Using 1H-Magnetic Resonance Spectroscopy to Evaluate the Efficacy of Pharmacological Treatments in Parkinson’s Disease: A Systematic Review
Abstract
1. Introduction
2. Methods
- Intervention (I): pharmacological treatments, including symptomatic and potentially disease-modifying therapies;
- Comparison (C): HC subjects (i.e., individuals without PD and not undergoing pharmacological treatment), or within-subject comparisons between treated patients and their pre-treatment baseline condition;
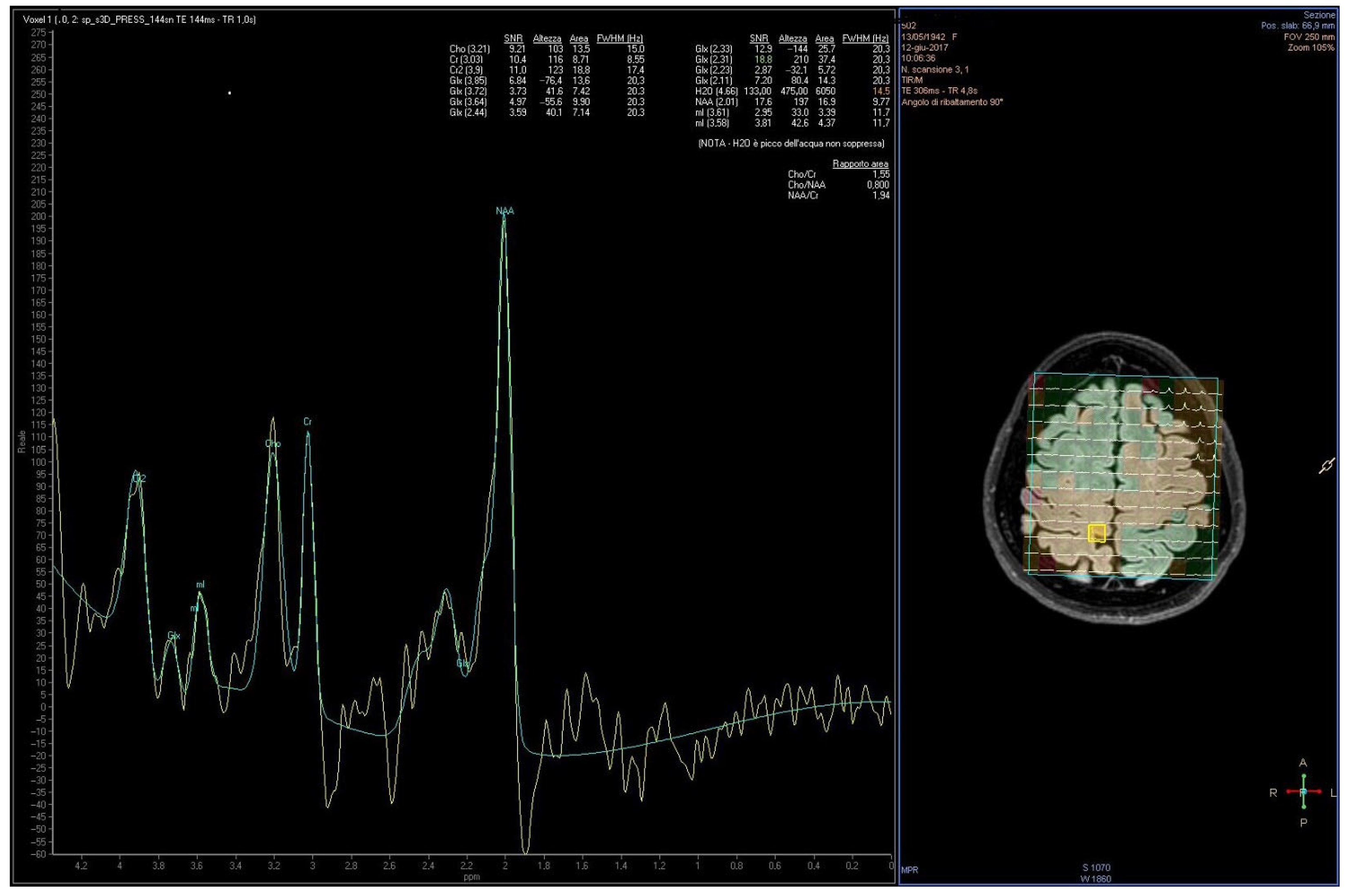
- Outcome (O): quantitative changes in cerebral neurometabolic profiles measured by 1H-MRS, with a focus on specific metabolites such as NAA, Cho, Cr, mI, Glx, and GABA, considered as potential indicators of treatment response.
