Metabolomic Insight into Implications of Induction Chemotherapy Followed by Concomitant Chemoradiotherapy in Locally Advanced Head and Neck Cancer
Abstract
:1. Introduction
2. Results
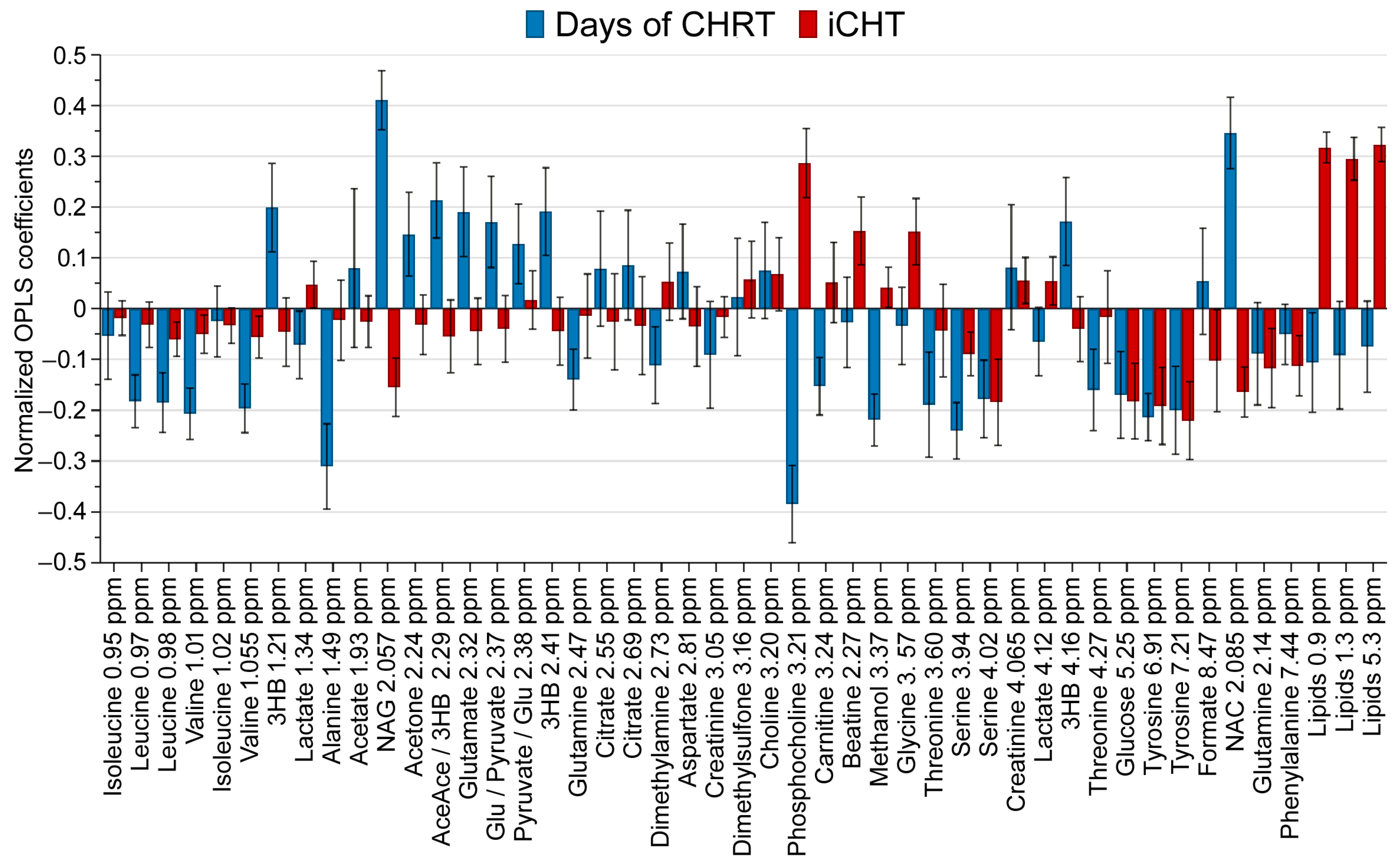
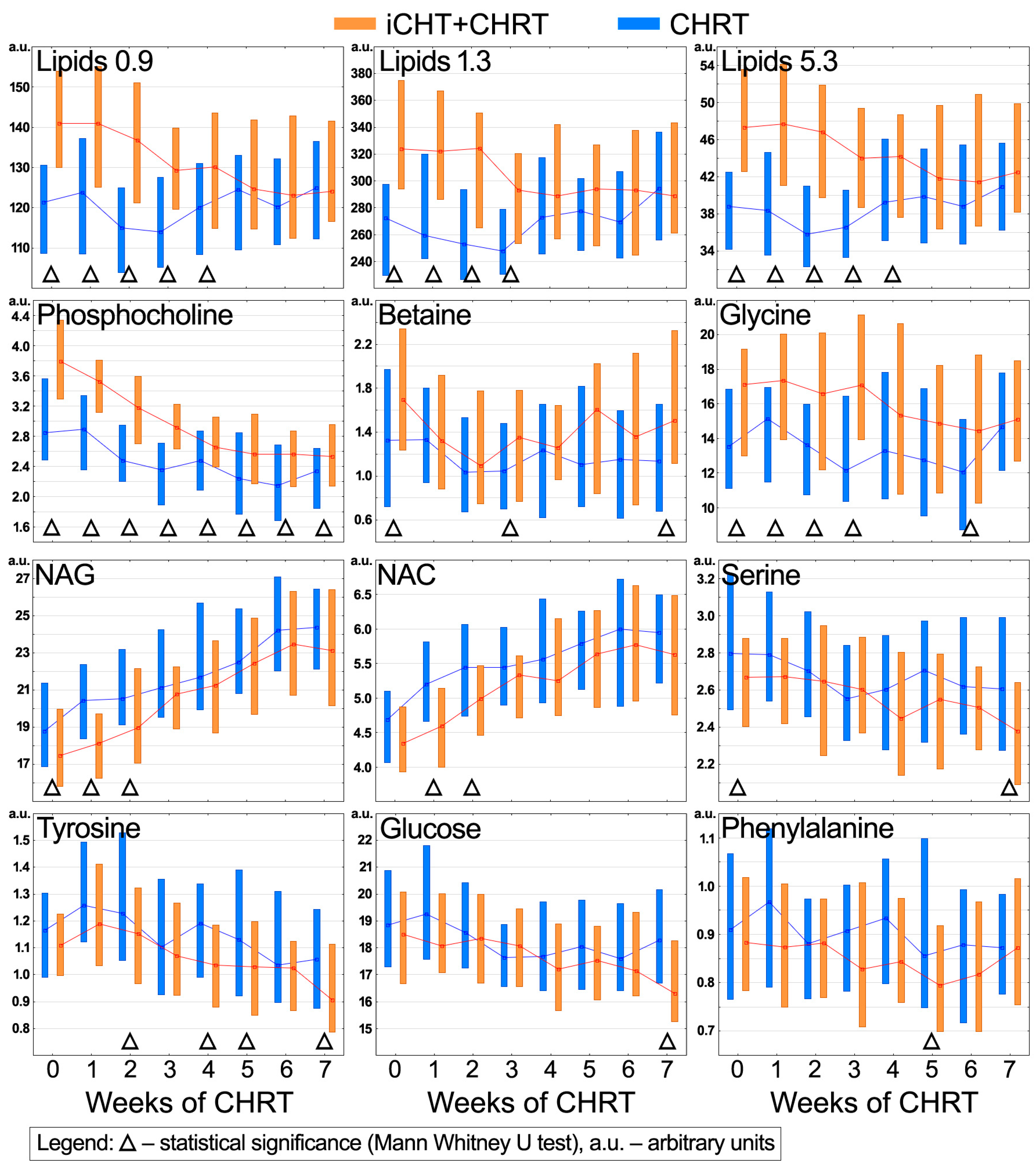
2.1. Influence of Induction Chemotherapy and cCHRT on the Blood Serum Metabolic Profile
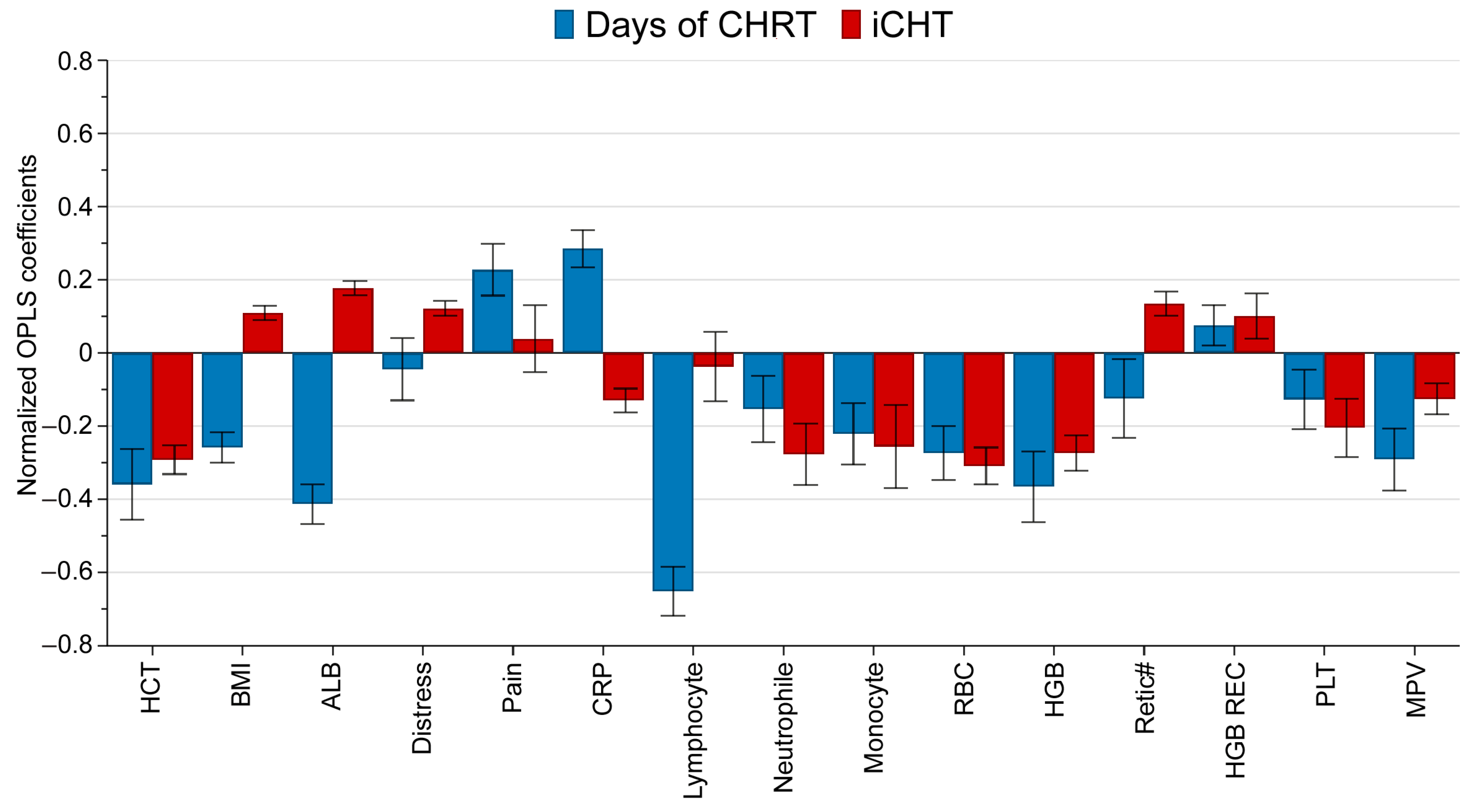
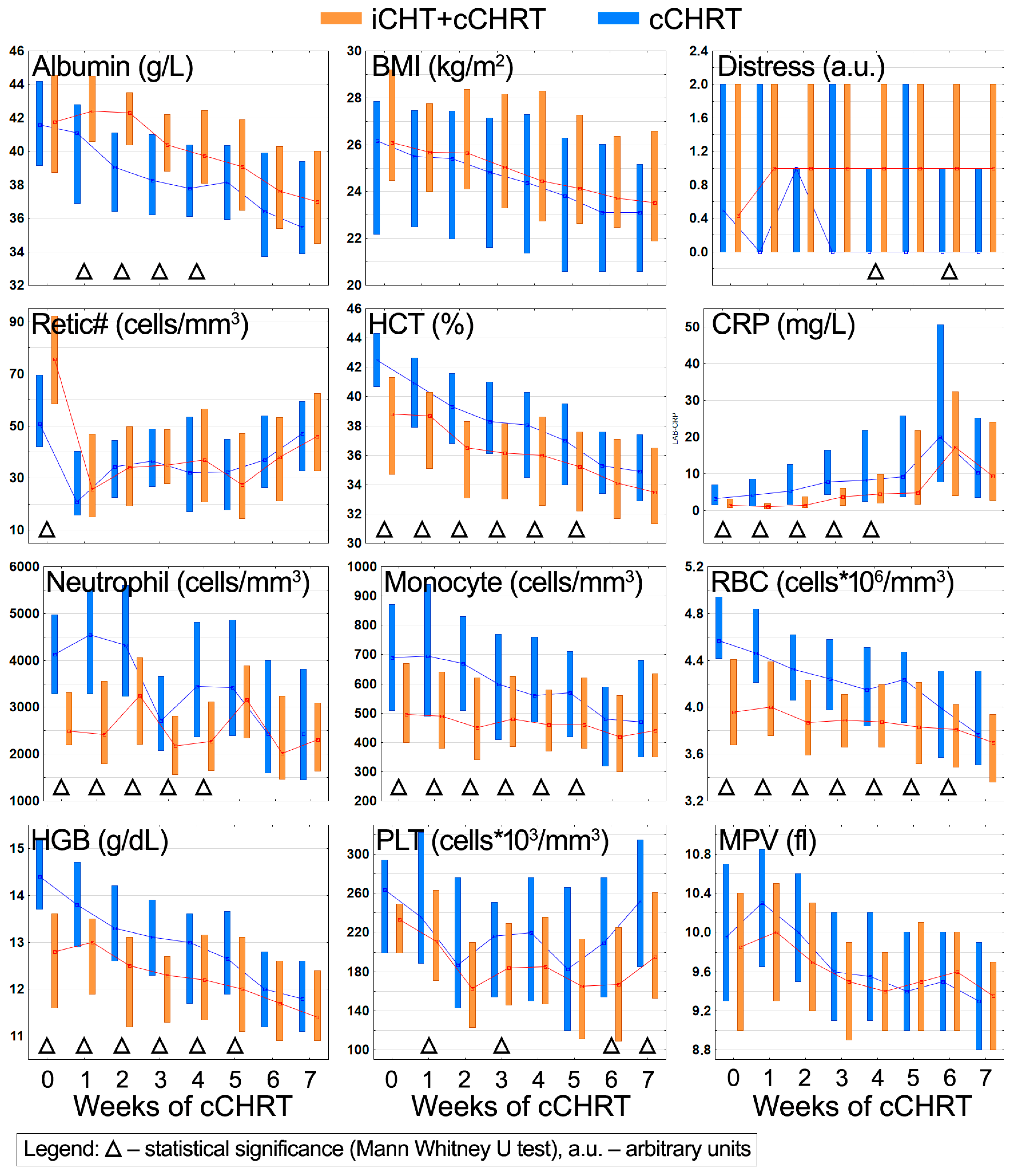
2.2. Influence of Induction Chemotherapy and cCHRT on Clinical Parameters
2.3. Potential Biasing Factors—Tissue Volume Exposure to the Radiation Treatment
3. Discussion
3.1. Direct Impact of iCHT on the Metabolic and Clinical Statuses of the Patients
- Disturbed lipid metabolism (increased blood serum lipids and phospholipids);
- Deregulated folate cycle of one-carbon metabolism (elevated glycine, betaine, lowered serine);
- Downregulated inflammation (lowered NAG, NAC and CRP);
- Ongoing and/or recovery from chemotherapy-induced hematological toxicity (anemia, neutropenia, and monocytopenia).
3.2. iCHT Consequences during the cCHRT Course
- I—iCHT-induced alterations persist throughout the whole cCHRT course;
- II—iCHT-induced alterations vanish during the cCHRT course;
- III—cCHRT enhances iCHT-induced alterations to a significant level, or iCHT intensifies cCHRT-induced alterations.
- Most of the metabolic and clinical alterations induced by iCHT are temporary and disappear during or at the completion of cCHRT;
- The only lasting effect, maintained until at least a week after the end of cCHRT, is a significantly elevated level of phosphocholine;
- iCHT may intensify some of the metabolic and clinical alterations caused by cCHRT (phenylalanine—tyrosine metabolism; thrombocytopenia; distress).
3.3. Limitations of the Study
4. Materials and Methods
4.1. Characteristics of the Patients’ Groups
4.2. Clinical Monitoring of Patients
4.3. Blood Serum Samples Collection
4.4. Serum Sample Preparation for NMR
4.5. NMR Measurement Protocol
4.6. Spectra Post-Processing
4.7. Metabolite Identification and Quantification
4.8. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gau, M.; Karabajakian, A.; Reverdy, T.; Neidhardt, E.M.; Fayette, J. Induction chemotherapy in head and neck cancers: Results and controversies. Oral. Oncol. 2019, 95, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Haddad, R.I.; Posner, M.; Hitt, R.; Cohen, E.E.W.; Schulten, J.; Lefebvre, J.L.; Vermorken, J.B. Induction chemotherapy in locally advanced squamous cell carcinoma of the head and neck: Role, controversy, and future directions. Ann. Oncol. 2018, 29, 1130–1140. [Google Scholar] [CrossRef] [PubMed]
