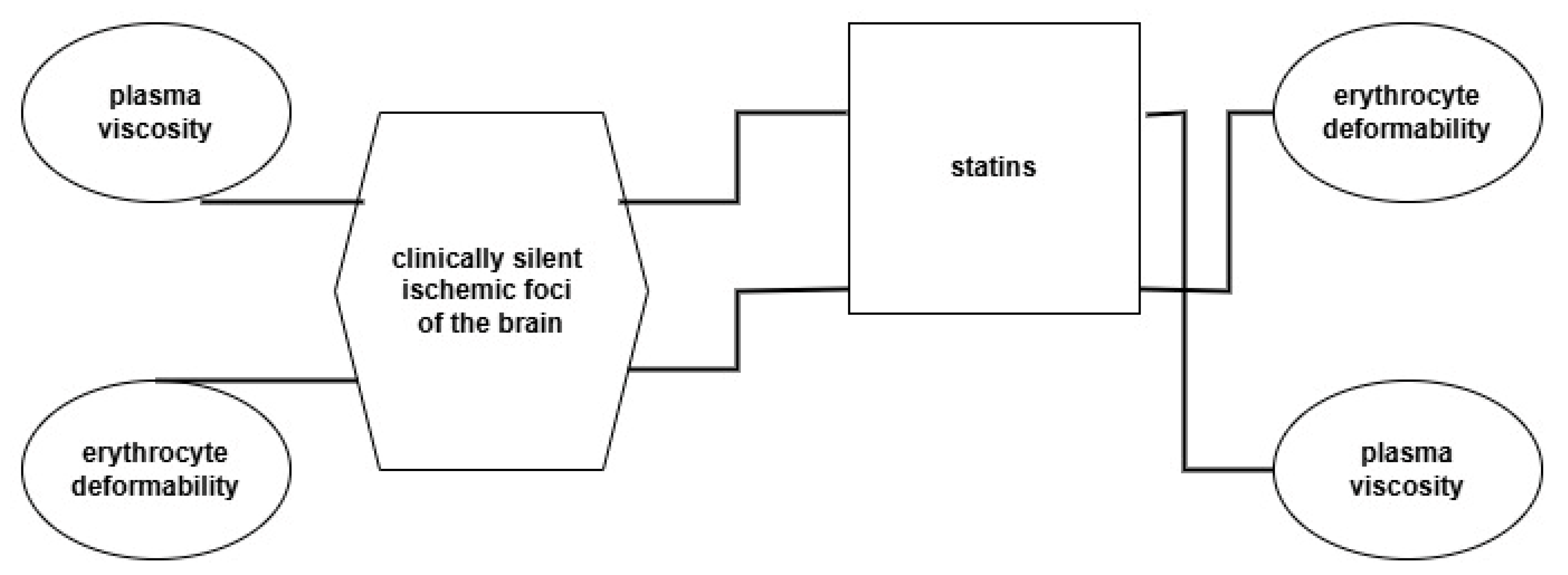
The Effect of Statin Therapy on Hemorheological Parameters of Patients with Clinically Silent Ischemic Foci of the Brain
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baskurt, O.K.; Hardeman, M.R.; Rampling, M.W.; Meiselman, H.J. Handbook of Hemorheology and Hemodynamics; IOS Press: Amsterdam, The Netherlands, 2007. [Google Scholar]
- Nader, E.; Skinner, S.; Romana, M.; Fort, R.; Lemonne, N.; Guillot, N.; Gauthier, A.; Antoine-Jonville, S.; Renoux, C.; Hardy-Dessources, M.-D.; et al. Blood Rheology: Key Parameters, Impact on Blood Flow, Role in Sickle Cell Disease and Effects of Exercise. Front. Physiol. 2019, 10, 1329. [Google Scholar] [CrossRef] [PubMed]
- Sloop, G.D.; De Mast, Q.; Pop, G.; Weidman, J.J.; Cyr, J.A. The Role of Blood Viscosity in Infectious Diseases. Cureus 2020, 12, e7090. [Google Scholar] [CrossRef] [PubMed]
- Késmárky, G.; Kenyeres, P.; Rábai, M.; Tóth, K. Plasma viscosity: A forgotten variable. Clin. Hemorheol. Microcirc. 2008, 39, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Kwaan, H.C. Role of plasma proteins in whole blood viscosity: A brief clinical review. Clin. Hemorheol. Microcirc. 2010, 44, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Marcinkowska-Gapińska, A.; Kowal, P. Hemorheological studies of chosen clinical cases. J. Med. Sci. 2015, 84, 197–200. [Google Scholar] [CrossRef]
- Kowal, P.; Marcinkowska-Gapińska, A. Hemorheological changes dependent on the time from the onset of ischemic stroke. J. Neurol. Sci. 2007, 258, 132–136. [Google Scholar] [CrossRef] [PubMed]
- Szapary, L.; Horvarth, B.; Marton, Z.; Alexy, T. Hemorheological disturbances in patients with chronic cerebrovascular diseases. Clin. Hemorheol. Microcirc. 2004, 31, 1–9. [Google Scholar] [PubMed]
- Chen, G.; Zhao, L.; Liu, Y.W.; Liao, F.; Han, D.; Zhou, H. Regulation of blood viscosity in disease prevention and treatment. Chin. Sci. Bull. 2012, 57, 946–1952. [Google Scholar] [CrossRef]
- Momtselidze, N.; Mantskava, M.; Mchedlishvili, G. Hemorheological disorders during ischemic brain infarcts in patients with and without diabetes mellitus. Clin. Hemorheol. Microcirc. 2006, 35, 261–264. [Google Scholar] [PubMed]
- Tichomirowa, I.A.; Oslyakova, A.O.; Mikhailova, S.G. Microcirculation and blood rheology in patients with cerebrovascular disorders. Clin. Hemorheol. Microcirc. 2011, 49, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Gyawali, P.; Lillicrap, T.P.; Esperon, C.G.; Bhattarai, A.; Bivard, A.; Spratt, N. Whole Blood Viscosity and Cerebral Blood Flow in Acute Ischemic Stroke. Semin. Thromb. Hemost. 2024, 50, 580–591. [Google Scholar] [CrossRef] [PubMed]
- Yoshiyasu, T.; Kiyoto, S.; Masaya, K.; Tsutomu, T. Hemorheologic profiles of plasma fibrinogen and blood viscosity from silent to acute and chronic cerebral infarctions. J. Neurol. Sci. 1997, 147, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Antonova, N.; Velcheva, I. Hemorheological disturbances ad characteristic parameters in patients with cerebrovascular disease. Clin. Hemorheol. Microcirc. 1999, 21, 405–408. [Google Scholar] [PubMed]
