Disparity in the Influence of Implant Provisional Materials on Human Gingival Fibroblasts with Different Phases of Cell Settlement: An In Vitro Study
Abstract
1. Introduction
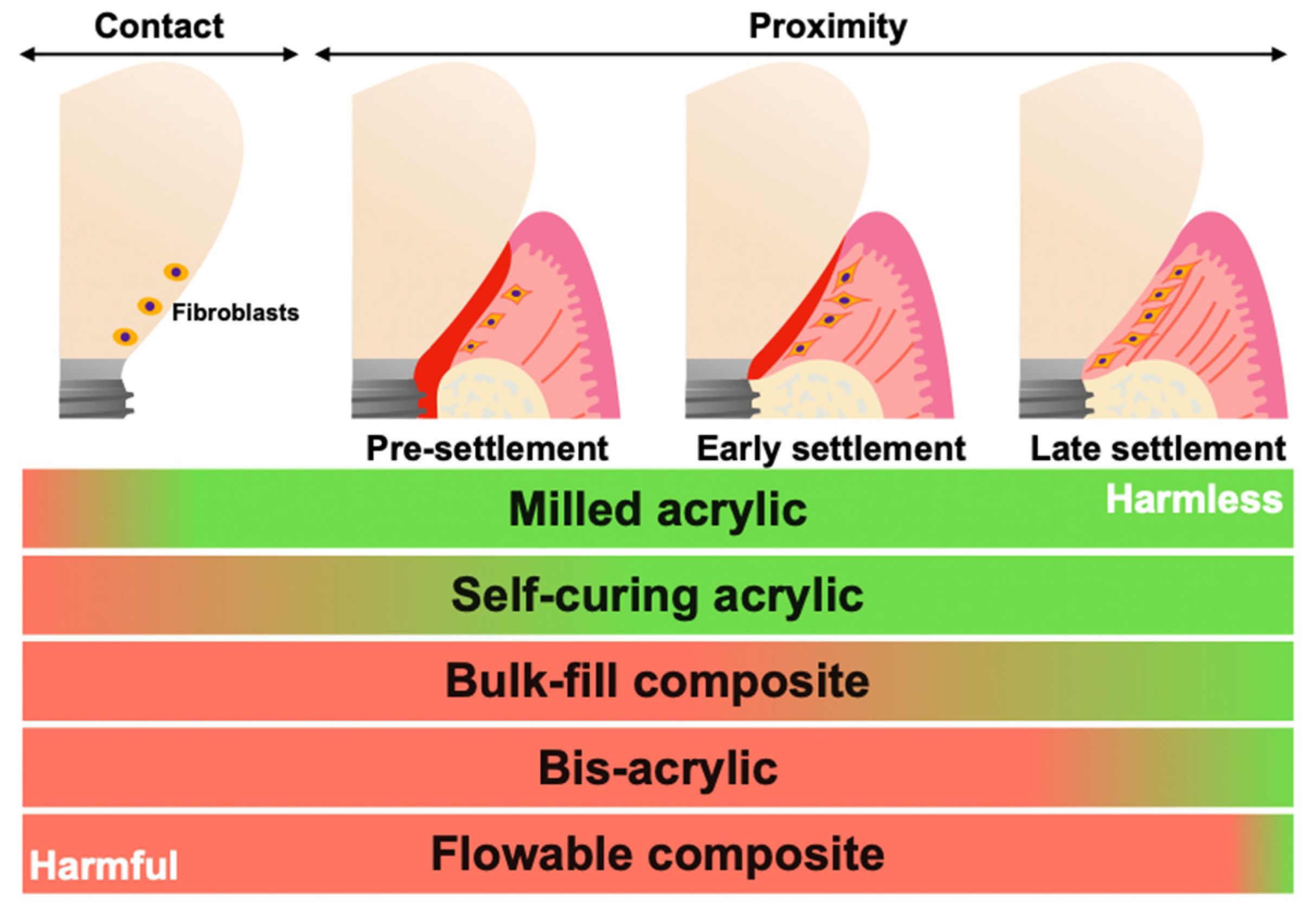
2. Results
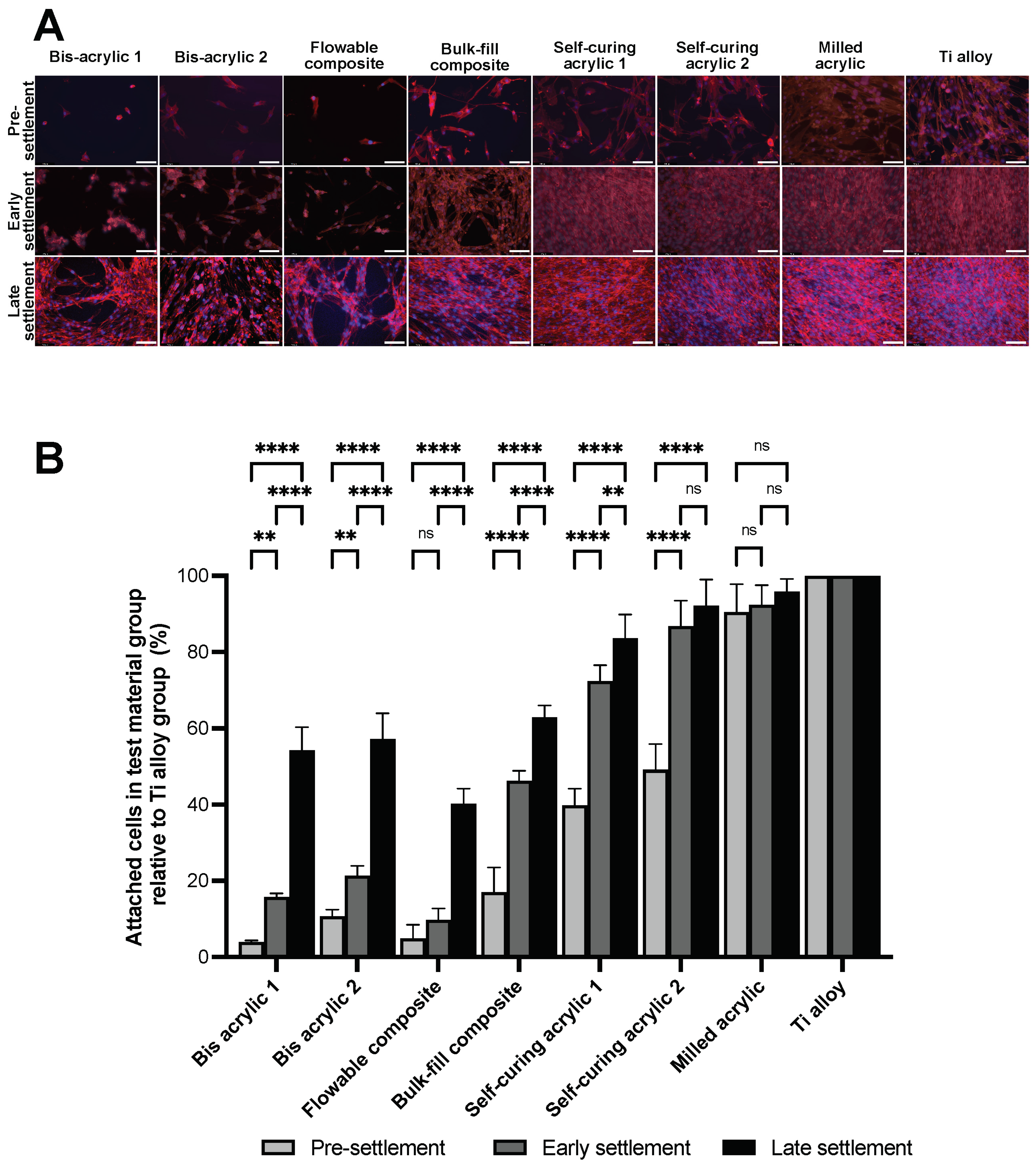
2.1. Growth of Fibroblasts on Test Materials
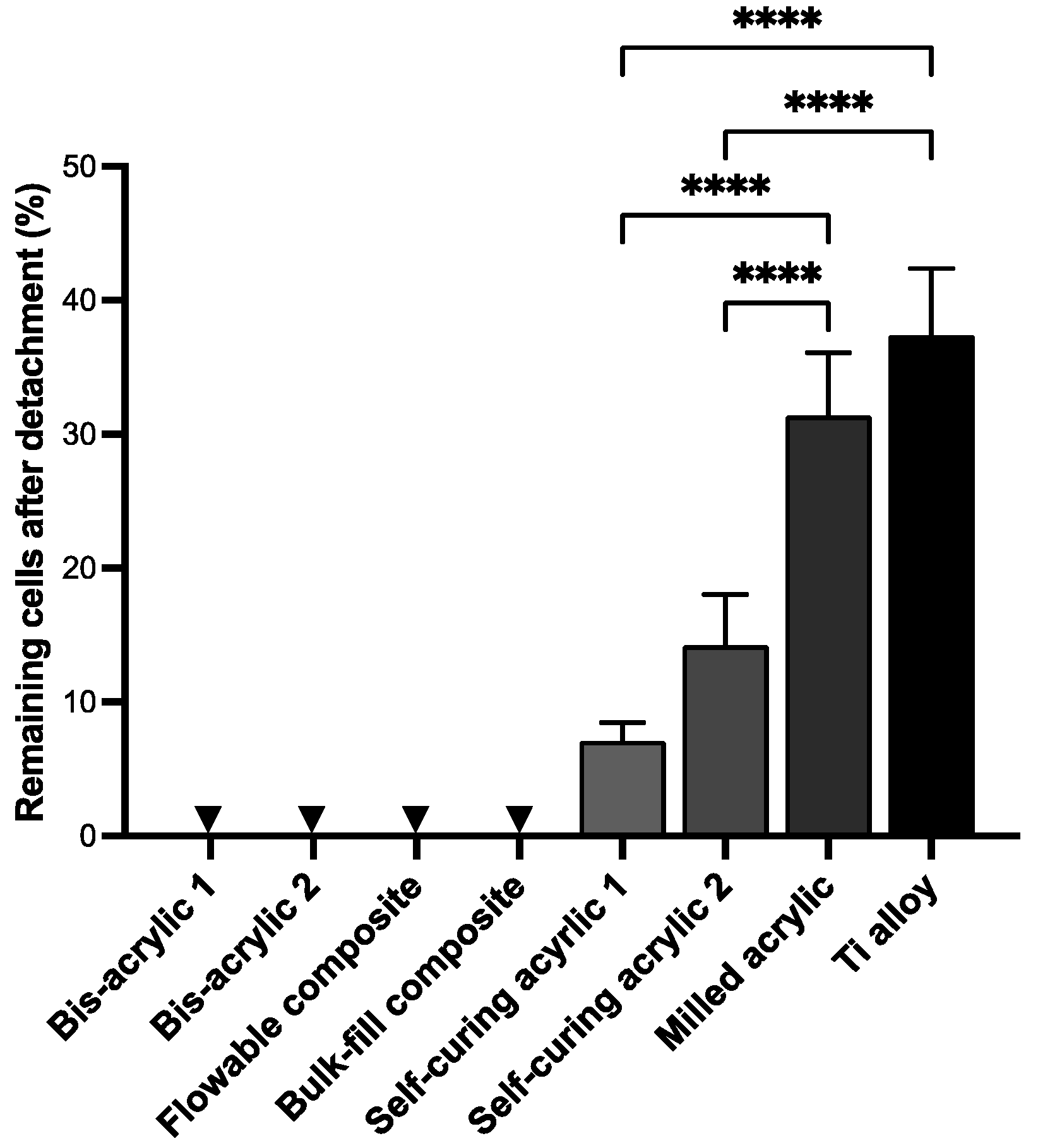
2.2. Cell Retention Ability
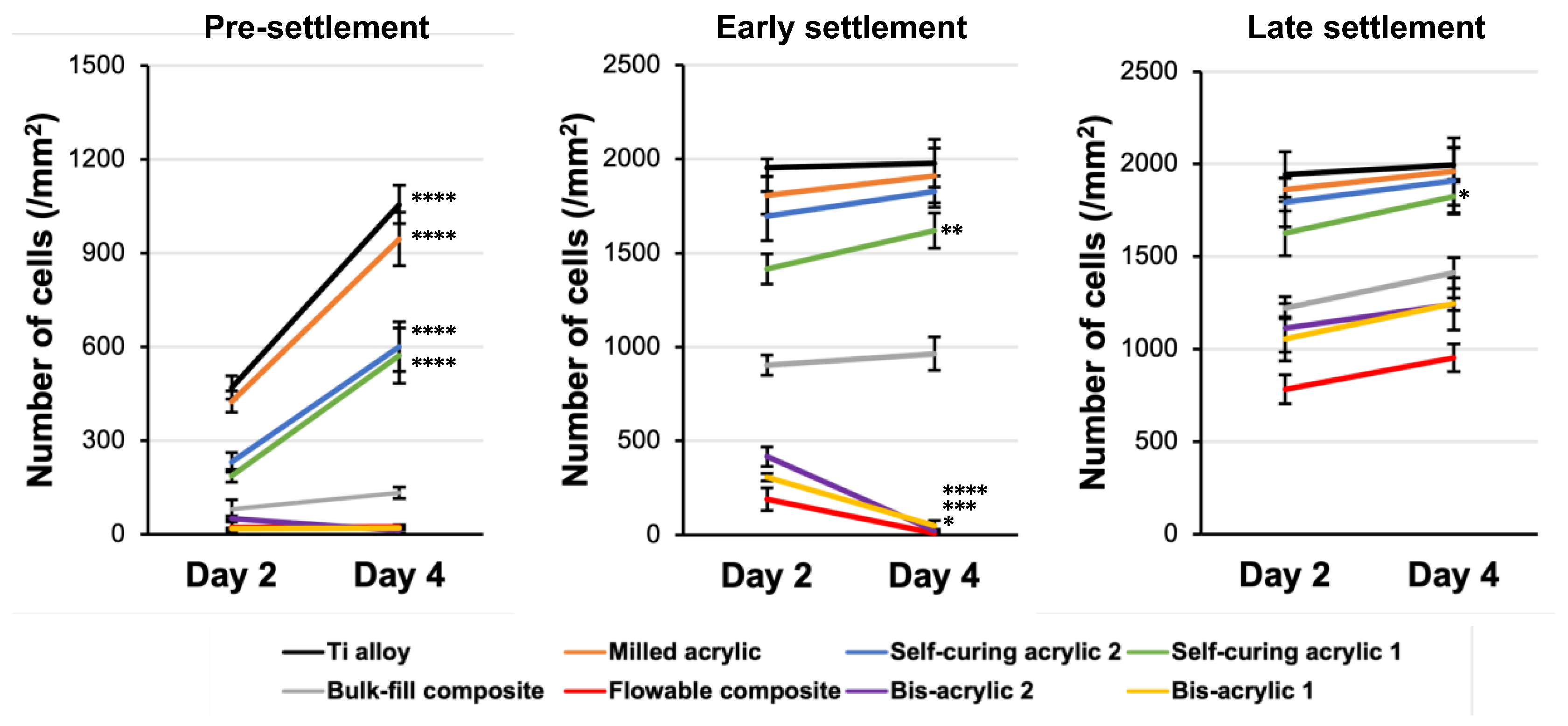
2.3. Fibroblast Growth at Different Phases of Cell Settlement
2.4. Collagen Deposition
3. Discussion
4. Materials and Methods
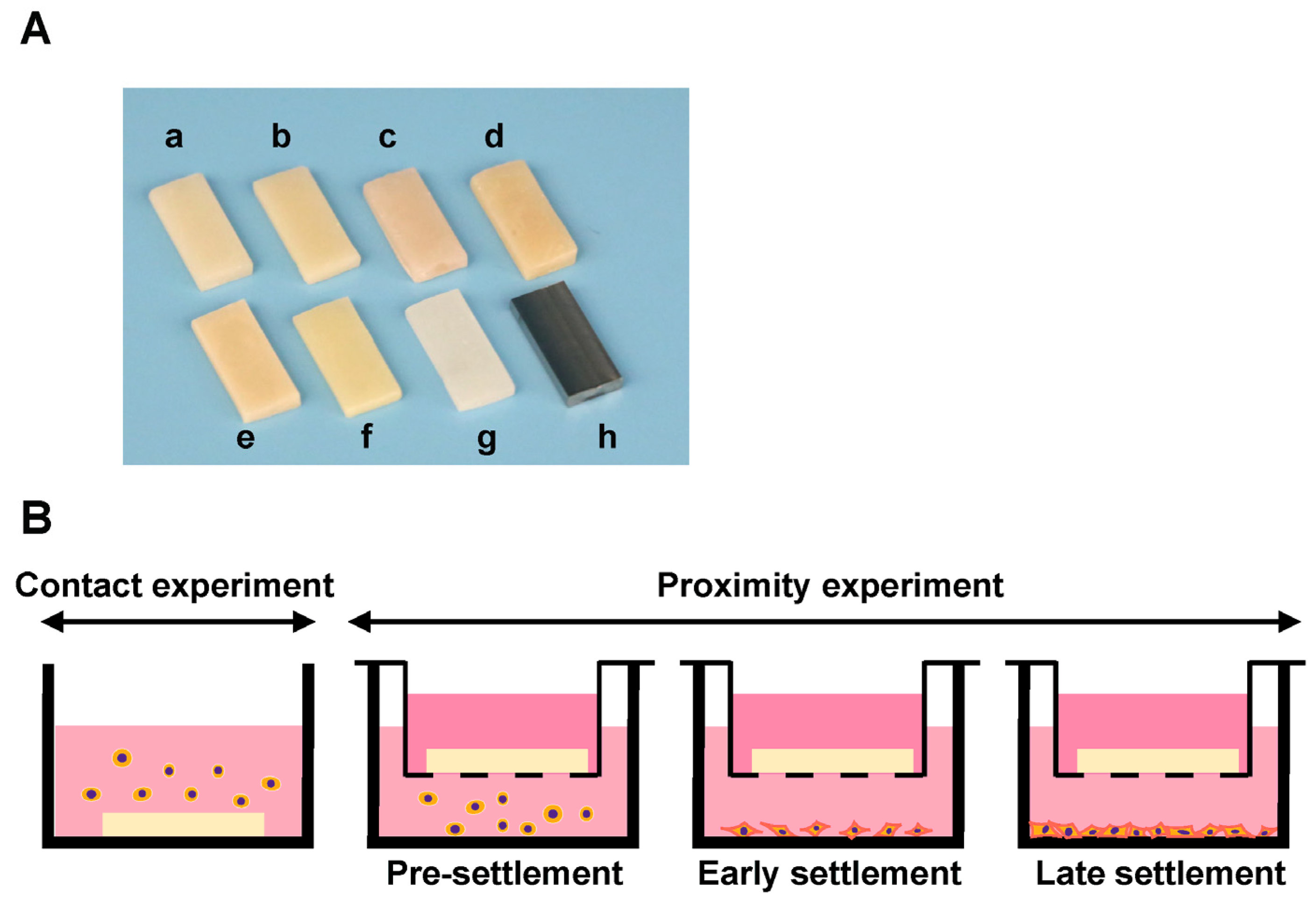
4.1. Material Preparation
4.2. Cell Culture and Material Placement
4.3. Quantification of Attached and Propagated Cells with Fluorescence Microscopy
4.4. Cell Retention Assay
4.5. Collagen Deposition
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schwarz, F.; Ramanauskaite, A. It is all about peri-implant tissue health. Periodontology 2000 2022, 88, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Khater, A.G.A.; Gehrke, S.A.; Serra, P.; Francesco, I.; Di Carmine, M.; Tari, S.R.; Leo, L.; Lorusso, F. Current Status of Peri-Implant Diseases: A Clinical Review for Evidence-Based Decision Making. J. Funct. Biomater. 2023, 14, 210. [Google Scholar] [CrossRef] [PubMed]
- Korsch, M.; Marten, S.M.; Stoll, D.; Prechtl, C.; Dotsch, A. Microbiological findings in early and late implant loss: An observational clinical case-controlled study. BMC Oral Health 2021, 21, 112. [Google Scholar] [CrossRef] [PubMed]
- Welander, M.; Abrahamsson, I.; Berglundh, T. The mucosal barrier at implant abutments of different materials. Clin. Oral Implant. Res. 2008, 19, 635–641. [Google Scholar] [CrossRef]
- Bordin, S.; Flemmig, T.F.; Verardi, S. Role of fibroblast populations in peri-implantitis. Int. J. Oral Maxillofac. Implant. 2009, 24, 197–204. [Google Scholar]
- Kan, J.Y.K.; Rungcharassaeng, K.; Deflorian, M.; Weinstein, T.; Wang, H.L.; Testori, T. Immediate implant placement and provisionalization of maxillary anterior single implants. Periodontology 2000 2018, 77, 197–212. [Google Scholar] [CrossRef] [PubMed]
- Saito, H.; Chu, S.J.; Reynolds, M.A.; Tarnow, D.P. Provisional Restorations Used in Immediate Implant Placement Provide a Platform to Promote Peri-implant Soft Tissue Healing: A Pilot Study. Int. J. Periodontics Restor. Dent. 2016, 36, 47–52. [Google Scholar] [CrossRef]
- Zhuang, J.; Wang, Y.; Song, Y.; Qu, F.; Xu, C. The application of individualized abutment-crown integrated provisional restoration in optimizing the peri-implant soft tissue contour in the esthetic zone. J. Esthet. Restor. Dent. 2021, 33, 560–566. [Google Scholar] [CrossRef]
- Gonzalez-Martin, O.; Lee, E.; Weisgold, A.; Veltri, M.; Su, H. Contour Management of Implant Restorations for Optimal Emergence Profiles: Guidelines for Immediate and Delayed Provisional Restorations. Int. J. Periodontics Restor. Dent. 2020, 40, 61–70. [Google Scholar] [CrossRef]
