Effect of Mexican Propolis on Wound Healing in a Murine Model of Diabetes Mellitus
Abstract
1. Introduction
2. Results
2.1. Chemical Characterization
2.2. Toxicity
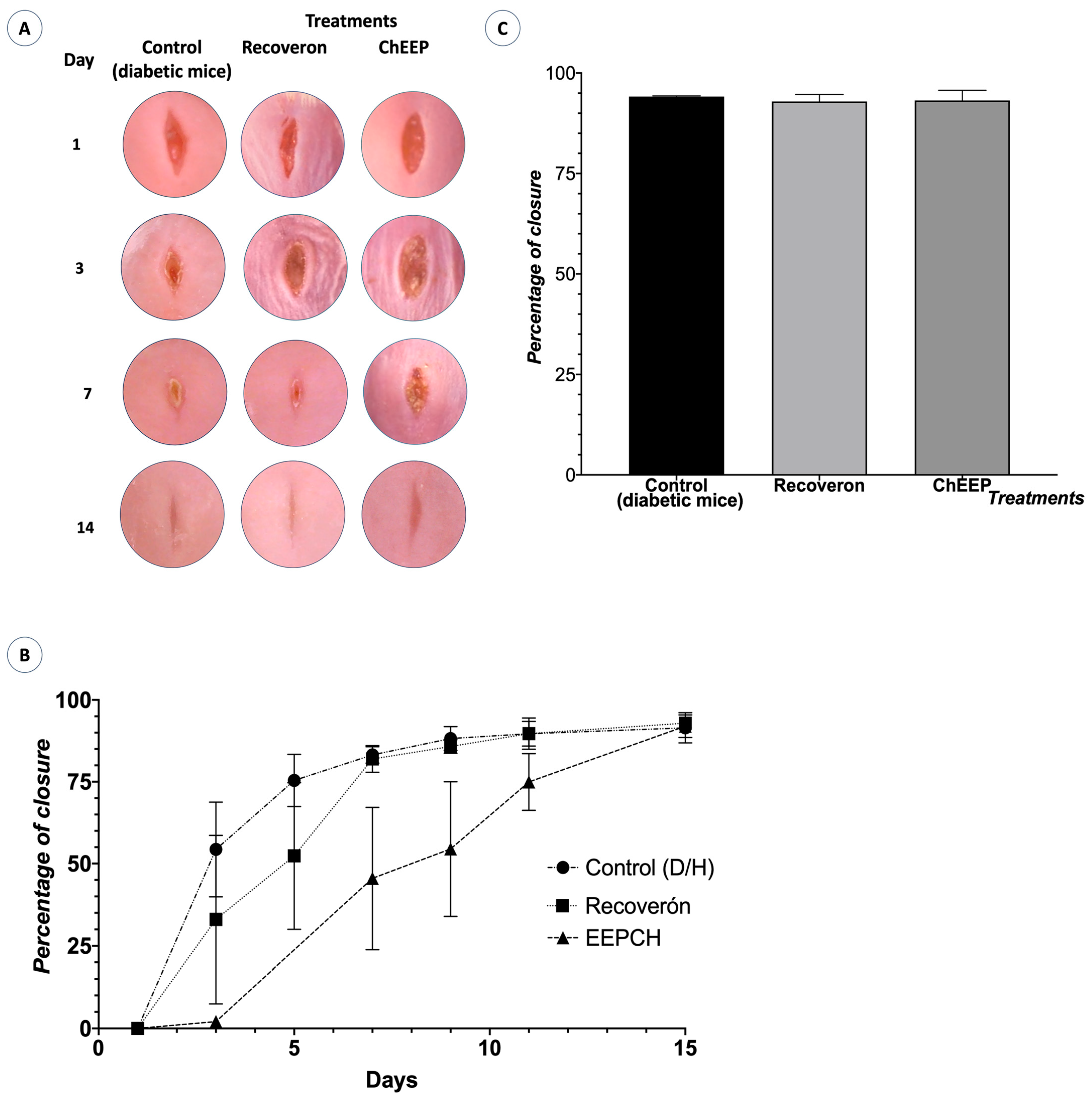
2.3. Closing Speed
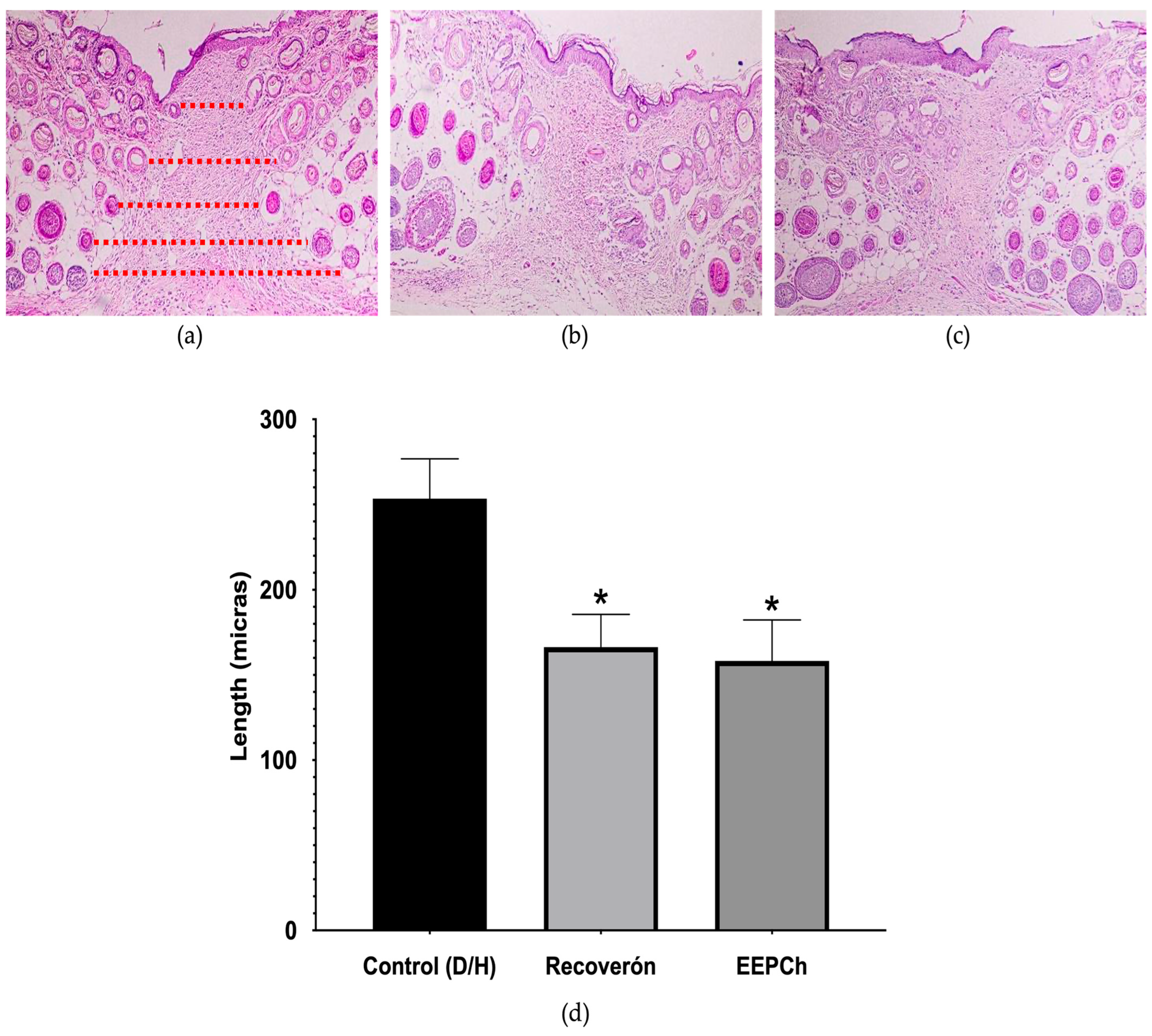
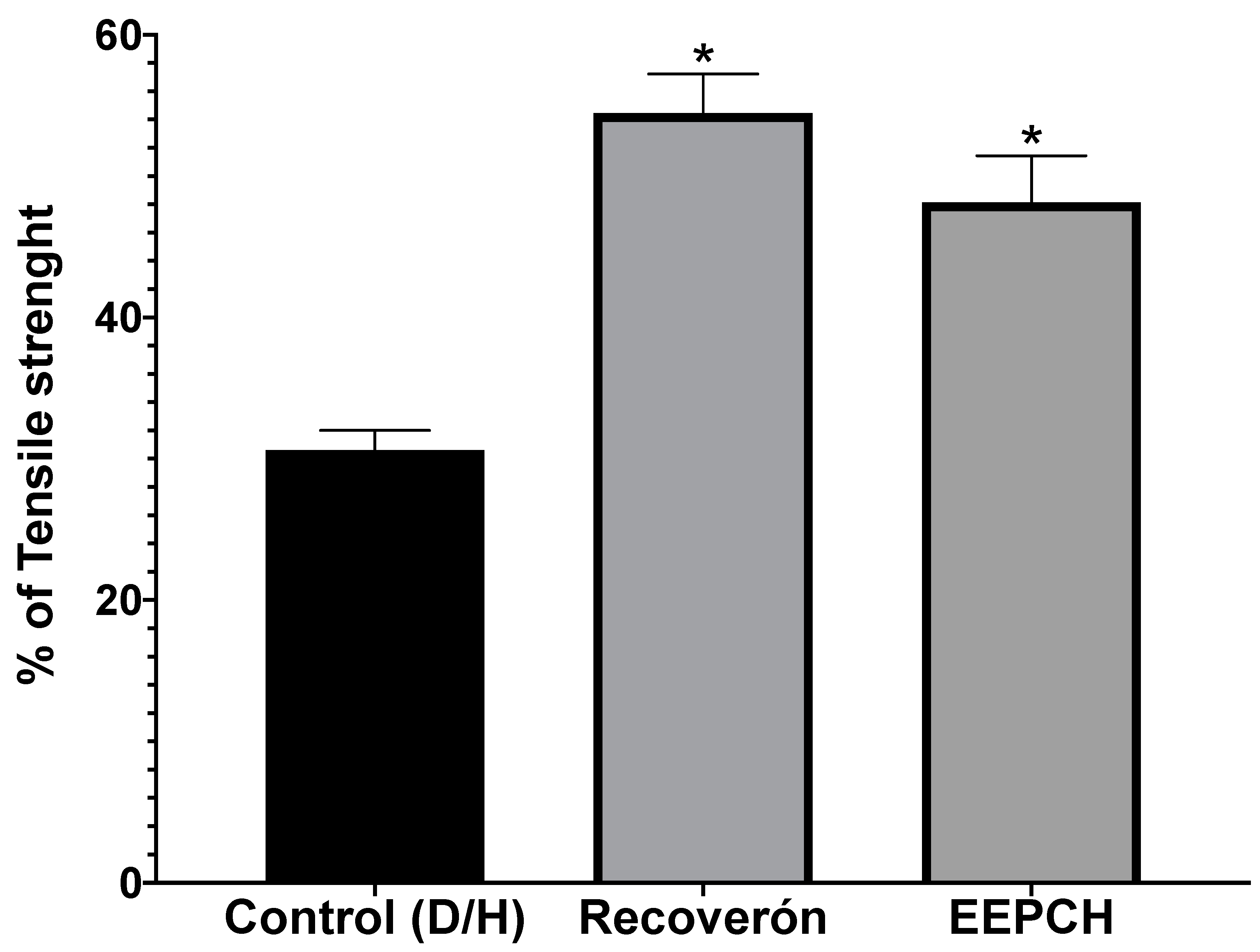
2.4. Tensile Strength
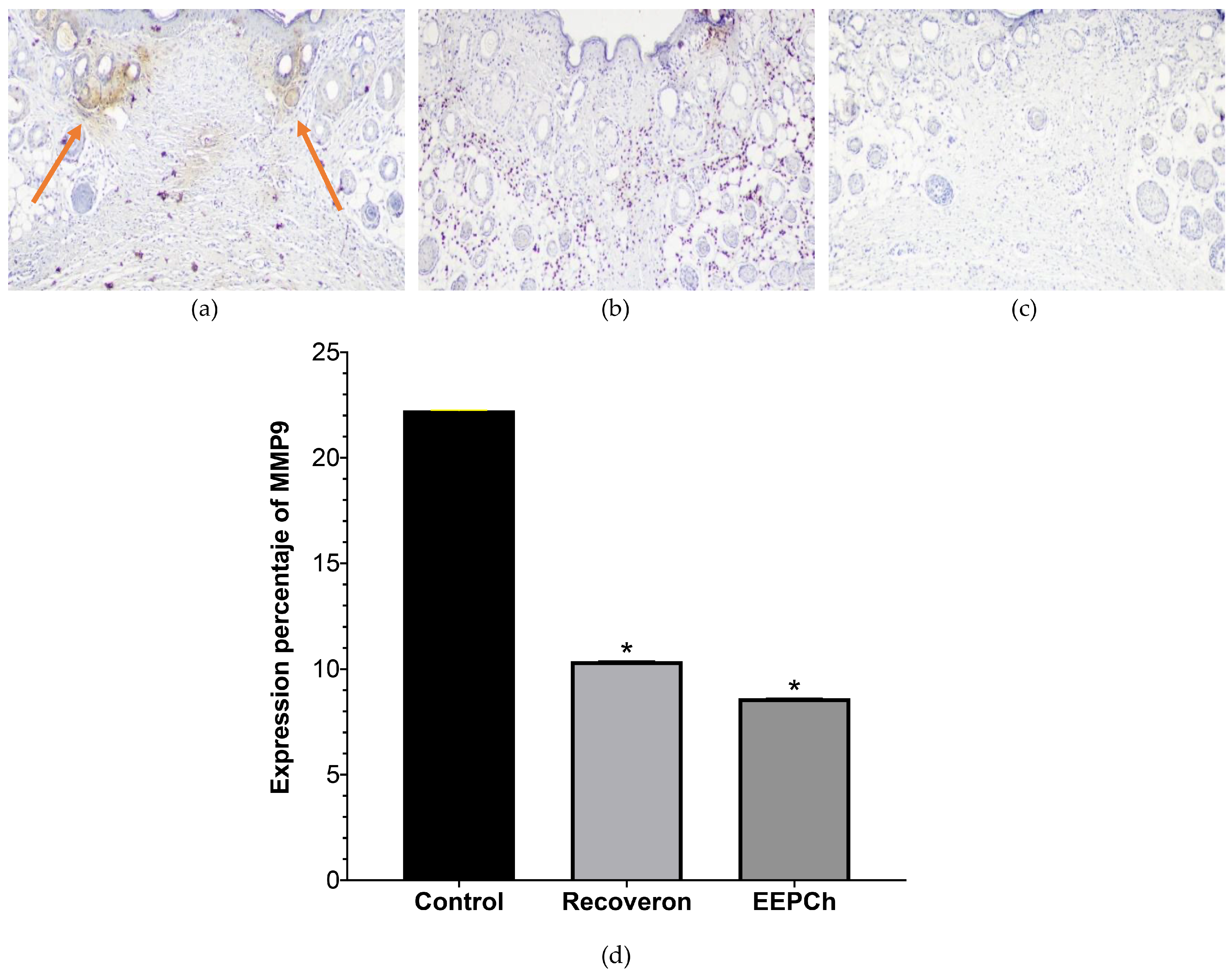
2.5. Quantification of α—Actin and MMP9 by Immunohistochemical Analysis
3. Discussion
4. Materials and Methods
4.1. Chemicals and Solvents
4.2. Propolis
4.3. Organoleptic Properties
4.4. Antioxidant Capacity
4.5. Total Phenols
4.6. Total Flavonoids
4.7. Fractionation of ChEEP
4.8. Preparatory Plate
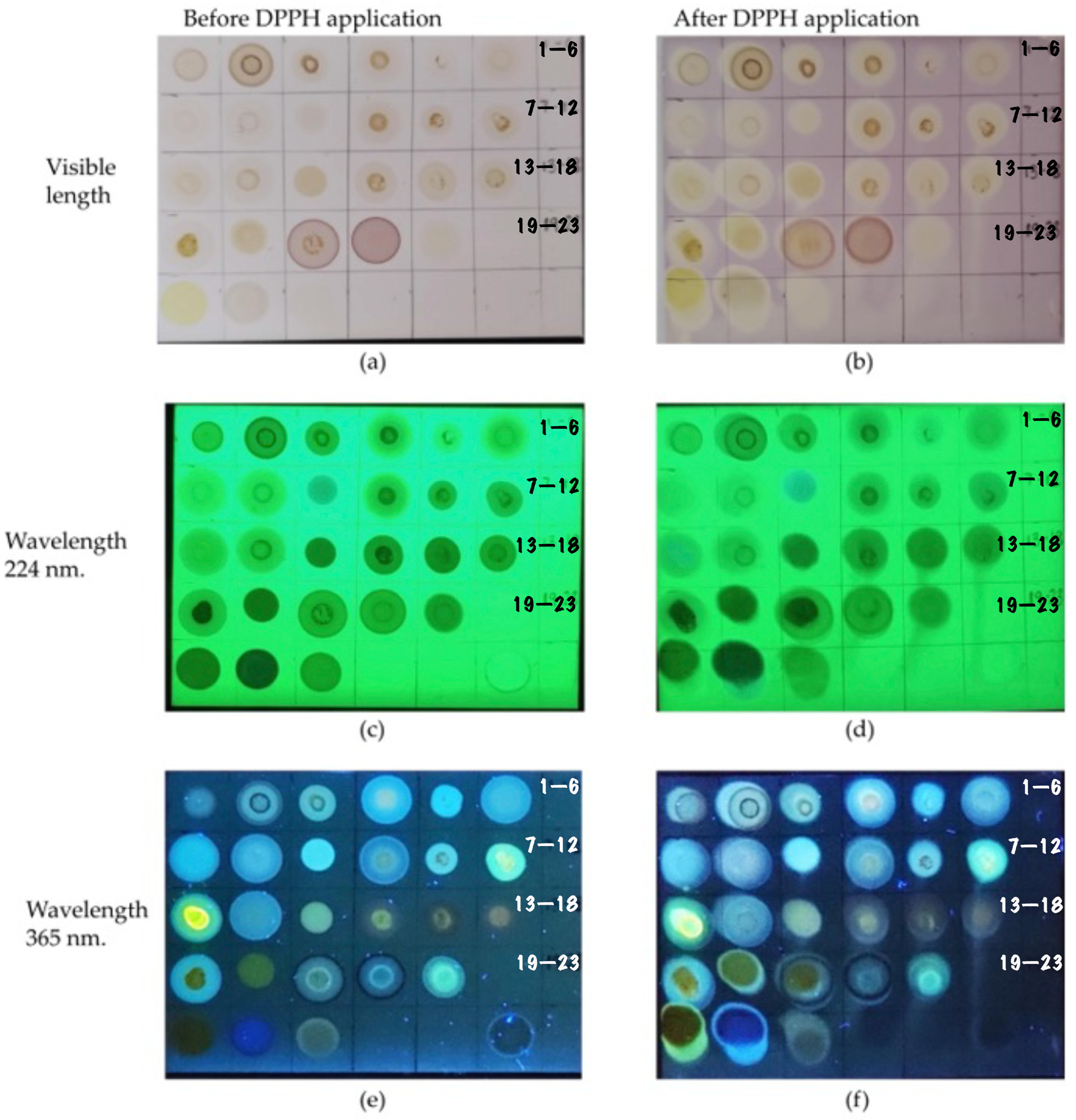
4.9. Antioxidant Capacity Determination by Thin Layer Chromatography (TLC)
4.10. GC–MS
4.11. HPLC—DAD
4.12. HPLC–MS
4.13. Laboratory Animals
4.14. DM Induction
4.15. Healing Efficiency
4.15.1. Closing Speed
4.15.2. Tensile Strength
4.16. Immunohistochemical Analysis
4.17. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yousef, H.; Alhajj, M.; Sharma, S. Anatomy, Skin (Integument), Epidermis. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2023. [Google Scholar]
- Guarín-Corredor, C.; Quiroga-Santamaría, P.; Landínez-Parra, N.S. Proceso de Cicatrización de heridas de piel, campos endógenos y su relación con las heridas crónicas. Rev. De La Fac. De Med. 2013, 61, 441–448. [Google Scholar]
- Ibrahim, N.I.; Wong, S.K.; Mohamed, I.N.; Mohamed, N.; Chin, K.-Y.; Ima-Nirwana, S.; Shuid, A.N. Wound healing properties of selected natural products. Int. J. Environ. Res. Public Health 2018, 15, 2360. [Google Scholar] [CrossRef] [PubMed]
