Multiplexed Quantification of First-Trimester Serum Biomarkers in Healthy Pregnancy
Abstract
1. Introduction
2. Results
2.1. Clinical and Demographic Characteristics
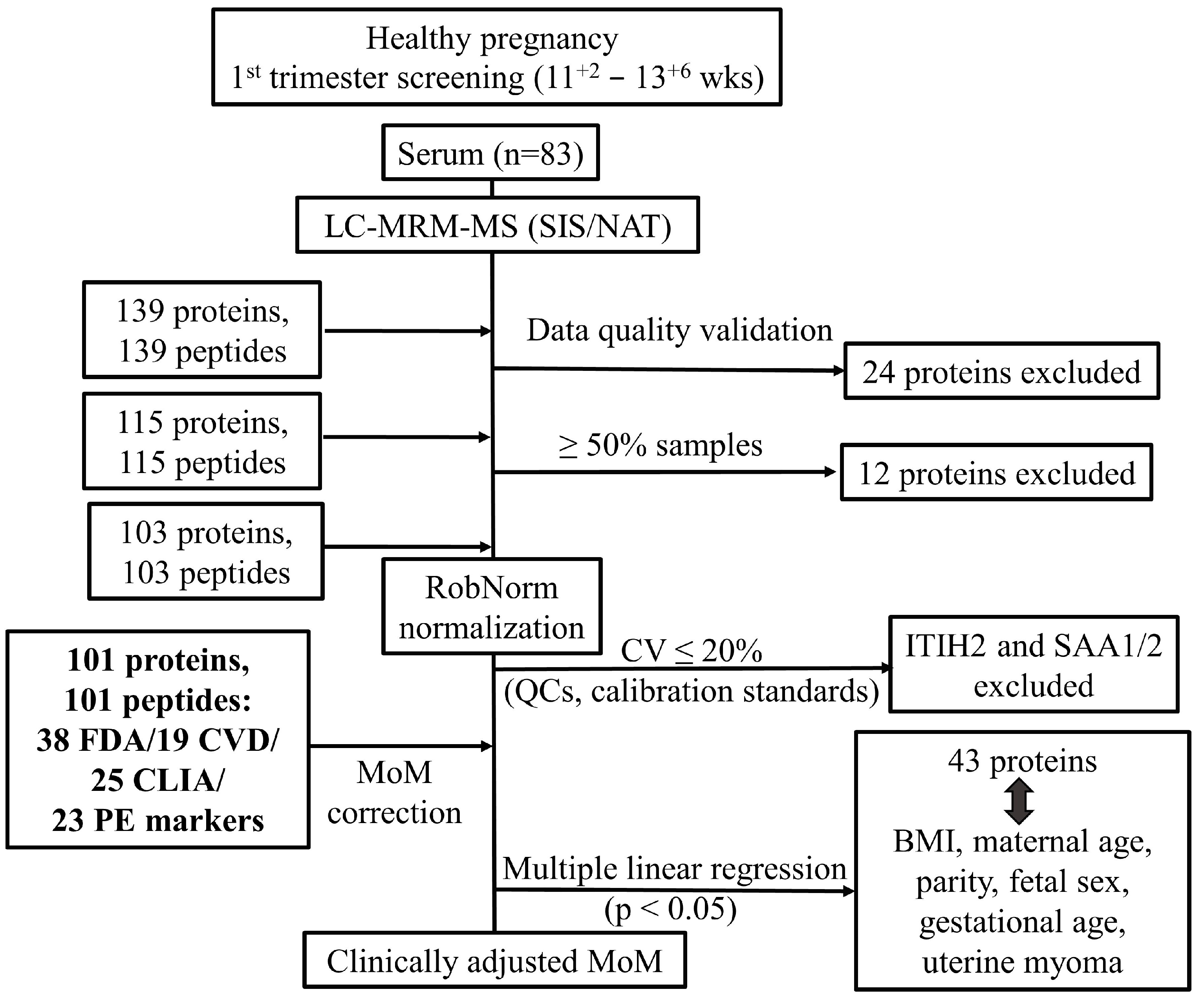
2.2. Analytical Performance and Data Normalization
2.3. First Trimester Serum Proteome Profiling
2.4. Associations Between Serum Proteome and Clinical Parameters
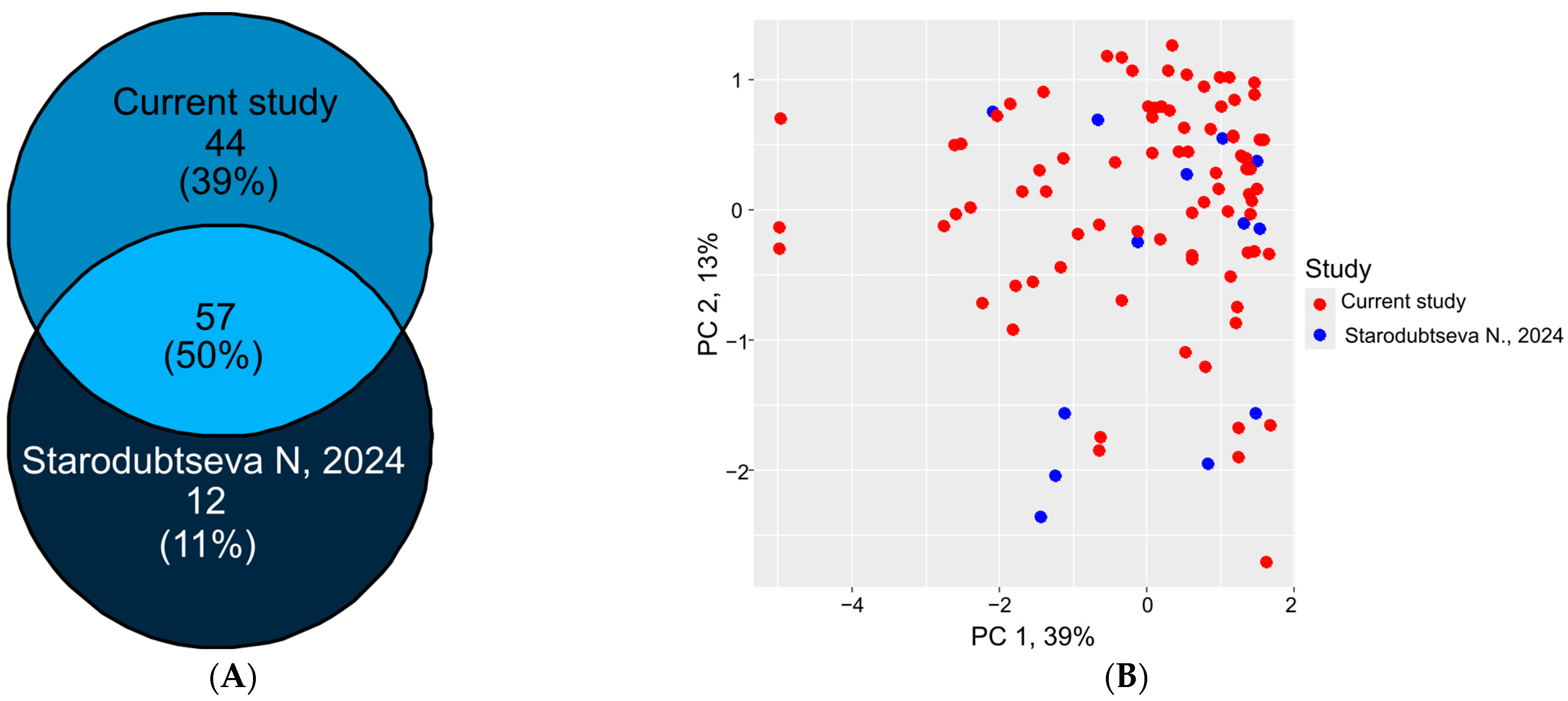
2.5. Proteomic Data Comparison and Validation
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Sample Preparation
4.3. LC-MRM-MS Analysis
4.4. Data Preprocessing, Quality Control, and Quantitative Analysis
4.5. Statistical Analysis and Normalization
4.6. Reference Value Establishment and Clinical Parameter Association
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| PE | Preeclampsia |
| IUGR | Intrauterine growth restriction |
| SIS | Stable isotope-labeled standards |
| NAT | Natural synthetic proteotypic peptides |
| CV | Coefficient of variation |
| DIA | Data-independent acquisition |
| ELISA | Enzyme-linked immunosorbent assay |
| PEA | Proximity extension assay |
| HLOQ | The highest limit of quantification |
| UHPLC | Ultra-high-performance liquid chromatography |
| LC-MS | Liquid chromatography–mass-spectrometry |
| LLOQ | The lowest limit of quantification |
| LOESS | Locally estimated scatterplot smoothing |
| MoM | Multiply of medians |
| MRM | Multiply reaction monitoring |
| MS | Mass spectrometry |
| QC | Quality control |
| SPE | Solid-phase extraction |
| MAP | Mean arterial pressure |
| UtA-PI | Pulsatility index of the left and right uterine arteries |
References
- Beimers, W.F.; Overmyer, K.A.; Sinitcyn, P.; Lancaster, N.M.; Quarmby, S.T.; Coon, J.J. Technical Evaluation of Plasma Proteomics Technologies. J. Proteome Res. 2025, 24, 3074–3087. [Google Scholar] [CrossRef] [PubMed]
- Sun, B.B.; Suhre, K.; Gibson, B.W. Promises and Challenges of populational Proteomics in Health and Disease. Mol. Cell. Proteomics 2024, 23, 100786. [Google Scholar] [CrossRef] [PubMed]
- Čuklina, J.; Lee, C.H.; Williams, E.G.; Sajic, T.; Collins, B.C.; Rodríguez Martínez, M.; Sharma, V.S.; Wendt, F.; Goetze, S.; Keele, G.R.; et al. Diagnostics and correction of batch effects in large-scale proteomic studies: A tutorial. Mol. Syst. Biol. 2021, 17, e10240. [Google Scholar] [CrossRef]
- Badrick, T. Biological variation: Understanding why it is so important? Pract. Lab. Med. 2021, 23, e00199. [Google Scholar] [CrossRef]
- Xu, R.; Gong, C.X.; Duan, C.M.; Huang, J.C.; Yang, G.Q.; Yuan, J.J.; Zhang, Q.; Xiong, X.; Yang, Q. Age-Dependent Changes in the Plasma Proteome of Healthy Adults. J. Nutr. Health Aging 2020, 24, 846–856. [Google Scholar] [CrossRef] [PubMed]
- Murtoniemi, K.; Kalapotharakos, G.; Vahlberg, T.; Räikkonen, K.; Kajantie, E.; Hämäläinen, E.; Åkerström, B.; Villa, P.M.; Hansson, S.R.; Laivuori, H. Longitudinal changes in plasma hemopexin and alpha-1-microglobulin concentrations in women with and without clinical risk factors for preeclampsia. PLoS ONE 2019, 14, e0226520. [Google Scholar] [CrossRef] [PubMed]
