology and numbers of sensors required for the monitoring;
- -
- a monitoring paradigm—continuous signal transmission or delayed data transfer;
- -
- real-time data processing and analysis or off-line operations, secondary parameter computation and storage on-board or remote solutions;
- -
- direct patient participation or other caregivers operations, and, indirectly but obviously, who the subjects to be monitored are and their features (age, sex, body build, etc.), which are also pieces of information very relevant for aesthetical specifications. Secondary function requirements are related to the production and maintenance of the sensors and the devices.
- -
- integration of textile wiring through conductive yarns connecting the sensor to the measuring device;
- -
- sweat and thermal management to assure a good quality and then garment acceptance to the users;
- -
- specific requirements for washing, ironing, and sterilization or disinfection should be considered if applicable in special applications (e.g., monitoring in an Intensive Care Unit or in the case of the presence of exposed or open wounds).
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ECG | Electro-Cardio-Gram |
| EEG | Electro-Encephalo-Gram |
| EMG | Electro-Myo-Gram |
| ENG | Electro-Neuro-Gram |
| EOG | Electro-Oculo-Gram |
| GUI | Graphical User Interface |
| IMU | Inertial Movement Unit |
| NIRS | Near Infra-Red Spectroscopy |
| PCB | Printed Circuit Board |
| PHS | Personal Health Systems |
| POF | Plastic Optical Fiber |
| SpO2 | Peripheral Capillary Oxygen Saturation |
| UI | User Interface |
| WBS | Wearable Biomedical Systems |
| WHS | Wearable Health Systems |
References
- Bughin, L.; Chui, M.; Manyika, J. Ten IT-Enabled Business Trends for the Decade Ahead, McKinsey Quarterly, May 2013. Available online: http://www.mckinsey.com/industries/high-tech/our-insights/ten-it-enabled-business-trends-for-the-decade-ahead (accessed on 26 April 2016).
- Harrop, P.; Hayward, J.; Das, R.; Holland, G. Wearable Technology 2015–2025: Technologies, Markets, Forecasts E-Textiles, Wearable Electronics, Medical Diagnostics/Telemedicine, Smart Glasses, Smart Wristbands and More. Available online: http://www.idtechex.com/research/reports/wearable-technology-2015-2025-technologies-markets-forecasts-000427.asp (accessed on 26 April 2016).
- Facts and Statistics on Wearable Technology. Available online: http://www.statista.com/topics/1556/wearable-technology/ (accessed on 26 April 2016).
- Lymberis, A.; Gatzoulis, L. Wearable Health Systems: From smart technologies to real applications. In Proceedings of the 28th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, New York City, NY, USA, 31 August–3 September 2006; pp. 6789–6792.
- Fashioning Health & Wellness: An Interview with Misfit Wearables. Available online: http://fashioningtech.com/profiles/blogs/fashioning-health-wellness-an-interview-with-misfit-wearables (accessed on 26 April 2016).