- Conget, I. Diagnosis, classification and cathogenesis of diabetes mellitus. Rev. Esp. De Cardiol. 2002, 55, 528–535. [Google Scholar] [CrossRef]
- Benavides, J. Reparación de heridas cutáneas. Rev. Asoc. Col. Dermatol 2008, 16, 29–35. [Google Scholar]
- Wilkinson, H.N.; Hardman, M.J. Wound healing: Cellular mechanisms and pathological outcomes. Open Biol. 2020, 10, 200223. [Google Scholar] [CrossRef]
- Hanses, F.; Park, S.; Rich, J.; Lee, J.C. Reduced neutrophil apoptosis in diabetic mice during staphylococcal infection leads to prolonged Tnfα production and reduced neutrophil clearance. PLoS ONE 2011, 6, e23633. [Google Scholar] [CrossRef]
- Khanna, S.; Biswas, S.; Shang, Y.; Collard, E.; Azad, A.; Kauh, C.; Bhasker, V.; Gordillo, G.M.; Sen, C.K.; Roy, S. Macrophage dysfunction impairs resolution of inflammation in the wounds of diabetic mice. PLoS ONE 2010, 5, e9539. [Google Scholar] [CrossRef]
- Wong, S.L.; Demers, M.; Martinod, K.; Gallant, M.; Wang, Y.; Goldfine, A.B.; Kahn, C.R.; Wagner, D.D. Diabetes primes neutrophils to undergo NETosis, which impairs wound healing. Nat. Med. 2015, 21, 815–819. [Google Scholar] [CrossRef] [PubMed]
- Gardiner, M.; Vicaretti, M.; Sparks, J.; Bansal, S.; Bush, S.; Liu, M.; Darling, A.; Harry, E.; Burke, C.M. A longitudinal study of the diabetic skin and wound microbiome. PeerJ 2017, 5, e3543. [Google Scholar] [CrossRef]
