Anti-Inflammatory Klotho Protein Serum Concentration Correlates with Interferon Gamma Expression Related to the Cellular Activity of Both NKT-like and T Cells in the Process of Human Aging
Abstract
1. Introduction
2. Results
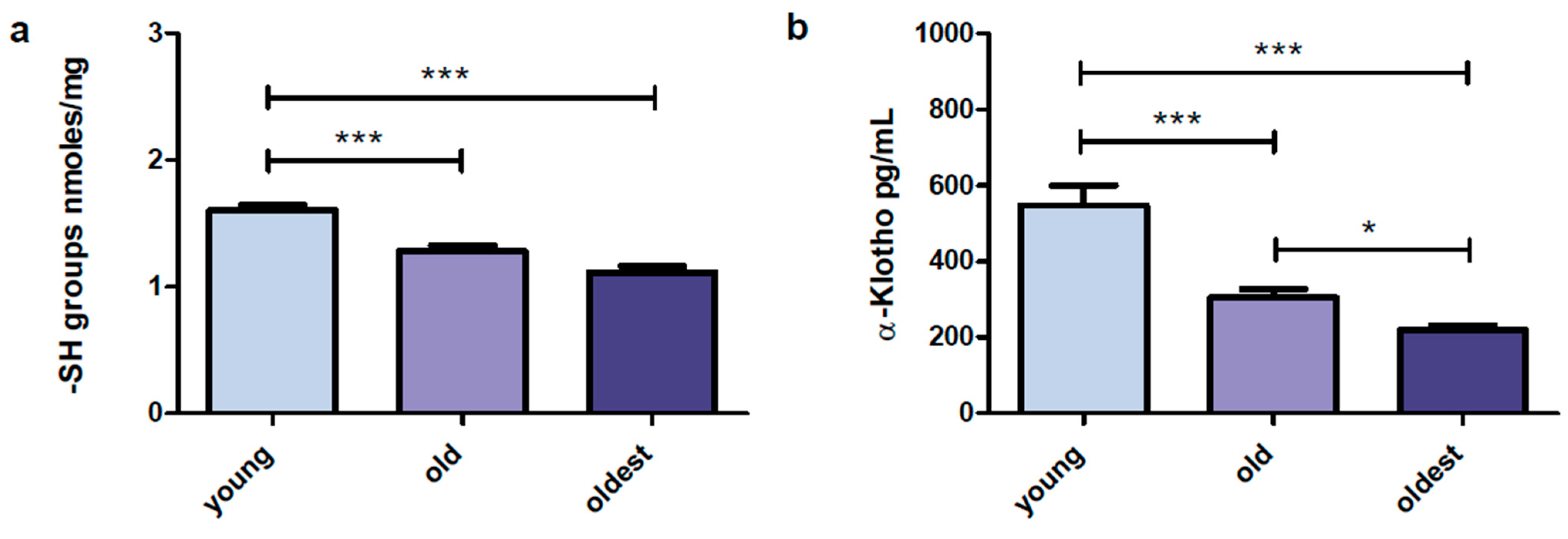
2.1. Content of Sulfhydryl (-SH) Groups in Serum Samples
2.2. α-Klotho Concentration in Serum Samples
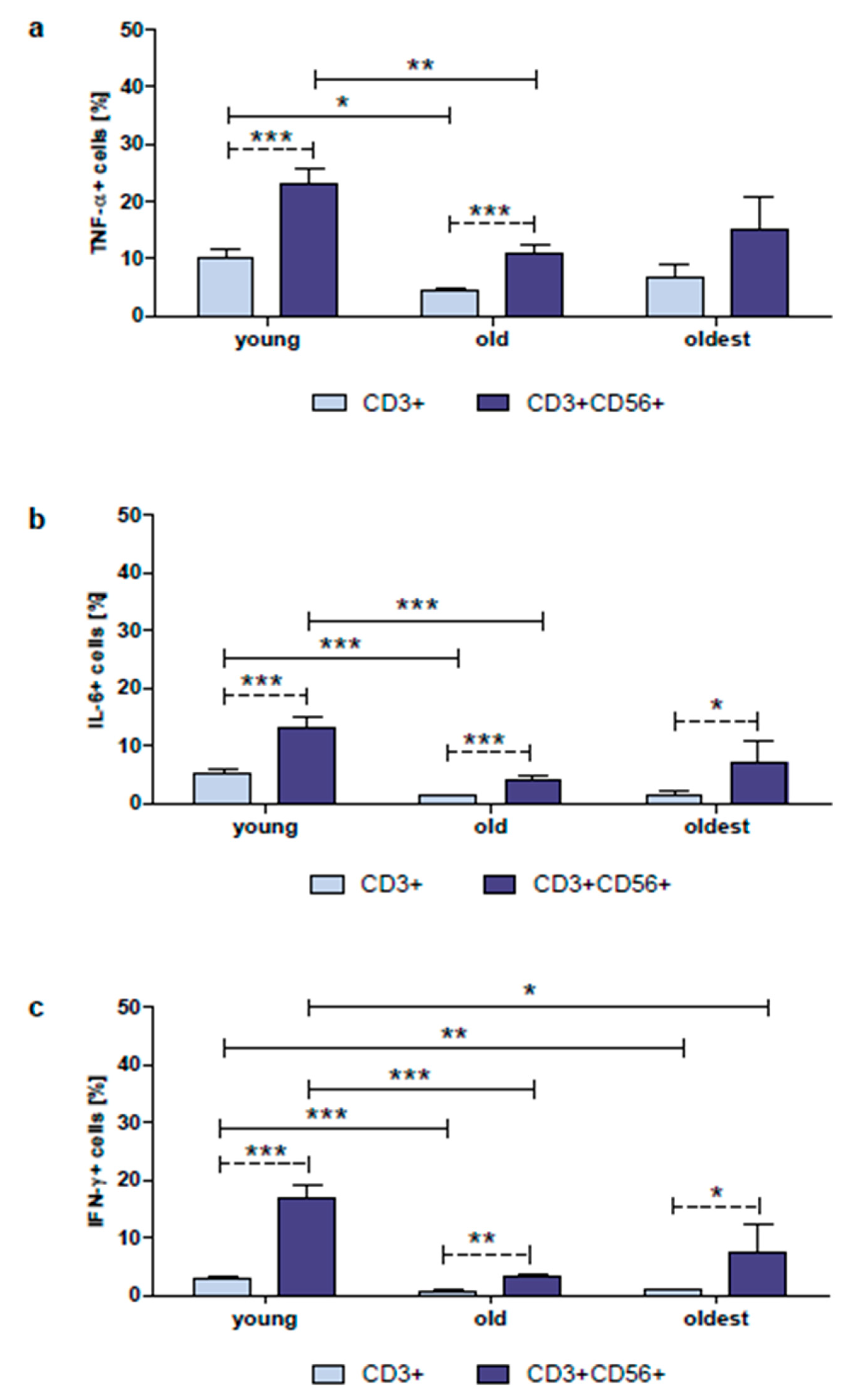
2.3. Expression of TNF-α, IL-6 and IFN-γ in Non-Cultured CD3+ and CD3+CD56+ Cells
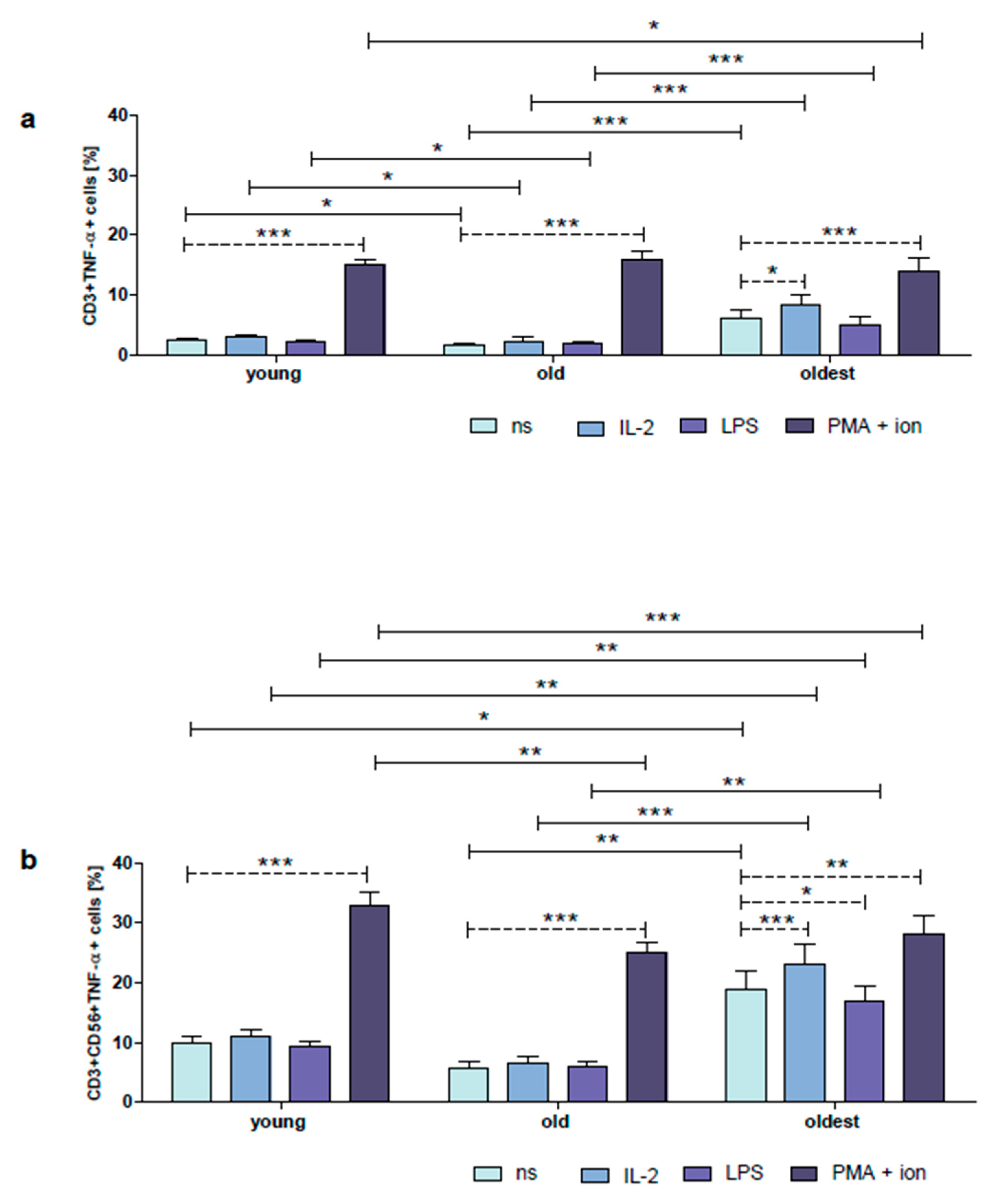
2.4. Expression of TNF-α in Cultured, Unstimulated or Stimulated with IL-2, LPS and PMA with Ionomycin CD3+ and CD3+CD56+ Cells
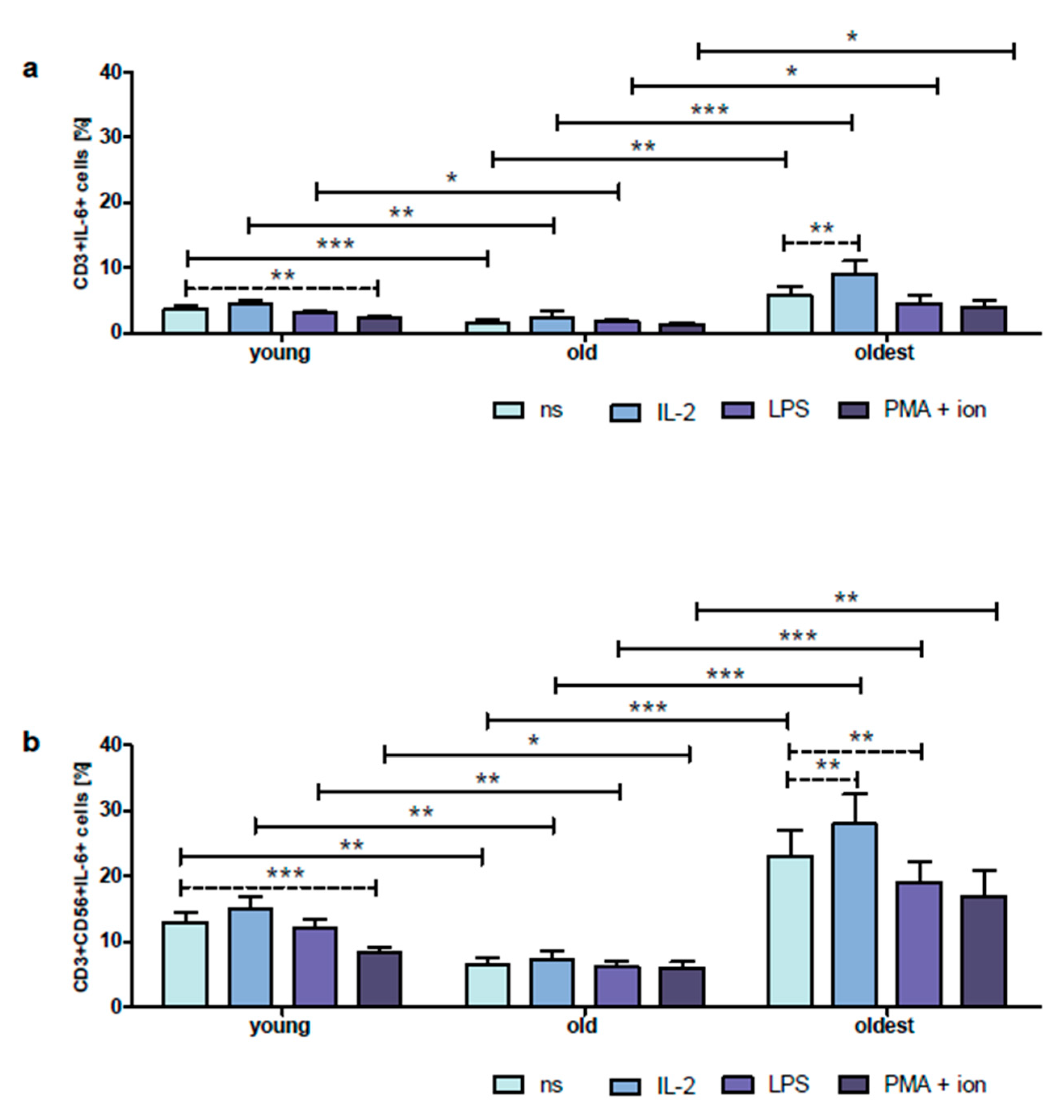
2.5. Expression of IL-6 in Cultured, Unstimulated or Stimulated with IL-2, LPS and PMA with Ionomycin CD3+ and CD3+CD56+ Cells
2.6. Expression of IFN-γ in Cultured, Non-Stimulated or Stimulated with IL-2, LPS and PMA with Ionomycin CD3+ and CD3+CD56+ Cells
2.7. Relationships between Age and Serum Concentrations of α-Klotho and -SH Groups
2.8. Relationships between the Studied Parameters Analyzed in Non-Cultured CD3+ and CD3+CD56+ Cells
2.9. Relationships between the Studied Parameters Analyzed in Cultivated CD3+ and CD3+CD56+ Cells
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. Staining of Surface and Intracellular Antigens in Whole Blood Samples for Flow Cytometry
4.3. Preparation of Peripheral Blood Mononuclear Cell Cultures
4.4. Staining of Surface and Intracellular Antigens in Peripheral Blood Mononuclear Cells for Flow Cytometry
4.5. Serum Sample Collection
4.6. Determination of the Total –SH Group Content in Serum
4.7. Determination of α-Klotho Concentration in Serum
4.8. Statistics
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fulop, T.; Larbi, A.; Pawelec, G.; Khalil, A.; Cohen, A.A.; Hirokawa, K.; Witkowski, J.M.; Franceschi, C. Immunology of Aging: The Birth of Inflammaging. Clin. Rev. Allergy Immunol. 2021, 64, 109–122. [Google Scholar] [CrossRef] [PubMed]
- Leyane, T.S.; Jere, S.W.; Houreld, N.N. Oxidative Stress in Ageing and Chronic Degenerative Pathologies: Molecular Mechanisms Involved in Counteracting Oxidative Stress and Chronic Inflammation. Int. J. Mol. Sci 2022, 23, 7273. [Google Scholar] [CrossRef] [PubMed]
- Höhn, A.; Weber, D.; Jung, T.; Ott, C.; Hugo, M.; Kochlik, B.; Kehm, R.; König, J.; Grune, T.; Castro, J.P. Happily (n)Ever after: Aging in the Context of Oxidative Stress, Proteostasis Loss and Cellular Senescence. Redox Biol. 2017, 11, 482–501. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Bonafe, M.; Valensin, S.; Olivieri, F.; De Luca, M.; Ottaviani, E.; De Benedictis, G. Inflamm-Aging. An Evolutionary Perspective on Immunosenescence. Ann. N. Y. Acad. Sci 2000, 908, 244–254. [Google Scholar] [CrossRef] [PubMed]
- Pomatto, L.C.D.; Davies, K.J.A. The Role of Declining Adaptive Homeostasis in Ageing. J. Physiol. 2017, 595, 7275. [Google Scholar] [CrossRef] [PubMed]
- Dugan, B.; Conway, J.; Duggal, N.A. Inflammaging as a Target for Healthy Ageing. Age Ageing 2023, 52, afac328. [Google Scholar] [CrossRef]
- Pattabiraman, G.; Palasiewicz, K.; Galvin, J.P.; Ucker, D.S. Aging-Associated Dysregulation of Homeostatic Immune Response Termination (and Not Initiation). Aging Cell 2017, 16, 585–593. [Google Scholar] [CrossRef]
- Fülöp, T.; Larbi, A.; Witkowski, J.M. Human Inflammaging. Gerontology 2019, 65, 495–504. [Google Scholar] [CrossRef]
