Sex Differences in Sphingosine-1-Phosphate Levels Are Dependent on Ceramide Synthase 1 and Ceramidase in Lung Physiology and Tumor Conditions
Abstract
1. Introduction
2. Results
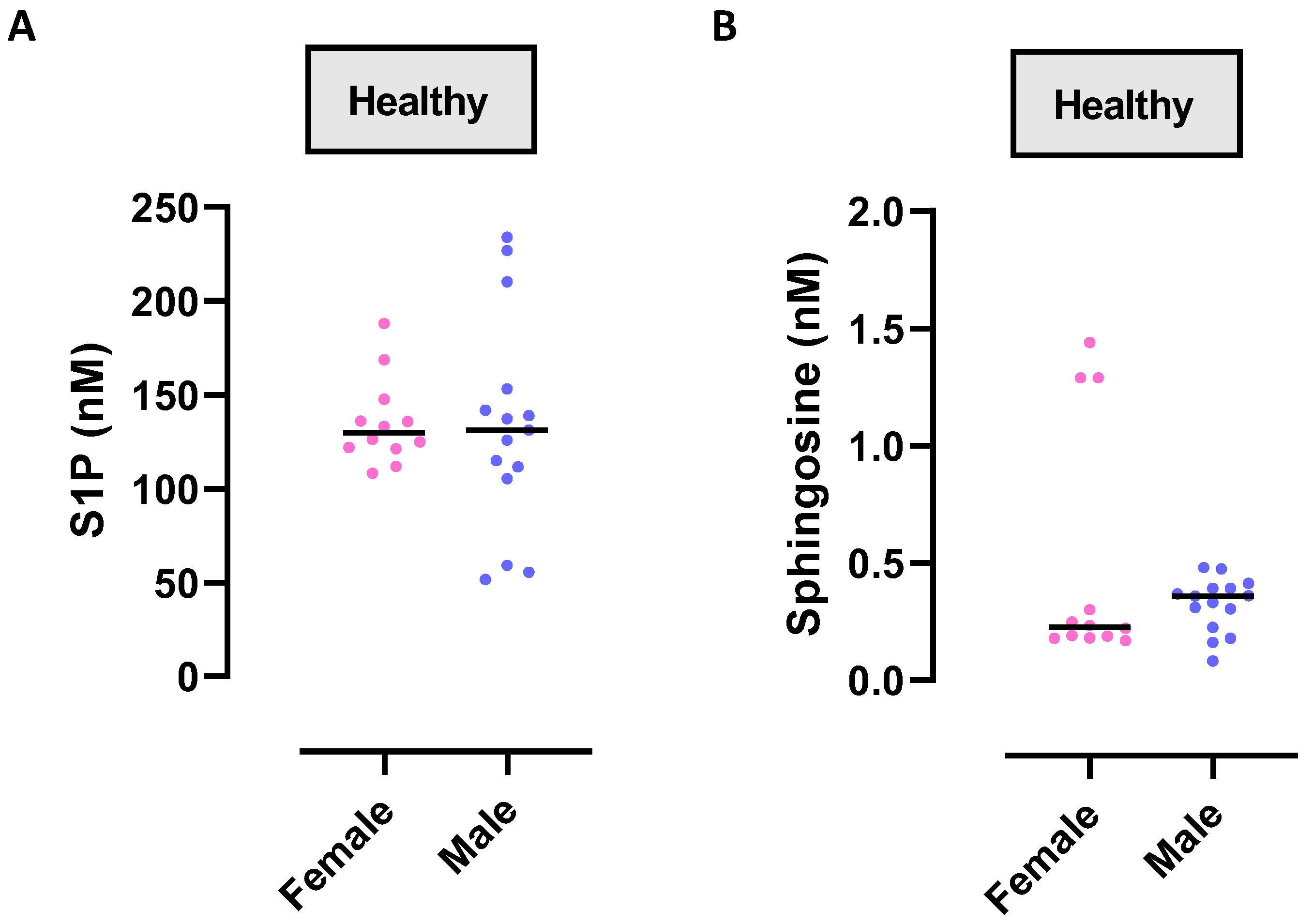
2.1. Circulating Levels of S1P in Physiological Conditions: A Comparison between Females and Males
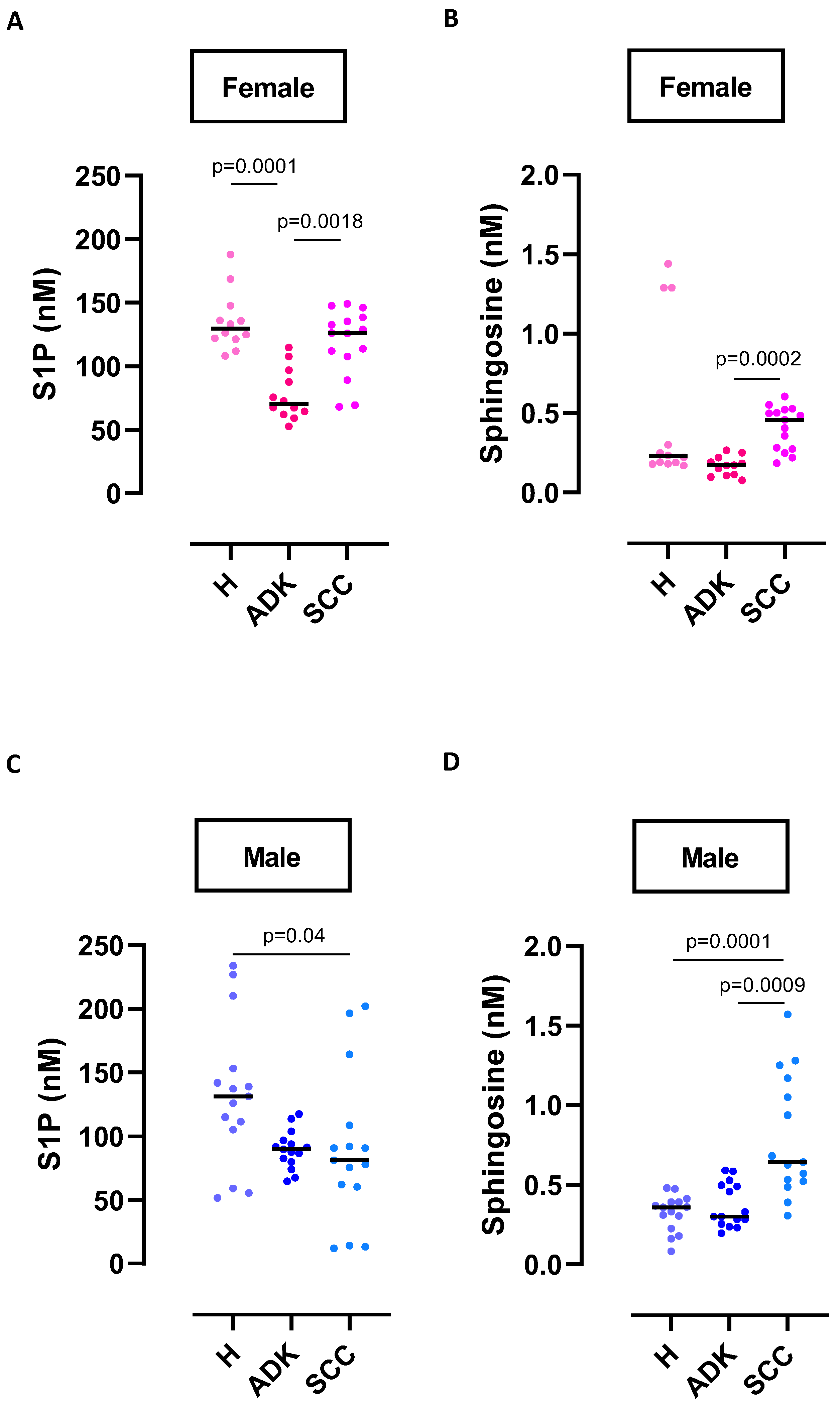
2.2. Circulating S1P Levels in NSCLC Patients: Comparison between Females and Males
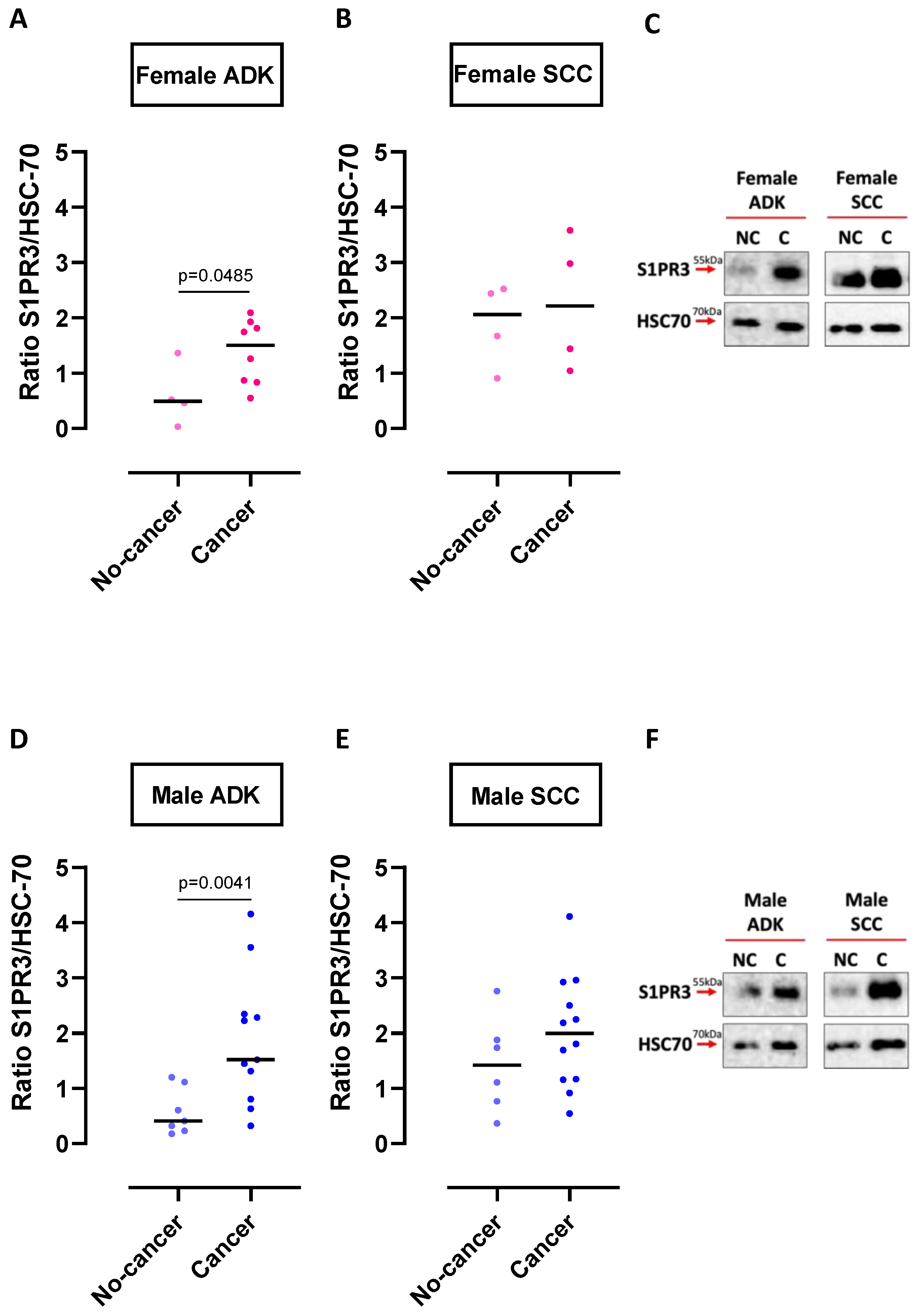
2.3. S1PR3 Expression in Non-Cancerous and Cancerous Lung Tissues of ADK and SCC Patients: Comparison between Females and Males
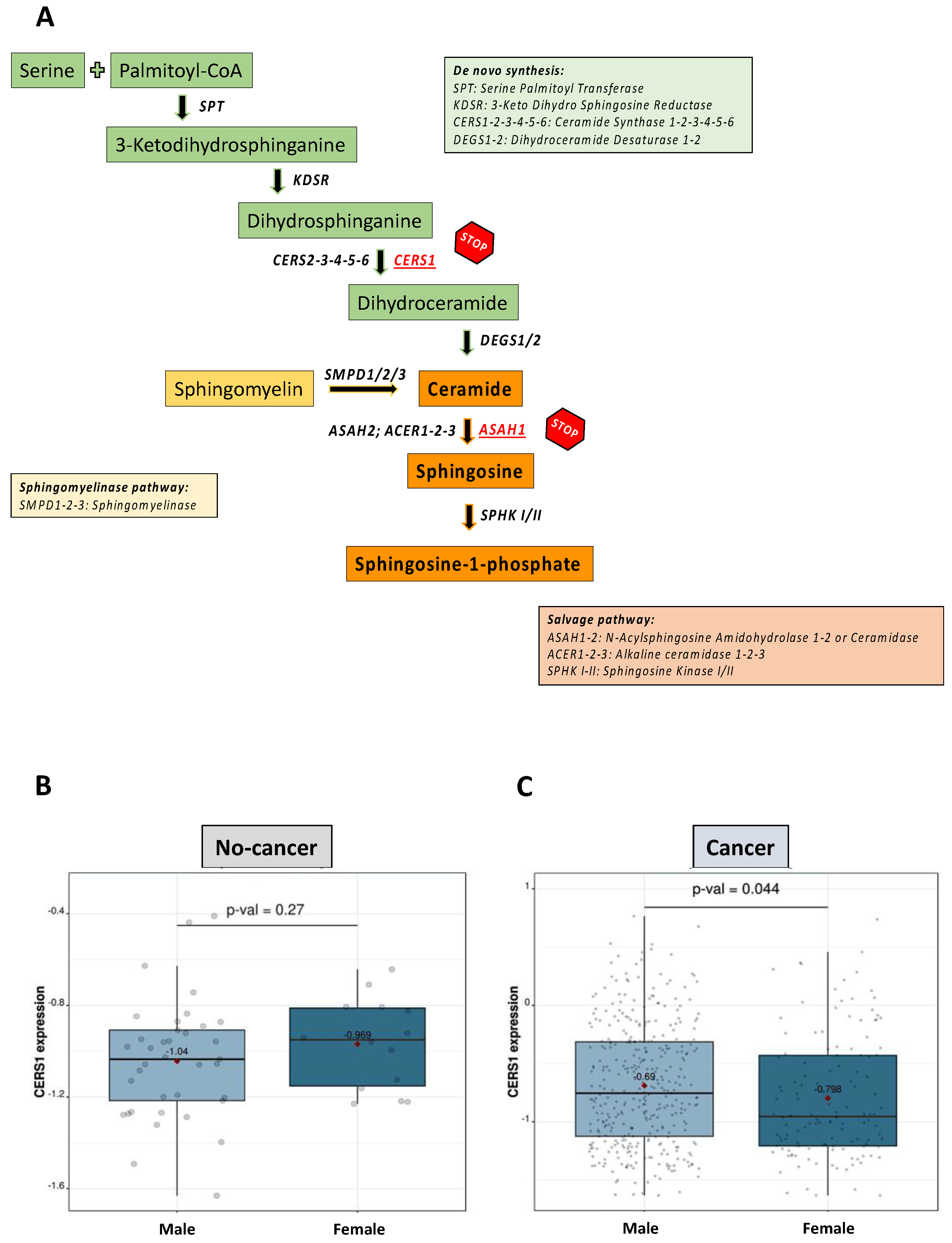
2.4. Evaluation of S1P Metabolic Enzymes in Non-Cancerous and Cancerous Lung Tissues of Female and Male SCC Patients
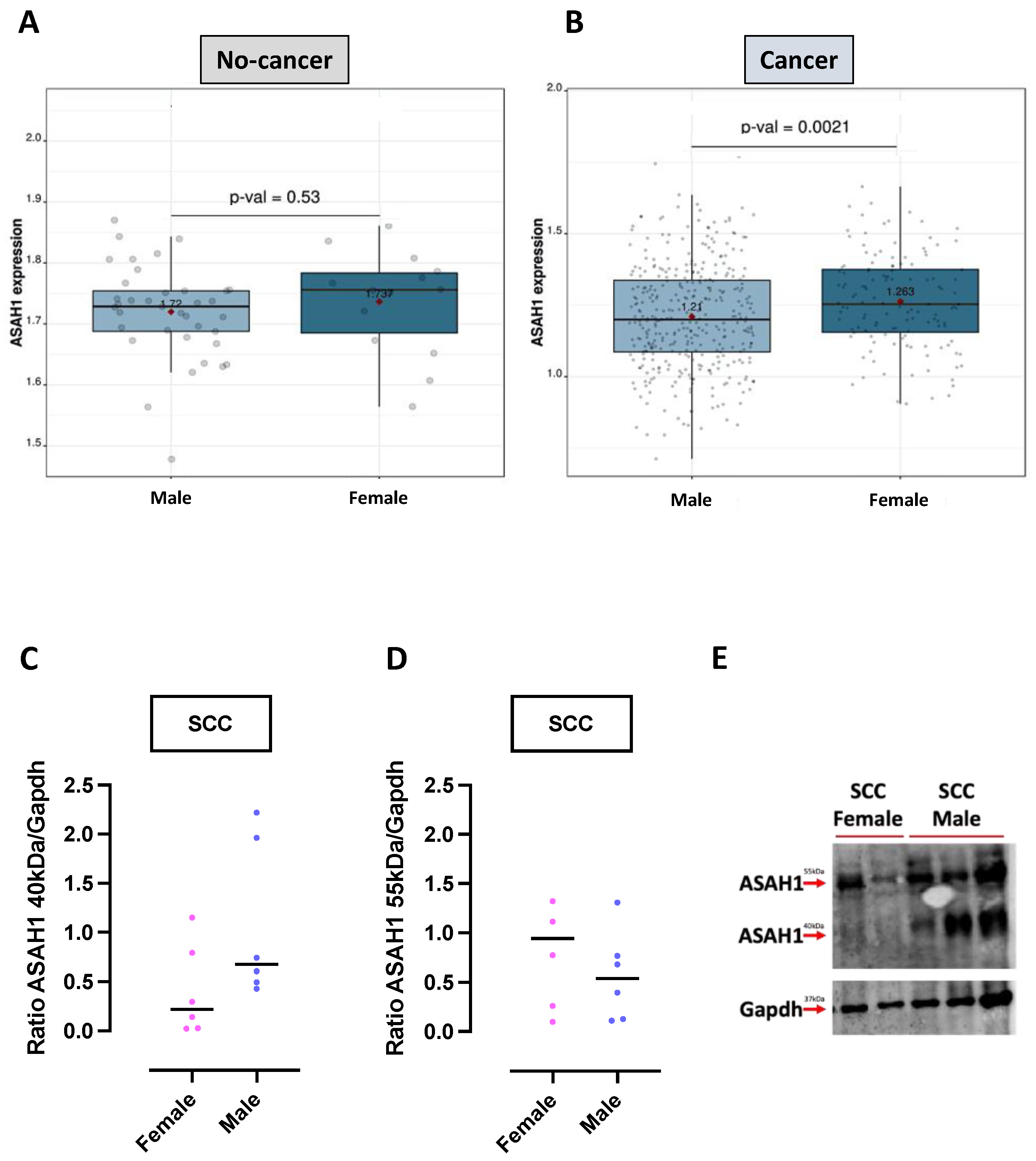
2.5. Ceramidase (ASAH1) Expression in Non-Cancerous and Cancerous Lung Tissues of Female and Male SCC Patients
3. Discussion
- S1P circulating levels are not different between males and females during physiological conditions;
- S1P metabolic pathways are not altered in males and females in physiological states;
- Circulating S1P levels are higher in physiological conditions compared to pathological neoplastic conditions (as in the case of NSCLC);
- Alteration of the ceramide/S1P axis makes the difference between male and female SCC patients, as well as SCC versus ADK patients;
