Acetylcholinesterase as a Multifunctional Target in Amyloid-Driven Neurodegeneration: From Dual-Site Inhibitors to Anti-Agregation Strategies
Abstract
1. Introduction
2. Structural and Functional Characteristics of Acetylcholinesterase
3. Approved Acetylcholinesterase Inhibitors and Their Limitations
4. New Trends in AChE Pharmacophores
Comparison Between Dual-Site Inhibitors and Anti-Aggregation Strategies
| Feature | Dual-Site Inhibitors | Anti-Aggregation Strategies | References |
|---|---|---|---|
| Biological target | AChE (CAS + PAS) | Aβ peptides (monomers, oligomers, fibrils) | [55,104] |
| Mechanism of action |
|
| [103,104] |
| Representative classes of compounds |
|
| [103,105,106,107,108,109] |
| Therapeutic effect | Symptomatic improvement through cholinergic enhancement; disease-modifying effect by reducing Aβ aggregation | Primarily disease-modifying; reduces plaque load and toxic oligomers; limited immediate symptomatic benefit | [55,103,110] |
| Scope of activity | Targeting AChE-mediated pathways and partial Aβ aggregation | Targeting Aβ aggregation independently of enzymatic activity; some approaches also affect tau pathology | [55,102,103] |
| Limitations |
|
| [55,102,103] |
5. Experimental Techniques Driving Pharmacophore Validation
6. Challenges and Future Directions
7. Conclusions
Funding
Conflicts of Interest
Abbreviations
| ACh | Acetylcholine |
| AChE | Acetylcholinesterase |
| AD | Alzheimer’s Disease |
| ADME | Absorption, Distribution, Metabolism, and Excretion |
| AI | Artificial Intelligence |
| BACE-1 | Beta-site Amyloid Precursor Protein Cleaving Enzyme 1 |
| BBB | Blood–Brain Barrier |
| CAS | Catalytic Active Site |
| CNS | Central Nervous System |
| DTE | Dithienylethene |
| EMA | European Medicines Agency |
| FDA | U.S. Food and Drug Administration |
| GSK-3β | Glycogen Synthase Kinase 3 Beta |
| iPSC | Induced Pluripotent Stem Cell |
| ITC | Isothermal Titration Calorimetry |
| MAO-B | Monoamine Oxidase B |
| MTDLs | Multi-Target-Directed Ligands |
| OH | Oxyanion Hole |
| PAS | Peripheral Anionic Site |
| PDEs | Phosphodiesterases |
| SPR | Surface Plasmon Resonance |
References
- Martyn, J.A.; Fagerlund, M.J.; Eriksson, L.I. Basic principles of neuromuscular transmission. Anaesthesia 2009, 64, 1–9. [Google Scholar] [CrossRef]
- Huang, Q.; Liao, C.; Ge, F.; Ao, J.; Liu, T. Acetylcholine bidirectionally regulates learning and memory. J. Neurorestoratology 2022, 10, 100002. [Google Scholar] [CrossRef]
- Chen, Z.R.; Huang, J.B.; Yang, S.L.; Hong, F.F. Role of Cholinergic Signaling in Alzheimer’s Disease. Molecules 2022, 27, 1816. [Google Scholar] [CrossRef]
- Yamashita, K.I.; Uehara, T.; Taniwaki, Y.; Tobimatsu, S.; Kira, J.I. Long-Term Effect of Acetylcholinesterase Inhibitors on the Dorsal Attention Network of Alzheimer’s Disease Patients: A Pilot Study Using Resting-State Functional Magnetic Resonance Imaging. Front. Aging Neurosci. 2022, 14, 810206. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.Y.; Al Jerdi, S.; MacDonald, R.; Triggle, C.R. Alzheimer’s disease and its treatment-yesterday, today, and tomorrow-PubMed. Front. Pharmacol. 2024, 15, 1399121. [Google Scholar] [CrossRef]
- Grossberg, G.T. Cholinesterase Inhibitors for the Treatment of Alzheimer’s Disease: Getting On and Staying On. Curr. Ther. Res. Clin. Exp. 2003, 64, 216–235. [Google Scholar] [CrossRef]
- Marucci, G.; Buccioni, M.; Ben, D.D.; Lambertucci, C.; Volpini, R.; Amenta, F. Efficacy of acetylcholinesterase inhibitors in Alzheimer’s disease. Neuropharmacology 2021, 190, 108352. [Google Scholar] [CrossRef]
- Ruangritchankul, S.; Chantharit, P.; Srisuma, S.; Gray, L.C. Adverse Drug Reactions of Acetylcholinesterase Inhibitors in Older People Living with Dementia: A Comprehensive Literature Review. Ther. Clin. Risk Manag. 2021, 17, 927–949. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhang, Y.; Wang, J.; Xia, Y.; Zhang, J.; Chen, L. Recent advances in Alzheimer’s disease: Mechanisms, clinical trials and new drug development strategies. Signal Transduct. Target. Ther. 2024, 9, 211. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.A.; Khan, F.; Song, M. Alleviation of Neurological Disorders by Targeting Neurodegenerative-Associated Enzymes: Natural and Synthetic Molecules. Int. J. Mol. Sci. 2025, 26, 4707. [Google Scholar] [CrossRef]
- Zhao, X.; Hu, Q.; Wang, X.; Li, C.; Chen, X.; Zhao, D.; Qiu, Y.; Xu, H.; Wang, J.; Ren, L.; et al. Dual-target inhibitors based on acetylcholinesterase: Novel agents for Alzheimer’s disease. Eur. J. Med. Chem. 2024, 279, 116810. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, H.; Chen, H.Z. AChE Inhibition-based Multi-target-directed Ligands, a Novel Pharmacological Approach for the Symptomatic and Disease-modifying Therapy of Alzheimer’s Disease. Curr. Neuropharmacol. 2016, 14, 364–375. [Google Scholar] [CrossRef]
- Azam, U.; Naseer, M.M.; Rochais, C. Analysis of skeletal diversity of multi-target directed ligands (MTDLs) targeting Alzheimer’s disease. Eur. J. Med. Chem. 2025, 286, 117277. [Google Scholar] [CrossRef]
- Colletier, J.P.; Fournier, D.; Greenblatt, H.M.; Stojan, J.; Sussman, J.L.; Zaccai, G.; Silman, I.; Weik, M. Structural insights into substrate traffic and inhibition in acetylcholinesterase. EMBO J. 2006, 25, 2746–2756. [Google Scholar] [CrossRef] [PubMed]
- Luque, F.J.; Muñoz-Torrero, D. Acetylcholinesterase: A Versatile Template to Coin Potent Modulators of Multiple Therapeutic Targets. Acc. Chem. Res. 2024, 57, 450–467. [Google Scholar] [CrossRef]
