Galectin-3 and Strain Imaging for Early Heart Failure Prediction After First Myocardial Infarction
Abstract
1. Introduction
2. Results
2.1. Patient Characteristics
2.2. Gal-3 Concentration and Other Biomarkers
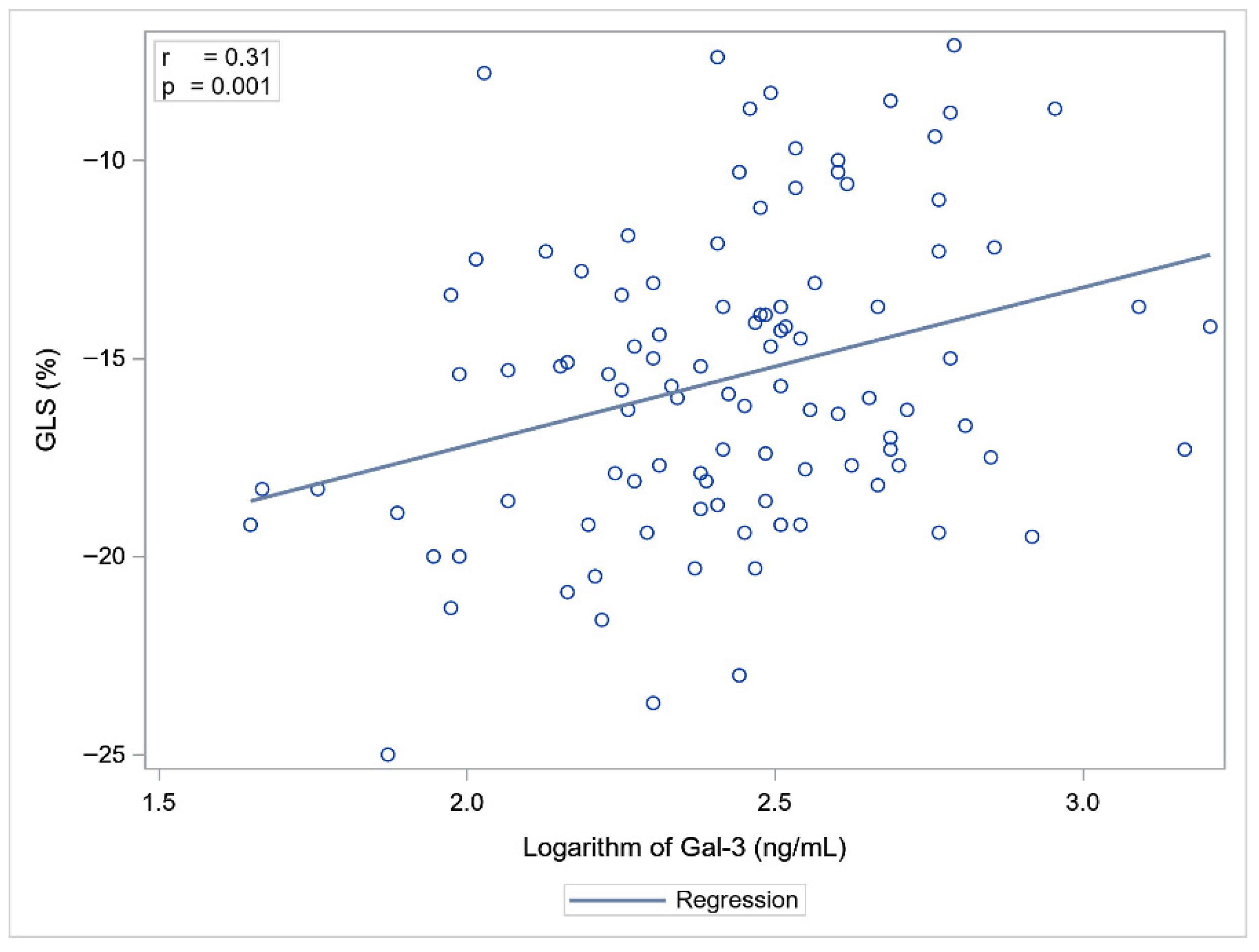
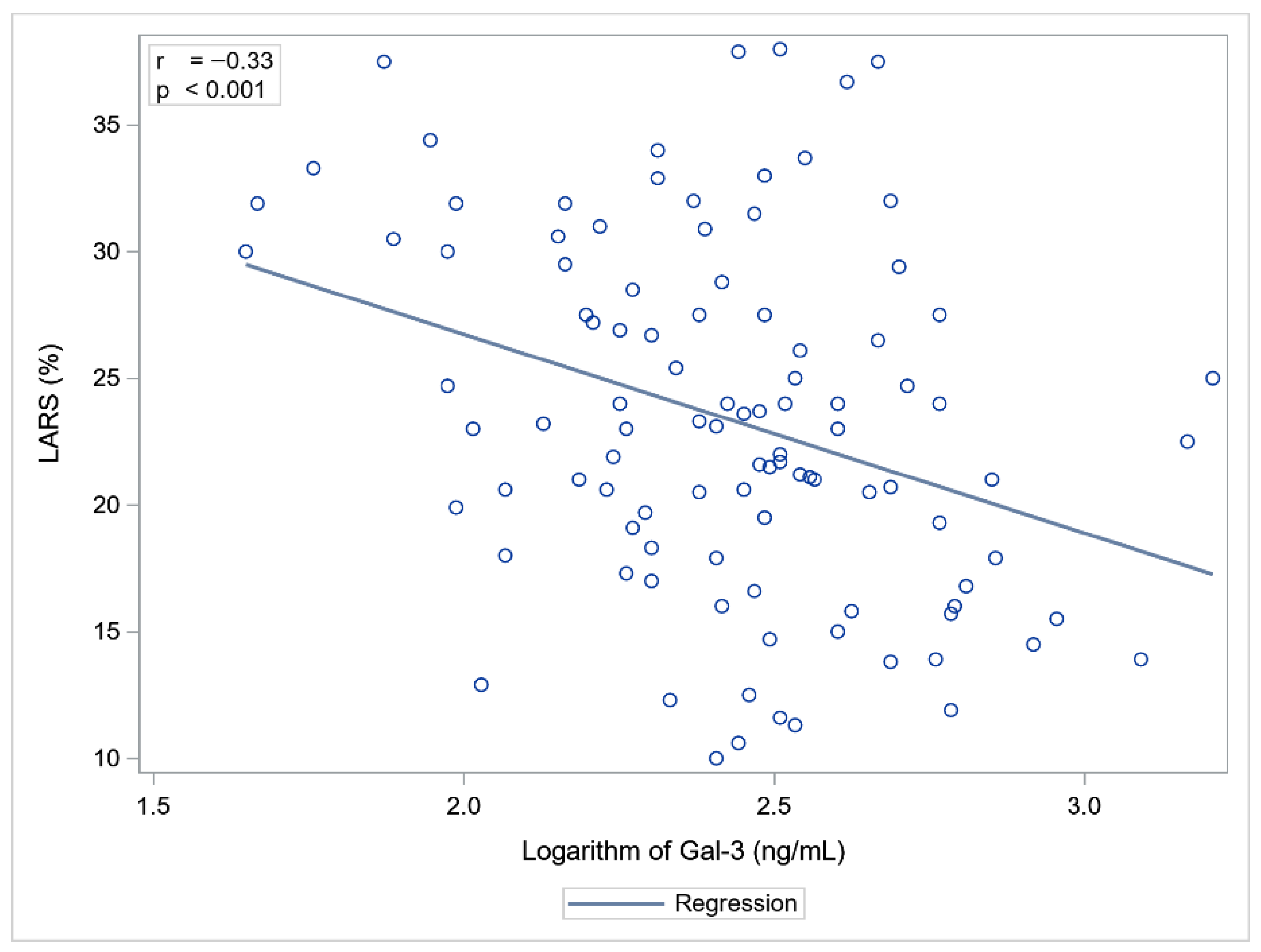
2.3. Echocardiographic Parameters in Relation to Biomarkers
2.4. Gal-3 Prognostic Value in STEMI/NSTEMI
3. Discussion
Study Limitations
4. Materials and Methods
4.1. Study Population and Design
4.2. Biomarker Analysis
4.3. Echocardiography
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MI | Myocardial infarction |
| HF | Heart failure |
| Gal-3 | Galectin-3 |
| NT-proBNP | N-terminal pro B-type natriuretic peptide |
| LV | Left ventricular |
| STEMI | ST-segment elevation myocardial infarction |
| NSTEMI | Non-ST-segment elevation myocardial infarction |
| TTE | Transthoracic echocardiography |
| LVEF | Left ventricular ejection fraction |
| STE | Speckle tracking echocardiography |
| SGLT-2 | Sodium–glucose co-transporter 2 |
| CKD | Chronic kidney disease |
| LAD | Left anterior descending artery |
| GLS | Global longitudinal strain |
| LARS | Left atrial reservoir strain |
| TAPSE | Tricuspid annular plane systolic excursion |
| pPCI | Primary percutaneous coronary intervention |
| LAVi | Left atrial indexed volume |
References
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, e895–e1032. [Google Scholar] [CrossRef] [PubMed]
- Suthahar, N.; Meijers, W.C.; Silljé, H.H.W.; Ho, J.E.; Liu, F.T.; de Boer, R.A. Galectin-3 Activation and Inhibition in Heart Failure and Cardiovascular Disease: An Update. Theranostics 2018, 8, 593–609. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.E.; Liu, C.; Lyass, A.; Courchesne, P.; Pencina, M.J.; Vasan, R.S.; Larson, M.G.; Levy, D. Galectin-3, a marker of cardiac fibrosis, predicts incident heart failure in the community. J. Am. Coll. Cardiol. 2012, 60, 1249–1256. [Google Scholar] [CrossRef]
- Toprak, G.; Yüksel, H.; Demirpençe, Ö.; Islamoglu, Y.; Evliyaoglu, O.; Mete, N. Fibrosis in heart failure subtypes. Eur. Rev. Med. Pharmacol. Sci. 2013, 17, 2302–2309. [Google Scholar]
- Zaborska, B.; Sikora-Frąc, M.; Smarż, K.; Pilichowska-Paszkiet, E.; Budaj, A.; Sitkiewicz, D.; Sygitowicz, G. The Role of Galectin-3 in Heart Failure-The Diagnostic, Prognostic and Therapeutic Potential-Where Do We Stand? Int. J. Mol. Sci. 2023, 24, 13111. [Google Scholar] [CrossRef]
- Bosnjak, I.; Selthofer-Relatic, K.; Vcev, A. Prognostic value of galectin-3 in patients with heart failure. Dis. Markers 2015, 2015, 690205. [Google Scholar] [CrossRef]