- García-Bailo, B.; Brenner, D.R.; Nielsen, D.; Lee, H.J.; Domanski, D.; Kuzyk, M.; Borchers, C.H.; Badawi, A.; Karmali, M.A.; El-Sohemy, A. Dietary patterns and ethnicity are associated with distinct plasma proteomic groups. Am. J. Clin. Nutr. 2012, 95, 352–361. [Google Scholar] [CrossRef]
- Kononikhin, A.S.; Starodubtseva, N.L.; Brzhozovskiy, A.G.; Tokareva, A.O.; Kashirina, D.N.; Zakharova, N.V.; Bugrova, A.E.; Indeykina, M.I.; Pastushkova, L.K.; Larina, I.M.; et al. Absolute Quantitative Targeted Monitoring of Potential Plasma Protein Biomarkers: A Pilot Study on Healthy Individuals. Biomedicines 2024, 12, 2403. [Google Scholar] [CrossRef]
- Papapavlou Lingehed, G.; Hellberg, S.; Huang, J.; Khademi, M.; Kockum, I.; Carlsson, H.; Tjernberg, I.; Svenvik, M.; Lind, J.; Blomberg, M.; et al. Plasma protein profiling reveals dynamic immunomodulatory changes in multiple sclerosis patients during pregnancy. Front. Immunol. 2022, 13, 930947. [Google Scholar] [CrossRef]
- Pernemalm, M.; Sandberg, A.; Zhu, Y.; Boekel, J.; Tamburro, D.; Schwenk, J.M.; Björk, A.; Wahren-Herlenius, M.; Åmark, H.; Östenson, C.G.; et al. In-depth human plasma proteome analysis captures tissue proteins and transfer of protein variants across the placenta. eLife 2019, 8, e41608. [Google Scholar] [CrossRef]
- Wishart, D.S.; Bartok, B.; Oler, E.; Liang, K.Y.H.; Budinski, Z.; Berjanskii, M.; Guo, A.; Cao, X.; Wilson, M. MarkerDB: An online database of molecular biomarkers. Nucleic Acids Res. 2021, 49, D1259–D1267. [Google Scholar] [CrossRef]
- Anderson, N.L. The clinical plasma proteome: A survey of clinical assays for proteins in plasma and serum. Clin. Chem. 2010, 56, 177–185. [Google Scholar] [CrossRef]
- Ngo, D.; Sinha, S.; Shen, D.; Kuhn, E.W.; Keyes, M.J.; Shi, X.; Benson, M.D.; O’Sullivan, J.F.; Keshishian, H.; Farrell, L.A.; et al. Aptamer-Based Proteomic Profiling Reveals Novel Candidate Biomarkers and Pathways in Cardiovascular Disease. Circulation 2016, 134, 270–285. [Google Scholar] [CrossRef]
- Jones, J.J.; Wilcox, B.E.; Benz, R.W.; Babbar, N.; Boragine, G.; Burrell, T.; Christie, E.B.; Croner, L.J.; Cun, P.; Dillon, R.; et al. A plasma-based protein marker panel for colorectal cancer detection identified by multiplex targeted mass spectrometry. Clin. Color. Cancer 2016, 15, 186–194.e13. [Google Scholar] [CrossRef]
- Landegren, U.; Hammond, M. Cancer diagnostics based on plasma protein biomarkers: Hard times but great expectations. Mol. Oncol. 2021, 15, 1715–1726. [Google Scholar] [CrossRef]
