Hydrophobic Drug Delivery Platforms Based on Covalent Organic Frameworks for Combined Treatment of Alzheimer’s Disease
Abstract
1. Introduction
2. Results
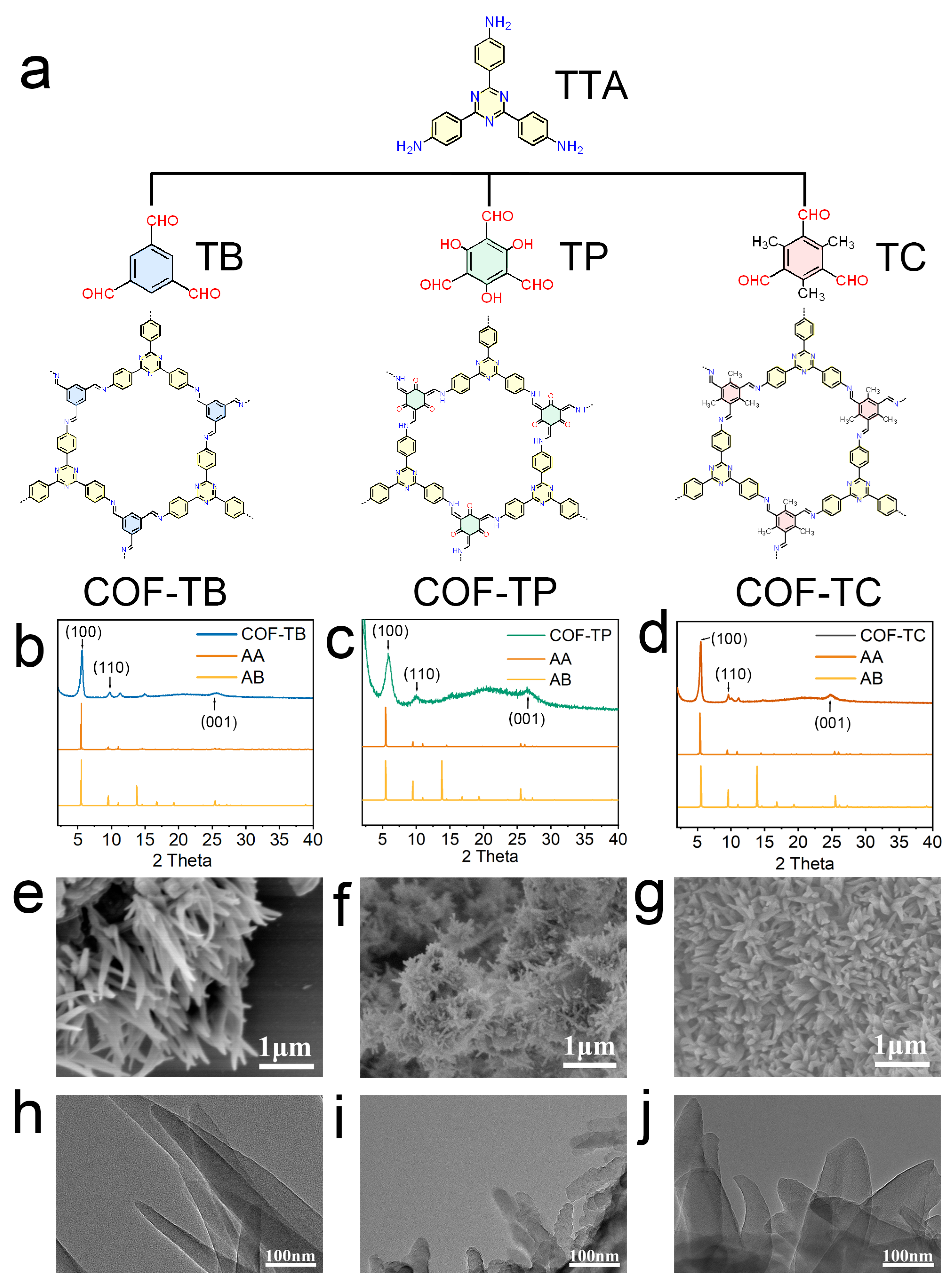
2.1. Synthesis and Characterization of COFs
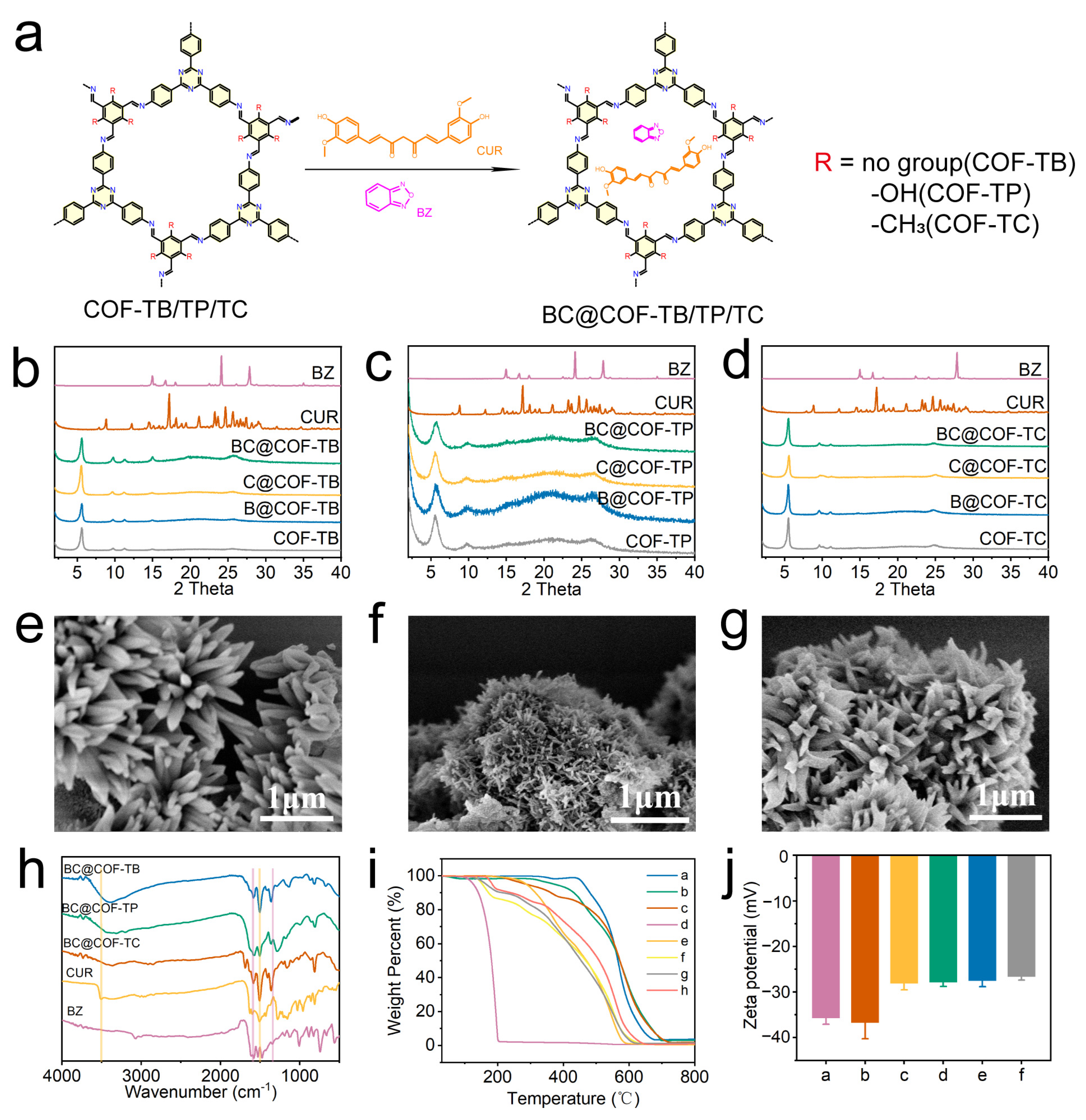
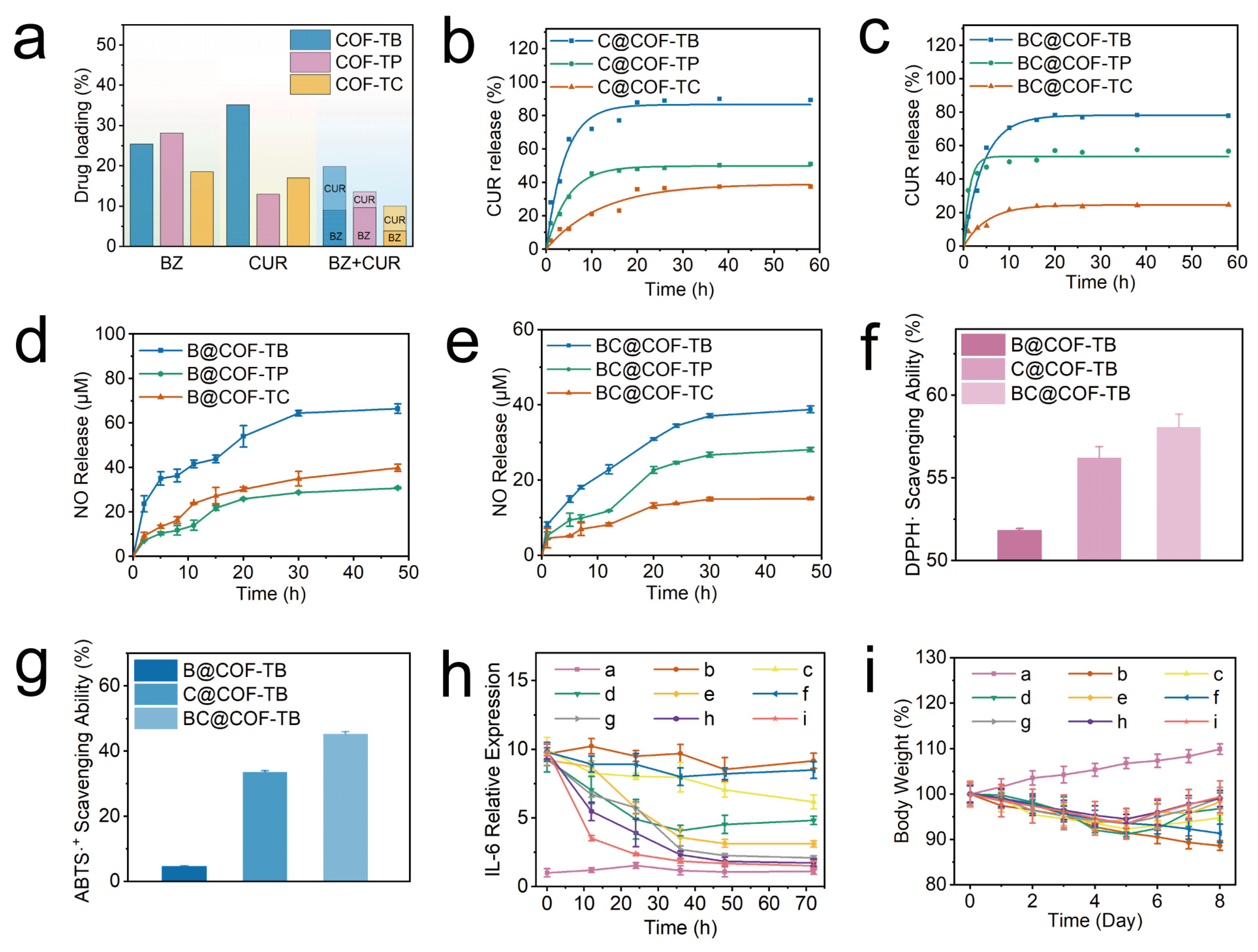
2.2. Drug Loading Capacity of COFs
2.3. Loading and Release of BZ and CUR from COFs
2.4. Antioxidant Properties of B@COF-TB, C@COF-TB, and BC@COF-TB
2.5. In Vivo Properties of B@COF-TB, C@COF-TB and BC@COF-TB
2.5.1. Anti-Inflammatory Effects of B@COF-TB, C@COF-TB, and BC@COF-TB
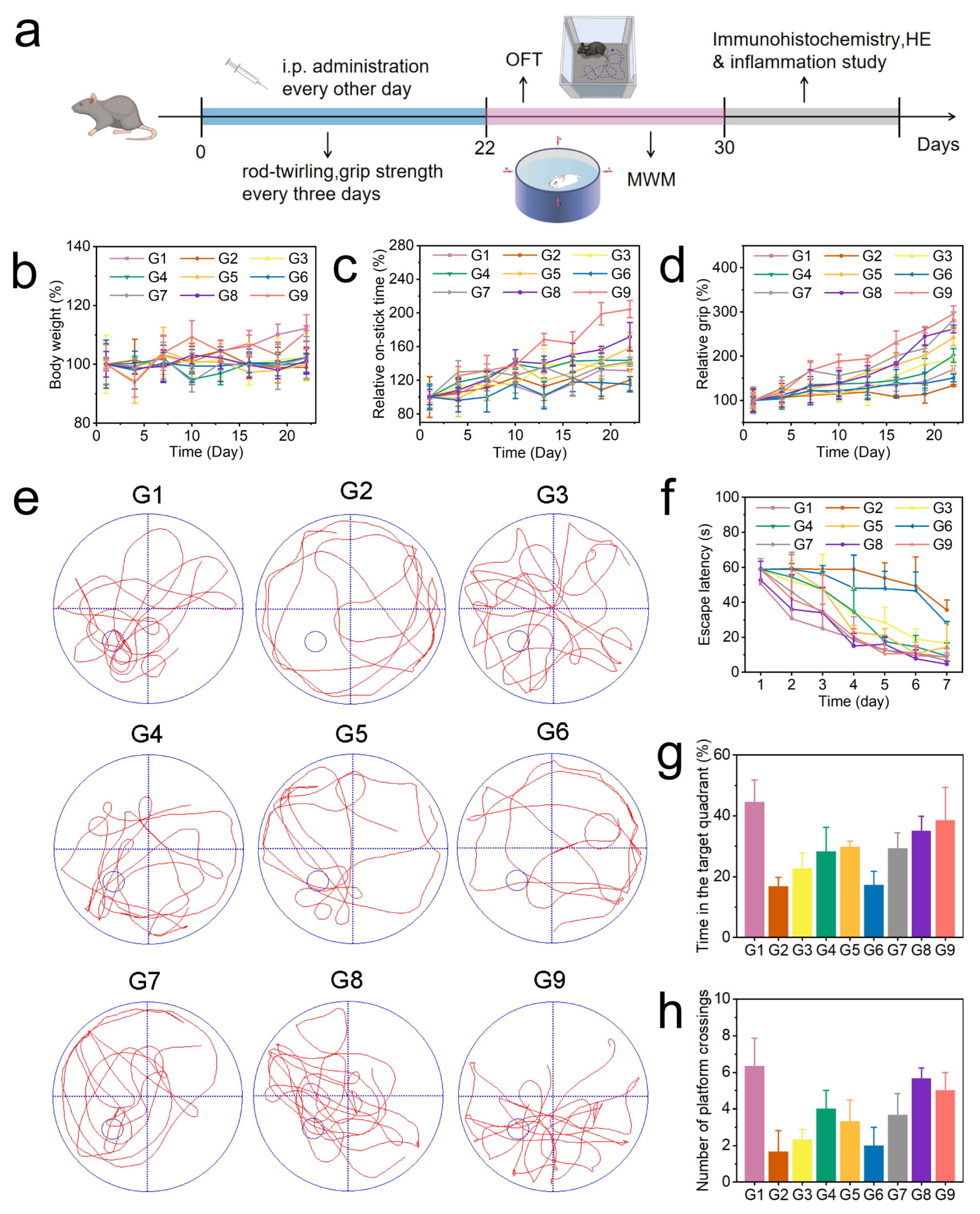
2.5.2. Therapeutic Effect of BC@COF-TB on AD Mice
2.6. BC@COF-TB Allaeviates Inflammatory Injury and Aβ Deposition in AD Mice
3. Discussion
4. Materials and Methods
4.1. Materials, Measurements and Characterization
4.2. Synthesis of COFs
4.3. Drug Loading into COFs
4.4. Detection of Nitric Oxide
4.5. Detection of CUR
4.6. Determination of Drug Loading
4.6.1. Determination of BZ Loading in B@COF-TB, B@COF-TP, B@COF-TC, BC@COF-TB, BC@COF-TP, BC@COF-TC
4.6.2. Determination of CUR Loading in C@COF-TB, C@COF-TP, C@COF-TC, BC@COF-TB, BC@COF-TP, BC@COF-TC
4.7. Study on Drug Release In Vitro
4.8. Antioxidant Activity Test
- A = sample group solution absorbance.
- A0 = blank group solution absorbance.
- A = sample group solution absorbance.
- A0 = blank group solution absorbance.
4.9. LPS-Induced Inflammation Model Anti-Inflammatory Experiments
4.10. Hemolysis Experiment
4.11. Animal Experiment
4.11.1. Grouping Situation
4.11.2. Behavioral Tests
4.12. Western Blotting Analysis
4.13. Immunohistochemistry
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AD | Alzheimer’s disease |
| COFs | covalent organic frameworks |
| CUR | curcumin |
| BZ | benzofuroxan |
| TTA | Disperse 4,4′,4″-(1,3,5-Triazine-2,4,6-triyl) trianiline |
| TB | benzene-1,3,5-tricarboxaldehyde |
| TP | 2,4,6-triformylphloroglucinol |
| TC | 2,4,6-trimethylbenzene-1,3,5-tricarbaldehyde |
| TGA | thermogravimetric analysis |
| IL-6 | interleukin-6 |
| LPS | lipopolysaccharide |
| ELISA | enzyme-linked immunosorbent assay |
| TNF-α | tumor necrosis factor-α |
| AChE | acetylcholinesterase |
References
