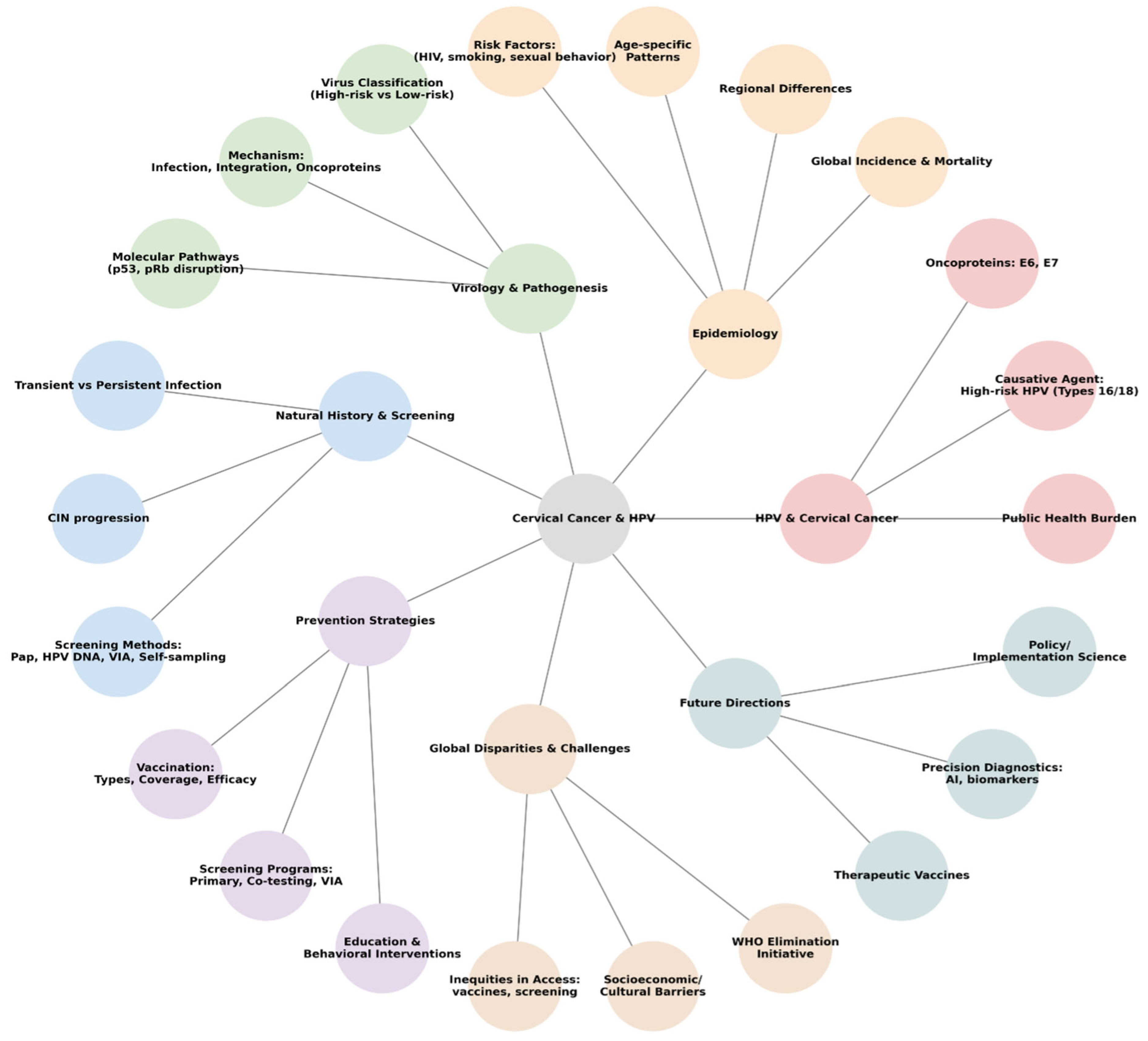
Cervical Cancer in the Era of HPV: Translating Molecular Mechanisms into Preventive Public Health Action
Abstract
1. Introduction
2. Epidemiology
2.1. Global Incidence and Mortality
2.2. Regional and National Trends
2.3. HPV Prevalence and High-Risk Types
2.4. Age-Specific and Histology Patterns
2.5. Risk Factors Beyond HPV
- HIV co-infection: Women living with HIV (WLWH) have an up to six-fold higher risk of cervical cancer, partly due to compromised immunity and hrHPV persistence; globally, an estimated 5% of all cervical cancer cases are attributable to HIV co-infection;
- Sexual behavior: Early sexual debut, a higher number of partners, and the infection status of partners increase hrHPV acquisition;
- Smoking: Tobacco use contributes independently to cervical neoplasia progression;
- Immunosuppression: Aside from HIV, medical immunosuppression (e.g., transplant, steroids) raises its risk;
- Socioeconomic factors: Poverty, limited access to screening/vaccines, and education deficits amplify its risk, especially in marginalized communities.
- Human leukocyte antigen (HLA) polymorphisms: Certain human leukocyte antigen variants may yield proteins with a lower affinity for HPV antigens, impeding immune clearance and increasing persistence risk;
- The TP53 codon 72 polymorphism: A variant in TP53 (P72R) has been linked to heightened vulnerability; studies report that the Arginine/Arginine (Arg/Arg) genotype is associated with increased risk of HPV-associated cervical cancer;
- Long-term oral contraceptive (OC) use: Among women with hrHPV infections, OC use over 5 years might double to quadruple their cervical cancer risk;
- High parity: A meta-analysis found that women with high parity (many full-term pregnancies) have significantly elevated odds of developing cervical cancer compared to that in low-parity women;
- Lower levels of vitamins A, C, E, and folate have been associated with a higher risk of cervical dysplasia and cancer, highlighting the role of antioxidant defenses in modifying HPV-related progression;
- Chlamydia trachomatis co-infection: Meta-analyses reveal that women with concurrent HPV and Chlamydia trachomatis infection have a substantially higher risk of cervical cancer;
- The depletion of protective Lactobacillus species and overrepresentation of anaerobes (e.g., Gardnerella, Prevotella, Sneathia) have been associated with higher rates of hrHPV infection and progression to precancer/cancer. Metagenomic studies observed a correlation between such dysbiosis and a higher severity of cervical lesions;
- An elevated vaginal pH (>5), often accompanying microbial shifts, has also been linked to a 10–20% increase in HPV positivity risk in premenopausal women.
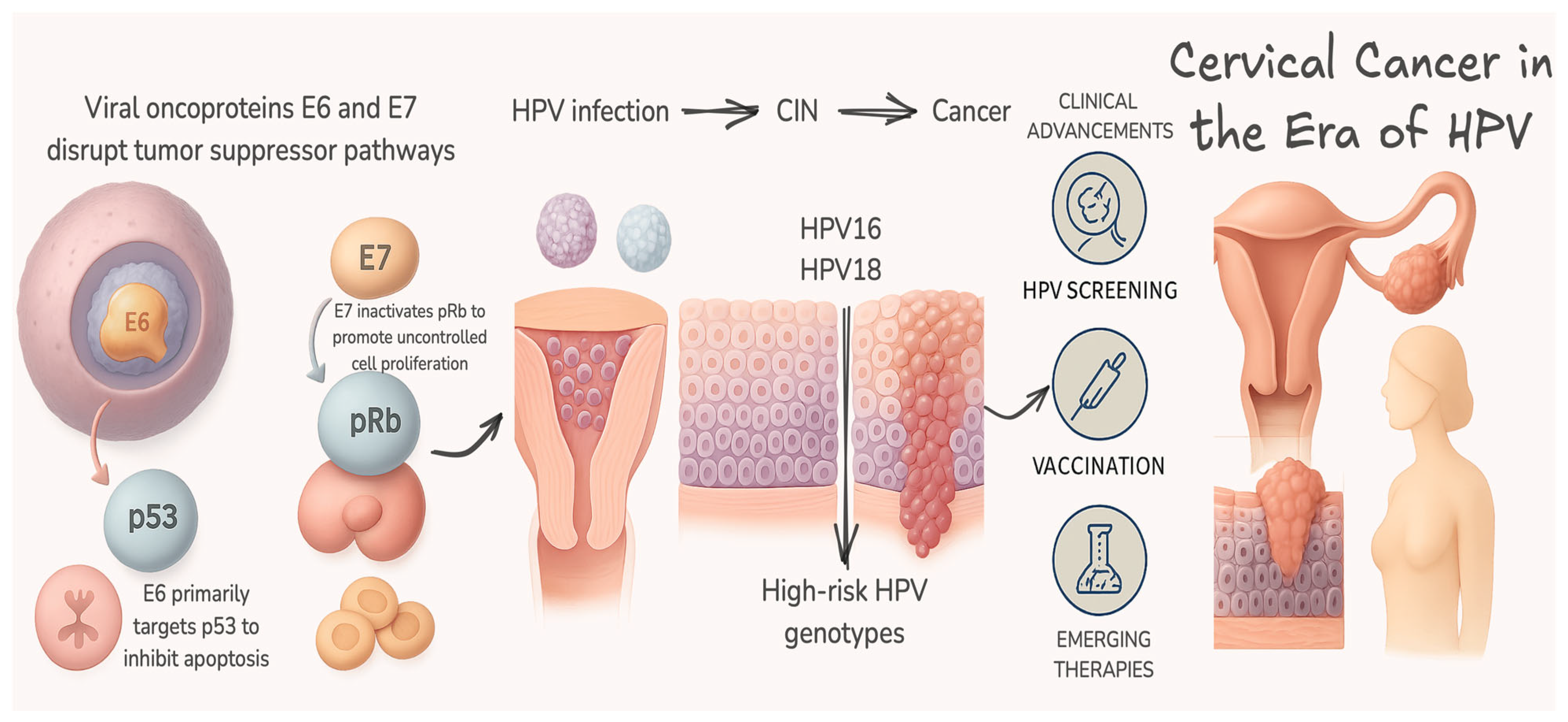
3. Virology and Pathogenesis
3.1. HPV Classification: Low-Risk vs. High-Risk
3.2. Infection Mechanisms and the Viral Life Cycle
3.3. Oncoproteins E6 and E7: Central Drivers of Transformation
3.4. Beyond E6/E7: Additional Viral and Host Factors
4. Natural History and Screening
4.1. The Course of HPV Infection: Transient Versus Persistent
4.2. Cervical Intraepithelial Neoplasia
- CIN1 (low-grade dysplasia): Often transient and usually regresses spontaneously.
- CIN2/3 (high-grade dysplasia): A risk of progression to invasive carcinoma—natural history data emphasize close monitoring of CIN2 in young women due to frequent regression, while CIN3 is generally treated promptly due to a higher progression risk. Management aligns with the guidelines, balancing the risks of overtreatment versus progression to cancer.
4.3. Post-Treatment Surveillance
5. Prevention Strategies
5.1. HPV Vaccination
- Bivalent (HPV-16/18);
- Quadrivalent (HPV-6/11/16/18);
- Nonavalent (HPV-6/11/16/18/31/33/45/52/58).
5.2. Breakthrough Disease After HPV Vaccination
- Infection with HPV types not included in the administered vaccine;
- Vaccination initiated after HPV exposure;
- Incomplete vaccination series or an older age at first dose.
- A 19-year-old woman developed biopsy-confirmed CIN3 two years after completing the quadrivalent HPV vaccine series; genotyping revealed a non-vaccine HPV type [159]. Similarly, a 33-year-old woman who had received a quadrivalent vaccination in 2006 was later diagnosed with CIN3 [160]. Another report described a 30-year-old woman, vaccinated after sexual debut, who was diagnosed with adenocarcinoma in situ in the cervix—highlighting that vaccination does not treat pre-existing infections [161].