- Cunha, L.L.; Perazzio, S.F.; Azzi, J.; Cravedi, P.; Riella, L.V. Remodeling of the Immune Response with Aging: Immunosenescence and Its Potential Impact on COVID-19 Immune Response. Front. Immunol. 2020, 11, 1748. [Google Scholar] [CrossRef]
- Ferrucci, L.; Corsi, A.; Lauretani, F.; Bandinelli, S.; Bartali, B.; Taub, D.D.; Guralnik, J.M.; Longo, D.L. The Origins of Age-Related Proinflammatory State. Blood 2005, 105, 2294–2299. [Google Scholar] [CrossRef]
- Sendama, W. The Effect of Ageing on the Resolution of Inflammation. Ageing Res. Rev. 2020, 57, 101000. [Google Scholar] [CrossRef] [PubMed]
- Fulop, T. Immunosenescence Is Both Functional/Adaptive and Dysfunctional/Maladaptive. Semin. Immunopathol. 2020, 42, 521–536. [Google Scholar] [CrossRef] [PubMed]
- Tohyama, O.; Imura, A.; Iwano, A.; Freund, J.N.; Henrissat, B.; Fujimori, T.; Nabeshima, Y.I. Klotho Is a Novel β-Glucuronidase Capable of Hydrolyzing Steroid β-Glucuronides. J. Biol. Chem. 2004, 279, 9777–9784. [Google Scholar] [CrossRef]
- Dalton, G.D.; Xie, J.; An, S.W.; Huang, C.L. New Insights into the Mechanism of Action of Soluble Klotho. Front. Endocrinol. 2017, 8, 323. [Google Scholar] [CrossRef]
- Typiak, M.; Piwkowska, A. Antiinflammatory Actions of Klotho: Implications for Therapy of Diabetic Nephropathy. Int. J. Mol. Sci. 2021, 22, 956. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.; Groen, A.; Molostvov, G.; Lu, T.; Lilley, K.S.; Snead, D.; James, S.; Wilkinson, I.B.; Ting, S.; Hsiao, L.L.; et al. A-Klotho Expression in Human Tissues. J. Clin. Endocrinol. Metab. 2015, 100, E1308–E1318. [Google Scholar] [CrossRef]
- Cheikhi, A.; Barchowsky, A.; Sahu, A.; Shinde, S.N.; Pius, A.; Clemens, Z.J.; Li, H.; Kennedy, C.A.; Hoeck, J.D.; Franti, M.; et al. Klotho: An Elephant in Aging Research. J. Gerontol.—Ser. A Biol. Sci. Med. Sci. 2019, 74, 1031–1042. [Google Scholar] [CrossRef]
- Witkowski, J.M.; Soroczyńska-Cybula, M.; Bryl, E.; Smoleńska, Ż.; Jóźwik, A. Klotho—A Common Link in Physiological and Rheumatoid Arthritis-Related Aging of Human CD4+ Lymphocytes. J. Immunol. 2007, 178, 771–777. [Google Scholar] [CrossRef]
- Mytych, J.; Romerowicz-Misielak, M.; Koziorowski, M. Klotho Protects Human Monocytes from LPS-Induced Immune Impairment Associated with Immunosenescent-like Phenotype. Mol. Cell Endocrinol. 2018, 470, 1–13. [Google Scholar] [CrossRef]
- Imura, A.; Iwano, A.; Tohyama, O.; Tsuji, Y.; Nozaki, K.; Hashimoto, N.; Fujimori, T.; Nabeshima, Y.I. Secreted Klotho Protein in Sera and CSF: Implication for Post-Translational Cleavage in Release of Klotho Protein from Cell Membrane. FEBS Lett. 2004, 565, 143–147. [Google Scholar] [CrossRef]
- Abraham, C.R.; Li, A. Aging-Suppressor Klotho: Prospects in Diagnostics and Therapeutics. Ageing Res. Rev. 2022, 82, 101766. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Wu, S.; Ren, H.; Gu, J. Klotho Suppresses RIG-I-Mediated Senescence-Associated Inflammation. Nat. Cell Biol. 2011, 13, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Cui, W.; Leng, B.; Wang, G. Klotho Protein Inhibits H2O2-Induced Oxidative Injury in Endothelial Cells via Regulation of PI3K/AKT/Nrf2/HO-1 Pathways. Can. J. Physiol. Pharmacol. 2019, 97, 370–376. [Google Scholar] [CrossRef]