- De Rossi, D.; Lymberis, A. New generation of smart wearable health systems and applications. IEEE Trans. Inf. Technol. Biomed. 2005, 9, 293–294. [Google Scholar] [CrossRef] [PubMed]
- Andreoni, G.; Bernabei, M.; Perego, P.; Barichello, A.; Piccini, L. Example of Clinical Applications of Wearable Monitoring System. Int. J. Comput. Res. 2011, 18, 323–339. [Google Scholar]
- Piccini, L.; Ciani, O.; Andreoni, G. New emerging biomedical technologies for home-care and telemedicine applications: The Sensorwear project. In New Developments in Biomedical Engineering; Campolo, D., Ed.; In-Tech: Rijeka, Croatia, 2010; Chapter 34; pp. 675–684. [Google Scholar]
- Cho, G. Smart Clothing: Technology and Applications; CRC Press: Boca Raton, FL, USA, 2009. [Google Scholar]
- Muschiato, S.; Romero, M.; Perego, P.; Costa, F.; Andreoni, G. Designing Wearable and Environmental Systems for Elderly Monitoring at Home. In Advances in Social and Organizational Factors; Vink, P., Ed.; CRC Press: Boca Raton, FL, USA, 2012; Chapter 48; pp. 463–469. [Google Scholar]
- Bernabei, M.; Preatoni, E.; Mendez, M.; Piccini, L.; Porta, M.; Andreoni, G. A Novel Automatic Method for Monitoring Tourette Motor Tics through a Wearable Device. Mov. Disord. 2010, 25, 1967–1972. [Google Scholar] [CrossRef] [PubMed]
- Perego, P.; Moltani, A.; Andreoni, G. Sport monitoring with Smart Wearable System. In Studies in Health Technology and Informatics, Proceedings of the 9th International Conference on Wearable Micro and Nano Technologies for Personalized Health, pHealth 2012, Porto, Portugal, 26–28 June 2012; Blobel, B., Pharow, P., Sousa, F., Eds.; IOS Press: Washington, DC, USA, 2012; pp. 224–228. [Google Scholar]
- Perego, P.; Moltani, A.; Fusca, M.; Andreoni, G. Wearable monitoring systems in pre-term newborns care. In Studies in Health Technology and Informatics, Proceedings of the 9th International Conference on Wearable Micro and Nano Technologies for Personalized Health, pHealth 2012, Porto, Portugal, 26–28 June 2012; Blobel, B., Pharow, P., Sousa, F., Eds.; IOS Press: Washington, DC, USA, 2012; pp. 203–209. [Google Scholar]