- Larger cohort and trial data corroborate that lesions can still emerge in vaccinated populations, albeit at much lower rates. In the Costa Rica HPV Vaccine Trial (years 7–11), vaccinated women experienced a reduction in overall high-grade disease but showed a relative increase in CIN2+/CIN3+ caused by non-vaccine HPV types, consistent with type replacement or unmasking [162]. A Swedish nationwide cohort reported an incidence of invasive cervical cancer of 47 per 100,000 in vaccinated women compared with 94 per 100,000 in unvaccinated women—confirming strong but incomplete protection [151].
- Importantly, the timing and completeness of vaccination influence breakthrough risk. Scottish data indicate that one or two doses at ages 12–13 confer measurable protection, whereas those at an older age generally require three doses for the optimal effect; infections and lesions can still occur during the vaccination course, especially if the exposure precedes completion [148,150].
5.3. Screening Programs, Screening Methods, and the Impact of Vaccination
5.4. Education and Behavioral Interventions
- Social mobilization models, such as the Information–Motivation–Behavioral Skills model, have improved community awareness and empowerment for self-sampling initiatives;
- Studies in the U.S. have found that women educated through culturally competent interventions were more likely to engage in self-sampling and referral follow-up;
- Awareness barriers persist, as only around 6.5% of some communities had heard of self-sampling, though 75% felt confident in performing it after education;
- Digital platforms and artificial intelligence (AI)-enhanced systems are being introduced to prompt eligible individuals, support training, and facilitate follow-up referrals;
- Moving forward, scaling universal vaccine coverage, enabling accessible screening, and investing in culturally informed education are essential to advancing toward the WHO target of cervical cancer elimination.
6. Global Disparities and Challenges
6.1. Inequities in Vaccine and Screening Access
6.2. Socioeconomic, Cultural, and Health System Barriers
- Low awareness of HPV and its link to cervical cancer is widespread, as seen in Ghana and Venezuela, where knowledge gaps persist even among healthcare personnel;
- Cultural barriers and stigma related to sexual health deter vaccine uptake and participation in pelvic exams, especially in conservative communities;
- Health system limitations, such as shortages of skilled pathologists and a lack of screening logistics, exacerbate inequities. For instance, Ghana relies heavily on a small number of urban-based pathologists, depriving rural areas of services.
6.3. Innovations Addressing Disparities
- Self-sampling for HPV has emerged as a scalable alternative in both high- and low-resource settings;
- Self-sampling is cost-effective in LMICs—studies in India and China show that combined annual self-testing and nonavalent vaccination offers superior health and economic outcomes;
- Mailed kits in the U.S. safety net significantly boost screening in underserved communities;
- The WHO-endorsed screen-and-treat model replaces multiple visits with point-of-care testing and treatment in a single visit—crucial for LMICs.
6.4. The WHO Cervical Cancer Elimination Initiative
6.5. Steps Forward
- Scaling single-dose vaccination, simplifying logistics and reducing cost barriers;
- Expanding self-sampling, integrating it into HIV and primary care services, supported by community education;
- Investing in the capacity of the health system, including data systems, workforce training, and supply chain logistics;
- Utilizing innovative delivery models, such as mobile clinics and AI-based image analysis, to reach underserved populations;
- Engaging communities and women leaders, empowering them to increase the acceptance and supervision of prevention programs;
- Securing funding, supported by global pledges;
- In essence, cervical cancer disproportionally impacts women in LMICs, reflecting systemic inequities in vaccine access, screening capacity, and healthcare infrastructure. Barriers that range from cultural stigma to resource shortages compound the crisis. Nonetheless, digital health tools, self-sampling, simplified vaccination strategies, and WHO’s ambitious elimination framework offer a roadmap to equity and control. The imperative now is swift, integrated action and sustained investment.
7. Future Directions
7.1. Therapeutic HPV Vaccines and Immunotherapies
- A novel therapeutic vaccine (Vvax001) targeting HPV16 E6/E7 showed lesion regression in 17 of 18 CIN3 patients, with half experiencing complete regression and durable HPV clearance up to 19 weeks following vaccination;
- In-depth reviews describe multiple platforms—peptide, DNA, ribonucleic acid (RNA), and viral/inactivated vectors—currently in phase II and III trials, designed for CIN and invasive cancer treatment;
- New candidates like mHTV-03E2, an messenger RNA (mRNA)-based vaccine targeting HPV-16/18, have shown potent immunogenicity and strong preclinical efficacy;
- Industry efforts include Transgene’s TG4001 (HPV16 E6/E7), in phase II for metastatic cervical cancers.
7.2. Precision Diagnostics: Biomarkers and AI
- DNA methylation markers and HPV integration assays offer improved specificity in distinguishing remote/transient infections from lesions with malignant potential;
- Liquid biopsies detecting circulating HPV DNA may enable the early detection of cancer and real-time monitoring of treatment responses;
- AI-based image analyses (e.g., self-supervised learning on cytology slides) enhance automated triage and extend the diagnostic capacity to low-resource settings;
- These advances are especially beneficial in regions with a limited presence of specialists, allowing telepathology and remote diagnostics to close care gaps.
7.3. Expanded Vaccination Strategies
- Single-dose regimens for the nonavalent vaccine have demonstrated efficacy, offering cost-effective strategies for LMICs;
- Gender-neutral vaccination campaigns are gaining momentum, strengthening herd immunity and reducing non-cervical HPV cancers;
- Boosting vaccine equity requires immune profiling, affordable generics, cold-chain adaptation, and political commitment.
7.4. Self-Sampling and Decentralized Screening: The Integration of Prevention and Cancer Care, Policy, and Implementation Science
- The FDA-approved Teal Health at-home HPV test delivers clinical-equivalent sensitivity and the potential to close screening gaps, particularly among underserved populations;
- Combining therapeutic vaccinations post-surgery may reduce recurrence rates, while observational data support its efficacy;
- Point-of-care integrations: Merging HIV services, self-sampling, and AI tools, focusing on high-risk groups, and maximizing the screening yield;
- Modeling studies emphasize that scaling the 90-70-90 strategies with adult catch-ups could lead to elimination by 2061;
- Essential enablers include political will, funding, cold chain logistics for vaccines, community education, and accurate data systems;
- By reducing the reliance on clinic-based visits, these tools democratize early detection.
8. Conclusions
- Equitable vaccine delivery, including simplified dosing strategies and broader gender coverage;
- Accessible screening, leveraging self-sampling and HPV-based methods embedded into health systems;
- Innovative implementation, supporting diagnostics, treatment, and data systems tailored to low-resource contexts;
- Global solidarity, ensuring political commitment and sustained financing to close the equity gap.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| 2-valent/bvalent/bHPV vaccine | Bivalent (HPV-16/18) |
| 4-valent/qvalent/qHPV vaccine | Quadrivalent (HPV-6/11/16/18) |
| 9-valent/9vHPV vaccine | Nonavalent (HPV-6/11/16/18/31/33/45/52/58) |
| AI | Artificial Intelligence |
| ASHA | Accredited Social Health Activist |
| Arg | Arginine |
| CIN | Cervical intraepithelial neoplasia |
| CIN1 | Cervical intraepithelial neoplasia grade 1 |
| CIN2 | Cervical intraepithelial neoplasia grade 2 |
| CIN3 | Cervical intraepithelial neoplasia grade 3 |
| DNA | Deoxyribonucleic acid |
| E2F | Early Region 2 binding factor |
| E6AP | ubiquitin-protein ligase E3A |
| EGFR | Epidermal growth factor receptor |
| FDA | Food and Drug Administration |
| HIV | Human immunodeficiency virus |
| HLA | Human leukocyte antigen |
| HPV | Human papillomavirus |
| HPVs | Human papillomaviruses |
| hrHPV | High-risk HPV |
| hTERT | Human telomerase |
| LBC | Liquid-based cytology |
| LCR | Long control region |
| LMICs | Low- and middle-income countries |
| lrHPV | Low-risk HPV |
| MHC-I | Major Histocompatibility Complex Class I |
| mRNA | Messenger RNA |
| OC | Oral contraceptive |
| OR | Odds ratio |
| pRb | Retinoblastoma protein |
| RE-AIM | Reach, Effectiveness, Adoption, Implementation, and Maintenance |
| RNA | Ribonucleic acid |
| SCC | Squamous cell carcinoma |
| SEER | Surveillance, Epidemiology, and End Results Program |
| STIs | Sexually transmitted infections |
| UK | United Kingdom |
| US | United States |
| USPSTF | United States Preventive Services Task Force |
| VIA | Visual inspection with acetic acid |
| WLWH | Women living with HIV |
| WHO | World Health Organization |
References
- Zhou, L.; Li, Y.; Wang, H.; Qin, R.; Han, Z.; Li, R. Global cervical cancer elimination: Quantifying the status, progress, and gaps. BMC Med. 2025, 23, 67. [Google Scholar] [CrossRef] [PubMed]
- Jafari Sales, A.; Hosseini-Karkaj, K.; Soleymanpour, K.; Kadkhodaei-Ilkhechi, G.; Farahnaki-Sadabadi, M.; Pashazadeh, M. Human Papillomavirus and Cervical Cancer: A Narrative Review. Mod. Care J. 2025, 22, e159690. [Google Scholar] [CrossRef]
- Cervical Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer (accessed on 4 July 2025).
- Wu, J.; Jin, Q.; Zhang, Y.; Ji, Y.; Li, J.; Liu, X.; Duan, H.; Feng, Z.; Liu, Y.; Zhang, Y.; et al. Global burden of cervical cancer: Current estimates, temporal trend and future projections based on the GLOBOCAN 2022. J. Natl. Cancer Cent. 2025, 5, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Ramakrishnan, S.; Partricia, S.; Mathan, G. Overview of high-risk HPV’s 16 and 18 infected cervical cancer: Pathogenesis to prevention. Biomed. Pharmacother. 2015, 70, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Okunade, K.S. Human papillomavirus and cervical cancer. J. Obs. Gynaecol. 2020, 40, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Cervical Cancer Causes, Risk Factors, and Prevention. Available online: https://www.cancer.gov/types/cervical/causes-risk-prevention (accessed on 4 July 2025).