- de Boer, R.A.; Yu, L.; van Veldhuisen, D.J. Galectin-3 in cardiac remodeling and heart failure. Curr. Heart Fail. Rep. 2010, 7, 1–8. [Google Scholar] [CrossRef]
- Cheng, W.; Maciej, R.; Thiele, H.; Büttner, P. Galectin-3 levels and long-term all-cause mortality and hospitalization in heart failure patients: A meta-analysis. ESC Heart Fail. 2024, 11, 2566–2577. [Google Scholar] [CrossRef]
- Sygitowicz, G.; Tomaniak, M.; Filipiak, K.J.; Kołtowski, Ł.; Sitkiewicz, D. Galectin-3 in Patients with Acute Heart Failure: Preliminary Report on First Polish Experience. Adv. Clin. Exp. Med. 2016, 25, 617–623. [Google Scholar] [CrossRef]
- de Boer, R.A.; Lok, D.J.; Jaarsma, T.; van der Meer, P.; Voors, A.A.; Hillege, H.L.; van Veldhuisen, D.J. Predictive value of plasma galectin-3 levels in heart failure with reduced and preserved ejection fraction. Ann. Med. 2011, 43, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Lok, D.J.; Van Der Meer, P.; de la Porte, P.W.; Lipsic, E.; Van Wijngaarden, J.; Hillege, H.L.; van Veldhuisen, D.J. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: Data from the DEAL-HF study. Clin. Res. Cardiol. 2010, 99, 323–328. [Google Scholar] [CrossRef]
- Al-Salam, S.; Hashmi, S.; Jagadeesh, G.S.; Tariq, S. Galectin-3: A Cardiomyocyte Antiapoptotic Mediator at 24-Hour Post Myocardial Infarction. Cell Physiol. Biochem. 2020, 54, 287–302. [Google Scholar] [CrossRef]
- Cassaglia, P.; Penas, F.; Betazza, C.; Fontana Estevez, F.; Miksztowicz, V.; Martínez Naya, N.; Llamosas, M.C.; Noli Truant, S.; Wilensky, L.; Volberg, V.; et al. Genetic Deletion of Galectin-3 Alters the Temporal Evolution of Macrophage Infiltration and Healing Affecting the Cardiac Remodeling and Function after Myocardial Infarction in Mice. Am. J. Pathol. 2020, 190, 1789–1800. [Google Scholar] [CrossRef]
- Sanchez-Mas, J.; Lax, A.; Asensio-Lopez, M.C.; Fernandez-Del Palacio, M.J.; Caballero, L.; Garrido, I.P.; Pastor, F.; Januzzi, J.L.; Pascual-Figal, D.A. Galectin-3 expression in cardiac remodeling after myocardial infarction. Int. J. Cardiol. 2014, 172, e98–e101. [Google Scholar] [CrossRef] [PubMed]
- Di Tano, G.; Caretta, G.; De Maria, R.; Parolini, M.; Bassi, L.; Testa, S.; Pirelli, S. Galectin-3 predicts left ventricular remodelling after anterior-wall myocardial infarction treated by primary percutaneous coronary intervention. Heart 2017, 103, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Redondo, A.; Paradela-Dobarro, B.; Moscoso, I.; Moure-Álvarez, M.; Cebro-Márquez, M.; González-Juanatey, J.R.; García-Seara, J.; Álvarez, E. Galectin-3 and soluble RAGE as new biomarkers of post-infarction cardiac remodeling. J. Mol. Med. 2021, 99, 943–953. [Google Scholar] [CrossRef]