- Tans, R.; Verschuren, L.; Wessels, H.J.C.T.; Bakker, S.J.L.; Tack, C.J.; Gloerich, J.; van Gool, A.J. The future of protein biomarker research in type 2 diabetes mellitus. Expert Rev. Proteom. 2019, 16, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Zakharova, N.V.; Bugrova, A.E.; Indeykina, M.I.; Fedorova, Y.B.; Kolykhalov, I.V.; Gavrilova, S.I.; Nikolaev, E.N.; Kononikhin, A.S. Proteomic Markers and Early Prediction of Alzheimer’s Disease. Biochemistry 2022, 87, 762–776. [Google Scholar] [CrossRef] [PubMed]
- Starodubtseva, N.; Tokareva, A.; Kononikhin, A.; Brzhozovskiy, A.; Bugrova, A.; Kukaev, E.; Muminova, K.; Nakhabina, A.; Frankevich, V.E.; Nikolaev, E.; et al. First-Trimester Preeclampsia-Induced Disturbance in Maternal Blood Serum Proteome: A Pilot Study. Int. J. Mol. Sci. 2024, 25, 10653. [Google Scholar] [CrossRef] [PubMed]
- Starodubtseva, N.L.; Tokareva, A.O.; Volochaeva, M.V.; Kononikhin, A.S.; Brzhozovskiy, A.G.; Bugrova, A.E.; Timofeeva, A.V.; Kukaev, E.N.; Tyutyunnik, V.L.; Kan, N.E.; et al. Quantitative Proteomics of Maternal Blood Plasma in Isolated Intrauterine Growth Restriction. Int. J. Mol. Sci. 2023, 24, 16832. [Google Scholar] [CrossRef]
- Gaither, C.; Popp, R.; Mohammed, Y.; Borchers, C.H. Determination of the concentration range for 267 proteins from 21 lots of commercial human plasma using highly multiplexed multiple reaction monitoring mass spectrometry. Analyst 2020, 145, 3634–3644. [Google Scholar] [CrossRef]
- Kitteringham, N.R.; Jenkins, R.E.; Lane, C.S.; Elliott, V.L.; Park, B.K. Multiple reaction monitoring for quantitative biomarker analysis in proteomics and metabolomics. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2009, 877, 1229–1239. [Google Scholar] [CrossRef]
- Jiang, Y.; Rex, D.A.B.; Schuster, D.; Neely, B.A.; Rosano, G.L.; Volkmar, N.; Momenzadeh, A.; Peters-Clarke, T.M.; Egbert, S.B.; Kreimer, S.; et al. Comprehensive Overview of Bottom-Up Proteomics Using Mass Spectrometry. ACS Meas. Sci. Au 2024, 4, 338–417. [Google Scholar] [CrossRef]
- Wright, D.; Silva, M.; Papadopoulos, S.; Wright, A.; Nicolaides, K.H. Serum pregnancy-associated plasma protein-A in the three trimesters of pregnancy: Effects of maternal characteristics and medical history. Ultrasound Obstet. Gynecol. 2015, 46, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Álvez, M.B.; Edfors, F.; von Feilitzen, K.; Zwahlen, M.; Mardinoglu, A.; Edqvist, P.H.; Sjöblom, T.; Lundin, E.; Rameika, N.; Enblad, G.; et al. Next generation pan-cancer blood proteome profiling using proximity extension assay. Nat. Commun. 2023, 14, 4308. [Google Scholar] [CrossRef]
- Kotol, D.; Woessmann, J.; Hober, A.; Álvez, M.B.; Tran Minh, K.H.; Pontén, F.; Fagerberg, L.; Uhlén, M.; Edfors, F. Absolute Quantification of Pan-Cancer Plasma Proteomes Reveals Unique Signature in Multiple Myeloma. Cancers 2023, 15, 4764. [Google Scholar] [CrossRef]
- Hüttenhain, R.; Soste, M.; Selevsek, N.; Röst, H.; Sethi, A.; Carapito, C.; Farrah, T.; Deutsch, E.W.; Kusebauch, U.; Moritz, R.L.; et al. Reproducible quantification of cancer-associated proteins in body fluids using targeted proteomics. Sci. Transl. Med. 2012, 4, 142ra94. [Google Scholar] [CrossRef] [PubMed]
