Exploring the Potential of Oral Butyrate Supplementation in Metabolic Dysfunction-Associated Steatotic Liver Disease: Subgroup Insights from an Interventional Study
Abstract
1. Introduction
2. Results
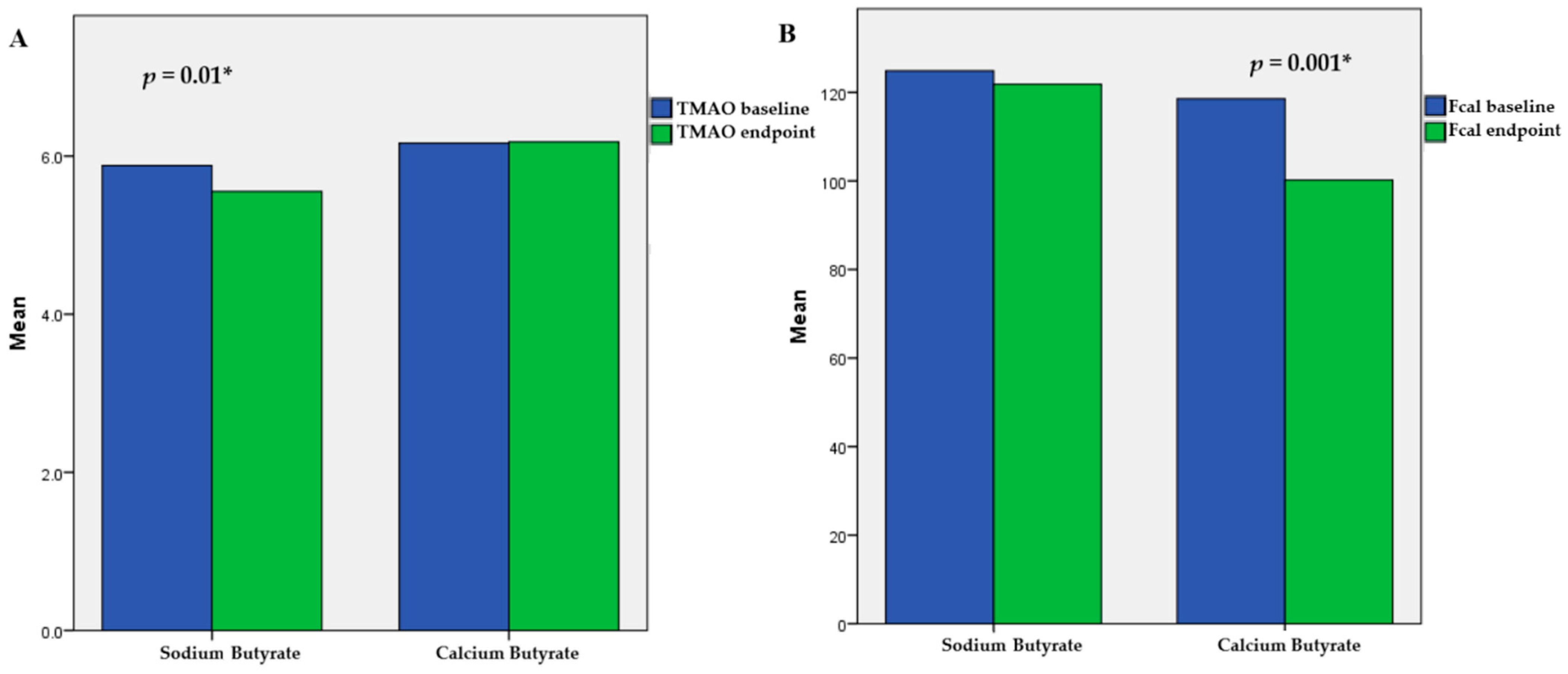
2.1. Mixed-Effects Model Results
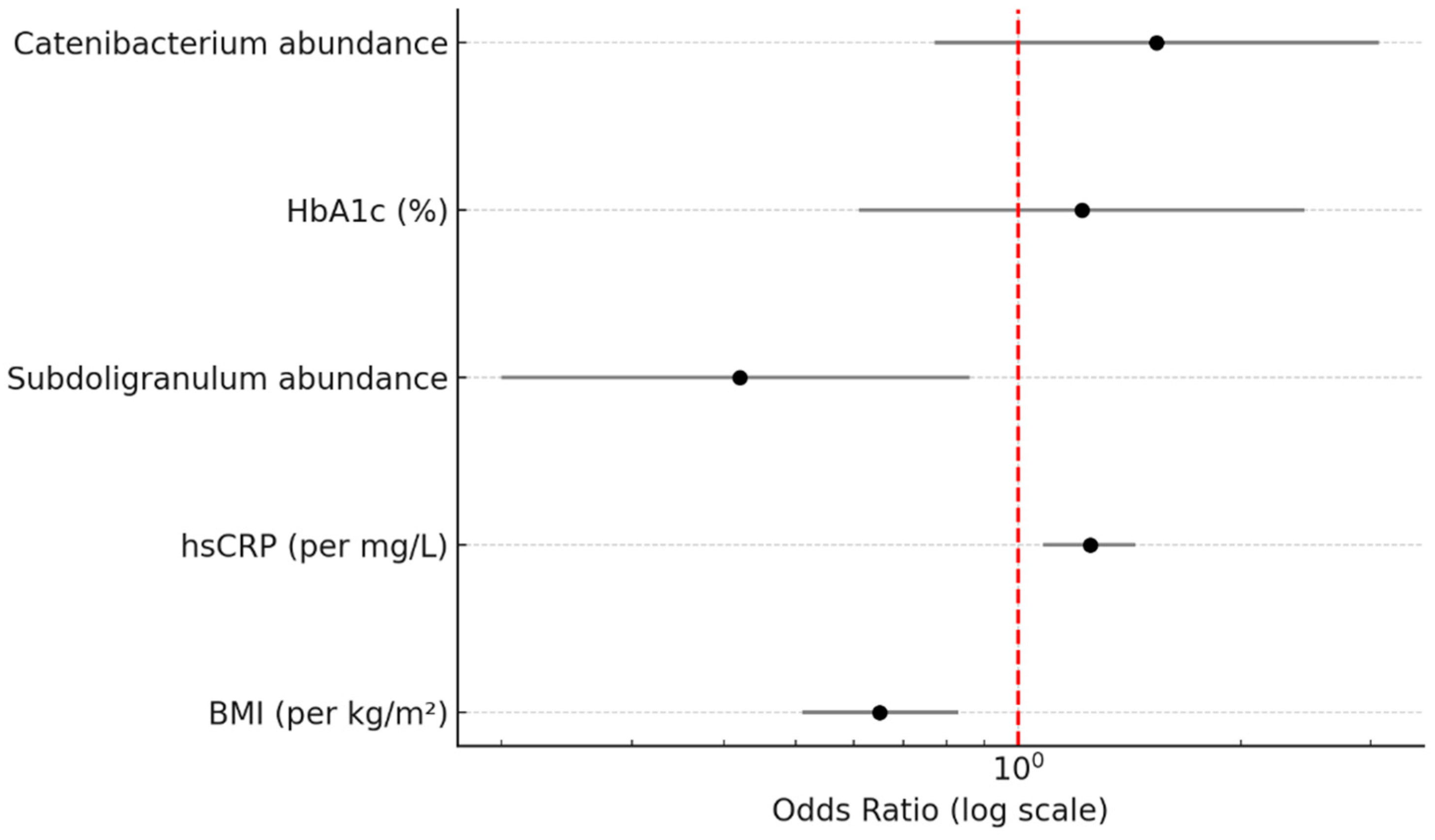
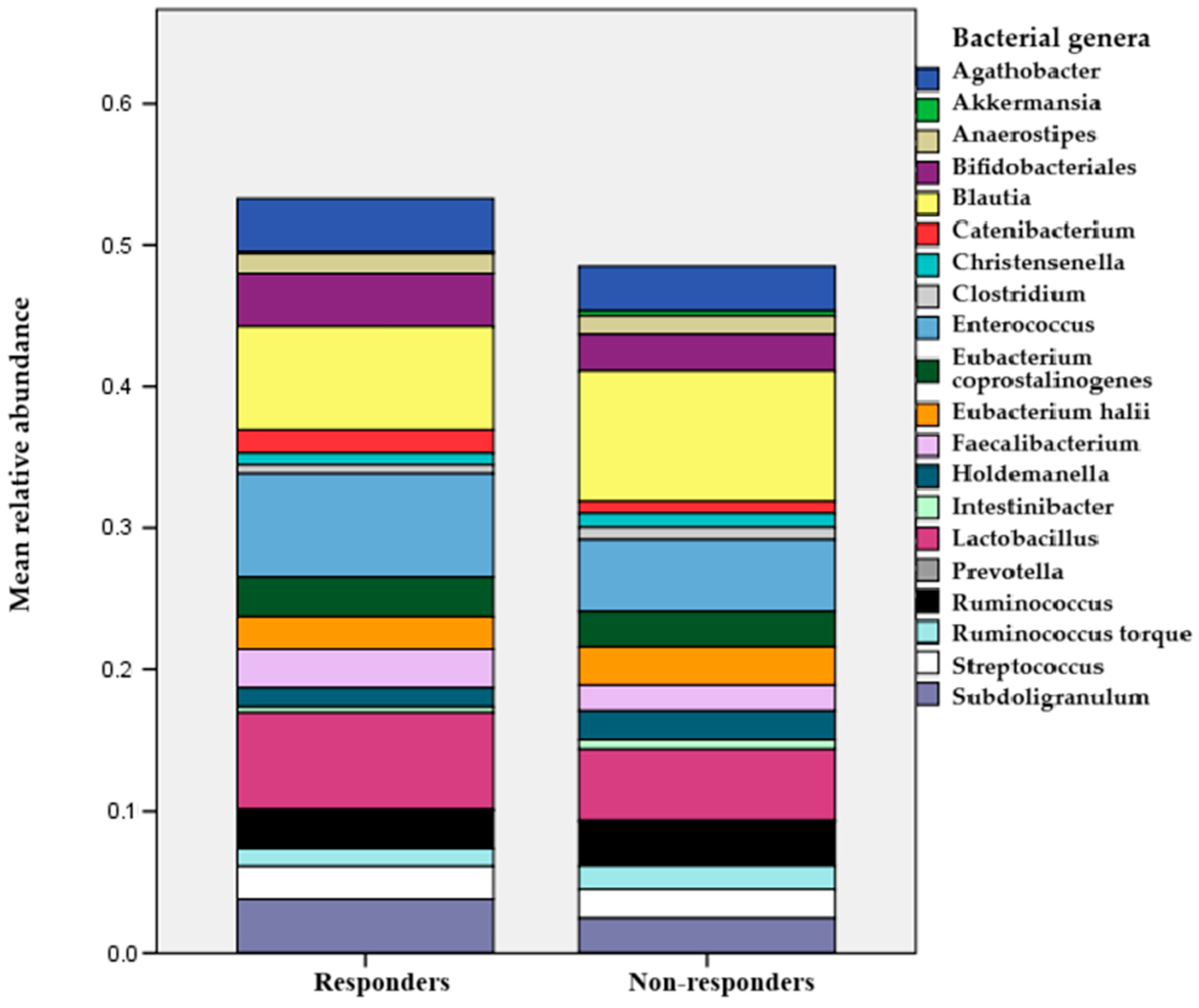
2.2. Insights from Subgroup Analysis
3. Discussion
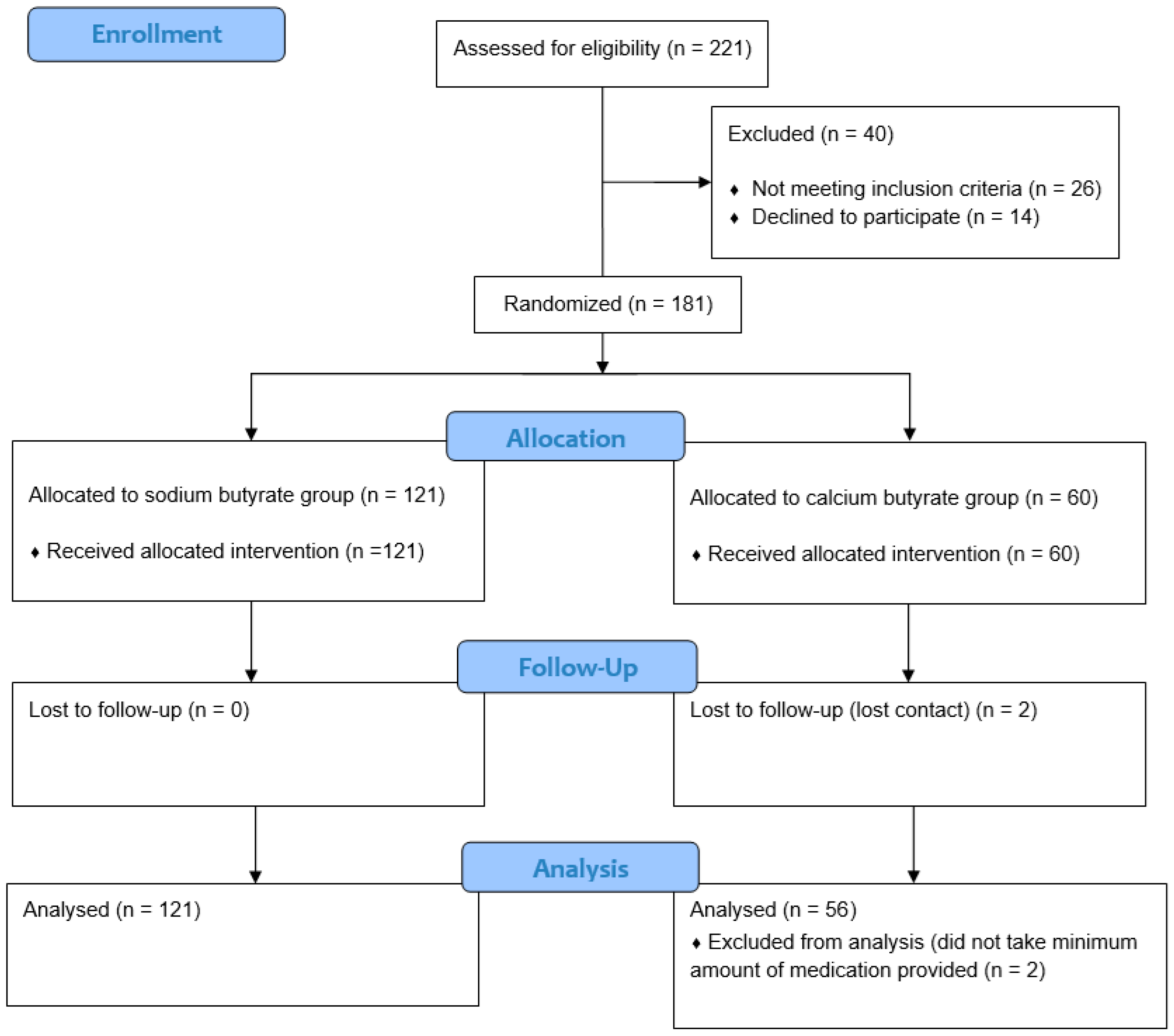
4. Materials and Methods
4.1. Intervention
4.2. Assessment
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
Appendix A
| Parameter | Sodium Butyrate | Calcium Butyrate | p |
|---|---|---|---|
| N | 121 | 56 | - |
| Δ ALT (U/L) | −0.3 ± 9.7 | −0.2 ± 9.4 | 0.95 |
| Δ AST (U/L) | 0.6 ± 8.6 | 0.8 ± 7.1 | 0.88 |
| Δ GGT (U/L) | −0.3 ± 6.3 | 0.6 ± 6.4 | 0.34 |
| Δ hsCRP (mg/L) | 0.5 ± 2.1 | 0.8 ± 2.4 | 0.36 |
| Δ Interleukin 6 (pg/mL) | 1.5 ± 9.6 | 0.8 ± 10.8 | 0.68 |
| Δ CK18F (U/L) | 1.3 ± 22.4 | −5.5 ± 22.8 | 0.065 |
| Δ TMAO (μmol/L) | 10 ± 6 | 0.1 ± 1.3 | 0.001 |
| Δ Fecal Calprotectin (μg/g) | 3 ± 26.6 | 9 ± 31.9 | 0.16 |
| Δ CAP (dB/m) | 2 ± 11.8 | 0.2 ± 18.1 | 0.42 |
| Δ LSM (kPA) | −0.09 ± 0.6 | 0.2 ± 0.6 | 0.22 |
| Δ HSI | 0 ± 1.33 | 0.1 ± 1.2 | 0.61 |
| Δ FLI | −4.1 ± 12.3 | 0.5 ± 15.8 | 0.036 |
| Δ FIB−4 | 0.02 ± 0.06 | 0.023 ± 0.04 | 0.81 |
| ΔNFS | 0.015 ± 0.03 | 0.016 ± 0.04 | 0.88 |
| Outcome Variable | Estimate | Std. Error | 95% CI | p-Value |
|---|---|---|---|---|
| CAP (dB/m) | −0.95 | 1.21 | [−3.30, 1.40] | 0.680 |
| LSM (kPa) | −0.20 | 0.34 | [−0.90, 0.50] | 0.550 |
| TMAO (μmol/L) | −1.32 | 0.52 | [−2.35, −0.29] | * 0.021 |
| Fecal Calprotectin (μg/g) | −18.90 | 8.60 | [−35.70, −2.10] | * 0.031 |
| HIS | −0.05 | 0.11 | [−0.27, 0.17] | 0.610 |
| FLI | −2.35 | 1.16 | [−4.62, −0.08] | * 0.047 |
| FIB-4 | −0.004 | 0.033 | [−0.068, 0.06] | 0.9 |
| NFS | 0.015 | 0.067 | [−0.117, 0.148] | 0.82 |
| Family/Genera | β-Coefficient | Raw p | FDR-Adjusted p |
|---|---|---|---|
| Enterococcaceae | −37.023 | 0.01 | 0.278 |
| Veillonellaceae | 300.079 | 0.104 | 0.739 |
| Coriobacteriaceae | 199.65 | 0.109 | 0.739 |
| Enterobacteriaceae | 224.791 | 0.245 | 0.742 |
| Prevotellaceae | 136.228 | 0.302 | 0.742 |
| Bacteroidaceae | 151.436 | 0.42 | 0.81 |
| Streptococcaceae | 17.595 | 0.636 | 0.959 |
| Lachnospiraceae | 6.783 | 0.639 | 0.959 |
| Bifidobacteriaceae | 11.13 | 0.824 | 0.99 |
| Ruminococcaceae | −0.737 | 0.97 | 0.99 |
| Lactobacillaceae | −0.582 | 0.974 | 0.99 |
| Enterococcus | −31.042 | 0.063 | 0.739 |
| Blautia | 31.603 | 0.243 | 0.742 |
| Ruminicoccus | 53.649 | 0.287 | 0.742 |
| Catenibacterium | −49.063 | 0.29 | 0.742 |
| Subdoligranum | 35.249 | 0.511 | 0.862 |
| Streptococcus | 14.144 | 0.706 | 0.99 |
| Holdemanella | 8.714 | 0.856 | 0.99 |
| Ruminicoccus T | 4.436 | 0.963 | 0.99 |
| Faecalibacterium | 2.45 | 0.966 | 0.99 |
| Lactobacillus | −0.582 | 0.974 | 0.99 |
Appendix B