- Grossner-Schreiber, B.; Herzog, M.; Hedderich, J.; Duck, A.; Hannig, M.; Griepentrog, M. Focal adhesion contact formation by fibroblasts cultured on surface-modified dental implants: An in vitro study. Clin. Oral Implant. Res. 2006, 17, 736–745. [Google Scholar] [CrossRef]
- Kim, Y.S.; Ko, Y.; Kye, S.B.; Yang, S.M. Human gingival fibroblast (HGF-1) attachment and proliferation on several abutment materials with various colors. Int. J. Oral Maxillofac. Implant. 2014, 29, 969–975. [Google Scholar] [CrossRef] [PubMed]
- Bajantri, P.; Rodrigues, S.J.; Shama Prasada, K.; Pai, U.Y.; Shetty, T.; Saldanha, S.; Mahesh, M.; Hegde, P.; Sales, A.; Mukherjee, S.; et al. Cytotoxicity of Dental Cements on Soft Tissue Associated with Dental Implants. Int. J. Dent. 2022, 2022, 4916464. [Google Scholar] [CrossRef] [PubMed]
- Bandarra, S.; Neves, J.; Paraiso, A.; Mascarenhas, P.; Ribeiro, A.C.; Barahona, I. Biocompatibility of self-adhesive resin cement with fibroblast cells. J. Prosthet. Dent. 2021, 125, 705.e1–705.e7. [Google Scholar] [CrossRef] [PubMed]
- Gautam, R.; Singh, R.D.; Sharma, V.P.; Siddhartha, R.; Chand, P.; Kumar, R. Biocompatibility of polymethylmethacrylate resins used in dentistry. J. Biomed. Mater. Res. B Appl. Biomater. 2012, 100, 1444–1450. [Google Scholar] [CrossRef] [PubMed]
- Ulker, M.; Ulker, H.E.; Zortuk, M.; Bulbul, M.; Tuncdemir, A.R.; Bilgin, M.S. Effects of current provisional restoration materials on the viability of fibroblasts. Eur. J. Dent. 2009, 3, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.S.; Kim, H.C.; Park, S.I.; Yun, H.J.; Ryu, J.J. Comparison of Various Implant Provisional Resin Materials for Cytotoxicity and Attachment to Human Gingival Fibroblasts. Int. J. Oral Maxillofac. Implant. 2019, 34, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Van Landuyt, K.L.; Nawrot, T.; Geebelen, B.; De Munck, J.; Snauwaert, J.; Yoshihara, K.; Scheers, H.; Godderis, L.; Hoet, P.; Van Meerbeek, B. How much do resin-based dental materials release? A meta-analytical approach. Dent. Mater. 2011, 27, 723–747. [Google Scholar] [CrossRef]
- Duruk, G.; Akkuc, S.; Ugur, Y. Evaluation of residual monomer release after polymerization of different restorative materials used in pediatric dentistry. BMC Oral Health 2022, 22, 232. [Google Scholar] [CrossRef]
- Bezgin, T.; Cimen, C.; Ozalp, N. Evaluation of Residual Monomers Eluted from Pediatric Dental Restorative Materials. Biomed. Res. Int. 2021, 2021, 6316171. [Google Scholar] [CrossRef]
- Ogawa, T.; Tanaka, M.; Matsuya, S.; Aizawa, S.; Koyano, K. Setting characteristics of five autopolymerizing resins measured by an oscillating rheometer. J. Prosthet. Dent. 2001, 85, 170–176. [Google Scholar] [CrossRef]
- Çelebi, N.; Yüzügüllü, B.; Canay, Ş.; Yücel, Ü. Effect of polymerization methods on the residual monomer level of acrylic resin denture base polymers. Polym. Adv. Technol. 2008, 19, 201–206. [Google Scholar] [CrossRef]