- Osmani, V.; Hörner, L.; Nkurunziza, T.; Rank, S.; Tanaka, L.F.; Klug, S.J. Global prevalence of cervical human papillomavirus in women aged 50 years and older with normal cytology: A systematic review and meta-analysis. Lancet Microbe 2025, 6, 100955. [Google Scholar] [CrossRef]
- Skinner, S.R.; Wheeler, C.M.; Romanowski, B.; Castellsagué, X.; Lazcano-Ponce, E.; Del Rosario-Raymundo, M.R.; Vallejos, C.; Minkina, G.; Pereira Da Silva, D.; McNeil, S.; et al. Progression of HPV infection to detectable cervical lesions or clearance in adult women: Analysis of the control arm of the VIVIANE study. Int. J. Cancer 2016, 138, 2428–2438. [Google Scholar] [CrossRef]
- Win, T.Z.K.; Simms, K.; Thinn, M.M.; Tin, K.N.; Aung, S.; Feletto, E.; Bateson, D.; Canfell, K. A Review of Human Papillomavirus Prevalence and Cervical Cancer in Myanmar. J. Epidemiol. Glob. Health 2025, 15, 89. [Google Scholar] [CrossRef]
- Borda, H.; Bloem, P.; Akaba, H.; Guillaume, D.; Willens, V.; Jurgensmeyer, M.; Muralidharan, K.; Limaye, R. Status of HPV disease and vaccination programmes in LMICs: Introduction to special issue. Vaccine 2024, 42, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Forman, D.; de Martel, C.; Lacey, C.J.; Soerjomataram, I.; Lortet-Tieulent, J.; Bruni, L.; Vignat, J.; Ferlay, J.; Bray, F.; Plummer, M.; et al. Global burden of human papillomavirus and related diseases. Vaccine 2012, 30 (Suppl. S5), F12–F23. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, E.M.; Kornepati, A.V.R.; Goldstein, M.; Bogerd, H.P.; Poling, B.C.; Whisnant, A.W.; Kastan, M.B.; Cullen, B.R. Inactivation of the Human Papillomavirus E6 or E7 Gene in Cervical Carcinoma Cells by Using a Bacterial CRISPR/Cas RNA-Guided Endonuclease. J. Virol. 2014, 88, 11965–11972. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, R.; Das, S.S.; Biswal, S.S.; Nath, A.; Das, D.; Basu, A.; Malik, S.; Kumar, L.; Kar, S.; Singh, S.K.; et al. Mechanistic role of HPV-associated early proteins in cervical cancer: Molecular pathways and targeted therapeutic strategies. Crit. Rev. Oncol. Hematol. 2022, 174, 103675. [Google Scholar] [CrossRef]
- Fischer, M.; Uxa, S.; Stanko, C.; Magin, T.M.; Engeland, K. Human papilloma virus E7 oncoprotein abrogates the p53-p21-DREAM pathway. Sci. Rep. 2017, 7, 2603. [Google Scholar] [CrossRef]
- Zhang, Y.; Qiu, K.; Ren, J.; Zhao, Y.; Cheng, P. Roles of human papillomavirus in cancers: Oncogenic mechanisms and clinical use. Signal Transduct. Target. Ther. 2025, 10, 44. [Google Scholar] [CrossRef]
- Huber, J.; Mueller, A.; Sailer, M.; Regidor, P.A. Human papillomavirus persistence or clearance after infection in reproductive age. What is the status? Review of the literature and new data of a vaginal gel containing silicate dioxide, citric acid, and selenite. Womens Health 2021, 17, 17455065211020702. [Google Scholar] [CrossRef]
- Rodríguez, A.C.; Schiffman, M.; Herrero, R.; Wacholder, S.; Hildesheim, A.; Castle, P.E.; Solomon, D.; Burk, R.; Proyecto Epidemiológico Guanacaste Group. Rapid Clearance of Human Papillomavirus and Implications for Clinical Focus on Persistent Infections. JNCI J. Natl. Cancer Inst. 2008, 100, 513–517. [Google Scholar] [CrossRef]
- Yusupov, A.; Popovsky, D.; Mahmood, L.; Kim, A.S.; Akman, A.E.; Yuan, H. The nonavalent vaccine: A review of high-risk HPVs and a plea to the CDC. Am. J. Stem. Cells 2019, 8, 52–64. [Google Scholar]
- Bruni, L.; Saura-Lázaro, A.; Montoliu, A.; Brotons, M.; Alemany, L.; Diallo, M.S.; Afsar, O.Z.; LaMontagne, D.S.; Mosina, L.; Contreras, M.; et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev. Med. 2021, 144, 106399. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Zhang, L.; Chen, Y.; Zhang, Y.; Wang, L.; Cai, R.; Li, M.; Dai, Y.; Dang, L.; Chen, H.; et al. Global HPV vaccination programs and coverage rates: A systematic review. EClinicalMedicine 2025, 84, 103290. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, S.; Agarwal, P.; Gupta, N. A comprehensive narrative review of challenges and facilitators in the implementation of various HPV vaccination program worldwide. Cancer Med. 2024, 13, e6862. [Google Scholar] [CrossRef]
- Bhalerao, V.; Gotarkar, S.; Muneshwar, K. The Impact of HPV Vaccination on Cervical Cancer in adolescent females: A narrative review. J. Fam. Med. Prim. Care 2024, 13, 4775–4782. [Google Scholar] [CrossRef]
- de Martel, C.; Plummer, M.; Vignat, J.; Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 2017, 141, 664–670. [Google Scholar] [CrossRef]
- Cervical Cancer Screening. Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3240 (accessed on 4 July 2025).
- Cervical Cancer Screening. Available online: https://www.ncbi.nlm.nih.gov/books/NBK65734/ (accessed on 4 July 2025).
- Gopalkrishnan, K.; Karim, R. Addressing Global Disparities in Cervical Cancer Burden: A Narrative Review of Emerging Strategies. Curr. HIV/AIDS Rep. 2025, 22, 18. [Google Scholar] [CrossRef]
- Eun, T.J.; Perkins, R.B. Screening for Cervical Cancer. Med. Clin. N. Am. 2020, 104, 1063–1078. [Google Scholar] [CrossRef] [PubMed]
- Kamath Mulki, A.; Withers, M. Human Papilloma Virus self-sampling performance in low- and middle-income countries. BMC Women’s Health 2021, 21, 12. [Google Scholar] [CrossRef]
- Duan, R.; Yang, H.; Zhai, X.; Yu, J.; Lu, C.; Yang, W.; Long, T.; Dao, Y.; Li, G.; Zhou, Y.; et al. Accuracy and acceptability of self-sampling HPV testing in cervical cancer screening: A population-based study in rural Yunnan, China. Sci. Rep. 2025, 15, 26390. [Google Scholar] [CrossRef] [PubMed]
- 2023 Global State of Cervical Cancer Awareness Report. Available online: https://www.bgi.com/global/news/bgi-genomics-global-2023-state-of-cervical-cancer-awareness-report (accessed on 4 July 2025).
- Ssentongo, P.; McCall-Hosenfeld, J.S.; Calo, W.A.; Moss, J.; Lengerich, E.J.; Chinchilli, V.M.; Ba, D.M. Association of human papillomavirus vaccination with cervical cancer screening: A systematic review and meta-analysis. Medicine 2022, 101, e29329. [Google Scholar] [CrossRef] [PubMed]
- Di Giuseppe, G.; Folcarelli, L.; Lanzano, R.; Napolitano, F.; Pavia, M. HPV Vaccination and Cervical Cancer Screening: Assessing Awareness, Attitudes, and Adherence in Detained Women. Vaccines 2022, 10, 1280. [Google Scholar] [CrossRef]
- Lin, W.; Wang, Y.; Liu, Z.; Chen, B.; Yuan, S.; Wu, B.; Gong, L. Awareness and attitude towards human papillomavirus and its vaccine among females with and without daughter(s) who participated in cervical cancer screening in Shenzhen, China. Trop. Med. Int. Health 2019, 24, 1054–1063. [Google Scholar] [CrossRef]
- Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. Available online: https://www.who.int/publications/i/item/9789240014107 (accessed on 4 July 2025).
- Ji, L.; Chen, M.; Yao, L. Strategies to eliminate cervical cancer in China. Front. Oncol. 2023, 13, 1105468. [Google Scholar] [CrossRef]
- Yang, X.; Qi, S.; Dai, L.; Ye, Q.; Li, X. Trends in HPV-positive cervical cancer prevalence: A retrospective study from 2013 to 2020. Virol. J. 2025, 22, 199. [Google Scholar] [CrossRef]
- Canfell, K.; Kim, J.J.; Brisson, M.; Keane, A.; Simms, K.T.; Caruana, M.; Burger, E.A.; Martin, D.; Nguyen, D.T.N.; Bénard, É.; et al. Mortality impact of achieving WHO cervical cancer elimination targets: A comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet 2020, 395, 591–603. [Google Scholar] [CrossRef] [PubMed]
- 5 fast facts about HPV and cervical cancer. Available online: https://www.unicef.org/stories/fast-facts-hpv-cervical-cancer (accessed on 4 July 2025).
- Petersen, Z.; Jaca, A.; Ginindza, T.G.; Maseko, G.; Takatshana, S.; Ndlovu, P.; Zondi, N.; Zungu, N.; Varghese, C.; Hunting, G.; et al. Barriers to uptake of cervical cancer screening services in low-and-middle-income countries: A systematic review. BMC Women’s Health 2022, 22, 486. [Google Scholar] [CrossRef]
- Stelzle, D.; Tanaka, L.F.; Lee, K.K.; Ibrahim Khalil, A.; Baussano, I.; Shah, A.S.V.; McAllister, D.A.; Gottlieb, S.L.; Klug, S.J.; Winkler, A.S.; et al. Estimates of the global burden of cervical cancer associated with HIV. Lancet Glob. Health 2020, 9, e119, Correction in Lancet Glob. Health 2021, 9, e161–e169. [Google Scholar] [CrossRef]
- Human papillomavirus and cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/human-papilloma-virus-and-cancer (accessed on 4 July 2025).
- Cancer Stat Facts: Cervical Cancer. Available online: https://seer.cancer.gov/statfacts/html/cervix.html (accessed on 4 July 2025).
- Key Statistics for Cervical Cancer. Available online: https://www.cancer.org/cancer/types/cervical-cancer/about/key-statistics.html (accessed on 4 July 2025).
- Cheng, X.; Wang, P.; Cheng, L.; Zhao, F.; Liu, J. Trends in cervical cancer incidence and mortality in the United States, 1975–2018: A population-based study. Front. Med. 2025, 12, 1579446. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.K.; Aimagambetova, G.; Ukybassova, T.; Kongrtay, K.; Azizan, A. Human Papillomavirus Infection and Cervical Cancer: Epidemiology, Screening, and Vaccination—Review of Current Perspectives. J. Oncol. 2019, 2019, 3257939. [Google Scholar] [CrossRef]
- Zhang, S.; Xu, H.; Zhang, L.; Qiao, Y. Cervical cancer: Epidemiology, risk factors and screening. Chin. J. Cancer Res. 2020, 32, 720–728. [Google Scholar] [CrossRef]
- HPV PREVENTION AT A GLANCE. Available online: https://hpvcentre.net/hpvatglance.php (accessed on 4 July 2025).
- Human Papillomavirus and Related Diseases Report. Available online: https://hpvcentre.net/statistics/reports/XWX.pdf (accessed on 4 July 2025).
