Midkine Deficiency Attenuates Lipopolysaccharide-Induced Pulmonary Inflammation
Abstract
1. Introduction
2. Results
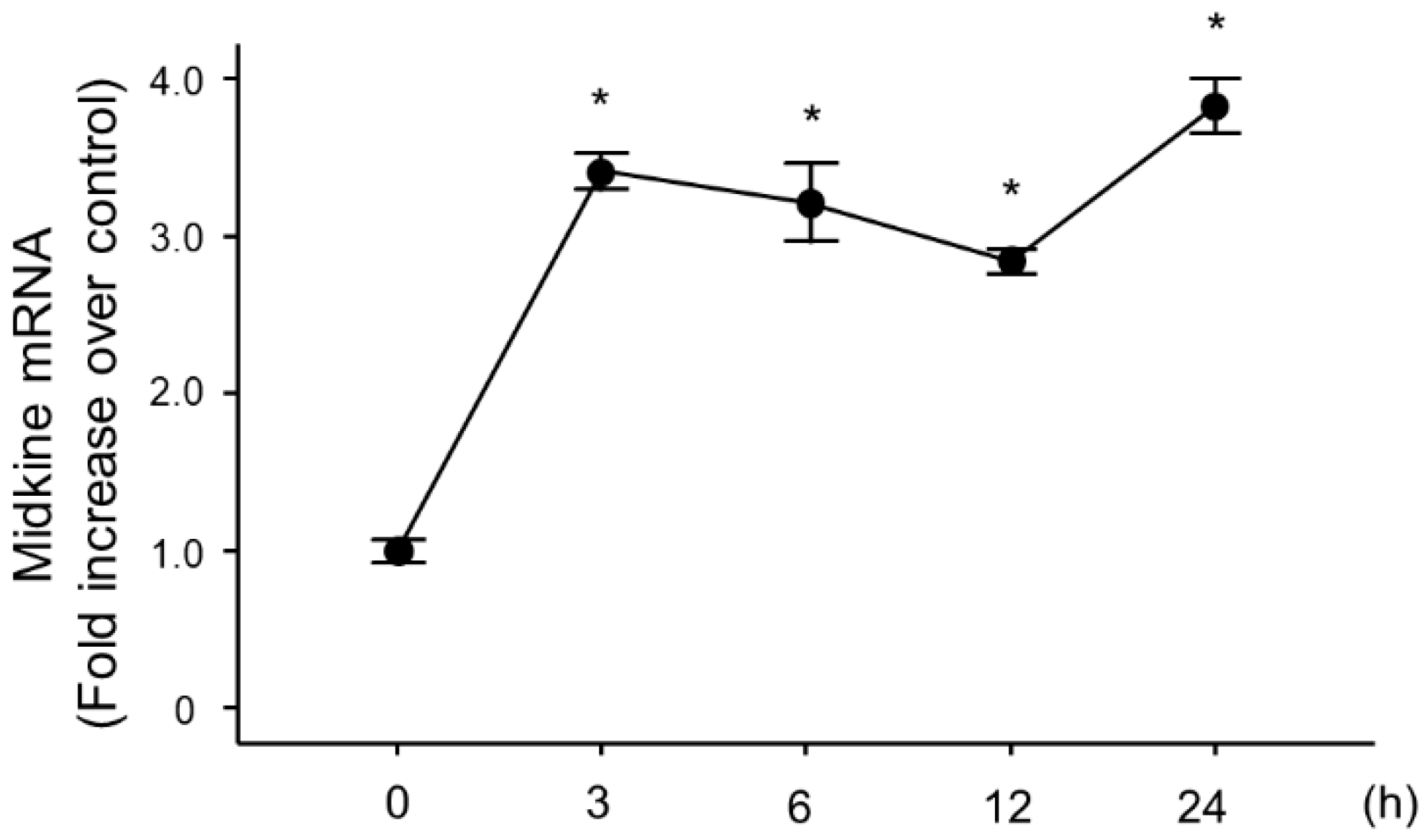
2.1. Change in Midkine Expression in Lung Tissues After LPS Administration
2.2. Bronchoalveolar Lavage Findings in Midkine-Deficient Mice
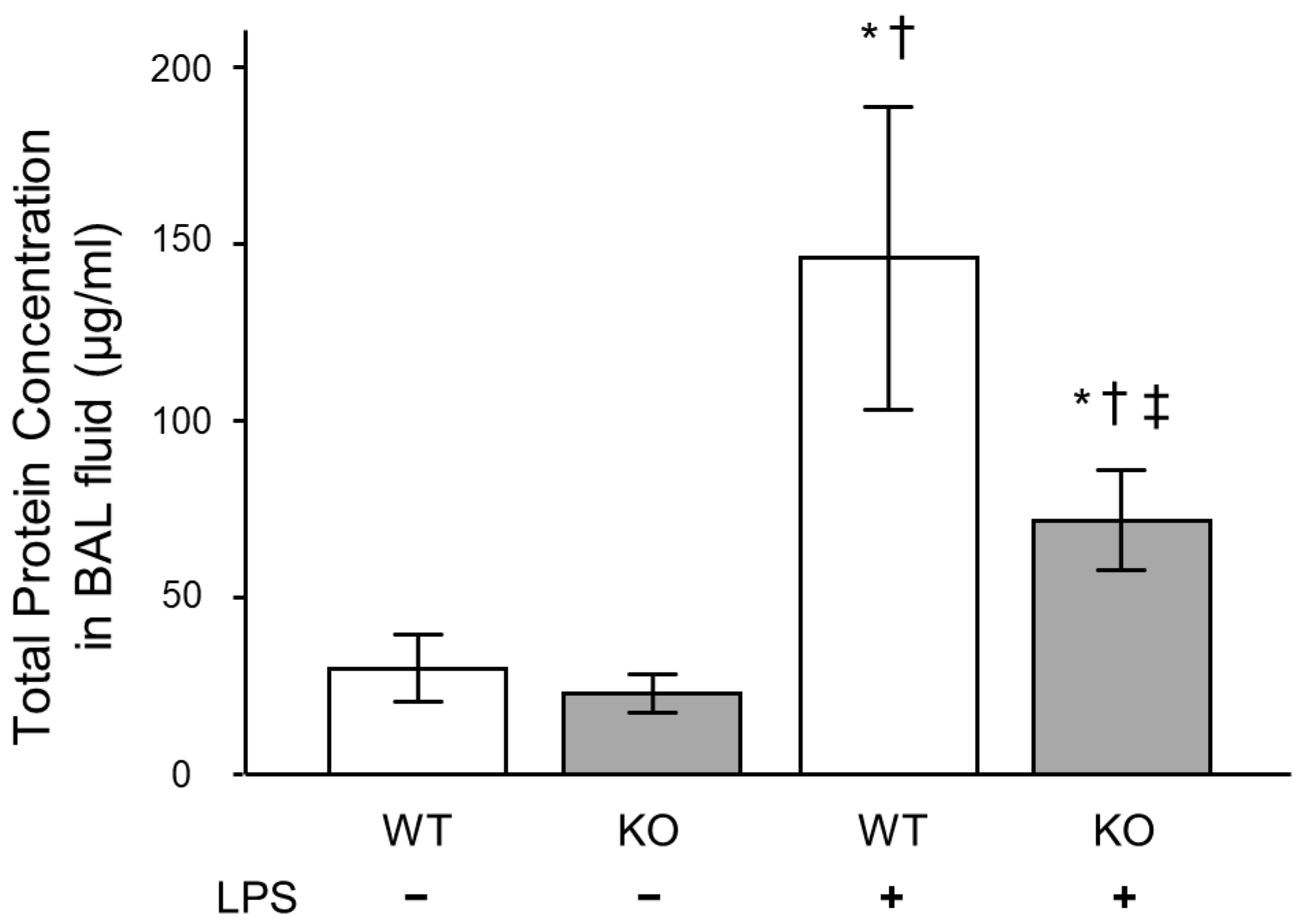
2.3. Inflammatory Cytokine and Total Protein Concentrations in Bronchoalveolar Lavage Fluid of Midkine-Deficient Mice
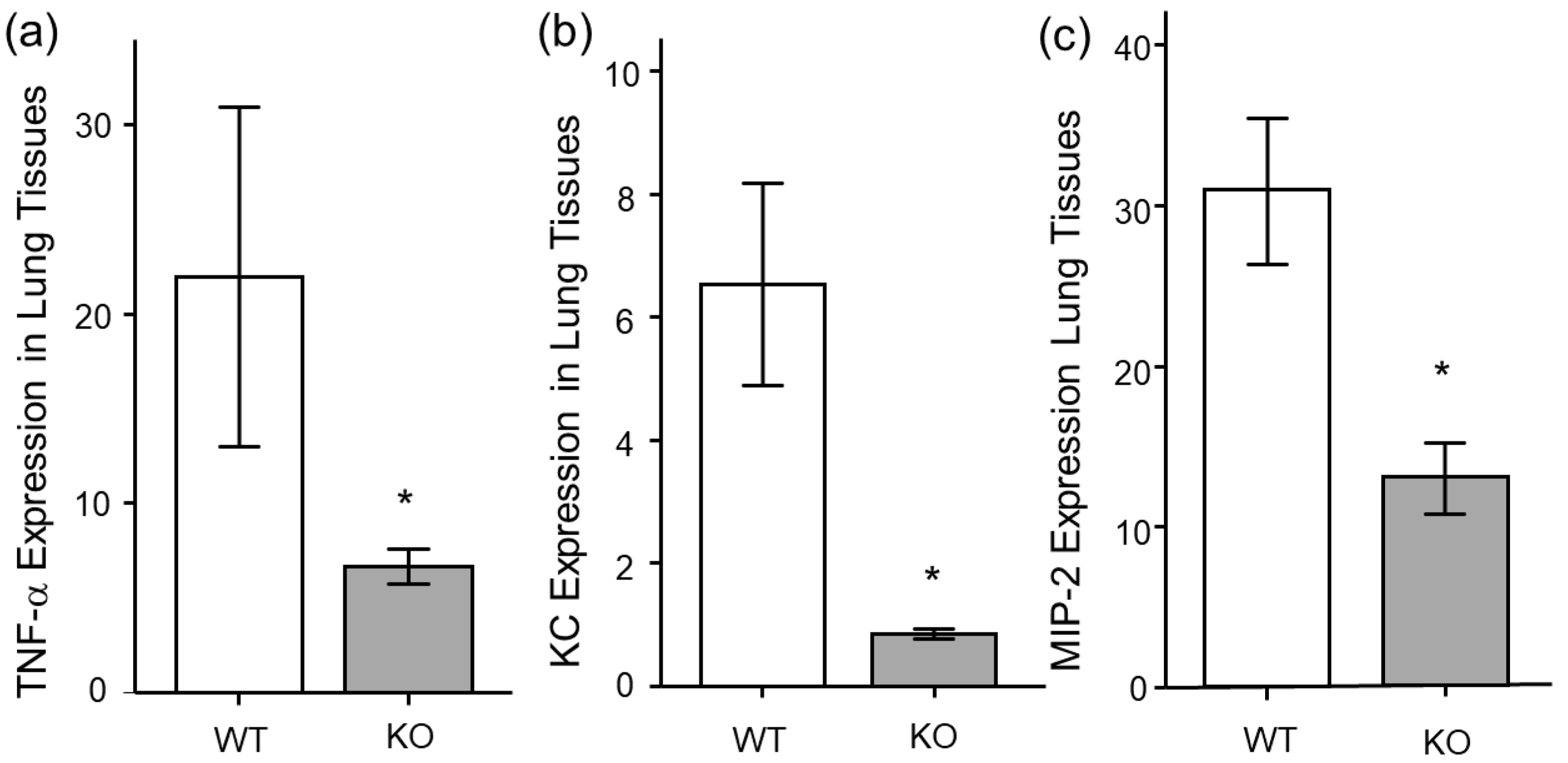
2.4. Inflammatory Cytokine Expression in Lung Tissues of Midkine-Deficient Mice
2.5. Histopathological Analysis of Midkine-Deficient Mice
2.6. Change in Midkine mRNA Expression in Bronchial Epithelial Cells After LPS Stimulation
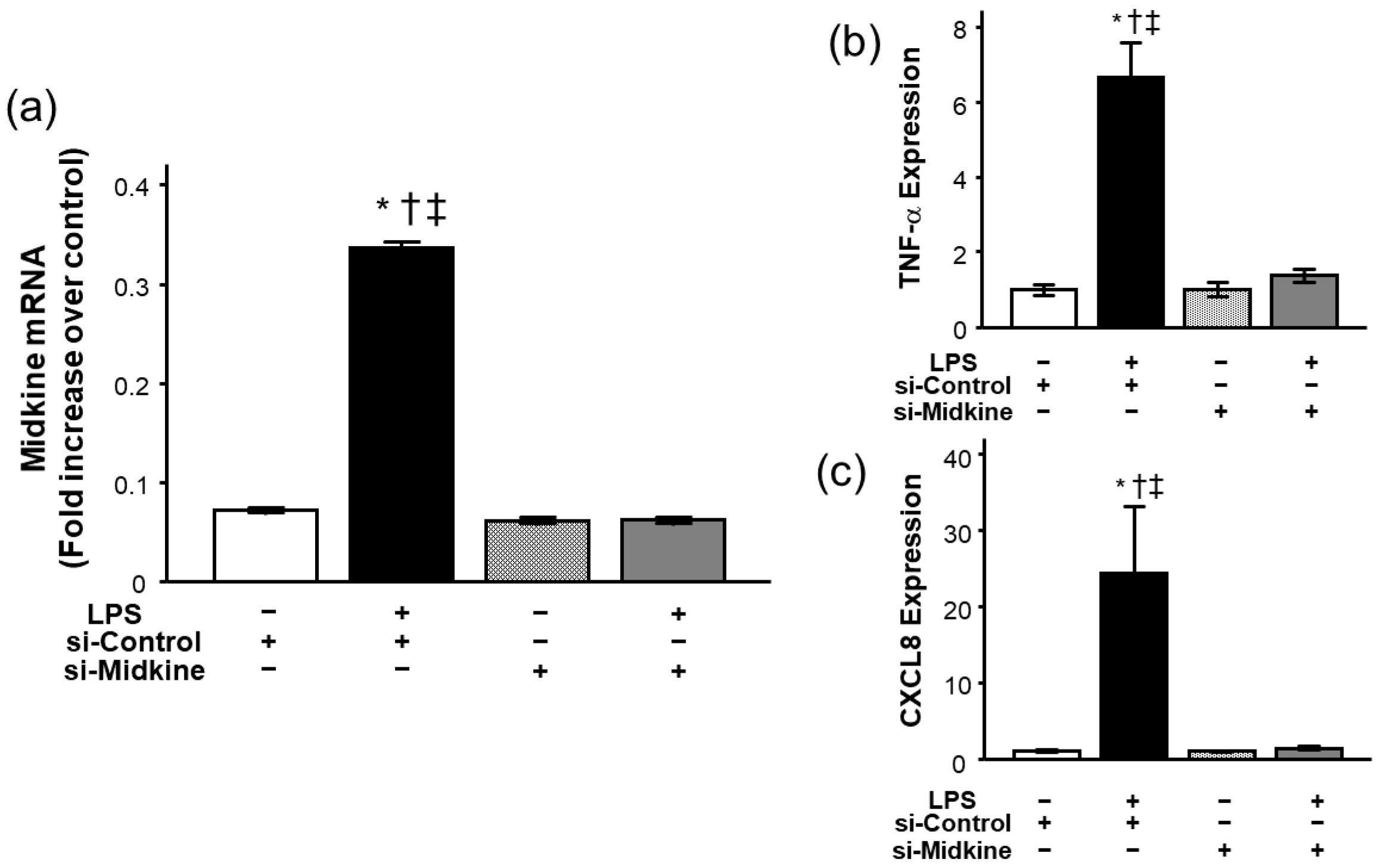
2.7. Effect of Midkine Knockdown on LPS-Induced TNF-α and CXCL8 Expressions in Bronchial Epithelial Cells
3. Discussion
4. Materials and Methods
4.1. Reagents
4.2. Animal Protocols
4.3. Isolation of RNA
4.4. Time Course of Midkine Expression
4.5. Measurement of mRNA
4.6. Preparation of Lung Homogenates
4.7. Measurement of Midkine, Inflammatory Cytokine, and Protein Concentrations
4.8. Pathological Evaluation of Lung Sections
4.9. Cell Culture
4.10. Knockdown of Midkine
4.11. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thompson, B.T.; Chamber, R.C.; Liu, K.D. Acute respiratory distress syndrome. N. Engl. J. Med. 2017, 377, 562–572. [Google Scholar] [CrossRef]
- Bos, L.D.J.; Ware, L.B. Acute respiratory distress syndrome: Causes, pathophysiology, and phenotypes. Lancet 2022, 400, 1145–1156. [Google Scholar] [CrossRef] [PubMed]
- Matthay, M.A.; Zemans, R.L.; Zimmerman, G.A.; Arabi, Y.M.; Beitler, J.R.; Mercat, A.; Herridge, M.; Randolph, A.G.; Calfee, C.S. Acute respiratory distress syndrome. Nat. Rev. Dis. Primers 2019, 5, 18. [Google Scholar] [CrossRef]