- Nakagawa, K.; Saita, M.; Ikeda, T.; Hirota, M.; Park, W.; Lee, M.C.; Ogawa, T. Biocompatibility of 4-META/MMA-TBB resin used as a dental luting agent. J. Prosthet. Dent. 2015, 114, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Kojima, N.; Yamada, M.; Paranjpe, A.; Tsukimura, N.; Kubo, K.; Jewett, A.; Ogawa, T. Restored viability and function of dental pulp cells on poly-methylmethacrylate (PMMA)-based dental resin supplemented with N-acetyl cysteine (NAC). Dent. Mater. 2008, 24, 1686–1693. [Google Scholar] [CrossRef] [PubMed]
- Goncalves, F.P.; Alves, G.; Guimaraes, V.O.J.; Gallito, M.A.; Oliveira, F.; Scelza, M.Z. Cytotoxicity Evaluation of Two Bis-Acryl Composite Resins Using Human Gingival Fibroblasts. Braz. Dent. J. 2016, 27, 492–496. [Google Scholar] [CrossRef] [PubMed]
- Parikh, V.; Cheng, D.H.; Linsley, C.; Shah, K.C. Bond strength of three chairside crown reline materials to milled polymethyl methacrylate resin. J. Prosthet. Dent. 2021, 125, 544.e1–544.e8. [Google Scholar] [CrossRef] [PubMed]
- Shibasaki, S.; Takamizawa, T.; Suzuki, T.; Nojiri, K.; Tsujimoto, A.; Barkmeier, W.W.; Latta, M.A.; Miyazaki, M. Influence of Different Curing Modes on Polymerization Behavior and Mechanical Properties of Dual-Cured Provisional Resins. Oper. Dent. 2017, 42, 526–536. [Google Scholar] [CrossRef] [PubMed]
- Amin, B.M.; Aras, M.A.; Chitre, V. A comparative evaluation of the marginal accuracy of crowns fabricated from four commercially available provisional materials: An in vitro study. Contemp. Clin. Dent. 2015, 6, 161–165. [Google Scholar] [CrossRef]
- Hussain, B.; Thieu, M.K.L.; Johnsen, G.F.; Reseland, J.E.; Haugen, H.J. Can CAD/CAM resin blocks be considered as substitute for conventional resins? Dent. Mater. 2017, 33, 1362–1370. [Google Scholar] [CrossRef]
- Wei, X.; Pan, Y.; Wang, M.; Wang, Y.; Lin, H.; Jiang, L.; Lin, D.; Cheng, H. Comparative analysis of leaching residual monomer and biological effects of four types of conventional and CAD/CAM dental polymers: An in vitro study. Clin. Oral Investig. 2022, 26, 2887–2898. [Google Scholar] [CrossRef]
- Burgers, R.; Schubert, A.; Muller, J.; Krohn, S.; Rodiger, M.; Leha, A.; Wassmann, T. Cytotoxicity of 3D-printed, milled, and conventional oral splint resins to L929 cells and human gingival fibroblasts. Clin. Exp. Dent. Res. 2022, 8, 650–657. [Google Scholar] [CrossRef]
- Aati, S.; Chauhan, A.; Shrestha, B.; Rajan, S.M.; Aati, H.; Fawzy, A. Development of 3D printed dental resin nanocomposite with graphene nanoplatelets enhanced mechanical properties and induced drug-free antimicrobial activity. Dent. Mater. 2022, 38, 1921–1933. [Google Scholar] [CrossRef] [PubMed]