- Bader, J.M.; Albrecht, V.; Mann, M. MS-Based Proteomics of Body Fluids: The End of the Beginning. Mol. Cell. Proteomics 2023, 22, 100577. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.E.; Mann, M. Mass Spectrometry–Based Proteomics Turns Quantitative. Nat. Chem. Biol. 2005, 1, 252–262. [Google Scholar] [CrossRef]
- Addona, T.A.; Shi, X.; Keshishian, H.; Mani, D.R.; Burgess, M.; Gillette, M.A.; Clauser, K.R.; Shen, D.; Lewis, G.D.; Farrell, L.A.; et al. A pipeline that integrates the discovery and verification of plasma protein biomarkers reveals candidate markers for cardiovascular disease. Nat. Biotechnol. 2011, 29, 635–643. [Google Scholar] [CrossRef]
- Tsai, I.J.; Su, E.C.Y.; Tsai, I.L.; Lin, C.Y. Clinical assay for the early detection of colorectal cancer using mass spectrometric wheat germ agglutinin multiple reaction monitoring. Cancers 2021, 13, 2190. [Google Scholar] [CrossRef]
- Wortelboer, E.J.; Koster, M.P.H.; Kuc, S.; Eijkemans, M.J.C.; Bilardo, C.M.; Schielen, P.C.J.I.; Visser, G.H.A. Longitudinal trends in fetoplacental biochemical markers, uterine artery pulsatility index and maternal blood pressure during the first trimester of pregnancy. Ultrasound Obstet. Gynecol. 2011, 38, 383–388. [Google Scholar] [CrossRef]
- Tsiakkas, A.; Duvdevani, N.; Wright, A.; Wright, D.; Nicolaides, K.H. Serum placental growth factor in the three trimesters of pregnancy: Effects of maternal characteristics and medical history. Ultrasound Obstet. Gynecol. 2015, 45, 591–598. [Google Scholar] [CrossRef]
- Starodubtseva, N.; Poluektova, A.; Tokareva, A.; Kukaev, E.; Avdeeva, A.; Rimskaya, E.; Khodzayeva, Z. Proteome-Based Maternal Plasma and Serum Biomarkers for Preeclampsia: A Systematic Review and Meta-Analysis. Life 2025, 15, 776. [Google Scholar] [CrossRef]
- European Medicines Agency. ICH Guideline M10 on Bioanalytical Method Validation and Study Sample Analysis; ICH Harmonised Guideline: Geneva, Switzerland, 2022; Volume 44. [Google Scholar]
- Bhowmick, P.; Roome, S.; Borchers, C.H.; Goodlett, D.R.; Mohammed, Y. An Update on MRMAssayDB: A Comprehensive Resource for Targeted Proteomics Assays in the Community. J. Proteome Res. 2021, 20, 2105–2115. [Google Scholar] [CrossRef]
- Kuku, K.O.; Oyetoro, R.; Hashemian, M.; Livinski, A.A.; Shearer, J.J.; Joo, J.; Psaty, B.M.; Levy, D.; Ganz, P.; Roger, V.L. Proteomics for heart failure risk stratification: A systematic review. BMC Med. 2024, 22, 34. [Google Scholar] [CrossRef]
- Stakhneva, E.M.; Striukova, E.V.; Ragino, Y.I. Proteomic studies of blood and vascular wall in atherosclerosis. Int. J. Mol. Sci. 2021, 22, 13267. [Google Scholar] [CrossRef]
- Clinical Laboratory Improvement Amendments. Available online: https://www.fda.gov/medical-devices/medical-device-databases/clinical-laboratory-improvement-amendments-download-data (accessed on 16 August 2025).