- Velcheva, I.; Antonova, N.; Ivanov, I. Plasma lipids and blood viscosity in patients with cerebrovascular disease. Clin. Hemorheol. Microcirc. 2006, 35, 155–157. [Google Scholar] [PubMed]
- Li, R.Y.; Cao, Z.G.; Li, Y.; Wang, R.T. Increased whole blood viscosity is associated with silent cerebral infarction. Clin. Hemorheol. Microcirc. 2015, 59, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Marcinkowska-Gapińska, A.; Siemieniak, I.; Kawałkiewicz, W.; Stieler, O.; Hojan-Jezierska, D.; Kubisz, L. Interdependence of Rheological and Biochemical Parameters of Blood in a Group of Patients with Clinically Silent Multifocal Vascular Cerebral Lesions. Biomedicine 2023, 11, 2063. [Google Scholar] [CrossRef] [PubMed]
- Maciejewska, B.; Marcinkowska-Gapińska, A.; Iwanowski, P.; Maciejewska-Szaniec, Z.; Kowal, P. Biochemical parameters of patients with clinically silent cerebral lesions depend on gender—A preliminary study. Fam. Med. Prim. Care Rev. 2020, 22, 208–211. [Google Scholar] [CrossRef]
- Fanning, J.P.; Wong, A.A.; Fraser, J. The epidemiology of silent brain infarction: A systematic review of population-based cohorts. BMC Med. 2014, 12, 119. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.; Wang, Z.; Dong, J.; Yu, M.; Zhou, Y. Lipoprotein(a) and panvascular disease. Lipids Health Dis. 2025, 24, 186. [Google Scholar] [CrossRef] [PubMed]
- Moriarty, P.M.; Gibson, C.A. Association between hematological parameters and high-density lipoprotein cholesterol. Curr. Opin. Cardiol. 2005, 20, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Nara, M.; Sumino, H.; Nara, M.; Machida, T.; Amagai, H.; Nakajima, K.; Murakami, M. Impaired Blood Rheology and Elevated Remnant-likeLipoprotein Particle Cholesterol in Hypercholesterolemic Subjects. Int. J Med. Res. 2009, 37, 308–317. [Google Scholar] [CrossRef] [PubMed]
- Pryzwan, T.; Dolibog, P.; Kierszniok, K.; Pietrzyk, B. Blood rheological properties and methods of their measurement. Ann. Acad. Med. Siles. (Online) 2024, 78, 1–10. [Google Scholar] [CrossRef]
- Koenig, W.; Ernst, E. The possible role of hemorheology in atherothrombogenesis. Atherosclerosis 1992, 94, 93–107. [Google Scholar] [CrossRef] [PubMed]
- Białecki, R.; Adamczyk, W.; Borys, D.; Głowacki, J.; Gracka, M.; Melka, B.; Psiuk-Masymowicz, K.; Ostrowski, Z.; Rojczyk, M.; Wasilewski, J. Blood flow in deforming vessels. J Phys. Conf. Ser. 2024, 2766, 012191. [Google Scholar] [CrossRef]
- Wasilewski, J.; Poloński, L. Importance of fibrynogen and the rheological properties of blond In atherosclerosis and coronary disease. Chor. Serca I Naczyń 2010, 7, 62–71. [Google Scholar]