- Lempel, E.; Czibulya, Z.; Kovacs, B.; Szalma, J.; Toth, A.; Kunsagi-Mate, S.; Varga, Z.; Boddi, K. Degree of Conversion and BisGMA, TEGDMA, UDMA Elution from Flowable Bulk Fill Composites. Int. J. Mol. Sci. 2016, 17, 732. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.H.; Lin, Y.M.; Lai, Y.L.; Lee, S.Y. Mechanical properties, accuracy, and cytotoxicity of UV-polymerized 3D printing resins composed of Bis-EMA, UDMA, and TEGDMA. J. Prosthet. Dent. 2020, 123, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Leyva Del Rio, D.; Johnston, W.M. Effect of monomer composition and filler fraction on surface microhardness and depth of cure of experimental resin composites. Eur. J. Oral Sci. 2023, 131, e12933. [Google Scholar] [CrossRef] [PubMed]
- Gul, P.; Miloglu, F.D.; Akgul, N.; Kadioglu, Y. Effect of Different Extraction Media on Quantification of the Released Monomers from Dental Composite. Asian J. Chem. 2013, 25, 2994–3000. [Google Scholar] [CrossRef]
- Hampe, T.; Wiessner, A.; Frauendorf, H.; Alhussein, M.; Karlovsky, P.; Burgers, R.; Krohn, S. A comparative in vitro study on monomer release from bisphenol A-free and conventional temporary crown and bridge materials. Eur. J. Oral Sci. 2021, 129, e12826. [Google Scholar] [CrossRef] [PubMed]
- Landenberger, P.; Baumann, L.; Gerhardt-Szep, S.; Ruttermann, S. The effect of new anti-adhesive and antibacterial dental resin filling materials on gingival fibroblasts. Dent. Mater. 2021, 37, 1416–1424. [Google Scholar] [CrossRef]
- Tsitrou, E.; Kelogrigoris, S.; Koulaouzidou, E.; Antoniades-Halvatjoglou, M.; Koliniotou-Koumpia, E.; van Noort, R. Effect of extraction media and storage time on the elution of monomers from four contemporary resin composite materials. Toxicol. Int. 2014, 21, 89–95. [Google Scholar] [CrossRef]
- Alshali, R.Z.; Salim, N.A.; Sung, R.; Satterthwaite, J.D.; Silikas, N. Analysis of long-term monomer elution from bulk-fill and conventional resin-composites using high performance liquid chromatography. Dent. Mater. 2015, 31, 1587–1598. [Google Scholar] [CrossRef]
- Bainbridge, P. Wound healing and the role of fibroblasts. J. Wound Care 2013, 22, 407–412. [Google Scholar]
- Nevins, M.; Nevins, M.L.; Camelo, M.; Boyesen, J.L.; Kim, D.M. Human histologic evidence of a connective tissue attachment to a dental implant. Int. J. Periodontics Restor. Dent. 2008, 28, 111–121. [Google Scholar]
- Roy, M.; Corti, A.; Dominici, S.; Pompella, A.; Cerea, M.; Chelucci, E.; Dorocka-Bobkowska, B.; Daniele, S. Biocompatibility of Subperiosteal Dental Implants: Effects of Differently Treated Titanium Surfaces on the Expression of ECM-Related Genes in Gingival Fibroblasts. J. Funct Biomater. 2023, 14, 59. [Google Scholar] [CrossRef] [PubMed]
- Garrod, D.R. Cell to cell and cell to matrix adhesion. BMJ 1993, 306, 703–705. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Taghva, O.; Amini Sedeh, S.; Ejeian, F.; Amini, S. Comparison of Adhesion and Proliferation of Human Gingival Fibroblasts on Acellular Dermal Matrix with and without Low Level Diode Laser Irradiation, an in vitro Study. J. Dent. 2022, 23, 106–112. [Google Scholar]