- Female SCCs show an altered metabolism of S1P due to an inactive ASAH1, which most likely does not need to be activated due to the absence of the substrate derived from CERS1, which mRNA is downregulated.
4. Materials and Methods
4.1. Human Samples
4.2. Sphingosine and S1P Extraction from Human Plasma
4.3. LC-MS/MS Analysis
4.4. Western Blotting Analysis
4.5. Analysis of Transcripts Expression
4.6. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cantalupo, A.; Di Lorenzo, A. S1P Signaling and De Novo Biosynthesis in Blood Pressure Homeostasis. J. Pharmacol. Exp. Ther. 2016, 358, 359–370. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.B.; Jersmann, H.; Truong, T.T.; Hamon, R.; Roscioli, E.; Ween, M.; Pitman, M.R.; Pitson, S.M.; Hodge, G.; Reynolds, P.N.; et al. Disrupted epithelial/macrophage crosstalk via Spinster homologue 2-mediated S1P signaling may drive defective macrophage phagocytic function in COPD. PLoS ONE 2017, 12, e0179577. [Google Scholar] [CrossRef] [PubMed]
- Terlizzi, M.; Colarusso, C.; Ferraro, G.; Monti, M.C.; De Rosa, I.; Somma, P.; Salvi, R.; Pinto, A.; Sorrentino, R. Intracellular Sphingosine-1-Phosphate Receptor 3 Contributes to Lung Tumor Cell Proliferation. Cell. Physiol. Biochem. 2021, 55, 539–552. [Google Scholar] [CrossRef]