- Fanelli, A.; Signorini, M.G.; Perego, P.; Magenes, G.; Andreoni, G. A smart wearable prototype for fetal monitoring. In Proceedings of the 4th International Conference on Applied Human Factors and Ergonomics (AHFE), San Francisco, CA, USA, 21–25 July 2012.
- Andre, D.; Teller, A. Studies in Health Technology and Informatics. Health Care Anywhere Today 2005, 118, 89–110. [Google Scholar]
- Webster, J.G. (Ed.) Medical Instrumentation Application and Design, 4th ed.; John Wiley & Sons: New York City, NY, USA, 2006.
- De Rossi, D.; Lymberis, A. (Eds.) Wearable eHealth Systems for Personalised Health Management; IOS Press: Amsterdam, The Netherlands, 2004.
- Van Langenhove, L. (Ed.) Smart Textiles for Medicine and Healthcare: Materials, Systems and Applications; CRC Press: Boca Raton, FL, USA, 2007.
- Stoppa, M.; Chiolerio, A. Review Wearable Electronics and Smart Textiles: A Critical Review. Sensors 2014, 14, 11957–11992. [Google Scholar] [CrossRef] [PubMed]
- Saenz-Cogollo, J.F.; Pau, M.; Fraboni, B.; Bonfiglio, A. Pressure Mapping Mat for Tele-Home Care Applications. Sensors 2016, 16, 365. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Hwang, S.H.; Yoon, H.N.; Lee, W.K.; Park, K.S. Heart Rate Variability Monitoring during Sleep Based on Capacitively Coupled Textile Electrodes on a Bed. Sensors 2015, 15, 11295–11311. [Google Scholar] [CrossRef] [PubMed]
- Moltani, L.A.L.; Andreoni, G. Sensor for Measurement of Physiological Electrical Signals. Eur. Patent WO2016009251, 15 July 2014. [Google Scholar]
- Meziane, N.; Webster, J.G.; Attari, M.; Nimunkar, A.J. Dry electrodes for electrocardiography. Physiol. Meas. 2013, 34, R47–R69. [Google Scholar] [CrossRef] [PubMed]
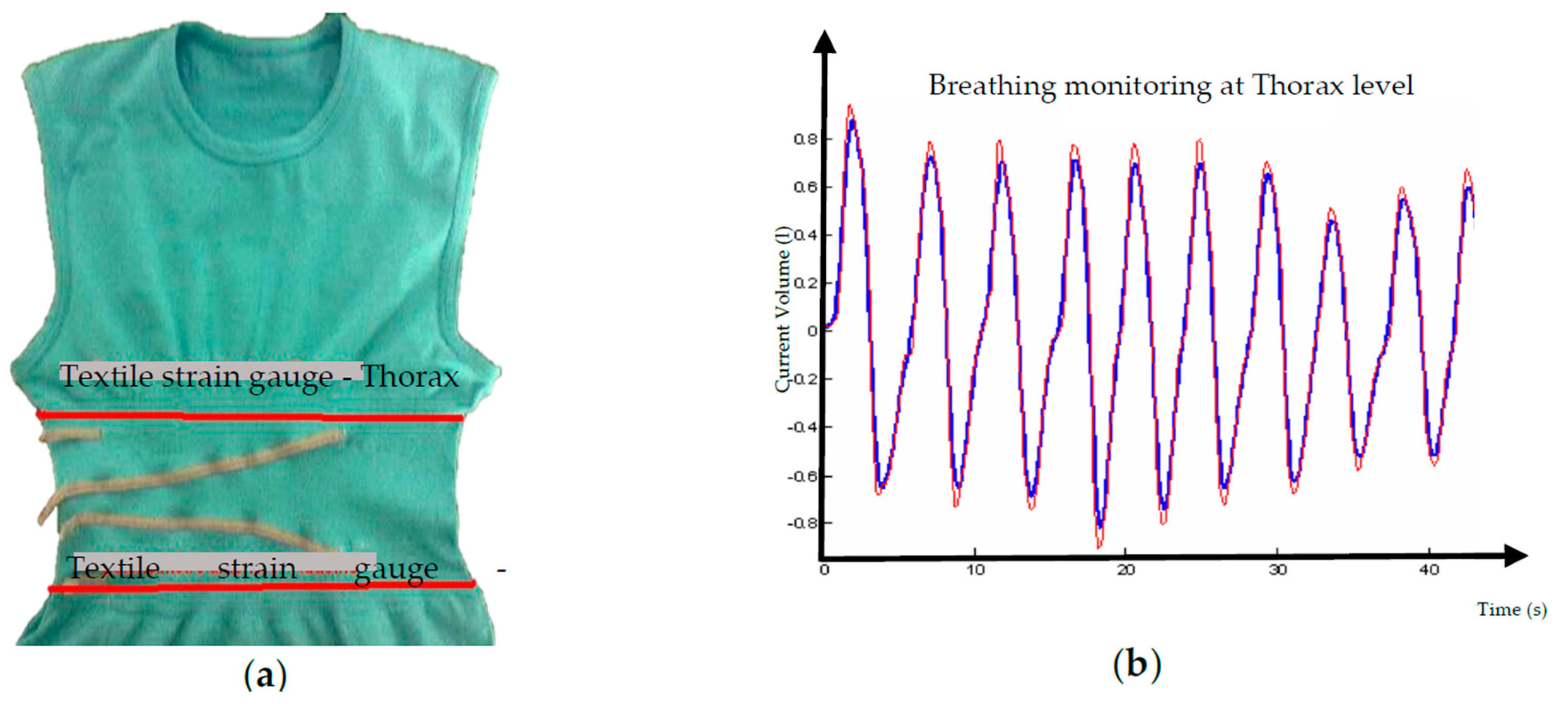
- Andreoni, G.; Fanelli, A.; Witkowska, I.; Perego, P.; Fusca, M.; Mazzola, M.; Signorini, M.G. Sensor validation for wearable monitoring system in ambulatory monitoring: Application to textile electrodes. In Proceedings of the 7th International Conference on Pervasive Computing Technologies for Healthcare, Venice, Italy, 5–8 May 2013; pp. 169–175.
