Abnormalities of Oocyte Maturation: Mechanisms and Implications
Abstract
1. Introduction
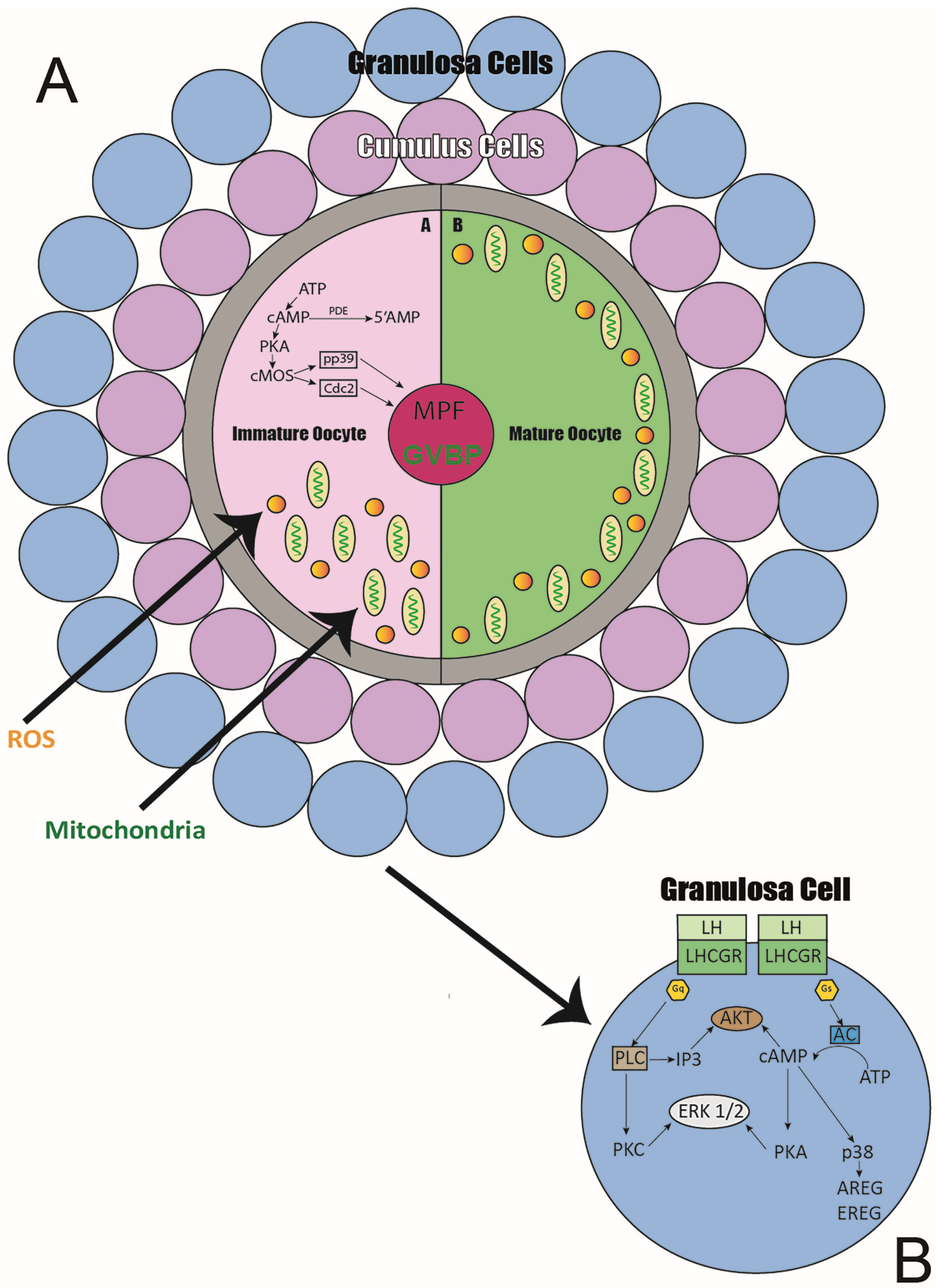
2. Oocyte Maturation—Nuclear Maturation
3. Oocyte Maturation—Cytoplasmic Maturation
4. Oocyte Maturation—Mitochondrial Maturation
5. Maturation of Oocytes—Other Factors Influencing Maturation
6. Materials and Methods
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grettka, K.; Idzik, K.; Lewandowska, K.; Świętek, K.; Palini, S.; Silvestris, F. Ovarian Stem Cells for Women’s Infertility: State of the Art. Biomedicines 2024, 12, 1139. [Google Scholar] [CrossRef]
- McLaren, A. Sex determination in mammals. Oxf. Rev. Reprod. Biol. 1991, 13, 1–33. [Google Scholar] [CrossRef]
- Guo, F.; Yan, L.; Guo, H.; Li, L.; Hu, B.; Zhao, Y.; Yong, J.; Hu, Y.; Wang, X.; Wei, Y.; et al. The Transcriptome and DNA Methylome Landscapes of Human Primordial Germ Cells. Cell 2015, 161, 1437–1452. [Google Scholar] [CrossRef] [PubMed]
- Wolf, U. The molecular genetics of human sex determination. J. Mol. Med. 1995, 73, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, T.; Miyayama, Y.; Fuyuta, M. The origin, migration and fine morphology of human primordial germ cells. Anat. Rec. 1977, 188, 315–329. [Google Scholar] [CrossRef] [PubMed]
- Bolcun-Filas, E.; Handel, M.A. Meiosis: The chromosomal foundation of reproduction. Biol. Reprod. 2018, 99, 112–126. [Google Scholar] [CrossRef]
- Gunes, S.O.; Mahmutoglu, A.M.; Agarwal, A. Genetic and epigenetic effects in sex determination. Birth Defects Res. C Embryo Today 2016, 108, 321–336. [Google Scholar] [CrossRef]
- Zickler, D.; Kleckner, N. Meiosis: Dances Between Homologs. Annu. Rev. Genet. 2023, 57, 1–63. [Google Scholar] [CrossRef]
- Wang, X.; Pepling, M.E. Regulation of meiotic prophase one in mammalian oocytes. Front. Cell Dev. Biol. 2021, 9, 667306. [Google Scholar] [CrossRef]
- Grey, C.; de Massy, B. Coupling crossover and synaptonemal complex in meiosis. Genes Dev. 2022, 36, 4–6. [Google Scholar] [CrossRef]
- Llano, E.; Pendás, A.M. Synaptonemal Complex in Human Biology and Disease. Cells 2023, 12, 1718. [Google Scholar] [CrossRef] [PubMed]
- Stringer, J.M.; Alesi, L.R.; Winship, A.L.; Hutt, K.J. Beyond apoptosis: Evidence of other regulated cellular pathways in the ovary throughout development and life. Hum. Reprod. Update 2023, 29, 434–456. [Google Scholar] [CrossRef] [PubMed]
- Findlay, J.K.; Hutt, K.J.; Hickey, M.; Anderson, R.A. How is the number ofprimordial follicles in the ovarian reserve established? Biol. Reprod. 2015, 93, 111. [Google Scholar] [CrossRef]
- Gondos, B.; Bhiraleus, P.; Hobel, C.J. Ultrastructural observations ongerm cells in human fetal ovaries. Am. J. Obstet. Gynecol. 1971, 110, 644–652. [Google Scholar] [CrossRef]
- Pepling, M.E. Follicular assembly: Mechanisms of action. Reproduction 2012, 143, 139–149. [Google Scholar] [CrossRef]
- Wang, C.; Zhou, B.; Xia, G. Mechanismscontrollinggermlinecyst breakdown and primordial follicle formation. Cell. Mol. Life Sci. 2017, 74, 2547–2566. [Google Scholar] [CrossRef]
- Guigon, C.J.; Cohen-Tannoudji, M. Reconsidérer le rôle de la lignéegerminale dans la différenciation et la fonction de l‘ovaire [Reconsidering the roles of female germ cells in ovarian development and folliculogenesis]. Biol. Aujourdhui 2011, 205, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Hsueh, A.J.W.; Kawamura, K.; Cheng, Y.; Fauser, B.C.J.M. Intraovarian control of early folliculogenesis. Endocr. Rev. 2015, 36, 1–24. [Google Scholar] [CrossRef]
- Kim, J.; You, Y.-J. Oocyte quiescence: From formation to awakening. Endocrinology 2022, 163, bqac049. [Google Scholar] [CrossRef]