- Yager, D.R.; Chen, S.M.; Ward, S.I.; Olutoye, O.O.; Diegelmann, R.F.; Kelman Cohen, I. Ability of chronic wound fluids to degrade peptide growth factors is associated with increased levels of elastase activity and diminished levels of proteinase inhibitors. Wound Repair Regen. 1997, 5, 23–32. [Google Scholar] [CrossRef]
- Martins, V.L.; Caley, M.; O’Toole, E.A. Matrix metalloproteinases and epidermal wound repair. Cell Tissue Res. 2013, 351, 255–268. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Qian, Y.; Jin, R.; Wo, Y.; Chen, J.; Wang, C.; Wang, D. Effects of TRAP-1-Like Protein (TLP) Gene on Collagen Synthesis Induced by TGF-β/Smad Signaling in Human Dermal Fibroblasts. PLoS ONE 2013, 8, e55899. [Google Scholar] [CrossRef]
- Hozzein, W.N.; Badr, G.; Al Ghamdi, A.A.; Sayed, A.; Al-Waili, N.S.; Garraud, O. Topical Application of Propolis Enhances Cutaneous Wound Healing by Promoting TGF-Beta/Smad-Mediated Collagen Production in a Streptozotocin-Induced Type I Diabetic Mouse Model. Cell. Physiol. Biochem. 2015, 37, 940–954. [Google Scholar] [CrossRef]
- Ramos, A.; Miranda, J. Propolis: A review of its anti-inflammatory and healing actions. J. Venom. Anim. Toxins Incl. Trop. Dis. 2007, 13, 697–710. [Google Scholar] [CrossRef]
- Ivanovska, N.; Stefanova, Z.; Valeva, V.; Neychev, H. Immunodulatory action of propolis: VII. A comparative study on cinnamic and caffeic acid lysine derivatives. Dokl. Na Bulg. Akad. Na Nauk. 1993, 46, 115–118. [Google Scholar]
- Anjum, S.I.; Ullah, A.; Khan, K.A.; Attaullah, M.; Khan, H.; Ali, H.; Bashir, M.A.; Tahir, M.; Ansari, M.J.; Ghramh, H.A.; et al. Composition and functional properties of propolis (bee glue): A review. Saudi J. Biol. Sci. 2019, 26, 1695–1703. [Google Scholar] [CrossRef]