- Berza, N.; Zodzika, J.; Kivite-Urtane, A.; Baltzer, N.; Curkste, A.; Pole, I.; Nygård, M.; Pärna, K.; Stankunas, M.; Tisler, A.; et al. Understanding the high-risk human papillomavirus prevalence and associated factors in the European country with a high incidence of cervical cancer. Eur. J. Public Health 2024, 34, 826–832. [Google Scholar] [CrossRef] [PubMed]
- Mazurec, K.; Trzeszcz, M.; Mazurec, M.; Kobierzycki, C.; Jach, R.; Halon, A. Distribution of 14 High-Risk HPV Types and p16/Ki67 Dual-Stain Status in Post-Colposcopy Histology Results: Negative, Low- and High-Grade Cervical Squamous Intraepithelial Lesions. Cancers 2024, 16, 3401. [Google Scholar] [CrossRef]
- Shi, R.; Qi, W.; Wang, Z.; Cai, J.; Zhao, M.; Wang, Z. High-risk human papillomavirus genotype distribution and attribution to cervical lesions in a Shanxi Province screening population. Sci. Rep. 2025, 15, 28217. [Google Scholar] [CrossRef] [PubMed]
- Aden, D.; Zaheer, S.; Khan, S.; Jairajpuri, Z.S.; Jetley, S. Navigating the landscape of HPV-associated cancers: From epidemiology to prevention. Pathol.-Res. Pract. 2024, 263, 155574. [Google Scholar] [CrossRef]
- Li, S.; Liu, C.; Weng, L. Exploring Cervical Adenocarcinoma: Epidemiological Insights, Diagnostic and Therapeutic Challenges, and Pathogenetic Mechanisms. Cancer Med. 2025, 14, e70620. [Google Scholar] [CrossRef]
- Islami, F.; Fedewa, S.A.; Jemal, A. Trends in cervical cancer incidence rates by age, race/ethnicity, histological subtype, and stage at diagnosis in the United States. Prev. Med. 2019, 123, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Broshkevitch, C.J.; Barnabas, R.V.; Liu, G.; Palanee-Phillips, T.; Rao, D.W. Enhanced cervical cancer and HIV interventions reduce the disproportionate burden of cervical cancer cases among women living with HIV: A modeling analysis. PLoS ONE 2024, 19, e0301997. [Google Scholar] [CrossRef]
- Luvián-Morales, J.; Gutiérrez-Enríquez, S.O.; Granados-García, V.; Torres-Poveda, K. Risk factors for the development of cervical cancer: Analysis of the evidence. Front. Oncol. 2024, 14, 1378549. [Google Scholar] [CrossRef]
- Fonseca-Moutinho, J.A. Smoking and cervical cancer. ISRN Obs. Gynecol. 2011, 2011, 847684. [Google Scholar] [CrossRef] [PubMed]
- Bowden, S.J.; Doulgeraki, T.; Bouras, E.; Markozannes, G.; Athanasiou, A.; Grout-Smith, H.; Kechagias, K.S.; Ellis, L.B.; Zuber, V.; Chadeau-Hyam, M.; et al. Risk factors for human papillomavirus infection, cervical intraepithelial neoplasia and cervical cancer: An umbrella review and follow-up Mendelian randomisation studies. BMC Med. 2023, 21, 274. [Google Scholar] [CrossRef] [PubMed]
- Khalil, A.; Mpunga, T.; Wei, F.; Baussano, I.; de Martel, C.; Bray, F.; Stelzle, D.; Dryden-Peterson, S.; Jaquet, A.; Horner, M.J.; et al. Age-specific burden of cervical cancer associated with HIV: A global analysis with a focus on sub-Saharan Africa. Int. J. Cancer 2021, 150, 761–772. [Google Scholar] [CrossRef]
- Li, X.; Wu, J.; Wu, Y.; Duan, Z.; Luo, M.; Li, L.; Li, S.; Jia, Y. Imbalance of Vaginal Microbiota and Immunity: Two Main Accomplices of Cervical Cancer in Chinese Women. Int. J. Womens Health 2023, 15, 987–1002. [Google Scholar] [CrossRef]
- Mazinani, S.; Aghazadeh, M.; Poortahmasebi, V.; Arafi, V.; Hasani, A. Cervical cancer pathology and vaginal and gut microbiota: Conception of the association. Lett. Appl. Microbiol. 2025, 78, ovaf088. [Google Scholar] [CrossRef]
- Peng, Y.; Tang, Q.; Wu, S.; Zhao, C. Associations of Atopobium, Garderella, Megasphaera, Prevotella, Sneathia, and Streptococcus with human papillomavirus infection, cervical intraepithelial neoplasia, and cancer: A systematic review and meta-analysis. BMC Infect. Dis. 2025, 25, 708. [Google Scholar] [CrossRef]
- Mitra, A.; MacIntyre, D.A.; Marchesi, J.R.; Lee, Y.S.; Bennett, P.R.; Kyrgiou, M. The vaginal microbiota, human papillomavirus infection and cervical intraepithelial neoplasia: What do we know and where are we going next? Microbiome 2016, 4, 58. [Google Scholar] [CrossRef]
- Chen, H.; Luo, L.; Wen, Y.; He, B.; Ling, H.; Shui, J.; He, P.; Hou, X.; Tang, S.; Li, Z. Chlamydia trachomatis and Human Papillomavirus Infection in Women From Southern Hunan Province in China: A Large Observational Study. Front. Microbiol. 2020, 11, 827. [Google Scholar] [CrossRef]
- Zhu, H.; Shen, Z.; Luo, H.; Zhang, W.; Zhu, X. Chlamydia Trachomatis Infection-Associated Risk of Cervical Cancer: A Meta-Analysis. Medicine 2016, 95, e3077. [Google Scholar] [CrossRef] [PubMed]
- Javadi, K.; Ferdosi-Shahandashti, E.; Rajabnia, M.; Khaledi, M. Vaginal microbiota and gynecological cancers: A complex and evolving relationship. Infect. Agent. Cancer 2024, 19, 27. [Google Scholar] [CrossRef]
- Wei, Z.-T.; Chen, H.-L.; Wang, C.-F.; Yang, G.-L.; Han, S.-M.; Zhang, S.-L. Depiction of Vaginal Microbiota in Women with High-Risk Human Papillomavirus Infection. Front. Public Health 2021, 8, 587298. [Google Scholar] [CrossRef] [PubMed]
- Koster, S.; Gurumurthy, R.K.; Kumar, N.; Prakash, P.G.; Dhanraj, J.; Bayer, S.; Berger, H.; Kurian, S.M.; Drabkina, M.; Mollenkopf, H.-J.; et al. Modelling Chlamydia and HPV co-infection in patient-derived ectocervix organoids reveals distinct cellular reprogramming. Nat. Commun. 2022, 13, 1030. [Google Scholar] [CrossRef] [PubMed]
- Tekalegn, Y.; Sahiledengle, B.; Woldeyohannes, D.; Atlaw, D.; Degno, S.; Desta, F.; Bekele, K.; Aseffa, T.; Gezahegn, H.; Kene, C. High parity is associated with increased risk of cervical cancer: Systematic review and meta-analysis of case-control studies. Womens Health 2022, 18, 17455065221075904. [Google Scholar] [CrossRef]
- Bovo, A.C.; Pedrão, P.G.; Guimarães, Y.M.; Godoy, L.R.; Resende, J.C.P.; Longatto-Filho, A.; Reis, R.D. Combined Oral Contraceptive Use and the Risk of Cervical Cancer: Literature Review. Rev. Bras. Ginecol. Obstet. 2023, 45, e818–e824. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.S.; Bratti, M.C.; Rodríguez, A.C.; Herrero, R.; Burk, R.D.; Porras, C.; González, P.; Sherman, M.E.; Wacholder, S.; Lan, Z.E.; et al. Common Variants in Immune and DNA Repair Genes and Risk for Human Papillomavirus Persistence and Progression to Cervical Cancer. J. Infect. Dis. 2009, 199, 20–30. [Google Scholar] [CrossRef]
- Hu, X.; Zhang, Z.; Ma, D.; Huettner, P.C.; Massad, L.S.; Nguyen, L.; Borecki, I.; Rader, J.S. TP53, MDM2, NQO1, and susceptibility to cervical cancer. Cancer Epidemiol. Biomark. Prev. 2010, 19, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Adebamowo, S.N.; Adeyemo, A.; Adebayo, A.; Achara, P.; Alabi, B.; Bakare, R.A.; Famooto, A.O.; Obende, K.; Offiong, R.; Olaniyan, O.; et al. Genome, HLA and polygenic risk score analyses for prevalent and persistent cervical human papillomavirus (HPV) infections. Eur. J. Hum. Genet. 2024, 32, 708–716. [Google Scholar] [CrossRef]
- Human Papillomavirus (HPV) Infection. Available online: https://www.ncbi.nlm.nih.gov/books/NBK321770/ (accessed on 4 July 2025).
- Haręża, D.A.; Wilczyński, J.R.; Paradowska, E. Human Papillomaviruses as Infectious Agents in Gynecological Cancers. Oncogenic Properties of Viral Proteins. Int. J. Mol. Sci. 2022, 23, 1818. [Google Scholar] [CrossRef]
- Cerqueira, C.; Schiller, J.T. Papillomavirus assembly: An overview and perspectives. Virus Res. 2017, 231, 103–107. [Google Scholar] [CrossRef]
- Egawa, N.; Egawa, K.; Griffin, H.; Doorbar, J. Human Papillomaviruses; Epithelial Tropisms, and the Development of Neoplasia. Viruses 2015, 7, 3863–3890. [Google Scholar] [CrossRef]
- Kirk, A.; Graham, S.V. The human papillomavirus late life cycle and links to keratinocyte differentiation. J. Med. Virol. 2024, 96, e29461. [Google Scholar] [CrossRef] [PubMed]
- Finnen, R.L.; Erickson, K.D.; Chen, X.S.; Garcea, R.L. Interactions between papillomavirus L1 and L2 capsid proteins. J Virol 2003, 77, 4818–4826. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Ma, Y.; Zhang, N.; Li, L.; Fu, Y.; Li, L.; Zhai, Q. Methylation testing versus cervical cytology for triage of HPV-positive women: A comparative study. Diagn. Microbiol. Infect. Dis. 2025, 113, 116917. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Elfström, K.M.; Dillner, J. Human papillomavirus-based cervical screening and long-term cervical cancer risk: A randomised health-care policy trial in Sweden. Lancet Public Health 2024, 9, e886–e895. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D. A review of cross-protection against oncogenic HPV by an HPV-16/18 AS04-adjuvanted cervical cancer vaccine: Importance of virological and clinical endpoints and implications for mass vaccination in cervical cancer prevention. Gynecol. Oncol. 2008, 110, S18–S25. [Google Scholar] [CrossRef]
- Cho, E.H.; Park, M.S.; Woo, H.Y.; Park, H.; Kwon, M.J. Evaluation of clinical usefulness of HPV-16 and HPV-18 genotyping for cervical cancer screening. J. Gynecol. Oncol. 2024, 35, e72. [Google Scholar] [CrossRef] [PubMed]
- Zou, Z.; Fairley, C.K.; Ong, J.J.; Shen, M.; Chow, E.P.F.; Liu, H.; Xia, R.; Li, R.; Hocking, J.; Zhuang, G.; et al. Impact of achieving WHO’s 90-70-90 targets on cervical cancer elimination and potential benefits in preventing other HPV-related cancers in China: A modelling study. EClinicalMedicine 2024, 77, 102878. [Google Scholar] [CrossRef] [PubMed]
- Sumiec, E.G.; Yim, Z.Y.; Mohy-Eldin, H.; Nedjai, B. The current state of DNA methylation biomarkers in self-collected liquid biopsies for the early detection of cervical cancer: A literature review. Infect. Agent. Cancer 2024, 19, 62. [Google Scholar] [CrossRef]
- Gomes, M.; Provaggi, E.; Pembe, A.B.; Olaitan, A.; Gentry-Maharaj, A. Advancing Cervical Cancer Prevention Equity: Innovations in Self-Sampling and Digital Health Technologies Across Healthcare Settings. Diagnostics 2025, 15, 1176. [Google Scholar] [CrossRef]
- Zolfi, E.; Khaleghi Mehr, F.; Emtiazi, N.; Moradi, Y. A review of the carcinogenic potential of human papillomavirus (HPV) in urological cancers. Virol. J. 2025, 22, 53. [Google Scholar] [CrossRef]
- Williams, G.A., 2nd; Wu, A.A.; Eugene, H.C.; Tsai, Y.C.; Wong, M.; Nonogaki, H.; Roden, R.B.S.; Hung, C.F.; Wu, T.C.; Vang, R.; et al. Clinicopathologic Features and Viral Status of Low-risk HPV6 and HPV11-Associated Squamous Cell Carcinoma of the Uterine Cervix and Vulva. Am. J. Surg. Pathol. 2025, 49, 458–470. [Google Scholar] [CrossRef] [PubMed]
- Mlynarczyk-Bonikowska, B.; Rudnicka, L. HPV Infections—Classification, Pathogenesis, and Potential New Therapies. Int. J. Mol. Sci. 2024, 25, 7616. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Huang, H.; Tang, Y.; Ren, X.; Jiang, X.; Tian, M.; Li, W. Unveiling the multifaceted realm of human papillomavirus: A comprehensive exploration of biology, interactions, and advances in cancer management. Front. Immunol. 2024, 15, 1430544. [Google Scholar] [CrossRef] [PubMed]
- Human papillomavirus vaccines: WHO position paper. Available online: https://www.who.int/publications/i/item/who-wer9750-645-672 (accessed on 4 July 2025).
