Relationship of SCFAs to Maternal and Child Anthropometric Measurements
Abstract
1. Introduction
2. Results
3. Discussion
3.1. Neonatal SCFAs and Body Weight and BMI of Women
3.2. Neonatal SCFAs and Neonatal Body Weight and Apgar Score
3.3. Neonatal SCFAs and Weight Gain During Pregnancy
3.4. Metabolic Role of SCFAs
3.5. Limitations
4. Materials and Methods
4.1. Study Group
4.2. Determination of SCFAs in a Stool Sample
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
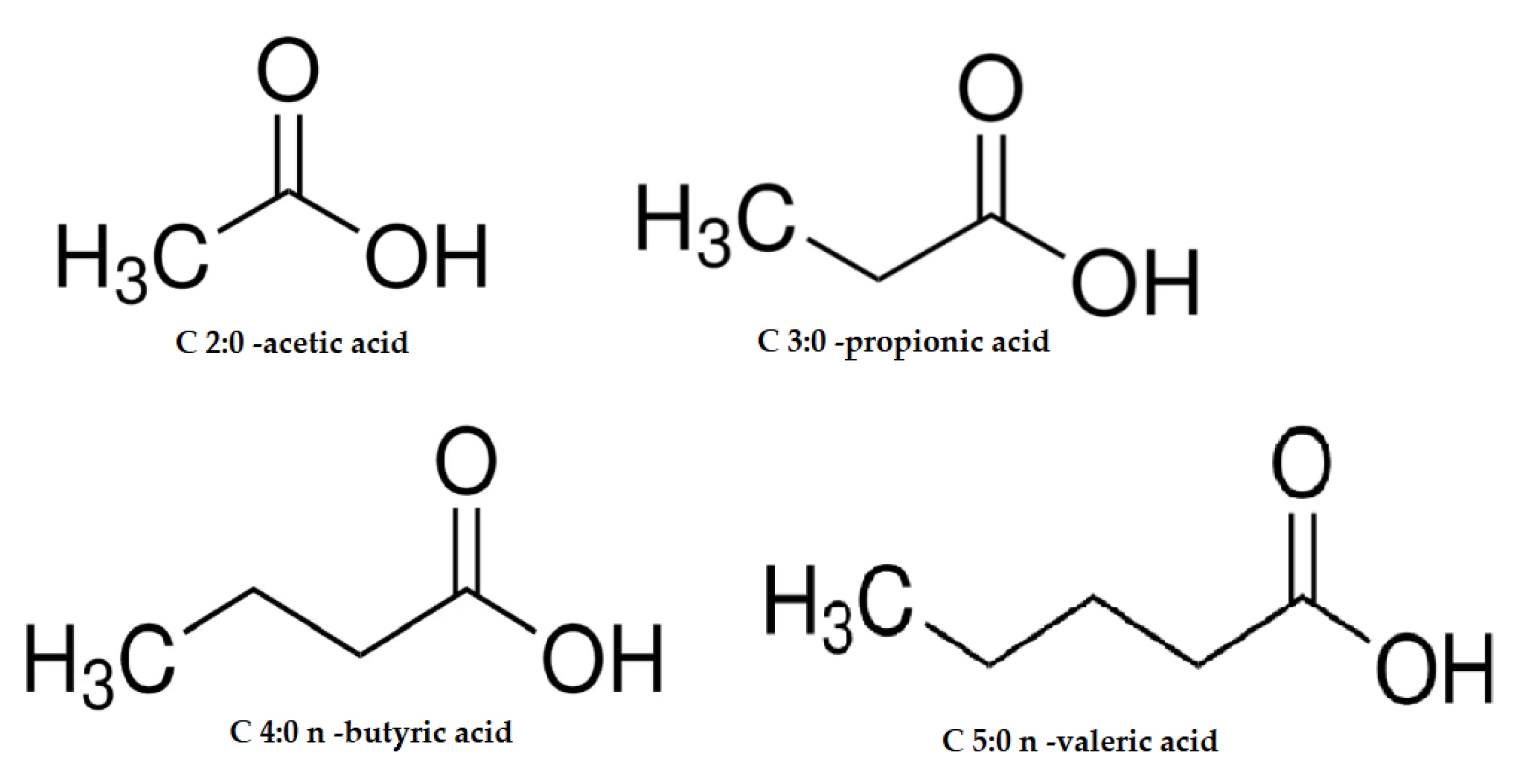
| BCFA | branched-chain short-chain fatty acid |
| BMI | body mass index |
| C 2:0 | acetic acid |
| C 3:0 | propionic acid |
| C 4:0 i | isobutyric acid |
| C 4:0 n | butyric acid |
| C 5:0 i | isovaleric acid |
| C 5:0 n | valeric acid |
| C 6:0 n | caproic acid |
| C 7:0 | heptanoic acid |
| SCFA | short-chain fatty acid |
References
- Chambers, E.; Preston, T.; Frost, G.; Morrison, D. Role of Gut Microbiota-Generated Short-Chain Fatty Acids in Metabolic and Cardiovascular Health. Curr. Nutr. Rep. 2018, 7, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Darzi, J.; Frost, G.; Robertson, M.D. Postgraduate Symposium Do SCFA have a role in appetite regulation? Proc. Nutr. Soc. 2011, 70, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Xiong, R.; Zhou, D.; Wu, S.; Huang, S.-Y.; Saimaiti, A.; Yang, A.; Shang, A.; Zhao, C.-N.; Gan, R.-Y.; Li, H.-B.; et al. Health Benefits and Side Effects of Short-Chain Fatty Acids. Foods 2022, 18, 2863. [Google Scholar] [CrossRef] [PubMed]
- Sahuri-Arisoylu, M.; Mould, R.; Shinjyo, N.; Bligh, S.; Nunn, A.; Guy, G.W.; Thomas, E.L.; Bell, J.D. Acetate Induces Growth Arrest in Colon Cancer Cells Through Modulation of Mitochondrial Function. Front. Nutr. 2021, 8, 588466. [Google Scholar] [CrossRef]
- Scheppach, W. Effects of short chain fatty acids on gut morphology and function. Gut 1994, 1, 35–38. [Google Scholar] [CrossRef]
- Xia, Z.; Han, Y.; Wang, K.; Guo, S.; Wu, D.; Huang, X.; Li, Z.; Zhu, L. Oral administration of propionic acid during lactation enhances the colonic barrier function. Lipids Health Dis. 2017, 16, 62. [Google Scholar] [CrossRef]
- Vidra, A.; Németh, A. Bio-produced Propionic Acid: A Review. Period. Polytech. Chem. Eng. 2018, 62, 57–67. [Google Scholar] [CrossRef]
- Gonzalez-Garcia, R.; McCubbin, T.; Navone, L.; Stowers, C.; Nielsen, L.; Marcellin, E. Microbial Propionic Acid Production. Fermentation 2017, 3, 21. [Google Scholar] [CrossRef]