- Vaskivuo, T.E.; Anttonen, M.; Herva, R.; Billig, H.; Dorland, M.; Velde, E.R.T.; Stenbäck, F.; Heikinheimo, M.; Tapanainen, J.S. Survival of human ovarian follicles from fetal to adult life: Apoptosis, apoptosis-related proteins, and transcription factor GATA-41. J. Clin. Endocrinol. Metab. 2001, 86, 3421–3429. [Google Scholar] [CrossRef]
- Zhang, Y.; Yan, Z.; Qin, Q.; Nisenblat, V.; Chang, H.-M.; Yu, Y.; Wang, T.; Lu, C.; Yang, M.; Yang, S.; et al. Transcriptome Landscape of Human Folliculogenesis Reveals Oocyte and Granulosa Cell Interactions. Mol. Cell 2018, 72, 1021–1034.e4. [Google Scholar] [CrossRef]
- Gilchrist, R.B.; Ritter, L.J.; Myllymaa, S.; Kaivo-Oja, N.; Dragovic, R.A.; Hickey, T.E.; Ritvos, O.; Mottershead, D.G. Molecular basis of oocyte-paracrine signaling that promotes granulosa cell proliferation. J. Cell Sci. 2006, 119 Pt 18, 3811–3821. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, N.; Yoshioka, N.; Takae, S.; Sugishita, Y.; Tamura, M.; Hashimoto, S.; Morimoto, Y.; Kawamura, K. Successful fertility preservation following ovarian tissue vitrification in patients with primary ovarian insufficiency. Hum. Reprod. 2015, 30, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Warzych, E.; Lipinska, P. Energy metabolism of follicular environment during oocyte growth and maturation. J. Reprod. Dev. 2020, 66, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Heikinheimo, O.; Gibbons, W.E. The molecular mechanisms of oocyte maturation and early embryonic development are unveiling new insights into reproductive medicine. Mol. Hum. Reprod. 1998, 4, 745–756. [Google Scholar] [CrossRef]
- Pan, B.; Li, J. The art of oocyte meiotic arrest regulation. Reprod. Biol. Endocrinol. 2019, 17, 8. [Google Scholar] [CrossRef]
- Sen, A.; Caiazza, F. Oocyte Maturation A story of arrest and release. Front. Biosci. 2013, S5, 451–477. [Google Scholar] [CrossRef]
- Gilchrist, R.B.; Luciano, A.M.; Richani, D.; Zeng, H.T.; Wang, X.; De Vos, M.; Sugimura, S.; Smitz, J.; Richard, F.J.; Thompson, J.G. Oocyte maturation and quality: Role of cyclic nucleotides. Reproduction 2016, 152, R143–R157. [Google Scholar] [CrossRef]
- Törnell, J.; Billig, H.; Hillensjö, T. Regulation of oocyte maturation by changes in ovarian levels of cyclic nucleotides. Hum. Reprod. 1991, 6, 411–422. [Google Scholar] [CrossRef]
- Conti, M.; Andersen, C.B.; Richard, F.; Mehats, C.; Chun, S.-Y.; Horner, K.; Jin, C.; Tsafriri, A. Role of cyclic nucleotide signaling in oocyte maturation. Mol. Cell. Endocrinol. 2002, 187, 153–159. [Google Scholar] [CrossRef]
- Tsafriri, A.; Chun, S.-Y.; Zhang, R.; Hsueh, A.; Conti, M. Oocyte maturation involves compartmentalization and opposing changes of camp levels in follicular somatic and germ cells: Studies using selective phosphodiesterase inhibitors. Dev. Biol. 1996, 178, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Petersen, T.S.; Kristensen, S.G.; Jeppesen, J.V.; Grøndahl, M.L.; Wissing, M.L.; Macklon, K.T.; Andersen, C.Y. Distribution and function of 3′,5′-Cyclic-AMP phosphodiesterases in the human ovary. Mol. Cell. Endocrinol. 2015, 403, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Dekel, N. Cellular, biochemical and molecular mechanisms regulating oocyte maturation. Mol. Cell. Endocrinol. 2005, 234, 19–25. [Google Scholar] [CrossRef]
- Wu, X.-Q.; Zhang, X.; Li, X.-H.; Cheng, H.-H.; Kuai, Y.-R.; Wang, S.; Guo, Y.-L. Translocation of classical PKC and cortical granule exocytosis of the human oocyte in germinal vesicle and metaphase II stage. Acta Pharmacol. Sin. 2006, 27, 1353–1358. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, S.; Basu, D.; Ak, N.; Priyadarshini, A. Molecular mechanism of oocyte maturation. Soc. Reprod. Fertil. Suppl. 2007, 63, 45–55. [Google Scholar]
