Cell Therapy as Target Therapy against Colon Cancer Stem Cells
Abstract
1. Introduction
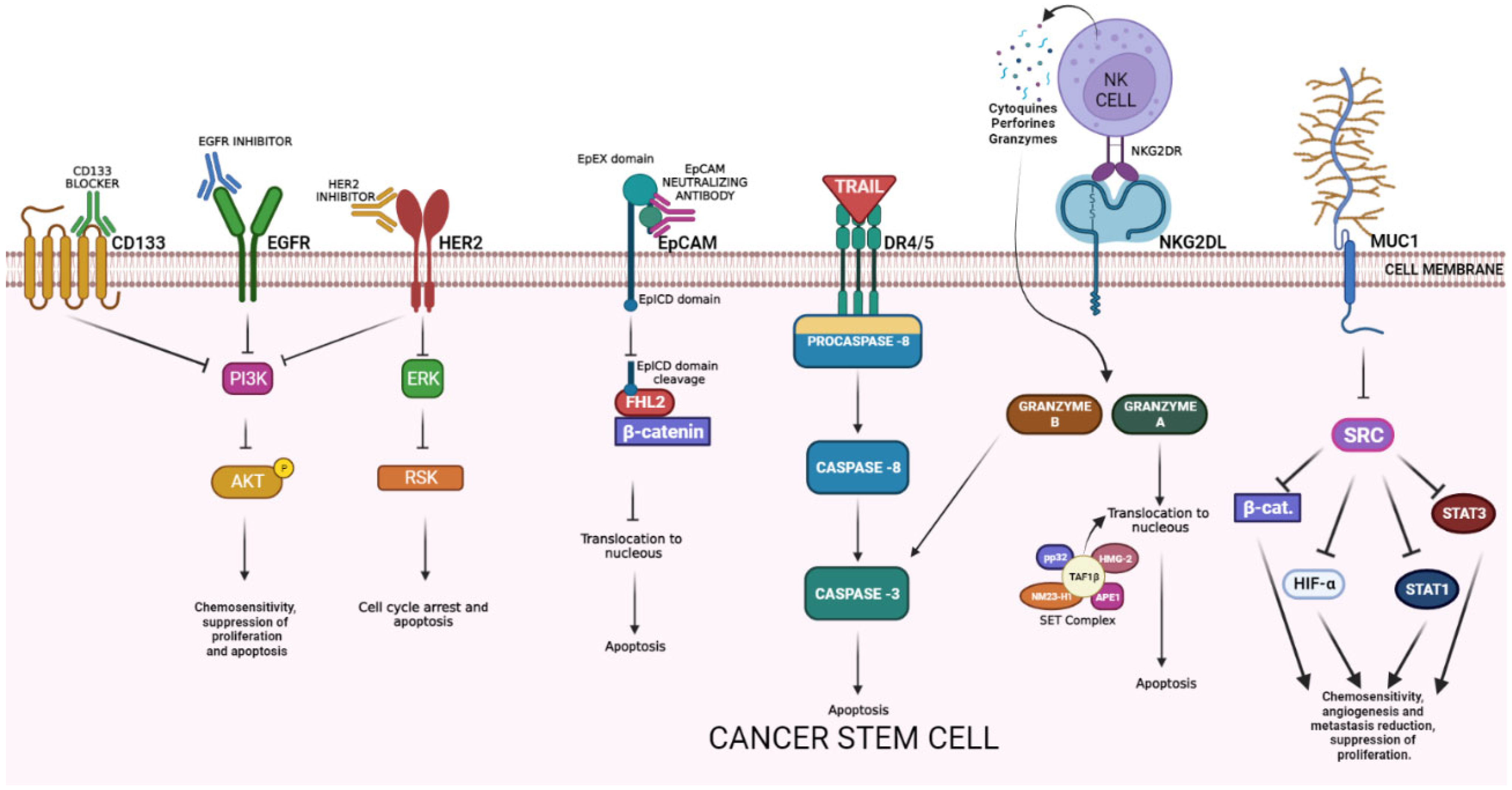
2. Specific Targets Used in CRC Cell Therapy with Potential Antitumoral Effect against CSCs
3. The Consensus Molecular Subtype Classification for CRC
4. Cell Types Used in CRC Immunotherapy
4.1. T-Cells
4.1.1. Checkpoint Inhibitor Drugs
4.1.2. Adoptive T-Cell Therapy
4.1.3. T-Cell Receptor Therapy
4.1.4. Chimeric Antigen Receptor T Cell
4.2. Natural Killer (NK) Cells
4.3. Macrophages
4.3.1. Preventing Monocyte Infiltration in CRC
4.3.2. Repolarizing TAMs
4.4. Stem Cells
4.4.1. MSC as a Platform for Suicide Gene Delivery
4.4.2. MSC with an Oncolytic Virus (OV)
5. Limitations of Cellular Therapy on Advanced CRC Treatment
6. Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sun, H.R.; Wang, S.; Yan, S.C.; Zhang, Y.; Nelson, P.J.; Jia, H.L.; Qin, L.X.; Dong, Q.Z. Therapeutic Strategies Targeting Cancer Stem Cells and Their Microenvironment. Front. Oncol. 2019, 9, 1104. [Google Scholar] [CrossRef] [PubMed]
- Kuşoğlu, A.; Avcı, Ç.B. Cancer Stem Cells: A Brief Review of Current Status. Gene 2019, 681, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.C.; Liao, T.T.; Yang, M.H. Immune Adaptation of Colorectal Cancer Stem Cells and Their Interaction with the Tumor Microenvironment. Front. Oncol. 2020, 10, 588542. [Google Scholar] [CrossRef] [PubMed]
- Zalewski, A.; Snook, A.E.; Waldman, S.A. Stem Cells as Therapeutic Targets in Colorectal Cancer. Pers. Med. 2021, 18, 171–183. [Google Scholar] [CrossRef]
- Du, L.; Cheng, Q.; Zheng, H.; Liu, J.; Liu, L.; Chen, Q. Targeting Stemness of Cancer Stem Cells to Fight Colorectal Cancers. Semin. Cancer Biol. 2022, 82, 150–161. [Google Scholar] [CrossRef]
- Aponte, P.M.; Caicedo, A. Stemness in Cancer: Stem Cells, Cancer Stem Cells, and Their Microenvironment. Stem Cells Int. 2017, 2017, 5619472. [Google Scholar] [CrossRef]
- Phi, L.T.H.; Sari, I.N.; Yang, Y.-G.; Lee, S.-H.; Jun, N.; Kim, K.S.; Lee, Y.K.; Kwon, H.Y. Cancer Stem Cells (CSCs) in Drug Resistance and Their Therapeutic Implications in Cancer Treatment. Stem Cells Int. 2018, 2018, 5416923. [Google Scholar] [CrossRef]
- Aravindhan, S.; Ejam, S.S.; Lafta, M.H.; Markov, A.; Yumashev, A.V.; Ahmadi, M. Mesenchymal Stem Cells and Cancer Therapy: Insights into Targeting the Tumour Vasculature. Cancer Cell Int. 2021, 21, 158. [Google Scholar] [CrossRef]
- Veselov, V.V.; Nosyrev, A.E.; Jicsinszky, L.; Alyautdin, R.N.; Cravotto, G. Targeted Delivery Methods for Anticancer Drugs. Cancers 2022, 14, 622. [Google Scholar] [CrossRef]
- Feng, Y.; Gao, S.; Gao, Y.; Wang, X.; Chen, Z.; Feng, Y.; Gao, S.; Gao, Y.; Wang, X.; Chen, Z. Anti-EGFR Antibody Sensitizes Colorectal Cancer Stem-like Cells to Fluorouracil-Induced Apoptosis by Affecting Autophagy. Oncotarget 2016, 7, 81402–81409. [Google Scholar] [CrossRef]