- Moon, Y.H.; Yoon, M.K.; Moon, J.S.; Kang, J.H.; Kim, S.H.; Yang, H.S.; Kim, M.S. Focal adhesion linker proteins expression of fibroblast related to adhesion in response to different transmucosal abutment surfaces. J. Adv. Prosthodont. 2013, 5, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Matsuura, T.; Komatsu, K.; Chao, D.; Lin, Y.C.; Oberoi, N.; McCulloch, K.; Cheng, J.; Orellana, D.; Ogawa, T. Cell Type-Specific Effects of Implant Provisional Restoration Materials on the Growth and Function of Human Fibroblasts and Osteoblasts. Biomimetics 2022, 7, 243. [Google Scholar] [CrossRef] [PubMed]
- Matsuura, T.; Komatsu, K.; Choi, K.; Suzumura, T.; Cheng, J.; Chang, T.L.; Chao, D.; Ogawa, T. Conditional Mitigation of Dental-Composite Material-Induced Cytotoxicity by Increasing the Cure Time. J. Funct. Biomater. 2023, 14, 119. [Google Scholar] [CrossRef]
- Jorge, J.H.; Giampaolo, E.T.; Machado, A.L.; Vergani, C.E. Cytotoxicity of denture base acrylic resins: A literature review. J. Prosthet. Dent. 2003, 90, 190–193. [Google Scholar] [CrossRef]
- Schweikl, H.; Spagnuolo, G.; Schmalz, G. Genetic and cellular toxicology of dental resin monomers. J. Dent. Res. 2006, 85, 870–877. [Google Scholar] [CrossRef]
- Kraus, D.; Wolfgarten, M.; Enkling, N.; Helfgen, E.H.; Frentzen, M.; Probstmeier, R.; Winter, J.; Stark, H. In-vitro cytocompatibility of dental resin monomers on osteoblast-like cells. J. Dent. 2017, 65, 76–82. [Google Scholar] [CrossRef]
- Haugen, H.J.; Marovic, D.; Par, M.; Thieu, M.K.L.; Reseland, J.E.; Johnsen, G.F. Bulk Fill Composites Have Similar Performance to Conventional Dental Composites. Int. J. Mol. Sci. 2020, 21, 5136. [Google Scholar] [CrossRef] [PubMed]
- Komatsu, K.; Hamajima, K.; Ozawa, R.; Kitajima, H.; Matsuura, T.; Ogawa, T. Novel Tuning of PMMA Orthopedic Bone Cement Using TBB Initiator: Effect of Bone Cement Extracts on Bioactivity of Osteoblasts and Osteoclasts. Cells 2022, 11, 3999. [Google Scholar] [CrossRef] [PubMed]
- Sugita, Y.; Okubo, T.; Saita, M.; Ishijima, M.; Torii, Y.; Tanaka, M.; Iwasaki, C.; Sekiya, T.; Tabuchi, M.; Mohammadzadeh Rezaei, N.; et al. Novel Osteogenic Behaviors around Hydrophilic and Radical-Free 4-META/MMA-TBB: Implications of an Osseointegrating Bone Cement. Int. J. Mol. Sci. 2020, 21, 2405. [Google Scholar] [CrossRef] [PubMed]
- Tsukimura, N.; Yamada, M.; Aita, H.; Hori, N.; Yoshino, F.; Chang-Il Lee, M.; Kimoto, K.; Jewett, A.; Ogawa, T. N-acetyl cysteine (NAC)-mediated detoxification and functionalization of poly(methyl methacrylate) bone cement. Biomaterials 2009, 30, 3378–3389. [Google Scholar] [CrossRef] [PubMed]
- Emmler, J.; Seiss, M.; Kreppel, H.; Reichl, F.X.; Hickel, R.; Kehe, K. Cytotoxicity of the dental composite component TEGDMA and selected metabolic by-products in human pulmonary cells. Dent. Mater. 2008, 24, 1670–1675. [Google Scholar] [CrossRef] [PubMed]
