Serum Calretinin and Genetic Variability as a Prognostic and Predictive Factor in Malignant Mesothelioma
Abstract
:1. Introduction
2. Results
2.1. Patients’ Characteristics and Genotype Frequencies
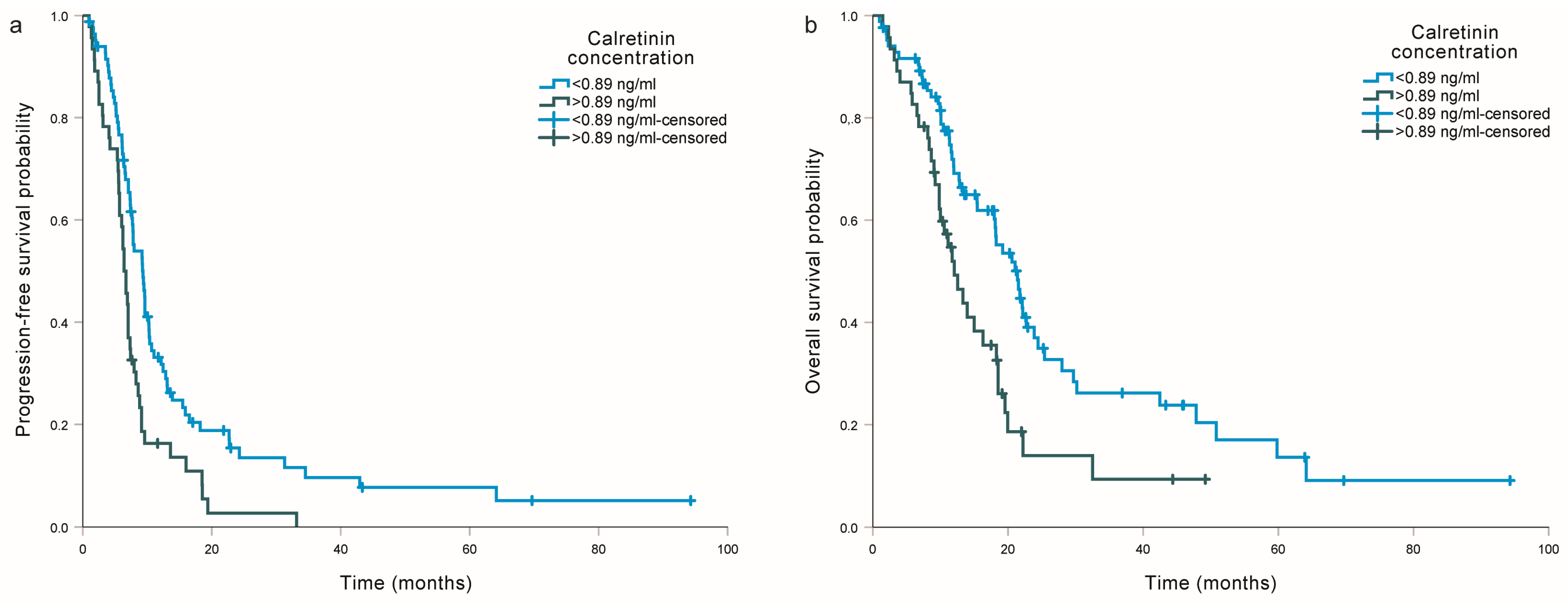
2.2. Association of Calretinin with Progression-Free Survival and Overall Survival from Diagnosis
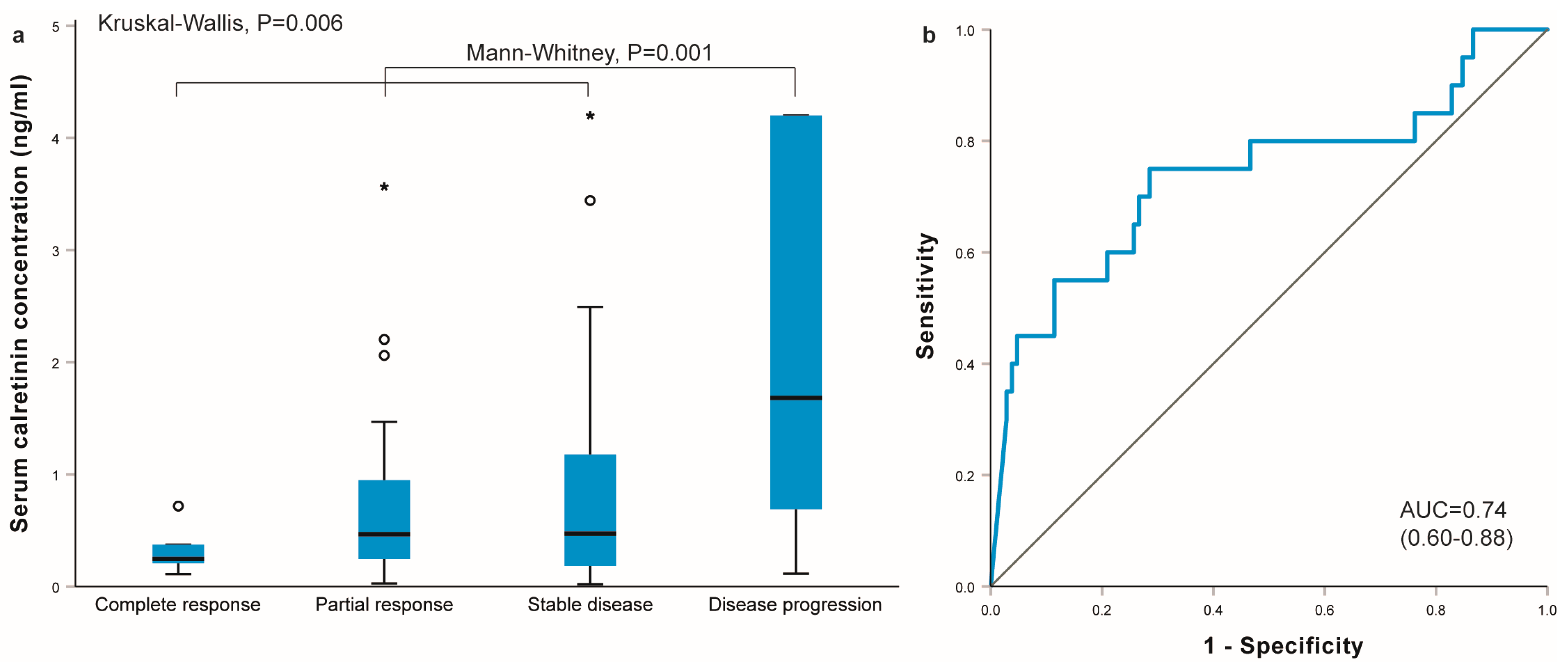
2.3. Association of Calretinin with the Outcome of Cisplatin-Based Chemotherapy
2.4. Association of Calretinin with Progression-Free Survival and Overall Survival from the Beginning of Chemotherapy
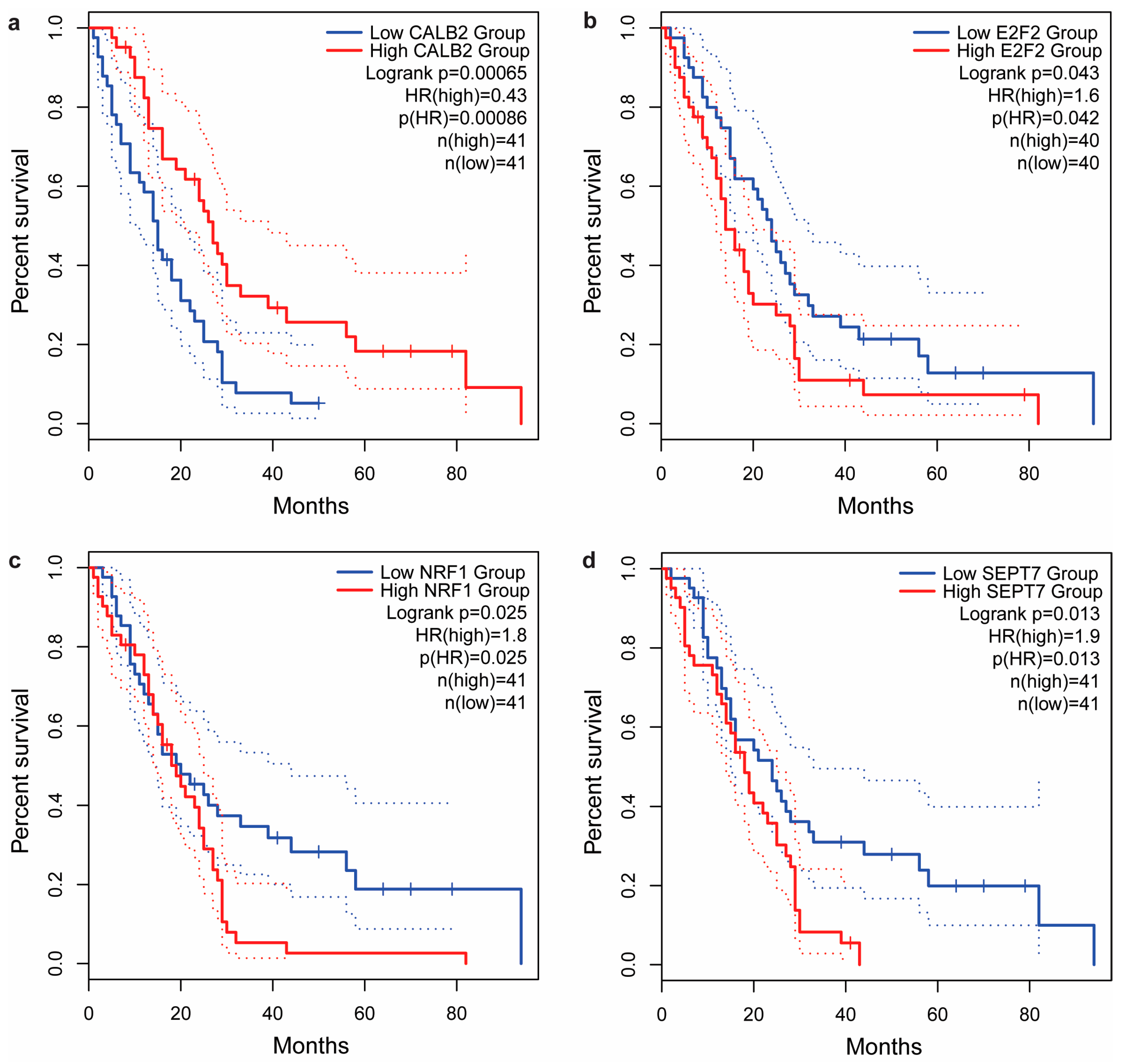
2.5. In Silico Analysis of Tumor Tissue mRNA Expression
3. Discussion
4. Materials and Methods
4.1. Study Population
4.2. Treatment Response and Survival Assessment
4.3. Single-Nucleotide Polymorphism (SNP) Selection, DNA Extraction, and Genotyping
4.4. Measurement of Serum Calretinin
4.5. Bioinformatic Analysis: Tissue Gene Expression
4.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Štrbac, D.; Dolžan, V. Novel and Future Treatment Options in Mesothelioma: A Systematic Review. Int. J. Mol. Sci. 2022, 23, 1975. [Google Scholar] [CrossRef]
- He, J.; Xu, S.; Pan, H.; Li, S.; He, J. Does size matter?—A population-based analysis of malignant pleural mesothelioma. Transl. Lung Cancer Res. 2020, 9, 1041–1052. [Google Scholar] [CrossRef]
- Kovac, V.; Zwitter, M.; Zagar, T. Improved survival after introduction of chemotherapy for malignant pleural mesothelioma in Slovenia: Population-based survey of 444 patients. Radiol. Oncol. 2012, 46, 136–144. [Google Scholar] [CrossRef]
- Rondon, L.; Fu, R.; Patel, M.R. Success of Checkpoint Blockade Paves the Way for Novel Immune Therapy in Malignant Pleural Mesothelioma. Cancers 2023, 15, 2940. [Google Scholar] [CrossRef] [PubMed]
- Deiana, C.; Fabbri, F.; Tavolari, S.; Palloni, A.; Brandi, G. Improvements in Systemic Therapies for Advanced Malignant Mesothelioma. Int. J. Mol. Sci. 2023, 24, 10415. [Google Scholar] [CrossRef] [PubMed]
- Chevallier, M.; Kim, F.; Friedlaender, A.; Addeo, A. Pleural Mesothelioma in the Era of Immunotherapy. Clin. Med. Insights Oncol. 2023, 17, 11795549231178173. [Google Scholar] [CrossRef] [PubMed]
- Cristaudo, A.; Bonotti, A.; Guglielmi, G.; Fallahi, P.; Foddis, R. Serum mesothelin and other biomarkers: What have we learned in the last decade? J. Thorac. Dis. 2018, 10, S353–S359. [Google Scholar] [CrossRef]
- Pass, H.I.; Levin, S.M.; Harbut, M.R.; Melamed, J.; Chiriboga, L.; Donington, J.; Huflejt, M.; Carbone, M.; Chia, D.; Goodglick, L.; et al. Fibulin-3 as a blood and effusion biomarker for pleural mesothelioma. N. Engl. J. Med. 2012, 367, 1417–1427. [Google Scholar] [CrossRef]
- Kovac, V.; Dodic-Fikfak, M.; Arneric, N.; Dolzan, V.; Franko, A. Fibulin-3 as a biomarker of response to treatment in malignant mesothelioma. Radiol. Oncol. 2015, 49, 279–285. [Google Scholar] [CrossRef]