Stool Microbiome Determination Details
References
- Le, M.H.; Yeo, Y.H.; Li, X.; Li, J.; Zou, B.; Wu, Y.; Ye, Q.; Huang, D.Q.; Zhao, C.; Zhang, J.; et al. 2019 Global NAFLD prevalence: A systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2022, 20, 2809–2817. [Google Scholar] [CrossRef] [PubMed]
- Targher, G.; Byrne, C.D.; Tilg, H. MASLD: A systemic metabolic disorder with cardiovascular and malignant complications. Gut 2024, 73, 691–702. [Google Scholar] [CrossRef] [PubMed]
- Schwärzler, J.; Grabherr, F.; Grander, C.; Adolph, T.E.; Tilg, H. The pathophysiology of MASLD: An immunometabolic perspective. Expert Rev. Clin. Immunol. 2024, 20, 375–386. [Google Scholar] [CrossRef]
- Vallianou, N.G.; Kounatidis, D.; Psallida, S.; Vythoulkas-Biotis, N.; Adamou, A.; Zachariadou, T.; Kargioti, S.; Karampela, I.; Dalamaga, M. NAFLD/MASLD and the Gut-Liver Axis: From Pathogenesis to Treatment Options. Metabolites 2024, 14, 366. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Hong, J.; Wang, Y.; Pei, M.; Wang, L.; Gong, Z. Trimethylamine-N-Oxide Pathway: A Potential Target for the Treatment of MAFLD. Front. Mol. Biosci. 2021, 8, 733507. [Google Scholar] [CrossRef] [PubMed]
- Amiri, P.; Arefhosseini, S.; Bakhshimoghaddam, F.; Jamshidi Gurvan, H.; Hosseini, S.A. Mechanistic insights into the pleiotropic effects of butyrate as a potential therapeutic agent on NAFLD management: A systematic review. Front. Nutr. 2022, 9, 1037696. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fusco, W.; Lorenzo, M.B.; Cintoni, M.; Porcari, S.; Rinninella, E.; Kaitsas, F.; Lener, E.; Mele, M.C.; Gasbarrini, A.; Collado, M.C.; et al. Short-Chain Fatty-Acid-Producing Bacteria: Key Components of the Human Gut Microbiota. Nutrients 2023, 15, 2211. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yan, H.; Ajuwon, K.M. Butyrate modifies intestinal barrier function in IPEC-J2 cells through a selective upregulation of tight junction proteins and activation of the Akt signaling pathway. PLoS ONE 2017, 12, e0179586. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhao, Z.H.; Wang, Z.X.; Zhou, D.; Han, Y.; Ma, F.; Hu, Z.; Xin, F.Z.; Liu, X.L.; Ren, T.Y.; Zhang, F.; et al. Sodium Butyrate Supplementation Inhibits Hepatic Steatosis by Stimulating Liver Kinase B1 and Insulin-Induced Gene. Cell. Mol. Gastroenterol. Hepatol. 2021, 12, 857–871. [Google Scholar] [CrossRef]
- Li, Y.; Xu, S.; Mihaylova, M.M.; Zheng, B.; Hou, X.; Jiang, B.; Park, O.; Luo, Z.; Lefai, E.; Shyy, J.Y.; et al. AMPK phosphorylates and inhibits SREBP activity to attenuate hepatic steatosis and atherosclerosis in diet-induced insulin-resistant mice. Cell Metab. 2011, 13, 376–388. [Google Scholar] [CrossRef]