- Burd, E.M. Human papillomavirus and cervical cancer. Clin. Microbiol. Rev. 2003, 16, 1–17. [Google Scholar] [CrossRef]
- Muñoz, N.; Bosch, F.X.; Sanjosé, S.d.; Herrero, R.; Castellsagué, X.; Shah, K.V.; Snijders, P.J.F.; Meijer, C.J.L.M. Epidemiologic Classification of Human Papillomavirus Types Associated with Cervical Cancer. N. Engl. J. Med. 2003, 348, 518–527. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Q.; He, M.; Mao, Z.; Huang, Y.; Li, X.; Long, L.; Guo, M.; Zou, D. Advancing the Fight Against Cervical Cancer: The Promise of Therapeutic HPV Vaccines. Vaccines 2025, 13, 92. [Google Scholar] [CrossRef]
- Human Papillomavirus Type 51. Available online: https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/human-papillomavirus-type-51 (accessed on 4 July 2025).
- Nikolic, N.; Basica, B.; Strbac, M.; Terzic, L.; Patic, A.; Kovacevic, G.; Velicki, R.; Petrovic, D.; Mandic, A.; Petrovic, V. Prevalence of Carcinogenic Genotypes of HPV-Infected Women in a Ten-Year Period (2014–2023) in Vojvodina, Serbia. Medicina 2024, 60, 922. [Google Scholar] [CrossRef]
- Liu, Y.; Ai, H. Comprehensive insights into human papillomavirus and cervical cancer: Pathophysiology, screening, and vaccination strategies. Biochim. Biophys. Acta (BBA)-Rev. Cancer 2024, 1879, 189192. [Google Scholar] [CrossRef]
- Pavelescu, L.A.; Mititelu-Zafiu, N.L.; Mindru, D.E.; Vladareanu, R.; Curici, A. Molecular Insights into HPV-Driven Cervical Cancer: Oncoproteins, Immune Evasion, and Epigenetic Modifications. Microorganisms 2025, 13, 1000. [Google Scholar] [CrossRef]
- Baba, S.K.; Alblooshi, S.S.E.; Yaqoob, R.; Behl, S.; Al Saleem, M.; Rakha, E.A.; Malik, F.; Singh, M.; Macha, M.A.; Akhtar, M.K.; et al. Human papilloma virus (HPV) mediated cancers: An insightful update. J. Transl. Med. 2025, 23, 483. [Google Scholar] [CrossRef]
- Downham, L.; Jaafar, I.; Rol, M.L.; Nyawira Nyaga, V.; Valls, J.; Baena, A.; Zhang, L.; Gunter, M.J.; Arbyn, M.; Almonte, M. Accuracy of HPV E6/E7 oncoprotein tests to detect high-grade cervical lesions: A systematic literature review and meta-analysis. Br. J. Cancer 2024, 130, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Janiszewska, J.; Kostrzewska-Poczekaj, M.; Wierzbicka, M.; Brenner, J.C.; Giefing, M. HPV-driven oncogenesis-much more than the E6 and E7 oncoproteins. J. Appl. Genet. 2025, 66, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Obanya, D.I.; Wootton, L.M.; Morgan, E.L. Advances in understanding the mechanisms of the human papillomavirus oncoproteins. Biochem. Soc. Trans. 2025, 53, 565–577. [Google Scholar] [CrossRef]
- Han, F.; Guo, X.-y.; Jiang, M.-x.; Xia, N.-s.; Gu, Y.; Li, S.-w. Structural biology of the human papillomavirus. Structure 2024, 32, 1877–1892. [Google Scholar] [CrossRef]
- Mahendra, I.N.B.; Prayudi, P.K.A.; Dwija, I.; Suwiyoga, K. HPV16-E6/E7 Oncogene Mutation and p53 Expression among Indonesian Women with Cervical Cancer. Asian Pac J Cancer Prev 2022, 23, 2705–2711. [Google Scholar] [CrossRef] [PubMed]
- Mesplède, T.; Gagnon, D.; Bergeron-Labrecque, F.; Azar, I.; Sénéchal, H.; Coutlée, F.; Archambault, J. p53 degradation activity, expression, and subcellular localization of E6 proteins from 29 human papillomavirus genotypes. J. Virol. 2012, 86, 94–107. [Google Scholar] [CrossRef]
- Mir, B.A.; Ahmad, A.; Farooq, N.; Priya, M.V.; Siddiqui, A.H.; Asif, M.; Manzoor, R.; Ishqi, H.M.; Alomar, S.Y.; Rahaman, P.F. Increased expression of HPV-E7 oncoprotein correlates with a reduced level of pRb proteins via high viral load in cervical cancer. Sci. Rep. 2023, 13, 15075. [Google Scholar] [CrossRef]
- Wang, H.; Mo, P.; Ren, S.; Yan, C. Activating transcription factor 3 activates p53 by preventing E6-associated protein from binding to E6. J. Biol. Chem. 2010, 285, 13201–13210. [Google Scholar] [CrossRef]
- de Freitas, A.C.; de Oliveira, T.H.A.; Barros, M.R., Jr.; Venuti, A. hrHPV E5 oncoprotein: Immune evasion and related immunotherapies. J Exp Clin Cancer Res 2017, 36, 71. [Google Scholar] [CrossRef]
- Liu, X.; Clements, A.; Zhao, K.; Marmorstein, R. Structure of the Human Papillomavirus E7 Oncoprotein and Its Mechanism for Inactivation of the Retinoblastoma Tumor Suppressor*. J. Biol. Chem. 2006, 281, 578–586. [Google Scholar] [CrossRef] [PubMed]
- Diakite, I.; Martins, B.; Owusu-Edusei, K.; Palmer, C.; Patterson-Lomba, O.; Gomez-Lievano, A.; Zion, A.; Simpson, R.; Daniels, V.; Elbasha, E. Structured Literature Review to Identify Human Papillomavirus’s Natural History Parameters for Dynamic Population Models of Vaccine Impacts. Infect. Dis. Ther. 2024, 13, 965–990. [Google Scholar] [CrossRef] [PubMed]
- Gravitt, P.E.; Winer, R.L. Natural History of HPV Infection across the Lifespan: Role of Viral Latency. Viruses 2017, 9, 267. [Google Scholar] [CrossRef]
- Zhao, M.; Kang, P.; Zhu, L.; Zhou, D.; Cui, M.; Zhang, M.; Jia, J.; Luo, L. Global pattern of persistent human papillomavirus infection in female genital tract: An update system review and meta-analysis. iScience 2024, 27, 110991. [Google Scholar] [CrossRef] [PubMed]
- Graham, S.V. The human papillomavirus replication cycle, and its links to cancer progression: A comprehensive review. Clin. Sci. 2017, 131, 2201–2221. [Google Scholar] [CrossRef]
- Ali, M.; Sinha, R.; Kumar, A.; Karim, S.; Irfan, M.; Kumar, S.; Sinha, S.; Kumar, A.; Ghosh, A.; Singh, M. HPV DNA status and clinical history of patients are supplements for accurate reporting of the cytological Pap smear. Sci. Rep. 2024, 14, 17486. [Google Scholar] [CrossRef]
- Della Fera, A.N.; Warburton, A.; Coursey, T.L.; Khurana, S.; McBride, A.A. Persistent Human Papillomavirus Infection. Viruses 2021, 13, 321. [Google Scholar] [CrossRef]
- Kombe Kombe, A.J.; Li, B.; Zahid, A.; Mengist, H.M.; Bounda, G.-A.; Zhou, Y.; Jin, T. Epidemiology and Burden of Human Papillomavirus and Related Diseases, Molecular Pathogenesis, and Vaccine Evaluation. Front. Public Health 2021, 8, 552028. [Google Scholar] [CrossRef]
- Perkins, R.B.; Guido, R.S.; Castle, P.E.; Chelmow, D.; Einstein, M.H.; Garcia, F.; Huh, W.K.; Kim, J.J.; Moscicki, A.B.; Nayar, R.; et al. 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors. J. Low. Genit. Tract. Dis. 2020, 24, 102–131, Erratum in J. Low. Genit. Tract. Dis. 2021, 25, 330–331. [Google Scholar] [CrossRef] [PubMed]
- Sykes, P.H.; Simcock, B.J.; Innes, C.R.; Harker, D.; Williman, J.A.; Whitehead, M.; van der Griend, R.A.; Lawton, B.A.; Hibma, M.; Fitzgerald, P.; et al. Predicting regression of cervical intraepithelial neoplasia grade 2 in women under 25 years. Am. J. Obstet. Gynecol. 2022, 226, 222.e1–222.e13. [Google Scholar] [CrossRef] [PubMed]
- Moscicki, A.B.; Ma, Y.; Wibbelsman, C.; Darragh, T.M.; Powers, A.; Farhat, S.; Shiboski, S. Rate of and risks for regression of cervical intraepithelial neoplasia 2 in adolescents and young women. Obs. Gynecol. 2010, 116, 1373–1380. [Google Scholar] [CrossRef]
- Ehret, A.; Bark, V.N.; Mondal, A.; Fehm, T.N.; Hampl, M. Regression rate of high-grade cervical intraepithelial lesions in women younger than 25 years. Arch. Gynecol. Obstet. 2023, 307, 981–990. [Google Scholar] [CrossRef]
- Lee, M.H.; Finlayson, S.J.; Gukova, K.; Hanley, G.; Miller, D.; Sadownik, L.A. Outcomes of Conservative Management of High Grade Squamous Intraepithelial Lesions in Young Women. J. Low. Genit. Tract Dis. 2018, 22, 212–218. [Google Scholar] [CrossRef]
- de Sanjosé, S.; Brotons, M.; Pavón, M.A. The natural history of human papillomavirus infection. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 47, 2–13. [Google Scholar] [CrossRef] [PubMed]
- Bedell, S.L.; Goldstein, L.S.; Goldstein, A.R.; Goldstein, A.T. Cervical Cancer Screening: Past, Present, and Future. Sex. Med. Rev. 2020, 8, 28–37. [Google Scholar] [CrossRef]
- Cuschieri, K.; Bhatia, R.; Cruickshank, M.; Hillemanns, P.; Arbyn, M. HPV testing in the context of post-treatment follow up (test of cure). J. Clin. Virol. 2016, 76, S56–S61. [Google Scholar] [CrossRef]
- Ramírez, A.T.; Valls, J.; Baena, A.; Rojas, F.D.; Ramírez, K.; Álvarez, R.; Cristaldo, C.; Henríquez, O.; Moreno, A.; Reynaga, D.C.; et al. Performance of cervical cytology and HPV testing for primary cervical cancer screening in Latin America: An analysis within the ESTAMPA study. Lancet Reg. Health–Am. 2023, 26, 100593. [Google Scholar] [CrossRef] [PubMed]
- Alonso, I.; Torné, A.; Puig-Tintoré, L.M.; Esteve, R.; Quinto, L.; Campo, E.; Pahisa, J.; Ordi, J. Pre- and post-conization high-risk HPV testing predicts residual/recurrent disease in patients treated for CIN 2–3. Gynecol. Oncol. 2006, 103, 631–636. [Google Scholar] [CrossRef]
- Clarke, M.A.; Deshmukh, A.A.; Suk, R.; Roberts, J.; Gilson, R.; Jay, N.; Stier, E.A.; Wentzensen, N. A systematic review and meta-analysis of cytology and HPV-related biomarkers for anal cancer screening among different risk groups. Int. J. Cancer 2022, 151, 1889–1901. [Google Scholar] [CrossRef]
- Mariani, L.; Sandri, M.T.; Preti, M.; Origoni, M.; Costa, S.; Cristoforoni, P.; Bottari, F.; Sideri, M. HPV-Testing in Follow-up of Patients Treated for CIN2+ Lesions. J. Cancer 2016, 7, 107–114. [Google Scholar] [CrossRef]
- Immunization Coverage. Available online: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed on 4 July 2025).