- Marasco, R.A. Current and evolving treatment strategies for the Alzheimer disease continuum. Am. J. Manag. Care 2020, 26, S167–S176. [Google Scholar] [CrossRef]
- Ren, Q.; Chen, H.; Chen, Y.; Song, Z.; Ouyang, S.; Lian, S.; Tao, J.; Song, Y.; Zhao, P. Imine-Linked Covalent Organic Framework Modulates Oxidative Stress in Alzheimer’s Disease. ACS Appl. Mater. Interfaces 2023, 15, 4947–4958. [Google Scholar] [CrossRef]
- Wimo, A.; Seeher, K.; Cataldi, R.; Cyhlarova, E.; Dielemann, J.L.; Frisell, O.; Guerchet, M.; Jonsson, L.; Malaha, A.K.; Nichols, E.; et al. The worldwide costs of dementia in 2019. Alzheimers Dement. 2023, 19, 2865–2873. [Google Scholar] [CrossRef]
- Lauretti, E.; Dincer, O.; Pratico, D. Glycogen synthase kinase-3 signaling in Alzheimer’s disease. Biochim. Biophys. Acta-Mol. Cell Res. 2020, 1867, 118664. [Google Scholar] [CrossRef]
- Prados, M.J.; Liu, Y.; Jun, H.; Lam, J.; Mattke, S. Projecting the long-term societal value of a disease-modifying treatment for Alzheimer’s disease in the United States. Alzheimers Dement. 2022, 18, 142–151. [Google Scholar] [CrossRef]
- Wang, Y.C.; Kung, W.M.; Chung, Y.H.; Kumar, S. Drugs to Treat Neuroinflammation in Neurodegenerative Disorders. Curr. Med. Chem. 2024, 31, 1818–1829. [Google Scholar] [CrossRef]
- Reitz, C.; Brayne, C.; Mayeux, R. Epidemiology of Alzheimer disease. Nat. Rev. Neurol. 2011, 7, 137–152. [Google Scholar] [CrossRef] [PubMed]
- Zheng, D.S.; Zhuo, B.T.; Zheng, G.Z.Y.; Hua, J.J.; Zhang, J.G.; Wang, C.J.; Wang, Y.H.; Zhang, Z.L.; Lin, H.L. The associations of energy adjusted dietary inflammatory index with brain structure and cognitive function. Innov. Med. 2023, 1, 100036. [Google Scholar] [CrossRef]
- Xu, H.Y.; Feng, G.S.; Li, R.; Gao, P.; Qiao, J. ADpred: A non-invasive model for three types of dementia and mild cognitive impairment. Innov. Med. 2023, 1, 100026. [Google Scholar] [CrossRef]
- Lin, R.R.; Huang, H.F.; Tao, Q.Q. Advancing the battle against Alzheimer’s Disease: A focus ontargeting tau pathology by antisense oligonucleotide. Innov. Med. 2023, 1, 100020. [Google Scholar] [CrossRef]
- Bai, R.; Guo, J.; Ye, X.Y.; Xie, Y.; Xie, T. Oxidative stress: The core pathogenesis and mechanism of Alzheimer’s disease. Ageing Res. Rev. 2022, 77, 101619. [Google Scholar] [CrossRef] [PubMed]