- Schillebeeckx, E.; van Meerbeeck, J.P.; Lamote, K. Clinical utility of diagnostic biomarkers in malignant pleural mesothelioma: A systematic review and meta-analysis. Eur. Respir. Rev. 2021, 30, 210057. [Google Scholar] [CrossRef]
- Barone, E.; Gemignani, F.; Landi, S. Overexpressed genes in malignant pleural mesothelioma: Implications in clinical management. J. Thorac. Dis. 2018, 10, S369–S382. [Google Scholar] [CrossRef] [PubMed]
- Goricar, K.; Dolzan, V.; Lenassi, M. Extracellular Vesicles: A Novel Tool Facilitating Personalized Medicine and Pharmacogenomics in Oncology. Front. Pharmacol. 2021, 12, 671298. [Google Scholar] [CrossRef] [PubMed]
- Goričar, K.; Holcar, M.; Mavec, N.; Kovač, V.; Lenassi, M.; Dolžan, V. Extracellular Vesicle Enriched miR-625-3p Is Associated with Survival of Malignant Mesothelioma Patients. J. Pers. Med. 2021, 11, 1014. [Google Scholar] [CrossRef]
- Blum, W.; Pecze, L.; Rodriguez, J.W.; Steinauer, M.; Schwaller, B. Regulation of calretinin in malignant mesothelioma is mediated by septin 7 binding to the CALB2 promoter. BMC Cancer 2018, 18, 475. [Google Scholar] [CrossRef] [PubMed]
- Wörthmüller, J.; Salicio, V.; Oberson, A.; Blum, W.; Schwaller, B. Modulation of Calretinin Expression in Human Mesothelioma Cells Reveals the Implication of the FAK and Wnt Signaling Pathways in Conferring Chemoresistance towards Cisplatin. Int. J. Mol. Sci. 2019, 20, 5391. [Google Scholar] [CrossRef]
- Casjens, S.; Johnen, G.; Raiko, I.; Pesch, B.; Taeger, D.; Töpfer, C.; Schonefeld, S.; Moebus, S.; Jöckel, K.-H.; Brüning, T.; et al. Re-evaluation of potential predictors of calretinin and mesothelin in a population-based cohort study using assays for the routine application in clinical medicine. BMJ Open 2021, 11, e039079. [Google Scholar] [CrossRef] [PubMed]
- Greening, D.W.; Ji, H.; Chen, M.; Robinson, B.W.S.; Dick, I.M.; Creaney, J.; Simpson, R.J. Secreted primary human malignant mesothelioma exosome signature reflects oncogenic cargo. Sci. Rep. 2016, 6, 32643. [Google Scholar] [CrossRef]
- Zupanc, C.; Franko, A.; Štrbac, D.; Dodič Fikfak, M.; Kovač, V.; Dolžan, V.; Goričar, K. Serum Calretinin as a Biomarker in Malignant Mesothelioma. J. Clin. Med. 2021, 10, 4875. [Google Scholar] [CrossRef]
- Aguilar-Madrid, G.; Pesch, B.; Calderón-Aranda, E.S.; Burek, K.; Jiménez-Ramírez, C.; Juárez-Pérez, C.A.; Ochoa-Vázquez, M.D.; Torre-Bouscoulet, L.; Acosta-Saavedra, L.C.; Sada-Ovalle, I.; et al. Biomarkers for Predicting Malignant Pleural Mesothelioma in a Mexican Population. Int. J. Med. Sci. 2018, 15, 883–891. [Google Scholar] [CrossRef]
- Johnen, G.; Gawrych, K.; Raiko, I.; Casjens, S.; Pesch, B.; Weber, D.G.; Taeger, D.; Lehnert, M.; Kollmeier, J.; Bauer, T.; et al. Calretinin as a blood-based biomarker for mesothelioma. BMC Cancer 2017, 17, 386. [Google Scholar] [CrossRef]