- Yalçın, E.; Aslan, S.; Toğaçar, M.; Demir, S.C. A Hybrid Artificial Intelligence Approach for Down Syndrome Risk Prediction in First Trimester Screening. Diagnostics 2025, 15, 1444. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, S.; Momsen, G.; Sundberg, K.; Friis-Hansen, L.; Jørgensen, F.S. First-trimester risk calculation for trisomy 13, 18, and 21: Comparison of the screening efficiency between 2 locally developed programs and commercial software. Clin. Chem. 2011, 57, 1023–1031. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Cortes, M.; Arigita, M.; Falguera, G.; Seres, A.; Guix, D.; Baldrich, E.; Acera, A.; Torrent, A.; Rodriguez-Veret, A.; Lopez-Quesada, E.; et al. Contingent screening for Down syndrome completed in the first trimester: A multicenter study. Ultrasound Obstet. Gynecol. 2012, 39, 396–400. [Google Scholar] [CrossRef]
- Rifai, N. Tietz Fundamentals of Clinical Chemistry and Molecular Diagnostics, 8th ed.; Elsevier: Amsterdam, The Netherlands, 2018; ISBN 9780323549738. [Google Scholar]
- Wang, M.; Jiang, L.; Jian, R.; Chan, J.Y.; Liu, Q.; Snyder, M.P.; Tang, H. RobNorm: Model-based robust normalization method for labeled quantitative mass spectrometry proteomics data. Bioinformatics 2021, 37, 815–821. [Google Scholar] [CrossRef] [PubMed]
- Arend, L.; Adamowicz, K.; Schmidt, J.R.; Burankova, Y.; Zolotareva, O.; Tsoy, O.; Pauling, J.K.; Kalkhof, S.; Baumbach, J.; List, M.; et al. Systematic evaluation of normalization approaches in tandem mass tag and label-free protein quantification data using PRONE. Brief. Bioinform. 2025, 26, bbaf201. [Google Scholar] [CrossRef]
- Patel, M.A.; Fraser, D.D.; Daley, M.; Cepinskas, G.; Veraldi, N.; Grazioli, S. The plasma proteome differentiates the multisystem inflammatory syndrome in children (MIS-C) from children with SARS-CoV-2 negative sepsis. Mol. Med. 2024, 30, 51. [Google Scholar] [CrossRef]
- Dubois, E.; Galindo, A.N.; Dayon, L.; Cominetti, O. Assessing normalization methods in mass spectrometry-based proteome profiling of clinical samples. BioSystems 2022, 215–216, 104661. [Google Scholar] [CrossRef] [PubMed]
- Chua, A.E.; Pfeifer, L.D.; Sekera, E.R.; Hummon, A.B.; Desaire, H. Workflow for Evaluating Normalization Tools for Omics Data Using Supervised and Unsupervised Machine Learning. J. Am. Soc. Mass Spectrom. 2023, 34, 2775–2784. [Google Scholar] [CrossRef]
- Kronenberg, F.; Utermann, G. Lipoprotein(a): Resurrected by genetics. J. Intern. Med. 2013, 273, 6–30. [Google Scholar] [CrossRef] [PubMed]
- Tsimikas, S. A Test in Context: Lipoprotein(a): Diagnosis, Prognosis, Controversies, and Emerging Therapies. J. Am. Coll. Cardiol. 2017, 69, 692–711. [Google Scholar] [CrossRef]
- Kronenberg, F. Lipoprotein(a). Handb. Exp. Pharmacol. 2022, 270, 201–232. [Google Scholar] [CrossRef]
- Patel, A.P.; Wang, M.; Pirruccello, J.P.; Ellinor, P.T.; Ng, K.; Kathiresan, S.; Khera, A.V. Lp(a) (Lipoprotein[a]) Concentrations and Incident Atherosclerotic Cardiovascular Disease New Insights from a Large National Biobank. Arterioscler. Thromb. Vasc. Biol. 2021, 41, 465–474. [Google Scholar] [CrossRef]
- Bergmark, C.; Dewan, A.; Orsoni, A.; Merki, E.; Miller, E.R.; Shin, M.J.; Binder, C.J.; Hörkkö, S.; Krauss, R.M.; Chapman, M.J.; et al. A novel function of lipoprotein [a] as a preferential carrier of oxidized phospholipids in human plasma. J. Lipid Res. 2008, 49, 2230–2239. [Google Scholar] [CrossRef] [PubMed]
- Van Der Valk, F.M.; Bekkering, S.; Kroon, J.; Yeang, C.; Van Den Bossche, J.; Van Buul, J.D.; Ravandi, A.; Nederveen, A.J.; Verberne, H.J.; Scipione, C.; et al. Oxidized phospholipids on Lipoprotein(a) elicit arterial wall inflammation and an inflammatory monocyte response in humans. Circulation 2016, 134, 611–624. [Google Scholar] [CrossRef]
- Ekelund, L.; Laurell, C.B. The pregnancy zone protein response during gestation: A metabolic challenge. Scand. J. Clin. Lab. Investig. 1994, 54, 623–629. [Google Scholar] [CrossRef]