- Chafer-Dolz, B.; Cecilia, J.M.; Imbernón, B.; Núñez-Delicado, E.; Casaña-Giner, V.; Cerón-Carrasco, J.P. Discovery of novel acetylcholinesterase inhibitors through AI-powered structure prediction and high-performance computing-enhanced virtual screening. RSC Adv. 2025, 15, 4262–4273. [Google Scholar] [CrossRef] [PubMed]
- Vijayan, R.S.K.; Kihlberg, J.; Cross, J.B.; Poongavanam, V. Enhancing preclinical drug discovery with artificial intelligence. Drug Discov. Today 2022, 27, 967–984. [Google Scholar] [CrossRef]
- Sobha, A.; Ganapathy, A.; Mohan, S.; Madhusoodanan, N.; Babysulochana, A.D.; Alaganandan, K.; Somappa, S.B. Novel small molecule-based acetylcholinesterase (AChE) inhibitors: From biological perspective to recent developments. Eur. J. Med. Chem. Rep. 2024, 12, 100237. [Google Scholar] [CrossRef]
- Žužek, M.C. Advances in Cholinesterase Inhibitor Research—An Overview of Preclinical Studies of Selected Organoruthenium(II) Complexes. Int. J. Mol. Sci. 2024, 25, 9049. [Google Scholar] [CrossRef]
- de Almeida, R.B.M.; Barbosa, D.B.; Bomfim, M.R.D.; Amparo, J.A.O.; Andrade, B.S.; Costa, S.L.; Campos, J.M.; Cruz, J.N.; Santos, C.B.R.; Leite, F.H.A.; et al. Identification of a Novel Dual Inhibitor of Acetylcholinesterase and Butyrylcholinesterase: In Vitro and In Silico Studies. Pharmaceuticals 2023, 16, 95. [Google Scholar] [CrossRef]
- Pourtaher, H.; Hasaninejad, A.; Zare, S.; Tanideh, N.; Iraji, A. The anti-Alzheimer potential of novel spiroindolin-1,2-diazepine derivatives as targeted cholinesterase inhibitors with modified substituents. Sci. Rep. 2023, 13, 11952. [Google Scholar] [CrossRef]
- Poggialini, F.; Governa, P.; Vagaggini, C.; Maramai, S.; Lamponi, S.; Mugnaini, C.; Brizzi, A.; Purgatorio, R.; de Candia, M.; Catto, M.; et al. Light-mediated activation/deactivation control and in vitro ADME-Tox profiling of a donepezil-like Dual AChE/MAO-B Inhibitor. Eur. J. Pharm. Sci. 2025, 209, 107066. [Google Scholar] [CrossRef] [PubMed]
- Rossi, M.; Freschi, M.; Nascente, L.d.C.; Salerno, A.; Teixeira, S.d.M.V.; Nachon, F.; Chantegreil, F.; Soukup, O.; Prchal, L.; Malaguti, M.; et al. Sustainable Drug Discovery of Multi-Target-Directed Ligands for Alzheimer’s Disease. J. Med. Chem. 2021, 64, 4972–4990. [Google Scholar] [CrossRef]
- Huang, L.K.; Kuan, Y.C.; Lin, H.W.; Hu, C.J. Clinical trials of new drugs for Alzheimer disease: A 2020–2023 update. J. Biomed. Sci. 2023, 30, 83. [Google Scholar] [CrossRef]
- Cummings, J.; Zhou, Y.; Lee, G.; Zhong, K.; Fonseca, J.; Cheng, F. Alzheimer’s disease drug development pipeline: 2024. Alzheimer’s Dement. Transl. Res. Clin. Interv. 2024, 10, e12465. [Google Scholar] [CrossRef]
- Romano, J.D.; Tatonetti, N.P. Informatics and Computational Methods in Natural Product Drug Discovery: A Review and Perspectives. Front. Genet. 2019, 10, 368. [Google Scholar] [CrossRef]
- Atanasova, M.; Dimitrov, I.; Ivanov, S.; Georgiev, B.; Berkov, S.; Zheleva-Dimitrova, D.; Doytchinova, I. Virtual Screening and Hit Selection of Natural Compounds as Acetylcholinesterase Inhibitors. Molecules 2022, 27, 3139. [Google Scholar] [CrossRef]
- Čolović, M.B.; Krstić, D.Z.; Lazarević-Pašti, T.D.; Bondžić, A.M.; Vasić, V.M. Acetylcholinesterase Inhibitors: Pharmacology and Toxicology. Curr. Neuropharmacol. 2013, 11, 315–335. [Google Scholar] [CrossRef]
- Silman, I.; Sussman, J.L. Acetylcholinesterase: How is structure related to function? Chem.-Biol. Interact. 2008, 175, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Dvir, H.; Silman, I.; Harel, M.; Rosenberry, T.L.; Sussman, J.L. Acetylcholinesterase: From 3D structure to function. Chem.-Biol. Interact. 2010, 187, 10–22. [Google Scholar] [CrossRef] [PubMed]
- Thapa, S.; Lv, M.; Xu, H. Acetylcholinesterase: A Primary Target for Drugs and Insecticides. Mini Rev. Med. Chem. 2017, 17, 1665–1676. [Google Scholar] [CrossRef]
- Barak, D.; Kronman, C.; Ordentlich, A.; Ariel, N.; Bromberg, A.; Marcus, D.; Lazar, A.; Velan, B.; Shafferman, A. Acetylcholinesterase peripheral anionic site degeneracy conferred by amino acid arrays sharing a common core. J. Biol. Chem. 1994, 269, 6296–6305. [Google Scholar] [CrossRef] [PubMed]
- Bourne, Y.; Kolb, H.C.; Radić, Z.; Sharpless, K.B.; Taylor, P.; Marchot, P. Freeze-frame inhibitor captures acetylcholinesterase in a unique conformation. Proc. Natl. Acad. Sci. USA 2004, 101, 1449–1454. [Google Scholar] [CrossRef] [PubMed]
- Gao, D.; Zhan, C.G. Modeling effects of oxyanion hole on the ester hydrolysis catalyzed by human cholinesterases. J. Phys. Chem. 2005, 109, 23070–23076. [Google Scholar] [CrossRef] [PubMed]
- Axelsen, P.H.; Harel, M.; Silman, I.; Sussman, J.L. Structure and dynamics of the active site gorge of acetylcholinesterase: Synergistic use of molecular dynamics simulation and X-ray crystallography. Protein Sci. A Publ. Protein Soc. 1994, 3, 188–197. [Google Scholar] [CrossRef]
- Bourne, Y.; Radic, Z.; Sulzenbacher, G.; Kim, E.; Taylor, P.; Marchot, P. Substrate and product trafficking through the active center gorge of acetylcholinesterase analyzed by crystallography and equilibrium binding. J. Biol. Chem. 2006, 281, 29256–29267. [Google Scholar] [CrossRef]
- Soreq, H.; Seidman, S. Acetylcholinesterase—new roles for an old actor. Nat. Rev. Neurosci. 2001, 2, 294–302. [Google Scholar] [CrossRef]
- FDA Approved Drug Products. Available online: http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm (accessed on 1 September 2025).
- EMA Approved Drug Products. Available online: https://www.ema.europa.eu/en/medicines (accessed on 1 September 2025).