- Inclusion Criteria
- Included participants with a clinically diagnosed PD;
- Investigated the effects of pharmacological treatments, either symptomatic or potentially disease-modifying;
- Employed 1H-MRS as the imaging modality to measure at least one of the following neurometabolites: NAA, Cho, Cr, Glx, mI, or GABA;
- Included either a HC group and a pre- versus post-treatment comparison within the PD group;
- Published in English.
- Exclusion Criteria
- Conducted on animal models or cell lines;
- Employed neuroimaging techniques other than 1H-MRS (e.g., phosphorus MRS);
- Did not evaluate pharmacological treatment efficacy through 1H-MRS;
- Conference proceeding without accompanying full-text articles;
- Lacked original quantitative data on pharmacological treatment effects assessed via 1H-MRS;
- Applied 1H-MRS for diagnostic or comparative purposes, without assessing therapeutic outcomes;
- Investigated non-pharmacological interventions;
- PD patients already undergoing treatment without baseline (pre-treatment) metabolic assessment;
- Retracted articles;
- Not published in English.
- Risk of Bias Assessment
3. Results and Discussion
3.1. Study Selection
- Employed neuroimaging techniques other than 1H-MRS (e.g., phosphorus MRS) (n = 1);
- Did not evaluate pharmacological treatment efficacy through 1H-MRS (n = 6);
- Applied 1H-MRS for diagnostic or comparative purposes only, without assessing therapeutic outcomes (n = 11);
- Included PD patients already undergoing treatment without baseline pre-treatment metabolic evaluation (n = 6).
- Lacked original quantitative data on pharmacological treatment effects assessed via 1H-MRS (n = 2);
- Inadequate study design due to inclusion of non-pharmacological interventions (n = 2);
- Retracted articles (n = 2);
- Conference proceeding without an available full-text article (n = 1).
3.2. Risk of Bias Assessment
- Selection bias, due to the lack of or insufficient reporting on randomization and allocation concealment procedures (Q1, Q2, Q3). Only the studies by Mazuel et al. [13] and Chagas et al. [56] explicitly reported randomization; however, only Mazuel et al. [13] described an adequate method. None of the studies provided a clear description of allocation concealment.
- Attrition bias was evident in the study by Bonanno et al. [36], which reported a high dropout rate and an unassessable differential dropout.
3.3. Study Characteristics
3.3.1. Levodopa
3.3.2. MAO-B Inhibitors
3.3.3. Cannabidiol
3.3.4. Dopamine Agonists
3.4. Methodological Limitations of the Included Studies
3.5. Results Interpretation
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BBB | Blood–Brain Barrier |
| BDNF | Brain-Derived Neurotrophic Factor |
| CBD | Cannabidiol |
| Cho | Choline |
| COMT | Catechol-O-Methyltransferase |
| Cr | Creatine |
| CSF | Cerebrospinal fluid |
| DOPAC | Dihydroxyphenylacetic Acid |
| GABA | Gamma-Amminobutyric Acid |
| GLP-1 | Glucagon-like Peptide-1 |
| Glu | Glutamate |
| Glx | Glutamate + Glutamine |
| 1H-MRS | Proton Magnetic Resonance Spectroscopy |
| H&Y | Hoehn and Yahr |
| HC(s) | Health Control(s) |
| IPD | Idiopathic Parkinson’s disease |
| ITT | Intention-to-treat |
| MAO-B | Monoamine Oxidase B |
| MR | Magnetic Resonance |
| MRI | Magnetic Resonance Imaging |
| MRS | Magnetic Resonance Spectroscopic |
| MRSI | Magnetic Resonance Spectroscopic Imaging |
| NA | Not applicable |
| NAA | N-acetylaspartate |
| NIH | National Institutes of Health |
| NMDA | N-methyl-D-aspartate |
| NR | Not Reported |
| PD | Parkinson’s Disease |
| PDQ-39 | The Parkinson’s Disease Questionnaire |
| PET | Positron emission tomography imaging |
| PICO | Population, Intervention, Comparison, Outcome |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| ROS | Reactive oxygen species |
| SN | Substantia Nigra |