- Butterfield, J.T.; Kim, H.; Knauer, D.J.; Nevala, W.K.; Markovic, S.N. Identification of a peptide-peptide binding motif in the coating of nab-paclitaxel nanoparticles with clinical antibodies: Bevacizumab, rituximab, and trastuzumab. Sci. Rep. 2017, 7, 14476. [Google Scholar] [CrossRef] [PubMed]
- El-Samaligy, M.S.; Rohdewald, P. Reconstituted collagen nanoparticles, a novel drug carrier delivery system. J. Pharm. Pharmacol. 1983, 35, 537–539. [Google Scholar] [CrossRef] [PubMed]
- Engelberth, S.A.; Hempel, N.; Bergkvist, M. Development of nanoscale approaches for ovarian cancer therapeutics and diagnostics. Crit. Rev. Oncog. 2014, 19, 281–315. [Google Scholar] [CrossRef]
- Liu, Z.; Fan, A.C.; Rakhra, K.; Sherlock, S.; Goodwin, A.; Chen, X.; Yang, Q.; Felsher, D.W.; Dai, H. Supramolecular Stacking of Doxorubicin on Carbon Nanotubes for In Vivo Cancer Therapy. Angew. Chem.-Int. Edit. 2009, 48, 7668–7672. [Google Scholar] [CrossRef]
- Vidal, F.; Guzman, L. Dendrimer nanocarriers drug action: Perspective for neuronal pharmacology. Neural Regen. Res. 2015, 10, 1029–1031. [Google Scholar] [CrossRef]
- You, J.; Zhang, G.; Li, C. Exceptionally High Payload of Doxorubicin in Hollow Gold Nanospheres for Near-Infrared Light-Triggered Drug Release. ACS Nano 2010, 4, 1033–1041. [Google Scholar] [CrossRef]
- Li, X.M.; Wu, Z.Z.; Zhang, B.; Pan, Y.; Meng, R.; Chen, H.Q. Fabrication of chitosan hydrochloride and carboxymethyl starch complex nanogels as potential delivery vehicles for curcumin. Food Chem. 2019, 293, 197–203. [Google Scholar] [CrossRef]
- Tan, C.; Xie, J.; Zhang, X.; Cai, J.; Xia, S. Polysaccharide-based nanoparticles by chitosan and gum arabic polyelectrolyte complexation as carriers for curcumin. Food Hydrocoll. 2016, 57, 236–245. [Google Scholar] [CrossRef]
- Meng, T.; Wang, X.Y.; Jiang, S.S.; Chen, S.R.; Zhou, S.N.; Zhu, Y.H.; Wu, J.; Hu, D.Y.; Yan, Y.W.; Zhang, G.Y. Delivery of Small-Molecule Drugs and Protein Drugs by Injectable Acid-Responsive Self-Assembled COF Hydrogels for Combinatorial Lung Cancer Treatment. ACS Appl. Mater. Interfaces 2023, 15, 42354–42368. [Google Scholar] [CrossRef]