- Naidoo, D.; Govender, K.; Mantell, J.E. Breaking barriers: Why including boys and men is key to HPV prevention. BMC Med. 2024, 22, 525. [Google Scholar] [CrossRef]
- Kim, J.; Choe, Y.J.; Park, J.; Cho, J.; Cheong, C.; Oh, J.-K.; Park, M.; Shim, E.; Yu, S.-Y. Comparative Effects of Bivalent, Quadrivalent, and Nonavalent Human Papillomavirus Vaccines in The Prevention of Genotype-Specific Infection: A Systematic Review and Network Meta-Analysis. Infect. Chemother. 2024, 56, 37–46. [Google Scholar] [CrossRef]
- Williamson, A.L. Recent Developments in Human Papillomavirus (HPV) Vaccinology. Viruses 2023, 15, 1440. [Google Scholar] [CrossRef]
- Kamolratanakul, S.; Pitisuttithum, P. Human Papillomavirus Vaccine Efficacy and Effectiveness against Cancer. Vaccines 2021, 9, 1413. [Google Scholar] [CrossRef]
- Asare, M.; Elizondo, A.; Dwumfour-Poku, M.; Mena, C.; Gutierrez, M.; Mamudu, H.M. Intervention to Increase Cervical Cancer Screening Behavior among Medically Underserved Women: Effectiveness of 3R Communication Model. Healthcare 2023, 11, 1323. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Choi, W.; Shim, E. Cost-Effectiveness of Human Papillomavirus Vaccination in the UK: Two Versus Single-Dose of Nonavalent HPV Vaccination. Am. J. Prev. Med. 2024, 67, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Harper, D.M.; Navarro-Alonso, J.A.; Bosch, F.X.; Paavonen, J.; Stanley, M.; Sasieni, P.; Yébenes, M.; Martínez-Martínez, N.; Rodriguez, Á.; García, A.; et al. Impact of human papillomavirus vaccines in the reduction of infection, precursor lesions, and cervical cancer: A systematic literature review. Hum. Vaccin. Immunother. 2025, 21, 2497608. [Google Scholar] [CrossRef]
- Rostami Varnousfaderani, M.; Khoshnazar, Z.; Zeratie, H.; Hosseini Koukamari, P. Optimizing HPV vaccine effectiveness: Impact of vaccination age and dose schedule on immunogenicity and cervical cancer prevention. Front. Public Health 2025, 13, 1544220. [Google Scholar] [CrossRef]
- Gardasil 9. Available online: https://www.merck.com/product/usa/pi_circulars/g/gardasil_9/gardasil_9_pi.pdf (accessed on 4 July 2025).
- Gardasil. Available online: https://www.fda.gov/files/vaccines%2C%20blood%20%26%20biologics/published/Package-Insert---Gardasil.pdf (accessed on 4 July 2025).
- Cervavarix. Available online: https://www.fda.gov/media/78013/download?attachment (accessed on 4 July 2025).
- Zaman, K.; Schuind, A.E.; Adjei, S.; Antony, K.; Aponte, J.J.; Buabeng, P.B.; Qadri, F.; Kemp, T.J.; Hossain, L.; Pinto, L.A.; et al. Safety and immunogenicity of Innovax bivalent human papillomavirus vaccine in girls 9–14 years of age: Interim analysis from a phase 3 clinical trial. Vaccine 2024, 42, 2290–2298. [Google Scholar] [CrossRef]
- Walrinvax. Available online: https://extranet.who.int/prequal/vaccines/p/walrinvaxr (accessed on 4 July 2025).
- Cervavac. Available online: https://www.seruminstitute.com/product_ind_cervavac.php (accessed on 4 July 2025).
- Gardasil. Available online: https://www.ema.europa.eu/en/documents/product-information/gardasil-epar-product-information_en.pdf (accessed on 4 July 2025).
- Cervarix. Available online: https://www.ema.europa.eu/en/documents/product-information/cervarix-epar-product-information_en.pdf (accessed on 4 July 2025).
- WHO PUBLIC ASSESSMENT REPORT (WHOPAR) Cecolin. Available online: https://extranet.who.int/prequal/sites/default/files/vwa_vaccine/FVP-P-389_HVP_Innovax_WHOPAR_2025.pdf (accessed on 4 July 2025).
- Falcaro, M.; Soldan, K.; Ndlela, B.; Sasieni, P. Effect of the HPV vaccination programme on incidence of cervical cancer and grade 3 cervical intraepithelial neoplasia by socioeconomic deprivation in England: Population based observational study. BMJ 2024, 385, e077341. [Google Scholar] [CrossRef]
- Checchi, M.; Mesher, D.; Panwar, K.; Anderson, A.; Beddows, S.; Soldan, K. The impact of over ten years of HPV vaccination in England: Surveillance of type-specific HPV in young sexually active females. Vaccine 2023, 41, 6734–6744. [Google Scholar] [CrossRef] [PubMed]
- Palmer, T.; Wallace, L.; Pollock, K.G.; Cuschieri, K.; Robertson, C.; Kavanagh, K.; Cruickshank, M. Prevalence of cervical disease at age 20 after immunisation with bivalent HPV vaccine at age 12–13 in Scotland: Retrospective population study. BMJ 2019, 365, l1161. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Ploner, A.; Elfström, K.M.; Wang, J.; Roth, A.; Fang, F.; Sundström, K.; Dillner, J.; Sparén, P. HPV Vaccination and the Risk of Invasive Cervical Cancer. N. Engl. J. Med. 2020, 383, 1340–1348. [Google Scholar] [CrossRef] [PubMed]
- Patel, C.; Brotherton, J.M.; Pillsbury, A.; Jayasinghe, S.; Donovan, B.; Macartney, K.; Marshall, H. The impact of 10 years of human papillomavirus (HPV) vaccination in Australia: What additional disease burden will a nonavalent vaccine prevent? Eurosurveillance 2018, 23, 1700737. [Google Scholar] [CrossRef]
- Gargano, J.W.; Stefanos, R.; Dahl, R.M.; Castilho, J.L.; Bostick, E.A.; Niccolai, L.M.; Park, I.U.; Blankenship, S.; Brackney, M.M.; Chan, K.; et al. Trends in Cervical Precancers Identified Through Population-Based Surveillance-Human Papillomavirus Vaccine Impact Monitoring Project, Five Sites, United States, 2008–2022. MMWR Morb. Mortal. Wkly. Rep. 2025, 74, 96–101. [Google Scholar] [CrossRef]
- Nonboe, M.H.; Napolitano, G.M.; Schroll, J.B.; Andersen, B.; Bennetsen, M.H.; Christiansen, S.; Frandsen, A.P.; Rygaard, C.; Salmani, R.; Høgdall, E.V.S.; et al. Human papillomavirus prevalence in first, second and third cervical cell samples from women HPV-vaccinated as girls, Denmark, 2017 to 2024: Data from the Trial23 cohort study. Eurosurveillance 2025, 30, 2400820. [Google Scholar] [CrossRef]
- Mikalsen, M.P.; Simonsen, G.S.; Sørbye, S.W. Impact of HPV Vaccination on the Incidence of High-Grade Cervical Intraepithelial Neoplasia (CIN2+) in Women Aged 20–25 in the Northern Part of Norway: A 15-Year Study. Vaccines 2024, 12, 421. [Google Scholar] [CrossRef]
- Drolet, M.; Bénard, É.; Pérez, N.; Brisson, M.; Ali, H.; Boily, M.-C.; Baldo, V.; Brassard, P.; Brotherton, J.M.L.; Callander, D.; et al. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: Updated systematic review and meta-analysis. Lancet 2019, 394, 497–509. [Google Scholar] [CrossRef]
- Reuschenbach, M.; Doorbar, J.; del Pino, M.; Joura, E.A.; Walker, C.; Drury, R.; Rauscher, A.; Saah, A.J. Prophylactic HPV vaccines in patients with HPV-associated diseases and cancer. Vaccine 2023, 41, 6194–6205. [Google Scholar] [CrossRef]
- Arbyn, M.; Xu, L.; Simoens, C.; Martin-Hirsch, P.P. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst. Rev. 2018, 5, Cd009069. [Google Scholar] [CrossRef]
- Sladič, M.; Taneska, P.; Cvjetičanin, B.; Velikonja, M.; Smrkolj, V.; Smrkolj, Š. Cervical Intraepithelial Neoplasia Grade 3 in a HPV-Vaccinated Patient: A Case Report. Medicina 2022, 58, 339. [Google Scholar] [CrossRef]
- McLucas, B.; Vail, E.; Chua, K.J.; Walt, G. Cervical intraepithelial neoplasia grade 3 in a patient following Gardasil vaccination. BMJ Case Rep. 2019, 12, e230366. [Google Scholar] [CrossRef] [PubMed]
- Makris, G.M.; Karakitsos, P.; Kotsifa, E.; Margari, N.; Poulakaki, N.; Sergentanis, T.N.; Battista, M.J.; Chrelias, C.; Papantoniou, N. Endocervical Carcinogenesis and HPV Vaccination: An Occasional Circumstance or a Gap in the Chain? Case Rep. Obstet. Gynecol. 2017, 2017, 4976741. [Google Scholar] [CrossRef] [PubMed]
- Shing, J.Z.; Hu, S.; Herrero, R.; Hildesheim, A.; Porras, C.; Sampson, J.N.; Schussler, J.; Schiller, J.T.; Lowy, D.R.; Sierra, M.S.; et al. Precancerous cervical lesions caused by non-vaccine-preventable HPV types after vaccination with the bivalent AS04-adjuvanted HPV vaccine: An analysis of the long-term follow-up study from the randomised Costa Rica HPV Vaccine Trial. Lancet Oncol. 2022, 23, 940–949. [Google Scholar] [CrossRef] [PubMed]
- Tabibi, T.; Barnes, J.M.; Shah, A.; Osazuwa-Peters, N.; Johnson, K.J.; Brown, D.S. Human Papillomavirus Vaccination and Trends in Cervical Cancer Incidence and Mortality in the US. JAMA Pediatr. 2022, 176, 313–316. [Google Scholar] [CrossRef]
- Gupta, C.; Dolma, K.G.; Sherpa, M.L.; Bag, A.; Byahut, A. Human papillomavirus vaccine: Success and challenges. J. Biosci. 2025, 50, 51. [Google Scholar] [CrossRef]
- Malone, C.; Barnabas, R.V.; Buist, D.S.M.; Tiro, J.A.; Winer, R.L. Cost-effectiveness studies of HPV self-sampling: A systematic review. Prev. Med. 2020, 132, 105953. [Google Scholar] [CrossRef]
- Sachan, P.L.; Singh, M.; Patel, M.L.; Sachan, R. A Study on Cervical Cancer Screening Using Pap Smear Test and Clinical Correlation. Asia Pac. J. Oncol. Nurs. 2018, 5, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Lucksom, P.G.; Sherpa, M.L.; Pradhan, A.; Lal, S.; Gupta, C. Advances in HPV Screening Tests for Cervical Cancer-A Review. J. Obstet. Gynaecol. India 2022, 72, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Tambvekar, S.E.; Balsarkar, G. Modernizing Cervical Cytology Screening with Liquid-Based Methods at Community-Level Hospitals: A Much-Needed Breakthrough for India. J. Obstet. Gynecol. India 2024, 74, 371–377. [Google Scholar] [CrossRef]
- NHS Rolls Out More Personalised Cervical Screening for Millions. Available online: https://www.england.nhs.uk/2025/06/nhs-rolls-out-more-personalised-cervical-screening-for-millions/ (accessed on 4 July 2025).
- U.S. Preventive Services Task Force Issues Draft Recommendation Statement on Screening for Cervical Cancer. Available online: https://www.uspreventiveservicestaskforce.org/uspstf/sites/default/files/file/supporting_documents/cervical-cancer-screening-draft-rec-bulletin_0.pdf (accessed on 4 July 2025).