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; van Haren, F.; Larsson, A.; McAuley, D.F.; et al. LUNG SAFE Investigators; ESICM Trials Group., Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016, 315, 788–800. [Google Scholar] [CrossRef] [PubMed]
- Rajdev, K.; Spanel, A.J.; McMillan, S.; Lahan, S.; Boer, B.; Birge, J.; Thi, M. Pulmonary barotrauma in COVID-19 patients with ards on invasive and non-invasive positive pressure ventilation. J. Intensive Care Med. 2021, 36, 1013–1017. [Google Scholar] [CrossRef] [PubMed]
- Beitler, J.R.; Thompson, B.T.; Baron, R.M.; Bastarache, J.A.; Denlinger, L.C.; Esserman, L.; Gong, M.N.; LaVange, L.M.; Lewis, R.J.; Marshall, J.C.; et al. Advancing precision medicine for acute respiratory distress syndrome. Lancet Respir. Med. 2022, 10, 107–120. [Google Scholar] [CrossRef]
- Matthay, M.A.; Arabi, Y.; Arroliga, A.C.; Bernard, G.; Bersten, A.D.; Brochard, L.J.; Calfee, C.S.; Combes, A.; Daniel, B.M.; Ferguson, N.D.; et al. A new global definition of acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2024, 209, 37–47. [Google Scholar] [CrossRef]
- Kadomatsu, K.; Tomomura, M.; Muramatsu, T. cDNA cloning and sequencing of a new gene intensely expressed in early differentiation stages of embryonal carcinoma cells and in mid-gestation period of mouse embryogenesis. Biochem. Biophys. Res. Commun. 1988, 151, 1312–1318. [Google Scholar] [CrossRef]
- Yildirim, B.; Kulak, K.; Bilir, A. Midkine (MDK) in cancer and drug resistance: From inflammation to therapy. Discov. Oncol. 2025, 16, 1062. [Google Scholar] [CrossRef]
- Fei, H.; Chen, T.; Jiang, H. Autocrine and paracrine effects of MDK promote lymph node metastasis of cervical squamous cell carcinoma. iScience 2024, 27, 110077. [Google Scholar] [CrossRef]
- Yang, X.; Sun, S.; Kuang, X.; Lu, X.; Xiao, H.; Duan, Y.; Xiong, Y.; Zhang, D.; Xu, Y.; Zhu, J.; et al. Midkine expression as a candidate biomarker to predict the recurrence of stage IA lung adenocarcinoma. JTO Clin. Res. Rep. 2025, 6, 100858. [Google Scholar] [CrossRef]