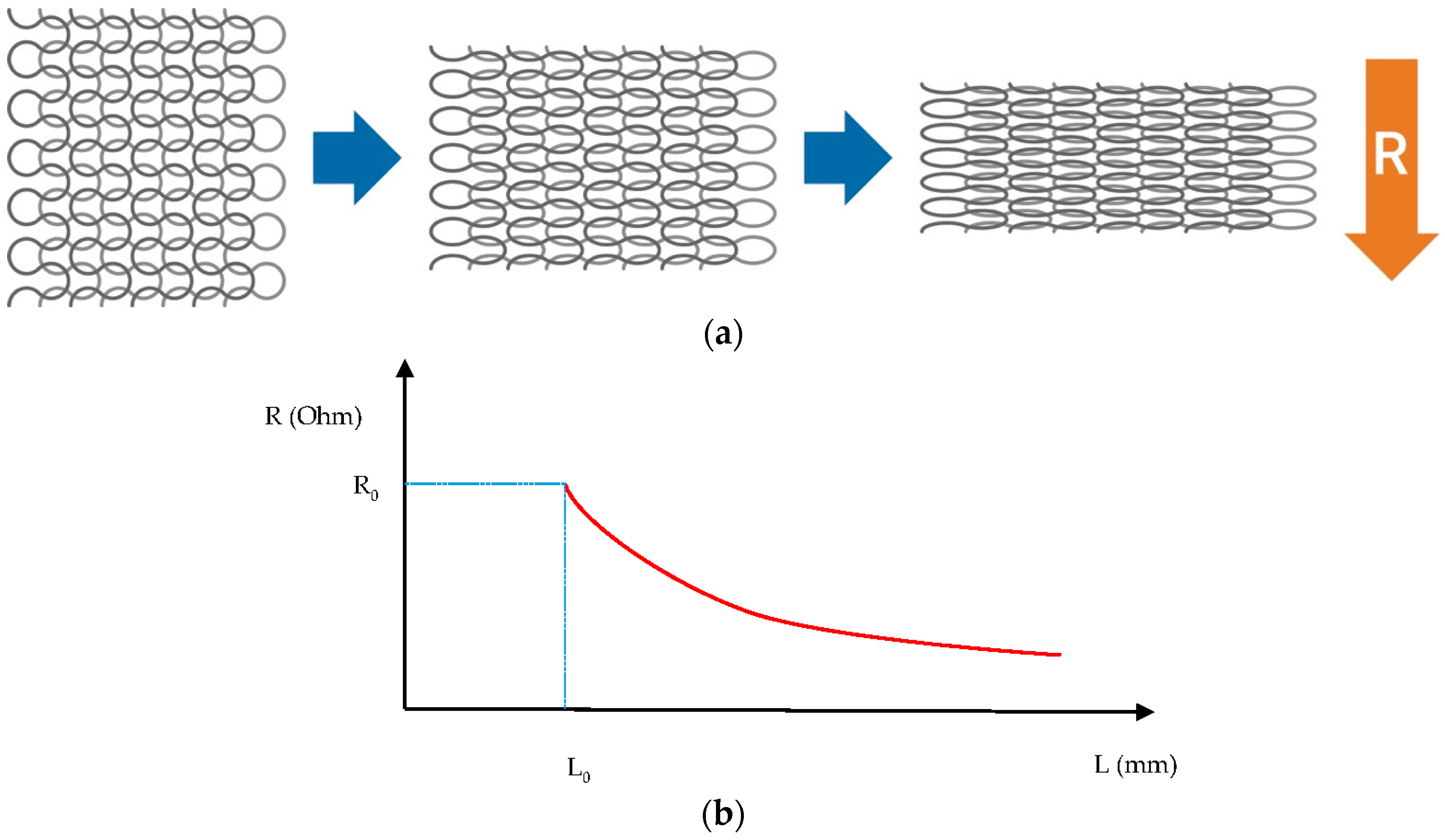
- Perego, P.; Andreoni, G.; Tarabini, M. Textile Performance Assessment for Smart T-Shirt Development, Mechanical and electrical study for conductive yarn. In Proceedings of the eTELEMED 2016: The Eighth International Conference on eHealth, Telemedicine, and Social Medicine (with DIGITAL HEALTHY LIVING 2016/MATH 2016), Venice, Italy, 24–28 April 2016; pp. 263–268.