- Sela-Abramovich, S.; Edry, I.; Galiani, D.; Nevo, N.; Dekel, N. Disruption of gap junctional communication within the ovarian follicle induces oocyte maturation. Endocrinology 2006, 147, 2280–2286. [Google Scholar] [CrossRef]
- Wang, J.; Cao, W.L.; Liu, X.J. Protein kinase A[PKA]-restrictive and PKA-permissive phases of oocyte maturation. Cell Cycle 2006, 5, 213–217. [Google Scholar] [CrossRef][Green Version]
- Wells, D.; Bermudez, M.; Steuerwald, N.; Thornhill, A.; Walker, D.; Malter, H.; Delhanty, J.; Cohen, J. Expression of genes regulating chromosome segregation, the cell cycle and apoptosis during human preimplantation development. Hum. Reprod. 2005, 20, 1339–1348. [Google Scholar] [CrossRef]
- Cadenas, J.; Poulsen, L.C.; Nikiforov, D.; Grøndahl, M.L.; Kumar, A.; Bahnu, K.; Englund, A.L.M.; Malm, J.; Marko-Varga, G.; Pla, I.; et al. Regulation of human oocyte maturation in vivo during the final maturation of follicles. Hum. Reprod. 2023, 38, 686–700. [Google Scholar] [CrossRef]
- Norris, R.P.; Ratzan, W.J.; Freudzon, M.; Mehlmann, L.M.; Krall, J.; Movsesian, M.A.; Wang, H.; Ke, H.; Nikolaev, V.O.; Jaffe, L.A. Cyclic GMP from the surroundings AMP and meiosis in the mouse oocyte. Development 2009, 136, 1869–1878. [Google Scholar] [CrossRef]
- Procházka, R.; Petlach, M.; Nagyová, E.; Němcová, L. Effect of epidermal growth factor-like peptides on pig cumulus cell expansion, oocyte maturation, and acquisition of developmental competence in vitro: Comparison with gonadotropins. Reproduction 2011, 141, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Feuerstein, P.; Cadoret, V.; Dalbies-Tran, R.; Guérif, F.; Royère, D. Le dialogueovocyte-cumulus [Oocyte-cumulusdialog]. Gynecol. Obstet. Fertil. 2006, 34, 793–800. (In French) [Google Scholar] [CrossRef] [PubMed]
- Byskov, A.G.; Andersen, C.Y.; Nordholm, L.; Thogersen, H.; Guoliang, X.; Wassmann, O.; Andersen, J.V.; Guddal, E.; Roed, T. Chemical structure of sterols that activate oocyte meiosis. Nature 1995, 374, 559–562. [Google Scholar] [CrossRef] [PubMed]
- Byskov, A.G.; Andersen, C.Y.; Leonardsen, L. Role of meiosis activating sterols, MAS, in induced oocyte maturation. Mol. Cell. Endocrinol. 2002, 187, 189–196. [Google Scholar] [CrossRef]
- Cadenas, J.; Pors, S.E.; Hansen, C.P.; Olufsen, S.M.; Subiran, C.; Bøtkjær, J.A.; La Cour Poulsen, L.; Fedder, J.; Dueholm, M.; Colmorn, L.B.; et al. Midkinecharacterization in human ovaries: Potential new variants in follicles. F&S Sci. 2023, 4, 294–301. [Google Scholar]
- Gómez, E.; Tarín, J.J.; Pellicer, A. Oocyte maturation in humans: The role of gonadotropins and growth factors. Fertil. Steril. 1993, 60, 40–46. [Google Scholar] [CrossRef]
- Gómez, E.; Santos, M.d.L.; Ruiz, A.; Tarín, J.; Remohí, J.; Pellicer, A. Effects of epidermal growth factor in the final stages of nuclear and cytoplasmic oocyte maturation. Hum. Reprod. 1993, 8, 691–694. [Google Scholar] [CrossRef] [PubMed]
- Kawano, Y.; Narahara, H.; Matsui, N.; Nasu, K.; Miyamura, K.; Miyakawa, I. Insulin-like growth factor-binding protein-1 in human follicular fluid: A marker for oocyte maturation. Gynecol. Obstet. Investig. 1997, 44, 145–148. [Google Scholar] [CrossRef]
- Moor, R.M.; Dai, Y.; Lee, C.; Fulka, J., Jr. Oocyte maturation and embryonic failure. Hum. Reprod. Update 1998, 4, 223–226. [Google Scholar] [CrossRef]