| T | Tesla |
| tCr | total Creatine |
| tNAA | total N-acetylaspartate |
| UPDRS | Unified Parkinson’s Disease Rating Scale |
| VOI | Volume of interest |
References
- Obeso, J.A.; Rodriguez-Oroz, M.C.; Rodriguez, M.; Lanciego, J.L.; Artieda, J.; Gonzalo, N.; Olanow, C.W. Pathophysiology of the basal ganglia in Parkinson’s disease. Trends Neurosci. 2000, 23, S8–S19. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J. Parkinson’s disease: Clinical features and diagnosis. J. Neurol. Neurosurg. Psychiatry 2008, 79, 368–376. [Google Scholar] [CrossRef]
- Chaudhuri, K.R.; Schapira, A.H.V. Non-motor symptoms of Parkinson’s disease: Dopaminergic pathophysiology and treatment. Lancet Neurol. 2009, 8, 464–474. [Google Scholar] [CrossRef]
- Tolosa, E.; Garrido, A.; Scholz, S.W.; Poewe, W. Challenges in the diagnosis of Parkinson’s disease. Lancet Neurol. 2021, 20, 385–397. [Google Scholar] [CrossRef]
- Morris, H.R.; Spillantini, M.G.; Sue, C.M.; Williams-Gray, C.H. The pathogenesis of Parkinson’s disease. Lancet 2024, 403, 293–304. [Google Scholar] [CrossRef]
- Absalyamova, M.; Traktirov, D.; Burdinskaya, V.; Artemova, V.; Muruzheva, Z.; Karpenko, M. Molecular basis of the development of Parkinson’s disease. Neuroscience 2025, 565, 292–300. [Google Scholar] [CrossRef]
- Dias, V.; Junn, E.; Mouradian, M.M. The role of oxidative stress in Parkinson’s disease. J. Park. Dis. 2013, 3, 461–491. [Google Scholar] [CrossRef]
- Isik, S.; Yeman Kiyak, B.; Akbayir, R.; Seyhali, R.; Arpaci, T. Microglia Mediated Neuroinflammation in Parkinson’s Disease. Cells 2023, 12, 1012. [Google Scholar] [CrossRef] [PubMed]
- Nachman, E.; Verstreken, P. Synaptic proteostasis in Parkinson’s disease. Curr. Opin. Neurobiol. 2022, 72, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Hou, X.; Watzlawik, J.O.; Fiesel, F.C.; Springer, W. Autophagy in Parkinson’s Disease. J. Mol. Biol. 2020, 432, 2651–2672. [Google Scholar] [CrossRef] [PubMed]
- Kanda, S.; Bishop, J.F.; Eglitis, M.A.; Yangk, Y.; Mouradian, M.M. Enhanced vulnerability to oxidative stress by a-synuclein mutations and c-terminal truncation. Neuroscience 2000, 97, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Dorsey, E.R.; Sherer, T.; Okun, M.S.; Bloem, B.R. The emerging evidence of the Parkinson pandemic. J. Park. Dis. 2018, 8, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Mazuel, L.; Chassain, C.; Jean, B.; Pereira, B.; Cladière, A.; Speziale, C.; Durif, F. Proton MR spectroscopy for diagnosis and evaluation of treatment efficacy in Parkinson disease. Radiology 2016, 278, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Bloem, B.R.; Okun, M.S.; Klein, C. Parkinson’s disease. Lancet 2021, 397, 2284–2303. [Google Scholar] [CrossRef]
- Münchau, A.; Bhatia, K.P. Pharmacological treatment of Parkinson’s disease. Postgrad. Med. J. 2000, 76, 602–610. [Google Scholar] [CrossRef]
- Kalia, L.V.; Lang, A.E. Parkinson’s disease. Lancet 2015, 386, 896–912. [Google Scholar] [CrossRef]
- Deeks, E.D. Safinamide: First global approval. Drugs 2015, 75, 705–711. [Google Scholar] [CrossRef]
- Roberts, J.W.; Cora-Locatelli, G.; Bravi, D.; Amantea, M.A.; Mouradian, M.M.; Chase, T.N. Catechol-O-methyltransferase inhibitor tolcapone prolongs levodopa/carbidopa action in parkinsonian patients. Neurology 1993, 43, 2685–2688. [Google Scholar] [CrossRef]
- Nutt, J.G.; Woodward, W.R.; Beckner, R.M.; Stone, C.K.; Berggren, K.; Carter, J.H.; Gancher, S.T.; Hammerstad, J.P.; Gordin, A. Effect of peripheral catechol-O-methyltransferase inhibition on the pharmacokinetics and pharmacodynamics of levodopa in parkinsonian patients. Neurology 1994, 44, 913–919. [Google Scholar] [CrossRef]
- Kaakkola, S.; Gordin, A.; Männistö, P.T. General properties and clinical possibilities of new selective inhibitors of catechol O-methyltransferase. Gen. Pharmacol. 1994, 25, 813–824. [Google Scholar] [CrossRef] [PubMed]