- Andreoni, G. Il Fattore Uomo nel Design; Aracne Editrice: Roma, Italy, 2012. (In Italian) [Google Scholar]
- Gemperle, F.; Kasabach, C.; Stivoric, J.; Bauer, M.; Martin, R. Design for Wearability. In Proceedings of the 2nd IEEE International Symposium on Wearable Computers, ISWC ’98, Washington, DC, USA, 19–20 October 1998.
- Standoli, C.; Perego, P.; Mazzola, M.; Mazzola, A.; Guarneri, R.; Andreoni, G. PEGASO: A smart wearable sensors’ system for counter-fighting overweight in teenagers. In Proceedings of the 2nd International Electronic Conference on Sensors and Applications, 15–30 November 2015. [CrossRef]
- Andreoni, G. Sistemi di sensori indossabili per il monitoraggio: Dalla Ricerca al Mercato. In Sistemi Indossabili Intelligenti per la Salute e la Protezione dell’Uomo; Bonfiglio, A., Cerutti, S., De Rossi, D., Magenes, G., Eds.; Patron: Bologna, Italy, 2008; pp. 357–384. (In Italian) [Google Scholar]



| No. | Signal 1 | Parameter (s) | Sensor | Typology |
|---|---|---|---|---|
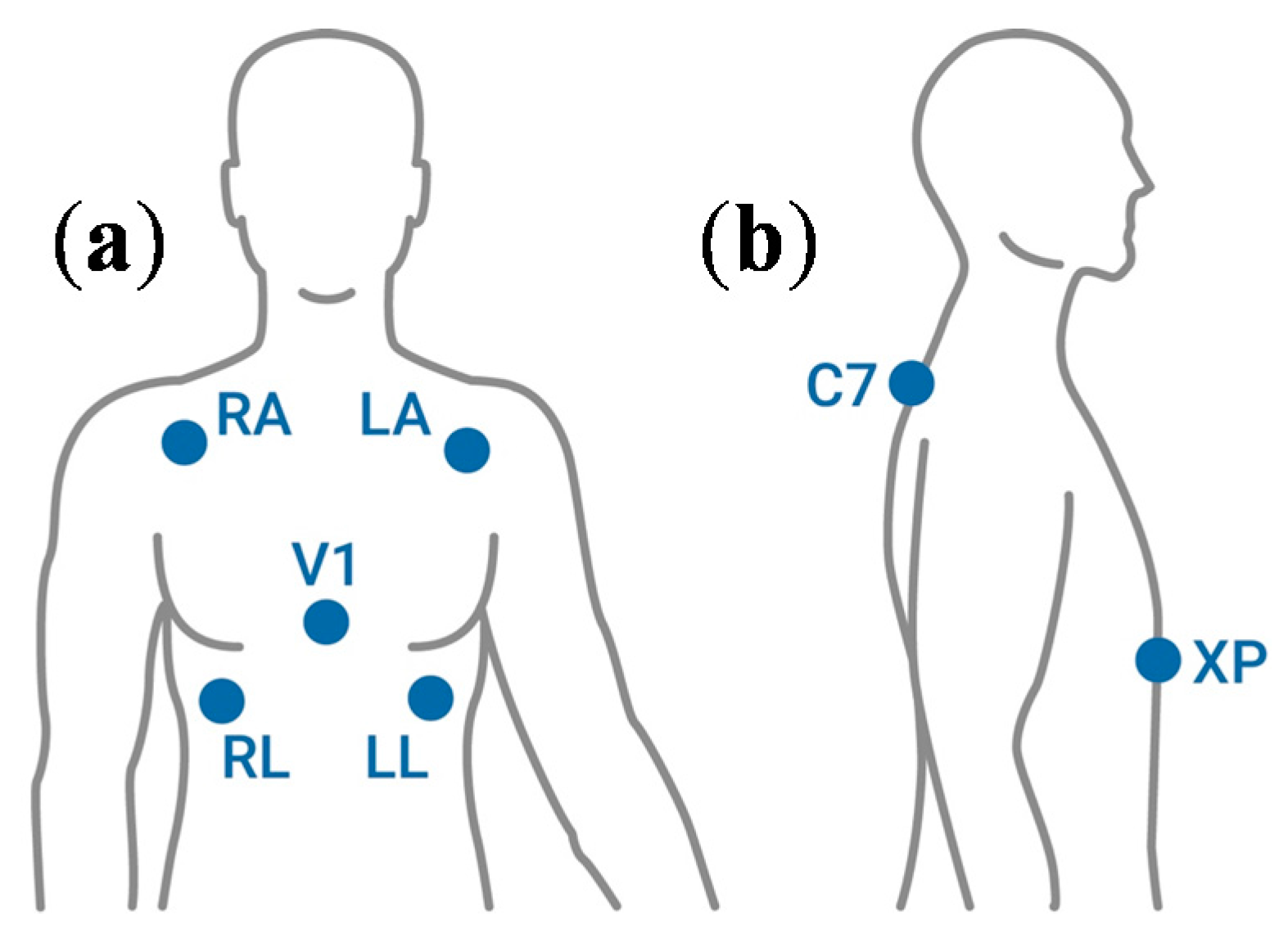
| 1 | ECG | Electrical heart activity, Heart Rate | electrode | Adhesive, textile, plate |
| 2 | EEG | Electrical Brain activity | electrode | Plate, textile prototypes |