- Vermorken, J.B. Where and when to Use Induction Chemotherapy in Head and Neck Squamous Cell Cancer. In Critical Issues in Head and Neck Oncology; Vermorken, J.B., Budach, V., Leemans, C.R., Machiels, J.P., Nicolai, P., O’Sullivan, B., Eds.; Springer: Cham, Switzerland, 2021; pp. 155–180. [Google Scholar]
- Vidal, L.; Ben Aharon, I.; Limon, D.; Cohen, E.; Popovtzer, A. Role of Induction Chemotherapy Prior to Chemoradiation in Head and Neck Squamous Cell Cancer-Systematic Review and Meta-analysis. Cancer J. 2017, 23, 79–83. [Google Scholar] [CrossRef]
- Albers, A.E.; Grabow, R.; Qian, X.; Jumah, M.D.; Hofmann, V.M.; Krannich, A.; Pecher, G. Efficacy and toxicity of docetaxel combination chemotherapy for advanced squamous cell cancer of the head and neck. Mol. Clin. Oncol. 2017, 7, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Rapidis, A.; Sarlis, N.; Lefebvre, J.L.; Kies, M. Docetaxel in the treatment of squamous cell carcinoma of the head and neck. Ther. Clin. Risk Manag. 2008, 4, 865–886. [Google Scholar] [CrossRef] [PubMed]
- Jin, T.; Qin, W.F.; Jiang, F.; Jin, Q.F.; Wei, Q.C.; Jia, Y.S.; Sun, X.N.; Li, W.F.; Chen, X.Z. Cisplatin and Fluorouracil Induction Chemotherapy with or without Docetaxel in Locoregionally Advanced Nasopharyngeal Carcinoma. Transl. Oncol. 2019, 12, 633–639. [Google Scholar] [CrossRef]
- Peng, H.; Chen, L.; Zhang, Y.; Li, W.F.; Mao, Y.P.; Liu, X.; Zhang, F.; Guo, R.; Liu, L.Z.; Tian, L.; et al. The Tumour Response to Induction Chemotherapy has Prognostic Value for Long-Term Survival Outcomes after Intensity-Modulated Radiation Therapy in Nasopharyngeal Carcinoma. Sci. Rep. 2016, 6, 24835. [Google Scholar] [CrossRef]
- Hsieh, C.Y.; Lein, M.Y.; Yang, S.N.; Wang, Y.C.; Lin, Y.J.; Lin, C.Y.; Hua, C.H.; Tsai, M.H.; Lin, C.C. Dose-dense TPF induction chemotherapy for locally advanced head and neck cancer: A phase II study. BMC Cancer 2020, 20, 832. [Google Scholar] [CrossRef]