- Lagocka, R.; Jakubowska, K.; Chlubek, D.; Buczkowska-Radlinska, J. Elution study of unreacted TEGDMA from bulk-fill composite (SDR Dentsply) using HPLC. Adv. Med. Sci. 2015, 60, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Polydorou, O.; Trittler, R.; Hellwig, E.; Kummerer, K. Elution of monomers from two conventional dental composite materials. Dent. Mater. 2007, 23, 1535–1541. [Google Scholar] [CrossRef] [PubMed]
- Sideridou, I.; Tserki, V.; Papanastasiou, G. Effect of chemical structure on degree of conversion in light-cured dimethacrylate-based dental resins. Biomaterials 2002, 23, 1819–1829. [Google Scholar] [CrossRef]
- Att, W.; Yamada, M.; Kojima, N.; Ogawa, T. N-Acetyl cysteine prevents suppression of oral fibroblast function on poly(methylmethacrylate) resin. Acta Biomater. 2009, 5, 391–398. [Google Scholar] [CrossRef]
- Chang, M.C.; Lin, L.D.; Wu, M.T.; Chan, C.P.; Chang, H.H.; Lee, M.S.; Sun, T.Y.; Jeng, P.Y.; Yeung, S.Y.; Lin, H.J.; et al. Effects of Camphorquinone on Cytotoxicity, Cell Cycle Regulation and Prostaglandin E2 Production of Dental Pulp Cells: Role of ROS, ATM/Chk2, MEK/ERK and Hemeoxygenase-1. PLoS ONE 2015, 10, e0143663. [Google Scholar] [CrossRef]
- Matsuura, T.; Komatsu, K.; Ogawa, T. N-Acetyl Cysteine-Mediated Improvements in Dental Restorative Material Biocompatibility. Int. J. Mol. Sci. 2022, 23, 15869. [Google Scholar] [CrossRef] [PubMed]
- Volk, J.; Ziemann, C.; Leyhausen, G.; Geurtsen, W. Non-irradiated campherquinone induces DNA damage in human gingival fibroblasts. Dent. Mater. 2009, 25, 1556–1563. [Google Scholar] [CrossRef] [PubMed]
- Stansbury, J.W. Curing dental resins and composites by photopolymerization. J. Esthet. Dent. 2000, 12, 300–308. [Google Scholar] [CrossRef]
- Iwaki, M.; Kanazawa, M.; Arakida, T.; Minakuchi, S. Mechanical properties of a polymethyl methacrylate block for CAD/CAM dentures. J. Oral Sci. 2020, 62, 420–422. [Google Scholar] [CrossRef] [PubMed]
- Yin, Q.; Pi, X.; Ren, G.; Liu, Z.; Liu, H.; Wang, M.; Hu, C.; Zhao, H.; Li, D.; Yin, J. A novel bispecific antibody alleviates bleomycin-induced systemic sclerosis injury. Int. Immunopharmacol. 2020, 85, 106644. [Google Scholar] [CrossRef] [PubMed]
- Lefeuvre, M.; Amjaad, W.; Goldberg, M.; Stanislawski, L. TEGDMA induces mitochondrial damage and oxidative stress in human gingival fibroblasts. Biomaterials 2005, 26, 5130–5137. [Google Scholar] [CrossRef]
- Stanislawski, L.; Lefeuvre, M.; Bourd, K.; Soheili-Majd, E.; Goldberg, M.; Perianin, A. TEGDMA-induced toxicity in human fibroblasts is associated with early and drastic glutathione depletion with subsequent production of oxygen reactive species. J. Biomed. Mater. Res. A 2003, 66, 476–482. [Google Scholar] [CrossRef]