- Zhou, D.; Chen, Y.W.; Zhao, Z.H.; Yang, R.X.; Xin, F.Z.; Liu, X.L.; Pan, Q.; Zhou, H.; Fan, J.G. Sodium butyrate reduces high-fat diet-induced non-alcoholic steatohepatitis through upregulation of hepatic GLP-1R expression. Exp. Mol. Med. 2018, 50, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Pant, K.; Yadav, A.K.; Gupta, P.; Islam, R.; Saraya, A.; Venugopal, S.K. Butyrate induces ROS-mediated apoptosis by modulating miR-22/SIRT-1 pathway in hepatic cancer cells. Redox Biol. 2017, 12, 340–349. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fogacci, F.; Giovannini, M.; Di Micoli, V.; Grandi, E.; Borghi, C.; Cicero, A.F.G. Effect of Supplementation of a Butyrate-Based Formula in Individuals with Liver Steatosis and Metabolic Syndrome: A Randomized Double-Blind Placebo-Controlled Clinical Trial. Nutrients 2024, 16, 2454. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, D.; Kim, H.J.; Lee, C.H.; Yang, J.I.; Kim, W.; Kim, Y.J.; Yoon, J.H.; Cho, S.H.; Sung, M.W.; et al. Hepatic steatosis index: A simple screening tool reflecting nonalcoholic fatty liver disease. Dig. Liver Dis. 2010, 42, 503–508. [Google Scholar] [CrossRef]
- Bedogni, G.; Bellentani, S.; Miglioli, L.; Masutti, F.; Passalacqua, M.; Castiglione, A.; Tiribelli, C. The Fatty Liver Index: A simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006, 6, 33. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Grau, A.; Gabriel-Medina, P.; Rodriguez-Algarra, F.; Villena, Y.; Lopez-Martínez, R.; Augustín, S.; Pons, M.; Cruz, L.M.; Rando-Segura, A.; Enfedaque, B.; et al. Assessing Liver Fibrosis Using the FIB4 Index in the Community Setting. Diagnostics 2021, 11, 2236. [Google Scholar] [CrossRef]
- Treeprasertsuk, S.; Björnsson, E.; Enders, F.; Suwanwalaikorn, S.; Lindor, K.D. NAFLD fibrosis score: A prognostic predictor for mortality and liver complications among NAFLD patients. World J. Gastroenterol. 2013, 19, 1219–1229. [Google Scholar] [CrossRef]
- Biciusca, T.; Stan, S.I.; Balteanu, M.A.; Cioboata, R.; Ghenea, A.E.; Danoiu, S.; Bumbea, A.M.; Biciusca, V. The Role of the Fatty Liver Index (FLI) in the Management of Non-Alcoholic Fatty Liver Disease: A Systematic Review. Diagnostics 2023, 13, 3316. [Google Scholar] [CrossRef]
- Kim, B.S.; Kim, H.J.; Jeon, S.W.; Kim, K.H.; Kim, D.W.; Shin, J.H. Comparing non-alcoholic fatty liver disease indices in predicting the prevalence and incidence of metabolic syndrome in middle-aged adults. Heliyon 2025, 7, e43073. [Google Scholar] [CrossRef]
- Stefanakis, K.; Mingrone, G.; George, J.; Mantzoros, C.S. Accurate non-invasive detection of MASH with fibrosis F2-F3 using a lightweight machine learning model with minimal clinical and metabolomic variables. Metabolism 2025, 163, 156082. [Google Scholar] [CrossRef]
- Mózes, F.E.; Lee, J.A.; Vali, Y.; Alzoubi, O.; Staufer, K.; Trauner, M.; Paternostro, R.; Stauber, R.E.; Holleboom, A.G.; van Dijk, A.M.; et al. Performance of non-invasive tests and histology for the prediction of clinical outcomes in patients with non-alcoholic fatty liver disease: An individual participant data meta-analysis. Lancet Gastroenterol. Hepatol. 2023, 8, 704–713. [Google Scholar] [CrossRef] [PubMed]