- Romero, A.; San Hipólito-Luengo, Á.; Villalobos, L.A.; Vallejo, S.; Valencia, I.; Michalska, P.; Pajuelo-Lozano, N.; Sánchez-Pérez, I.; León, R.; Bartha, J.L.; et al. The Angiotensin-(1-7)/Mas Receptor Axis Protects from Endothelial Cell Senescence via Klotho and Nrf2 Activation. Aging Cell 2019, 18, e12913. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Li, Z.; Li, B.; Zhu, X.; Lai, X. Klotho Improves Diabetic Cardiomyopathy by Suppressing the NLRP3 Inflammasome Pathway. Life Sci. 2019, 234, 116773. [Google Scholar] [CrossRef] [PubMed]
- Romero, A.; Dongil, P.; Valencia, I.; Vallejo, S.; Hipólito Luengo, Á.S.; Díaz-Aray, G.; Bartha, J.L.; González-Arlanzón, M.M.; Rivilla, F.; De La Cuesta, F.; et al. Pharmacological Blockade of NLRP3 Inflammasome/IL1β-Positive Loop Mitigates Endothelial Cell Senescence and Dysfunction. Aging Dis. 2022, 13, 284–297. [Google Scholar] [CrossRef]
- Martín-Núñez, E.; Pérez-Castro, A.; Tagua, V.G.; Hernández-Carballo, C.; Ferri, C.; Pérez-Delgado, N.; Rodríguez-Ramos, S.; Cerro-López, P.; López-Castillo, Á.; Delgado-Molinos, A.; et al. Klotho Expression in Peripheral Blood Circulating Cells Is Associated with Vascular and Systemic Inflammation in Atherosclerotic Vascular Disease. Sci. Rep. 2022, 12, 8422. [Google Scholar] [CrossRef]
- Michel, J.J.; Griffin, P.; Vallejo, A.N. Functionally Diverse NK-like T Cells Are Effectors and Predictors of Successful Aging. Front. Immunol. 2016, 7, 530. [Google Scholar] [CrossRef]
- Kaszubowska, L. Telomere Shortening and Ageing of the Immune System. J. Physiol. Pharmacol. 2008, 59, 169–186. [Google Scholar]
- Marrella, V.; Facoetti, A.; Cassani, B. Cellular Senescence in Immunity against Infections. Int. J. Mol. Sci. 2022, 23, 11845. [Google Scholar] [CrossRef]
- Miller, J.P.; Allman, D. The Decline in B Lymphopoiesis in Aged Mice Reflects Loss of Very Early B-Lineage Precursors. J. Immunol. 2003, 171, 2326–2330. [Google Scholar] [CrossRef] [PubMed]
- Frasca, D.; Riley, R.L.; Blomberg, B.B. Effect of Age on the Immunoglobulin Class Switch. Crit. Rev. Immunol. 2004, 24, 297–320. [Google Scholar] [CrossRef]
- Huang, H.; Patel, D.D.; Manton, K.G. The Immune System in Aging: Roles of Cytokines, T Cells and NK Cells. Front. Biosci. 2005, 10, 192–215. [Google Scholar] [CrossRef] [PubMed]
- Lemster, B.H.; Michel, J.J.; Montag, D.T.; Paat, J.J.; Studenski, S.A.; Newman, A.B.; Vallejo, A.N. Induction of CD56 and TCR-Independent Activation of T Cells with Aging. J. Immunol. 2008, 180, 1979–1990. [Google Scholar] [CrossRef]
- Abedin, S.; Michel, J.J.; Lemster, B.; Vallejo, A.N. Diversity of NKR Expression in Aging T Cells and in T Cells of the Aged: The New Frontier into the Exploration of Protective Immunity in the Elderly. Exp. Gerontol. 2005, 40, 537–548. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Cui, X.; Cui, C.; Zhang, J.; Zhou, F.; Zhang, Z.; Fu, Y.; Xu, J.; Chu, Z.; Liu, J.; et al. The Function of CD3+CD56+ NKT-like Cells in HIV-Infected Individuals. Biomed. Res. Int. 2014, 2014, 863625. [Google Scholar] [CrossRef]
- Almeida, J.; Casanova, M.; Santos-rosa, M.; Tarazona, R.; Solana, R.; Rodrigues-santos, P. Natural Killer T-like Cells: Immunobiology and Role in Disease. Int. J. Mol. Sci. 2023, 24, 2743. [Google Scholar] [CrossRef]
- Peralbo, E.; Alonso, C.; Solana, R. Invariant NKT and NKT-like Lymphocytes: Two Different T Cell Subsets That Are Differentially Affected by Ageing. Exp. Gerontol. 2007, 42, 703–708. [Google Scholar] [CrossRef]
- Brennan, P.J.; Brigl, M.; Brenner, M.B. Invariant Natural Killer T Cells: An Innate Activation Scheme Linked to Diverse Effector Functions. Nat. Rev. Immunol. 2013, 13, 101–117. [Google Scholar] [CrossRef]