- National Institute for Health and Care Excellence: Guidelines. In Dementia: Assessment, Management and Support for People Living with Dementia and Their Carers; National Institute for Health and Care Excellence (NICE): London, UK, 2018.
- Tan, C.C.; Yu, J.T.; Wang, H.F.; Tan, M.S.; Meng, X.F.; Wang, C.; Jiang, T.; Zhu, X.C.; Tan, L. Efficacy and safety of donepezil, galantamine, rivastigmine, and memantine for the treatment of Alzheimer’s disease: A systematic review and meta-analysis. J. Alzheimer’s Dis. 2014, 41, 615–631. [Google Scholar] [CrossRef]
- Di Santo, S.G.; Prinelli, F.; Adorni, F.; Caltagirone, C.; Musicco, M. A meta-analysis of the efficacy of donepezil, rivastigmine, galantamine, and memantine in relation to severity of Alzheimer’s disease. J. Alzheimer’s Dis. 2013, 35, 349–361. [Google Scholar] [CrossRef]
- Gill, S.S.; Anderson, G.M.; Fischer, H.D.; Bell, C.M.; Li, P.; Normand, S.-L.T.; Rochon, P.A. Syncope and its consequences in patients with dementia receiving cholinesterase inhibitors: A population-based cohort study. Arch. Intern. Med. 2009, 169, 867–873. [Google Scholar] [CrossRef]
- Miculas, D.C.; Negru, P.A.; Bungau, S.G.; Behl, T.; Hassan, S.S.u.; Tit, D.M. Pharmacotherapy Evolution in Alzheimer’s Disease: Current Framework and Relevant Directions. Cells 2022, 12, 131. [Google Scholar] [CrossRef]
- Agis-Torres, A.; Sölhuber, M.; Fernandez, M.; Sanchez-Montero, J. Multi-Target-Directed Ligands and other Therapeutic Strategies in the Search of a Real Solution for Alzheimer’s Disease. Curr. Neuropharmacol. 2014, 12, 2–36. [Google Scholar] [CrossRef]
- Niazi, S.K.; Magoola, M.; Mariam, Z. Innovative Therapeutic Strategies in Alzheimer’s Disease: A Synergistic Approach to Neurodegenerative Disorders. Pharmaceuticals 2024, 17, 741. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Gupta, V.; Sharma, S. Donepezil. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2025. [Google Scholar]
- Kalola, U.K.; Patel, P.; Nguyen, H. Galantamine. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2025. [Google Scholar]
- Patel, P.H.; Gupta, V. Rivastigmine. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2025. [Google Scholar]
- Thangeswaran, D.; Shamsuddin, S.; Balakrishnan, V. A comprehensive review on the progress and challenges of tetrahydroisoquinoline derivatives as a promising therapeutic agent to treat Alzheimer’s disease. Heliyon 2024, 10, e30788. [Google Scholar] [CrossRef] [PubMed]
- Codony, S.; Pont, C.; Griñán-Ferré, C.; Pede-Mattatelli, A.D.; Calvó-Tusell, C.; Feixas, F.; Osuna, S.; Jarné-Ferrer, J.; Naldi, M.; Bartolini, M.; et al. Discovery and In Vivo Proof of Concept of a Highly Potent Dual Inhibitor of Soluble Epoxide Hydrolase and Acetylcholinesterase for the Treatment of Alzheimer’s Disease. J. Med. Chem. 2022, 65, 4909–4925. [Google Scholar] [CrossRef]
- Zagórska, A.; Jaromin, A. Perspectives for New and More Efficient Multifunctional Ligands for Alzheimer′s Disease Therapy. Molecules 2020, 25, 3337. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Mahajan, A.; Ambatwar, R.; Khatik, G.L. Recent Advancements in the Treatment of Alzheimer’s Disease: A Multitarget-directed Ligand Approach. Curr. Med. Chem. 2024, 31, 6032–6062. [Google Scholar] [CrossRef]
- Chen, R.; Li, X.; Chen, H.; Wang, K.; Xue, T.; Mi, J.; Ban, Y.; Zhu, G.; Zhou, Y.; Dong, W.; et al. Development of the “hidden” multi-target-directed ligands by AChE/BuChE for the treatment of Alzheimer’s disease. Eur. J. Med. Chem. 2023, 251, 115253. [Google Scholar] [CrossRef]
- Zueva, I.; Dias, J.; Lushchekina, S.; Semenov, V.; Mukhamedyarov, M.; Pashirova, T.; Babaev, V.; Nachon, F.; Petrova, N.; Nurullin, L.; et al. New evidence for dual binding site inhibitors of acetylcholinesterase as improved drugs for treatment of Alzheimer’s disease. Neuropharmacology 2019, 155, 131–141. [Google Scholar] [CrossRef]
- Alvarez, A.; Opazo, C.; Alarcón, R.; Garrido, J.; Inestrosa, N.C. Acetylcholinesterase promotes the aggregation of amyloid-β-peptide fragments by forming a complex with the growing fibrils. J. Mol. Biol. 1997, 272, 348–361. [Google Scholar] [CrossRef]
- Kumar, N.; Kumar, V.; Anand, P.; Kumar, V.; Dwivedi, A.R.; Kumar, V. Advancements in the development of multi-target directed ligands for the treatment of Alzheimer’s disease. Bioorganic Med. Chem. 2022, 61, 116742. [Google Scholar] [CrossRef]
- Obaid, R.J.; Naeem, N.; Mughal, E.U.; Al-Rooqi, M.M.; Sadiq, A.; Jassas, R.S.; Moussa, Z.; Ahmed, S.A. Inhibitory potential of nitrogen, oxygen and sulfur containing heterocyclic scaffolds against acetylcholinesterase and butyrylcholinesterase. RSC Adv. 2022, 12, 19764–19855. [Google Scholar] [CrossRef]