- Driessen, C.M.; de Boer, J.P.; Gelderblom, H.; Rasch, C.R.; de Jong, M.A.; Verbist, B.M.; Melchers, W.J.G.; Tesselaar, M.E.T.; van der Graaf, W.T.A.; Kaanders, J.H.A.M.; et al. Induction chemotherapy with docetaxel/cisplatin/5-fluorouracil followed by randomization to two cisplatin-based concomitant chemoradiotherapy schedules in patients with locally advanced head and neck cancer (CONDOR study) (Dutch Head and Neck Society 08-01): A randomized phase II study. Eur. J. Cancer 2016, 52, 77–84. [Google Scholar] [CrossRef]
- Mahdavi, H. Induction chemotherapy in locally advanced head and neck cancers, is there a best choice? Crit. Rev. Oncol. Hematol. 2023, 186, 103986. [Google Scholar] [CrossRef]
- Merlano, M.C.; Denaro, N.; Vecchio, S.; Licitra, L.; Curcio, P.; Benasso, M.; Bagicalupo, A.; Numico, G.; Russi, E.; Corvo, R.; et al. Phase III Randomized Study of Induction Chemotherapy Followed by Definitive Radiotherapy + Cetuximab Versus Chemoradiotherapy in Squamous Cell Carcinoma of Head and Neck: The INTERCEPTOR-GONO Study (NCT00999700). Oncology 2020, 98, 763–770. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.H.; Yen, Y.C.; Liu, S.H.; Yuan, S.P.; Wu, L.L.; Lee, F.P.; Lin, K.C.; Lai, M.T.; Wu, C.C.; Chen, T.M.; et al. Outcomes of Induction Chemotherapy for Head and Neck Cancer Patients: A Combined Study of Two National Cohorts in Taiwan. Medicine 2016, 95, e2845. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.E.W.; Karrison, T.G.; Kocherginsky, M.; Mueller, J.; Egan, R.; Huang, C.H.; Brockstein, B.E.; Agulnik, M.B.; Mittal, B.B.; Yunus, F.; et al. Phase III randomized trial of induction chemotherapy in patients with N2 or N3 locally advanced head and neck cancer. J. Clin. Oncol. 2014, 32, 2735–2743. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, M.C.; Wang, C.C.; Yang, C.C.; Lien, C.F.; Wang, C.C.; Shih, Y.C.; Yeh, S.A.; Hwang, T.Z. The role of induction chemotherapy in patients with locally advanced head and neck squamous cell carcinoma: A nationwide population-based matched study. Oral. Oncol. 2022, 128, 105848. [Google Scholar] [CrossRef] [PubMed]
- Izawa, N.; Onozawa, Y.; Hikosaka, T.; Hamauchi, S.; Tsushima, T.; Todaka, A.; Machida, N.; Haraguchi, Y.; Ogawa, H.; Nishimura, T.; et al. Efficacy and feasibility of docetaxel, cisplatin, and 5-fluorouracil induction chemotherapy for locally advanced head and neck squamous cell carcinoma classified as clinical nodal stage N2c, N3, or N2b with supraclavicular lymph node metastases. Int. J. Clin. Oncol. 2015, 20, 455–462. [Google Scholar] [CrossRef] [PubMed]