- De Angelis, M.L.; Zeuner, A.; Policicchio, E.; Russo, G.; Bruselles, A.; Signore, M.; Vitale, S.; De Luca, G.; Pilozzi, E.; Boe, A.; et al. Cancer Stem Cell-Based Models of Colorectal Cancer Reveal Molecular Determinants of Therapy Resistance. Stem Cells Transl. Med. 2016, 5, 511–523. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Dai, X.; Li, X.; Wang, H.; Liu, J.; Zhang, J.; Du, Y.; Xia, L. EGF Signalling Pathway Regulates Colon Cancer Stem Cell Proliferation and Apoptosis. Cell Prolif. 2012, 45, 413–419. [Google Scholar] [CrossRef]
- Oh, D.Y.; Bang, Y.J. HER2-Targeted Therapies—A Role beyond Breast Cancer. Nat. Rev. Clin. Oncol. 2019, 17, 33–48. [Google Scholar] [CrossRef] [PubMed]
- Seo, A.N.; Kwak, Y.; Kim, D.W.; Kang, S.B.; Choe, G.; Kim, W.H.; Lee, H.S. HER2 Status in Colorectal Cancer: Its Clinical Significance and the Relationship between HER2 Gene Amplification and Expression. PLoS ONE 2014, 9, e98528. [Google Scholar] [CrossRef] [PubMed]
- Kavuri, S.M.; Jain, N.; Galimi, F.; Cottino, F.; Leto, S.M.; Migliardi, G.; Searleman, A.C.; Shen, W.; Monsey, J.; Trusolino, L.; et al. HER2 Activating Mutations Are Targets for Colorectal Cancer Treatment. Cancer Discov. 2015, 5, 832–841. [Google Scholar] [CrossRef] [PubMed]
- El-Deiry, W.S.; Vijayvergia, N.; Xiu, J.; Scicchitano, A.; Lim, B.; Yee, N.S.; Harvey, H.A.; Gatalica, Z.; Reddy, S. Molecular Profiling of 6,892 Colorectal Cancer Samples Suggests Different Possible Treatment Options Specific to Metastatic Sites. Cancer Biol. Ther. 2015, 16, 1726–1737. [Google Scholar] [CrossRef]
- Afrǎsânie, V.A.; Marinca, M.V.; Alexa-Stratulat, T.; Gafton, B.; Pǎduraru, M.; Adavidoaiei, A.M.; Miron, L.; Rusu, C. KRAS, NRAS, BRAF, HER2 and Microsatellite Instability in Metastatic Colorectal Cancer-Practical Implications for the Clinician. Radiol. Oncol. 2019, 53, 265–274. [Google Scholar] [CrossRef]
- Styczen, H.; Nagelmeier, I.; Beissbarth, T.; Nietert, M.; Homayounfar, K.; Sprenger, T.; Boczek, U.; Stanek, K.; Kitz, J.; Wolff, H.A.; et al. HER-2 and HER-3 Expression in Liver Metastases of Patients with Colorectal Cancer. Oncotarget 2015, 6, 15065–15076. [Google Scholar] [CrossRef]
- Fusco, N.; Bosari, S. HER2 Aberrations and Heterogeneity in Cancers of the Digestive System: Implications for Pathologists and Gastroenterologists. World J. Gastroenterol. 2016, 22, 7926–7937. [Google Scholar] [CrossRef]
- Ivanova, M.; Venetis, K.; Guerini-Rocco, E.; Bottiglieri, L.; Mastropasqua, M.G.; Garrone, O.; Fusco, N.; Ghidini, M. HER2 in Metastatic Colorectal Cancer: Pathology, Somatic Alterations, and Perspectives for Novel Therapeutic Schemes. Life 2022, 12, 1403. [Google Scholar] [CrossRef]