- Linton, A.; Pavlakis, N.; O’Connell, R.; Soeberg, M.; Kao, S.; Clarke, S.; Vardy, J.; van Zandwijk, N. Factors associated with survival in a large series of patients with malignant pleural mesothelioma in New South Wales. Br. J. Cancer 2014, 111, 1860–1869. [Google Scholar] [CrossRef] [PubMed]
- Thapa, B.; Walkiewicz, M.; Murone, C.; Asadi, K.; Deb, S.; Barnett, S.; Knight, S.; Mitchell, P.; Liew, D.; Watkins, D.N.; et al. Calretinin but not caveolin-1 correlates with tumour histology and survival in malignant mesothelioma. Pathology 2016, 48, 660–665. [Google Scholar] [CrossRef] [PubMed]
- Kao, S.C.; Klebe, S.; Henderson, D.W.; Reid, G.; Chatfield, M.; Armstrong, N.J.; Yan, T.D.; Vardy, J.; Clarke, S.; van Zandwijk, N.; et al. Low calretinin expression and high neutrophil-to-lymphocyte ratio are poor prognostic factors in patients with malignant mesothelioma undergoing extrapleural pneumonectomy. J. Thorac. Oncol. 2011, 6, 1923–1929. [Google Scholar] [CrossRef] [PubMed]
- Link, T.; Passek, S.; Wimberger, P.; Frank, K.; Vassileva, Y.D.; Kramer, M.; Kuhlmann, J.D. Serum calretinin as an independent predictor for platinum resistance and prognosis in ovarian cancer. Int. J. Cancer 2020, 146, 2608–2618. [Google Scholar] [CrossRef] [PubMed]
- Casjens, S.; Weber, D.G.; Johnen, G.; Raiko, I.; Taeger, D.; Meinig, C.; Moebus, S.; Jöckel, K.H.; Brüning, T.; Pesch, B. Assessment of potential predictors of calretinin and mesothelin to improve the diagnostic performance to detect malignant mesothelioma: Results from a population-based cohort study. BMJ Open 2017, 7, e017104. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Wang, B.; Long, H.; Wen, F. Diagnostic accuracy of calretinin for malignant mesothelioma in serous effusions: A meta-analysis. Sci. Rep. 2015, 5, 9507. [Google Scholar] [CrossRef] [PubMed]
- Kresoja-Rakic, J.; Kapaklikaya, E.; Ziltener, G.; Dalcher, D.; Santoro, R.; Christensen, B.C.; Johnson, K.C.; Schwaller, B.; Weder, W.; Stahel, R.A.; et al. Identification of cis- and trans-acting elements regulating calretinin expression in mesothelioma cells. Oncotarget 2016, 7, 21272–21286. [Google Scholar] [CrossRef] [PubMed]
- Tavazoie, S.F.; Alarcon, C.; Oskarsson, T.; Padua, D.; Wang, Q.; Bos, P.D.; Gerald, W.L.; Massague, J. Endogenous human microRNAs that suppress breast cancer metastasis. Nature 2008, 451, 147–152. [Google Scholar] [CrossRef]
- Lehnert, M.; Weber, D.G.; Taeger, D.; Raiko, I.; Kollmeier, J.; Stephan-Falkenau, S.; Brüning, T.; Johnen, G.; Brik, A.; Burek, K.; et al. Determinants of plasma calretinin in patients with malignant pleural mesothelioma. BMC Res. Notes 2020, 13, 359. [Google Scholar] [CrossRef]
- Chapel, D.B.; Schulte, J.J.; Husain, A.N.; Krausz, T. Application of immunohistochemistry in diagnosis and management of malignant mesothelioma. Transl. Lung Cancer Res. 2020, 9, S3–S27. [Google Scholar] [CrossRef]