| 3 | EMG | Electrical muscle activity | electrode | Adhesive, textile prototypes |
| 4 | Respiration | Breathing rate, Volumes, respiratory times | Strain gauge; Electrode for impedance measure | Hardware probe, adhesive, textile sensor |
| 5 | Blood gas | SpO2, CO2, Heart rate | LED/optical | Hardware probe, POF for signal transmission |
| 6 | Blood pressure | Systolic/diastolic values, Heart rate | Cuff | Hardware System |
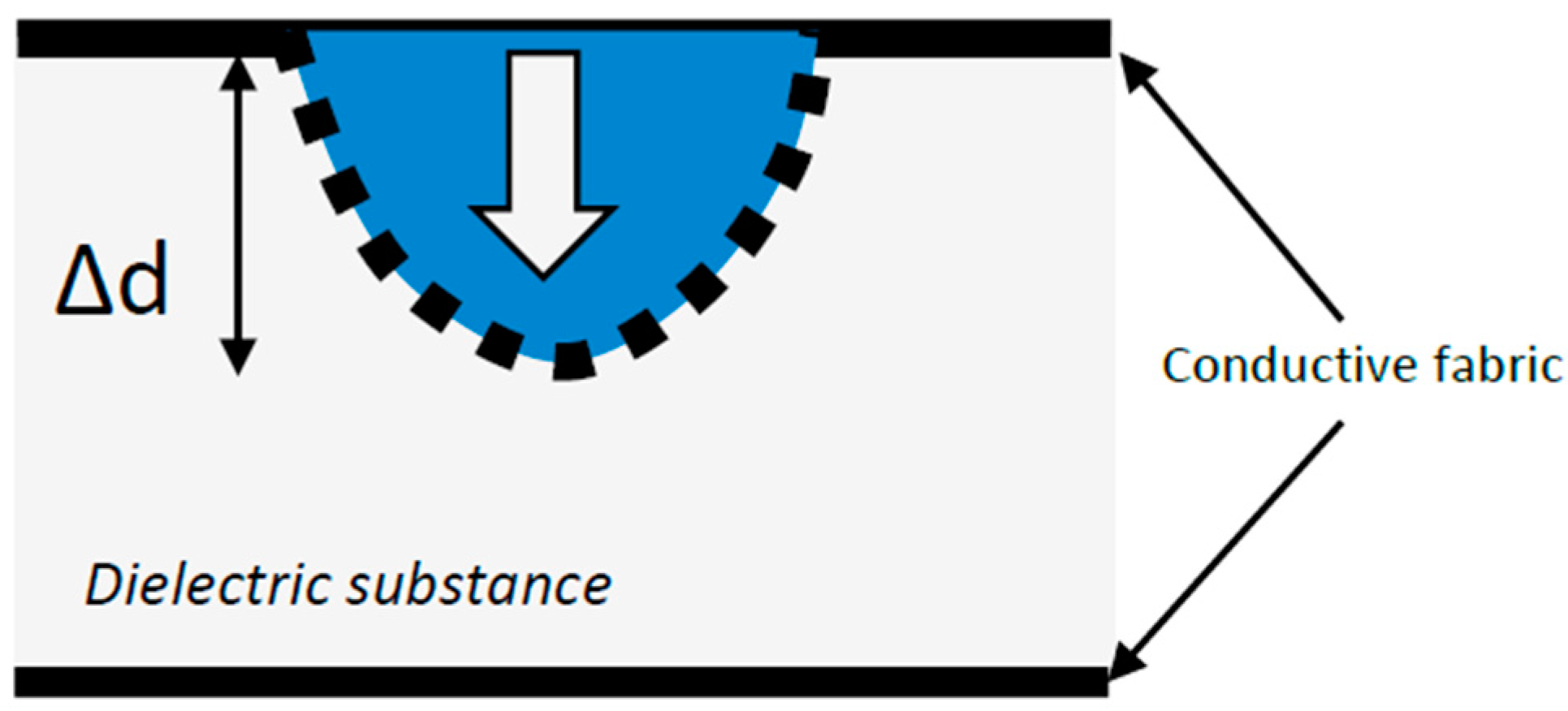
| 7 | Interface pressure | Contact pressure | Piezoresistive; capacitive | Piezoresistive ink, capacitive sensor both electric and textile |
| 8 | Resistance | GSR, Body impedance | Electrodes for Impedance measure | Hardware System |
| 9 | Temperature | Temperature | Piezoresistive | Hardware probe (thermistor) |
| Material | Merits | Demerits |
|---|---|---|
| Conductive rubber | High conductivity, easy to shape, cheap | Poor flexibility and permeability to air and liquid |
| Silver-coated polymer foam | High conductivity, easy to shape, flexible, antibacterial | Poor washability and permeability to air and liquid, possible oxidation |
| Metal-coated or sputtered fabric | High conductivity, fabric material | Poor washability, possible oxidation |