- Zhang, X.; Powell, K.; Li, L. Breast Cancer Stem Cells: Biomarkers, Identification and Isolation Methods, Regulating Mechanisms, Cellular Origin, and Beyond. Cancers 2020, 12, 3765. [Google Scholar] [CrossRef] [PubMed]
- Jung, D.H.; Bae, Y.J.; Kim, J.H.; Shin, Y.K.; Jeung, H.C. HER2 Regulates Cancer Stem Cell Activities via the Wnt Signaling Pathway in Gastric Cancer Cells. Oncology 2019, 97, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Liang, K.H.; Tso, H.C.; Hung, S.H.; Kuan, I.I.; Lai, J.K.; Ke, F.Y.; Chuang, Y.T.; Liu, I.J.; Wang, Y.P.; Chen, R.H.; et al. Extracellular Domain of EpCAM Enhances Tumor Progression through EGFR Signaling in Colon Cancer Cells. Cancer Lett. 2018, 433, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Eyvazi, S.; Farajnia, S.; Dastmalchi, S.; Kanipour, F.; Zarredar, H.; Bandehpour, M. Antibody Based EpCAM Targeted Therapy of Cancer, Review and Update. Curr. Cancer Drug. Targets 2018, 18, 857–868. [Google Scholar] [CrossRef] [PubMed]
- Gires, O.; Pan, M.; Schinke, H.; Canis, M.; Baeuerle, P.A. Expression and Function of Epithelial Cell Adhesion Molecule EpCAM: Where Are We after 40 Years? Cancer Metastasis Rev. 2020, 39, 969–987. [Google Scholar] [CrossRef]
- Gao, T.; Cen, Q.; Lei, H. A Review on Development of MUC1-Based Cancer Vaccine. Biomed. Pharmacother. 2020, 132, 110888. [Google Scholar] [CrossRef]
- Guo, M.; Luo, B.; Pan, M.; Li, M.; Xu, H.; Zhao, F.; Dou, J. Colorectal Cancer Stem Cell Vaccine with High Expression of MUC1 Serves as a Novel Prophylactic Vaccine for Colorectal Cancer. Int. Immunopharmacol. 2020, 88, 106850. [Google Scholar] [CrossRef]
- Li, W.; Zhang, N.; Jin, C.; Long, M.D.; Rajabi, H.; Yasumizu, Y.; Fushimi, A.; Yamashita, N.; Hagiwara, M.; Zheng, R.; et al. MUC1-C Drives Stemness in Progression of Colitis to Colorectal Cancer. JCI Insight 2020, 5, e137112. [Google Scholar] [CrossRef]
- Guo, M.; Luo, B.; Pan, M.; Li, M.; Zhao, F.; Dou, J. MUC1 Plays an Essential Role in Tumor Immunity of Colorectal Cancer Stem Cell Vaccine. Int. Immunopharmacol. 2020, 85, 106631. [Google Scholar] [CrossRef]
- Guo, M.; You, C.; Dong, W.; Luo, B.; Wu, Y.; Chen, Y.; Li, J.; Pan, M.; Li, M.; Zhao, F.; et al. The Surface Dominant Antigen MUC1 Is Required for Colorectal Cancer Stem Cell Vaccine to Exert Anti-Tumor Efficacy. Biomed. Pharmacother. 2020, 132, 110804. [Google Scholar] [CrossRef]
- Carrell, R.K.; Stanton, R.A.; Ethier, S.P.; LaRue, A.C.; Soloff, A.C. ICOSL-Augmented Adenoviral-Based Vaccination Induces a Bipolar Th17/Th1 T Cell Response against Unglycosylated MUC1 Antigen. Vaccine 2018, 36, 6262–6269. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.B.; Rocco, A.; Lamb, L.S.; Friedman, G.K.; Hjelmeland, A.B. Regulation of NKG2D Stress Ligands and Its Relevance in Cancer Progression. Cancers 2022, 14, 2339. [Google Scholar] [CrossRef] [PubMed]