- Ohta, S.; Muramatsu, H.; Senda, T.; Zou, K.; Iwata, H.; Muramatsu, T. Midkine is expressed during repair of bone fracture and promotes chondrogenesis. J. Bone Miner. Res. 1999, 14, 1132–1144. [Google Scholar] [CrossRef]
- Misa, K.; Tanino, Y.; Wang, X.; Nikaido, T.; Kikuchi, M.; Sato, Y.; Togawa, R.; Tanino, M.; Tanaka, S.; Kadomatsu, K.; et al. Involvement of midkine in the development of pulmonary fibrosis. Physiol. Rep. 2017, 5, e13383. [Google Scholar] [CrossRef]
- Weckbach, L.T.; Muramatsu, T.; Walzog, B. Midkine in inflammation. es hypoxia-induced proliferation and differentiation of hyman epithelial cells. Sci. World J. 2011, 11, 2491–2505. [Google Scholar] [CrossRef]
- Muramatsu, T. Midkine and pleiotrophin: Two related proteins involved in development, survival, inflammation and tumorigenesis. J. Biochem. 2002, 132, 359–371. [Google Scholar] [CrossRef] [PubMed]
- Maruyama, K.; Muramatsu, H.; Ishiguro, N.; Muramatsu, T. Midkine, a heparin-binding growth factor, is fundamentally involved in the pathogenesis of rheumatoid arthritis. Arthritis Rheum. 2004, 50, 1420–1429. [Google Scholar] [CrossRef] [PubMed]
- Shindo, E.; Nanki, T.; Kusunoki, N.; Shikano, K.; Kawazoe, M.; Sato, H.; Kaneko, K.; Muraoka, S.; Kaburaki, M.; Akasaka, Y.; et al. The growth factor midkine may play a pathophysiological role in rheumatoid arthritis. Mod. Rheumatol. 2017, 27, 54–59. [Google Scholar] [CrossRef]
- Wu, G.C.; Yuan, H.; Pan, H.F.; Ye, D.Q. Elevated plasma midkine and pleiotrophin levels in patients with systemic lupus erythematosus. Oncotarget 2017, 8, 40181–40189. [Google Scholar] [CrossRef] [PubMed]
- Nordin, S.L.; Jovic, S.; Kurut, A.; Andersson, C.; Gela, A.; Bjartell, A.; Morgelin, M.; Olin, A.I.; Lund, M.; Egesten, A. High expression of midkine in the airways of patients with cystic fibrosis. Am. J. Respir. Cell. Mol. Biol. 2013, 49, 935–942. [Google Scholar] [CrossRef]