- Spiegel, S.; Maczis, M.A.; Maceyka, M.; Milstien, S. New insights into functions of the sphingosine-1-phosphate transporter SPNS2. J. Lipid Res. 2019, 60, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Pyne, N.J.; Pyne, S. Sphingosine 1-phosphate and cancer. Nat. Rev. Cancer 2010, 10, 489–503. [Google Scholar] [CrossRef]
- Zhou, H.; Chen, T.; Huang, Z.; Liu, R.; Yang, J.; Hylemon, P.B. Sphingosine-1 phosphate promotes intestinal epithelial cell proliferation via S1PR2. Front. Biosci. 2017, 22, 596–608. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.K.; Volpe, E.; Palmieri, G.; Mattei, M.; Galati, D.; Martino, A.; Piccioni, M.S.; Valente, E.; Bonanno, E.; De Vito, P.; et al. Sphingosine 1–Phosphate Induces Antimicrobial Activity Both In Vitro and In Vivo. J. Infect. Dis. 2004, 189, 2129–2138. [Google Scholar] [CrossRef]
- Mrad, M.; Imbert, C.; Garcia, V.; Rambow, F.; Therville, N.; Carpentier, S.; Ségui, B.; Levade, T.; Azar, R.; Marine, J.-C.; et al. Downregulation of sphingosine kinase-1 induces protective tumor immunity by promoting M1 macrophage response in melanoma. Oncotarget 2016, 7, 71873–71886. [Google Scholar] [CrossRef]
- Yan, X.; Wang, J.; Zhu, Y.; Feng, W.; Zhai, C.; Liu, L.; Shi, W.; Wang, Q.; Zhang, Q.; Chai, L.; et al. S1P induces pulmonary artery smooth muscle cell proliferation by activating calcineurin/NFAT/OPN signaling pathway. Biochem. Biophys. Res. Commun. 2019, 516, 921–927. [Google Scholar] [CrossRef]