- Chirieac, L.R.; Pinkus, G.S.; Pinkus, J.L.; Godleski, J.; Sugarbaker, D.J.; Corson, J.M. The immunohistochemical characterization of sarcomatoid malignant mesothelioma of the pleura. Am. J. Cancer Res. 2011, 1, 14–24. [Google Scholar] [PubMed]
- Calthorpe, L.; Romero-Hernandez, F.; Miller, P.; Conroy, P.C.; Hirose, K.; Kim, A.; Kirkwood, K.; Nakakura, E.; Corvera, C.; Maker, A.V.; et al. Contemporary Trends in Malignant Peritoneal Mesothelioma: Incidence and Survival in the United States. Cancers 2022, 15, 229. [Google Scholar] [CrossRef] [PubMed]
- Shen, S.; Wei, Y.; Li, Y.; Duan, W.; Dong, X.; Lin, L.; You, D.; Tardon, A.; Chen, C.; Field, J.K.; et al. A multi-omics study links TNS3 and SEPT7 to long-term former smoking NSCLC survival. NPJ Precis. Oncol. 2021, 5, 39. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Fei, F.; Qu, J.; Li, C.; Li, Y.; Zhang, S. The role of septin 7 in physiology and pathological disease: A systematic review of current status. J. Cell Mol. Med. 2018, 22, 3298–3307. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Liu, L.; Fan, N.; Zhang, Q.; Wang, W.; Zheng, M.; Ma, L.; Li, Y.; Shi, L. The requirement of SEPT2 and SEPT7 for migration and invasion in human breast cancer via MEK/ERK activation. Oncotarget 2016, 7, 61587–61600. [Google Scholar] [CrossRef]
- Zupanc, C.; Franko, A.; Štrbac, D.; Dodič Fikfak, M.; Kovač, V.; Dolžan, V.; Goričar, K. Genetic factors influence serum calretinin levels in asbestos-related diseases. Abstracts from the 55th European Society of Human Genetics (ESHG) Conference. Eur. J. Hum. Genet. 2023, 31 (Suppl. S1), 1–12. [Google Scholar]
- Ye, L.; Wang, F.; Wu, H.; Yang, H.; Yang, Y.; Ma, Y.; Xue, A.; Zhu, J.; Chen, M.; Wang, J.; et al. Functions and Targets of miR-335 in Cancer. Oncol. Targets Ther. 2021, 14, 3335–3349. [Google Scholar] [CrossRef] [PubMed]
- Huo, W.; Zhang, M.; Li, C.; Wang, X.; Zhang, X.; Yang, X.; Fei, H. Correlation of microRNA-335 expression level with clinical significance and prognosis in non-small cell lung cancer. Medicine 2020, 99, e21369. [Google Scholar] [CrossRef] [PubMed]
- Lamberti, M.; Capasso, R.; Lombardi, A.; Di Domenico, M.; Fiorelli, A.; Feola, A.; Perna, A.F.; Santini, M.; Caraglia, M.; Ingrosso, D. Two Different Serum MiRNA Signatures Correlate with the Clinical Outcome and Histological Subtype in Pleural Malignant Mesothelioma Patients. PLoS ONE 2015, 10, e0135331. [Google Scholar] [CrossRef]
- Liu, R.; Guo, H.; Lu, S. MiR-335-5p restores cisplatin sensitivity in ovarian cancer cells through targeting BCL2L2. Cancer Med. 2018, 7, 4598–4609. [Google Scholar] [CrossRef]
- Byrne, M.J.; Nowak, A.K. Modified RECIST criteria for assessment of response in malignant pleural mesothelioma. Ann. Oncol. 2004, 15, 257–260. [Google Scholar] [CrossRef]