- Vallejo, A.N.; Hamel, D.L.; Mueller, R.G.; Ives, D.G.; Michel, J.J.; Boudreau, R.M.; Newman, A.B. Nk-like T Cells and Plasma Cytokines, but Not Anti-Viral Serology, Define Immune Fingerprints of Resilience and Mild Disability in Exceptional Aging. PLoS ONE 2011, 6, e26558. [Google Scholar] [CrossRef]
- Mehta, A.K.; Gracias, D.T.; Croft, M. TNF Activity and T Cells. Cytokine 2018, 101, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Croft, M. The Role of TNF Superfamily Members in T-Cell Function and Diseases. Nat. Rev. Immunol. 2009, 9, 271–285. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.S.; Mao, F.Y.; Zhao, Y.L.; Wang, T.T.; Chen, N.; Zhang, J.Y.; Cheng, P.; Li, W.H.; Lv, Y.P.; Teng, Y.S.; et al. Altered Phenotypic and Functional Characteristics of CD3+CD56+ NKT-like Cells in Human Gastric Cancer. Oncotarget 2016, 7, 55222–55230. [Google Scholar] [CrossRef] [PubMed]
- Lacy, P.; Stow, J.L. Cytokine Release from Innate Immune Cells: Association with Diverse Membrane Trafficking Pathways. Blood 2011, 118, 9–18. [Google Scholar] [CrossRef]
- Dorronsoro, A.; Lang, V.; Ferrin, I.; Fernández-Rueda, J.; Zabaleta, L.; Pérez-Ruiz, E.; Sepúlveda, P.; Trigueros, C. Intracellular Role of IL-6 in Mesenchymal Stromal Cell Immunosuppression and Proliferation. Sci. Rep. 2020, 10, 21853. [Google Scholar] [CrossRef]
- Cifaldi, L.; Prencipe, G.; Caiello, I.; Bracaglia, C.; Locatelli, F.; De Benedetti, F.; Strippoli, R. Inhibition of Natural Killer Cell Cytotoxicity by Interleukin-6 Implications for the Pathogenesis of Macrophage Activation Syndrome. Arthritis Rheumatol. 2015, 67, 3037–3046. [Google Scholar] [CrossRef]
- Ochayon, D.E.; Waggoner, S.N. The Effect of Unconventional Cytokine Combinations on NK-Cell Responses to Viral Infection. Front. Immunol. 2021, 12, 645850. [Google Scholar] [CrossRef]
- Burke, J.D.; Young, H.A. IFN-Γ: A Cytokine at the Right Time, Is in the Right Place. Semin. Immunol. 2019, 43, 101280. [Google Scholar] [CrossRef]
- Jorgovanovic, D.; Song, M.; Wang, L.; Zhang, Y. Roles of IFN-Γin Tumor Progression and Regression: A Review. Biomark. Res. 2020, 8, 49. [Google Scholar] [CrossRef]
- Nirschl, C.J.; Suárez-Fariñas, M.; Izar, B.; Prakadan, S.; Dannenfelser, R.; Tirosh, I.; Liu, Y.; Zhu, Q.; Devi, K.S.P.; Carroll, S.L.; et al. IFNγ-Dependent Tissue-Immune Homeostasis Is Co-Opted in the Tumor Microenvironment. Cell 2017, 170, 127–141.e15. [Google Scholar] [CrossRef]
- Gocher, A.M.; Workman, C.J.; Vignali, D.A.A. Interferon-γ: Teammate or Opponent in the Tumour Microenvironment? Nat. Rev. Immunol. 2022, 22, 158–172. [Google Scholar] [CrossRef] [PubMed]
- Lissoni, P.; Messina, G.; Pelizzoni, F.; Rovelli, F.; Brivio, F.; Monzon, A.; Crivelli, N.; Lissoni, A.; Tassoni, S.; Sassola, A.; et al. The Fascination of Cytokine Immunological Science. J. Infect. 2020, 3, 18–28. [Google Scholar] [CrossRef]
- Solana, R.; Tarazona, R.; Gayoso, I.; Lesur, O.; Dupuis, G.; Fulop, T. Innate Immunosenescence: Effect of Aging on Cells and Receptors of the Innate Immune System in Humans. Semin. Immunol. 2012, 24, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Fülöp, T.; Larbi, A.; Pawelec, G. Human T Cell Aging and the Impact of Persistent Viral Infections. Front. Immunol. 2013, 4, 271. [Google Scholar] [CrossRef] [PubMed]
- Fulop, T.; Larbi, A.; Dupuis, G.; Le Page, A.; Frost, E.H.; Cohen, A.A.; Witkowski, J.M.; Franceschi, C. Immunosenescence and Inflamm-Aging as Two Sides of the Same Coin: Friends or Foes? Front. Immunol. 2018, 8, 1960. [Google Scholar] [CrossRef]