- Asadi, P.; Mokhtari, N.; Asghari, S.; Rha, H.; Khodarahmi, G.; Jalali, H.; Amit Sharma, A.; Dinari, M.; Kim, S.J. Advanced Postsynthetic Modification of COF: Elevating Hydrophilicity for Efficient Doxorubicin Delivery. ACS Appl. Bio Mater. 2025, 8, 4325–4336. [Google Scholar] [CrossRef]
- Vyas, V.S.; Vishwakarma, M.; Moudrakovski, I.; Haase, F.; Savasci, G.; Ochsenfeld, C.; Spatz, J.P.; Lotsch, B.V. Exploiting Noncovalent Interactions in an Imine-Based Covalent Organic Framework for Quercetin Delivery. Adv. Mater. 2016, 28, 8749–8754. [Google Scholar] [CrossRef] [PubMed]
- Lei, G.; Qiao, C.Y.; Tang, Y.K.; Zhang, X.K.; Jiang, X.Q. Light-Activated Hypoxia-Sensitive Covalent Organic Framework for Tandem-Responsive Drug Delivery. Nano Lett. 2021, 21, 3218–3224. [Google Scholar] [CrossRef]
- Zhang, G.; Li, X.; Liao, Q.; Liu, Y.F.; Xi, K.; Huang, W.Y.; Jia, X.D. Water-dispersible PEG-curcumin/amine-functionalized covalent organic framework nanocomposites as smart carriers for in vivo drug delivery. Nat. Commun. 2018, 9, 2785. [Google Scholar] [CrossRef] [PubMed]
- Scicluna, M.C.; Vella-Zarb, L. Evolution of Nanocarrier Drug-Delivery Systems and Recent Advancements in Covalent Organic Framework–Drug Systems. ACS Appl. Nano Mater. 2020, 3, 3097–3115. [Google Scholar] [CrossRef]
- Guo, H.; Liu, Y.; Wu, N.; Sun, L.; Yang, W. Covalent Organic Frameworks (COFs): A Necessary Choice For Drug Delivery. ChemistrySelect 2022, 7, e202202538. [Google Scholar] [CrossRef]
- Gao, Q.; Bai, L.; Zhang, X.; Wang, P.; Li, P.; Zeng, Y.; Zou, R.; Zhao, Y. Synthesis of Microporous Nitrogen-Rich Covalent-Organic Framework and Its Application in CO2 Capture. Chin. J. Chem. 2014, 33, 90–94. [Google Scholar] [CrossRef]
- Grunenberg, L.; Kessler, C.; Teh, T.W.; Schuldt, R.; Heck, F.; Kastner, J.; Gross, J.; Hansen, N.; Lotsch, B.V. Probing Self-Diffusion of Guest Molecules in a Covalent Organic Framework: Simulation and Experiment. ACS Nano 2024, 18, 16091–16100. [Google Scholar] [CrossRef]
- Gomes, R.; Bhaumik, A. A new triazine functionalized luminescent covalent organic framework for nitroaromatic sensing and CO2 storage. RSC Adv. 2016, 6, 28047–28054. [Google Scholar] [CrossRef]
- Chen, X.; Li, Y.; Jia, L.; Yu, X.; Wang, Q.; Zhang, Y.; Zhang, Z.; Liang, E.; Han, B.; Li, J. N-doping and structural regularity of covalent organic frameworks (COFs) tune the catalytic activity for knoevenagel condensation reaction. J. Solid. State Chem. 2023, 328, 124352. [Google Scholar] [CrossRef]