- Raiko, I.; Sander, I.; Weber, D.G.; Raulf-Heimsoth, M.; Gillissen, A.; Kollmeier, J.; Scherpereel, A.; Bruning, T.; Johnen, G. Development of an enzyme-linked immunosorbent assay for the detection of human calretinin in plasma and serum of mesothelioma patients. BMC Cancer 2010, 10, 242. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Kang, B.; Li, C.; Chen, T.; Zhang, Z. GEPIA2: An enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res. 2019, 47, W556–W560. [Google Scholar] [CrossRef] [PubMed]
| All Patients (N = 265) | Patients Treated with Cisplatin (N = 239) | ||
|---|---|---|---|
| Characteristic | Category/Unit | N (%) | N (%) |
| Sex | Male | 197 (74.3) | 179 (74.9) |
| Female | 68 (25.7) | 60 (25.1) | |
| Age | Years, median (25–75%) | 66 (59–72) | 66 (59–72) |
| Stage | 1 | 17 (7.2) | 15 (7.1) |
| 2 | 60 (25.5) | 53 (25.1) | |
| 3 | 85 (36.2) | 77 (36.5) | |
| 4 | 72 (30.6) | 65 (30.8) | |
| Not determined | 1 (0.4) | 1 (0.5) | |
| Location | Pleura | 235 (88.7) | 211 (88.3) |
| Peritoneum | 30 (11.3) | 28 (11.7) | |
| Histological type | Epithelioid | 204 (77.0) | 186 (77.8) |
| Biphasic | 23 (8.7) | 21 (8.8) | |
| Sarcomatoid | 26 (9.8) | 23 (9.6) | |
| Not determined | 12 (4.5) | 9 (3.8) | |
| ECOG performance status | 0 | 15 (5.7) | 15 (6.3) |
| 1 | 137 (51.7) | 129 (54.0) | |
| 2 | 106 (40.0) | 92 (38.5) | |
| 3 | 7 (2.6) | 3 (1.3) | |
| Asbestos exposure | No | 66 (25.0) {1} | 60 (25.2) {1} |
| Yes | 198 (75.0) | 178 (74.8) | |
| Smoking | No | 146 (55.7) {3} | 132 (55.7) {2} |
| Yes | 116 (44.3) | 105 (44.3) | |
| CRP | mg/L, median (25–75%) | 23 (9–68.8) {29} | 21 (8–61) {20} |
| LDH | µkat/L, median (25–75%) | 2.72 (2.28–3.19) {28} | 2.69 (2.26–3.17) {20} |
| Pain | No | 109 (42.6) {9} | 101 (43.5) {7} |
| Yes | 147 (57.4) | 131 (56.5) | |
| Weight loss | No | 87 (34.7) {14} | 77 (34.1) {13} |
| Yes | 164 (65.3) | 149 (65.9) | |
| Chemotherapy regimen | No | 16 (6.0) | 0 (0.0) |
| Gemcitabine/cisplatin | 154 (58.1) | 154 (64.4) | |
| Pemetrexed/cisplatin | 85 (32.1) | 85 (35.6) | |
| Other | 10 (3.8) | 0 (0.0) | |
| Disease progression | No | 27 (10.2) | 25 (10.5) |
| Yes | 238 (89.8) | 214 (89.5) | |
| Death | No | 71 (26.8) | 67 (28.0) |
| Yes | 194 (73.2) | 172 (72.2) | |
| PFS | Months, median (25–75%) | 10.0 (6.3–16.2) ** | 8.2 (5.3–13.8) *** |
| OS | Months, median (25–75%) | 19.1 (10.0–29.4) ** | 9.5 (18.1–28.4) *** |
| Follow-up | Months, median (25–75%) | 45.5 (22.8–78.7) ** | 20.2 (44.4–75.5) *** |
| Calretinin concentration * | Ng/mL, median (25–75%) | 0.52 (0.22–1.43) | 0.51 (0.22–1.37) |
| PFS | OS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| SNP | Genotype | Median (25–75%) | HR (95% CI) | p | HR (95% CI)adj1 | Padj1 | Median (25–75%) | HR (95% CI) | p | HR (95% CI)adj2 | Padj2 |
| CALB2 rs1862818 | CC | 9.8 (5.9–14.5) | Reference | Reference | 16.7 (9.4–28.3) | Reference | Reference | ||||