- Di Tano, G.; Caretta, G.; De Maria, R.; Bettari, L.; Parolini, M.; Testa, S.; Pirelli, S. Galectin-3 and outcomes after anterior-wall myocardial infarction treated by primary percutaneous coronary intervention. Biomark. Med. 2018, 12, 21–26. [Google Scholar] [CrossRef]
- Asleh, R.; Enriquez-Sarano, M.; Jaffe, A.S.; Manemann, S.M.; Weston, S.A.; Jiang, R.; Roger, V.L. Galectin-3 Levels and Outcomes After Myocardial Infarction: A Population-Based Study. J. Am. Coll. Cardiol. 2019, 73, 2286–2295. [Google Scholar] [CrossRef] [PubMed]
- Tymińska, A.; Kapłon-Cieślicka, A.; Ozierański, K.; Budnik, M.; Wancerz, A.; Sypień, P.; Peller, M.; Maksym, J.; Balsam, P.; Opolski, G.; et al. Association of galectin-3 and soluble ST2 with in-hospital and 1-year outcomes in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. Pol. Arch. Intern. Med. 2019, 129, 770–780. [Google Scholar] [CrossRef]
- Köktürk, U.; Püşüroğlu, H.; Somuncu, M.U.; Akgül, Ö.; Uygur, B.; Özyılmaz, S.; Işıksaçan, N.; Sürgit, Ö.; Yıldırım, A. Short and Long-Term Prognostic Significance of Galectin-3 in Patients with ST-Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Angiology 2023, 74, 889–896. [Google Scholar] [CrossRef]
- Vucic, R.M.; Andrejic, O.M.; Stokanovic, D.; Stoimenov, T.J.; McClements, L.; Nikolic, V.N.; Sreckovic, M.; Veselinovic, M.; Aleksandric, S.; Popadic, V.; et al. Galectin-3 as a Prognostic Biomarker in Patients with First Acute Myocardial Infarction without Heart Failure. Diagnostics 2023, 13, 3348. [Google Scholar] [CrossRef]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef]
- Prastaro, M.; Pirozzi, E.; Gaibazzi, N.; Paolillo, S.; Santoro, C.; Savarese, G.; Losi, M.A.; Esposito, G.; Perrone Filardi, P.; Trimarco, B.; et al. Expert Review on the Prognostic Role of Echocardiography after Acute Myocardial Infarction. J. Am. Soc. Echocardiogr. 2017, 30, 431–443.e432. [Google Scholar] [CrossRef]
- Netala, V.R.; Hou, T.; Wang, Y.; Zhang, Z.; Teertam, S.K. Cardiovascular Biomarkers: Tools for Precision Diagnosis and Prognosis. Int. J. Mol. Sci. 2025, 26, 3218. [Google Scholar] [CrossRef]
- Frangogiannis, N.G. Regulation of the inflammatory response in cardiac repair. Circ. Res. 2012, 110, 159–173. [Google Scholar] [CrossRef]
- Filipe, M.D.; Meijers, W.C.; Rogier van der Velde, A.; de Boer, R.A. Galectin-3 and heart failure: Prognosis, prediction & clinical utility. Clin. Chim. Acta 2015, 443, 48–56. [Google Scholar] [CrossRef]
- de Boer, R.A.; Voors, A.A.; Muntendam, P.; van Gilst, W.H.; van Veldhuisen, D.J. Galectin-3: A novel mediator of heart failure development and progression. Eur. J. Heart Fail. 2009, 11, 811–817. [Google Scholar] [CrossRef]