- Fahn, S.; Oakes, D.; Shoulson, I.; Kieburtz, K.; Rudolph, A.; Lang, A.; Olanow, C.W.; Tanner, C.; Marek, K. Parkinson Study Group. Levodopa and the progression of Parkinson’s disease. N. Engl. J. Med. 2004, 351, 2498–2508. [Google Scholar] [CrossRef] [PubMed]
- Verschuur, C.V.M.; Suwijn, S.R.; Boel, J.A.; Post, B.; Bloem, B.R.; van Hilten, J.J.; van Laar, T.; Tissingh, G.; Munts, A.G.; Deuschl, G.; et al. Randomized Delayed-Start Trial of Levodopa in Parkinson’s Disease. N. Engl. J. Med. 2019, 380, 315–324. [Google Scholar] [CrossRef]
- Olanow, C.W.; Tatton, W.G.; Jenner, P. Mechanisms of cell death in Parkinson’s disease. In Parkinson’s Disease and Movement Disorders, 4th ed.; Jankovic, J., Tolosa, E., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2002. [Google Scholar]
- Tazik, S.; Johnson, S.; Lu, D.; Johnson, C.; Youdim, M.B.H.; Stockmeier, C.A.; Ou, X.M. Comparative neuroprotective effects of rasagiline and aminoindan with selegiline on dexamethasone-induced brain cell apoptosis. Neurotox. Res. 2009, 15, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Kincses, Z.T.; Vecsei, L. Pharmacological Therapy in Parkinson’s Disease: Focus on Neuroprotection. CNS Neurosci. Ther. 2011, 17, 345–367. [Google Scholar] [CrossRef]
- Ferrari-Toninelli, G.; Bonini, S.A.; Cenini, G.; Maccarinelli, G.; Grilli, M.; Uberti, D.; Memo, M. Dopamine receptor agonists for protection and repair in Parkinson’s disease. Curr. Top. Med. Chem. 2008, 8, 1089–1099. [Google Scholar] [CrossRef]
- Ossola, B.; Schendzielorz, N.; Chen, S.H.; Bird, G.S.; Tuominen, R.K.; Männistö, P.T.; Hong, J.S. Amantadine protects dopamine neurons by a dual action: Reducing activation of microglia and inducing expression of GNDF in astroglia. Neuropharmacology 2011, 61, 574–582, Erratum in Neuropharmacology 2012, 62, 1162. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J.; Tan, E.K. Parkinson’s disease: Etiopathogenesis and treatment. J. Neurol. Neurosurg. Psychiatry 2020, 91, 795–808. [Google Scholar] [CrossRef]
- Yacoubian, T.A.; Standaert, D.G. Targets for neuroprotection in Parkinson’s disease. Biochim. Biophys. Acta 2009, 1792, 676–687. [Google Scholar] [CrossRef]
- Movement Disorder Society Task Force on Rating Scales for Parkinson’s Disease. The Unified Parkinson’s Disease Rating Scale (UPDRS): Status and recommendations. Mov. Disord. 2003, 18, 738–750. [Google Scholar] [CrossRef]
- Franco, R.; Garrigós, C.; Lillo, J.; Rivas-Santisteban, R. The Potential of Metabolomics to Find Proper Biomarkers for Addressing the Neuroprotective Efficacy of Drugs Aimed at Delaying Parkinson’s and Alzheimer’s Disease Progression. Cells 2024, 13, 1288. [Google Scholar] [CrossRef]
- Ciurleo, R.; Di Lorenzo, G.; Bramanti, P.; Marino, S. Magnetic Resonance Spectroscopy: An in Vivo Molecular Imaging Biomarker for Parkinson’s Disease? Biomed. Res. Int. 2014, 2014, 519816. [Google Scholar] [CrossRef] [PubMed]
- Di Costanzo, A.; Trojsi, F.; Tosetti, M.; Giannatempo, G.M.; Nemore, F.; Piccirillo, M.; Bonavita, S.; Tedeschi, G.; Scarabino, T. High-field proton MRS of human brain. Eur. J. Radiol. 2003, 48, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Lin, A.; Ross, B.D.; Harris, K.; Wong, W. Efficacy of Proton Magnetic Resonance Spectroscopy in Neurological Diagnosis and Neurotherapeutic Decision Making. NeuroRx 2005, 2, 197–214. [Google Scholar] [CrossRef]
- De Stefano, N.; Filippi, M. MR spectroscopy in multiple sclerosis. J. Neuroimaging 2007, 17, 31–35. [Google Scholar] [CrossRef]
- Bonanno, L.; Ciurleo, R.; Marino, S.; Ruvolo, C.; Morabito, R.; Bramanti, A.; Corallo, F. Effect of MAO-B Inhibitors on Neurometabolic Profile of Patients Affected by Parkinson Disease: A Proton Magnetic Resonance Spectroscopy Study. J. Clin. Med. 2022, 11, 1931. [Google Scholar] [CrossRef]