- Uribe-Romo, F.J.; Hunt, J.R.; Furukawa, H.; Klöck, C.; O’Keeffe, M.; Yaghi, O.M. A Crystalline Imine-Linked 3-D Porous Covalent Organic Framework. J. Am. Chem. Soc. 2009, 131, 4570–4571. [Google Scholar] [CrossRef] [PubMed]
- Zou, Y.; Wang, P.; Zhang, A.; Qin, Z.; Li, Y.; Xianyu, Y.; Zhang, H. Covalent Organic Framework-Incorporated Nanofibrous Membrane as an Intelligent Platform for Wound Dressing. ACS Appl. Mater. Interfaces 2022, 14, 8680–8692. [Google Scholar] [CrossRef] [PubMed]
- Bai, L.; Phua, S.Z.; Lim, W.Q.; Jana, A.; Luo, Z.; Tham, H.P.; Zhao, L.; Gao, Q.; Zhao, Y. Nanoscale covalent organic frameworks as smart carriers for drug delivery. Chem. Commun. 2016, 52, 4128–4131. [Google Scholar] [CrossRef]
- Chen, Y.; Luo, X.; Zhang, J.; Hu, L.; Xu, T.; Li, W.; Chen, L.; Shen, M.; Ren, S.-B.; Han, D.-M.; et al. Bandgap engineering of covalent organic frameworks for boosting photocatalytic hydrogen evolution from water. J. Mater. Chem. A 2022, 10, 24620–24627. [Google Scholar] [CrossRef]
- Zhu, D.; Verduzco, R. Ultralow Surface Tension Solvents Enable Facile COF Activation with Reduced Pore Collapse. ACS Appl. Mater. Interfaces 2020, 12, 33121–33127. [Google Scholar] [CrossRef]
- Wu, W.N.; Chen, D.Y.; Zhang, M.Y.; Zhao, X.H.; Zhao, R.; Geng, C.Y.; Jia, J.T.; Zhu, G.S. Uranium Extraction from Seawater via Hydrogen Bond Porous Organic Cages. J. Am. Chem. Soc. 2025, 147, 2228–2236. [Google Scholar] [CrossRef]
- Wang, Z.H.; Jiang, L.; Jia, J.T.; Zhu, G.S. Targeted Synthesis of Interpenetration-Free Mesoporous Aromatic Frameworks by Manipulating Catalysts as Templates. Angew. Chem.-Int. Edit. 2025, 64, e202420746. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.C.; Cao, C.; Liu, W.; Zhang, H.; Li, Q.Y.; Zhu, S.Y.; Li, X.N.; Li, J.S.; Chang, J.F.; Hu, W.; et al. Pyridine-nitrogen conjugated covalent organic frameworks for high-efficiency gas-solid photocatalytic reduction of CO2 to CO. J. Energy Chem. 2025, 104, 127–135. [Google Scholar] [CrossRef]
- Zhao, X.; Li, A.C.; Yang, D.; Qiu, T.Y.; Zhao, Z.; Wang, S.L.; Mu, X.; Tan, H.Q. Coralloid W18O49@covalent organic frameworks S-scheme heterojunction for high efficiency photocatalytic aerobic oxidation. J. Colloid. Interface Sci. 2024, 653, 67–76. [Google Scholar] [CrossRef]