- Załęski, A.; Banaszkiewicz, A.; Walkowiak, J. Butyric acid in irritable bowel syndrome. Przegląd Gastroenterol. 2013, 8, 350–353. [Google Scholar] [CrossRef]
- Feng, Y.; Wang, Y.; Wang, P.; Huang, Y.; Wang, F. Short-Chain Fatty Acids Manifest Stimulative and Protective Effects on Intestinal Barrier Function Through the Inhibition of NLRP3 Inflammasome and Autophagy. Cell. Physiol. Biochem. 2018, 49, 190–205. [Google Scholar] [CrossRef]
- Banasiewicz, T.; Domagalska, D.; Borycka-Kiciak, K.; Rydzewska, G. Determination of butyric acid dosage based on clinical and experimental studies—A literature review. Gastroenterol. Rev. 2020, 15, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Mirzaei, R.; Afaghi, A.; Babakhani, S.; Sohrabi, M.; Hosseini-Fard, S.; Babolhavaeji, K.; Akbari, S.K.A.; Yousefimashouf, R.; Karampoor, S. Role of microbiota-derived short-chain fatty acids in cancer development and prevention. Biomed. Pharmacother. 2021, 139, 1. [Google Scholar] [CrossRef] [PubMed]
- Goffredo, M.; Mass, K.; Parks, E.; Wagner, D.; McClure, E.; Graf, J.; Savoye, M.; Pierpont, B.; Cline, G.; Santoro, N. Role of Gut Microbiota and Short Chain Fatty Acids in Modulating Energy Harvest and Fat Partitioning in Youth. J. Clin. Endocrinol. Metabolism. 2016, 101, 4367–4376. [Google Scholar] [CrossRef]
- Portincasa, P.; Bonfrate, L.; Vacca, M.; De Angelis, M.; Farella, I.; Lanza, E.; Khalil, M.; Wang, D.Q.-H.; Sperandio, M.; Di Ciaula, A. Gut Microbiota and Short Chain Fatty Acids: Implications in Glucose Homeostasis. Int. J. Mol. Sci. 2022, 23, 1105. [Google Scholar] [CrossRef]
- Hamer, H. Short Chain Fatty Acids and Colonic Health. Ph.D. Thesis, Maastricht University, Maastricht, The Netherlands, 2009. [Google Scholar]
- Den Besten, G.; Van Eunen, K.; Groen, A.; Venema, K.; Reijngoud, D.-J.; Bakker, B. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J. Lipid Res. 2013, 54, 2325–2340. [Google Scholar] [CrossRef]
- Hernández-Martínez, C.; Canals, J.; Voltas, N.; Martín-Luján, F.; Arija, V. Circulating Levels of Short-Chain Fatty Acids during Pregnancy and Infant Neurodevelopment. Nutrients 2022, 14, 3946. [Google Scholar] [CrossRef]
- Kimber-Trojnar, Ż.; Marciniak, A.; Patro-Małysza, J.; Marciniak, B.; Mielnik-Niedzielska, G.; Leszczyńska-Gorzelak, B. Programowanie płodowe. Ginekol. I Perinatol. Prakt. 2018, 2, 58–63. [Google Scholar]