- Jiang, C.S.; Ge, Y.X.; Cheng, Z.Q.; Song, J.L.; Wang, Y.Y.; Zhu, K.; Zhang, H. Discovery of new multifunctional selective acetylcholinesterase inhibitors: Structure-based virtual screening and biological evaluation. J. Comput.-Aided Mol. Des. 2019, 33, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Rana, M.; Pareek, A.; Bhardwaj, S.; Arya, G.; Nimesh, S.; Arya, H.; Bhatt, T.K.; Yaragorla, S.; Sharma, A.K. Aryldiazoquinoline based multifunctional small molecules for modulating Aβ42 aggregation and cholinesterase activity related to Alzheimer’s disease. RSC Adv. 2020, 10, 28827–28837. [Google Scholar] [CrossRef]
- Zou, D.; Liu, R.; Lv, Y.; Guo, J.; Zhang, C.; Xie, Y. Latest advances in dual inhibitors of acetylcholinesterase and monoamine oxidase B against Alzheimer’s disease. J. Enzym. Inhib. Med. Chem. 2023, 38, 2270781. [Google Scholar] [CrossRef]
- Banoo, R.; Nuthakki, V.K.; Wadje, B.N.; Sharma, A.; Bharate, S.B. Design, synthesis, and pharmacological evaluation of indole-piperidine amides as Blood−brain barrier permeable dual cholinesterase and β-secretase inhibitors. Eur. J. Med. Chem. 2024, 266, 116131. [Google Scholar] [CrossRef]
- Yao, H.; Uras, G.; Zhang, P.; Xu, S.; Yin, Y.; Liu, J.; Qin, S.; Li, X.; Allen, S.; Bai, R.; et al. Discovery of Novel Tacrine–Pyrimidone Hybrids as Potent Dual AChE/GSK-3 Inhibitors for the Treatment of Alzheimer’s Disease. J. Med. Chem. 2021, 64, 7483–7506. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Huang, Y.D.; Pan, T.; Zhang, T.; Su, T.; Li, X.; Luo, H.B.; Huang, L. Design, Synthesis, and Biological Evaluation of Dual-Target Inhibitors of Acetylcholinesterase (AChE) and Phosphodiesterase 9A (PDE9A) for the Treatment of Alzheimer’s Disease. ACS Chem. Neurosci. 2019, 10, 537–551. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Liu, L.; Zheng, L.; Feng, K.W.; Wang, H.T.; Xu, J.P.; Zhou, Z.Z. Discovery of novel 2,3-dihydro-1H-inden-1-ones as dual PDE4/AChE inhibitors with more potency against neuroinflammation for the treatment of Alzheimer’s disease. Eur. J. Med. Chem. 2022, 238, 114503. [Google Scholar] [CrossRef]
- Asim, A.; Jastrzębski, M.K.; Kaczor, A.A. Dual Inhibitors of Acetylcholinesterase and Monoamine Oxidase-B for the Treatment of Alzheimer’s Disease. Molecules 2025, 30, 2975. [Google Scholar] [CrossRef]
- Mohsin, N.u.A.; Ahmad, M. Donepezil: A review of the recent structural modifications and their impact on anti-Alzheimer activity. Braz. J. Pharm. Sci. 2020, 56, e18325. [Google Scholar] [CrossRef]
- Gucký, A.; Hamuľaková, S. Targeting Biometals in Alzheimer’s Disease with Metal Chelating Agents Including Coumarin Derivatives. CNS Drugs 2024, 38, 507–532. [Google Scholar] [CrossRef]
- Leuci, R.; Brunetti, L.; Laghezza, A.; Loiodice, F.; Tortorella, P.; Piemontese, L. Importance of Biometals as Targets in Medicinal Chemistry: An Overview about the Role of Zinc (II) Chelating Agents. Appl. Sci. 2020, 10, 4118. [Google Scholar] [CrossRef]
- Sharma, A.; Pachauri, V.; Flora, S.J.S. Advances in Multi-Functional Ligands and the Need for Metal-Related Pharmacology for the Management of Alzheimer Disease. Front. Pharmacol. 2018, 9, 1247. [Google Scholar] [CrossRef]
- Kozlowski, H.; Luczkowski, M.; Remelli, M.; Valensin, D. Copper, zinc and iron in neurodegenerative diseases (Alzheimer’s, Parkinson’s and prion diseases). Coord. Chem. Rev. 2012, 256, 2129–2141. [Google Scholar] [CrossRef]
- Krasnovskaya, O.; Spector, D.; Zlobin, A.; Pavlov, K.; Gorelkin, P.; Erofeev, A.; Beloglazkina, E.; Majouga, A. Metals in Imaging of Alzheimer’s Disease. Int. J. Mol. Sci. 2020, 21, 9190. [Google Scholar] [CrossRef] [PubMed]
- Chaves, S.; Piemontese, L.; Hiremathad, A.; Santos, M.A. Hydroxypyridinone Derivatives: A Fascinating Class of Chelators with Therapeutic Applications-An Update. Curr. Med. Chem. 2018, 25, 97–112. [Google Scholar] [CrossRef]
- Rawat, P.; Sehar, U.; Bisht, J.; Selman, A.; Culberson, J.; Reddy, P.H. Phosphorylated Tau in Alzheimer’s Disease and Other Tauopathies. Int. J. Mol. Sci. 2022, 23, 12841. [Google Scholar] [CrossRef]
- Ivanov, S.M.; Atanasova, M.; Dimitrov, I.; Doytchinova, I.A. Cellular polyamines condense hyperphosphorylated Tau, triggering Alzheimer’s disease. Sci. Rep. 2020, 10, 10098. [Google Scholar] [CrossRef] [PubMed]