- Bouvard, V.; Wentzensen, N.; Mackie, A.; Berkhof, J.; Brotherton, J.; Giorgi-Rossi, P.; Kupets, R.; Smith, R.; Arrossi, S.; Bendahhou, K.; et al. The IARC Perspective on Cervical Cancer Screening. N. Engl. J. Med. 2021, 385, 1908–1918. [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, Y.; Dai, Y.; Dang, L.; Ma, L.; Yang, C.; Li, Y.; Kong, L.; Wei, L.; Zhang, S.; et al. Effectiveness of High-risk Human Papillomavirus Testing for Cervical Cancer Screening in China: A Multicenter, Open-label, Randomized Clinical Trial. JAMA Oncol. 2021, 7, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Denny, L.; Kuhn, L.; Hu, C.-C.; Tsai, W.-Y.; Wright, T.C. Human Papillomavirus–Based Cervical Cancer Prevention: Long-term Results of a Randomized Screening Trial. JNCI J. Natl. Cancer Inst. 2010, 102, 1557–1567. [Google Scholar] [CrossRef]
- Ogilvie, G.S.; van Niekerk, D.; Krajden, M.; Smith, L.W.; Cook, D.; Gondara, L.; Ceballos, K.; Quinlan, D.; Lee, M.; Martin, R.E.; et al. Effect of Screening with Primary Cervical HPV Testing vs Cytology Testing on High-grade Cervical Intraepithelial Neoplasia at 48 Months: The HPV FOCAL Randomized Clinical Trial. Jama 2018, 320, 43–52. [Google Scholar] [CrossRef]
- Moy, L.M.; Zhao, F.-H.; Li, L.-Y.; Ma, J.-F.; Zhang, Q.-M.; Chen, F.; Song, Y.; Hu, S.-Y.; Balasubramanian, A.; Pan, Q.-J.; et al. Human papillomavirus testing and cervical cytology in primary screening for cervical cancer among women in rural China: Comparison of sensitivity, specificity, and frequency of referral. Int. J. Cancer 2010, 127, 646–656. [Google Scholar] [CrossRef] [PubMed]
- Kaya Terzi, N.; Yulek, O. Assessment of Cervicovaginal Smear and HPV DNA Co-Test for Cervical Cancer Screening: Implications for Diagnosis and Follow-Up Strategies. Diagnostics 2024, 14, 611. [Google Scholar] [CrossRef] [PubMed]
- Comparing Clinician-Collected and Self-Collected Tests for Detecting High-Risk HPV Infection among Female-to-Male Transgender Adults. Available online: https://www.ncbi.nlm.nih.gov/books/NBK595846/ (accessed on 4 July 2025).
- Ogilvie, G.S.; Patrick, D.M.; Schulzer, M.; Sellors, J.W.; Petric, M.; Chambers, K.; White, R.; FitzGerald, J.M. Diagnostic accuracy of self collected vaginal specimens for human papillomavirus compared to clinician collected human papillomavirus specimens: A meta-analysis. Sex. Transm. Infect. 2005, 81, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Mathews, C.S.; Sargent, A.; Cuschieri, K.; Rebolj, M.; Brentnall, A.R.; Mackie, A.; Mills, C.; Martinelli, C.; Wright, A.-M.; Hunt, K.; et al. HPValidate—Human papillomavirus testing with DNA and mRNA assays on self-collected samples in cervical screening: Comparison of test characteristics on three self-sampling devices. Br. J. Cancer 2025. [Google Scholar] [CrossRef] [PubMed]
- FDA Roundup. Available online: https://www.fda.gov/news-events/press-announcements/fda-roundup-may-17-2024 (accessed on 4 July 2025).
- Shastri, S.S.; McNeill, L.H.; Shete, S. Culturally Competent Education and Human Papillomavirus Self-Sampling Achieves Healthy People 2030 Cervical Screening Target Among Low-Income Non-Hispanic Black and Hispanic Women. JCO Glob. Oncol. 2024, e2400005. [Google Scholar] [CrossRef]
- Fullerton, M.M.; Ford, C.; D’Silva, C.; Chiang, B.; Onobrakpor, S.-I.; Dievert, H.; Yang, H.; Cabaj, J.; Ivers, N.; Davidson, S.; et al. HPV self-sampling implementation strategies to engage under screened communities in cervical cancer screening: A scoping review to inform screening programs. Front. Public Health 2024, 12, 1430968. [Google Scholar] [CrossRef] [PubMed]
- Hariprasad, R.; Srinivasan, M.; Ravi, P.; Tamang, H.; Sharma, A.; Pradhan, S.; Dhanasekaran, K. A qualitative study on ASHA workers’ perspective on HPV self-sampling in Sikkim India. Sci. Rep. 2025, 15, 15985. [Google Scholar] [CrossRef]
- Choi, H.; Dion, H.; Huang, M.; Sathyan, L.; Herfel, E.; Makhulo, B.; Ambaka, J.; Huchko, M.J. Applying the Information-Motivation-Behavioral Skills model to a video-assisted HPV intervention to promote self-screening uptake: A qualitative study in Western Kenya. BMJ Glob. Health 2025, 10, e017616. [Google Scholar] [CrossRef]
- Xiong, S.; Ghebre, R.; Kulasingam, S.; Mason, S.M.; Pratt, R.J.; Lazovich, D. Exploring factors associated with preferences for human papillomavirus (HPV) self-sampling among racially- and ethnically-diverse women in Minnesota: A cross-sectional study. Prev. Med. Rep. 2023, 34, 102243. [Google Scholar] [CrossRef]
- Global Cervical Cancer Elimination Forum. Available online: https://www.who.int/initiatives/cervical-cancer-elimination-initiative/cervical-cancer-forum/global-opportunity-and-challenge (accessed on 4 July 2025).
- Cervical Cancer Elimination Initiative. Available online: https://www.who.int/initiatives/cervical-cancer-elimination-initiative (accessed on 4 July 2025).
- Chidebe, R.C.W.; Osayi, A.; Torode, J.S. The Global Fund, Cervical Cancer, and HPV infections: What can low- and middle-income countries do to accelerate progress by 2030? EClinicalmedicine 2025, 81, 103127. [Google Scholar] [CrossRef]
- Ginsburg, O. Global disparities in HPV vaccination. Lancet Glob. Health 2016, 4, e428–e429. [Google Scholar] [CrossRef] [PubMed]
- Dorji, T.; Nopsopon, T.; Tamang, S.T.; Pongpirul, K. Human papillomavirus vaccination uptake in low-and middle-income countries: A meta-analysis. EClinicalMedicine 2021, 34, 100836. [Google Scholar] [CrossRef]
- Serrano, B.; Ibáñez, R.; Robles, C.; Peremiquel-Trillas, P.; de Sanjosé, S.; Bruni, L. Worldwide use of HPV self-sampling for cervical cancer screening. Prev. Med. 2022, 154, 106900. [Google Scholar] [CrossRef]
- Ken-Amoah, S.; Blay Mensah, L.B.; Eliason, S.; Anane-Fenin, B.; Agbeno, E.K.; Essuman, M.A.; Essien-Baidoo, S. Poor knowledge and awareness of human papillomavirus and cervical cancer among adult females in rural Ghana. Front. Trop. Dis. 2022, 3, 971266. [Google Scholar] [CrossRef]
- Ebu, N.I.; Abotsi-Foli, G.E.; Gakpo, D.F. Nurses’ and midwives’ knowledge, attitudes, and acceptance regarding human papillomavirus vaccination in Ghana: A cross-sectional study. BMC Nurs. 2021, 20, 11. [Google Scholar] [CrossRef] [PubMed]
- Dedey, F.; Nsaful, J.; Nartey, E.; Labi, J.; Adu-Aryee, N.A.; Kuti, C.; Clegg-Lamptey, J.-N. Assessing the impact of cervical cancer education in two high schools in Ghana. BMC Cancer 2024, 24, 1359. [Google Scholar] [CrossRef]
- Nartey, Y.; Amo-Antwi, K.; Osei-Ntiamoah, B.; Hill, P.C.; Dassah, E.T.; Asmah, R.H.; Nyarko, K.M.; Agambire, R.; Konney, T.O.; Yarney, J.; et al. Knowledge of Human Papillomavirus, Risk Factors and Screening for Cervical Cancer Among Women in Ghana. Cancer Control 2025, 32, 10732748251323765. [Google Scholar] [CrossRef]
- Nyaaba, J.A.; Akurugu, E. Knowledge, barriers and uptake towards Cervical Cancer screening among female health workers in Ghana: A perspective of the Health Belief Model. Int. J. Afr. Nurs. Sci. 2023, 19, 100587. [Google Scholar] [CrossRef]
- Appiah, R.S.; Boakye, K.; Appiah, G.; Aidoo, A.A.; Acquah-Hagan, G.; Singh, B.; Appiah, F.; Boateng, D. Rural-urban variations in cervical cancer screening uptake among women in Ghana: Evidence from the 2022 Ghana Demographic and Health Survey. BMC Women’s Health 2025, 25, 255. [Google Scholar] [CrossRef] [PubMed]
- Adebamowo, C.; Rossi, P.G.; Castle, P.E. Challenges and Opportunities for Global Cervical Cancer Elimination: How Can We Build a Model for Other Cancers? Am. Soc. Clin. Oncol. Educ. Book 2025, 45, e473702. [Google Scholar] [CrossRef]
- Avila-Aguero, M.L.; Ospina-Henao, S.; Brenes-Chacon, H.; Espinal-Tejada, C.; Trejo-Varon, R.; Morice, A. Human Papilloma Virus Vaccination as a Strategy to Eliminate Cervical Cancer: Challenges and Opportunities. Vaccines 2025, 13, 297. [Google Scholar] [CrossRef]
- Wu, Z.H.; An, Y.J.; Chu, Z.X.; Li, X.R.; Hou, A.Y.; Jiang, Y.J.; Hu, Q.H. Cost-effectiveness of self-sampling and enhanced strategies for HPV prevention among men who have sex with men in China: A modeling study. BMC Med. 2025, 23, 362. [Google Scholar] [CrossRef]
- Global Leaders Unite to Accelerate Cervical Cancer Elimination Efforts. Available online: https://www.who.int/westernpacific/news/item/19-06-2025-global-leaders-unite-to-accelerate-cervical-cancer-elimination-efforts (accessed on 4 July 2025).