- Castaldo, S.; Capasso, F. Propolis, an old remedy used in modern medicine. Fitoterapia 2002, 73, S1–S6. [Google Scholar] [CrossRef]
- Balderas-Cordero, D.; Canales-Alvarez, O.; Sánchez-Sánchez, R.; Cabrera-Wrooman, A.; Canales-Martinez, M.M.; Rodriguez-Monroy, M.A. Anti-Inflammatory and Histological Analysis of Skin Wound Healing through Topical Application of Mexican Propolis. Int. J. Mol. Sci. 2023, 24, 11831. [Google Scholar] [CrossRef] [PubMed]
- Vargas-Sánchez, R.; Torrescano-Urrutia, G.; Mendoza-Wilson, A.; Vallejo-Galland, V.; Acedo-Felix, E.; Sánchez-Escalante, J.; Sánchez-Escalante, A. Mecanismos involucrados en la actividad antioxidante y antibacteriana de propóleos. Biotecnia 2014, 16, 32–37. [Google Scholar] [CrossRef]
- Ruiz-Hurtado, P.A.; Garduño-Siciliano, L.; Domínguez-Verano, P.; Balderas-Cordero, D.; Gorgua-Jiménez, G.; Canales-Álvarez, O.; Canales-Martínez, M.M.; Rodríguez-Monroy, M.A. Propolis and its gastroprotective effects on nsaid-induced gastric ulcer disease: A systematic review. Nutrients 2021, 13, 3169. [Google Scholar] [CrossRef]
- NORMA Oficial Mexicana NOM-003-SAG/GAN-2017, Propóleos, Producción y Especificaciones Para su Procesamiento. CDMX, México. Diario Oficial de la Federación. Secretaria de Gobernación. Available online: https://www.dof.gob.mx/normasOficiales/6794/sagarpa11_C/sagarpa11_C.html#:~:text=1.1%20Esta%20Norma%20es%20de,y%20comercializaci%C3%B3n%20en%20el%20pa%C3%ADs (accessed on 24 October 2023).