- Natale, G.D.; Sabatino, G.; Sciacca, M.F.M.; Tosto, R.; Milardi, D.; Pappalardo, G. Aβ and Tau Interact with Metal Ions, Lipid Membranes and Peptide-Based Amyloid Inhibitors: Are These Common Features Relevant in Alzheimer’s Disease? Molecules 2022, 27, 5066. [Google Scholar] [CrossRef] [PubMed]
- Kumar, H.M.S.; Herrmann, L.; Tsogoeva, S.B. Structural hybridization as a facile approach to new drug candidates. Bioorganic Med. Chem. Lett. 2020, 30, 127514. [Google Scholar] [CrossRef]
- Islam, F.; Khadija, J.F.; Harun-Or-Rashid, M.; Rahaman, M.S.; Nafady, M.H.; Islam, M.R.; Akter, A.; Emran, T.B.; Wilairatana, P.; Mubarak, M.S. Bioactive Compounds and Their Derivatives: An Insight into Prospective Phytotherapeutic Approach against Alzheimer’s Disease. Oxidative Med. Cell. Longev. 2022, 2022, 5100904. [Google Scholar] [CrossRef]
- Yang, H.; Zeng, F.; Luo, Y.; Zheng, C.; Ran, C.; Yang, J. Curcumin Scaffold as a Multifunctional Tool for Alzheimer’s Disease Research-PubMed. Molecules 2022, 27, 3879. [Google Scholar] [CrossRef]
- Roy, A.; Khan, A.; Ahmad, I.; Alghamdi, S.; Rajab, B.S.; Babalghith, A.O.; Alshahrani, M.Y.; Islam, S.; Islam, M.R. Flavonoids a Bioactive Compound from Medicinal Plants and Its Therapeutic Applications. BioMed Res. Int. 2022, 2022, 5445291. [Google Scholar] [CrossRef] [PubMed]
- Chaachouay, N.; Zidane, L.; Chaachouay, N.; Zidane, L. Plant-Derived Natural Products: A Source for Drug Discovery and Development. Drugs Drug Candidates 2024, 3, 184–207. [Google Scholar] [CrossRef]
- Cichon, N.; Grabowska, W.; Gorniak, L.; Stela, M.; Harmata, P.; Ceremuga, M.; Bijak, M. Mechanistic and Therapeutic Insights into Flavonoid-Based Inhibition of Acetylcholinesterase: Implications for Neurodegenerative Diseases. Nutrients 2024, 17, 78. [Google Scholar] [CrossRef]
- Huang, W.; Wang, Y.; Tian, W.; Cui, X.; Tu, P.; Li, J.; Shi, S.; Liu, X. Biosynthesis Investigations of Terpenoid, Alkaloid, and Flavonoid Antimicrobial Agents Derived from Medicinal Plants. Antibiotics 2022, 11, 1380. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Fang, L.; Zhang, H.; Gou, S.; Chen, L. Design, synthesis and biological evaluation of multifunctional tacrine-curcumin hybrids as new cholinesterase inhibitors with metal ions-chelating and neuroprotective property. Bioorganic Med. Chem. 2017, 25, 2387–2398. [Google Scholar] [CrossRef]
- Zang, W.B.; Wei, H.L.; Zhang, W.W.; Ma, W.; Li, J.; Yao, Y. Curcumin hybrid molecules for the treatment of Alzheimer’s disease: Structure and pharmacological activities. Eur. J. Med. Chem. 2024, 265, 116070. [Google Scholar] [CrossRef]
- Stavrakov, G.; Philipova, I.; Lukarski, A.; Atanasova, M.; Zheleva, D.; Zhivkova, Z.D.; Ivanov, S.; Atanasova, T.; Konstantinov, S.; Doytchinova, I. Galantamine-Curcumin Hybrids as Dual-Site Binding Acetylcholinesterase Inhibitors. Molecules 2020, 25, 3341. [Google Scholar] [CrossRef]
- Singh, Y.P.; Prasad, S.; Kumar, H. Comprehensive Analysis on Galantamine Based Hybrids for the Management of Alzheimer’s Disease. Chem. Biol. Drug Des. 2024, 104, e70004. [Google Scholar] [CrossRef]
- Simeonova, R.; Zheleva, D.; Valkova, I.; Stavrakov, G.; Philipova, I.; Atanasova, M.; Doytchinova, I. A Novel Galantamine-Curcumin Hybrid as a Potential Multi-Target Agent against Neurodegenerative Disorders. Molecules 2021, 26, 1865. [Google Scholar] [CrossRef] [PubMed]
- Jana, S.; Mandlekar, S.; Marathe, P. Prodrug design to improve pharmacokinetic and drug delivery properties: Challenges to the discovery scientists. Curr. Med. Chem. 2010, 17, 3874–3908. [Google Scholar] [CrossRef]
- Rautio, J.; Kumpulainen, H.; Heimbach, T.; Oliyai, R.; Oh, D.; Järvinen, T.; Savolainen, J. Prodrugs: Design and clinical applications. Nat. Rev. Drug Discov. 2008, 7, 255–270. [Google Scholar] [CrossRef] [PubMed]
- Choudhary, D.; Goykar, H.; Kalyane, D.; Sreeharsha, N.; Tekade, R.K. Prodrug design for improving the biopharmaceutical properties of therapeutic drugs. In The Future of Pharmaceutical Product Development and Research; Elsevier: Amsterdam, The Netherlands, 2020; pp. 179–226. [Google Scholar] [CrossRef]
- Jornada, D.H.; Fernandes, G.F.d.S.; Chiba, D.E.; Melo, T.R.F.d.; Santos, J.L.d.; Chung, M.C. The Prodrug Approach: A Successful Tool for Improving Drug Solubility. Molecules 2016, 21, 42. [Google Scholar] [CrossRef] [PubMed]
- Lillethorup, I.A.; Hemmingsen, A.V.; Qvortrup, K. Prodrugs and their activation mechanisms for brain drug delivery. RSC Med. Chem. 2025, 16, 1037–1048. [Google Scholar] [CrossRef]
- Zeiadeh, I.; Najjar, A.; Karaman, R. Strategies for Enhancing the Permeation of CNS-Active Drugs through the Blood-Brain Barrier: A Review. Molecules 2018, 23, 1289. [Google Scholar] [CrossRef]