- Fosheim, I.K.; Jacobsen, D.P.; Sugulle, M.; Alnaes-Katjavivi, P.; Fjeldstad, H.E.S.; Ueland, T.; Lekva, T.; Staff, A.C. Serum amyloid A1 and pregnancy zone protein in pregnancy complications and correlation with markers of placental dysfunction. Am. J. Obstet. Gynecol. MFM 2023, 5, 100794. [Google Scholar] [CrossRef]
- Gao, G.; Xuan, C.; Yang, Q.; Liu, X.C.; Liu, Z.G.; He, G.W. Identification of Altered Plasma Proteins by Proteomic Study in Valvular Heart Diseases and the Potential Clinical Significance. PLoS ONE 2013, 8, e72111. [Google Scholar] [CrossRef]
- Kim, Y.; Kang, U.B.; Kim, S.; Lee, H.B.; Moon, H.G.; Han, W.; Noh, D.Y. A validation study of a multiple reaction monitoring-based proteomic assay to diagnose breast cancer. J. Breast Cancer 2020, 23, 113–114. [Google Scholar] [CrossRef]
- Youssef, L.; Erlandsson, L.; Åkerström, B.; Miranda, J.; Paules, C.; Crovetto, F.; Crispi, F.; Gratacos, E.; Hansson, S.R. Hemopexin and α1-microglobulin heme scavengers with differential involvement in preeclampsia and fetal growth restriction. PLoS ONE 2020, 15, e0239030. [Google Scholar] [CrossRef] [PubMed]
- Kalapotharakos, G.; Murtoniemi, K.; Åkerström, B.; Hämäläinen, E.; Kajantie, E.; Räikkönen, K.; Villa, P.; Laivuori, H.; Hansson, S.R. Plasma heme scavengers alpha-1microglobulin and hemopexin as biomarkers in high-risk pregnancies. Front. Physiol. 2019, 10, 300. [Google Scholar] [CrossRef] [PubMed]
- Anderson, U.D.; Gram, M.; Ranstam, J.; Thilaganathan, B.; Åkerström, B.; Hansson, S.R. Fetal hemoglobin, α1-microglobulin and hemopexin are potential predictive first trimester biomarkers for preeclampsia. Pregnancy Hypertens. 2016, 6, 103–109. [Google Scholar] [CrossRef]
- Smith, G.C.S.; Stenhouse, E.J.; Crossley, J.A.; Aitken, D.A.; Cameron, A.D.; Michael Connor, J. Early pregnancy levels of pregnancy-associated plasma protein A and the risk of intrauterine growth restriction, premature birth, preeclampsia, and stillbirth. J. Clin. Endocrinol. Metab. 2002, 87, 1762–1767. [Google Scholar] [CrossRef] [PubMed]
- Krantz, D.; Goetzl, L.; Simpson, J.L.; Thom, E.; Zachary, J.; Hallahan, T.W.; Silver, R.; Pergament, E.; Platt, L.D.; Filkins, K.; et al. Association of extreme first-trimester free human chorionic gonadotropin-β, pregnancy-associated plasma protein A, and nuchal translucency with intrauterine growth restriction and other adverse pregnancy outcomes. Am. J. Obstet. Gynecol. 2004, 191, 1452–1458. [Google Scholar] [CrossRef]
- Livrinova, V.; Petrov, I.; Samardziski, I.; Jovanovska, V.; Boshku, A.A.; Todorovska, I.; Dabeski, D.; Shabani, A. Clinical importance of low level of PAPP-A in first trimester of pregnancy-An obstetrical dilemma in chromosomally normal fetus. Open Access Maced. J. Med. Sci. 2019, 7, 1475–1479. [Google Scholar] [CrossRef]
- Dugoff, L.; Hobbins, J.C.; Malone, F.D.; Porter, T.F.; Luthy, D.; Comstock, C.H.; Hankins, G.; Berkowitz, R.L.; Merkatz, I.; Craigo, S.D.; et al. First-trimester maternal serum PAPP-A and free-beta subunit human chorionic gonadotropin concentrations and nuchal translucency are associated with obstetric complications: A population-based screening study (The FASTER Trial). Am. J. Obstet. Gynecol. 2004, 191, 1446–1451. [Google Scholar] [CrossRef]
- Savvidou, M.D.; Syngelaki, A.; Muhaisen, M.; Emelyanenko, E.; Nicolaides, K.H. First trimester maternal serum free β-human chorionic gonadotropin and pregnancy-associated plasma protein A in pregnancies complicated by diabetes mellitus. BJOG An Int. J. Obstet. Gynaecol. 2012, 119, 410–416. [Google Scholar] [CrossRef]
- Caliskan, R.; Atis, A.; Aydin, Y.; Acar, D.; Kiyak, H.; Topbas, F. PAPP-A concentrations change in patients with gestational diabetes. J. Obstet. Gynaecol. 2020, 40, 190–194. [Google Scholar] [CrossRef]
- Liu, S.; Shi, H.; He, S.; Hu, L.; Zhao, Y. Differences in physiological indicators between twin and singleton pregnancy. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2025, 169, 663–670. [Google Scholar] [CrossRef]
- Taneja, P.A.; Snyder, H.L.; de Feo, E.; Kruglyak, K.M.; Halks-Miller, M.; Curnow, K.J.; Bhatt, S. Noninvasive prenatal testing in the general obstetric population: Clinical performance and counseling considerations in over 85,000 cases. Prenat. Diagn. 2016, 36, 237–243. [Google Scholar] [CrossRef]