- de Bree, R.; Wolf, G.T.; de Keizer, B.; Nixon, I.J.; Hartl, D.M.; Forastiere, A.A.; Haigentz, M., Jr.; Rinaldo, A.; Rodrigo, J.P.; Saba, N.F.; et al. Response assessment after induction chemotherapy for head and neck squamous cell carcinoma: From physical examination to modern imaging techniques and beyond. Head Neck 2017, 39, 2329–2349. [Google Scholar] [CrossRef] [PubMed]
- Perri, F.; Della Vittoria Scarpati, G.; Pontone, M.; Marciano, M.L.; Ottaiano, A.; Cascella, M.; Sabbatino, F.; Guida, A.; Santorsola, M.; Maiolino, P.; et al. Cancer Cell Metabolism Reprogramming and Its Potential Implications on Therapy in Squamous Cell Carcinoma of the Head and Neck: A Review. Cancers 2022, 14, 3560. [Google Scholar] [CrossRef]
- Semrau, S.; Haderlein, M.; Schmidt, D.; Lell, M.; Wolf, W.; Waldfahrer, F.; Uder, M.; Iro, H.; Kuwert, T.; Fietkau, R.; et al. Single-Cycle Induction Chemotherapy Followed by Chemoradiotherapy or Surgery in Patients with Head and Neck Cancer: What are the Best Predictors of Remission and Prognosis? Cancer 2015, 121, 1214–1222. [Google Scholar] [CrossRef]
- Boguszewicz, Ł.; Bieleń, A.; Jarczewski, J.D.; Ciszek, M.; Skorupa, A.; Składowski, K.; Sokół, M. Molecular response to induction chemotherapy and its correlation with treatment outcome in head and neck cancer patients by means of NMR-based metabolomics. BMC Cancer 2021, 21, 410. [Google Scholar] [CrossRef]
- Boguszewicz, Ł.; Bieleń, A.; Ciszek, M.; Wendykier, J.; Szczepanik, K.; Skorupa, A.; Mrochem-Kwarciak, J.; Składowski, K.; Sokół, M. NMR-Based Metabolomics in Investigation of the Radiation Induced Changes in Blood Serum of Head and Neck Cancer Patients and Its Correlation with the Tissue Volumes Exposed to the Particulate Doses. Int. J. Mol. Sci. 2021, 22, 6310. [Google Scholar] [CrossRef]
- Boguszewicz, Ł.; Bieleń, A.; Mrochem-Kwarciak, J.; Skorupa, A.; Ciszek, M.; Heyda, A.; Wygoda, A.; Kotylak, A.; Składowski, K.; Sokół, M. NMR-based metabolomics in real-time monitoring of treatment induced toxicity and cachexia in head and neck cancer: A method for early detection of high risk patients. Metabolomics 2019, 15, 110. [Google Scholar] [CrossRef] [PubMed]
- Beckonert, O.; Keun, H.C.; Ebbels, T.M.; Bundy, J.; Holmes, E.; Lindon, J.C.; Nicholson, J.K. Metabolic profiling, metabolomic and metabonomic procedures for NMR spectroscopy of urine, plasma, serum and tissue extracts. Nat. Protoc. 2007, 2, 2692–2703. [Google Scholar] [CrossRef] [PubMed]