- Jaworska, K.; Kopacz, W.; Koper, M.; Ufnal, M. Microbiome-Derived Trimethylamine N-Oxide (TMAO) as a Multifaceted Biomarker in Cardiovascular Disease: Challenges and Opportunities. Int. J. Mol. Sci. 2024, 25, 12511. [Google Scholar] [CrossRef] [PubMed]
- Eyileten, C.; Jarosz-Popek, J.; Jakubik, D.; Gasecka, A.; Wolska, M.; Ufnal, M.; Postula, M.; Toma, A.; Lang, I.M.; Siller-Matula, J.M. Plasma Trimethylamine-N-Oxide Is an Independent Predictor of Long-Term Cardiovascular Mortality in Patients Undergoing Percutaneous Coronary Intervention for Acute Coronary Syndrome. Front. Cardiovasc. Med. 2021, 8, 728724. [Google Scholar] [CrossRef]
- Ferslew, B.C.; Xie, G.; Johnston, C.K.; Su, M.; Stewart, P.W.; Jia, W.; Brouwer, K.L.; Barritt, A.S., IV. Altered Bile Acid Metabolome in Patients with Nonalcoholic Steatohepatitis. Dig. Dis. Sci. 2015, 60, 3318–3328. [Google Scholar] [CrossRef] [PubMed]
- Calderón-Pérez, L.; Gosalbes, M.J.; Yuste, S.; Valls, R.M.; Pedret, A.; Llauradó, E.; Jimenez-Hernandez, N.; Artacho, A.; Pla-Pagà, L.; Companys, J.; et al. Gut metagenomic and short chain fatty acids signature in hypertension: A cross-sectional study. Sci. Rep. 2020, 10, 6436. [Google Scholar] [CrossRef]
- Jukic, A.; Bakiri, L.; Wagner, E.F.; Tilg, H.; Adolph, T.E. Calprotectin: From biomarker to biological function. Gut 2021, 70, 1978–1988. [Google Scholar] [CrossRef]
- Heinzel, S.; Jureczek, J.; Kainulainen, V.; Nieminen, A.I.; Suenkel, U.; von Thaler, A.K.; Kaleta, C.; Eschweiler, G.W.; Brockmann, K.; Aho, V.T.E.; et al. Elevated fecal calprotectin is associated with gut microbial dysbiosis, altered serum markers and clinical outcomes in older individuals. Sci. Rep. 2024, 14, 13513. [Google Scholar] [CrossRef]
- Firoozi, D.; Masoumi, S.J.; Mohammad-Kazem Hosseini Asl, S.; Labbe, A.; Razeghian-Jahromi, I.; Fararouei, M.; Lankarani, K.B.; Dara, M. Effects of short-chain fatty acid-butyrate supplementation on expression of circadian-clock genes, sleep quality, and inflammation in patients with active ulcerative colitis: A double-blind randomized controlled trial. Lipids Health Dis. 2024, 23, 216. [Google Scholar] [CrossRef]
- Tougaard, N.H.; Frimodt-Møller, M.; Salmenkari, H.; Stougaard, E.B.; Zawadzki, A.D.; Mattila, I.M.; Hansen, T.W.; Legido-Quigley, C.; Hörkkö, S.; Forsblom, C.; et al. Effects of Butyrate Supplementation on Inflammation and Kidney Parameters in Type 1 Diabetes: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Clin. Med. 2022, 11, 3573. [Google Scholar] [CrossRef]
- Smith, D.J.; Barri, A.; Herges, G.; Hahn, J.; Yersin, A.G.; Jourdan, A. In Vitro Dissolution and in Vivo Absorption of Calcium [1-14C] Butyrate in Free or Protected Forms. J. Agric. Food Chem. 2012, 60, 3151–3157. [Google Scholar] [CrossRef]