- Gill, S.S.; Small, R.K.; Thomas, D.G.; Patel, P.; Porteous, R.; van Bruggen, N.; Gadian, D.G.; Kauppinen, R.A.; Williams, S.R. Brain metabolites as 1H NMR markers of neuronal and glial disorders. NMR Biomed. 1989, 2, 196–200. [Google Scholar] [CrossRef]
- Garnett, M.R.; Blamire, A.M.; Corkill, R.G.; Cadoux-Hudson, T.A.; Rajagopalan, B.; Styles, P. Early proton magnetic resonance spectroscopy in normal-appearing brain correlates with outcome in patients following traumatic brain injury. Brain 2000, 123, 2046–2054. [Google Scholar] [CrossRef] [PubMed]
- Gasparovic, C.; Yeo, R.; Mannell, M.; Ling, J.; Elgie, R.; Phillips, J.; Doezema, D.; Mayer, A.R. Neurometabolite concentrations in gray and white matter in mild traumatic brain injury: An 1H-magnetic resonance spectroscopy study. J. Neurotrauma 2009, 26, 1635–1643. [Google Scholar] [CrossRef]
- Bowen, B.C.; Block, R.E.; Sanchez-Ramos, J.; Pattany, P.M.; Lampman, D.A.; Murdoch, J.B.; Quencer, R.M. Proton MR Spectroscopy of the Brain in 14 Patients with Parkinson Disease. AJNR Am. J. Neuroradiol. 1995, 16, 61–68. [Google Scholar]
- Clarke, C.E.; Lowry, M. Basal ganglia metabolite concentrations in idiopathic Parkinson’s disease and multiple system atrophy measured by proton magnetic resonance spectroscopy. Eur. J. Neurol. 2000, 7, 661–665. [Google Scholar] [CrossRef]
- O’Neill, J.; Schuff, N.; Marks, W.J., Jr.; Feiwell, R.; Aminoff, M.J.; Weiner, M.W. Quantitative 1H magnetic resonance spectroscopy and MRI of Parkinson’s disease. Mov. Disord. 2002, 17, 917–927. [Google Scholar] [CrossRef]
- Öz, G.; Terpstra, M.; Tkáč, I.; Aia, P.; Lowary, J.; Tuite, P.J.; Gruetter, R. Proton MRS of the unilateral substantia nigra in the human brain at 4 tesla: Detection of high GABA concentrations. Magn. Reson. Med. 2006, 55, 296–301. [Google Scholar] [CrossRef]
- Griffith, H.R.; Okonkwo, O.C.; O’Brien, T.; den Hollander, J.A. Reduced brain glutamate in patients with Parkinson’s disease. NMR Biomed. 2008, 21, 381–387. [Google Scholar] [CrossRef]
- Levin, B.E.; Katzen, H.L.; Maudsley, A.; Post, J.; Myerson, C.; Govind, V.; Nahab, F.; Scanlon, B.; Mittel, A. Whole-brain proton MR spectroscopic imaging in Parkinson’s disease. J. Neuroimaging 2014, 24, 39–44. [Google Scholar] [CrossRef]
- Nie, K.; Zhang, Y.; Huang, B.; Wang, L.; Zhao, J.; Huang, Z.; Gan, R.; Wang, L. Marked N-acetylaspartate and choline metabolite changes in Parkinson’s disease patients with mild cognitive impairment. Park. Relat. Disord. 2013, 19, 329–334. [Google Scholar] [CrossRef]
- Zhou, B.; Yuan, F.; He, Z.; Tan, C. Application of proton magnetic resonance spectroscopy on substantia nigra metabolites in Parkinson’s disease. Brain Imaging Behav. 2014, 8, 97–101. [Google Scholar] [CrossRef]
- Elmaki, E.E.A.; Gong, T.; Nkonika, D.M.; Wang, G. Examining alterations in GABA concentrations in the basal ganglia of patients with Parkinson’s disease using MEGA-PRESS MRS. Jpn. J. Radiol. 2018, 36, 194–199. [Google Scholar] [CrossRef]
- Guan, J.; Rong, Y.; Wen, Y.; Wu, H.; Qin, H.; Zhang, Q.; Chen, W. Detection and application of neurochemical profile by multiple regional 1H-MRS in Parkinson’s disease. Brain Behav. 2017, 7, e00792. [Google Scholar] [CrossRef] [PubMed]
- Gu, W.; He, C.; Chen, J.; Li, J. Proton Magnetic Resonance Spectroscopy for the Early Diagnosis of Parkinson Disease in the Substantia Nigra and Globus Pallidus: A Meta-Analysis With Trial Sequential Analysis. Front. Neurol. 2022, 13, 838230. [Google Scholar] [CrossRef] [PubMed]
- Guan, J.T.; Zheng, X.; Lai, L.; Sun, S.; Geng, Y.; Zhang, X.; Zhou, T.; Wu, H.Z.; Chen, J.Q.; Yang, Z.X.; et al. Proton Magnetic Resonance Spectroscopy for Diagnosis of Non-Motor Symptoms in Parkinson’s Disease. Front. Neurol. 2022, 13, 594711. [Google Scholar] [CrossRef] [PubMed]