- Sun, L.; Huang, X.J.; Kong, Y.H.; Jia, J.T.; Zhu, G.S. Hydrogen storage in a sandwich structure by assembly of BNs and MOFs. Chem. Commun. 2024, 60, 11976–11979. [Google Scholar] [CrossRef]
- Jiang, L.; Lin, L.; Wang, Z.H.; Ai, H.Y.; Jia, J.T.; Zhu, G.S. Constructing Isoreticular Metal-Organic Frameworks by Silver-Carbon Bonds. J. Am. Chem. Soc. 2024, 146, 22930–22936. [Google Scholar] [CrossRef]
- Jiang, L.; Jia, J.T.; Ma, Y.H.; Tian, Y.Y.; Zou, X.Q.; Zhu, G.S. Metal-carbon bond metal-organic frameworks with permanent porosity. Chem 2024, 10, 557–566. [Google Scholar] [CrossRef]
- Cao, L.Z.; Wang, C.; Wang, H.; Xu, X.M.; Tao, X.; Tan, H.Q.; Zhu, G.S. Rationally Designed Cyclooctatetrathiophene-Based Porous Aromatic Frameworks (COTh-PAFs) for Efficient Photocatalytic Hydrogen Peroxide Production. Angew. Chem.-Int. Edit. 2024, 63, e202402095. [Google Scholar] [CrossRef]
- Li, Z.H.; Yi, X.H.; Wang, Q.W.; Li, Y.M.; Li, D.T.; Palkovits, R.; Beine, A.K.; Liu, C.G.; Wang, X.H. Selective Production of Glycolic Acid from Cellulose Promoted by Acidic/Redox Polyoxometalates via Oxidative Hydrolysis. ACS Catal. 2023, 13, 4575–4586. [Google Scholar] [CrossRef]
- Li, S.L.; Xiao, Y.; Yan, H.; Yang, Y.T.; Tian, Y.Y.; Jing, X.F.; Zhu, G.S. Ultrafine platinum nanoparticles anchored in porous aromatic frameworks for efficient hydrogen evolution reaction. Chem. Commun. 2023, 59, 4766–4769. [Google Scholar] [CrossRef] [PubMed]
- Li, S.L.; Wang, Z.X.; Wang, T.N.; Yang, Y.T.; Xiao, Y.; Tian, Y.Y.; Zhu, H.; Jing, X.F.; Zhu, G.S. Preparation of Trimetallic-Organic Framework Film Electrodes via Secondary Growth for Efficient Oxygen Evolution Reaction. Chem.-Eur. J. 2023, 29, e202301129. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi, F.; Bagheri, H.; Barreto, G.E.; Read, M.I.; Sahebkar, A. Effects of Curcumin on Microglial Cells. Neurotox. Res. 2019, 36, 12–26. [Google Scholar] [CrossRef]
- Liang, D.; Shen, X.; Han, L.; Ren, H.; Zang, T.; Tan, L.; Lu, Z.; Liao, X.; Vetha, B.S.S.; Liu, Y.; et al. Dual-ROS Sensitive Moieties Conjugate Inhibits Curcumin Oxidative Degradation for Colitis Precise Therapy. Adv. Healthc. Mater. 2024, 13, e2303016. [Google Scholar] [CrossRef]