- Ziętek, M.; Celewicz, Z.; Szczuko, M. Short-Chain Fatty Acids, Maternal Microbiota and Metabolism in Pregnancy. Nutrients 2021, 13, 1244. [Google Scholar] [CrossRef]
- Saipudin, N.; Suhairom, N.; Abd Wahid, N. A Comparative Study on Faecal Short-Chain Fatty Acids Concen-tration in Lean, Overweight and Obese School Children. Asian J. Med. Biomed. 2022, 1, 77–83. [Google Scholar] [CrossRef]
- Martin-Gallausiau, C.; Marinelli, L.; Blottière, H.; Larraufie, P.; Lapaque, N. SCFA: Mechanisms and functional importance in the gut. Proc. Nutr. Soc. 2021, 80, 37–49. [Google Scholar] [CrossRef]
- Priyadarshini, M.; Thomas, A.; Alexandra, A.; Scholtens, D.; Wolever, T.; Josefson, A.; Layden, B.T. Maternal short-chain fatty acids are associated with metabolic parameters in mothers and newborns. Transl. Res. 2014, 164, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Szczuko, M.; Kikut, J.; Maciejewska, D.; Kulpa, D.; Celewicz, Z.; Ziętek, M. The Associations of SCFA with Anthropometric Parameters and Carbohydrate Metabolism in Pregnant Women. Int. J. Mol. Sci. 2020, 21, 9212. [Google Scholar] [CrossRef] [PubMed]
- Łoniewska, B.; Fraszczyk-Tousty, M.; Tousty, P.; Skonieczna-Żydecka, K.; Maciejewska-Markiewicz, D.; Łoniewski, I. Analysis of Fecal Short-Chain Fatty Acids (SCFAs) in Healthy Children during the First Two Years of Life: An Observational Prospective Cohort Study. Nutrients 2023, 15, 367. [Google Scholar] [CrossRef] [PubMed]
- Malinowska, A.; Majcher, M.; Hooiveld, G.; Przydatek, H.; Szaban, M.; Kurowiecka, A.; Schmidt, M. Experimental Capacity of Human Fecal Microbiota to Degrade Fiber and Produce Short-Chain Fatty Acids Is Associated with Diet Quality and Anthropometric Parameters. J. Nutr. 2023, 153, 2827–2841. [Google Scholar] [CrossRef]
- Yamamura, R.; Nakamura, K.; Ukawa, S.; Okada, E.; Nakagawa, T.; Imae, A.; Kunihiro, T.; Kimura, T.; Hirata, T.; Tamakoshi, A. Fecal short-chain fatty acids and obesity in a community-based Japanese population: The DOSANCO Health Study. Obes. Res. Clin. Pract. 2021, 15, 345–350. [Google Scholar] [CrossRef]
- Rios-Covian, D.; González, S.; Nogacka, A.; Arboleya, S.; Salazar, N.; Gueimonde, M.; de Los Reyes-Gavilán, C.G. An Overview on Fecal Branched Short-Chain Fatty Acids Along Human Life and as Related With Body Mass Index: Associated Dietary and Anthropometric Factors. Front. Microbiol. 2020, 11, 973. [Google Scholar] [CrossRef]