- Lupino, L.; Perry, T.; Margielewska, S.; Hollows, R.; Ibrahim, M.; Care, M.; Allegood, J.; Tooze, R.; Sabbadini, R.; Reynolds, G.; et al. Sphingosine-1-phosphate signalling drives an angiogenic transcriptional programme in diffuse large B cell lymphoma. Leukemia 2019, 33, 2884–2897. [Google Scholar] [CrossRef]
- Hansen, L.; Lohfink, N.; Vutukuri, R.; Kestner, R.I.; Trautmann, S.; Hecht, M.; Wagner, P.V.; Spitzer, D.; Khel, M.I.; Macas, J.; et al. Endothelial Sphingosine-1-Phosphate Receptor 4 Regulates Blood-Brain Barrier Permeability and Promotes a Homeostatic Endothelial Phenotype. J. Neurosci. 2022, 42, 1908–1929. [Google Scholar] [CrossRef] [PubMed]
- Roviezzo, F.; Sorrentino, R.; Iacono, V.M.; Brancaleone, V.; Terlizzi, M.; Riemma, M.A.; Bertolino, A.; Rossi, A.; Matteis, M.; Spaziano, G.; et al. Disodium cromoglycate inhibits asthma-like features induced by sphingosine-1-phosphate. Pharmacol. Res. 2016, 113, 626–635. [Google Scholar] [CrossRef] [PubMed]
- Sorrentino, R.; Bertolino, A.; Terlizzi, M.; Iacono, V.M.; Maiolino, P.; Cirino, G.; Roviezzo, F.; Pinto, A. B Cell Depletion Increases Sphingosine-1-Phosphate–Dependent Airway Inflammation in Mice. Am. J. Respir. Cell Mol. Biol. 2015, 52, 571–583. [Google Scholar] [CrossRef] [PubMed]
- Roviezzo, F.; Sorrentino, R.; Terlizzi, M.; Riemma, M.A.; Iacono, V.M.; Rossi, A.; Spaziano, G.; Pinto, A.; D’agostino, B.; Cirino, G. Toll-Like Receptor 4 Is Essential for the Expression of Sphingosine-1-Phosphate-Dependent Asthma-Like Disease in Mice. Front. Immunol. 2017, 8, 1336. [Google Scholar] [CrossRef] [PubMed]