- Santos-Parker, J.R.; Strahler, T.R.; Bassett, C.J.; Bispham, N.Z.; Chonchol, M.B.; Seals, D.R. Curcumin older adults by increasing nitric oxide bioavailability and reducing oxidative stress. Aging 2017, 9, 187–208. [Google Scholar] [CrossRef]
- Zhou, X.; Venigalla, M.; Raju, R.; Munch, G. Pharmacological considerations for treating neuroinflammation with curcumin in Alzheimer’s disease. J. Neural Transm. 2022, 129, 755–771. [Google Scholar] [CrossRef]
- Friedman, A.J.; Han, G.; Navati, M.S.; Chacko, M.; Gunther, L.; Alfieri, A.; Friedman, J.M. Sustained release nitric oxide releasing nanoparticles: Characterization of a novel delivery platform based on nitrite containing hydrogel/glass composites. Nitric Oxide 2008, 19, 12–20. [Google Scholar] [CrossRef]
- Jin, Y.; Liu, S.; Wang, X.; Wang, C.; Ruan, Q.; Li, W. Multifunctional Microneedle Patches Loaded With Engineered Nitric Oxide-Releasing Nanocarriers for Targeted and Synergistic Chronic Wound Therapy. Adv. Mater. 2025, 37, e202413108. [Google Scholar] [CrossRef]
- Williams, A.T.; Muller, C.R.; Govender, K.; Navati, M.S.; Friedman, A.J.; Friedman, J.M.; Cabrales, P. Control of systemic inflammation through early nitric oxide supplementation with nitric oxide releasing nanoparticles. Free Radic. Biol. Med. 2020, 161, 15–22. [Google Scholar] [CrossRef]
- Wu, M.; Lu, Z.; Wu, K.; Nam, C.; Zhang, L.; Guo, J. Recent advances in the development of nitric oxide-releasing biomaterials and their application potentials in chronic wound healing. J. Mat. Chem. B 2021, 9, 7063–7075. [Google Scholar] [CrossRef] [PubMed]
- Azargoonjahromi, A. Dual role of nitric oxide in Alzheimer’s disease. Nitric Oxide 2023, 134–135, 23–37. [Google Scholar] [CrossRef] [PubMed]
- Fershtat, L.L.; Zhilin, E.S. Recent Advances in the Synthesis and Biomedical Applications of Heterocyclic NO-Donors. Molecules 2021, 26, 5705. [Google Scholar] [CrossRef] [PubMed]
- Mancini, R.S.; Barden, C.J.; Weaver, D.F.; Reed, M.A. Furazans in Medicinal Chemistry. J. Mater. Chem. 2021, 64, 1786–1815. [Google Scholar] [CrossRef]
- Medana, C.; Ermondi, G.; Fruttero, R.; Distilo, A.; Ferretti, C.; Gasco, A. Furoxans as Nitric Oxide Donors. 4-Phenyl-3-furoxancarbonitrile: Thiol-Mediated Nitric Oxide Release and Biological Evaluation. J. Mater. Chem. 1994, 37, 4412–4416. [Google Scholar] [CrossRef]