- Yang, R.Y.; Rabinovich, G.A.; Liu, F.T. Galectins: Structure, function and therapeutic potential. Expert. Rev. Mol. Med. 2008, 10, e17. [Google Scholar] [CrossRef] [PubMed]
- O’Donoghue, M.L.; Morrow, D.A.; Cannon, C.P.; Jarolim, P.; Desai, N.R.; Sherwood, M.W.; Murphy, S.A.; Gerszten, R.E.; Sabatine, M.S. Multimarker Risk Stratification in Patients with Acute Myocardial Infarction. J. Am. Heart Assoc. 2016, 5, e002586. [Google Scholar] [CrossRef] [PubMed]
- Dekleva, M.; Djuric, T.; Djordjevic, A.; Soldatovic, I.; Stankovic, A.; Suzic Lazic, J.; Zivkovic, M. Sex-Related Differences in Heart Failure Development in Patients After First Myocardial Infarction: The Role of Galectin-3. Biomedicines 2024, 12, 2661. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo-Almorós, A.; Pello, A.; Aceña, Á.; Martínez-Milla, J.; González-Lorenzo, Ó.; Tarín, N.; Cristóbal, C.; Blanco-Colio, L.M.; Martín-Ventura, J.L.; Huelmos, A.; et al. Galectin-3 Is Associated with Cardiovascular Events in Post-Acute Coronary Syndrome Patients with Type-2 Diabetes. J. Clin. Med. 2020, 9, 1105. [Google Scholar] [CrossRef]
- Fu, H.; Nie, S.; Luo, P.; Ruan, Y.; Zhang, Z.; Miao, H.; Li, X.; Wen, S.; Bai, R. Galectin-3 and acute heart failure: Genetic polymorphisms, plasma level, myocardial fibrosis and 1-year outcomes. Biomark. Med. 2020, 14, 943–954. [Google Scholar] [CrossRef]
- Peacock, W.F. How galectin-3 changes acute heart failure decision making in the emergency department. Clin. Chem. Lab. Med. 2014, 52, 1409–1412. [Google Scholar] [CrossRef]
- Jiang, J.; Yang, B.; Sun, Y.; Jin, J.; Zhao, Z.; Chen, S. Diagnostic Value of Serum Concentration of Galectin-3 in Patients with Heart Failure with Preserved Ejection Fraction. Front. Cardiovasc. Med. 2021, 8, 829151. [Google Scholar] [CrossRef]
- Cahill, T.J.; Kharbanda, R.K. Heart failure after myocardial infarction in the era of primary percutaneous coronary intervention: Mechanisms, incidence and identification of patients at risk. World J. Cardiol. 2017, 9, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Jenča, D.; Melenovský, V.; Stehlik, J.; Staněk, V.; Kettner, J.; Kautzner, J.; Adámková, V.; Wohlfahrt, P. Heart failure after myocardial infarction: Incidence and predictors. ESC Heart Fail. 2021, 8, 222–237. [Google Scholar] [CrossRef] [PubMed]
- Seropian, I.M.; Cassaglia, P.; Miksztowicz, V.; González, G.E. Unraveling the role of galectin-3 in cardiac pathology and physiology. Front. Physiol. 2023, 14, 1304735. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2023, 44, 3627–3639. [Google Scholar] [CrossRef]