- Alexandru, V.; Gaspar, A.; Savin, S.; Toma, A.; Tatia, R.; Gille, E. Phenolic content, antioxidant activity and effect on collagen synthesis of a traditional wound healing polyherbal formula. Stud. Univ. Vasile Goldis Arad Life Sci. Ser. 2015, 25, 41. [Google Scholar]
- Polaka, S.; Katare, P.; Pawar, B.; Vasdev, N.; Gupta, T.; Rajpoot, K.; Sengupta, P.; Tekade, R.K. Emerging ROS-modulating technologies for augmentation of the wound healing process. ACS Omega 2022, 7, 30657–30672. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Pérez, B.; Canales Martínez, M.M.; Penieres Carrillo, J.G.; Cruz Sánchez, T.A. Chemical composition, antioxidant properties and antimicrobial activity of Mexican propolis. Acta Univ. 2020, 30, e2435. [Google Scholar]
- Al-Fatimi, M.; Wurster, M.; Schröder, G.; Lindequist, U. Antioxidant, antimicrobial and cytotoxic activities of selected medicinal plants from Yemen. J. Ethnopharmacol. 2007, 111, 657–666. [Google Scholar] [CrossRef]
- Bankova, V. Recent trends and important developments in propolis research. Evid.-Based Complement. Altern. Med. 2005, 2, 29–32. [Google Scholar] [CrossRef]
- Rivera-Yañez, N.; Rivera-Yañez, C.R.; Pozo-Molina, G.; Méndez-Catalá, C.F.; Méndez-Cruz, A.R.; Nieto-Yañez, O. Biomedical properties of propolis on diverse chronic diseases and its potential applications and health benefits. Nutrients 2020, 13, 78. [Google Scholar] [CrossRef]
- Alday-Provencio, S.; Diaz, G.; Rascon, L.; Quintero, J.; Alday, E.; Robles-Zepeda, R.; Garibay-Escobar, A.; Astiazaran, H.; Hernandez, J.; Velazquez, C. Sonoran propolis and some of its chemical constituents inhibit in vitro growth of Giardia lamblia trophozoites. Planta Medica 2015, 81, 742–747. [Google Scholar] [CrossRef]
- Menezes, P.d.P.; Frank, L.A.; Lima, B.d.S.; de Carvalho, Y.M.B.G.; Serafini, M.R.; Quintans-Júnior, L.J.; Pohlmann, A.R.; Guterres, S.S.; Araújo, A.A.d.S. Hesperetin-loaded lipid-core nanocapsules in polyamide: A new textile formulation for topical drug delivery. Int. J. Nanomed. 2017, 2069–2079. [Google Scholar] [CrossRef] [PubMed]
- Bagher, Z.; Ehterami, A.; Safdel, M.H.; Khastar, H.; Semiari, H.; Asefnejad, A.; Davachi, S.M.; Mirzaii, M.; Salehi, M. Wound healing with alginate/chitosan hydrogel containing hesperidin in rat model. J. Drug Deliv. Sci. Technol. 2020, 55, 101379. [Google Scholar] [CrossRef]
- Carvalho, M.T.; Araújo-Filho, H.G.; Barreto, A.S.; Quintans-Júnior, L.J.; Quintans, J.S.; Barreto, R.S. Wound healing properties of flavonoids: A systematic review highlighting the mechanisms of action. Phytomedicine 2021, 90, 153636. [Google Scholar] [CrossRef] [PubMed]
- Al-Roujayee, A.S. Naringenin improves the healing process of thermally-induced skin damage in rats. J. Int. Med. Res. 2017, 45, 570–582. [Google Scholar] [CrossRef]
- Salehi, M.; Ehterami, A.; Farzamfar, S.; Vaez, A.; Ebrahimi-Barough, S. Accelerating healing of excisional wound with alginate hydrogel containing naringenin in rat model. Drug Deliv. Transl. Res. 2021, 11, 142–153. [Google Scholar] [CrossRef]
- Salehi, M.; Vaez, A.; Naseri-Nosar, M.; Farzamfar, S.; Ai, A.; Ai, J.; Tavakol, S.; Khakbiz, M.; Ebrahimi-Barough, S. Naringin-loaded poly (ε-caprolactone)/gelatin electrospun mat as a potential wound dressing: In vitro and in vivo evaluation. Fibers Polym. 2018, 19, 125–134. [Google Scholar] [CrossRef]
- Kandhare, A.D.; Alam, J.; Patil, M.V.; Sinha, A.; Bodhankar, S.L. Wound healing potential of naringin ointment formulation via regulating the expression of inflammatory, apoptotic and growth mediators in experimental rats. Pharm. Biol. 2016, 54, 419–432. [Google Scholar] [CrossRef]
- Chen, L.-Y.; Cheng, H.-L.; Kuan, Y.-H.; Liang, T.-J.; Chao, Y.-Y.; Lin, H.-C. Therapeutic potential of luteolin on impaired wound healing in streptozotocin-induced rats. Biomedicines 2021, 9, 761. [Google Scholar] [CrossRef]
- Mohammadi, Z.; Sharif Zak, M.; Majdi, H.; Seidi, K.; Barati, M.; Akbarzadeh, A.; Latifi, A.M. The effect of chrysin-loaded nanofiber on wound healing process in male rat. Chem. Biol. Drug Des. 2017, 90, 1106–1114. [Google Scholar] [CrossRef]
- Pivec, T.; Kargl, R.; Maver, U.; Bračič, M.; Elschner, T.; Žagar, E.; Gradišnik, L.; Stana Kleinschek, K. Chemical structure–Antioxidant activity relationship of water–based enzymatic polymerized rutin and its wound healing potential. Polymers 2019, 11, 1566. [Google Scholar] [CrossRef]
- Özay, Y.; Güzel, S.; Yumrutaş, Ö.; Pehlivanoğlu, B.; Erdoğdu, İ.H.; Yildirim, Z.; Türk, B.A.; Darcan, S. Wound healing effect of kaempferol in diabetic and nondiabetic rats. J. Surg. Res. 2019, 233, 284–296. [Google Scholar] [CrossRef]
- Park, E.; Lee, S.M.; Jung, I.-K.; Lim, Y.; Kim, J.-H. Effects of genistein on early-stage cutaneous wound healing. Biochem. Biophys. Res. Commun. 2011, 410, 514–519. [Google Scholar] [CrossRef]
- Ruttanapattanakul, J.; Wikan, N.; Potikanond, S.; Nimlamool, W. Molecular Targets of Pinocembrin Underlying Its Regenerative Activities in Human Keratinocytes. Pharmaceuticals 2022, 15, 954. [Google Scholar] [CrossRef]