- Undas, A.; Podolec, P.; Zawilska, K.; Pieculewicz, M.; Jedlińsk, I.; Stepień, E.; Konarska-Kuszewska, E.; Węglarz, P.; Duszyńska, M.; Hanschke, E.; et al. Altered Fibrin clot struture/function in patients with cryptogenic ischemic stroke. Stroke 2009, 40, 1499–1501. [Google Scholar] [CrossRef] [PubMed]
- Kościelny, J.; Jung, E.M.; Mrowietz, C.; Kiesewetter, H.; Latza, R. Blood fluidity, fibrinogen, and cardiovascular risk factors of occlusive arterial disease: Results of the Aachen study. Clin. Hemorheol. Microcirc. 2004, 31, 185–195. [Google Scholar] [PubMed]
- Santos, M.T.; Valles, J.; Lago, A.; Tembl, J.; Snachez, E.; Moscardo, A.; Cosin, J. Residual platelet thromboxane A2 and prothrombotic effects of erythrocytes are important determinants of aspirin resistance in patients with vascular disease. J. Thromb. Haemost. 2008, 6, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Sirolli, V.; Strizzi, L.; Di Sante, S.; Robuffo, I.; Procopio, A. Platelet activation and platelet-erythrocyte aggregates in end-stage renal disease patients on hemodialysis. J. Thromb. Haemost. 2001, 86, 834–839. [Google Scholar] [CrossRef]
- Valles, J.; Santos, M.T.; Aznar, J.; Martinez, M.; Moscardo, A.; Pinon, M.; Broekman, J.; Marcus, A.J. Platelet-erythrocyte interactions enhance αIIbβ3integrin receptor activation and P-selectin expression during platelet recruitment: Down-regulation by aspirin ex vivo. Blood 2002, 99, 3978–3984. [Google Scholar] [CrossRef] [PubMed]
- Broncel, M.; Chojnowska-Jezierska, J.; Koter-Michalak, M.; Franiak, I. Erythrocyte fluidity in patients with hyperlipidemia during statins therapy. Pol. Arch. Med. Wewn. 2005, 13, 531–537. [Google Scholar]
- Elhwuegi, A.S.; Elfakhri, M.M. Pharmacological Profile and Mechanisms of Cardiovascular Protective Effects of Statins: An Update. Libyan Int. Med. Univ. J. 2025, 10, 18–28. [Google Scholar] [CrossRef]
- Cecchini, A.L.; Nicolazzi, M.A.; Covino, M.; Gasbarrini, A.; Massetti, M.; Flex, A. Statins in High Cardiovascular Risk Patients: Do Comorbidities and Characteristics Matter? Int. J. Mol. Sci. 2022, 23, 9326. [Google Scholar] [CrossRef] [PubMed]
- Jung, L.Y.; Lee, S.R.; Jung, J.M.; Kim, Y.S.; Lee, S.H.; Rhee, K.S. Rosuvastatin Reduces Blood Viscosity in Patients with Acute Coronary Syndrome. Korean Circ. J. 2016, 46, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Rasyid, A.; Harris, S.; Kurniawan, M.; Mesiano, T.; Hidayat, R. Fibrinogen and LDL Influence on Blood Viscosity and Outcome of Acute Ischemic Stroke Patients in Indonesia. Ann. Neurosci. 2019, 26, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Lowe, G.D.O.; Rumley, A.; Whincup, P.H.; Dansh, J. Hemostatic and rheological variable and risk of cardiovascular disease. Semin. Vasc. Med. 2002, 2, 429–440. [Google Scholar] [CrossRef] [PubMed]
- Musielak, M. Red blood cell-deformability measurement: Review of techniques. Clin. Hemoreol. Microcirc. 2009, 42, 47–64. [Google Scholar] [CrossRef] [PubMed]