- Njei, B.; Ameyaw, P.; Al-Ajlouni, Y.; Njei, L.P.; Boateng, S. Diagnosis and Management of Lean Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A Systematic Review. Cureus 2024, 16, e71451. [Google Scholar] [CrossRef]
- Freeman, A.M.; Acevedo, L.A.; Pennings, N. Insulin Resistance. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Steffl, M.; Bohannon, R.W.; Sontakova, L.; Tufano, J.J.; Shiells, K.; Holmerova, I. Relationship between sarcopenia and physical activity in older people: A systematic review and meta-analysis. Clin. Interv. Aging 2017, 12, 835–845. [Google Scholar] [CrossRef] [PubMed]
- Premkumar, M.; Anand, A.C. Lean Fatty Liver Disease: Through Thick and Thin. J. Clin. Exp. Hepatol. 2021, 11, 523–527. [Google Scholar] [CrossRef]
- Lee, Y.H.; Kim, S.U.; Song, K.; Park, J.Y.; Kim, D.Y.; Ahn, S.H.; Lee, B.W.; Kang, E.S.; Cha, B.S.; Han, K.H. Sarcopenia is associated with significant liver fibrosis independently of obesity and insulin resistance in nonalcoholic fatty liver disease: Nationwide surveys (KNHANES 2008–2011). Hepatology 2016, 63, 776–786. [Google Scholar] [CrossRef] [PubMed]
- Crişan, D.; Avram, L.; Morariu-Barb, A.; Grapa, C.; Hirişcau, I.; Crăciun, R.; Donca, V.; Nemeş, A. Sarcopenia in MASLD-Eat to Beat Steatosis, Move to Prove Strength. Nutrients 2025, 17, 178. [Google Scholar] [CrossRef]
- Saijo, Y.; Kiyota, N.; Kawasaki, Y.; Miyazaki, Y.; Kashimura, J.; Fukuda, M.; Kishi, R. Relationship between C-reactive protein and visceral adipose tissue in healthy Japanese subjects. Diabetes Obes. Metab. 2004, 6, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Van Hul, M.; Le Roy, T.; Prifti, E.; Dao, M.C.; Paquot, A.; Zucker, J.D.; Delzenne, N.M.; Muccioli, G.; Clément, K.; Cani, P.D. From correlation to causality: The case of Subdoligranulum. Gut Microbes 2020, 12, 1–13. [Google Scholar] [CrossRef]
- Van Immerseel, F.; Ducatelle, R.; De Vos, M.; Boon, N.; Van De Wiele, T.; Verbeke, K.; Rutgeerts, P.; Sas, B.; Louis, P.; Flint, H.J. Butyric acid-producing anaerobic bacteria as a novel probiotic treatment approach for inflammatory bowel disease. J. Med. Microbiol. 2010, 59 Pt 2, 141–143. [Google Scholar] [CrossRef]
- Leclercq, S.; Matamoros, S.; Cani, P.D.; Neyrinck, A.M.; Jamar, F.; Stärkel, P.; Windey, K.; Tremaroli, V.; Bäckhed, F.; Verbeke, K.; et al. Intestinal permeability, gut-bacterial dysbiosis, and behavioral markers of alcohol-dependence severity. Proc. Natl. Acad. Sci. USA 2014, 111, E4485–E4493. [Google Scholar] [CrossRef]
- Louis, S.; Tappu, R.M.; Damms-Machado, A.; Huson, D.H.; Bischoff, S.C. Characterization of the Gut Microbial Community of Obese Patients Following a Weight-Loss Intervention Using Whole Metagenome Shotgun Sequencing. PLoS ONE 2016, 11, e0149564. [Google Scholar] [CrossRef]
- Zhang, X.; Fang, Z.; Zhang, C.; Xia, H.; Jie, Z.; Han, X.; Chen, Y.; Ji, L. Effects of Acarbose on the Gut Microbiota of Prediabetic Patients: A Randomized, Double-blind, Controlled Crossover Trial. Diabetes Ther. 2017, 8, 293–307. [Google Scholar] [CrossRef]