- Barnes, F.L.; Sirard, M.A. Oocyte maturation. Semin. Reprod. Med. 2000, 18, 123–131. [Google Scholar] [CrossRef]
- Hassan, H.A. Clinical assisted reproduction: Cumulus cell contribution to cytoplasmic maturation and oocyte developmental competence in vitro. J. Assist. Reprod. Genet. 2001, 18, 539–543. [Google Scholar] [CrossRef]
- Alvarez Sedó, C.; Miguens, M.; Andreucci, S.; Ortiz, N.; Lorenzi, D.; Papier, S.; Nodar, F. Correlation Between Cytoplasmic Oocyte Maturation and Chromosomal Aneuploidies—Impact on fertilization, embryo quality, and pregnancy. JBRA Assist. Reprod. 2015, 19, 59–65. [Google Scholar] [PubMed]
- Wang, T.-H.; Chang, C.-L.; Wu, H.-M.; Chiu, Y.-M.; Chen, C.-K.; Wang, H.-S. Insulin-like growth factor-II (IGF-II), IGF-binding protein-3 (IGFBP-3), and IGFBP-4 in follicular fluid are associated with oocyte maturation and embryo development. Fertil. Steril. 2006, 86, 1392–1401. [Google Scholar] [CrossRef]
- Adhikari, D.; Lee, I.; Yuen, W.; Carroll, J. Oocytemitochondria—Key regulators of oocyte function and potential therapeutic targets for improving fertility. Biol. Reprod. 2022, 106, 366–377. [Google Scholar] [CrossRef]
- Jiang, Z.; Shen, H. Mitochondria: Emerging therapeutic strategies for oocyte rescue. Reprod. Sci. 2022, 29, 711–722. [Google Scholar] [CrossRef]
- Qi, L.; Chen, X.; Wang, J.; Lv, B.; Zhang, J.; Ni, B.; Xue, Z. Mitochondria: The panacea to improve oocyte quality? Ann. Transl. Med. 2019, 7, 789. [Google Scholar] [CrossRef] [PubMed]
- Kirillova, A.; Smitz, J.E.J.; Sukhikh, G.T.; Mazunin, I. The Role of Mitochondria in Oocyte Maturation. Cells 2021, 10, 2484. [Google Scholar] [CrossRef]
- Schatten, H.; Sun, Q.-Y.; Prather, R. The impact of mitochondrial function/dysfunction on IVF and new treatment possibilities for infertility. Reprod. Biol. Endocrinol. 2014, 12, 111. [Google Scholar] [CrossRef] [PubMed]
- Blerkom, J. Mitochondria in human oogenesis and preimplantation embryogenesis: Engines of metabolism, ionic regulation, and developmental competence. Reproduction 2004, 128, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Chappel, S. The role of mitochondria from mature oocyte to viable blastocyst. Obstet. Gynecol. Int. 2013, 2013, 183024. [Google Scholar] [CrossRef]
- Raad, G.; Tanios, J.; Yarkiner, Z.; Bazzi, M.; Mourad, Y.; Azoury, J.; Fakih, F.; Fakih, C. P-142 Alterations in mitochondrial DNA levels in luteal granulosa cells may affect the morphology of mature oocytes and subsequently their fertilization potential: A retrospective multicenter study. Hum. Reprod. 2023, 38, dead093.506. [Google Scholar] [CrossRef]
- Ge, H.; Tollner, T.L.; Hu, Z.; Dai, M.; Li, X.; Guan, H.; Shan, D.; Zhang, X.; Lv, J.; Huang, C.; et al. The importance of mitochondrial metabolic activity and mitochondrial DNA replication during oocyte maturation in vitro on oocyte quality and subsequent embryo developmental competence. Mol. Reprod. Dev. 2012, 79, 392–401. [Google Scholar] [CrossRef] [PubMed]
- Pasquariello, R.; Ermisch, A.; Silva, E.; McCormick, S.; Logsdon, D.; Barfield, J.; Schoolcraft, W.; Krisher, R. Alterations in oocyte mitochondrial number and function are related to spindle defects and occur with maternal aging in mice and humans. Biol. Reprod. 2018, 100, 971–981. [Google Scholar] [CrossRef] [PubMed]
- Matsuyama, S.; Nakamura, S.; Minabe, S.; Sakatani, M.; Takenouchi, N.; Sasaki, T.; Inoue, Y.; Iwata, H.; Kimura, K. Deterioration of mitochondrial biogenesis and degradation in the endometrium is a cause of subfertility in cows. Mol. Reprod. Dev. 2023, 90, 141–152. [Google Scholar] [CrossRef]