- Kobauri, P.; Dekker, F.J.; Szymanski, W.; Feringa, B.L. Rational Design in Photopharmacology with Molecular Photoswitches. Angew. Chem. Int. Ed. 2023, 62, e202300681. [Google Scholar] [CrossRef]
- Scheiner, M.; Sink, A.; Spatz, P.; Endres, E.; Decker, M. Photopharmacology on Acetylcholinesterase: Novel Photoswitchable Inhibitors with Improved Pharmacological Profiles. ChemPhotoChem 2020, 5, 149–159. [Google Scholar] [CrossRef]
- Chen, X.; Wehle, S.; Kuzmanovic, N.; Merget, B.; Holzgrabe, U.; König, B.; Sotriffer, C.A.; Decker, M. Acetylcholinesterase Inhibitors with Photoswitchable Inhibition of β-Amyloid Aggregation. ACS Chem. Neurosci. 2014, 5, 377–389. [Google Scholar] [CrossRef]
- Rehman, A.U.; Li, M.; Wu, B.; Ali, Y.; Rasheed, S.; Shaheen, S.; Liu, X.; Luo, R.; Zhang, J. Role of artificial intelligence in revolutionizing drug discovery. Fundam. Res. 2025, 5, 1273–1287. [Google Scholar] [CrossRef]
- Reynoso-García, M.F.; Nicolás-Álvarez, D.E.; Tenorio-Barajas, A.Y.; Reyes-Chaparro, A. Structural Bioinformatics Applied to Acetylcholinesterase Enzyme Inhibition. Int. J. Mol. Sci. 2025, 26, 3781. [Google Scholar] [CrossRef] [PubMed]
- Gangwal, A.; Lavecchia, A. Artificial Intelligence in Natural Product Drug Discovery: Current Applications and Future Perspectives. J. Med. Chem. 2025, 68, 3948–3969. [Google Scholar] [CrossRef] [PubMed]
- Cai, Z.; Zhang, G.; Zhang, X.; Liu, Y.; Fu, X. Current insights into computer-aided immunotherapeutic design strategies. Int. J. Immunopathol. Pharmacol. 2015, 28, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.; Lee, J.; Ahn, B.; Han, J.; Lim, M.H. Multi-target-directed therapeutic strategies for Alzheimer’s disease: Controlling amyloid-β aggregation, metal ion homeostasis, and enzyme inhibition. Chem. Sci. 2025, 16, 2105–2135. [Google Scholar] [CrossRef]
- Giorgetti, S.; Greco, C.; Tortora, P.; Aprile, F.A. Targeting Amyloid Aggregation: An Overview of Strategies and Mechanisms. Int. J. Mol. Sci. 2018, 19, 2677. [Google Scholar] [CrossRef]
- Niu, Z.; Gui, X.; Feng, S.; Reif, B. Aggregation Mechanisms and Molecular Structures of Amyloid-β in Alzheimer’s Disease. Chem.–A Eur. J. 2024, 30, e202400277. [Google Scholar] [CrossRef] [PubMed]
- Makhaeva, G.F.; Kovaleva, N.V.; Rudakova, E.V.; Boltneva, N.P.; Lushchekina, S.V.; Astakhova, T.Y.; Timokhina, E.N.; Serebryakova, O.G.; Shchepochkin, A.V.; Averkov, M.A.; et al. Derivatives of 9-phosphorylated acridine as butyrylcholinesterase inhibitors with antioxidant activity and the ability to inhibit β-amyloid self-aggregation: Potential therapeutic agents for Alzheimer’s disease. Front. Pharmacol. 2023, 14, 1219980. [Google Scholar] [CrossRef]
- Ţînţaş, M.L.; Gembus, V.; Alix, F.; Barré, A.; Coadou, G.; Truong, L.; Sebban, M.; Papamicaël, C.; Oulyadi, H.; Levacher, V. Rational design of carbamate-based dual binding site and central AChE inhibitors by a “biooxidisable” prodrug approach: Synthesis, in vitro evaluation and docking studies. Eur. J. Med. Chem. 2018, 155, 171–182. [Google Scholar] [CrossRef]
- Szałaj, N.; Bajda, M.; Dudek, K.; Brus, B.; Gobec, S.; Malawska, B. Multiple Ligands Targeting Cholinesterases and β-Amyloid: Synthesis, Biological Evaluation of Heterodimeric Compounds with Benzylamine Pharmacophore. Arch. Pharm. 2015, 348, 556–563. [Google Scholar] [CrossRef]
- Sun, Q.; Peng, D.Y.; Yang, S.G.; Zhu, X.L.; Yang, W.C.; Yang, G.F. Syntheses of coumarin–tacrine hybrids as dual-site acetylcholinesterase inhibitors and their activity against butylcholinesterase, Aβ aggregation, and β-secretase. Bioorganic Med. Chem. 2014, 22, 4784–4791. [Google Scholar] [CrossRef]
- Gupta, S.; Mohan, C.G. Dual Binding Site and Selective Acetylcholinesterase Inhibitors Derived from Integrated Pharmacophore Models and Sequential Virtual Screening. BioMed Res. Int. 2014, 2014, 291214. [Google Scholar] [CrossRef]
- Martins, M.M.; Branco, P.S.; Ferreira, L.M. Enhancing the Therapeutic Effect in Alzheimer’s Disease Drugs: The role of Polypharmacology and Cholinesterase inhibitors. ChemistrySelect 2023, 8, e202300461. [Google Scholar] [CrossRef]
- Carvalho, A.L.; Trincão, J.; Romão, M.J. X-ray crystallography in drug discovery. In Methods in Molecular Biology; Humana Press: Totowa, NJ, USA, 2009; Volume 572, pp. 31–56. [Google Scholar] [CrossRef]
- Bijak, V.; Szczygiel, M.; Lenkiewicz, J.; Gucwa, M.; Cooper, D.R.; Murzyn, K.; Minor, W. The current role and evolution of X-ray crystallography in drug discovery and development. Expert Opin. Drug Discov. 2023, 18, 1221–1230. [Google Scholar] [CrossRef] [PubMed]