- Nagana Gowda, G.A.; Raftery, D. Analysis of Plasma, Serum, and Whole Blood Metabolites Using 1H NMR Spectroscopy. Methods Mol. Biol. 2019, 2037, 17–34. [Google Scholar] [CrossRef] [PubMed]
- Psychogios, N.; Hau, D.D.; Peng, J.; Guo, A.C.; Mandal, R.; Bouatra, S.; Sinelnikov, I.; Krishnamurthy, R.; Eisner, R.; Gautam, B.; et al. The human serum metabolome. PLoS ONE 2011, 6, e16957. [Google Scholar] [CrossRef] [PubMed]
- Giskeødegård, G.F.; Madssen, T.S.; Euceda, L.R.; Tessem, M.B.; Moestue, S.A.; Bathen, T.F. NMR-based metabolomics of biofluids in cancer. NMR Biomed. 2018, 32, e3927. [Google Scholar] [CrossRef] [PubMed]
- Wold, S.; Sjöström, M.; Eriksson, L. PLS-regression: A basic tool of chemometrics. Chemom. Intell. Lab. Syst. 2001, 58, 109–130. [Google Scholar] [CrossRef]
- Trygg, J.; Wold, S. Orthogonal projections to latent structures (O-PLS). J. Chemom. 2002, 16, 119–128. [Google Scholar] [CrossRef]
- Yang, K.; Zhang, F.; Han, P.; Wang, Z.Z.; Deng, K.; Zhang, Y.Y.; Zhao, W.W.; Song, W.; Cai, Y.Q.; Li, K. Metabolomics approach for predicting response to neoadjuvant chemotherapy for colorectal cancer. Metabolomics 2018, 14, 110. [Google Scholar] [CrossRef]
- Lim, Y.J.; Tonial, N.C.; Hartjes, E.D.; Haig, A.; Velenosi, T.J.; Urquhart, B.L. Metabolomics for the identification of early biomarkers of nephrotoxicity in a mouse model of cisplatin-induced acute kidney injury. Biomed. Pharmacother. 2023, 163, 114787. [Google Scholar] [CrossRef]
- Yonezawa, K.; Nishiumi, S.; Kitamoto-Matsuda, J.; Fujita, T.; Morimoto, K.; Yamashita, D.; Saito, M.; Otsuki, N.; Irino, Y.; Shinohara, M.; et al. Serum and tissue metabolomics of head and neck cancer. Cancer Genom. Proteom. 2013, 10, 233–238, Erratum in Cancer Genom. Proteom. 2014, 11, 215. [Google Scholar]
- Scioscia, K.A.; Snyderman, C.H.; Wagner, R. Altered serum amino acid profiles in head and neck cancer. Nutr. Cancer 1998, 30, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Cobo-Dols, M.; Perez-Miranda, E.; Gil-Calle, S.; Ales-Diaz, I.; Villar-Chamorro, E.; Montesa-Pino, A.; Alcaide GarciaI, J.; Carabante-OcónI, F.; Benavides-Orgaz, M. Changes in the serum amino acids concentrations after first cycle as a factor predictive of tumor response to chemotherapy. Oncologia 2005, 28, 21–28. [Google Scholar] [CrossRef]