- Seraji-Bozorgzad, N.; Bao, F.; George, E.; Krstevska, S.; Gorden, V.; Chorostecki, J.; Santiago, C.; Zak, I.; Caon, C.; Khan, O. Longitudinal study of the substantia nigra in Parkinson disease: A high-field 1H-MR spectroscopy imaging study. Mov. Disord. 2015, 30, 1400–1404. [Google Scholar] [CrossRef]
- Shoeibi, A.; Verdipour, M.; Hoseini, A.; Moshfegh, M.; Olfati, N.; Layegh, P.; Dadgar-Moghadam, M.; Farzadfard, M.T.; Rezaeitalab, F.; Borji, N. Brain proton magnetic resonance spectroscopy in patients with Parkinson’s disease. Curr. J. Neurol. 2022, 21, 156–161. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Br. J. Manag. 2021, 372, n71. [Google Scholar] [CrossRef]
- Eriksen, M.B.; Frandsen, T.F. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: A systematic review. J. Med. Libr. Assoc. 2018, 106, 420–431. [Google Scholar] [CrossRef] [PubMed]
- Chagas, M.H.N.; Zuardi, A.W.; Tumas, V.; Pena-Pereira, M.A.; Sobreira, E.T.; Bergamaschi, M.M.; dos Santos, A.C.; Teixeira, A.L.; Hallak, J.E.C.; Crippa, J.A.S. Effects of cannabidiol in the treatment of patients with Parkinson’s disease: An exploratory double-blind trial. J. Psychopharmacol. 2014, 28, 1088–1098. [Google Scholar] [CrossRef] [PubMed]
- Clarke, C.E.; Lowry, M.; Horsman, A. Unchanged basal ganglia N-acetylaspartate and glutamate in idiopathic Parkinson’s disease measured by proton magnetic resonance spectroscopy. Mov. Disord. 1997, 12, 297–301. [Google Scholar] [CrossRef]
- Ciurleo, R.; Bonanno, L.; Di Lorenzo, G.; Bramanti, P.; Marino, S. Metabolic changes in de novo Parkinson’s disease after dopaminergic therapy: A proton magnetic resonance spectroscopy study. Neurosci. Lett. 2015, 599, 55–60. [Google Scholar] [CrossRef]
- Lucetti, C.; Del Dotto, P.; Gambaccini, G.; Ceravolo, R.; Logi, C.; Berti, C.; Rossi, G.; Bianchi, M.C.; Tosetti, M.; Murri, L.; et al. Influences of dopaminergic treatment on motor cortex in Parkinson disease: A MRI/MRS study. Mov. Disord. 2007, 22, 2170–2175. [Google Scholar] [CrossRef]
- Iuvone, T.; Esposito, G.; De Filippis, D.; Scuderi, C.; Steardo, L. Cannabidiol: A promising drug for neurodegenerative disorders? CNS Neurosci. Ther. 2009, 15, 65–75. [Google Scholar] [CrossRef]
- Ellis, C.M.; Lemmens, G.; Williams, S.C.; Simmons, A.; Dawson, J.; Leigh, P.N.; Chaudhuri, K.R. Changes in putamen N-acetylaspartate and choline ratios in untreated and levodopa-treated Parkinson’s disease: A proton magnetic resonance spectroscopy study. Neurology 1997, 49, 438–444. [Google Scholar] [CrossRef]
- Taylor-Robinson, S.D.; Turjanski, N.; Bhattacharya, S.; Seery, J.P.; Sargentoni, J.; Brooks, D.J.; Bryant, D.J.; Cox, I.J. A proton magnetic resonance spectroscopy study of the striatum and cerebral cortex in Parkinson’s disease. Metab. Brain Dis. 1999, 14, 45–55. [Google Scholar] [CrossRef]
- Lucetti, C.; Del Dotto, P.; Gambaccini, G.; Bernardini, S.; Bianchi, M.C.; Tosetti, M.; Bonuccelli, U. Proton magnetic resonance spectroscopy (1H-MRS) of motor cortex and basal ganglia in de novo Parkinson’s disease patients. Neurol. Sci. 2001, 22, 69–70. [Google Scholar] [CrossRef] [PubMed]
- Naoi, M.; Maruyama, W.; Yi, H.; Inaba, K.; Akao, Y.; Shamoto-Nagai, M. Mitochondria in neurodegenerative disorders: Regulation of the redox state and death signaling leading to neuronal death and survival. J. Neural Transm. 2009, 116, 1371–1381. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.L. A review of chemical issues in 1H NMR spectroscopy: N-acetyl-L-aspartate, creatine and choline. NMR Biomed. 1991, 4, 47–52. [Google Scholar] [CrossRef] [PubMed]
- De Graaf, A.A.; Deutz, N.E.; Bosman, D.K.; Chamuleau, R.A.; de Haan, J.G.; Bovee, W.M. The use of in vivo proton NMR to study the effects of hyperammonemia in the rat cerebral cortex. NMR Biomed. 1991, 4, 31–37. [Google Scholar] [CrossRef]

| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Quality Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mazuel et al. [13] | Yes | Yes | NR | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | NR | Good |
| Bonanno et al. [36] | No | NA | NA | No | Yes | Yes | No | NR | Yes | Yes | Yes | No | Yes | NA | Poor |
| Chagas et al. [56] | Yes | NR | NR | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | NR | Good |
| Clarke et al. [57] | No | NA | NA | No | NR | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | NA | Fair |
| Ciurleo et al. [58] | No | NA | NA | No | NR | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | NA | Fair |
| Lucetti et al. [59] | No | NA | NA | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | NA | Fair |
| Study | Population | Study Design | Study Aim | Drug | Metabolite (s) | Follow-Up Period (Baseline to Follow-Up MRS) | MRS Technique and VOI | Main Findings | Limits |
|---|---|---|---|---|---|---|---|---|---|
| Mazuel et al. [13] | 20 IPD patients; 20 age- and sex-matched HCs. | Randomized, blinded, permuted-block study. | To assess the neurochemical profile in the putamen of PD patients undergoing levodopa treatment (drug-on) or after withdrawal of levodopa medication (drug-off) compared with HCs to identify dopaminergic therapy–sensitive biomarkers of PD. | Levodopa (200 mg acute dose, Modopar). | tNAA tCr mI Glx | Twice at 1 week intervals, alternately in drug-off condition and in drug-on condition. | Single voxel, 3T scanner. Right and left putamen in axial, coronal and sagittal sections. | PD patients in drug-off condition showed significantly lower tNAA, tCr, and mI levels vs. HCs. After levodopa administration, tNAA and tCr increased to near-normal levels. No significant changes were observed in mI, Cho, or Glx between the two conditions. | Acute effect of levodopa, not representative of chronic therapy. Concomitant therapies (MAO-B, COMT inhibitors) potentially confounding. |
| Bonanno et al. [36] | 40 de novo PD patients (20 rasagiline, 20 selegiline); 40 age- and sex-matched HCs. | Longitudinal prospective controlled study. | To evaluate the effects of rasagiline and selegiline on neurometabolic profiles in the motor cortex of de novo PD patients. | MAO-B inhibitors: rasagiline (1 mg/day) and selegiline (10 mg/day). | NAA/Cr Cho/Cr | 12 months | Multi voxel, 3T scanner. Motor cortex including both hemispheres. | At baseline, PD patients had significantly lower NAA/Cr ratios than HCs. After 12 months of treatment with either rasagiline or selegiline, NAA/Cr significantly increased to values comparable with HCs. No significant changes were observed for Cho/Cr. | Biological fluctuations of neurometabolite concentrations over time, partly because of aging. |
| Chagas et al. [56] | 21 PD patients (3 groups of 7 subjects: placebo, CBD 75 mg, CBD 300 mg). | Randomized, double-blind, placebo-controlled exploratory trial. | To explore the effects of CBD on motor symptoms, quality of life, BDNF levels, and neurometabolic markers to evaluate potential neuroprotective effects (1H-MRS) in patients with PD. | Cannabidiol (CBD) 75 mg/day and CBD 300 mg/day. | NAA/Cr | 6 weeks | Single-voxel, 3T scanner. Bilateral basal ganglia (putamen). | No statistically significant changes in NAA/Cr ratios between the CBD and placebo groups at baseline and after 6 weeks. | Small sample size and short follow-up period (6 weeks). |