- Linge, H.M.; Andersson, C.; Nordin, S.L.; Olin, A.I.; Petersson, A.C.; Mörgelin, M.; Welin, A.; Bylund, J.; Bjermer, L.; Erjefält, J.; et al. Midkine is expressed and differentially processed during chronic obstructive pulmonary disease exacerbations and ventilator-associated pneumonia associated with Staphylococcus aureus infection. Mol. Med. 2013, 19, 314–323. [Google Scholar] [CrossRef]
- Nordon, S.L.; Sonesson, A.; Malmsten, M.; Mörgelin, M.; Egesten, A. The epithelium-produced growth fator midkine has fungicidal properties. J. Antimicrob. Chemother. 2012, 67, 1927–1936. [Google Scholar] [CrossRef] [PubMed]
- Nordin, S.L.; Andersson, C.; Bjermer, L.; Bjartell, A.; Mörgelin, M.; Egesten, A. Midkine is part of the antibacterial activity released at the surface of differentiated bronchial epithelial cells. J. Innate Immun. 2013, 5, 519–530. [Google Scholar] [CrossRef]
- Zhang, R.; Pan, Y.; Fanelli, V.; Wu, S.; Luo, A.A.; Islam, D.; Han, B.; Mao, P.; Ghazarian, M.; Zeng, W.; et al. Mechanical Stress and the Induction of Lung Fibrosis via the Midkine Signaling Pathway. Am. J. Respir. Crit. Care. Med. 2015, 192, 315–323. [Google Scholar] [CrossRef]
- Sato, W.; Kadomatsu, K.; Yuzawa, Y.; Muramatsu, H.; Hotta, N.; Matsuo, S.; Muramatsu, T. Midkine is involved in neutrophil infiltration into the tubulointerstitium in ischemic renal injury. J. Immunol. 2001, 167, 3463–3469. [Google Scholar] [CrossRef]
- Sato, W.; Takei, Y.; Yuzawa, Y.; Matsuo, S.; Kadomatsu, K.; Muramatsu, T. Midkine antisense oligodeoxyribonucleotide inhibits renal damage induced by ischemic reperfusion. Kidney Int. 2005, 67, 1330–1339. [Google Scholar] [CrossRef]
- Wang, J.; Takeuchi, H.; Sonobe, Y.; Jin, S.; Mizuno, T.; Miyakawa, S.; Fujiwara, M.; Nakamura, Y.; Kato, T.; Muramatsu, H.; et al. Inhibition of midkine alleviates experimental autoimmune encephalomyelitis through the expansion of regulatory t cell population. Proc. Natl. Acad. Sci. USA 2008, 105, 3915–3920. [Google Scholar] [CrossRef]