- Franeková, J.; Hošková, L.; Jabor, A. Galectin-3 as an independent prognostic factor after heart transplantation. Clin. Transplant. 2022, 36, e14592. [Google Scholar] [CrossRef]
- Srivatsan, V.; George, M.; Shanmugam, E. Utility of galectin-3 as a prognostic biomarker in heart failure: Where do we stand? Eur. J. Prev. Cardiol. 2015, 22, 1096–1110. [Google Scholar] [CrossRef]
- Andrejic, O.M.; Vucic, R.M.; Pavlovic, M.; McClements, L.; Stokanovic, D.; Jevtovic-Stoimenov, T.; Nikolic, V.N. Association between Galectin-3 levels within central and peripheral venous blood, and adverse left ventricular remodelling after first acute myocardial infarction. Sci. Rep. 2019, 9, 13145. [Google Scholar] [CrossRef] [PubMed]
- van der Velde, A.R.; Lexis, C.P.; Meijers, W.C.; van der Horst, I.C.; Lipsic, E.; Dokter, M.M.; van Veldhuisen, D.J.; van der Harst, P.; de Boer, R.A. Galectin-3 and sST2 in prediction of left ventricular ejection fraction after myocardial infarction. Clin. Chim. Acta 2016, 452, 50–57. [Google Scholar] [CrossRef]
- Weir, R.A.; Petrie, C.J.; Murphy, C.A.; Clements, S.; Steedman, T.; Miller, A.M.; McInnes, I.B.; Squire, I.B.; Ng, L.L.; Dargie, H.J.; et al. Galectin-3 and cardiac function in survivors of acute myocardial infarction. Circ. Heart Fail. 2013, 6, 492–498. [Google Scholar] [CrossRef]
- Klettas, D.; Georgiopoulos, G.; Rizvi, Q.; Oikonomou, D.; Magkas, N.; Bhuva, A.N.; Manisty, C.; Captur, G.; Aimo, A.; Nihoyannopoulos, P. Echocardiographic and Cardiac Magnetic Resonance Imaging-Derived Strains in Relation to Late Gadolinium Enhancement in Hypertrophic Cardiomyopathy. Am. J. Cardiol. 2022, 171, 132–139. [Google Scholar] [CrossRef]
- Ricken, K.; Lenselink, C.; Venema, C.S.; van der Horst, I.C.C.; van der Harst, P.; Pundziute-Do Prado, G.; Voors, A.A.; Lipsic, E. Left atrial strain predicts long-term heart failure outcomes after ST-elevation myocardial infarction. Int. J. Cardiol. 2025, 422, 132931. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367, Correction in Eur. Heart J. 2024, 45, 404–405. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth universal definition of myocardial infarction (2018). Eur. Heart J. 2019, 40, 237–269. [Google Scholar] [CrossRef]
- Smith, S.C., Jr.; Feldman, T.E.; Hirshfeld, J.W., Jr.; Jacobs, A.K.; Kern, M.J.; King, S.B., 3rd; Morrison, D.A.; O’Neil, W.W.; Schaff, H.V.; Whitlow, P.L.; et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention). Circulation 2006, 113, e166–e286. [Google Scholar] [CrossRef]