- Śliżewska, K.; Włodarczyk, M.; Sobczak, M.; Barczyńska, R.; Kapuśniak, J.; Socha, P.; Wierzbicka-Rucińska, A.; Kotowska, A. Comparison of the Activity of Fecal Enzymes and Concentration of SCFA in Healthy and Overweight Children. Nutrients 2023, 15, 987. [Google Scholar] [CrossRef]
- Ostrowska, J.; Samborowska, E.; Jaworski, M.; Toczyłowska, K.; Szostak-Węgierek, D. The Potential Role of SCFAs in Modulating Cardiometabolic Risk by Interacting with Adiposity Parameters and Diet. Nutrients 2024, 16, 266. [Google Scholar] [CrossRef]
- Chulenbayeva, L.; Issilbayeva, A.; Sailybayeva, A.; Bekbossynova, M.; Kozhakhmetov, S.; Kushugulova, A. Short-Chain Fatty Acids and Their Metabolic Interactions in Heart Failure. Biomedicines 2025, 13, 343. [Google Scholar] [CrossRef]
- Martindale, R.; Mundi, M.; Hurt, R.; McClave, S. Short-chain fatty acids in clinical practice: Where are we? Curr. Opin. Clin. Nutr. Metab. Care 2025, 28, 54–60. [Google Scholar] [CrossRef]

| Fatty Acids | AVG (mol/g Feces Dry Weight) | SD | Median | Standard Error |
|---|---|---|---|---|
| C2:0 | 55.02 | 7.329 | 55.755 | 1.105 |
| C3:0 | 10.375 | 2.125 | 10.692 | 0.32 |
| C4i | 4.974 | 1.212 | 5.065 | 0.183 |
| C4n | 4.473 | 2.13 | 3.947 | 0.321 |
| C5i | 3.128 | 0.931 | 2.926 | 0.14 |
| C5n | 1.156 | 1.781 | 0.467 | 0.268 |
| 3,4-methylovaleric | 1.318 | 1.51 | 0.747 | 0.228 |
| C6:0 | 18.52 | 4.416 | 19.196 | 0.666 |
| C7:0 | 1.037 | 1.396 | 0.471 | 0.21 |
| Pre-Delivery BW of Women | BW of Women at Delivery | Pre-Delivery BMI of Women | BMl of Women at Delivery | Gestational Weight Gain | Birth Weight | Apgar Score at 5 min | C2:0 | C3:0 | C4i | C4n | C5i | C5n | 3,4-Methylo valeric | C6:0 | C7:0 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-delivery BW of women | 1 | 0.940 | 0.962 | 0.962 | −0.156 | −0.232 | −0.087 | −0.202 | 0.127 | 0.076 | −0.034 | 0.034 | 0.105 | 0.100 | 0.141 | 0.143 |
| BW of women at delivery | 0.940 | 1 | 0.921 | 0.959 | 0.165 | −0.171 | −0.127 | −0.107 | 0.119 | 0.028 | −0.051 | −0.063 | 0.048 | 0.033 | 0.094 | 0.080 |
| Pre-delivery BMI of women | 0.962 | 0.921 | 1 | 0.942 | −0.049 | −0.174 | −0.114 | −0.166 | 0.100 | 0.079 | −0.048 | 0.041 | 0.072 | 0.068 | 0.131 | 0.131 |
| BMI of women at delivery | 0.962 | 0.959 | 0.942 | 1 | 0.212 | −0.212 | −0.131 | −0.066 | 0.107 | 0.036 | −0.073 | −0.041 | 0.018 | 0.003 | 0.068 | 0.052 |