| CT | 9.9 (6.6–16.9) | 0.88 (0.67–1.15) | 0.333 | 0.82 (0.60–1.11) | 0.199 | 21.2 (11.3–35.1) | 0.78 (0.58–1.05) | 0.099 | 0.79 (0.57–1.09) | 0.156 | |
| TT | 11.5 (6.6–20.5) | 0.81 (0.52–1.27) | 0.364 | 0.74 (0.45–1.21) | 0.233 | 24.4 (12.5–27.2) | 0.84 (0.52–1.37) | 0.480 | 0.85 (0.50–1.44) | 0.545 | |
| CT + TT | 10.0 (6.6–17.4) | 0.86 (0.67–1.11) | 0.256 | 0.80 (0.60–1.07) | 0.130 | 22.0 (11.5–33.7) | 0.79 (0.59–1.05) | 0.099 | 0.80 (0.59–1.09) | 0.157 | |
| CALB2 rs889704 | CC | 10.0 (6.6–16.9) | Reference | Reference | 18.5 (10.1–30.3) | Reference | Reference | ||||
| CA | 10.0 (6.0–12.6) | 1.14 (0.83–1.56) | 0.415 | 1.03 (0.72–1.46) | 0.890 | 20.3 (9.5–28.6) | 1.05 (0.73–1.51) | 0.777 | 1.14 (0.78–1.66) | 0.501 | |
| AA | 8.7 (4.8–8.7) | 1.76 (0.43–7.13) | 0.43 | 2.60 (0.63–10.68) | 0.185 | 16.2 (6.1–16.2) | 2.17 (0.53–8.81) | 0.279 | 3.59 (0.86–14.96) | 0.079 | |
| CA + AA | 9.7 (6.0–12.6) | 1.15 (0.85–1.57) | 0.362 | 1.06 (0.75–1.49) | 0.762 | 20.3 (9.4–28.6) | 1.08 (0.76–1.54) | 0.665 | 1.18 (0.81–1.71) | 0.381 | |
| CALB2 rs8063760 | CC | 10.2 (6.6–17.1) | Reference | Reference | 19.4 (10.0–29) | Reference | Reference | ||||
| CT | 9.4 (6.2–14.3) | 1.07 (0.81–1.41) | 0.622 | 1.26 (0.93–1.71) | 0.143 | 19.3 (11.6–32.5) | 0.88 (0.65–1.21) | 0.433 | 0.98 (0.70–1.38) | 0.920 | |
| TT | 7.9 (4.8–14.3) | 1.54 (0.90–2.63) | 0.114 | 1.22 (0.67–2.24) | 0.518 | 12.7 (7.1–24.7) | 1.59 (0.90–2.83) | 0.112 | 1.22 (0.66–2.25) | 0.527 | |
| CT + TT | 9.4 (6.1–14.3) | 1.13 (0.87–1.46) | 0.371 | 1.25 (0.94–1.67) | 0.128 | 18.2 (10.0–31.1) | 0.96 (0.72–1.29) | 0.783 | 1.02 (0.74–1.41) | 0.895 | |
| E2F2 rs2075995 | CC | 8.4 (5.5–15.0) | Reference | Reference | 16.0 (8.3–25.7) | Reference | Reference | ||||
| CA | 11.0 (6.6–16.2) | 0.82 (0.60–1.12) | 0.205 | 1.00 (0.71–1.42) | 0.989 | 20.7 (11.0–31.4) | 0.73 (0.52–1.02) | 0.066 | 0.95 (0.65–1.39) | 0.805 | |
| AA | 9.9 (6.2–16.5) | 0.93 (0.65–1.33) | 0.695 | 1.04 (0.70–1.55) | 0.846 | 18.1 (10.8–28.6) | 0.80 (0.54–1.19) | 0.268 | 1.03 (0.66–1.60) | 0.886 | |
| CA + AA | 10.2 (6.4–16.5) | 0.85 (0.64–1.14) | 0.286 | 1.02 (0.73–1.41) | 0.928 | 19.7 (10.8–31.2) | 0.75 (0.55–1.03) | 0.075 | 0.98 (0.68–1.40) | 0.903 | |
| MIR335 rs3807348 | GG | 9.4 (5.6–15.0) | Reference | Reference | 16.1 (7.6–25.6) | Reference | Reference | ||||
| GA | 10.6 (7.3–17.9) | 0.83 (0.61–1.13) | 0.239 | 0.98 (0.68–1.40) | 0.900 | 22.0 (11.8–35.1) | 0.69 (0.49–0.98) | 0.038 | 0.65 (0.45–0.95) | 0.028 | |
| AA | 8.2 (5.5–13.4) | 1.18 (0.83–1.68) | 0.353 | 1.40 (0.92–2.11) | 0.114 | 15.6 (8.3–26.2) | 1.08 (0.74–1.57) | 0.709 | 1.02 (0.67–1.55) | 0.914 | |
| GA + AA | 10.0 (6.6–16.3) | 0.93 (0.69–1.24) | 0.614 | 1.08 (0.77–1.52) | 0.650 | 19.7 (11.0–31.2) | 0.81 (0.59–1.11) | 0.184 | 0.76 (0.53–1.08) | 0.129 | |