- Daniels, R.A.; Turley, H.; Kimberley, F.C.; Liu, X.S.; Mongkolsapaya, J.; Ch’En, P.; Xu, X.N.; Jin, B.Q.; Pezzella, F.; Screaton, G.R. Expression of TRAIL and TRAIL Receptors in Normal and Malignant Tissues. Cell. Res. 2005, 15, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Snajdauf, M.; Havlova, K.; Vachtenheim, J.; Ozaniak, A.; Lischke, R.; Bartunkova, J.; Smrz, D.; Strizova, Z. The TRAIL in the Treatment of Human Cancer: An Update on Clinical Trials. Front. Mol. Biosci. 2021, 8, 628332. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, Y.; Kunita, A.; Iwata, C.; Komura, D.; Nishiyama, T.; Shimazu, K.; Takeshita, K.; Shibahara, J.; Kii, I.; Morishita, Y.; et al. The Niche Component Periostin Is Produced by Cancer-Associated Fibroblasts, Supporting Growth of Gastric Cancer through ERK Activation. Am. J. Pathol. 2014, 184, 859–870. [Google Scholar] [CrossRef]
- Akbari, M.; Shomali, N.; Faraji, A.; Shanehbandi, D.; Asadi, M.; Mokhtarzadeh, A.; Shabani, A.; Baradaran, B. CD133: An Emerging Prognostic Factor and Therapeutic Target in Colorectal Cancer. Cell Biol. Int. 2020, 44, 368–380. [Google Scholar] [CrossRef] [PubMed]
- Abbasian, M.; Mousavi, E.; Arab-Bafrani, Z.; Sahebkar, A. The Most Reliable Surface Marker for the Identification of Colorectal Cancer Stem-like Cells: A Systematic Review and Meta-Analysis. J. Cell. Physiol. 2019, 234, 8192–8202. [Google Scholar] [CrossRef]
- Ieta, K.; Tanaka, F.; Haraguchi, N.; Kita, Y.; Sakashita, H.; Mimori, K.; Matsumoto, T.; Inoue, H.; Kuwano, H.; Mori, M. Biological and Genetic Characteristics of Tumor-Initiating Cells in Colon Cancer. Ann. Surg. Oncol. 2008, 15, 638–648. [Google Scholar] [CrossRef]
- Vaiopoulos, A.G.; Kostakis, I.D.; Koutsilieris, M.; Papavassiliou, A.G. Colorectal Cancer Stem Cells. Stem Cells 2012, 30, 363–371. [Google Scholar] [CrossRef]
- Todaro, M.; Francipane, M.G.; Medema, J.P.; Stassi, G. Colon Cancer Stem Cells: Promise of Targeted Therapy. Gastroenterology 2010, 138, 2151–2162. [Google Scholar] [CrossRef]
- Zhi, Y.; Mou, Z.; Chen, J.; He, Y.; Dong, H.; Fu, X.; Wu, Y. B7H1 Expression and Epithelial-To-Mesenchymal Transition Phenotypes on Colorectal Cancer Stem-Like Cells. PLoS ONE 2015, 10, e0135528. [Google Scholar] [CrossRef] [PubMed]
- Ben-Porath, I.; Thomson, M.W.; Carey, V.J.; Ge, R.; Bell, G.W.; Regev, A.; Weinberg, R.A. An Embryonic Stem Cell–like Gene Expression Signature in Poorly Differentiated Aggressive Human Tumors. Nat. Genet. 2008, 40, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Schmohl, J.U.; Gleason, M.K.; Dougherty, P.R.; Miller, J.S.; Vallera, D.A. Heterodimeric Bispecific Single Chain Variable Fragments (ScFv) Killer Engagers (BiKEs) Enhance NK-Cell Activity Against CD133+ Colorectal Cancer Cells. Target. Oncol. 2016, 11, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Barzegar Behrooz, A.; Syahir, A.; Ahmad, S. CD133: Beyond a Cancer Stem Cell Biomarker. J. Drug Target. 2018, 27, 257–269. [Google Scholar] [CrossRef] [PubMed]