- Aitipamula, S.; Vangala, V.R. X-Ray Crystallography and its Role in Understanding the Physicochemical Properties of Pharmaceutical Cocrystals. J. Indian Inst. Sci. 2017, 97, 227–243. [Google Scholar] [CrossRef]
- Drie, J.H.V.; Tong, L. Cryo-EM as a powerful tool for drug discovery. Bioorganic Med. Chem. Lett. 2020, 30, 127524. [Google Scholar] [CrossRef]
- Leung, M.R.; Zeev-Ben-Mordehai, T. Cryo-electron microscopy of cholinesterases, present and future. J. Neurochem. 2020, 158, 1236–1243. [Google Scholar] [CrossRef]
- Olaru, A.; Bala, C.; Jaffrezic-Renault, N.; Aboul-Enein, H.Y. Surface plasmon resonance (SPR) biosensors in pharmaceutical analysis. Crit. Rev. Anal. Chem. 2015, 45, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Acharya, B.; Behera, A.; Behera, S. Optimizing drug discovery: Surface plasmon resonance techniques and their multifaceted applications. Chem. Phys. Impact 2024, 8, 100414. [Google Scholar] [CrossRef]
- Lima Cavalcanti, I.D.; Xavier Junior, F.H.; Santos Magalhães, N.S.; Lira Nogueira, M.C.B. Isothermal titration calorimetry (ITC) as a promising tool in pharmaceutical nanotechnology. Int. J. Pharm. 2023, 641, 123063. [Google Scholar] [CrossRef]
- Ward, W.H.; Holdgate, G.A. 7 Isothermal titration calorimetry in drug discovery. Prog. Med. Chem. 2001, 38, 309–376. [Google Scholar] [CrossRef]
- Upadhyay, V.; Lucas, A.; Patrick, C.; Mallela, K.M.G. Isothermal titration calorimetry and surface plasmon resonance methods to probe protein-protein interactions. Methods 2024, 225, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Siavashy, S.; Soltani, M.; Rahimi, S.; Hosseinali, M.; Guilandokht, Z.; Raahemifar, K. Recent advancements in microfluidic-based biosensors for detection of genes and proteins: Applications and techniques. Biosens. Bioelectron. X 2024, 19, 100489. [Google Scholar] [CrossRef]
- Maged, A.; Abdelbaset, R.; Mahmoud, A.A.; Elkasabgy, N.A. Merits and advances of microfluidics in the pharmaceutical field: Design technologies and future prospects. Drug Deliv. 2022, 29, 1549–1570. [Google Scholar] [CrossRef]
- Ross, J.A.; Mandenius, C.F. Cell-Based Assays Using Derived Human-Induced Pluripotent Cells in Drug Discovery and Development. In Methods in Molecular Biology; Humana: New York, NY, USA, 2025; Volume 2924, pp. 1–14. [Google Scholar] [CrossRef]
- Cerneckis, J.; Cai, H.; Shi, Y. Induced pluripotent stem cells (iPSCs): Molecular mechanisms of induction and applications. Signal Transduct. Target. Ther. 2024, 9, 112. [Google Scholar] [CrossRef]
- Wu, D.; Chen, Q.; Chen, X.; Han, F.; Chen, Z.; Wang, Y. The blood–brain barrier: Structure, regulation and drug delivery. Signal Transduct. Target. Ther. 2023, 8, 217. [Google Scholar] [CrossRef]
- Vleet, T.R.V.; Liguori, M.J.; James, J.; Lynch, I.; Rao, M.; Warder, S. Screening Strategies and Methods for Better Off-Target Liability Prediction and Identification of Small-Molecule Pharmaceuticals. SLAS Discov. 2019, 24, 1–24. [Google Scholar] [CrossRef]
- Guengerich, F.P. Mechanisms of Drug Toxicity and Relevance to Pharmaceutical Development. Drug Metab. Pharmacokinet. 2011, 26, 3–14. [Google Scholar] [CrossRef]
- Crucitti, D.; Pérez Míguez, C.; Díaz Arias, J.Á.; Fernandez Prada, D.B.; Mosquera Orgueira, A. De novo drug design through artificial intelligence: An introduction. Front. Hematol. 2024, 3, 1305741. [Google Scholar] [CrossRef]
- Mouchlis, V.D.; Afantitis, A.; Serra, A.; Fratello, M.; Papadiamantis, A.G.; Aidinis, V.; Lynch, I.; Greco, D.; Melagraki, G. Advances in De Novo Drug Design: From Conventional to Machine Learning Methods. Int. J. Mol. Sci. 2021, 22, 1676. [Google Scholar] [CrossRef] [PubMed]
- Mudshinge, S.R.; Deore, A.B.; Patil, S.; Bhalgat, C.M. Nanoparticles: Emerging carriers for drug delivery. Saudi Pharm. J. 2011, 19, 129–141. [Google Scholar] [CrossRef] [PubMed]
- Dhiman, N.; Awasthi, R.; Sharma, B.; Kharkwal, H.; Kulkarni, G.T. Lipid Nanoparticles as Carriers for Bioactive Delivery. Front. Chem. 2021, 9, 580118. [Google Scholar] [CrossRef] [PubMed]
- van Woensel, M.; Wauthoz, N.; Rosière, R.; Amighi, K.; Mathieu, V.; Lefranc, F.; van Gool, S.W.; de Vleeschouwer, S. Formulations for Intranasal Delivery of Pharmacological Agents to Combat Brain Disease: A New Opportunity to Tackle GBM? Cancers 2013, 5, 1020–1048. [Google Scholar] [CrossRef] [PubMed]
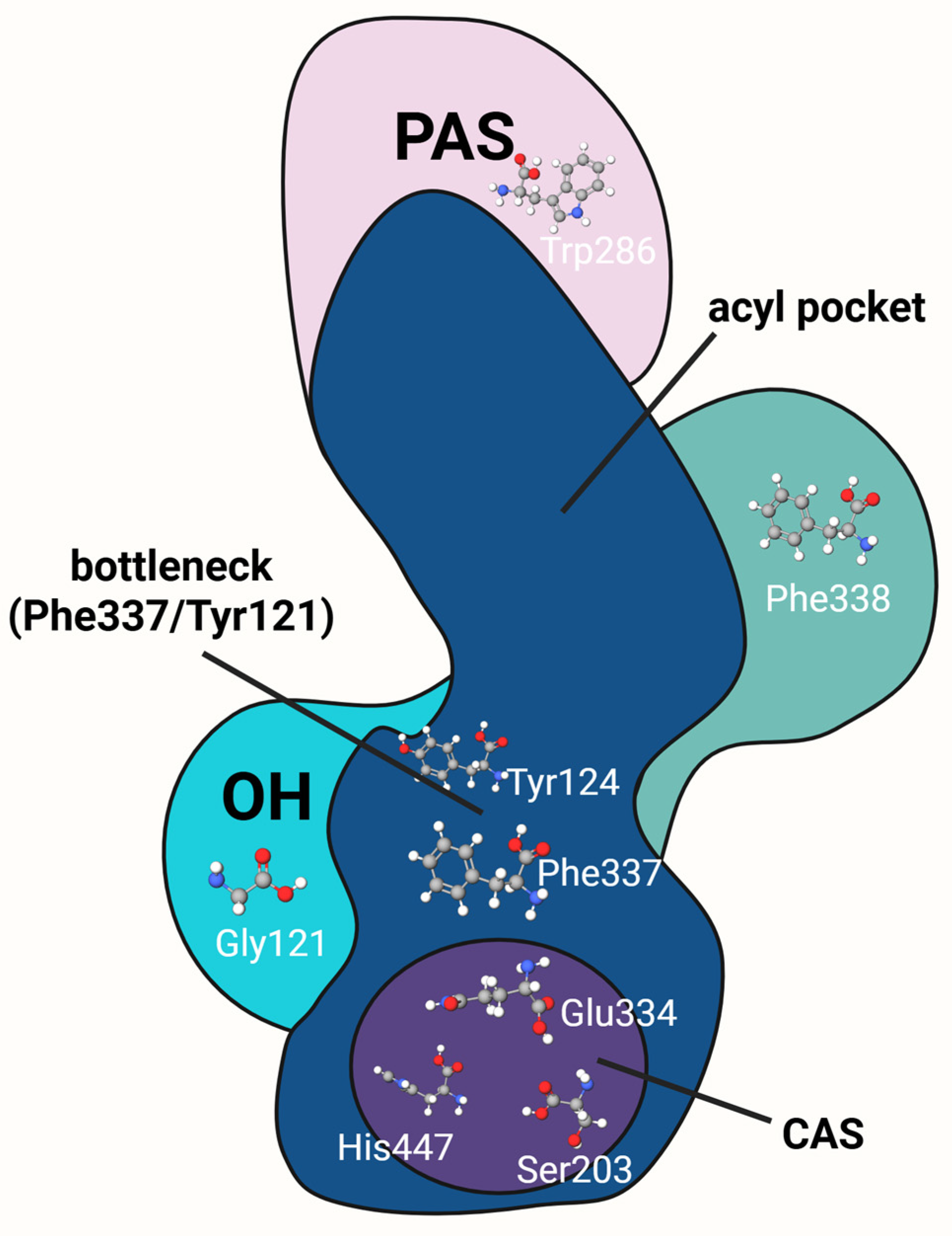

| Domain | Location | Key Amino Acids | Functions | References |
|---|---|---|---|---|