- van der Reest, J.; Cecchino, G.N.; Haigis, M.C.; Kordowitzki, P. Mitochondria: Their relevance during oocyte aging. Aging Res. Rev. 2021, 70, 101378. [Google Scholar] [CrossRef] [PubMed]
- Mihalas, B.P.; Marston, A.L.; Wu, L.E.; Gilchrist, R.B. Reproductive Ageing: Metabolic contribution to age-related chromosome missegregation in mammalian oocytes. Reproduction 2024, 168, e230510. [Google Scholar] [CrossRef] [PubMed]
- Barritt, J.; Brenner, C.; Malter, H.; Cohen, J. Mitochondria in human offspring derived from ooplasmic transplantation. Hum. Reprod. 2001, 16, 513–516. [Google Scholar] [CrossRef]
- Morimoto, Y.; Gamage, U.S.K.; Yamochi, T.; Saeki, N.; Morimoto, N.; Yamanaka, M.; Koike, A.; Miyamoto, Y.; Tanaka, K.; Fukuda, A.; et al. Mitochondrial Transfer into Human Oocytes Improved Embryo Quality and Clinical Outcomes in Recurrent Pregnancy Failure Cases. Int. J. Mol. Sci. 2023, 24, 2738. [Google Scholar] [CrossRef]
- Rodríguez-Varela, C.; Labarta, E. Role of Mitochondria Transfer in Infertility: A Commentary. Cells 2022, 11, 1867. [Google Scholar] [CrossRef]
- Mobarak, H.; Heidarpour, M.; Tsai, P.J.; Rezabakhsh, A.; Rahbarghazi, R.; Nouri, M.; Mahdipour, M. Autologous mitochondrial microinjection; a strategy to improve the oocyte quality and subsequent reproductive outcome during aging. Cell Biosci. 2019, 9, 95. [Google Scholar] [CrossRef]
- Yamada, M.; Sato, S.; Ooka, R.; Akashi, K.; Nakamura, A.; Miyado, K.; Akutsu, H.; Tanaka, M. Mitochondrial replacement by genome transfer in human oocytes: Efficacy, concerns, and legality. Reprod. Med. Biol. 2020, 20, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Gomzikova, M.; James, V.; Rizvanov, A. Mitochondria Donation by Mesenchymal Stem Cells: Current Understanding and Mitochondria Transplantation Strategies. Front. Cell Dev. Biol. 2021, 9, 653322. [Google Scholar] [CrossRef] [PubMed]
- Brenner, C.A.; Barritt, J.A.; Willadsen, S.; Cohen, J. Mitochondrial DNA heteroplasmy after human ooplasmic transplantation. Fertil. Steril. 2000, 74, 573–578. [Google Scholar] [CrossRef]
- Barritt, J.; Brenner, C.; Willadsen, S.; Cohen, J. Spontaneous and artificial changes in human ooplasmic mitochondria. Hum. Reprod. 2000, 15 (Suppl. S2), 207–217. [Google Scholar] [CrossRef]
- Lan, Y.; Zhang, S.; Gong, F.; Lu, C.; Lin, G.; Hu, L. The mitochondrial DNA copy number of cumulus granulosa cells may be related to the maturity of the oocyte cytoplasm. Hum. Reprod. 2020, 35, 1120–1129. [Google Scholar] [CrossRef] [PubMed]
- Novin, M.G.; Allahveisi, A.; Noruzinia, M.; Farhadifar, F.; Yousefian, E.; Fard, A.D.; Salimi, M. The relationship between transcript expression levels of nuclear-encoded [TFAM, NRF1] and mitochondrial-encoded [MT-CO1] genes in single human oocytes during oocyte maturation. Balkan J. Med. Genet. 2015, 18, 39–46. [Google Scholar] [CrossRef][Green Version]
- Bi, C.; Wang, L.; Fan, Y.; Yuan, B.; Alsolami, S.; Zhang, Y.; Zhang, P.; Huang, Y.; Yu, Y.; Belmonte, J.; et al. Quantitative haplotype-resolved analysis of mitochondrial DNA heteroplasmy in Human single oocytes, blastoids, and pluripotent stem cells. Nucleic Acids Res. 2023, 51, 3793–3805. [Google Scholar] [CrossRef]
- Zhang, H.; Esposito, M.; Pezet, M.G.; Aryaman, J.; Wei, W.; Klimm, F.; Calabrese, C.; Burr, S.P.; Macabelli, C.H.; Viscomi, C.; et al. Mitochondrial DNA heteroplasmy is modulated during oocyte development propagating mutation transmission. Sci. Adv. 2021, 7, eabi5657. [Google Scholar] [CrossRef]
- Fan, L.-H.; Wang, Z.-B.; Li, Q.-N.; Meng, T.-G.; Dong, M.-Z.; Hou, Y.; Ouyang, Y.-C.; Schatten, H.; Sun, Q.-Y. Absence of mitochondrial DNA methylation in mouse oocyte maturation, aging and early embryo development. Biochem. Biophys. Res. Commun. 2019, 513, 912–918. [Google Scholar] [CrossRef]