- Bozkurt, B.; Coats, A.J.S.; Tsutsui, H.; Abdelhamid, C.M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Böhm, M.; Butler, J.; et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur. J. Heart Fail. 2021, 23, 352–380. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14, Correction in J. Am. Soc. Echocardiogr. 2016, 29, 521. [Google Scholar] [CrossRef] [PubMed]
- Schiller, N.B.; Shah, P.M.; Crawford, M.; DeMaria, A.; Devereux, R.; Feigenbaum, H.; Gutgesell, H.; Reichek, N.; Sahn, D.; Schnittger, I.; et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J. Am. Soc. Echocardiogr. 1989, 2, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Badano, L.P.; Kolias, T.J.; Muraru, D.; Abraham, T.P.; Aurigemma, G.; Edvardsen, T.; D’Hooge, J.; Donal, E.; Fraser, A.G.; Marwick, T.; et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: A consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F., 3rd; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef]

| Variable | All Patients n = 105 | HF n = 34 | Without HF n = 71 | p Value |
|---|---|---|---|---|
| Demographic parameters | ||||
| Age (years) | 61 ± 11.1 | 63.8 ± 10.6 | 58.9 ± 11.3 | 0.04 |
| Male gender (%) | 81 (77%) | 25 (73%) | 56 (79%) | 0.54 |
| BMI (kg/m2) | 27 ± 4.0 | 25.4 ± 3.4 | 28.6 ± 3.8 | <0.001 |
| Smoking (%) | 46 (43.8%) | 16 (47%) | 30 (42.2%) | 0.93 |
| Comorbidities | ||||
| DM t.2 | 22 (21%) | 4 (11.8%) | 18 (25.3%) | 0.11 |
| Arterial hypertension | 73 (69.5%) | 23 (67.6%) | 50 (70.4%) | 0.77 |
| CKD | 6 (5.7%) | 5 (14.7%) | 1 (1.4%) | 0.01 |
| Hyperlipidaemia | 79 (75.2%) | 28 (82.3%) | 51 (71.8%) | 0.24 |
| Laboratory parameters | ||||
| Haemoglobin (g/dL) | 14.3 ± 1.4 | 14.0 ± 1.4 | 14.5 ± 1.4 | 0.14 |
| Creatinine (mg/dL), median | 0.84 [0.74–0.95] | 0.91 [0.81–1.2] | 0.81 [0.72–0.93] | 0.005 |
| Total cholesterol (mg/dL) | 200.6 ± 47.4 | 195 ± 51 | 203 ± 46 | 0.38 |
| LDL-C (mg/dL) | 122.8 ± 42.6 | 119 ± 46 | 125 ± 41 | 0.52 |
| HDL-C (mg/dL), median | 45 [39–55] | 48 [41–56] | 44 [38–54] | 0.19 |
| Triglycerides (mg/dL), median | 110 [68–178] | 80.5 [62–110] | 131 [71–193] | 0.002 |
| Non-HDL-C (mg/dL), median | 88 [67–135] | 78 [60–111] | 89 [70–144] | 0.09 |
| Troponin T * (ng/L), median | 1150 [345–3661] | 4734 [567–7014] | 810 [249–2459] | <0.001 |
| NT-proBNP (pg/mL) median | 485 [156–1443] | 1298 [635–2354] | 284 [109–800] | <0.001 |
| Galectin-3 (ng/mL) median | 11.6 [9.5–13.5] | 12.4 [11.5–15.1] | 10.8 [8.9–12.6] | <0.001 |
| Acute MI | ||||
| STEMI | 59 (56.1%) | 24 (70.6%) | 35 (49.3%) | 0.04 |
| NSTEMI | 46 (43.9%) | 10 (29.4%) | 36 (50.7%) | 0.04 |
| pPCI | 105 (100%) | 34 (100%) | 71 (100%) | |
| PCI second stage | 26 (25%) | 8 (24%) | 18 (25%) | 0.84 |