- Di Bona, D.; Accardi, G.; Virruso, C.; Candore, G.; Caruso, C. Association of Klotho Polymorphisms with Healthy Aging: A Systematic Review and Meta-Analysis. Rejuven. Res. 2014, 17, 212–216. [Google Scholar] [CrossRef]
- Shardell, M.; Semba, R.D.; Kalyani, R.R.; Bandinelli, S.; Prather, A.A.; Chia, C.W.; Ferrucci, L. Plasma Klotho and Frailty in Older Adults: Findings from the InCHIANTI Study. J. Gerontol.—Ser. A Biol. Sci. Med. Sci. 2019, 74, 1052–1058. [Google Scholar] [CrossRef]
- Yamazaki, Y.; Imura, A.; Urakawa, I.; Shimada, T.; Murakami, J.; Aono, Y.; Hasegawa, H.; Yamashita, T.; Nakatani, K.; Saito, Y.; et al. Establishment of Sandwich ELISA for Soluble Alpha-Klotho Measurement: Age-Dependent Change of Soluble Alpha-Klotho Levels in Healthy Subjects. Biochem. Biophys. Res. Commun. 2010, 398, 513–518. [Google Scholar] [CrossRef]
- Pedersen, L.; Pedersen, S.M.; Brasen, C.L.; Rasmussen, L.M. Soluble Serum Klotho Levels in Healthy Subjects. Comparison of Two Different Immunoassays. Clin. Biochem. 2013, 46, 1079–1083. [Google Scholar] [CrossRef]
- Droge, W.; Kinscherf, R.; Hildebrandt, W.; Schmitt, T. The Deficit in Low Molecular Weight Thiols as a Target for Antiageing Therapy. Curr. Drug Targets 2012, 7, 1505–1512. [Google Scholar] [CrossRef]
- Andriollo-Sanchez, M.; Hininger-Favier, I.; Meunier, N.; Venneria, E.; O’Connor, J.M.; Maiani, G.; Coudray, C.; Roussel, A.M. Age-Related Oxidative Stress and Antioxidant Parameters in Middle-Aged and Older European Subjects: The ZENITH Study. Eur. J. Clin. Nutr. 2005, 59, S58–S62. [Google Scholar] [CrossRef] [PubMed]
- Kaszubowska, L.; Kaczor, J.J.; Hak, L.; Dettlaff-Pokora, A.; Szarynska, M.; Kmiec, Z. Sensitivity of Natural Killer Cells to Activation in the Process of Ageing Is Related to the Oxidative and Inflammatory Status of the Elderly. J. Physiol. Pharmacol. 2011, 62, 101–109. [Google Scholar] [PubMed]
- Guia, S.; Cognet, C.; De Beaucoudrey, L.; Tessmer, M.S.; Jouanguy, E.; Berger, C.; Filipe-Santos, O.; Feinberg, J.; Camcioglu, Y.; Levy, J.; et al. A Role for Interleukin-12/23 in the Maturation of Human Natural Killer and CD56+ T Cells in Vivo. Blood 2008, 111, 5008–5016. [Google Scholar] [CrossRef] [PubMed]
- Kaszubowska, L.; Foerster, J.; Kmieć, Z. NKT-like (CD3 + CD56+) Cells Differ from T Cells in Expression Level of Cellular Protective Proteins and Sensitivity to Stimulation in the Process of Ageing. Immun. Ageing 2022, 19, 18. [Google Scholar] [CrossRef] [PubMed]
- Simmons, S.O.; Fan, C.Y.; Ramabhadran, R. Cellular Stress Response Pathway System as a Sentinel Ensemble in Toxicological Screening. Toxicol. Sci. 2009, 111, 202–225. [Google Scholar] [CrossRef] [PubMed]
- Kaszubowska, L.; Foerster, J.; Kaczor, J.J.; Schetz, D.; Ślebioda, T.J.; Kmieć, Z. Expression of Cellular Protective Proteins SIRT1, HSP70 and SOD2 Correlates with Age and Is Significantly Higher in NK Cells of the Oldest Seniors. Immun. Ageing 2017, 14, 3. [Google Scholar] [CrossRef]
- Schindowski, K.; Fröhlich, L.; Maurer, K.; Müller, W.E.; Eckert, A. Age-Related Impairment of Human T Lymphocytes’ Activation: Specific Differences between CD4+ and CD8+ Subsets. Mech. Ageing Dev. 2002, 123, 375–390. [Google Scholar] [CrossRef]
- Hassouneh, F.; Goldeck, D.; Pera, A.; van Heemst, D.; Eline Slagboom, P.; Pawelec, G.; Solana, R. Functional Changes of T-Cell Subsets with Age and Cmv Infection. Int. J. Mol. Sci 2021, 22, 9973. [Google Scholar] [CrossRef]