- Weinberg, J.M.; Bienholz, A.; Venkatachalam, M.A. The role of glycine in regulated cell death. Cell Mol. Life Sci. 2016, 73, 2285–2308. [Google Scholar] [CrossRef] [PubMed]
- Pan, S.; Fan, M.; Liu, Z.; Li, X.; Wang, H. Serine, glycine and one-carbon metabolism in cancer (Review). Int. J. Oncol. 2021, 58, 158–170. [Google Scholar] [CrossRef] [PubMed]
- Lionaki, E.; Ploumi, C.; Tavernarakis, N. One-Carbon Metabolism: Pulling the Strings behind Aging and Neurodegeneration. Cells 2022, 11, 214. [Google Scholar] [CrossRef] [PubMed]
- Locasale, J.W. Serine, glycine and one-carbon units: Cancer metabolism in full circle. Nat. Rev. Cancer 2013, 13, 572–583. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.N.; Dey, A.K.; Maddineni, R.; Kraus, W.E.; Huffman, K.M. GlycA measured by NMR spectroscopy is associated with disease activity and cardiovascular disease risk in chronic inflammatory diseases. Am. J. Prev. Cardiol. 2020, 4, 100120. [Google Scholar] [CrossRef] [PubMed]
- Connelly, M.A.; Otvos, J.D.; Shalaurova, I.; Playford, M.P.; Mehta, N.N. GlycA, a novel biomarker of systemic inflammation and cardiovascular disease risk. J. Transl. Med. 2017, 15, 219. [Google Scholar] [CrossRef]
- Boguszewicz, Ł.; Hajduk, A.; Mrochem-Kwarciak, J.; Skorupa, A.; Ciszek, M.; Heyda, A.; Składowski, K.; Sokół, M. 1H NMR based metabolomic approach to monitoring of the head and neck cancer treatment toxicity. Metabolomics 2016, 12, 102. [Google Scholar] [CrossRef]
- Tenório, M.C.D.S.; Graciliano, N.G.; Moura, F.A.; Oliveira, A.C.M.; Goulart, M.O.F. N-Acetylcysteine (NAC): Impacts on Human Health. Antioxidants 2021, 10, 967. [Google Scholar] [CrossRef]
- Lazzari, G.; Silvano, G. From Anemia to Erythropoietin Resistance in Head and Neck Squamous Cell Carcinoma Treatment: A Carousel Driven by Hypoxia. Onco Targets Ther. 2020, 13, 841–851. [Google Scholar] [CrossRef]
- Patysheva, M.; Frolova, A.; Larionova, I.; Afanas’ev, S.; Tarasova, A.; Cherdyntseva, N.; Kzhyshkowska, J. Monocyte programming by cancer therapy. Front. Immunol. 2022, 13, 994319. [Google Scholar] [CrossRef] [PubMed]
- Kondo, M.; Oshita, F.; Kato, Y.; Yamada, K.; Nomura, I.; Noda, K. Early monocytopenia after chemotherapy as a risk factor for neutropenia. Am. J. Clin. Oncol. 1999, 22, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Gao, L.; Xu, C.; Chu, L.; Gao, L.; Wu, R.; Liu, Y.; Liu, T.; Sun, X.J.; Ren, R. ARHGEF12 regulates erythropoiesis and is involved in erythroid regeneration after chemotherapy in acute lymphoblastic leukemia patients. Haematologica 2020, 105, 925–936. [Google Scholar] [CrossRef]