| Gestational weight gain | −0.156 | 0.165 | −0.049 | 0.212 | 1 | 0.203 | −0.050 | 0.240 | −0.072 | −0.036 | −0.063 | −0.259 | −0.173 | −0.200 | −0.078 | −0.169 |
| Birth weight | −0.232 | −0.171 | −0.174 | −0.212 | 0.203 | 1 | 0.021 | 0.193 | −0.071 | −0.145 | 0.151 | −0.240 | −0.067 | −0.142 | −0.153 | −0.126 |
| Apgar score at 5 min | −0.087 | −0.127 | −0.114 | −0.131 | −0.050 | 0.021 | 1 | −0.034 | 0.083 | 0.085 | 0.135 | 0.113 | 0.012 | −0.029 | −0.073 | −0.058 |
| C2:0 | −0.202 | −0.107 | −0.166 | −0.066 | 0.240 | 0.193 | −0.034 | 1 | −0.071 | −0.702 | −0.083 | −0.605 | −0.718 | −0.751 | −0486 | +0.737 |
| C3:0 | 0.127 | 0.119 | 0.100 | 0.107 | −0.072 | −0.071 | 0.083 | −0.071 | 1 | 0.073 | −0.576 | −0.023 | −0.299 | −0.266 | 0.215 | −0.328 |
| C4i | 0.076 | 0.028 | 0.079 | 0.036 | −0.036 | −0.145 | 0.085 | −0.702 | 0.073 | 1 | −0.214 | 0.130 | 0.225 | 0.269 | 0.672 | 0.245 |
| C4n | −0.034 | −0.051 | −0.048 | −0.073 | −0.063 | 0.151 | 0.135 | −0.083 | −0.576 | −0.214 | 1 | 0.254 | 0.516 | 0.480 | −0.590 | 0.488 |
| C5i | 0.034 | −0.063 | 0.041 | −0.041 | −0.259 | −0.240 | 0.113 | −0.605 | −0.023 | 0.130 | 0.254 | 1 | 0.757 | 0.797 | −0.166 | 0.741 |
| C5n | 0.105 | 0.048 | 0.072 | 0.018 | −0.173 | −0.067 | 0.012 | −0.718 | −0.299 | 0.225 | 0.516 | 0.757 | 1 | 0.974 | −0.182 | 0.982 |
| 3,4-methylovaleric | 0.100 | 0.033 | 0.068 | 0.003 | −0.200 | −0.142 | −0.029 | −0.751 | −0.266 | 0.269 | 0.480 | 0.797 | 0.974 | 1 | −0.143 | 0.979 |
| C6:0 | 0.141 | 0.094 | 0.131 | 0.068 | −0.078 | −0.153 | −0.073 | −0.486 | 0.215 | 0.672 | −0.590 | −0.166 | −0.182 | −0.143 | 1 | −0.124 |
| C7:0 | 0.143 | 0.080 | 0.131 | 0.052 | −0.169 | −0.126 | −0.058 | −0.737 | −0.328 | 0.245 | 0.488 | 0.741 | 0.982 | 0.979 | −0.124 | 1 |
| C2:0 | C3:0 | C4i | C4n | C5i | C5n | 3,4-Methylvaleric | C6:0 | C7:0 | |
|---|---|---|---|---|---|---|---|---|---|
| Pre-delivery BW of women | p = 5.95 | p = 2.39 | p = 9.91 | p = 1.18 | p = 3.60 | p = 9.39 | p = 1.06 | p = 6.71 | p = 8.03 |
| BW of women at delivery | p = 1.71 | p = 6.69 | p = 5.05 | p = 6.25 | p = 2.29 | p = 7.11 | p = 7.90 | p = 1.27 | p = 5.89 |
| Pre-delivery BMI of women | p = 7.29 | p = 8.39 | p = 6.62 | p = 6.56 | p = 6.11 | p = 5.56 | p = 5.60 | p = 1.19 | p = 5.51 |