- Moldoveanu, S.C.; David, V. Derivatization methods in GC and GC/MS. In Gas Chromatography—Derivatization, Sample Preparation, Application; IntechOpen: Rijeka, Croatia, 2018; Volume 9. [Google Scholar]
- Cui, J.; Duan, X.; Ke, L.; Pan, X.; Liu, J.; Song, X.; Ma, W.; Zhang, W.; Liu, Y.; Fan, Y. Extraction, purification, structural character and biological properties of propolis flavonoids: A review. Fitoterapia 2022, 157, 105106. [Google Scholar] [CrossRef]
- Garcia-Viguera, C.; Ferreres, F.; Tomas-Barberan, F. Study of Canadian propolis by GC-MS and HPLC. Z. Für Naturforschung C 1993, 48, 731–735. [Google Scholar] [CrossRef]
- Duran, N.; Muz, M.; Culha, G.; Duran, G.; Ozer, B. GC-MS analysis and antileishmanial activities of two Turkish propolis types. Parasitol. Res. 2011, 108, 95–105. [Google Scholar] [CrossRef]
- Jara, C.P.; Mendes, N.F.; Prado, T.P.d.; de Araujo, E.P. Bioactive fatty acids in the resolution of chronic inflammation in skin wounds. Adv. Wound Care 2020, 9, 472–490. [Google Scholar] [CrossRef]
- Silva, J.M.; Pereira, C.V.; Mano, F.; Silva, E.; Castro, V.n.I.; Sá-Nogueira, I.; Reis, R.L.; Paiva, A.; Matias, A.A.; Duarte, A.R.C. Therapeutic role of deep eutectic solvents based on menthol and saturated fatty acids on wound healing. ACS Appl. Bio Mater. 2019, 2, 4346–4355. [Google Scholar] [CrossRef]
- Chuah, X.Q.; Okechukwu, P.N.; Amini, F.; Teo, S.S. Eicosane, pentadecane and palmitic acid: The effects in: In vitro: Wound healing studies. Asian Pac. J. Trop. Biomed. 2018, 8, 490–499. [Google Scholar]
- Lotfy, M. Biological activity of bee propolis in health and disease. Asian Pac. J. Cancer Prev. 2006, 7, 22–31. [Google Scholar]
- Burdock, G. Review of the biological properties and toxicity of bee propolis (propolis). Food Chem. Toxicol. 1998, 36, 347–363. [Google Scholar] [CrossRef]
- Dasari, N.; Jiang, A.; Skochdopole, A.; Chung, J.; Reece, E.M.; Vorstenbosch, J.; Winocour, S. Updates in diabetic wound healing, inflammation, and scarring. Semin. Plast. Surg. 2021, 35, 153–158. [Google Scholar] [CrossRef]
- Voss, G.T.; Gularte, M.S.; Vogt, A.G.; Giongo, J.L.; Vaucher, R.A.; Echenique, J.V.; Soares, M.P.; Luchese, C.; Wilhelm, E.A.; Fajardo, A.R. Polysaccharide-based film loaded with vitamin C and propolis: A promising device to accelerate diabetic wound healing. Int. J. Pharm. 2018, 552, 340–351. [Google Scholar] [CrossRef]
- Khodabakhshi, D.; Eskandarinia, A.; Kefayat, A.; Rafienia, M.; Navid, S.; Karbasi, S.; Moshtaghian, J. In vitro and in vivo performance of a propolis-coated polyurethane wound dressing with high porosity and antibacterial efficacy. Colloids Surf. B Biointerfaces 2019, 178, 177–184. [Google Scholar] [CrossRef]
- Vaisberg, A.J.; Milla, M.; del Carmen Planas, M.; Cordova, J.L.; de Agusti, E.R.; Ferreyra, R.; del Carmen Mustiga, M.; Carlin, L.; Hammond, G.B. Taspine is the cicatrizant principle in Sangre de Grado extracted from Croton lechleri. Planta Medica 1989, 55, 140–143. [Google Scholar]
- Kapare, H.S.; Giram, P.S.; Raut, S.S.; Gaikwad, H.K.; Paiva-Santos, A.C. Formulation Development and Evaluation of Indian Propolis Hydrogel for Wound Healing. Gels 2023, 9, 375. [Google Scholar] [CrossRef]
- Hernandez-Hernandez, A.B.; Alarcon-Aguilar, F.J.; Garcia-Lorenzana, M.; Rodriguez-Monroy, M.A.; Canales-Martinez, M.M. Jatropha neopauciflora Pax latex exhibits wound-healing effect in normal and diabetic mice. J. Evid.-Based Integr. Med. 2021, 26, 2515690X20986762. [Google Scholar] [CrossRef]
- Wan, R.; Weissman, J.P.; Grundman, K.; Lang, L.; Grybowski, D.J.; Galiano, R.D. Diabetic wound healing: The impact of diabetes on myofibroblast activity and its potential therapeutic treatments. Wound Repair Regen. 2021, 29, 573–581. [Google Scholar] [CrossRef]
- Herrera-Matta, J.J. Factores que afectan la cicatrización. In Ciencias Básicas en Cirugía; Medical Times S. A. C.: Lima, Perú, 2006; p. 22. [Google Scholar]
- Abdollahi, M.; Ng, T.S.Y.; Rezaeizadeh, A.; Aamidor, S.; Twigg, S.M.; Min, D.; McLennan, S.V. Insulin treatment prevents wounding associated changes in tissue and circulating neutrophil MMP-9 and NGAL in diabetic rats. PLoS ONE 2017, 12, e0170951. [Google Scholar] [CrossRef]
- Ernawati, D.S.; Puspa, A. Expression of vascular endothelial growth factor and matrix metalloproteinase-9 in Apis mellifera Lawang propolis extract gel-treated traumatic ulcers in diabetic rats. Vet. World 2018, 11, 304. [Google Scholar] [CrossRef]
- Retamal, I.; Hernández, R.; Velarde, V.; Oyarzún, A.; Martínez, C.; Julieta González, M.; Martínez, J.; Smith, P.C. Diabetes alters the involvement of myofibroblasts during periodontal wound healing. Oral Dis. 2020, 26, 1062–1071. [Google Scholar]
- Chaudhary, A.; Bag, S.; Banerjee, P.; Chatterjee, J. Wound healing efficacy of Jamun honey in diabetic mice model through reepithelialization, collagen deposition and angiogenesis. J. Tradit. Complement. Med. 2020, 10, 529–543. [Google Scholar] [CrossRef]
- Zhan, K.; Ejima, H.; Yoshie, N. Antioxidant and adsorption properties of bioinspired phenolic polymers: A comparative study of catechol and gallol. ACS Sustain. Chem. Eng. 2016, 4, 3857–3863. [Google Scholar] [CrossRef]