| Catalytic Active Site (CAS) | Bottom of the active-site gorge | S203, H447, E334, W86, Y337 |
| [30,31] |
| Peripheral Anionic Site (PAS) | Entrance of the active-site gorge | Y72, B74, Y124, W286, Y341 |
| [14,32,33] |
| Oxyanion Hole (OH) | Near CAS within the active-site gorge | G121, G122, A204 |
| [34] |
| Acyl Pocket | Within the CAS region | F295, F297 |
| [31] |
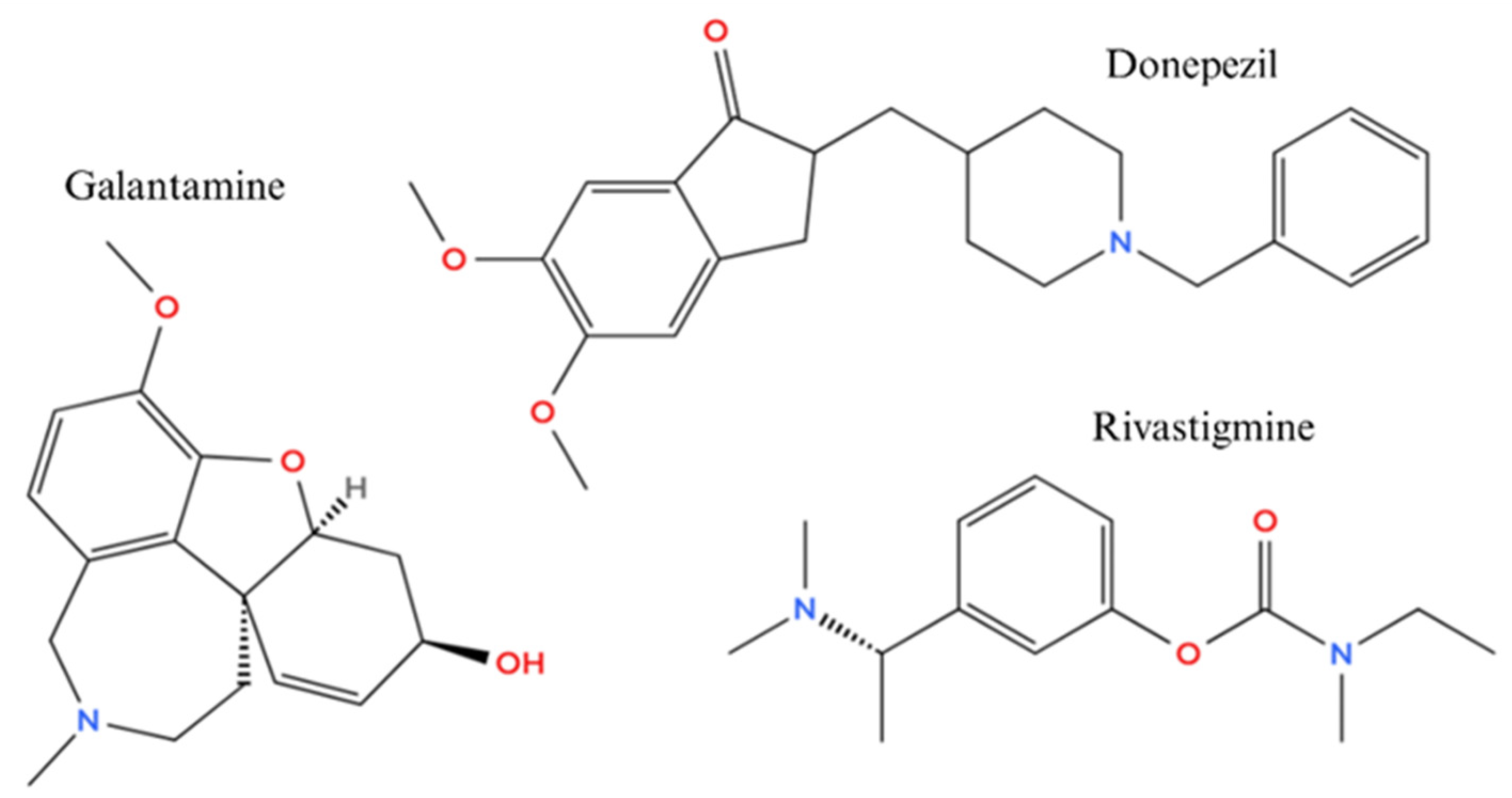
| Inhibitor | Mechanism | Clinical Benefit | Limitations | References |
|---|---|---|---|---|
| Donepezil | Reversible AChE inhibitor | Temporary cognitive improvement | Peripheral side effects, limited disease modification; gastrointestinal adverse effects include nausea, diarrhea, and vomiting | [38,41,43,47] |
| Galantamine | Reversible AChE inhibitor and allosteric modulator of nAChRs | Temporary cognitive improvement | Gastrointestinal adverse effects include loss of appetite, nausea, vomiting, diarrhea, and weight loss; clinical use may also be influenced by variability in central nervous system bioavailability related to formulation and patient-specific factors | [39,40,43,48] |
| Rivastigmine | Pseudo-irreversible AChE and BuChE inhibitor | Temporary cognitive improvement | Gastrointestinal adverse effects include nausea, vomiting, weight loss, and diarrhea, compounded by challenges related to dosing complexity | [38,42,43,49] |
| Strategy | Description | Representative Examples | Key Advantages | References |
|---|---|---|---|---|
| Conventional | Direct enzyme blockade enhancing cholinergic neurotransmission via competitive or non-competitive inhibition. | Donepezil, Rivastigmine, Galantamine |
| [38,39,41,42,43] |
| Dual site | Ligands targeting both CAS and PAS of AChE for enhanced inhibition and anti-amyloid activity. | Donepezil–benzofuran hybrids, Tacrine–coumarin hybrids, Bis-(7)-tacrine |
| [51,55,61,86] |
| Multi-target-directed ligands | Single molecules modulating AChE and other AD-related targets | Donepezil–MAO-B inhibitors, Tacrine–BACE-1 hybrids, Galantamine–GSK-3β conjugates, Coumarin–PDE inhibitors |
| [62,63,64,65,70,87,88] |
| Chelators | AChE inhibitors incorporating metal-chelating groups to mitigate metal-induced Aβ aggregation and oxidative stress. | Hydroxypyridinone derivatives, Cyclen-based AChE ligands, Tacrine–metal chelator conjugates |
| [68,69,70,71,72,73] |
| Hybrid ligand design | Fusion of natural and/or synthetic pharmacophores into single molecules to enhance multitarget efficacy and pharmacokinetics. | Curcumin–tacrine hybrids, Galantamine–flavonoid conjugates, Tacrine–resveratrol hybrids |
| [77,78,79,80,81,82,83,84,85,86,87,88] |
| Prodrug | Enzymatically activated inactive precursors designed to improve CNS delivery and reduce systemic toxicity. | Galantamine carbamates, Tacrine–prodrugs with lipophilic masking groups |
| [89,90,91,92,93,94] |
| Photopharmacology | Light-activated inhibitors with reversible control of AChE inhibition via photo-switchable molecular groups. | Azobenzene-based donepezil analogs, Dithienylethene (DTE)–tacrine hybrids, Photoresponsive tacrine derivatives |
| [22,95,96,97] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grabowska, W.; Bijak, M.; Szelenberger, R.; Gorniak, L.; Podogrocki, M.; Harmata, P.; Cichon, N. Acetylcholinesterase as a Multifunctional Target in Amyloid-Driven Neurodegeneration: From Dual-Site Inhibitors to Anti-Agregation Strategies. Int. J. Mol. Sci. 2025, 26, 8726. https://doi.org/10.3390/ijms26178726
Grabowska W, Bijak M, Szelenberger R, Gorniak L, Podogrocki M, Harmata P, Cichon N. Acetylcholinesterase as a Multifunctional Target in Amyloid-Driven Neurodegeneration: From Dual-Site Inhibitors to Anti-Agregation Strategies. International Journal of Molecular Sciences. 2025; 26(17):8726. https://doi.org/10.3390/ijms26178726
Chicago/Turabian StyleGrabowska, Weronika, Michal Bijak, Rafał Szelenberger, Leslaw Gorniak, Marcin Podogrocki, Piotr Harmata, and Natalia Cichon. 2025. "Acetylcholinesterase as a Multifunctional Target in Amyloid-Driven Neurodegeneration: From Dual-Site Inhibitors to Anti-Agregation Strategies" International Journal of Molecular Sciences 26, no. 17: 8726. https://doi.org/10.3390/ijms26178726
APA StyleGrabowska, W., Bijak, M., Szelenberger, R., Gorniak, L., Podogrocki, M., Harmata, P., & Cichon, N. (2025). Acetylcholinesterase as a Multifunctional Target in Amyloid-Driven Neurodegeneration: From Dual-Site Inhibitors to Anti-Agregation Strategies. International Journal of Molecular Sciences, 26(17), 8726. https://doi.org/10.3390/ijms26178726