- Lee, C.B.; Chae, S.U.; Jo, S.J.; Jerng, U.M.; Bae, S.K. The Relationship between the Gut Microbiome and Metformin as a Key for Treating Type 2 Diabetes Mellitus. Int. J. Mol. Sci. 2021, 22, 3566. [Google Scholar] [CrossRef] [PubMed]
- Cui, G.; Li, S.; Ye, H.; Yang, Y.; Jia, X.; Lin, M.; Chu, Y.; Feng, Y.; Wang, Z.; Shi, Z.; et al. Gut microbiome and frailty: Insight from genetic correlation and mendelian randomization. Gut Microbes 2023, 15, 2282795. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Matute, P.; Íñiguez, M.; Villanueva-Millán, M.J.; Oteo, J.A. Chapter 32—The oral, genital and gut microbiome in HIV infection. In Microbiome and Metabolome in Diagnosis, Therapy, and other Strategic Applications; Academic Press: Cambridge, MA, USA, 2019; pp. 307–323. [Google Scholar]
- Borges, N.A.; Mafra, D. The Gut Microbiome in Chronic Kidney Disease. In Microbiome and Metabolome in Diagnosis, Therapy, and Other Strategic Applications; Academic Press: Cambridge, MA, USA, 2018; pp. 349–356. [Google Scholar]
- da Silva, L.C.M.; de Oliveira, J.T.; Tochetto, S.; de Oliveira, C.P.M.S.; Sigrist, R.; Chammas, M.C. Ultrasound elastography in patients with fatty liver disease. Radiol. Bras. 2020, 53, 47–55. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ruggeri, S.; Buonocore, P.; Amoriello, T. New Validated Short Questionnaire for the Evaluation of the Adherence of Mediterranean Diet and Nutritional Sustainability in All Adult Population Groups. Nutrients 2022, 14, 5177. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Awwad, H.M.; Geisel, J.; Obeid, R. Determination of trimethylamine, trimethylamine N-oxide, and taurine in human plasma and urine by UHPLC-MS/MS technique. J. Chromatogr. B Analyt Technol. Biomed. Life Sci. 2016, 1038, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Scheppach, W.M.; Fabian, C.E.; Kasper, H.W. Fecal short-chain fatty acid (SCFA) analysis by capillary gas-liquid chromatography. Am. J. Clin. Nutr. 1987, 46, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Fiers, T.; Maes, V.; Sevens, C. Automation of toxicological screenings on a Hewlett Packard Chemstation GC-MS system. Clin. Biochem. 1996, 29, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Caporaso, J.G.; Lauber, C.L.; Walters, W.A.; Berg-Lyons, D.; Huntley, J.; Fierer, N.; Owens, S.M.; Betley, J.; Fraser, L.; Bauer, M.; et al. Ultra-high-throughput microbial community analysis on the Illumina HiSeq and MiSeq platforms. ISME J. 2012, 6, 1621–1624. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Edgar, R.C. UPARSE: Highly accurate OTU sequences from microbial amplicon reads. Nat. Methods 2013, 10, 996–998. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Garrity, G.M.; Tiedje, J.M.; Cole, J.R. Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl. Environ. Microbiol. 2007, 73, 5261–5267. [Google Scholar] [CrossRef] [PubMed]