| Length of all hospital stay (days), median | 9 [7–10] | 10 [8–13] | 9 [7–9] | <0.001 |
| CCU (days), median | 3 [3–4] | 4 [3–5] | 3 [3–4] | <0.001 |
| Infarct-related vessel | ||||
| LAD | 53 (50.5%) | 24 (70.6%) | 29 (40.8%) | 0.004 |
| LCX | 27 (25.7%) | 6 (17.6%) | 21 (29.6%) | 0.19 |
| RCA | 28 (26.7%) | 7 (20,6%) | 21 (29.6%) | 0.33 |
| Treatment | ||||
| ACEI | 85 (80.9%) | 29 (85.3%) | 56 (78.9%) | 0.43 |
| ARA-II | 15 (14.3%) | 4 (11.8%) | 10 (15.5%) | 0.77 |
| β-blockers | 88 (83.8%) | 29 (85.3%) | 59 (83.1%) | 0.78 |
| Diuretics | 24 (22.9%) | 19 (55.9%) | 5 (7.0%) | <0.001 |
| Aspirin | 101 (96.3%) | 32 (94.1%) | 69 (97.2%) | 0.59 |
| Clopidogrel | 20 (19.1%) | 10 (29.4%) | 10 (14.1%) | 0.06 |
| Ticagrelor | 54 (51.4%) | 18 (52.9%) | 36 (50.7%) | 0.83 |
| Prasugrel | 30 (28.6%) | 5 (14.7%) | 25 (35.2%) | 0.03 |
| Statins | 103 (98.1%) | 33 (97.1%) | 70 (98.6%) | 0.55 |
| SGLT-2 inhibitors | 25 (23.8%) | 19 (55.9%) | 6 (8.4%) | <0.001 |
| Aldosterone antagonists | 17 (16.2%) | 15 (44.1%) | 2 (2.8%) | <0.001 |
| Parameter | All Patients n = 105 | HF n = 34 | Without HF n = 71 | p Value |
|---|---|---|---|---|
| LV end diastolic diameter (mm) | 45.7 ± 5.4 | 46.4 ± 5.6 | 45.4 ± 5.3 | 0.36 |
| IVS (mm) | 12.1 ± 1.7 | 12.2 ± 1.9 | 12.1 ± 1.5 | 0.82 |
| LV posterior wall thickness (mm) | 11 ± 1.5 | 10.7 ± 1.7 | 11.0 ± 1.4 | 0.39 |
| LV end diastolic volume (mL) | 91.9 ± 25.1 | 96.5 ± 28.3 | 89.8 ± 23.3 | 0.20 |
| LAVi (mL/m2), median | 31.6 [27.3–40.9] | 34.3 [27.3–46.1] | 30.6 [27–38] | 0.20 |
| LV ejection fraction (%), median | 55 [47–60] | 43 [38–49] | 57 [51–60] | <0.001 |
| GLS (%) | −15.5 ± 3.8 | −12.9 ± 4.1 | −16.8 ± 2.9 | <0.001 |
| LARS (%) | 23.4 ± 6.9 | 19.8 ± 6.7 | 25.1 ± 6.4 | <0.001 |
| RVOT diameter (mm) | 29.6 ± 4 | 28.6 ± 3.8 | 30.1 ± 4.1 | 0.07 |
| TAPSE (mm) | 20 ± 3.1 | 19.4 ± 3.5 | 21.2 ± 2.8 | 0.005 |
| E wave (cm), median | 62.7 [50–78] | 63.5 [50–78] | 60 [50–70] | 0.47 |
| A wave (cm), median | 70 [56–87] | 62.5 [55–80] | 70 [60–87] | 0.20 |
| E/A, median | 0.85 [0.7–1.1] | 0.89 [0.7–1.4] | 0.82 [0.7–1] | 0.13 |
| e’ (cm), median | 8 [6–9] | 5.5 [5–7] | 7 [6–8.2] | 0.002 |
| E/e’, median | 9 [7.8–11] | 10 [8.2–12.2] | 8.4 [7.4–10] | 0.004 |
| Log Gal-3 | Log NT-proBNP | |||
|---|---|---|---|---|
| Variable | r | p Value | r | p Value |
| LVEF | −0.27 | 0.005 | −0.41 | <0.001 |
| GLS | 0.31 | 0.001 | 0.38 | <0.001 |
| LARS | −0.33 | 0.001 | −0.40 | <0.001 |
| Log NT-proBNP | 0.39 | <0.001 | ||
| LVEF < 50% Tertile 1 | 50% ≤ LVEF < 60% Tertile 2 | LVEF ≥ 60% Tertile 3 | p Value | |
| Gal-3 ng/mL | 12.3 [11.1–14.9] | 11.2 [9.5–12.8] | 10.8 [8.6–12.2] | 0.02 1 vs. 3: 0.02 |