- O’Keefe, J.H.; Carter, M.D.; Lavie, C.J. Primary and Secondary Prevention of Cardiovascular Diseases: A Practical Evidence-Based Approach. Mayo Clin. Proc. 2009, 84, 741–757. [Google Scholar] [CrossRef] [PubMed]
- Diener, H.C.; Hankey, G.J. Primary and Secondary Prevention of Ischemic Stroke and Cerebral Hemorrhage: JACC Focus Seminar. J. Am. Coll. Cardiol. 2020, 75, 1804–1818. [Google Scholar] [CrossRef] [PubMed]
- Beamer, N.; Coull, B.M.; Sexton, G.; de Garmo, P.; Knox, R.; Seaman, G. Fibrinogen and the albumin-globulin ratio in recurrent stroke. Stroke 1993, 24, 1133–1139. [Google Scholar] [CrossRef] [PubMed]
- Coull, B.M.; Beamer, N.; de Garmo, P.; Sexton, G.; Nordt, F.; Knox, R.; Seaman, G.V. Chronic blood hyperviscosity in subjects with acute stroke, transient ischemic attack, and risk factors for stroke. Stroke 1991, 22, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.; Lau, E.; Kay, R.; Lam, C.W.; Cheung, C.K.; Swaminathan, R.; Nicolls, M.G. A case control study of some hematological and biochemical variables in acute stroke and their prognostic value. Neuroepidemiology 1990, 9, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Ami, R.B.; Barshtein, G.; Zeltser, D.; Goldberg, Y.; Shapira, I.; Roth, A.; Keren, G.; Miller, H.; Prochorov, V.; Eldor, A.; et al. Parameters of red blood cell aggregation as correlates of the inflammatory state. Am. J. Physiol. Heart Circ. Physiol. 2001, 280, H1982–H1988. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, J.K.; Wenby, R.B.; Meiselman, H.J.; Fisher, T.C. The hydrodynamic radii of macromolecules and their effect on red blood cell aggregation. Biophys. J. 2004, 87, 4259–4270. [Google Scholar] [CrossRef] [PubMed]
- Cummings, D.M.; Ballas, S.K.; Ellison, M.J. Lack of effect of pentoxifylline on red blood cell deformability. J. Clin. Pharmacol. 1992, 32, 1050–1053. [Google Scholar] [CrossRef] [PubMed]
- Bath, P.M.; Bath-Hextall, F.J. Pentoxifylline, propentofylline and pentifylline for acute ischaemic stroke. Cochrane Database Syst. Rev. 2004, 3, CD000162. [Google Scholar] [CrossRef] [PubMed]
- Reinhart, W.H. Molecular biology and self-regulatory mechanisms of blood viscosity: A review. Biorheology 2001, 38, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Marioni, R.E.; Stewart, M.C.; Murray, G.D.; Deary, I.J.; Fowkes, F.G.R.; Lowe, G.D.O.; Rumley, A.; Price, J.F. Peripheral levels of fibrinogen, C-reactive protein, and plasma viscosity predict future cognitive decline in individuals without dementia. Psychosom. Med. 2009, 71, 901–906. [Google Scholar] [CrossRef] [PubMed]
- Dujowne, C.A.; Harris, W.S.; Altman, R.; Overhiser, R.W.; Black, D.M. Efect of atorvastatin on hmorheologic-hemostatic parameters and serum fibrinogen levels in hyperlipidemic patients. Am. J. Cardiol. 2000, 85, 350–353. [Google Scholar] [CrossRef] [PubMed]
- Szpernalowska, A.; Marcinkowska-Gapińska, A. Influence of physical activity on the values of hemorheological parameters. Qual. Sport 2024, 22, 54476. [Google Scholar] [CrossRef]