- Ferrara, L. Antioxidant activity of Tamarindus indica L. In Ingredienti Alimentari (Italy); PVI: Milano, Italy, 2005. [Google Scholar]
- Diaz-Uribe, C.E.; Vallejo, W.; Oliveros, G.; Muñoz, A. Study of scavenging capacity of naringin extracted from Citrus uranium peel against free radicals. Prospectiva 2016, 14, 31–35. [Google Scholar]
- Heo, H.J.; Kim, D.-O.; Shin, S.C.; Kim, M.J.; Kim, B.G.; Shin, D.-H. Effect of antioxidant flavanone, naringenin, from Citrus junos on neuroprotection. J. Agric. Food Chem. 2004, 52, 1520–1525. [Google Scholar] [CrossRef]
- Record, I.R.; Dreosti, I.E.; McInerney, J.K. The antioxidant activity of genistein in vitro. J. Nutr. Biochem. 1995, 6, 481–485. [Google Scholar] [CrossRef]
- Seelinger, G.; Merfort, I.; Schempp, C.M. Anti-oxidant, anti-inflammatory and anti-allergic activities of luteolin. Planta Medica 2008, 74, 1667–1677. [Google Scholar] [CrossRef]
- Rasul, A.; Millimouno, F.M.; Ali Eltayb, W.; Ali, M.; Li, J.; Li, X. Pinocembrin: A novel natural compound with versatile pharmacological and biological activities. BioMed Res. Int. 2013, 2013, 379850. [Google Scholar] [CrossRef]
- Han, A.-R.; Nam, B.; Kim, B.-R.; Lee, K.-C.; Song, B.-S.; Kim, S.H.; Kim, J.-B.; Jin, C.H. Phytochemical composition and antioxidant activities of two different color chrysanthemum flower teas. Molecules 2019, 24, 329. [Google Scholar] [CrossRef]
- Ivănescu, B.; Tuchiluș, C.; Corciovă, A.; Lungu, C.; Mihai, C.T.; Gheldiu, A.-M.; Vlase, L. Antioxidant, antimicrobial and cytotoxic activity of Tanacetum vulgare, Tanacetum corymbosum and Tanacetum macrophyllum extracts. Farmacia 2018, 66, 282–288. [Google Scholar]
- Hirano, R.; Sasamoto, W.; Matsumoto, A.; Itakura, H.; Igarashi, O.; Kondo, K. Antioxidant ability of various flavonoids against DPPH radicals and LDL oxidation. J. Nutr. Sci. Vitaminol. 2001, 47, 357–362. [Google Scholar] [CrossRef]
- Wang, J.; Fang, X.; Ge, L.; Cao, F.; Zhao, L.; Wang, Z.; Xiao, W. Antitumor, antioxidant and anti-inflammatory activities of kaempferol and its corresponding glycosides and the enzymatic preparation of kaempferol. PLoS ONE 2018, 13, e0197563. [Google Scholar] [CrossRef]
- Deldar, Y.; Pilehvar-Soltanahmadi, Y.; Dadashpour, M.; Montazer Saheb, S.; Rahmati-Yamchi, M.; Zarghami, N. An in vitro examination of the antioxidant, cytoprotective and anti-inflammatory properties of chrysin-loaded nanofibrous mats for potential wound healing applications. Artif. Cells Nanomed. Biotechnol. 2018, 46, 706–716. [Google Scholar] [CrossRef]
- Do Hoang Thu Trang, H.L.; Son, P.V.T. Investigation on the in vitro antioxidant capacity of methanol extract, fractions and flavones from Oroxylum indicum Linn bark. BJPS Braz. J. Pharm. Sci. 2018, 54. [Google Scholar]
- Huang, X.; Bao, X.; Liu, Y.; Wang, Z.; Hu, Q. Catechol-functional chitosan/silver nanoparticle composite as a highly effective antibacterial agent with species-specific mechanisms. Sci. Rep. 2017, 7, 1860. [Google Scholar] [CrossRef]
- Cvetnic, Z.; Vladimir-Knezevic, S. Antimicrobial activity of grapefruit seed and pulp ethanolic extract. Acta Pharm. 2004, 54, 243–250. [Google Scholar]
- Lee, K.A.; Moon, S.-H.; Lee, J.-Y.; Kim, K.-T.; Park, Y.-S.; Paik, H.-D. Antibacterial activity of a novel flavonoid, 7-O-butyl naringenin, against methicillin-resistant Staphylococcus aureus (MRSA). Food Sci. Biotechnol. 2013, 22, 1725–1728. [Google Scholar] [CrossRef]
- Ramnath, S.; Venkataramegowda, S. Antioxidant activity of Indian propolis—An in vitro evaluation. Int. J. Pharmacol. Phytochem. Ethnomedicine 2016, 5, 79–85. [Google Scholar] [CrossRef]
- Singleton, V.L.; Orthofer, R.; Lamuela-Raventós, R.M. Analysis of total phenols and other oxidation substrates and antioxidants by means of folin-ciocalteu reagent. In Methods in Enzymology; Elsevier: Amsterdam, The Netherlands, 1999; Volume 299, pp. 152–178. [Google Scholar]
- Ramamoorthy, P.K.; Bono, A. Antioxidant activity, total phenolic and flavonoid content of Morinda citrifolia fruit extracts from various extraction processes. J. Eng. Sci. Technol. 2007, 2, 70–80. [Google Scholar]
- Robards, K.; Ryan, D. Chapter 11—Preparative chromatography. In Principles and Practice of Modern Chromatographic Methods, 2nd ed.; Robards, K., Ryan, D., Eds.; Academic Press: Cambridge, MA, USA, 2022; pp. 495–513. [Google Scholar]
- Marston, A. Thin-layer chromatography with biological detection in phytochemistry. J. Chromatogr. A 2011, 1218, 2676–2683. [Google Scholar] [CrossRef]
- Gu, L.; Wu, T.; Wang, Z. TLC bioautography-guided isolation of antioxidants from fruit of Perilla frutescens var. acuta. LWT-Food Sci. Technol. 2009, 42, 131–136. [Google Scholar] [CrossRef]
- Rodriguez-Canales, M.; Medina-Romero, Y.M.; Rodriguez-Monroy, M.A.; Nava-Solis, U.; Bolaños-Cruz, S.I.; Mendoza-Romero, M.J.; Campos, J.E.; Hernandez-Hernandez, A.B.; Chirino, Y.I.; Cruz-Sanchez, T. Activity of propolis from Mexico on the proliferation and virulence factors of Candida albicans. BMC Microbiol. 2023, 23, 325. [Google Scholar] [CrossRef]