- Steffann, J.; Fallet, C. Mitochondrie et maturation ovocytaire [Mitochondria and oocyte maturation]. J. Gynecol. Obstet. Biol. Reprod. 2010, 39 (Suppl. S1), 11–13. [Google Scholar] [CrossRef]
- Homa, S.; Carroll, J.; Swann, K. Fertilization and early embryology: The role of calcium in mammalian oocyte maturation and egg activation. Hum. Reprod. 1993, 8, 1274–1281. [Google Scholar] [CrossRef]
- Ullah, G.; Jung, P.; Machaca, K. Modeling Ca2+ signaling differentiation during oocyte maturation. Cell Calcium 2007, 42, 556–564. [Google Scholar] [CrossRef]
- Battaglia, D.E.; Klein, N.A.; Soules, M.R. Changes in centrosomal domains during meiotic maturation in the human oocyte. Mol. Hum. Reprod. 1996, 2, 845–851. [Google Scholar] [CrossRef]
- Itskovitz, J.; Rubattu, S.; Rosenwaks, Z.; Liu, H.C.; Sealey, J.E. Relationship of follicular fluid prorenin to oocyte maturation, steroid levels, and outcome of in vitro fertilization. J. Clin. Endocrinol. Metab. 1991, 72, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Llonch, S.; Barragán, M.; Nieto, P.; Mallol, A.; Elosua-Bayes, M.; Lorden, P.; Ruiz, S.; Zambelli, F.; Heyn, H.; Vassena, R.; et al. Single human oocyte transcriptome analysis reveals distinct maturation stage-dependent pathways impacted by age. Aging Cell 2021, 20, e13360. [Google Scholar] [CrossRef] [PubMed]
- Buratini, J.; Dellaqua, T.T.; Carone, D.; Renzini, M.M.; Canto, M.D. Oocyte secreted factors suppress the expression of prostaglandin synthase-2 [PTGS2], a key maturation promoter in cumulus cells: The oocyte is not in a hurry, P-651. Hum. Reprod. 2022, 37 (Suppl. S1), deac107.600. [Google Scholar] [CrossRef]
- Peters, A.E.; Ford, E.A.; Roman, S.D.; Bromfield, E.G.; Nixon, B.; Pringle, K.G.; Sutherland, J.M. Impact of Bisphenol A and its alternatives on oocyte health: A scoping review. Hum. Reprod. Update 2024, 30, 653–691. [Google Scholar] [CrossRef]
- Pan, Z.N.; Zhuang, L.L.; Zhao, H.S.; Yin, S.Y.; Chu, M.; Liu, X.Y.; Bao, H.C. Propylparaben exposure impairs G2/M and meta-phase-anaphase transition during mouse oocyte maturation. Ecotoxicol. Environ. Saf. 2024, 283, 116798. [Google Scholar] [CrossRef] [PubMed]
- Hsia, L.H.; Lee, T.H.; Lin, Y.H.; Huang, Y.Y.; Chang, H.J.; Liu, Y.L. Dual trigger improves the pregnancy rate in fresh in vitro fertili-zation (IVF) cycles compared with the human chorionic gonadotropin (hCG) trigger: A systematic review and meta-analysis of randomized trials. J. Assist. Reprod. Genet. 2023, 40, 2063–2077. [Google Scholar] [CrossRef]
- Gotschel, F.; Sonigo, C.; Becquart, C.; Sellami, I.; Mayeur, A.; Grynberg, M. New Insights on In Vitro Maturation of Oocytes for Fertility Preservation. Int. J. Mol. Sci. 2024, 25, 10605. [Google Scholar] [CrossRef]
- Hatırnaz, Ş.; Hatırnaz, E.; Tan, J.; Çelik, S.; Çalışkan, C.S.; Başbuğ, A.; Aydın, G.; Bahadırlı, A.; Bülbül, M.; Çelik, H.; et al. True empty follicle syndrome is a subtype of oocyte maturation abnormalities. J. Turk. Soc. Obstet. Gynecol. 2024, 21, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Yu, R.; Shi, Q.; Wu, Z.-J.; Li, Q.; Mu, J.; Chen, B.; Shi, J.; Ni, R.; Wu, L.; et al. COX15 deficiency causes oocyte ferroptosis. Proc. Natl. Acad. Sci. USA 2024, 121, e2406174121. [Google Scholar] [CrossRef] [PubMed]
- Hatirnaz, S.; Hatirnaz, E.; Çelik, S.; Çalışkan, C.S.; Tinelli, A.; Malvasi, A.; Sparic, R.; Baldini, D.; Stark, M.; Dahan, M.H. Unraveling the Puzzle: Oocyte Maturation Abnormalities (OMAS). Diagnostics 2022, 12, 2501. [Google Scholar] [CrossRef] [PubMed]