- Obinata, H.; Hla, T. Sphingosine 1-phosphate and inflammation. Int. Immunol. 2019, 31, 617–625. [Google Scholar] [CrossRef]
- Tran, H.B.; Macowan, M.G.; Abdo, A.; Donnelley, M.; Parsons, D.; Hodge, S. Enhanced inflammasome activation and reduced sphingosine-1 phosphate S1P signalling in a respiratory mucoobstructive disease model. J. Inflamm. 2020, 17, 16. [Google Scholar] [CrossRef]
- Murakami, K.; Kohno, M.; Kadoya, M.; Nagahara, H.; Fujii, W.; Seno, T.; Yamamoto, A.; Oda, R.; Fujiwara, H.; Kubo, T.; et al. Knock Out of S1P3 Receptor Signaling Attenuates Inflammation and Fibrosis in Bleomycin-Induced Lung Injury Mice Model. PLoS ONE 2014, 9, e106792. [Google Scholar] [CrossRef]
- Terlizzi, M.; Colarusso, C.; Falanga, A.; Somma, P.; De Rosa, I.; Panico, L.; Pinto, A.; Maiolino, P.; Sorrentino, R. Induction of Inflammation Disrupts the Negative Interplay between STING and S1P Axis That Is Observed during Physiological Conditions in the Lung. Int. J. Mol. Sci. 2023, 24, 8303. [Google Scholar] [CrossRef]
- Terlizzi, M.; Colarusso, C.; Ferraro, G.; Monti, M.C.; Cerqua, I.; Roviezzo, F.; Pinto, A.; Sorrentino, R. Sphingosine-1-Phosphate Contributes to TLR9-Induced TNF-α Release in Lung Tumor Cells. Cell. Physiol. Biochem. 2021, 55, 222–234. [Google Scholar] [CrossRef]