- Huang, W.; Fan, Y.; Cheng, X.; Liang, H.; Pan, H.; Xiao, T.; Chen, M.; Guan, J. A preliminary Study on the Effect of Head and Neck Chemoradiotherapy on Systematic Immunity. Dose Response 2019, 17, 1559325819884186. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, H.; Sakakura, K.; Mito, I.; Ida, S.; Chikamatsu, K. Dynamic changes in immune cell profile in head and neck squamous cell carcinoma: Immunomodulatory effects of chemotherapy. Cancer Sci. 2016, 107, 1065–1071. [Google Scholar] [CrossRef]
- Liu, P.; Wu, J.; Yu, X.; Guo, L.; Zhao, L.; Ban, T.; Huang, Y. Metabolomics and Network Analyses Reveal Phenylalanine and Tyrosine as Signatures of Anthracycline-Induced Hepatotoxicity. Pharmaceuticals 2023, 16, 797. [Google Scholar] [CrossRef]
- Feng, Y.; Feng, Y.; Gu, L.; Liu, P.; Cao, J.; Zhang, S. The Critical Role of Tetrahydrobiopterin (BH4) Metabolism in Modulating Radiosensitivity: BH4/NOS Axis as an Angel or a Devil. Front. Oncol. 2021, 11, 720632. [Google Scholar] [CrossRef]
- Felger, J.C.; Li, L.; Marvar, P.J.; Woolwine, B.J.; Harrison, D.G.; Raison, C.L.; Miller, A.H. Tyrosine metabolism during interferon-alpha administration: Association with fatigue and CSF dopamine concentrations. Brain Behav. Immun. 2013, 31, 153–160. [Google Scholar] [CrossRef]
- Willson, K.J.; Nott, L.M.; Broadbridge, V.T.; Price, T. Hepatic encephalopathy associated with cancer or anticancer therapy. Gastrointest. Cancer Res. 2013, 6, 11–16. [Google Scholar]
- Dainiak, N. Hematologic consequences of exposure to ionizing radiation. Exp. Hematol. 2002, 30, 513–528. [Google Scholar] [CrossRef] [PubMed]
- Pytel, A.; Zielińska, A.; Staś, J.; Chabowski, M. Quality of Life, Psychological Distress, and Nutritional Status of Polish Patients with Head and Neck Cancer Treated with Radiotherapy. J. Clin. Med. 2023, 12, 659. [Google Scholar] [CrossRef] [PubMed]
- Hajduk, A.; Składowski, K.; Boguszewicz, Ł.; Mrochem-Kwarciak, J.; Hutnik, M.; Lukaszczyk-Wideł, B.; Rutkowski, T.; Wygoda, A.; Przeorek, W.; Goleń, M.; et al. Acute radiation sequelae evaluation in head and neck cancer patients. A new concept of comprehensive scoring system—Multiparametric monitoring. Eur. Arch. Otorhinolaryngol. 2012, 269, 1357. [Google Scholar]