| Factor | Description |
|---|---|
| cAMP (Cyclic Adenosine Monophosphate) | The decrease in intracellular cAMP levels is associated with the resumption of meiosis in the oocyte [28]. |
| PDE (Phosphodiesterase) | An enzyme that degrades cyclic nucleotides such as cAMP, regulating the resumption of meiosis [29]. |
| PKA (Protein Kinase A) | Kinase that regulates oocyte maturation; its inactivation is necessary for GVBD [32,36]. |
| PKG (Protein Kinase G) | Involved in the signaling cascade that regulates meiosis; activated by cGMP [33]. |
| PKC (Protein Kinase C) | Calcium-activated kinase involved in the regulation of oocyte maturation [33]. |
| cGMP (Cyclic Guanosine Monophosphate) | Molecule that, through the regulation of cAMP, participates in the control of oocyte maturation [27]. |
| MPF (Maturation-Promoting Factor) | A kinase complex that promotes oocyte maturation and progression through meiosis [24]. |
| C-mos | Oocyte-specific kinase essential for the activation of MPF during maturation [24]. |
| AC (Adenylate Cyclase C) | An enzyme that catalyzes the conversion of ATP to cAMP, activated by the pre-ovulatory LH surge [35]. |
| VDBP (Vitamin D Binding Protein) | A protein whose role decreases during nuclear maturation in response to the LH surge [35]. |
| Gap Junctions | Cellular connections that break down during maturation, reducing the transfer of cGMP [35]. |
| p34cdc2 Kinase | A subunit of MPF involved in the control of the meiotic cell cycle [24]. |
| Cyclin B | A regulatory subunit of MPF, whose activity is necessary for meiotic progression [24]. |
| Factor | Description |
|---|---|
| cAMP/cGMP regulated by CNP | Low and non-variable CNP levels during the final maturation of the follicle. GDF9 and BMP15 are present in very low concentrations [38,39]. |
| EGF-related peptides (AREG, EREG) | AREG is upregulated during the first 12–17 h of follicular maturation. EGF and IGF-I enhance in vitro oocyte maturation. However, a 6 h incubation with EGF does not affect the cytoplasmic maturation of oocytes obtained after treatment [38,40,45,46]. |
| Growth factors (GDF9, BMP15, MDK) | MDK is upregulated during the first 12–17 h, whereas GDF9 and BMP15 show low influence in regulating oocyte maturation in vivo [38,41,44]. |
| Meiosis-activating sterol (FF-MAS) | Genes regulating the synthesis and metabolism of FF-MAS are significantly controlled to favor accumulation during the first 12–17 h of follicular maturation [42,43]. |
| Insulin-like growth factors (IGF) | Elevated concentrations of IGFBP-1 are correlated with mature oocytes and high embryonic quality. IGF-II, IGFBP-3, and IGFBP-4 are associated with better early embryonic development; PAPP-A is linked to late embryonic development [47,48]. |
| Bidirectional communication oocyte-granulosa | The oocyte relies on granulosa cells for essential nutrients and regulatory signals. Preincubation of oocytes with intact cumulus before ICSI improves treatment outcomes [49,50,53]. |
| Oocyte developmental competence | In vitro matured oocytes from atretic follicles show greater competence for embryonic development compared to those from actively growing follicles [49,51]. |
| Cytoplasmic and chromosomal status of oocytes | Immature oocytes show a high frequency of chromosomal abnormalities and metaphase plate defects compared to mature oocytes [51]. |
| Factor | Description |
|---|---|
| Increase of mtDNA during oocyte maturation | The increase in mtDNA copies and mitochondrial distribution are crucial for oocyte maturation, supporting ATP production [52]. |