- Alberro, A.; Iribarren-Lopez, A.; Sáenz-Cuesta, M.; Matheu, A.; Vergara, I.; Otaegui, D. Inflammaging Markers Characteristic of Advanced Age Show Similar Levels with Frailty and Dependency. Sci. Rep. 2021, 11, 4358. [Google Scholar] [CrossRef]
- Liao, W.; Lin, J.-X.; Leonard, W.J. Interleukin-2 at the Crossroads of Effector Responses, Tolerance, and Immunotherapy. Immunity 2013, 38, 13–25. [Google Scholar] [CrossRef]
- Wu, Y.; Tian, Z.; Wei, H. Developmental and Functional Control of Natural Killer Cells by Cytokines. Front. Immunol. 2017, 8, 930. [Google Scholar] [CrossRef] [PubMed]
- Bessoles, S.; Fouret, F.; Dudal, S.; Besra, G.S.; Sanchez, F.; Lafont, V. IL-2 Triggers Specific Signaling Pathways in Human NKT Cells Leading to the Production of pro- and Anti-Inflammatory Cytokines. J. Leukoc. Biol. 2008, 84, 224–233. [Google Scholar] [CrossRef]
- Kanevskiy, L.M.; Telford, W.G.; Sapozhnikov, A.M.; Kovalenko, E.I. Lipopolysaccharide Induces IFN-γ Production in Human NK Cells. Front. Immunol. 2013, 4, 11. [Google Scholar] [CrossRef]
- Mcaleer, J.P.; Vella, A.T. Understanding How Lipopolysaccharide Impacts CD4 T Cell Immunity. Crit. Rev. Immunol. 2008, 28, 281–299. [Google Scholar] [PubMed]
- Purvis, H.A.; Stoop, J.N.; Mann, J.; Woods, S.; Kozijn, A.E.; Hambleton, S.; Robinson, J.H.; Isaacs, J.D.; Anderson, A.E.; Hilkens, C.M.U. Low-Strength T-Cell Activation Promotes Th17 Responses. Blood 2010, 116, 4829–4837. [Google Scholar] [CrossRef]
- Hou, H.; Zhou, Y.; Yu, J.; Mao, L.; Bosco, M.J.; Wang, J.; Lu, Y.; Mao, L.; Wu, X.; Wang, F.; et al. Establishment of the Reference Intervals of Lymphocyte Function in Healthy Adults Based on IFN-γ Secretion Assay upon Phorbol-12-Myristate-13-Acetate/Ionomycin Stimulation. Front. Immunol. 2018, 9, 172. [Google Scholar] [CrossRef]
- Romera-Cárdenas, G.; Thomas, L.M.; Lopez-Cobo, S.; García-Cuesta, E.M.; Long, E.O.; Reyburn, H.T. Ionomycin Treatment Renders NK Cells Hyporesponsive. PLoS ONE 2016, 11, e0150998. [Google Scholar] [CrossRef]
- Chopra, R.K.; Nagel, J.E.; Chrest, F.J.; Immunology, W.H.A.C. Impaired Phorbol Ester and Calcium Ionophore Induced Proliferation of T Cells from Old Humans. Clin. Exp. Immunol. 1987, 70, 456–462. [Google Scholar] [PubMed]
- Kaszubowska, L.; Foerster, J.; Kaczor, J.J.; Schetz, D.; Ślebioda, T.J.; Kmieć, Z. NK Cells of the Oldest Seniors Represent Constant and Resistant to Stimulation High Expression of Cellular Protective Proteins SIRT1 and HSP70. Immun. Ageing 2018, 15, 12. [Google Scholar] [CrossRef]
- Van Epps, P.; Banks, R.; Aung, H.; Betts, M.R.; Canaday, D.H. Age-Related Differences in Polyfunctional T Cell Responses. Immun. Ageing 2014, 11, 14. [Google Scholar] [CrossRef] [PubMed]
- van der Geest, K.S.M.; Kroesen, B.J.; Horst, G.; Abdulahad, W.H.; Brouwer, E.; Boots, A.M.H. Impact of Aging on the Frequency, Phenotype, and Function of CD161-Expressing T Cells. Front. Immunol. 2018, 9, 752. [Google Scholar] [CrossRef] [PubMed]
- Bernin, H.; Fehling, H.; Marggraff, C.; Tannich, E.; Lotter, H. The Cytokine Profile of Human NKT Cells and PBMCs Is Dependent on Donor Sex and Stimulus. Med. Microbiol. Immunol. 2016, 205, 321–332. [Google Scholar] [CrossRef] [PubMed]