- Donovan, K.A.; Grassi, L.; McGinty, H.L.; Jacobsen, P.B. Validation of the distress thermometer worldwide: State of the science. Psychooncology 2014, 23, 241–250. [Google Scholar] [CrossRef]
- Jensen, M.P.; McFarland, C.A. Increasing the reliability and validity of pain intensity measurement in chronic pain patients. Pain 1993, 55, 195–203. [Google Scholar] [CrossRef]
| cCHRT | iCHT + cCHRT | |
|---|---|---|
| Number of patients | 53 | 54 |
| Age (median) | 60 (41–75) | 55 (22–71) |
| Sex | ||
| M | 43 | 38 |
| F | 10 | 16 |
| TNM stage | ||
| II | 3 | |
| III | 12 | 10 |
| IV | 38 | 44 |
| Tumor localization | ||
| Larynx | 22 | 12 |
| Oropharynx | 15 | 18 |
| Hypopharynx | 13 | 11 |
| Nasopharynx | 3 | 13 |
| HPV status | ||
| Positive | 1 | 0 |
| Negative | 52 | 54 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boguszewicz, Ł.; Bieleń, A.; Ciszek, M.; Skorupa, A.; Mrochem-Kwarciak, J.; Składowski, K.; Sokół, M. Metabolomic Insight into Implications of Induction Chemotherapy Followed by Concomitant Chemoradiotherapy in Locally Advanced Head and Neck Cancer. Int. J. Mol. Sci. 2024, 25, 188. https://doi.org/10.3390/ijms25010188
Boguszewicz Ł, Bieleń A, Ciszek M, Skorupa A, Mrochem-Kwarciak J, Składowski K, Sokół M. Metabolomic Insight into Implications of Induction Chemotherapy Followed by Concomitant Chemoradiotherapy in Locally Advanced Head and Neck Cancer. International Journal of Molecular Sciences. 2024; 25(1):188. https://doi.org/10.3390/ijms25010188
Chicago/Turabian StyleBoguszewicz, Łukasz, Agata Bieleń, Mateusz Ciszek, Agnieszka Skorupa, Jolanta Mrochem-Kwarciak, Krzysztof Składowski, and Maria Sokół. 2024. "Metabolomic Insight into Implications of Induction Chemotherapy Followed by Concomitant Chemoradiotherapy in Locally Advanced Head and Neck Cancer" International Journal of Molecular Sciences 25, no. 1: 188. https://doi.org/10.3390/ijms25010188
APA StyleBoguszewicz, Ł., Bieleń, A., Ciszek, M., Skorupa, A., Mrochem-Kwarciak, J., Składowski, K., & Sokół, M. (2024). Metabolomic Insight into Implications of Induction Chemotherapy Followed by Concomitant Chemoradiotherapy in Locally Advanced Head and Neck Cancer. International Journal of Molecular Sciences, 25(1), 188. https://doi.org/10.3390/ijms25010188