- Hendris, H.F.; Weststrate, J.A.; Vliet, T.; Meijer, G.W. Spreads enriched with three different levels of vegetable oil sterols and the degree of cholestetol lowering in normocholesterolaemic and mildly hypercholesterolaemic subjects. Eur. J. Nutr. 1999, 53, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Noakes, M.; Clifton, P.M.; Doornbos, A.M.E.; Trautwein, E.A. Plant sterol ester-enriched milk and yoghurt effectively reduce serum cholesterol in modestly hypercholesterolemic subjects. Eur. J. Nutr. 2005, 44, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Irace, C.; Carallo, C.; Scavelli, F.; Esposito, T.; De Franceschi, M.S.; Tripolino, C.; Gnasso, A. Influence of blood lipids on plasma and blood viscosity. Clin. Hemorheol. Microcirc. 2014, 57, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Carallo, C.; Irace, C.; Franceschi, M.S.; Esposito, T.; Tripolino, C.; Scavelli, V.; Merante, V.; Gnasso, A. The effect of HDL cholesterol on blood viscosity and plasma viscosity in healthy subjects. Clin. Hemorheol. Microcirc. 2013, 55, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Brun, J.F.; Varlet-Marie, E.; Myzia, J.; Mauverger, E.R.; Pretrius, E. Metabolic Influences Modulating Erythrocyte Deformability and Eryptosis. Metabolites 2022, 12, 4. [Google Scholar] [CrossRef] [PubMed]
- Uydu, H.A.; Yıldırmış, S.; Örem, C.; Calapoglu, M.; Alver, A.; Kural, B.; Örem, A. The Effects of Atorvastatin Therapy on Rheological Characteristics of Erythrocyte Membrane, Serum Lipid Profile and Oxidative Status in Patients with Dyslipidemia. J. Membr. Biol. 2012, 245, 697–705. [Google Scholar] [CrossRef] [PubMed]
- Martínez, M.; Vayá, A.; Gil, L.; Martí, R.; Dalmau, J.; Aznar, J. The cholesterol/phospholipid ratio of the erythrocyte membrane in children with familial hypercholesterolemia. Its relationship with plasma lipids and red blood cell aggregability. Clin. Hemorheol. Microcirc. 1998, 18, 259–263. [Google Scholar] [PubMed]
- Martinez, M.; Vaya, A.; Mart, R.; Gil, L.; Luch, I.; Carmena, R.; Aznar, J. Erythrocyte membrane cholesterol/phospholipid changes and hemorheological modifications in familiar hypercholesterolemia treated with lovastatin. Thromb. Res. 1996, 83, 375–388. [Google Scholar] [CrossRef] [PubMed]
- Paradkar, S.; Gambhire, P. The Role of Cytoskeleton of a Red Blood Cell in Its Deformability. J. Indian Inst. Sci. 2021, 101, 39–46. [Google Scholar] [CrossRef]
- Barshtein, G.; Pajic-Lijakovic, I.; Gural, A. Deformability of Stored Red Blood Cells. Front. Physiol. 2021, 22, 722896. [Google Scholar] [CrossRef] [PubMed]
- Horváth, Á.; Erostyák, J.; Szőke, É. Effect of Lipid Raft Disruptors on Cell Membrane Fluidity Studied by Fluorescence Spectroscopy. Int. J. Mol. Sci. 2022, 23, 13729. [Google Scholar] [CrossRef] [PubMed]