| NRF1 rs13241028 | TT | 10.7 (6.8–15.0) | Reference | Reference | 18.2 (11.8–27.8) | Reference | Reference | ||||
| TC | 7.5 (5.6–16.3) | 1.13 (0.86–1.49) | 0.365 | 1.23 (0.92–1.67) | 0.166 | 19.3 (7.3–33.7) | 0.94 (0.69–1.26) | 0.668 | 1.04 (0.75–1.45) | 0.794 | |
| CC | 9.9 (5.5–14.1) | 0.88 (0.47–1.62) | 0.672 | 0.70 (0.28–1.77) | 0.449 | 29.4 (9.6–*) | 0.58 (0.27–1.25) | 0.164 | 0.72 (0.29–1.81) | 0.489 | |
| TC + CC | 8.0 (5.6–16.3) | 1.10 (0.84–1.43) | 0.490 | 1.19 (0.88–1.59) | 0.257 | 19.3 (8.0–35.1) | 0.89 (0.66–1.19) | 0.416 | 1.01 (0.74–1.39) | 0.942 | |
| SEPTIN7 rs3801339 | TT | 11.6 (7.9–19.4) | Reference | Reference | 22.0 (11.5–28.6) | Reference | Reference | ||||
| TC | 8.8 (6.0–16.3) | 1.27 (0.90–1.80) | 0.176 | 1.28 (0.88–1.88) | 0.203 | 15.6 (10.0–29.0) | 1.08 (0.74–1.56) | 0.702 | 1.21 (0.81–1.80) | 0.361 | |
| CC | 9.7 (6.1–14.7) | 1.47 (1.02–2.13) | 0.039 | 1.76 (1.17–2.64) | 0.007 | 20.6 (9.6–31.4) | 09.5 (0.64–1.42) | 0.796 | 1.11 (0.72–1.71) | 0.630 | |
| TC + CC | 9.4 (6.0–14.9) | 1.35 (0.97–1.86) | 0.074 | 1.44 (1.01–2.06) | 0.046 | 17.5 (9.6–30.0) | 1.02 (0.72–1.45) | 0.905 | 1.17 (0.80–1.69) | 0.421 | |
| Disease Control Rate | PFS | OS | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Calretinin Concentration | CR + PR + SD | PD | OR (95% CI) | p | Median (25–75%) | HR (95% CI) | p | Median (25–75%) | HR (95% CI) | p |
| Serum concentration (ng/mL) | 0.45 (0.21–1.07) * | 1.68 (0.58–4.20) * | 2.18 (1.51–3.14) | <0.001 | / | 1.21 (1.05–1.40) | 0.010 | / | 1.23 (1.04–1.45) | 0.013 |
| <0.51 ng/mL, N (%) ** | 57 (91.9) | 5 (8.1) | Ref. | 7.9 (5.5–13.1) | Ref. | 21.0 (10.1–42.5) | Ref. | |||
| >0.51 ng/mL, N (%) ** | 48 (76.2) | 15 (23.8) | 3.56 (1.21–10.52) | 0.021 | 7.0 (5.5–10.3) | 1.38 (0.95–2.01) | 0.090 | 15.0 (9.2–22.1) | 1.6 (0.95–2.26) | 0.085 |
| <0.89 ng/mL, N (%) *** | 75 (93.8) | 5 (6.3) | Ref. | 9.3 (6.1–13.9) | Ref. | 21.4 (11.4–42.5) | Ref. | |||
| >0.89 ng/mL, N (%) *** | 30 (66.7) | 15 (33.3) | 7.50 (2.50–22.47) | <0.001 | 6.4 (4.2–8.8) | 1.88 (1.28–2.77) | 0.001 | 12.1 (8.3–19.6) | 1.91 (1.22–2.97) | 0.004 |
| SNP | Genotype | SD + PD N (%) | PR + CR N (%) | OR (95% CI) | p | OR (95% CI)adj | Padj |
|---|---|---|---|---|---|---|---|
| CALB2 rs1862818 | CC | 79 (71.8) | 31 (28.2) | Reference | Reference | ||
| CT | 58 (59.2) | 40 (40.8) | 1.76 (0.99–3.13) | 0.056 | 1.69 (0.87–3.29) | 0.121 | |
| TT | 14 (60.9) | 9 (39.1) | 1.64 (0.64–4.17) | 0.301 | 1.31 (0.47–3.65) | 0.607 | |
| CT + TT | 72 (59.5) | 49 (40.5) | 1.73 (1.00–3.01) | 0.050 | 1.60 (0.85–3.01) | 0.142 | |
| CALB2 rs889704 | CC | 113 (63.5) | 65 (36.5) | Reference | Reference | ||
| CA | 35 (70.0) | 15 (30.0) | 0.75 (0.38–1.47) | 0.395 | 0.76 (0.34–1.72) | 0.511 | |
| AA | 3 (100) | 0 (0) | / | 0.306 | / | / | |
| CA + AA | 38 (71.7) | 15 (28.3) | 0.69 (0.35–1.34) | 0.271 | 0.65 (0.29–1.45) | 0.294 | |