- Kojima, H.; Kosugi, T.; Sato, W.; Sato, Y.; Maeda, K.; Kato, N.; Kato, K.; Inaba, S.; Ishimoto, T.; Tsuboi, N.; et al. Deficiency of growth factor midkine exacerbates necrotizing glomerular injuries in progressive glomerulonephritis. Am. J. Pathol. 2013, 182, 410–419. [Google Scholar] [CrossRef]
- Ohuchida, T.; Okamoto, K.; Akahane, K.; Higure, A.; Todoroki, H.; Abe, Y.; Kikuchi, M.; Ikematsu, S.; Muramatsu, T.; Itoh, H. Midkine protects hepatocellular carcinoma cells against trail-mediated apoptosis through down-regulation of caspase-3 activity. Cancer 2004, 100, 2430–2436. [Google Scholar] [CrossRef]
- Neumaier, E.E.; Rothhammer, V.; Linnerbauer, M. The role of midkine in health and disease. Front. Immunol. 2023, 14, 1310094. [Google Scholar] [CrossRef] [PubMed]
- Takenaka, H.; Horiba, M.; Ishiguro, H.; Sumida, A.; Hojo, M.; Usui, A.; Akita, T.; Sakuma, S.; Ueda, Y.; Kodama, I.; et al. Midkine prevents ventricular remodeling and improves long-term survival after myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 2009, 296, H462–H469. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, P.R.; Mucenski, M.L.; Le Cras, T.D.; Nichols, W.C.; Whitsett, J.A. Midkine is regulated by hypoxia and causes pulmonary vascular remodeling. J. Biol. Chem. 2004, 279, 37124–37132. [Google Scholar] [CrossRef]
- Zhang, H.; Okamoto, M.; Panzhinskiy, E.; Zawada, W.M.; Das, M. PKCγ/midkine pathway drives hypoxia-induced proliferation and differentiation of hyman epithelial cells. Am. J. Physiol. Cell Physiol. 2014, 306, C648–C658. [Google Scholar] [CrossRef][Green Version]
- Chang, W.; Peng, F.; Sun, Q.; Meng, S.S.; Qiu, H.B.; Xu, J.Y. Plasma midkine is associated with 28-day mortality and organ function in sepsis. J. Intensive Care Med. 2020, 35, 1290–1296. [Google Scholar] [CrossRef] [PubMed]