- Klein, S.L.; Flanagan, K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef]
- Cerqua, I.; Terlizzi, M.; Bilancia, R.; Riemma, M.A.; Citi, V.; Martelli, A.; Pace, S.; Spaziano, G.; D’agostino, B.; Werz, O.; et al. 5α-dihydrotestosterone abrogates sex bias in asthma like features in the mouse. Pharmacol. Res. 2020, 158, 104905. [Google Scholar] [CrossRef] [PubMed]
- Snäkä, T.; Bekkar, A.; Desponds, C.; Prével, F.; Claudinot, S.; Isorce, N.; Teixeira, F.; Grasset, C.; Xenarios, I.; Lopez-Mejia, I.C.; et al. Sex-Biased Control of Inflammation and Metabolism by a Mitochondrial Nod-Like Receptor. Front. Immunol. 2022, 13, 882867. [Google Scholar] [CrossRef]
- Chen, K.-H.E.; Lainez, N.M.; Coss, D. Sex Differences in Macrophage Responses to Obesity-Mediated Changes Determine Migratory and Inflammatory Traits. J. Immunol. 2021, 206, 141–153. [Google Scholar] [CrossRef]
- Guo, S.; Yu, Y.; Zhang, N.; Cui, Y.; Zhai, L.; Li, H.; Zhang, Y.; Li, F.; Kan, Y.; Qin, S. Higher level of plasma bioactive molecule sphingosine 1-phosphate in women is associated with estrogen. Biochim. Biophys. Acta (BBA) Mol. Cell Biol. Lipids 2014, 1841, 836–846. [Google Scholar] [CrossRef]
- Yin, J.; Guo, Y.-M.; Chen, P.; Xiao, H.; Wang, X.-H.; DiSanto, M.E.; Zhang, X.-H. Testosterone regulates the expression and functional activity of sphingosine-1-phosphate receptors in the rat corpus cavernosum. J. Cell. Mol. Med. 2018, 22, 1507–1516. [Google Scholar] [CrossRef] [PubMed]