| BMI of women at delivery | p = 4.02 | p = 3.31 | p = 1.62 | p = 8.82 | p = 1.13 | p = 1.20 | p = 1.18 | p = 6.98 | p = 4.51 |
| Gestational weight gain | p = 3.77 | p = 0.006 p < 0.05 | p = 1.95 | p = 1.19 | p = 2.18 | p = 3.18 | p = 3.76 | p = 0.001 p < 0.05 | p = 1.37 |
| Birth weight | p = 7.71 | p = 5.06 | p = 4.72 | p = 4.42 | p = 4.63 | p = 4.46 | p = 4.52 | p = 6.03 | p = 4.48 |
| Apgar score at 5 min | p = 5.51 | p = 0.06 | p = 1.22 | p = 4.27 | p = 2.31 | p = 1.09 | p = 1.09 | p = 2.11 | p = 2.69 |
| Breastfeeding | p = 2.48 | p = 3.04 | p = 4.45 | p = 6.27 | p = 8.55 | p = 0.5 | p = 0.15 | p = 3.79 | p = 0.78 |
| Supplementary feeding | p = 2.34 | p = 1.66 | p = 3.67 | p = 5.02 | p = 8.03 | p = 0.02 p < 0.05 | p = 0.002 p < 0.05 | p = 2.16 | p = 0.03 p < 0.05 |
| Parameters | AVG | SD | Median | Min–Max |
|---|---|---|---|---|
| Age [years] | 31.17 | 4.49 | 30.5 | 22–40 |
| Weight before delivery [kg] | 68.28 | 17.59 | 65 | 40–126 |
| Weight at birth [kg] | 82.19 | 16.55 | 80 | 52–142 |
| BMI before delivery [kg/m2] | 24.56 | 6.05 | 22.73 | 15.94–48.01 |
| BMI at delivery [kg/m2] | 29.57 | 5.62 | 28.4 | 19.84–54.11 |
| Weight gain [kg] | 14.24 | 7.01 | 13 | −2–37 |
| Weight at birth [g] | 3286.34 | 394.79 | 3285 | 2090–4390 |
| Apgar score at 5 min. | 9.78 | 0.0576 | 10 | 7–10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szczuko, M.; Szabunia, N.; Radkiewicz, J.; Jamioł-Milc, D.; Machałowski, T.; Ziętek, M. Relationship of SCFAs to Maternal and Child Anthropometric Measurements. Int. J. Mol. Sci. 2025, 26, 6424. https://doi.org/10.3390/ijms26136424
Szczuko M, Szabunia N, Radkiewicz J, Jamioł-Milc D, Machałowski T, Ziętek M. Relationship of SCFAs to Maternal and Child Anthropometric Measurements. International Journal of Molecular Sciences. 2025; 26(13):6424. https://doi.org/10.3390/ijms26136424
Chicago/Turabian StyleSzczuko, Małgorzata, Natalia Szabunia, Julia Radkiewicz, Dominika Jamioł-Milc, Tomasz Machałowski, and Maciej Ziętek. 2025. "Relationship of SCFAs to Maternal and Child Anthropometric Measurements" International Journal of Molecular Sciences 26, no. 13: 6424. https://doi.org/10.3390/ijms26136424
APA StyleSzczuko, M., Szabunia, N., Radkiewicz, J., Jamioł-Milc, D., Machałowski, T., & Ziętek, M. (2025). Relationship of SCFAs to Maternal and Child Anthropometric Measurements. International Journal of Molecular Sciences, 26(13), 6424. https://doi.org/10.3390/ijms26136424