- Cossu, M.; Van Bon, L.; Nierkens, S.; Bellocchi, C.; Santaniello, A.; Dolstra, H.; Beretta, L.; Radstake, T.R.D.J. The Magnitude of Cytokine Production by Stimulated CD56+ Cells Is Associated with Early Stages of Systemic Sclerosis. Clin. Immunol. 2016, 173, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Michel, J.J.; Turesson, C.; Lemster, B.; Atkins, S.R.; Iclozan, C.; Bongartz, T.; Wasko, M.C.; Matteson, E.L.; Vallejo, A.N. CD56-Expressing T Cells That Have Features of Senescence Are Expanded in Rheumatoid Arthritis. Arthritis Rheum. 2007, 56, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Correia, M.P.; Costa, A.V.; Uhrberg, M.; Cardoso, E.M.; Arosa, F.A. IL-15 Induces CD8+ T Cells to Acquire Functional NK Receptors Capable of Modulating Cytotoxicity and Cytokine Secretion. Immunobiology 2011, 216, 604–612. [Google Scholar] [CrossRef]
- Takayama, E.; Koike, Y.; Ohkawa, T.; Majima, T.; Fukasawa, M.; Shinomiya, N.; Yamaguchi, T.; Konishi, M.; Hiraide, H.; Tadakuma, T.; et al. Functional and Vβ Repertoire Characterization of Human CD8+ T-Cell Subsets with Natural Killer Cell Markers, CD56+ CD57- T Cells, CD56+ CD57+ T Cells and CD56- CD57+ T Cells. Immunology 2003, 108, 211–219. [Google Scholar] [CrossRef]
- Frenay, A.R.S.; de Borst, M.H.; Bachtler, M.; Tschopp, N.; Keyzer, C.A.; van den Berg, E.; Bakker, S.J.L.; Feelisch, M.; Pasch, A.; van Goor, H. Serum Free Sulfhydryl Status Is Associated with Patient and Graft Survival in Renal Transplant Recipients. Free Radic. Biol. Med. 2016, 99, 345–351. [Google Scholar] [CrossRef]
- Hotamisligil, G.S.; Davis, R.J. Cell Signaling and Stress Responses. Cold Spring Harb. Perspect. Biol. 2016, 8, a006072. [Google Scholar] [CrossRef]
- Nakiboneka, R.; Mugaba, S.; Auma, B.O.; Kintu, C.; Lindan, C.; Nanteza, M.B.; Kaleebu, P.; Serwanga, J. Interferon Gamma (IFN-γ) Negative CD4+ and CD8+ T-Cells Can Produce Immune Mediators in Response to Viral Antigens. Vaccine 2019, 37, 113–122. [Google Scholar] [CrossRef]
- Lee, J.; Park, K.H.; Ryu, J.H.; Bae, H.J.; Choi, A.; Lee, H.; Lim, J.; Han, K.; Park, C.H.; Jung, E.S.; et al. Natural Killer Cell Activity for IFN-Gamma Production as a Supportive Diagnostic Marker for Gastric Cancer. Oncotarget 2017, 8, 70431–70440. [Google Scholar] [CrossRef]
- Zhu, Y.; Song, D.; Song, Y.; Wang, X. Interferon Gamma Induces Inflammatory Responses through the Interaction of CEACAM1 and PI3K in Airway Epithelial Cells. J. Transl. Med. 2019, 17, 147. [Google Scholar] [CrossRef] [PubMed]
- Güzel, M.; Nazıroğlu, M.; Akpınar, O.; Çınar, R. Interferon Gamma-Mediated Oxidative Stress Induces Apoptosis, Neuroinflammation, Zinc Ion Influx, and TRPM2 Channel Activation in Neuronal Cell Line: Modulator Role of Curcumin. Inflammation 2021, 44, 1878–1894. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J. Yin and Yang Interplay of IFN- g in Inflammation and Autoimmune Disease Find the Latest Version: Yin and Yang Interplay of IFN- γ in Inflammation and Autoimmune Disease. J. Clin. Investig. 2007, 117, 871–873. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Oh, J.; Choi, J.Y.; Jang, J.Y.; Kang, M.W.; Lee, C.E. Identification of Human Thioredoxin as a Novel IFN-Gamma-Induced Factor: Mechanism of Induction and Its Role in Cytokine Production. BMC Immunol. 2008, 9, 64. [Google Scholar] [CrossRef]
- Seifert, U.; Bialy, L.P.; Ebstein, F.; Bech-Otschir, D.; Voigt, A.; Schröter, F.; Prozorovski, T.; Lange, N.; Steffen, J.; Rieger, M.; et al. Immunoproteasomes Preserve Protein Homeostasis upon Interferon-Induced Oxidative Stress. Cell 2010, 142, 613–624. [Google Scholar] [CrossRef]