| CALB2 rs8063760 | CC | 87 (62.6) | 52 (37.4) | Reference | Reference | ||
| CT | 51 (65.4) | 27 (34.6) | 0.89 (0.50–1.58) | 0.681 | 0.86 (0.45–1.67) | 0.664 | |
| TT | 13 (92.9) | 1 (7.1) | 0.13 (0.02–1.01) | 0.051 | 0.17 (0.02–1.46) | 0.107 | |
| CT + TT | 64 (69.6) | 28 (30.4) | 0.73 (0.42–1.28) | 0.276 | 0.74 (0.39–1.41) | 0.361 | |
| E2F2 rs2075995 | CC | 40 (70.2) | 17 (29.8) | Reference | Reference | ||
| CA | 76 (64.4) | 42 (35.6) | 1.30 (0.66–2.57) | 0.450 | 0.84 (0.39–1.82) | 0.657 | |
| AA | 35 (62.5) | 21 (37.5) | 1.41 (0.64–3.09) | 0.389 | 1.51 (0.63–3.63) | 0.355 | |
| CA + AA | 111 (63.8) | 63 (36.2) | 1.34 (0.70–2.55) | 0.380 | 1.02 (0.50–2.11) | 0.951 | |
| MIR335 rs3807348 | GG | 45 (78.9) | 12 (21.1) | Reference | Reference | ||
| GA | 64 (55.7) | 51 (44.3) | 2.99 (1.43–6.23) | 0.004 | 3.32 (1.40–7.89) | 0.007 | |
| AA | 42 (71.2) | 17 (28.8) | 1.52 (0.65–3.55) | 0.336 | 1.65 (0.61–4.49) | 0.324 | |
| GA + AA | 106 (60.9) | 68 (39.1) | 2.41 (1.19–4.87) | 0.015 | 2.69 (1.17–6.18) | 0.020 | |
| NRF1 rs13241028 | TT | 88 (63.3) | 51 (36.7) | Reference | Reference | ||
| TC | 57 (70.4) | 24 (29.6) | 0.73 (0.40–1.31) | 0.287 | 0.64 (0.33–1.23) | 0.182 | |
| CC | 6 (54.5) | 5 (45.5) | 1.44 (0.42–4.95) | 0.565 | 1.89 (0.33–10.7) | 0.473 | |
| TC + CC | 63 (68.5) | 29 (31.5) | 0.79 (0.45–1.39) | 0.419 | 0.70 (0.37–1.32) | 0.270 | |
| SEPTIN7 rs3801339 | TT | 29 (60.4) | 19 (39.6) | Reference | Reference | ||
| TC | 73 (64.6) | 40 (35.4) | 0.84 (0.42–1.68) | 0.614 | 0.93 (0.41–2.09) | 0.860 | |
| CC | 49 (70.0) | 21 (30.0) | 0.65 (0.30–1.42) | 0.281 | 0.56 (0.23–1.38) | 0.209 | |
| TC + CC | 122 (66.7) | 61 (33.3) | 0.76 (0.40–1.47) | 0.419 | 0.77 (0.36–1.66) | 0.506 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zupanc, C.; Franko, A.; Štrbac, D.; Kovač, V.; Dolžan, V.; Goričar, K. Serum Calretinin and Genetic Variability as a Prognostic and Predictive Factor in Malignant Mesothelioma. Int. J. Mol. Sci. 2024, 25, 190. https://doi.org/10.3390/ijms25010190
Zupanc C, Franko A, Štrbac D, Kovač V, Dolžan V, Goričar K. Serum Calretinin and Genetic Variability as a Prognostic and Predictive Factor in Malignant Mesothelioma. International Journal of Molecular Sciences. 2024; 25(1):190. https://doi.org/10.3390/ijms25010190
Chicago/Turabian StyleZupanc, Cita, Alenka Franko, Danijela Štrbac, Viljem Kovač, Vita Dolžan, and Katja Goričar. 2024. "Serum Calretinin and Genetic Variability as a Prognostic and Predictive Factor in Malignant Mesothelioma" International Journal of Molecular Sciences 25, no. 1: 190. https://doi.org/10.3390/ijms25010190
APA StyleZupanc, C., Franko, A., Štrbac, D., Kovač, V., Dolžan, V., & Goričar, K. (2024). Serum Calretinin and Genetic Variability as a Prognostic and Predictive Factor in Malignant Mesothelioma. International Journal of Molecular Sciences, 25(1), 190. https://doi.org/10.3390/ijms25010190