- Webb, K.; Hlady, V.; Tresco, P.A. Relative importance of surface wettability and charged functional groups on NIH 3T3 fibroblast attachment, spreading, and cytoskeletal organization. J. Biomed. Mater. Res. 1998, 41, 422–430. [Google Scholar] [CrossRef]
- Huang, H.H.; Ho, C.T.; Lee, T.H.; Lee, T.L.; Liao, K.K.; Chen, F.L. Effect of surface roughness of ground titanium on initial cell adhesion. Biomol. Eng. 2004, 21, 93–97. [Google Scholar] [CrossRef]
- Zareidoost, A.; Yousefpour, M.; Ghaseme, B.; Amanzadeh, A. The relationship of surface roughness and cell response of chemical surface modification of titanium. J. Mater. Sci. Mater. Med. 2012, 23, 1479–1488. [Google Scholar] [CrossRef]
- Pires, L.A.; de Meira, C.R.; Tokuhara, C.K.; de Oliveira, F.A.; Dainezi, V.B.; Zardin Graeff, M.S.; Fortulan, C.A.; de Oliveira, R.C.; Puppin-Rontani, R.M.; Borges, A.F.S. Wettability and pre-osteoblastic behavior evaluations of a dense bovine hydroxyapatite ceramics. J. Oral Sci. 2020, 62, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Suzumura, T.; Matsuura, T.; Komatsu, K.; Sugita, Y.; Maeda, H.; Ogawa, T. Vacuum Ultraviolet (VUV) Light Photofunctionalization to Induce Human Oral Fibroblast Transmigration on Zirconia. Cells 2023, 12, 2542. [Google Scholar] [CrossRef] [PubMed]
- Majhy, B.; Priyadarshini, P.; Sen, A.K. Effect of surface energy and roughness on cell adhesion and growth—Facile surface modification for enhanced cell culture. RSC Adv. 2021, 11, 15467–15476. [Google Scholar] [CrossRef] [PubMed]
- Page-McCaw, A.; Ewald, A.J.; Werb, Z. Matrix metalloproteinases and the regulation of tissue remodelling. Nat. Rev. Mol. Cell Biol. 2007, 8, 221–233. [Google Scholar] [CrossRef]
- Williams, R.C.; Skelton, A.J.; Todryk, S.M.; Rowan, A.D.; Preshaw, P.M.; Taylor, J.J. Leptin and Pro-Inflammatory Stimuli Synergistically Upregulate MMP-1 and MMP-3 Secretion in Human Gingival Fibroblasts. PLoS ONE 2016, 11, e0148024. [Google Scholar] [CrossRef]
- Beklen, A.; Ainola, M.; Hukkanen, M.; Gurgan, C.; Sorsa, T.; Konttinen, Y.T. MMPs, IL-1, and TNF are regulated by IL-17 in periodontitis. J. Dent. Res. 2007, 86, 347–351. [Google Scholar] [CrossRef]
- Zhang, Y.; Xiao, J.F.; Yang, H.F.; Jiao, Y.; Cao, W.W.; Shi, H.M.; Cun, J.F.; Tay, F.R.; Ping, J.; Xiao, Y.H. N-Acetyl Cysteine as a Novel Polymethyl Methacrylate Resin Component: Protection against Cell Apoptosis and Genotoxicity. Oxidative Med. Cell Longev. 2019, 2019, 1301736. [Google Scholar] [CrossRef]
- Nishimiya, H.; Yamada, M.; Ueda, T.; Sakurai, K. N-acetyl cysteine alleviates inflammatory reaction of oral epithelial cells to poly (methyl methacrylate) extract. Acta Odontol. Scand. 2015, 73, 616–625. [Google Scholar] [CrossRef]
- Ikeda, T.; Ueno, T.; Saruta, J.; Hirota, M.; Park, W.; Ogawa, T. Ultraviolet Treatment of Titanium to Enhance Adhesion and Retention of Oral Mucosa Connective Tissue and Fibroblasts. Int. J. Mol. Sci. 2021, 22, 12396. [Google Scholar] [CrossRef]