- Bianca, R.D.d.V.; Sorrentino, R.; Sorrentino, R.; Imbimbo, C.; Palmieri, A.; Fusco, F.; Maggi, M.; De Palma, R.; Cirino, G.; Mirone, V. Sphingosine 1-Phosphate Induces Endothelial Nitric-Oxide Synthase Activation through Phosphorylation in Human Corpus Cavernosum. J. Pharmacol. Exp. Ther. 2005, 316, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Siegfried, J.M. Sex and Gender Differences in Lung Cancer and Chronic Obstructive Lung Disease. Endocrinology 2021, 163, bqab254. [Google Scholar] [CrossRef]
- Stabile, L.P.; Rothstein, M.E.; Cunningham, D.E.; Land, S.R.; Dacic, S.; Keohavong, P.; Siegfried, J.M. Prevention of tobacco carcinogen-induced lung cancer in female mice using antiestrogens. Carcinogenesis 2012, 33, 2181–2189. [Google Scholar] [CrossRef]
- Duma, N.; Santana-Davila, R.; Molina, J.R. Non-Small Cell Lung Cancer: Epidemiology, Screening, Diagnosis, and Treatment. Mayo. Clin. Proc. 2019, 94, 1623–1640. [Google Scholar] [CrossRef]
- Barrera-Rodriguez, R.; Morales-Fuentes, J. Lung cancer in women. Lung Cancer 2012, 3, 79–89. [Google Scholar]
- Lung Cancer-Non-Small Cell: Statistics. Approved by the Cancer.Net Editorial Board, 3/2023. Available online: https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/statistics (accessed on 29 May 2023).