| GLS > −14.2% Tertile 1 | −14.2% ≥ GLS > −17.7% Tertile 2 | GLS ≤ −17.7% Tertile 3 | p Value | |
| Gal-3 ng/mL | 12.2 [11.1–14.7] | 11.9 [10–14.2] | 10.1 [7.9–12] | 0.002 1 vs. 3: 0.004 |
| LARS ≤ 20.5% Tertile 1 | 20,5% < LARS ≤ 26.5% Tertile 2 | LARS > 26.5% Tertile 3 | p Value | |
| Gal-3 ng/mL | 12.1 [10.3–15.9] | 11.9 [9.6–13] | 10.1 [8.6–12.1] | 0.006 1 vs. 3: 0.006 |
| Regression Coefficient ± SE | Partial Correlation Coefficient | p Value | |
|---|---|---|---|
| GLS | |||
| Log Troponin T | 1.16 ± 0.22 | 0.47 | <0.001 |
| Log Gal-3 | 2.97 ± 1.09 | 0.26 | 0.008 |
| LARS | |||
| Log Troponin T | −1.68 ± 0.42 | −0.37 | <0.001 |
| Log Gal-3 | −6.37 ± 2.08 | −0.29 | 0.003 |
| Variable | OR [95% CI] | p Value |
|---|---|---|
| Age | 1.041 [1.002–1.082] | 0.04 |
| Creatinine | 12.7 [1.52–105.6] | 0.02 |
| GLS | 1.397 [1.204–1.621] | <0.001 |
| LARS | 0.880 [0.818–0.946] | <0.001 |
| Troponin T, units = 10 | 1.004 [1.002–1.006] | <0.001 |
| Gal-3 | 1.202 [1.056–1.369] | 0.005 |
| Variable | OR [95% CI] | p Value | AUC |
|---|---|---|---|
| GLS | 1.36 [1.17–1.59] | <0.001 | 0.833 |
| Gal-3 (log, per 0.1 unit) | 1.78 [1.16–2.73] | 0.008 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sikora-Frąc, M.; Sygitowicz, G.; Pilichowska-Paszkiet, E.; Smarż, K.; Maciejewski, P.; Kokowicz, P.; Prządka, M.; Budaj, A.; Zaborska, B. Galectin-3 and Strain Imaging for Early Heart Failure Prediction After First Myocardial Infarction. Int. J. Mol. Sci. 2025, 26, 10718. https://doi.org/10.3390/ijms262110718
Sikora-Frąc M, Sygitowicz G, Pilichowska-Paszkiet E, Smarż K, Maciejewski P, Kokowicz P, Prządka M, Budaj A, Zaborska B. Galectin-3 and Strain Imaging for Early Heart Failure Prediction After First Myocardial Infarction. International Journal of Molecular Sciences. 2025; 26(21):10718. https://doi.org/10.3390/ijms262110718
Chicago/Turabian StyleSikora-Frąc, Małgorzata, Grażyna Sygitowicz, Ewa Pilichowska-Paszkiet, Krzysztof Smarż, Paweł Maciejewski, Piotr Kokowicz, Marta Prządka, Andrzej Budaj, and Beata Zaborska. 2025. "Galectin-3 and Strain Imaging for Early Heart Failure Prediction After First Myocardial Infarction" International Journal of Molecular Sciences 26, no. 21: 10718. https://doi.org/10.3390/ijms262110718
APA StyleSikora-Frąc, M., Sygitowicz, G., Pilichowska-Paszkiet, E., Smarż, K., Maciejewski, P., Kokowicz, P., Prządka, M., Budaj, A., & Zaborska, B. (2025). Galectin-3 and Strain Imaging for Early Heart Failure Prediction After First Myocardial Infarction. International Journal of Molecular Sciences, 26(21), 10718. https://doi.org/10.3390/ijms262110718