- Stanzani, A.; Sansone, A.; Brenna, C.; Baldassarro, V.A.; Alastra, G.; Lorenzini, L.; Chatgilialoglu, C.; Laface, I.; Ferreri, C.; Neri, L.M.; et al. Erythrocyte Plasma Membrane Lipid Composition Mirrors That of Neurons and Glial Cells in Murine Experimental In Vitro and In Vivo Inflammation. Cells 2023, 12, 561. [Google Scholar] [CrossRef] [PubMed]
- Vermeer, S.E.; Longstreth, W.T.; Koudstaal, P.J. Silent brain infarcts: A systematic review. Lancet Neurol. 2007, 6, 611–619. [Google Scholar] [CrossRef] [PubMed]
- Marcinkowska-Gapińska, A.; Gapiński, J.; Elikowski, W.; Jaroszyk, F.; Kubisz, L. Comparison of three rheological models of shear flow behavior studied on blood samples from post-infarction patients. Med. Biol. Eng. Comput. 2007, 45, 837–844. [Google Scholar] [CrossRef] [PubMed]
| Rheological Parameters | Control Group (Without Statins) n = 14 | p | Patient Group (Without Statins) n = 50 |
|---|---|---|---|
| Hematocrit [%] | 41.3 ± 0.9 | 0.44 | 42.0 ± 0.4 |
| Plasma viscosity ηp [mPas] | 1.42 ± 0.04 | 0.73 | 1.41 ± 0.01 |
| Relative viscosity of whole blood at a shear rate of 0.1 [s−1] | 28 ± 4 | 0.49 | 26 ± 1 |
| Relative viscosity of whole blood at a shear rate of 1 [s−1] | 14 ± 1 | 0.64 | 13.4 ± 0.6 |
| Relative viscosity of whole blood at a shear rate of 10 [s−1] | 5.7 ± 0.2 | 1 | 5.7 ± 0.1 |
| Relative viscosity of whole blood at a shear rate of 100 [s−1] | 3.32 ± 0.08 | 0.44 | 3.43 ± 0.07 |
| Queamada model parameter k0 | 4.33 ± 0.04 | 0.005 | 4.17 ± 0.03 |
| Queamada model parameter k∞ | 1.79 ± 0.02 | 0.05 | 1.69 ± 0.03 |
| Queamada model parameter γ’c | 6.2 ± 0.9 | 0.35 | 5.6 ± 0.3 |
| Parameters Biochemical | Control Group (Without Statins) n = 14 | p | Patient Group (Without Statins) n = 50 |
|---|---|---|---|
| fibrinogen | 4.1 ± 0.3 | 0.34 | 3.7 ± 0.2 |
| IgM | 1.4 ± 0.1 | 0.004 | 1.01 ± 0.07 |
| IgG | 9.4 ± 0.5 | 0.11 | 10.7 ± 0.4 |
| IgA | 2 ± 1 | 0.6 | 2.3 ± 0.1 |
| ESR | 8.4 ± 1.1 | 0.049 | 12 ± 1 |
| Albumins/globulins | 1.83 ± 0.12 | 0.009 | 1.56 ± 0.04 |
| Total protein | 70.3 ± 1.5 | 0.39 | 71.8 ± 0.8 |
| Glucose | 5.08 ± 0.09 | 0.22 | 5.46 ± 0.15 |
| Cholesterol | 5.7 ± 0.3 | 0.47 | 5.45 ± 0.16 |
| Rheological Parameters | Control Group (Statins) n = 3 | p | Patient Group (Statins) n = 19 |
|---|---|---|---|
| Hematocrit [%] | 39.5 ± 0.9 | 0.21 | 41.6 ± 0.6 |
| Plasma viscosity ηp [mPas] | 1.54 ± 0.05 | 0.03 | 1.34 ± 0.03 |
| Relative viscosity of whole blood at a shear rate of 0.1 [s−1] | 22 ± 7 | 0.42 | 29 ± 3 |
| Relative viscosity of whole blood at a shear rate of 1 [s−1] | 11 ± 1 | 0.27 | 14 ± 1 |
| Relative viscosity of whole blood at a shear rate of 10 [s−1] | 5.7 ± 0.2 | 0.64 | 6.2 ± 0.4 |
| Relative viscosity of whole blood at a shear rate of 100 [s−1] | 3.32 ± 0.08 | 0.48 | 3.7 ± 0.2 |
| Queamada model parameter k0 | 4.33 ± 0.14 | 0.72 | 4.27 ± 0.06 |
| Queamada model parameter k∞ | 1.75 ± 0.05 | 0.56 | 1.86 ± 0.07 |
| Queamada model parameter γ’c | 6.2 ± 0.9 | 0.39 | 5.0 ± 0.5 |
| Parameters Biochemical | Control Group (Statins) n = 3 | p | Patient Group (Statins) n = 19 |