| Woven metal fabric | Controlled conductivity, fabric material | Difficult to handle, skin irritation, low elasticity |
| Woven conductive polymer fabric | Fabric material, elasticity | Low conductivity |
| Carbon yarn | High mechanical resistance, high thermal insulation | Average conductivity, skin irritation, low elasticity |
| Stainless steel yarn | High conductivity, no skin interaction | Low elasticity, high weight |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andreoni, G.; Standoli, C.E.; Perego, P. Defining Requirements and Related Methods for Designing Sensorized Garments. Sensors 2016, 16, 769. https://doi.org/10.3390/s16060769
Andreoni G, Standoli CE, Perego P. Defining Requirements and Related Methods for Designing Sensorized Garments. Sensors. 2016; 16(6):769. https://doi.org/10.3390/s16060769
Chicago/Turabian StyleAndreoni, Giuseppe, Carlo Emilio Standoli, and Paolo Perego. 2016. "Defining Requirements and Related Methods for Designing Sensorized Garments" Sensors 16, no. 6: 769. https://doi.org/10.3390/s16060769
APA StyleAndreoni, G., Standoli, C. E., & Perego, P. (2016). Defining Requirements and Related Methods for Designing Sensorized Garments. Sensors, 16(6), 769. https://doi.org/10.3390/s16060769