- Braumüller, H.; Mauerer, B.; Andris, J.; Berlin, C.; Wieder, T.; Kesselring, R. The Cytokine Network in Colorectal Cancer: Implications for New Treatment Strategies. Cells 2022, 12, 138. [Google Scholar] [CrossRef] [PubMed]
- López-Camacho, E.; Prado-Vázquez, G.; Martínez-Pérez, D.; Ferrer-Gómez, M.; Llorente-Armijo, S.; López-Vacas, R.; Díaz-Almirón, M.; Gámez-Pozo, A.; Vara, J.Á.F.; Feliu, J.; et al. A Novel Molecular Analysis Approach in Colorectal Cancer Suggests New Treatment Opportunities. Cancers 2023, 15, 1104. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.P.; Rai, S.; Pandey, A.; Singh, N.K.; Srivastava, S. Molecular Subtypes of Colorectal Cancer: An Emerging Therapeutic Opportunity for Personalized Medicine. Genes Dis. 2021, 8, 133–145. [Google Scholar] [CrossRef]
- Włodarczyk, M.; Włodarczyk, J.; Siwiński, P.; Sobolewska-Włodarczyk, A.; Fichna, J. Genetic Molecular Subtypes in Optimizing Personalized Therapy for Metastatic Colorectal Cancer. Curr. Drug Targets 2018, 19, 1731–1737. [Google Scholar] [CrossRef]
- Stintzing, S.; Wirapati, P.; Lenz, H.-J.; Neureiter, D.; Fischer von Weikersthal, L.; Decker, T.; Kiani, A.; Kaiser, F.; Al-Batran, S.; Heintges, T.; et al. Consensus Molecular Subgroups (CMS) of Colorectal Cancer (CRC) and First-Line Efficacy of FOLFIRI plus Cetuximab or Bevacizumab in the FIRE3 (AIO KRK-0306) Trial. Ann. Oncol. 2019, 30, 1796–1803. [Google Scholar] [CrossRef]
- Sconocchia, G.; Eppenberger, S.; Spagnoli, G.C.; Tornillo, L.; Droeser, R.; Caratelli, S.; Ferrelli, F.; Coppola, A.; Arriga, R.; Lauro, D.; et al. NK Cells and T Cells Cooperate during the Clinical Course of Colorectal Cancer. Oncoimmunology 2014, 3, e952197. [Google Scholar] [CrossRef]
- Valenzuela, G.; Canepa, J.; Simonetti, C.; Solo de Zaldívar, L.; Marcelain, K.; González-Montero, J. Consensus Molecular Subtypes of Colorectal Cancer in Clinical Practice: A Translational Approach. World J. Clin. Oncol. 2021, 12, 1000–1008. [Google Scholar] [CrossRef] [PubMed]
- Juat, D.J.; Hachey, S.J.; Billimek, J.; Del Rosario, M.P.; Nelson, E.L.; Hughes, C.C.W.; Zell, J.A. Adoptive T-Cell Therapy in Advanced Colorectal Cancer: A Systematic Review. Oncologist 2022, 27, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Ramutton, T.; Buccheri, S.; Dieli, F.; Todaro, M.; Stassi, G.; Meraviglia, S. Γδ T Cells as a Potential Tool in Colon Cancer Immunotherapy. Immunotherapy 2014, 6, 989–999. [Google Scholar] [CrossRef] [PubMed]