|---|---|---|---|
| Fibrinogen | 4.8 ± 0.8 | 0.07 | 3.6 ± 0.2 |
| IgM | 1.4 ± 0.1 | 0.05 | 0.95 ± 0.08 |
| IgG | 9.4 ± 0.5 | 0.88 | 9.7 ± 0.5 |
| IgA | 2 ± 1 | 0.65 | 2.4 ± 0.2 |
| ESR | 8.4 ± 1.1 | 0.76 | 11 ± 2 |
| Albumins/globulins | 1.83 ± 0.12 | 0.047 | 1.58 ± 0.04 |
| Total protein | 70.3 ± 1.5 | 0.9 | 71 ± 1 |
| Glucose | 5.08 ± 0.09 | 0.6 | 5.7 ± 0.3 |
| Cholesterol | 5.7 ± 0.3 | 0.04 | 4.5 ± 0.2 |
| Rheological Parameters | Patient Group (Statins) n = 19 | p | Patient Group (Without Statins) n = 50 |
|---|---|---|---|
| Hematocrit [%] | 41.6 ± 0.6 | 0.6 | 42.0 ± 0.4 |
| Plasma viscosity ηp [mPas] | 1.34 ± 0.03 | 0.007 | 1.41 ± 0.01 |
| Relative viscosity of whole blood at a shear rate of 0.1 [s−1] | 29 ± 3 | 0.23 | 26 ± 1 |
| Relative viscosity of whole blood at a shear rate of 1 [s−1] | 14 ± 1 | 0.61 | 13.4 ± 0.6 |
| Relative viscosity of whole blood at a shear rate of 10 [s−1] | 6.2 ± 0.4 | 0.1 | 5.7 ± 0.1 |
| Relative viscosity of whole blood at a shear rate of 100 [s−1] | 3.7 ± 0.2 | 0.11 | 3.43 ± 0.07 |
| Queamada model parameter k0 | 4.27 ± 0.06 | 0.1 | 4.17 ± 0.03 |
| Queamada model parameter k∞ | 1.86 ± 0.07 | 0.01 | 1.69 ± 0.03 |
| Queamada model parameter γ’c | 5.0 ± 0.5 | 0.3 | 5.6 ± 0.3 |
| Biochemical Parameters | Patient Group (Statins) n = 19 | p | Patient Group (Without Statins) n = 50 |
|---|---|---|---|
| fibrinogen | 3.6 ± 0.2 | 0.l78 | 3.7 ± 0.2 |
| IgM | 0.95 ± 0.08 | 0.63 | 1.01 ± 0.07 |
| IgG | 9.7 ± 0.5 | 0.17 | 10.7 ± 0.4 |
| IgA | 2.4 ± 0.2 | 0.63 | 2.3 ± 0.1 |
| ESR | 11 ± 2 | 0.63 | 12 ± 1 |
| Albumins/globulins | 1.58 ± 0.04 | 0.77 | 1.56 ± 0.04 |
| Total proteins | 71 ± 1 | 0.58 | 71.8 ± 0.8 |
| Glucose | 5.7 ± 0.3 | 0.44 | 5.46 ± 0.15 |
| Cholesterol | 4.5 ± 0.2 | 0.002 | 5.45 ± 0.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcinkowska-Gapińska, A.; Siemieniak, I. The Effect of Statin Therapy on Hemorheological Parameters of Patients with Clinically Silent Ischemic Foci of the Brain. Int. J. Mol. Sci. 2025, 26, 7039. https://doi.org/10.3390/ijms26157039
Marcinkowska-Gapińska A, Siemieniak I. The Effect of Statin Therapy on Hemorheological Parameters of Patients with Clinically Silent Ischemic Foci of the Brain. International Journal of Molecular Sciences. 2025; 26(15):7039. https://doi.org/10.3390/ijms26157039
Chicago/Turabian StyleMarcinkowska-Gapińska, Anna, and Izabela Siemieniak. 2025. "The Effect of Statin Therapy on Hemorheological Parameters of Patients with Clinically Silent Ischemic Foci of the Brain" International Journal of Molecular Sciences 26, no. 15: 7039. https://doi.org/10.3390/ijms26157039
APA StyleMarcinkowska-Gapińska, A., & Siemieniak, I. (2025). The Effect of Statin Therapy on Hemorheological Parameters of Patients with Clinically Silent Ischemic Foci of the Brain. International Journal of Molecular Sciences, 26(15), 7039. https://doi.org/10.3390/ijms26157039