- Ketenci, S.; Kalayci, M.U.; Dündar, B.; Duranay, R.; Aynacıoğlu, A.S. Elevated serum midkine levels in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infected patients. Int. Immunopharmacol. 2022, 110, 108939. [Google Scholar] [CrossRef]
- Xu, J.Y.; Chang, W.; Sun, Q.; Peng, F.; Yang, Y. Pulmonary midkine inhibition ameliorates sepsis induced lung injury. J. Transl. Med. 2021, 19, 91. [Google Scholar] [CrossRef] [PubMed]
- Weckbach, L.T.; Groesser, L.; Borgolte, J.; Pagel, J.I.; Pogoda, F.; Schymeinsky, J.; Müller-Höcker, J.; Shakibaei, M.; Muramatsu, T.; Deindl, E.; et al. Midkine acts as proangiogenic cytokine in hypoxia-induced angiogenesis. Am. J. Physiol. Heart Circ. Physiol. 2012, 303, H429–H438. [Google Scholar] [CrossRef]
- Takada, T.; Toriyama, K.; Muramatsu, H.; Song, X.J.; Torii, S.; Muramatsu, T. Midkine, a retinoic acid-inducible heparin-binding cytokine in inflammatory responses: Chemotactic activity to neutrophils and association with inflammatory synovitis. J. Biochem. 1997, 122, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Weckbach, L.T.; Gola, A.; Winkelmann, M.; Jakob, S.M.; Groesser, L.; Borgolte, J.; Pogoda, F.; Pick, R.; Pruenster, M.; Müller-Höcker, J.; et al. The cytokine midkine supports neutrophil trafficking during acute inflammation by promoting adhesion via β2 integrins (CD11/CD18). Blood 2014, 123, 1887–1896. [Google Scholar] [CrossRef]
- Herter, J.M.; Mayadas, T.N. Midkine, a middle manager of β2 integrins. Blood 2014, 123, 1777–1779. [Google Scholar] [CrossRef]
- Weckbach, L.T.; Grabmaier, U.; Uhl, A.; Gess, S.; Boehm, F.; Zehrer, A.; Pick, R.; Salvermoser, M.; Czermak, T.; Pircher, J.; et al. Midkine drives cardiac inflammation by promoting neutrophil trafficking and netosis in myocarditis. J. Exp. Med. 2019, 216, 350–368. [Google Scholar] [CrossRef]
- Liu, G.; Ren, X.; Li, Y.; Li, H. Midkine promotes kidney injury in diabetic kidney disease by increasing neutrophil extracellular traps formation. Ann. Transl. Med. 2022, 10, 693. [Google Scholar] [CrossRef]