- Dröge, L.; Herraiz, I.; Zeisler, H.; Schlembach, D.; Stepan, H.; Küssel, L.; Henrich, W.; Galindo, A.; Verlohren, S. Maternal serum sFlt-1/PlGF ratio in twin pregnancies with and without pre-eclampsia in comparison with singleton pregnancies. Ultrasound Obstet. Gynecol. 2015, 45, 286–293. [Google Scholar] [CrossRef]
- Romero, R.; Erez, O.; Maymon, E.; Xu, Z.; Pacora, P.; Done, B.; Hassan, S.S.; Tarca, A.L.; Arbor, A.; Lansing, E. The Maternal Plasma Proteome Changes as a Function of Gestational Age in Normal Pregnancy: A Longitudinal Study. Am. J. Obstet. Gynecol. 2017, 155, 1683–1695. [Google Scholar] [CrossRef]
- Poon, L.C.Y.; Zymeri, N.A.; Zamprakou, A.; Syngelaki, A.; Nicolaides, K.H. Protocol for measurement of mean arterial pressure at 11-13 weeks’ gestation. Fetal Diagn. Ther. 2012, 31, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Plasencia, W.; Maiz, N.; Bonino, S.; Kaihura, C.; Nicolaides, K.H. Uterine artery Doppler at 11 + 0 to 13 + 6 weeks in the prediction of preeclampsia. Ultrasound Obstet. Gynecol. 2007, 30, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Bugrova, A.E.; Strelnikova, P.A.; Kononikhin, A.S.; Zakharova, N.V.; Diyachkova, E.O.; Brzhozovskiy, A.G.; Indeykina, M.I.; Kurochkin, I.N.; Averyanov, A.V.; Nikolaev, E.N. Targeted MRM-analysis of plasma proteins in frozen whole blood samples from patients with COVID-19: A retrospective study. Clin. Chem. Lab. Med. 2024, 63, 448–457. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, M.; Weigl, K.; Tikk, K.; Holland-Letz, T.; Schrotz-King, P.; Borchers, C.H.; Brenner, H. Multiplex quantitation of 270 plasma protein markers to identify a signature for early detection of colorectal cancer. Eur. J. Cancer 2020, 127, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Domanski, D.; Percy, A.J.; Yang, J.; Chambers, A.G.; Hill, J.S.; Freue, G.V.C.; Borchers, C.H. MRM-based multiplexed quantitation of 67 putative cardiovascular disease biomarkers in human plasma. Proteomics 2012, 12, 1222–1243. [Google Scholar] [CrossRef] [PubMed]
- MacLean, B.X.; Pratt, B.S.; Egertson, J.D.; MacCoss, M.J.; Smith, R.D.; Baker, E.S. Using Skyline to Analyze Data-Containing Liquid Chromatography, Ion Mobility Spectrometry, and Mass Spectrometry Dimensions. J. Am. Soc. Mass Spectrom. 2018, 29, 2182–2188. [Google Scholar] [CrossRef]
- Lee, J.; Park, J.; Lim, M.S.; Seong, S.J.; Seo, J.J.; Park, S.M.; Lee, H.W.; Yoon, Y.R. Quantile normalization approach for liquid chromatography-mass spectrometry-based metabolomic data from healthy human volunteers. Anal. Sci. 2012, 28, 801–805. [Google Scholar] [CrossRef]
- Ballman, K.V.; Grill, D.E.; Oberg, A.L.; Therneau, T.M. Faster cyclic loess: Normalizing RNA arrays via linear models. Bioinformatics 2004, 20, 2778–2786. [Google Scholar] [CrossRef]
- Bolstad, B.M.; Irizarry, R.A.; Astrand, M.; Speed, T.P. A comparison of normalization methods for high density oligonucleotide array data based on variance and bias. Bioinformatics 2003, 19, 185–193. [Google Scholar] [CrossRef]
- Johnson, W.E.; Li, C.; Rabinovic, A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics 2007, 8, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Leek, J.T.; Johnson, W.E.; Parker, H.S.; Jaffe, A.E.; Storey, J.D. The SVA package for removing batch effects and other unwanted variation in high-throughput experiments. Bioinformatics 2012, 28, 882–883. [Google Scholar] [CrossRef]
- Ritchie, M.E.; Phipson, B.; Wu, D.; Hu, Y.; Law, C.W.; Shi, W.; Smyth, G.K. Limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015, 43, e47. [Google Scholar] [CrossRef]
- Wickham, H. Reshaping data with the reshape package. J. Stat. Softw. 2007, 21, 1–20. [Google Scholar] [CrossRef]
- Wickham, H. Elegant Graphics for Data Analysis: Ggplot2; Springer: Berlin/Heidelberg, Germany, 2008; ISBN 978-0-387-78170-9. [Google Scholar]
- Kolde, R. Pheatmap: Pretty Heatmaps. Available online: https://CRAN.R-project.org/package=pheatmap (accessed on 16 August 2025).