- Quast, C.; Pruesse, E.; Yilmaz, P.; Gerken, J.; Schweer, T.; Yarza, P.; Peplies, J.; Glöckner, F.O. The SILVA ribosomal RNA gene database project: Improved data processing and web-based tools. Nucleic Acids Res. 2013, 41, D590–D596. [Google Scholar] [CrossRef]
- Murphy, D.F.; McDonald, A.; Power, C.; Unwin, A.; MacSullivan, R. Measurement of pain: A comparison of the visual analogue with a nonvisual analogue scale. Clin. J. Pain 1987, 3, 197–199. [Google Scholar] [CrossRef]
- Raosoft Software. Calculate Your Sample Size. Available online: http://www.raosoft.com/samplesize.html (accessed on 1 December 2023).
- Ferro, Y.; Montalcini, T.; Mazza, E.; Foti, D.; Angotti, E.; Gliozzi, M.; Nucera, S.; Paone, S.; Bombardelli, E.; Aversa, I.; et al. Randomized Clinical Trial: Bergamot Citrus and Wild Cardoon Reduce Liver Steatosis and Body Weight in Non-diabetic Individuals Aged Over 50 Years. Front. Endocrinol. 2020, 11, 494. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mitrović, M.; Dobrosavljević, A.; Odanović, O.; Knežević-Ivanovski, T.; Kralj, Đ.; Erceg, S.; Perućica, A.; Svorcan, P.; Stanković-Popović, V. The effects of synbiotics on the liver steatosis, inflammation, and gut microbiome of metabolic dysfunction-associated liver disease patients-randomized trial. Rom. J. Intern. Med. 2024, 62, 184–193. [Google Scholar] [CrossRef]
- Shimizu, M.; Suzuki, K.; Kato, K.; Jojima, T.; Iijima, T.; Murohisa, T.; Iijima, M.; Takekawa, H.; Usui, I.; Hiraishi, H.; et al. Evaluation of the effects of dapagliflozin, a sodium-glucose co-transporter-2 inhibitor, on hepatic steatosis and fibrosis using transient elastography in patients with type 2 diabetes and non-alcoholic fatty liver disease. Diabetes Obes. Metab. 2019, 21, 285–292. [Google Scholar] [CrossRef]
| Parameter | Sodium Butyrate | Calcium Butyrate | p |
|---|---|---|---|
| N | 121 | 56 | - |
| Gender (female) | 56 (46%) | 28 (50%) | 0.38 |
| Age | 51 ± 15 | 50 ± 16 | 0.68 |
| BMI | 27.8 ± 1.4 | 27.5 ± 1.8 | 0.19 |
| ALT (U/L) | 59 ± 10 | 61 ± 10 | 0.2 |
| AST (U/L) | 56 ± 11 | 57 ± 11 | 0.34 |
| GGT (U/L) | 70 ± 18 | 69 ± 19 | 0.9 |
| Total cholesterol (mg/dL) | 355 ± 18 | 351 ± 18 | 0.24 |
| Triglycerides (mg/dL) | 166 ± 38 | 167 ± 36 | 0.86 |
| HbA1c (%) | 6.5 ± 0.5 | 6.6 ± 0.5 | 0.09 |
| hsCRP (mg/L) | 3.2 (1.1–9.1) | 4 (1.1–9.2) | 0.9 |
| Interleukin 6 (pg/mL) | 42.2 ± 9.2 | 40.7 ± 8.5 | 0.31 |
| CK18F (U/L) | 248 ± 38 | 248 ± 32 | 0.93 |
| TMAO (μmol/L) | 4.3 ± 2 | 4 ± 2.1 | 0.4 |
| Stool SCFA (mmol/L) | 176 ± 36 | 167 ± 36 | 0.13 |
| Fecal Calprotectin (μg/g) | 100 (70–130) | 90 (70–120) | 0.23 |
| Baseline CAP (dB/m) | 290 ± 21 | 289 ± 19 | 0.82 |
| Baseline LSM (kPA) | 4.3 ± 2.4 | 4.9 ± 2.6 | 0.09 |
| Baseline HSI | 38 ± 2.6 | 37.1 ± 2.6 | 0.21 |
| Baseline FLI | 74.4 ± 4.5 | 75.2 ± 4.1 | 0.23 |