- Voigt, A.; Rahnefeld, A.; Kloetzel, P.M.; Krüger, E. Cytokine-Induced Oxidative Stress in Cardiac Inflammation and Heart Failure-How the Ubiquitin Proteasome System Targets This Vicious Cycle. Front. Physiol. 2013, 4, 42. [Google Scholar] [CrossRef]
- Kaszubowska, L.; Foerster, J.; Kwiatkowski, P.; Schetz, D. NKT-like Cells Reveal Higher than T Lymphocytes Expression of Cellular Protective Proteins HSP70 and SOD2 and Comparably Increased Expression of SIRT1 in the Oldest Seniors. Folia Histochem. Cytobiol. 2018, 56, 231–240. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-Mental State”. A Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatry Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of Illness in the Aged. The Index of Adl: A Standardized Measure of Biological and Psychosocial Function. JAMA 1963, 185, 914–919. [Google Scholar] [CrossRef]

| Cell Population | CD3+ [%] | CD3+CD56+ [%] | ||||
|---|---|---|---|---|---|---|
| Parameter | TNF-α “0” | IL-6 “0” | IFN-γ “0” | TNF-α “0” | IL-6 “0” | IFN-γ “0” |
| α-Klotho | ns | ns | 0.37 ** | ns | ns | 0.34 ** |
| SH groups | 0.29 * | 0.38 ** | 0.4 ** | 0.41 ** | 0.45 *** | 0.36 ** |
| Age | ns | −0.32 * | −0.52 *** | ns | −0.31* | −0.46 *** |
| Cell Population | CD3+ [%] | CD3+CD56+ [%] | |||||
|---|---|---|---|---|---|---|---|
| Parameter | Stimulation Type | TNF-α | IL-6 | IFN-γ | TNF-α | IL-6 | IFN-γ |
| α-Klotho | none | ns | ns | 0.34 ** | ns | ns | 0.25 * |
| IL-2 | ns | ns | 0.44 *** | ns | ns | 0.35 ** | |
| LPS | ns | ns | 0.49 *** | ns | ns | 0.39 *** | |
| PMA+ion | ns | ns | 0.22 * | ns | ns | 0.32 ** | |
| -SH groups | none | ns | ns | 0.3 ** | ns | ns | ns |
| IL-2 | ns | ns | 0.36 ** | ns | ns | 0.22 * | |
| LPS | ns | ns | 0.34 ** | ns | ns | ns | |
| PMA+ion | ns | ns | ns | ns | ns | ns | |
| Age | none | ns | ns | −0.32 ** | ns | ns | −0.24 * |
| IL-2 | 0.23 * | ns | −0.37 *** | ns | ns | −0.26 * | |
| LPS | 0.26 ** | ns | −0.4 *** | ns | ns | −0.23 * | |
| PMA+ion | ns | ns | −0.33 *** | ns | ns | −0.42 *** | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaszubowska, L.; Foerster, J.; Kaczor, J.J.; Karnia, M.J.; Kmieć, Z. Anti-Inflammatory Klotho Protein Serum Concentration Correlates with Interferon Gamma Expression Related to the Cellular Activity of Both NKT-like and T Cells in the Process of Human Aging. Int. J. Mol. Sci. 2023, 24, 8393. https://doi.org/10.3390/ijms24098393
Kaszubowska L, Foerster J, Kaczor JJ, Karnia MJ, Kmieć Z. Anti-Inflammatory Klotho Protein Serum Concentration Correlates with Interferon Gamma Expression Related to the Cellular Activity of Both NKT-like and T Cells in the Process of Human Aging. International Journal of Molecular Sciences. 2023; 24(9):8393. https://doi.org/10.3390/ijms24098393
Chicago/Turabian StyleKaszubowska, Lucyna, Jerzy Foerster, Jan Jacek Kaczor, Mateusz Jakub Karnia, and Zbigniew Kmieć. 2023. "Anti-Inflammatory Klotho Protein Serum Concentration Correlates with Interferon Gamma Expression Related to the Cellular Activity of Both NKT-like and T Cells in the Process of Human Aging" International Journal of Molecular Sciences 24, no. 9: 8393. https://doi.org/10.3390/ijms24098393
APA StyleKaszubowska, L., Foerster, J., Kaczor, J. J., Karnia, M. J., & Kmieć, Z. (2023). Anti-Inflammatory Klotho Protein Serum Concentration Correlates with Interferon Gamma Expression Related to the Cellular Activity of Both NKT-like and T Cells in the Process of Human Aging. International Journal of Molecular Sciences, 24(9), 8393. https://doi.org/10.3390/ijms24098393