- Lai, X.; Yu, L.; Huang, X.; Gardner, W.; Bamford, S.E.; Pigram, P.J.; Wang, S.; Brun, A.P.L.; Muir, B.W.; Song, J.; et al. Enhanced Nitric Oxide Delivery Through Self-Assembling Nanoparticles for Eradicating Gram-Negative Bacteria. Adv. Healthc. Mater. 2024, 13, e2403046. [Google Scholar] [CrossRef]
- Fershtat, L.L.; Makhova, N.N. Molecular Hybridization Tools in the Development of Furoxan-Based NO-Donor Prodrugs. ChemMedChem 2017, 12, 622–638. [Google Scholar] [CrossRef]
- Zhong, D.; Jin, K.; Wang, R.; Chen, B.; Zhang, J.; Ren, C.; Chen, X.; Lu, J.; Zhou, M. Microalgae-Based Hydrogel for Inflammatory Bowel Disease and Its Associated Anxiety and Depression. Adv. Mater. 2024, 36, 2312275. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Xiang, P.; Duro-Castano, A.; Cai, H.; Guo, B.; Liu, X.; Yu, Y.; Lui, S.; Luo, K.; Bowen Ke, B.; et al. Rapid amyloid-β clearance and cognitive recovery through multivalent modulation of blood–brain barrier transport. Sig. Transduct. Target. Ther. 2025, 10, 331. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, Y.; Wang, Z.; Xi, E.; Yang, F.; Gao, N. Hydrophobic Drug Delivery Platforms Based on Covalent Organic Frameworks for Combined Treatment of Alzheimer’s Disease. Int. J. Mol. Sci. 2025, 26, 10803. https://doi.org/10.3390/ijms262110803
Zhao Y, Wang Z, Xi E, Yang F, Gao N. Hydrophobic Drug Delivery Platforms Based on Covalent Organic Frameworks for Combined Treatment of Alzheimer’s Disease. International Journal of Molecular Sciences. 2025; 26(21):10803. https://doi.org/10.3390/ijms262110803
Chicago/Turabian StyleZhao, Yun, Ziwei Wang, Enpeng Xi, Fuming Yang, and Nan Gao. 2025. "Hydrophobic Drug Delivery Platforms Based on Covalent Organic Frameworks for Combined Treatment of Alzheimer’s Disease" International Journal of Molecular Sciences 26, no. 21: 10803. https://doi.org/10.3390/ijms262110803
APA StyleZhao, Y., Wang, Z., Xi, E., Yang, F., & Gao, N. (2025). Hydrophobic Drug Delivery Platforms Based on Covalent Organic Frameworks for Combined Treatment of Alzheimer’s Disease. International Journal of Molecular Sciences, 26(21), 10803. https://doi.org/10.3390/ijms262110803