| Baseline FIB-4 | 1.49 (1.10–1.87) | 1.46 (1.05–1.82) | 0.76 |
| Baseline NFS | −1.13 (−1.95 to −0.32) | −1.21 (−2.02 to −0.40) | 0.82 |
| Parameter | Responder | Non-Responder | p |
|---|---|---|---|
| N | 30 | 147 | - |
| BMI | 26.1 ± 1.7 | 27.8 ± 1.7 | * 0.001 |
| ALT (U/L) | 60 ± 13 | 60 ± 9 | 0.87 |
| AST (U/L) | 57 ± 12 | 57 ± 11 | 0.74 |
| GGT (U/L) | 68 ± 20 | 71 ± 18 | 0.583 |
| Total cholesterol (mg/dL) | 350 ± 20 | 354 ± 17 | 0.27 |
| Triglycerides (mg/dL) | 166 ± 38 | 167 ± 36 | 0.54 |
| HbA1c (%) | 6.7 ± 0.4 | 6.4 ± 0.5 | * 0.037 |
| hsCRP (mg/L) | 7.7 (6–9.6) | 4.2 (4–5.6) | * 0.002 |
| Interleukin 6 (pg/mL) | 41 ± 8 | 42 ± 9 | 0.47 |
| CK18F (U/L) | 247 ± 30 | 248 ± 37 | 0.8 |
| TMAO (μmol/L) | 3.9 ± 2.4 | 4.2 ± 1.9 | 0.42 |
| Stool SCFA (mmol/L) | 176 ± 36 | 174 ± 37 | 0.24 |
| Fecal Calprotectin (μg/g) | 140 ± 90 | 120 ± 80 | 0.3 |
| Baseline CAP (dB/m) | 295 ± 19 | 288 ± 21 | 0.1 |
| Baseline LSM (kPA) | 5 ± 2.5 | 4.4 ± 2.5 | 0.18 |
| Baseline HSI | 37.5 ± 2.6 | 36.5 ± 2.6 | 0.137 |
| Baseline FLI | 74.5 ± 4.5 | 75 ± 4.0 | 0.62 |
| Baseline FIB-4 | 1.51 (1.05–1.76) | 1.49 (1.1–1.87) | 0.93 |
| Baseline NFS | −1.17 (−1.97 to −0.4) | −1.11 (−2.01 to −0.37) | 0.24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitrović, M.; Stanković Popović, V.; Erceg, S.; Perišić Mitrović, M.; Dobrosavljević, A.; Stupar, A.; Vuković, P.; Zlatković, D.; Svorcan, P. Exploring the Potential of Oral Butyrate Supplementation in Metabolic Dysfunction-Associated Steatotic Liver Disease: Subgroup Insights from an Interventional Study. Int. J. Mol. Sci. 2025, 26, 5561. https://doi.org/10.3390/ijms26125561
Mitrović M, Stanković Popović V, Erceg S, Perišić Mitrović M, Dobrosavljević A, Stupar A, Vuković P, Zlatković D, Svorcan P. Exploring the Potential of Oral Butyrate Supplementation in Metabolic Dysfunction-Associated Steatotic Liver Disease: Subgroup Insights from an Interventional Study. International Journal of Molecular Sciences. 2025; 26(12):5561. https://doi.org/10.3390/ijms26125561
Chicago/Turabian StyleMitrović, Miloš, Verica Stanković Popović, Sanja Erceg, Milena Perišić Mitrović, Ana Dobrosavljević, Andrej Stupar, Petra Vuković, Dušan Zlatković, and Petar Svorcan. 2025. "Exploring the Potential of Oral Butyrate Supplementation in Metabolic Dysfunction-Associated Steatotic Liver Disease: Subgroup Insights from an Interventional Study" International Journal of Molecular Sciences 26, no. 12: 5561. https://doi.org/10.3390/ijms26125561
APA StyleMitrović, M., Stanković Popović, V., Erceg, S., Perišić Mitrović, M., Dobrosavljević, A., Stupar, A., Vuković, P., Zlatković, D., & Svorcan, P. (2025). Exploring the Potential of Oral Butyrate Supplementation in Metabolic Dysfunction-Associated Steatotic Liver Disease: Subgroup Insights from an Interventional Study. International Journal of Molecular Sciences, 26(12), 5561. https://doi.org/10.3390/ijms26125561