| Clarke et al. [57] | 5 patients with moderately severe IPD; 5 age-matched HCs. | Short-term pre-post controlled study. | To investigate neuronal loss in IPD by quantifying NAA, Cr, and Cho in the lentiform nucleus, and to assess changes in Glx levels inside the basal ganglia before and after acute dopaminergic stimulation. | Apomorphine (rapidly acting dopamine agonist), single subcutaneous dose. | Cho, Cr, NAA (absolute quantification) Glx/Cr | 10–15 min | Single-voxel, 1.5T scanner. Putamen and globus pallidus (lentiform nucleus) in the hemisphere contralateral to the most severely affected side. | No significant differences in striatal metabolite concentrations (NAA, Cho, Cr) or Glx/Cr ratio were observed between IPD patients and controls, nor before and after apomorphine administration. | Very small sample size. Post-treatment assessment performed shortly after drug administration (10–15 min), potentially inadequate to detect metabolic changes. |
| Ciurleo et al. [58] | 20 de novo drug-naïve PD patients; 15 age-matched HCs. | Longitudinal prospective controlled study. | To evaluate neurometabolic changes in the motor cortex of de novo PD patients before and after ropinirole treatment. | Ropinirole (dopamine agonist), 6 mg/day. | NAA/Cr NAA/Cho Cho/Cr | 10 months | Multi-voxel, 1.5T scanner. Corpus callous including white matter and mesial motor cortex of both hemispheres. | At baseline, PD patients showed decreased NAA/Cr and NAA/Cho, and increased Cho/Cr ratios vs. HCs. After 10 months of ropinirole therapy, NAA/Cr and NAA/Cho significantly increased. | Small sample size. Possible influence of disease progression on MRSI data at 10-month follow-up. Lack spectroscopic data on HCs at follow-up. |
| Lucetti et al. [59] | 11 de novo PD patients; 11 age-matched HCs. | Longitudinal prospective controlled study. | To investigate neurochemical and metabolic changes in the motor cortex of de novo PD patients before and after 6 months treatment with the dopamine agonist pergolide. | Pergolide (dopamine agonist), 1 mg three times daily. | Cho/Cr NAA/Cr mI/Cr | 6 months | Single-voxel, 1.5T scanner. Medial surface of the motor cortex including left and right cortical sides. | At baseline, PD patients showed reduced Cho/Cr and NAA/Cr ratios compared to controls. After 6 months of pergolide therapy, Cho/Cr significantly increased, indicating metabolic normalization; NAA/Cr also increased, though not significantly | VOI centered on the medial surface of the motor cortex, but possible inclusion of supplementary areas. No hemispheric separation in data analysis. Lack of CSF content measurement and correction, with potential MRS signal contamination. CSF alterations induced by pergolide treatment cannot be ruled out. Lack spectroscopy data on HCs at follow-up. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bonanno, L.; Caporlingua, M.; Castellano, J.; Quartarone, A.; Ciurleo, R. Using 1H-Magnetic Resonance Spectroscopy to Evaluate the Efficacy of Pharmacological Treatments in Parkinson’s Disease: A Systematic Review. Int. J. Mol. Sci. 2025, 26, 9351. https://doi.org/10.3390/ijms26199351
Bonanno L, Caporlingua M, Castellano J, Quartarone A, Ciurleo R. Using 1H-Magnetic Resonance Spectroscopy to Evaluate the Efficacy of Pharmacological Treatments in Parkinson’s Disease: A Systematic Review. International Journal of Molecular Sciences. 2025; 26(19):9351. https://doi.org/10.3390/ijms26199351
Chicago/Turabian StyleBonanno, Lilla, Miriana Caporlingua, Jole Castellano, Angelo Quartarone, and Rosella Ciurleo. 2025. "Using 1H-Magnetic Resonance Spectroscopy to Evaluate the Efficacy of Pharmacological Treatments in Parkinson’s Disease: A Systematic Review" International Journal of Molecular Sciences 26, no. 19: 9351. https://doi.org/10.3390/ijms26199351
APA StyleBonanno, L., Caporlingua, M., Castellano, J., Quartarone, A., & Ciurleo, R. (2025). Using 1H-Magnetic Resonance Spectroscopy to Evaluate the Efficacy of Pharmacological Treatments in Parkinson’s Disease: A Systematic Review. International Journal of Molecular Sciences, 26(19), 9351. https://doi.org/10.3390/ijms26199351