| Improvement of oocyte quality with mitochondrial treatments | Targeted treatments and supplements aimed at mitochondria can improve oocyte quality by increasing ATP and reducing oxidative stress [52]. |
| Interaction between mitochondria and nucleus in epigenetic regulation | Mitochondrial metabolites influence epigenetic modifiers, adjusting gene expression to metabolic needs [52]. |
| Correlation between mtDNA, ATP, and oocyte quality | Oocyte quality depends on the amount of mtDNA and ATP; suboptimal in vitro conditions can damage mitochondrial function [54]. |
| Antioxidants and improvement of mitochondrial function | Antioxidants can reduce oxidative stress, improving oocyte quality during maturation [54]. |
| mtDNA defects and failure of oocyte maturation | Quantitative or qualitative mtDNA defects are associated with oocyte maturation failure in reproductive disorders [54]. |
| Increase of mtDNA and decrease of oocyte quality | An excess of mtDNA in granulosa cells is correlated with lower oocyte quality and reduced fertility [55]. |
| Mitochondrial dysfunction in aged oocytes | In aged oocytes, there is reduced mitochondrial activity and increased mtDNA copies, linked to a decline in oocyte quality [56]. |
| Relationship between oocytes and granulosa cells | In aged oocytes, reduced mitochondrial activity and an increase in mtDNA copies are observed, which are associated with a decline in oocyte quality [56]. |
| Correlation between nuclear and mitochondrial genes | During maturation, nuclear and mitochondrial genes show correlated expression, indicating a coordinated regulation of ATP production [58]. |
| Rare mtDNA variants and pre-implantation diagnosis | Rare mtDNA variants in oocytes can affect the pre-implantation diagnosis of mitochondrial diseases [59]. |
| Preferential replication of mtDNA mutations | Some mtDNA mutations promote the replication of mitochondria with high membrane potential, leading to the transmission of pathogenic mutations [60]. |
| Role of mtDNA methylation | mtDNA methylation, not detected during oocyte maturation, could influence gene expression and aging [61]. |
| Selection of mtDNA mutations during gametogenesis | Some mtDNA mutations undergo negative selection during gametogenesis, affecting oocyte maturation at critical levels [62]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baldini, G.M.; Lot, D.; Malvasi, A.; Laganà, A.S.; Vimercati, A.; Dellino, M.; Cicinelli, E.; Baldini, D.; Trojano, G. Abnormalities of Oocyte Maturation: Mechanisms and Implications. Int. J. Mol. Sci. 2024, 25, 12197. https://doi.org/10.3390/ijms252212197
Baldini GM, Lot D, Malvasi A, Laganà AS, Vimercati A, Dellino M, Cicinelli E, Baldini D, Trojano G. Abnormalities of Oocyte Maturation: Mechanisms and Implications. International Journal of Molecular Sciences. 2024; 25(22):12197. https://doi.org/10.3390/ijms252212197
Chicago/Turabian StyleBaldini, Giorgio Maria, Dario Lot, Antonio Malvasi, Antonio Simone Laganà, Antonella Vimercati, Miriam Dellino, Ettore Cicinelli, Domenico Baldini, and Giuseppe Trojano. 2024. "Abnormalities of Oocyte Maturation: Mechanisms and Implications" International Journal of Molecular Sciences 25, no. 22: 12197. https://doi.org/10.3390/ijms252212197
APA StyleBaldini, G. M., Lot, D., Malvasi, A., Laganà, A. S., Vimercati, A., Dellino, M., Cicinelli, E., Baldini, D., & Trojano, G. (2024). Abnormalities of Oocyte Maturation: Mechanisms and Implications. International Journal of Molecular Sciences, 25(22), 12197. https://doi.org/10.3390/ijms252212197