- Bolger, M.S.; Ross, D.S.; Jiang, H.; Frank, M.M.; Ghio, A.J.; Schwartz, D.A.; Wright, J.R. Complement levels and activity in the normal and LPS-injured lung. Am. J. Physiol. Lung Cell. Mol. Physiol. 2007, 292, L748–L759. [Google Scholar] [CrossRef] [PubMed]
- Rittirsch, D.; Flierl, M.A.; Day, D.E.; Nadeau, B.A.; McGuire, S.R.; Hoesel, L.M.; Ipaktchi, K.; Zetoune, F.S.; Sarma, J.V.; Leng, L.; et al. Acute lung injury induced by lipopolysaccharide is independent of complement activation. J. Immunol. 2008, 180, 7664–7672. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Che, W.; Zhao, M. Ulinastatin post-treatment attenuates lipopolysaccharide-induced acute lung injury in rats and human alveolar epithelial cells. Int. J. Mol. Med. 2017, 39, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Hao, Q.; Gudapati, V.; Monsel, A.; Park, J.H.; Hu, S.; Kato, H.; Lee, J.H.; Zhou, L.; He, H.; Lee, J.W. Mesenchymal stem cell-derived extracellular vesicles decrease lung injury in mice. J. Immunol. 2019, 203, 1961–1972. [Google Scholar] [CrossRef]
- Nakamura, E.; Kadomatsu, K.; Yuasa, S.; Muramatsu, H.; Mamiya, T.; Nabeshima, T.; Fan, Q.W.; Ishiguro, K.; Matsubara, S.; Kaname, T.; et al. Disruption of the midkine gene (Mdk) results in altered expression of calcium binding protein in the hippocampus of infant mice and their abnormal behaviour. Genes Cells 1998, 3, 811–822. [Google Scholar] [CrossRef]
- Tanino, Y.; Makita, H.; Miyamoto, K.; Betsuyaku, T.; Ohtsuka, Y.; Nishihira, J.; Nishimura, M. Role of macrophage migration inhibitory factor in bleomycin-induced lung injury and fibrosis in mice. Am. J. Physiol. Lung Cell. Mol. Physiol. 2002, 283, L156–L162. [Google Scholar] [CrossRef]
- Tanino, Y.; Chang, M.Y.; Wang, X.; Gill, S.E.; Skerrett, S.; McGuire, J.K.; Sato, S.; Nikaido, T.; Kojima, T.; Munakata, M.; et al. Syndecan-4 regulates early neutrophil migration and pulmonary inflammation in response to lipopolysaccharide. Am. J. Respir. Cell Mol. Biol. 2012, 47, 196–202. [Google Scholar] [CrossRef]