- Stanley, M.; Schuind, A.; Muralidharan, K.K.; Guillaume, D.; Willens, V.; Borda, H.; Jurgensmeyer, M.; Limaye, R. Evidence for an HPV one-dose schedule. Vaccine 2024, 42, S16–S21. [Google Scholar] [CrossRef]
- Bula, A.K.; Mhango, P.; Tsidya, M.; Chimwaza, W.; Kaira, P.; Ghambi, K.; Heitner, J.; Lee, F.; McGue, S.; Chinula, L.; et al. Client perspectives and satisfaction with integrating facility and community-based HPV self-sampling for cervical cancer screening with family planning: A mixed method study. BMC Public Health 2025, 25, 1718. [Google Scholar] [CrossRef] [PubMed]
- Arrossi, S.; Thouyaret, L.; Herrero, R.; Campanera, A.; Magdaleno, A.; Cuberli, M.; Barletta, P.; Laudi, R.; Orellana, L. Effect of self-collection of HPV DNA offered by community health workers at home visits on uptake of screening for cervical cancer (the EMA study): A population-based cluster-randomised trial. Lancet Glob. Health 2015, 3, e85–e94. [Google Scholar] [CrossRef] [PubMed]
- Tourneau, C.L.; Rolland, F.; Capitain, O.; Cassier, P.A.; Fumet, J.D.; Salas, S.; Daste, A.; Manso, L.; Bermejo-Perez, M.-J.; Casado, A.; et al. Randomized phase II trial evaluating the combination of TG4001, an HPV16 therapeutic vaccine, and avelumab (ave) in patients (pts) with immunotherapy-naïve recurrent and/or metastatic (R/M) HPV16-positive cervical or anogenital cancer. J. Clin. Oncol. 2025, 43, 2638. [Google Scholar] [CrossRef]
- Zhao, X.; Zhang, Y.; Trejo-Cerro, O.; Kaplan, E.; Li, Z.; Albertsboer, F.; El Hammiri, N.; Mariz, F.C.; Banks, L.; Ottonello, S.; et al. A safe and potentiated multi-type HPV L2-E7 nanoparticle vaccine with combined prophylactic and therapeutic activity. npj Vaccines 2024, 9, 119. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, Q.; Ma, L.; Lv, K.; Han, L.; Chen, Y.; Zhou, R.; Zhou, H.; Chen, H.; Wang, Y.; et al. Development of an mRNA-based therapeutic vaccine mHTV-03E2 for high-risk HPV-related malignancies. Mol. Ther. 2024, 32, 2340–2356. [Google Scholar] [CrossRef] [PubMed]
- Eerkens, A.L.; Esajas, M.D.; Brummel, K.; Vledder, A.; van Rooij, N.; Plat, A.; Avalos Haro, S.B.; Paijens, S.T.; Slagter-Menkema, L.; Schuuring, E.; et al. Vvax001, a Therapeutic Vaccine, for Patients with HPV16-Positive High-grade Cervical Intraepithelial Neoplasia: A Phase II Trial. Clin Cancer Res 2025, 31, 1016–1026. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Cao, C.; Wu, P.; Huang, X.; Ma, D. Advances in cervical cancer: Current insights and future directions. Cancer Commun. 2025, 45, 77–109. [Google Scholar] [CrossRef]
- Stegmüller, T.; Abbet, C.; Bozorgtabar, B.; Clarke, H.; Petignat, P.; Vassilakos, P.; Thiran, J.P. Self-supervised learning-based cervical cytology for the triage of HPV-positive women in resource-limited settings and low-data regime. Comput. Biol. Med. 2024, 169, 107809. [Google Scholar] [CrossRef]
- Burmeister, C.A.; Khan, S.F.; Schäfer, G.; Mbatani, N.; Adams, T.; Moodley, J.; Prince, S. Cervical cancer therapies: Current challenges and future perspectives. Tumour Virus Res. 2022, 13, 200238. [Google Scholar] [CrossRef]
- Wang, R.; Huang, H.; Yu, C.; Li, X.; Wang, Y.; Xie, L. Current status and future directions for the development of human papillomavirus vaccines. Front. Immunol. 2024, 15, 1362770. [Google Scholar] [CrossRef]
- Fitzpatrick, M.B.; Behrens, C.M.; Hibler, K.; Parsons, C.; Kaplan, C.; Orso, R.; Parker, L.; Memmel, L.; Collins, A.; McNicholas, C.; et al. Clinical Validation of a Vaginal Cervical Cancer Screening Self-Collection Method for At-Home Use: A Nonrandomized Clinical Trial. JAMA Netw. Open 2025, 8, e2511081. [Google Scholar] [CrossRef]
- Han, L.; Zhang, B. Can prophylactic HPV vaccination reduce the recurrence of cervical lesions after surgery? Review and prospect. Infect. Agents Cancer 2023, 18, 66. [Google Scholar] [CrossRef] [PubMed]
- Pruski, D.; Millert-Kalińska, S.; Jach, R.; Przybylski, M. Effect of vaccination against HPV in the HPV-positive patients not covered by primary prevention on the disappearance of infection. Sci. Rep. 2025, 15, 12642. [Google Scholar] [CrossRef] [PubMed]
- Petráš, M.; Lomozová, D.; Dvořák, V.; Dvořák, V., Jr.; Malinová, J.; Trnková, M.; Fišer, I.; Dlouhý, P.; Rosina, J.; Lesná, I.K. Early and long-term effects of prophylactic and post-excision human papillomavirus vaccination on recurrent high-grade cervical intraepithelial neoplasia relative to margin status: A retrospective cohort study in the Czech Republic. Lancet Reg. Health–Eur. 2025, 55, 101337. [Google Scholar] [CrossRef] [PubMed]
- Alarid-Escudero, F.; Gracia, V.; Wolf, M.; Zhao, R.; Easterly, C.W.; Kim, J.J.; Canfell, K.; de Kok, I.M.C.M.; Barnabas, R.V.; Kulasingam, S. State-level disparities in cervical cancer prevention and outcomes in the United States: A modeling study. JNCI J. Natl. Cancer Inst. 2024, 117, 737–746. [Google Scholar] [CrossRef] [PubMed]
| Domain | Component | Details/Significance |
|---|---|---|
| Etiology | High-Risk HPV Types | HPV16 and HPV18 account for ~70% of cervical cancer cases worldwide |
| Transmission | Primarily through sexual contact; peak incidence shortly after sexual debut | |
| Molecular Mechanism | E6 Oncoprotein | Binds E6AP to degrade p53, impairing apoptosis and DNA repair |
| E7 Oncoprotein | Inactivates pRb, driving cell cycle progression and genomic instability | |
| Natural History | Infection Progression | Mostly clears spontaneously; persistent infection may lead to CIN and invasive cancer |
| Co-Factors | Immunosuppression (e.g., HIV), smoking, early sexual activity, parity, OC use | |
| Prevention | Prophylactic Vaccines | Bivalent, quadrivalent, and nonavalent |
| WHO Vaccine Target | 90% of girls fully vaccinated by age 15 by 2030 | |
| Screening | Primary Testing Methods | Pap smear, HPV DNA test, co-testing, VIA |
| Emerging Tools | Self-sampling, methylation biomarkers, AI-enhanced cytology | |
| Global Disparities | LMIC Burden | 90% of cervical cancer deaths occur in LMICs |
| Access Gaps | Unequal access to vaccines, trained personnel, and diagnostic infrastructure | |
| Future Directions | Therapeutic Vaccines | Target E6/E7 in persistent HPV or CIN2/3; promising in early trials |
| Elimination Goals | WHO: <4 cases per 100,000 women/year (global elimination threshold) |
| Category | HPV Types |
|---|---|
| Group 1 carcinogens | 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 |
| (carcinogenic to humans) | |
| Considered high-risk | |
| Group 2A carcinogens | 68 |
| (probably carcinogenic to humans) | |
| Group 2B carcinogens | 26, 30, 34, 53, 66, 67, 69, 70, 73, 82, 85, 97 |
| (possibly carcinogenic to humans) | |
| Group 3 | 6, 11 |
| (low-risk) |
| Viral Protein | Cellular Target(s) | Biological Effect | Resulting Phenotype |
|---|---|---|---|
| E5 | EGFR, MHC-I | Enhances growth factor signaling, downregulates antigen presentation | Immune evasion, cell proliferation |
| E6 | p53 | Promotes ubiquitin-mediated degradation of p53 | Inhibits apoptosis, impairs DNA repair |
| E7 | pRb | Disrupts the pRb-E2F complex | Uncontrolled cell cycle progression |
| Product (Maker) | HPV Types (Valency) | Label Dosing (Regulatory) |
|---|---|---|
| Gardasil 9 (MSD/Merck) | 6, 11, 16, 18, 31, 33, 45, 52, 58 (9-valent) | Two doses (9–14 y) or three doses (≥15 y/immunocompromised) per label |
| Gardasil/Silgard (MSD)—quadrivalent | 6, 11, 16, 18 (4-valent) | Two doses (9–13 y) or three doses (≥14 y/immunocompromised) per label |
| Cervarix (GSK)—bivalent | 16, 18 (2-valent) | Two doses (9–14 y) or three doses (≥15 y/immunocompromised) per label |
| Cecolin (Innovax, China)—bivalent | 16, 18 (2-valent) | Two doses (9–14 y) or three doses (≥15 y/immunocompromised) per label |
| Walrinva (Zerun/Walvax, China)—bivalent | 16, 18 (2-valent) | Standard 2/3 doses by age |
| CERVAVAC (Serum Institute of India)—quadrivalent | 6, 11, 16, 18 (4-valent) | Indian authorization of 2/3 doses by age |
| Country/Setting | Vaccine/Program (Cohorts) | Outcome Measured | Key Real-World Impact | Study Period |
|---|---|---|---|---|
| England (national) [148] | bHPV vaccine then qHPV vaccine/9vHPV vaccine; routine at 12–13 y | Cervical cancer; CIN3 | Marked reductions across all deprivation groups; strongest when vaccinated at routine age | From 2006 up to 2020 follow-up |
| England (surveillance) [149] | Initially bHPV vaccine (Cervarix) at 12–13 y; changed to qHPV vaccine Gardasil in 2012 (HPV 16/18/6/11) | HPV16/18 infection prevalence | Around a 90% reduction in HPV16/18 in young women offered vaccination | 2010–2020 |
| Scotland (national) [150] | bHPV vaccine; high school program | CIN2 and CIN3 | Reduction in pre-invasive cervical disease in vaccinated cohorts | Women aged between 20 and 60 years by 2016 |
| Sweden (national cohort) [151] | qHPV vaccine | Invasive cervical cancer | Vaccination associated with substantially lower cervical cancer risk; strongest when vaccinated <17 y | 2006–2017 |
| Australia (national, school-based) [152] | qHPV vaccine | HPV-related disease, including high-grade abnormalities | Large population-level reductions in HPV-related outcomes; early decline in cervical abnormalities within 5 years | 2007–2016 |
| United States (HPV-IMPACT, CDC) [153] | Mixed vaccines: bHPV vaccine, qHPV vaccine and 9vHPV vaccine | CIN2 and CIN3 (screen-detected) | Among women 20–24 y, CIN2+ ↓79% and CIN3+ ↓80% from 2008 to 2022; has also declined in 25–29 y | 2008–2022 |
| Denmark (population data) [154] | National program | HPV-16/18 infection prevalence | HPV16/18 prevalence in vaccinated women fell from 15–17% pre-vaccine to <1% by 2021 | 2017–2024 |
| Norway (regional, real-world) [155] | National program | CIN2+/CIN3+ | CIN2+ incidence decreased markedly after initial rise; no cervical cancers recorded in vaccinated cohorts in this series | 2008–2022 |
| Multi-country meta-analysis [156] | Programs with high coverage | HPV infections; genital warts; CIN2+ | Countries with multi-cohort, high-coverage programs show larger direct impact and herd effects; significant reductions in HPV infection and CIN2+ | 2014–2018 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boldeanu, L.; Assani, M.-Z.; Boldeanu, M.V.; Siloși, I.; Manolea, M.-M.; Văduva, C.-C.; Assani, A.-D.; Dijmărescu, A.L. Cervical Cancer in the Era of HPV: Translating Molecular Mechanisms into Preventive Public Health Action. Int. J. Mol. Sci. 2025, 26, 8463. https://doi.org/10.3390/ijms26178463
Boldeanu L, Assani M-Z, Boldeanu MV, Siloși I, Manolea M-M, Văduva C-C, Assani A-D, Dijmărescu AL. Cervical Cancer in the Era of HPV: Translating Molecular Mechanisms into Preventive Public Health Action. International Journal of Molecular Sciences. 2025; 26(17):8463. https://doi.org/10.3390/ijms26178463
Chicago/Turabian StyleBoldeanu, Lidia, Mohamed-Zakaria Assani, Mihail Virgil Boldeanu, Isabela Siloși, Maria-Magdalena Manolea, Constantin-Cristian Văduva, Alexandru-Dan Assani, and Anda Lorena Dijmărescu. 2025. "Cervical Cancer in the Era of HPV: Translating Molecular Mechanisms into Preventive Public Health Action" International Journal of Molecular Sciences 26, no. 17: 8463. https://doi.org/10.3390/ijms26178463
APA StyleBoldeanu, L., Assani, M.-Z., Boldeanu, M. V., Siloși, I., Manolea, M.-M., Văduva, C.-C., Assani, A.-D., & Dijmărescu, A. L. (2025). Cervical Cancer in the Era of HPV: Translating Molecular Mechanisms into Preventive Public Health Action. International Journal of Molecular Sciences, 26(17), 8463. https://doi.org/10.3390/ijms26178463