- Terlizzi, M.; Colarusso, C.; Somma, P.; De Rosa, I.; Panico, L.; Pinto, A.; Sorrentino, R. S1P-Induced TNF-α and IL-6 Release from PBMCs Exacerbates Lung Cancer-Associated Inflammation. Cells 2022, 11, 2524. [Google Scholar] [CrossRef] [PubMed]
- Rosen, H.; Stevens, R.C.; Hanson, M.; Roberts, E.; Oldstone, M.B. Sphingosine-1-Phosphate and Its Receptors: Structure, Signaling, and Influence. Annu. Rev. Biochem. 2013, 82, 637–662. [Google Scholar] [CrossRef] [PubMed]
- Blaho, V.A.; Hla, T. An update on the biology of sphingosine 1-phosphate receptors. J. Lipid Res. 2014, 55, 1596–1608. [Google Scholar] [CrossRef] [PubMed]
- Terlizzi, M.; Colarusso, C.; De Rosa, I.; De Rosa, N.; Somma, P.; Curcio, C.; Sanduzzi, A.Z.; Micheli, P.; Molino, A.; Saccomanno, A.; et al. Circulating and tumor-associated caspase-4: A novel diagnostic and prognostic biomarker for non-small cell lung cancer. Oncotarget 2018, 9, 19356–19367. [Google Scholar] [CrossRef]
- Terlizzi, M.; Molino, A.; Colarusso, C.; Somma, P.; De Rosa, I.; Troisi, J.; Scala, G.; Salvi, R.; Pinto, A.; Sorrentino, R. Altered lung tissue lipidomic profile in caspase-4 positive non-small cell lung cancer (NSCLC) patients. Oncotarget 2020, 11, 3515–3525. [Google Scholar] [PubMed]
- Cai, L.; Lin, S.; Girard, L.; Zhou, Y.; Yang, L.; Ci, B.; Zhou, Q.; Luo, D.; Yao, B.; Tang, H.; et al. LCE: An open web portal to explore gene expression and clinical associations in lung cancer. Oncogene 2019, 38, 2551–2564. [Google Scholar] [CrossRef]
| Male | Female | |||
|---|---|---|---|---|
| S1P (Median) | S1PR3 (Median) | S1P (Median) | S1PR3 (Median) | |
| ADK | 89.83 nM | 1.52 | 70.13 nM | 1.5 |
| [79.81–96.80 range] | [0.63–3.55 range] | [61.98–96.80 range] | [0.55–2.09 range] | |
| SCC | 81.06 nM | 1.99 | 126 nM | 2.21 |
| [60.31–108.6 range] | [1.158–2.924 range] | [107.7–138.3 range] | [1.041–3.583 range] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Terlizzi, M.; Colarusso, C.; Ferraro, G.; Falanga, A.; Monti, M.C.; Somma, P.; De Rosa, I.; Panico, L.; Pinto, A.; Sorrentino, R. Sex Differences in Sphingosine-1-Phosphate Levels Are Dependent on Ceramide Synthase 1 and Ceramidase in Lung Physiology and Tumor Conditions. Int. J. Mol. Sci. 2023, 24, 10841. https://doi.org/10.3390/ijms241310841
Terlizzi M, Colarusso C, Ferraro G, Falanga A, Monti MC, Somma P, De Rosa I, Panico L, Pinto A, Sorrentino R. Sex Differences in Sphingosine-1-Phosphate Levels Are Dependent on Ceramide Synthase 1 and Ceramidase in Lung Physiology and Tumor Conditions. International Journal of Molecular Sciences. 2023; 24(13):10841. https://doi.org/10.3390/ijms241310841
Chicago/Turabian StyleTerlizzi, Michela, Chiara Colarusso, Giusy Ferraro, Anna Falanga, Maria Chiara Monti, Pasquale Somma, Ilaria De Rosa, Luigi Panico, Aldo Pinto, and Rosalinda Sorrentino. 2023. "Sex Differences in Sphingosine-1-Phosphate Levels Are Dependent on Ceramide Synthase 1 and Ceramidase in Lung Physiology and Tumor Conditions" International Journal of Molecular Sciences 24, no. 13: 10841. https://doi.org/10.3390/ijms241310841
APA StyleTerlizzi, M., Colarusso, C., Ferraro, G., Falanga, A., Monti, M. C., Somma, P., De Rosa, I., Panico, L., Pinto, A., & Sorrentino, R. (2023). Sex Differences in Sphingosine-1-Phosphate Levels Are Dependent on Ceramide Synthase 1 and Ceramidase in Lung Physiology and Tumor Conditions. International Journal of Molecular Sciences, 24(13), 10841. https://doi.org/10.3390/ijms241310841