| Clinical Characteristic | Value |
|---|---|
| Age, years | 30.5 (27.4; 32.8) 20.5–37.3 |
| BMI, kg/m2 | 21.2 (19.2; 23.0) 15.6–30.1 |
| Gestational age at blood collection, weeks | 12.4 (12.1; 12.9) 11.3–13.9 |
| Gestational age at delivery, weeks | 39.5 (39; 40.2) 37.5–41.2 |
| Uterine myoma, n (%) | 8 (10%) |
| Anemia during pregnancy, n (%) | 27 (33%) |
| Fetal sex (male) | 41 (49%) |
| Parity, n (%) | 1–40 (48%) 2–32 (39%) 3–10 (12%) 4–1 (1%) |
| 1st screening | |
| PAPP-A, mLU/mL | 3.03 (2.08; 4.59) 0.598–9.761 |
| PAPP-A, MoM | 0.95 (0.65; 1.47) 0.196–4.271 |
| PlGF, pg/ml | 25.3 (20.2; 35) 13.3–54 |
| PlGF, MoM | 0.84 (0.61; 1.03) 0.374–1.521 |
| free β-HGC, ng/ml | 52.61 (37.38; 75.54) 12.57–224.31 |
| free β-HGC, MoM | 0.99 (0.78; 1.2) 0.533–1.667 |
| UtA-PI | 1.57 (1.29; 2.02) 0.89–2.655 |
| UtA-PI, MoM | 0.99 (0.78; 1.2) 0.533–1.667 |
| MAP, mmHg | 83.33 (77.46; 86.46) 66–98.833 |
| MAP, MoM | 0.98 (0.94; 1.04) 0.8027–1.1755 |
| Risk of PE | 1357.5 (516.75; 2816.5) 63–15,320 |
| Risk of IUGR | 554 (377; 877) 81–2501 |
| Risk of preterm delivery | 2115.5 (890; 3209.75) 5–5026 |
| Risk of 21th trisomy (background) | 618 (405; 830) 159–1108 |
| Risk of 21th trisomy (adjusted) | 9997 (5206; 15,160) 227–22,160 |
| Risk of 18th trisomy (background) | 1471 (976; 2115) 381–2787 |
| Risk of 18th trisomy (adjusted) | 2870 (16,161; 41,012) 409–55,750 |
| Risk of 13th trisomy (background) | 4589 (3065; 6609) 1197–8722 |
| Risk of 13th trisomy (adjusted) | 83,050 (45,488; 122,252) 9180–174,431 |
| Clinical | Direction of Association | Protein (Gene Name) |
|---|---|---|
| BMI | direct | ATRN, CA4BPA, CP, F12, C1QA, C1R, C3, CFB, CFI, HP, HABP2, APCS |
| reverse | AHSG, SERPINC1, APOA4, APOD, CA1, HBA1, IGFBP3, SERPING1, AZGP1 | |
| Age | direct | SERPIND1 |
| reverse | A2M | |
| Parity | direct | AGT, APOC3, CNDP1, CA1, IGHG1, KNG1, PLG |
| reverse | ATRN, F12, SERPINA6, SELL, PAPP-A, ALB | |
| Gestational age at blood collection | direct | VTN |
| reverse | HRG | |
| Uterine myoma | direct | KNG1 |
| reverse | APOA4, SPARC | |
| Male fetal sex | direct | BTD, CA1 |
| reverse | SERPINA3, APOH, CP, C5, C9, HBA1, LRG1, PROS1, AZGP1 |
| Screening | LC-MS | R | p-Value |
|---|---|---|---|
| 3.03 (2.08; 4.59) IU/mL | 6.59 (4.84; 8.82) nM | 0.65 | <0.001 |
| 0.95 (0.65; 1.47) MoM | 6.59 (4.84; 8.82) nM | 0.56 | <0.001 |
| 0.95 (0.65; 1.47) MoM | 0.95 (0.65; 1.28) MoM | 0.58 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Starodubtseva, N.; Tokareva, A.; Kononikhin, A.; Brzhozovskiy, A.; Bugrova, A.; Kukaev, E.; Poluektova, A.; Frankevich, V.; Nikolaev, E.; Sukhikh, G. Multiplexed Quantification of First-Trimester Serum Biomarkers in Healthy Pregnancy. Int. J. Mol. Sci. 2025, 26, 7970. https://doi.org/10.3390/ijms26167970
Starodubtseva N, Tokareva A, Kononikhin A, Brzhozovskiy A, Bugrova A, Kukaev E, Poluektova A, Frankevich V, Nikolaev E, Sukhikh G. Multiplexed Quantification of First-Trimester Serum Biomarkers in Healthy Pregnancy. International Journal of Molecular Sciences. 2025; 26(16):7970. https://doi.org/10.3390/ijms26167970
Chicago/Turabian StyleStarodubtseva, Natalia, Alisa Tokareva, Alexey Kononikhin, Alexander Brzhozovskiy, Anna Bugrova, Evgenii Kukaev, Alina Poluektova, Vladimir Frankevich, Evgeny Nikolaev, and Gennady Sukhikh. 2025. "Multiplexed Quantification of First-Trimester Serum Biomarkers in Healthy Pregnancy" International Journal of Molecular Sciences 26, no. 16: 7970. https://doi.org/10.3390/ijms26167970
APA StyleStarodubtseva, N., Tokareva, A., Kononikhin, A., Brzhozovskiy, A., Bugrova, A., Kukaev, E., Poluektova, A., Frankevich, V., Nikolaev, E., & Sukhikh, G. (2025). Multiplexed Quantification of First-Trimester Serum Biomarkers in Healthy Pregnancy. International Journal of Molecular Sciences, 26(16), 7970. https://doi.org/10.3390/ijms26167970