| Materials | Principal Compositions | Curing Modality |
|---|---|---|
| Bis-acrylic 1 (Integrity® Multi + Cure Temporary Crown and Bridge Material, Dentsply Sirona, Chariotte, NC, USA) | Acrylates and methacrylates (bis- and multifunctional) Barium boro alumino silicate glass | Dual-curing (chemical-curing and light-curing) |
| Bis-acrylic 2 (Visalys® Temp, Kettenbach GmbH & Co. KG, Eschenburg, Germany) | Aliphatic dimethacrylate, Poly(alkyleneglycol) diacrylate, hydroquinone monomethyl ether | Chemical-curing |
| Flowable composite (Aeliteflo™, BISCO Inc., Schaumburg, IL, USA) | Bis-GMA, TEGDMA | Light-curing |
| Bulk–fill composite (Aelite™ Aesthetic Enamel, BISCO Inc.) | Ytterbium Fluoride, Bis-GMA, UDMA Bis-EMA, TEGDMA | Light-curing |
| Self-curing acrylic 1 (JET Tooth Shade, Lang Dental Manufacturing Company Inc., Wheeling, IL, USA) | (liquid) MMA, N,N-Dimethyl-p-Toluidine (powder) 2-Propenoic acid, 2-methyl-, methyl ester homopolymer, Diethyl Phthalate | Chemical-curing |
| Self-curing acrylic 2 (UNIFAST™ Trad, GC, Tokyo, Japan) | (liquid) MMA, N,N-dimethyl-p-toluidine (powder) PMMA, Dibenzoyl peroxide | Chemical-curing |
| Milled acrylic (Vivid PMMA Disc, Pearson™ Dental Supply Co., Sylmar, CA, USA) | PMMA | Pre-curing (chemical-curing with high pressure and high temperature) |
| Ti alloy | Ti-6Al-4V (Grade 5) | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsuura, T.; Stavrou, S.; Komatsu, K.; Cheng, J.; Pham, A.; Ferreira, S.; Baba, T.; Chang, T.-L.; Chao, D.; Ogawa, T. Disparity in the Influence of Implant Provisional Materials on Human Gingival Fibroblasts with Different Phases of Cell Settlement: An In Vitro Study. Int. J. Mol. Sci. 2024, 25, 123. https://doi.org/10.3390/ijms25010123
Matsuura T, Stavrou S, Komatsu K, Cheng J, Pham A, Ferreira S, Baba T, Chang T-L, Chao D, Ogawa T. Disparity in the Influence of Implant Provisional Materials on Human Gingival Fibroblasts with Different Phases of Cell Settlement: An In Vitro Study. International Journal of Molecular Sciences. 2024; 25(1):123. https://doi.org/10.3390/ijms25010123
Chicago/Turabian StyleMatsuura, Takanori, Stella Stavrou, Keiji Komatsu, James Cheng, Alisa Pham, Stephany Ferreira, Tomomi Baba, Ting-Ling Chang, Denny Chao, and Takahiro Ogawa. 2024. "Disparity in the Influence of Implant Provisional Materials on Human Gingival Fibroblasts with Different Phases of Cell Settlement: An In Vitro Study" International Journal of Molecular Sciences 25, no. 1: 123. https://doi.org/10.3390/ijms25010123
APA StyleMatsuura, T., Stavrou, S., Komatsu, K., Cheng, J., Pham, A., Ferreira, S., Baba, T., Chang, T.-L., Chao, D., & Ogawa, T. (2024). Disparity in the Influence of Implant Provisional Materials on Human Gingival Fibroblasts with Different Phases of Cell Settlement: An In Vitro Study. International Journal of Molecular Sciences, 25(1), 123. https://doi.org/10.3390/ijms25010123