- Tanino, Y.; Wang, X.; Nikaido, T.; Misa, K.; Sato, Y.; Togawa, R.; Kawamata, T.; Kikuchi, M.; Frevert, C.W.; Tanino, M.; et al. Syndecan-4 inhibits the development of pulmonary fibrosis by attenuating TGF-β signaling. Int. J. Mol. Sci. 2019, 20, 4989. [Google Scholar] [CrossRef]
- Tang, S.E.; Wu, S.Y.; Chu, S.J.; Tzeng, Y.S.; Peng, C.K.; Lan, C.C.; Perng, W.C.; Wu, C.P.; Huang, K.L. Pre-treatment with ten-minute carbon dioxide inhalation prevents lipopolysaccharide-induced lung injury in mice via down-regulation of toll-like receptor 4 expression. Int. J. Mol. Sci. 2019, 20, 6293. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanino, Y.; Wang, X.; Nikaido, T.; Sato, Y.; Togawa, R.; Watanabe, N.; Tanino, M.; Kadomatsu, K.; Shibata, Y. Midkine Deficiency Attenuates Lipopolysaccharide-Induced Pulmonary Inflammation. Int. J. Mol. Sci. 2025, 26, 8519. https://doi.org/10.3390/ijms26178519
Tanino Y, Wang X, Nikaido T, Sato Y, Togawa R, Watanabe N, Tanino M, Kadomatsu K, Shibata Y. Midkine Deficiency Attenuates Lipopolysaccharide-Induced Pulmonary Inflammation. International Journal of Molecular Sciences. 2025; 26(17):8519. https://doi.org/10.3390/ijms26178519
Chicago/Turabian StyleTanino, Yoshinori, Xintao Wang, Takefumi Nikaido, Yuki Sato, Ryuichi Togawa, Natsumi Watanabe, Mishie Tanino, Kenji Kadomatsu, and Yoko Shibata. 2025. "Midkine Deficiency Attenuates Lipopolysaccharide-Induced Pulmonary Inflammation" International Journal of Molecular Sciences 26, no. 17: 8519. https://doi.org/10.3390/ijms26178519
APA StyleTanino, Y., Wang, X., Nikaido, T., Sato, Y., Togawa, R., Watanabe, N., Tanino, M., Kadomatsu, K., & Shibata, Y. (2025). Midkine Deficiency Attenuates Lipopolysaccharide-Induced Pulmonary Inflammation. International Journal of Molecular Sciences, 26(17), 8519. https://doi.org/10.3390/ijms26178519