- Rivera-Yañez, N.; Rodriguez-Canales, M.; Nieto-Yañez, O.; Jimenez-Estrada, M.; Ibarra-Barajas, M.; Canales-Martinez, M.; Rodriguez-Monroy, M. Hypoglycaemic and antioxidant effects of propolis of Chihuahua in a model of experimental diabetes. Evid. Based Complement. Altern. Med. 2018, 2018, 4360356. [Google Scholar] [CrossRef]


| Organoleptic Properties | ||||
|---|---|---|---|---|
| Colour | Odour | Flavour | Consistency | |
| ChEEP | Dark yellow | Waxy balsamic | Slightly spicy | Rigid |
| General Chemical Characterization | |||||
|---|---|---|---|---|---|
| Propolis | Yield | Medium Antioxidant Capacity | Total Phenol Content | Total Flavonoid Content | |
| ChEEP | 300 g | 67% | 29.46 µg/mL | 32.53% | 5.68% |
| CompoundType of Compound/Fraction | Retention Time | Percentage Area (%) | Similarity Percentage |
|---|---|---|---|
| α—Bisabololsesquiterpene/a | 15.8178 | 0.647 | 94 |
| Palmitic acidfatty acid/a | 20.6293 | 1.97 | 99 |
| Hexadecanalaldehyde/a | 22.4513 | 0.315 | 99 |
| Heneicosanealcane/a | 23.8755 | 0.072 | 99 |
| cis—13—Octadecenoic acid, methyl esterfatty acid/a | 23.946 | 3.098 | 99 |
| 2—nonadecanoneceton/a | 24.0102 | 1.497 | 99 |
| Stearic acidfatty acid/a | 24.4015 | 0.689 | 99 |
| Bicyclo[10.8.0]eicosane, cis—hydrocarbon/a | 26.1336 | 1.015 | 97 |
| Methyl 18—methylnonadecanoate/a | 27.8786 | 1.883 | 99 |
| Pinostrobine chalconechalcone/a | 29.2194 | 2.701 | 98 |
| 13—Docosen—1—ol, (Z)/a | 29.5203 | 1.146 | 98 |
| 9—Nonadecenehydrocarbon/a | 30.2138 | 0.572 | 95 |
| Eicosanealcane/a | 30.6051 | 1.132 | 97 |
| Behenic acidfatty acid/a | 31.0991 | 1.905 | 99 |
| Tectocrysineflavone/a | 32.2731 | 0.412 | 95 |
| Lignoceric acidfatty acid/a | 34.095 | 3.337 | 98 |
| Cerotic acidfatty acid/a | 36.8793 | 0.808 | 91 |
| 1—Nonadecenehydrocarbon/a | 38.7397 | 1.836 | 95 |
| 1—Docosenehydrocarbon/a | 38.8295 | 1.39 | 97 |
| Isohexanehydrocarbon/b | 1.5246 | 0.16 | 91 |
| 1—Heptacosanolalcohol/b | 32.1962 | 7.798 | 95 |
| β—d—glucosemonosacarid/c | 16.5878 | 0.245 | 91 |
| α—D—Glucopiranosemonosacaride/c | 20.6295 | 3.406 | 94 |
| D—manosemonosacaride/c | 21.1491 | 2.393 | 91 |
| Oxirane, hexadecylhydrocarbon/c | 26.1274 | 0.388 | 95 |
| Pinostrobine chalconechalcone/c, a | 29.2324 | 0.537 | 97 |
| Lignoceric acidfatty acid/c, a | 34.0824 | 0.354 | 90 |
| CompoundType of Compound/Fraction | Retention Time | Total Abundance | Match |
|---|---|---|---|
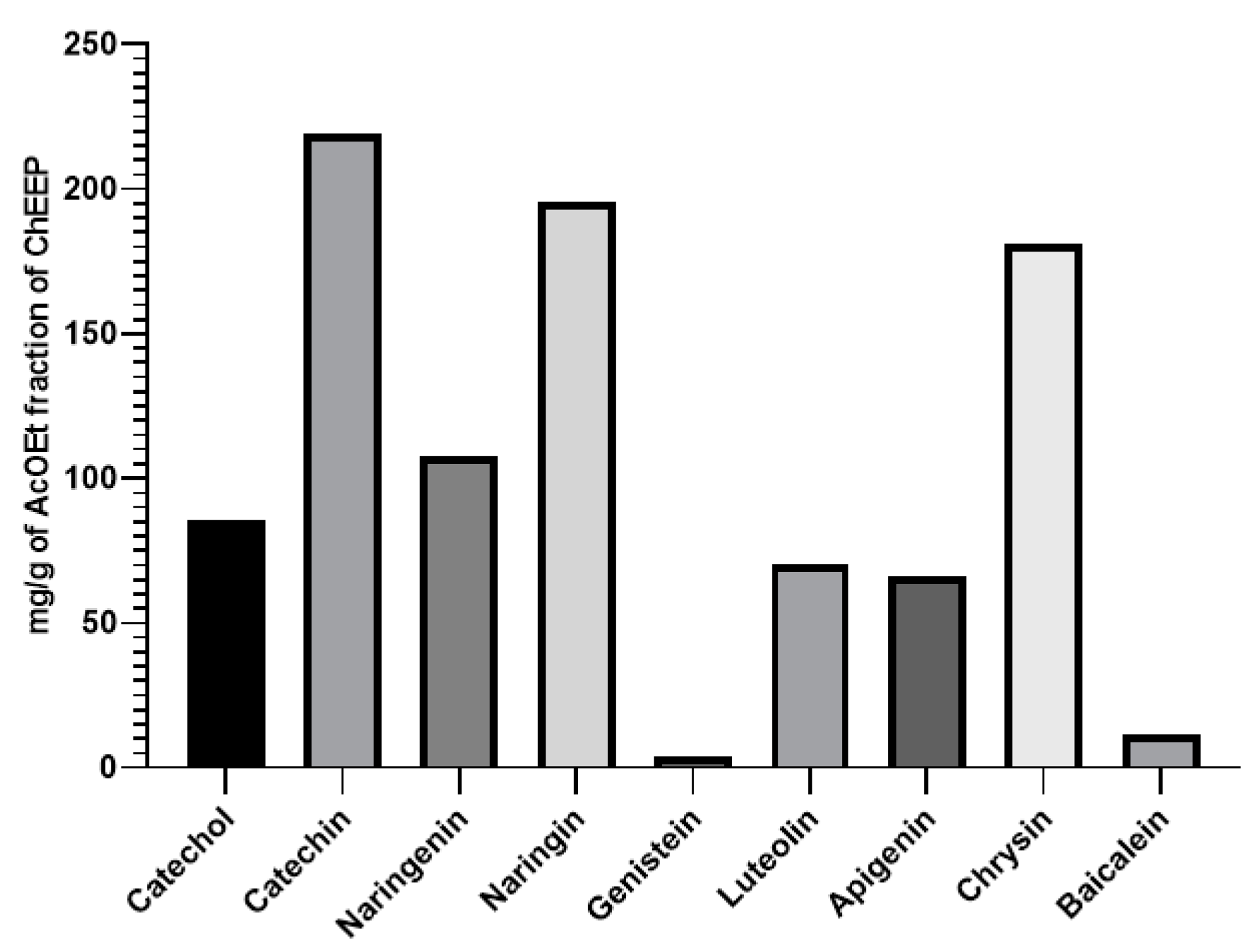
| CatecholPhenol/1–4, 6–12, 14–16, 22–23 | 2.362–2.940 | 85.2983 | 802–894 |
| CatechinFlavonol/1–23 | 2.169–3.434 | 219.024 | 904–982 |
| NaringinFlavanone/2–4, 12–18, 20–23 | 3.968–5.703 | 195.693 | 805–941 |
| NaringeninFlavanone/2–4, 11–23 | 9.968–8.98 | 107.7774 | 823–979 |
| GenisteinIsoflavone/13 | 3.231 | 3.94 | 823 |
| LuteolinFlavone/13, 16–18 | 7.749–9.889 | 70.53 | 829–923 |
| ApigeninFlavone/16–18 | 6.921–7.789 | 66.2 | 843–889 |
| PinocembrinFlavanone/18, 21 | 8.529, 11.873 | 180.97 | 981, 999 |
| ChrysinFlavone/18, 20–22 | 12.165–12.991 | 11.5 | 801–961 |
| CompoundType of Compound/Fraction | Retention Time | Error (ppm) |
|---|---|---|
| KaemferolFlavonol/13, 14, 15, 17, 18 and 19 | 285.0545–285.0671 | −2.94, 3.68, −9.81, −8.16, −6.41 and −8.04 |
| PinocembrinFlavanone/13, 14, 17 and 18 | 255.0461–255.0540 | −11.39, −2.96, 7.68 and 9.37 |
| AcacetinFlavone/13 and 14 | 283.0469–283.0519 | −1.79 and −3.26 |
| GenisteinIsoflavone/15, 16 and 17 | 269.0273–269.0402 | 4.98, −6 and 11.39 |
| ApigeninFlavone/15, 16 and 17 | 269.0646–269.0729 | −11.81, −3.05 and 12.67 |
| BaicaleinFlavone/15, 16 and 17 | 269.0595–269.0731 | 2.94, −1.57 and −9.98 |
| NaringeninFlavanon/18, 19, 20, 21, 22 and 23 | 271.0385–271.0437 | 6.34, 8.55, 3.38, 2.59, 2.92 and −1.81 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Canales-Alvarez, O.; Canales-Martinez, M.M.; Dominguez-Verano, P.; Balderas-Cordero, D.; Madrigal-Bujaidar, E.; Álvarez-González, I.; Rodriguez-Monroy, M.A. Effect of Mexican Propolis on Wound Healing in a Murine Model of Diabetes Mellitus. Int. J. Mol. Sci. 2024, 25, 2201. https://doi.org/10.3390/ijms25042201
Canales-Alvarez O, Canales-Martinez MM, Dominguez-Verano P, Balderas-Cordero D, Madrigal-Bujaidar E, Álvarez-González I, Rodriguez-Monroy MA. Effect of Mexican Propolis on Wound Healing in a Murine Model of Diabetes Mellitus. International Journal of Molecular Sciences. 2024; 25(4):2201. https://doi.org/10.3390/ijms25042201
Chicago/Turabian StyleCanales-Alvarez, Octavio, Maria Margarita Canales-Martinez, Pilar Dominguez-Verano, Daniela Balderas-Cordero, Eduardo Madrigal-Bujaidar, Isela Álvarez-González, and Marco Aurelio Rodriguez-Monroy. 2024. "Effect of Mexican Propolis on Wound Healing in a Murine Model of Diabetes Mellitus" International Journal of Molecular Sciences 25, no. 4: 2201. https://doi.org/10.3390/ijms25042201
APA StyleCanales-Alvarez, O., Canales-Martinez, M. M., Dominguez-Verano, P., Balderas-Cordero, D., Madrigal-Bujaidar, E., Álvarez-González, I., & Rodriguez-Monroy, M. A. (2024). Effect of Mexican Propolis on Wound Healing in a Murine Model of Diabetes Mellitus. International Journal of Molecular Sciences, 25(4), 2201. https://doi.org/10.3390/ijms25042201