- Frank, M.H.; Wilson, B.J.; Gold, J.S.; Frank, N.Y. Clinical Implications of Colorectal Cancer Stem Cells in the Age of Single-Cell Omics and Targeted Therapies. Gastroenterology 2021, 160, 1947–1960. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, Y.; Naito, M.; Yamada, T.; Aisu, N.; Daibo, K.; Mera, T.; Tanaka, T.; Naito, K.; Yasumoto, K.; Kamigaki, T.; et al. Adoptive Chemoimmunotherapy Using Activated T Cells for Stage IV Colorectal Cancer. Anticancer. Res. 2016, 36, 3741–3746. [Google Scholar]
- Parkhurst, M.R.; Joo, J.; Riley, J.P.; Yu, Z.; Li, Y.; Robbins, P.F.; Rosenberg, S.A. Characterization of Genetically Modified T-Cell Receptors That Recognize the CEA:691-699 Peptide in the Context of HLA-A2.1 on Human Colorectal Cancer Cells. Clin. Cancer Res. 2009, 15, 169–180. [Google Scholar] [CrossRef]
- Parkhurst, M.R.; Yang, J.C.; Langan, R.C.; Dudley, M.E.; Nathan, D.A.N.; Feldman, S.A.; Davis, J.L.; Morgan, R.A.; Merino, M.J.; Sherry, R.M.; et al. T Cells Targeting Carcinoembryonic Antigen Can Mediate Regression of Metastatic Colorectal Cancer but Induce Severe Transient Colitis. Mol. Ther. 2011, 19, 620–626. [Google Scholar] [CrossRef]
- Aparicio, C.; Belver, M.; Enríquez, L.; Espeso, F.; Núñez, L.; Sánchez, A.; de la Fuente, M.Á.; González-vallinas, M. Cell Therapy for Colorectal Cancer: The Promise of Chimeric Antigen Receptor (CAR)-T Cells. Int. J. Mol. Sci. 2021, 22, 1781. [Google Scholar] [CrossRef]
- Li, H.; Yang, C.; Cheng, H.; Huang, S.; Zheng, Y. CAR-T Cells for Colorectal Cancer: Target-Selection and Strategies for Improved Activity and Safety. J. Cancer 2021, 12, 1804–1814. [Google Scholar] [CrossRef]
- Feng, M.; Zhao, Z.; Yang, M.; Ji, J.; Zhu, D. T-Cell Based Immunotherapy in Colorectal Cancer. Cancer Lett. 2020, 498, 201–209. [Google Scholar] [CrossRef]
- Xu, J.; Meng, Q.; Sun, H.; Zhang, X.; Yun, J.; Li, B.; Wu, S.; Li, X.; Yang, H.; Zhu, H.; et al. HER2-Specific Chimeric Antigen Receptor-T Cells for Targeted Therapy of Metastatic Colorectal Cancer. Cell Death Dis. 2021, 12, 1109. [Google Scholar] [CrossRef] [PubMed]
- Magee, M.S.; Abraham, T.S.; Baybutt, T.R.; FlickingerJr, J.C.; Ridge, N.A.; Marszalowicz, G.P.; Prajapati, P.; Hersperger, A.R.; Waldman, S.A.; Snook, A.E. Human GUCY2C-Targeted Chimeric Antigen Receptor (CAR)-Expressing T Cells Eliminate Colorectal Cancer Metastases. Cancer Immunol. Res. 2018, 6, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Abbas, A.K.; Lichtman, A.H.; Pober, J.S. Cellular and Molecular Immunology; W.B. Saunders Company: Philadelphia, PA, USA, 1997. [Google Scholar]
- Gri, G.; Showe, L. Cutting Edge: Differentiation of Human NK Cells into NK1 and NK2 Subsets. J. Immunol. 1998, 161, 5821–5824. [Google Scholar]
- Chu, J.; Gao, F.; Yan, M.; Zhao, S.; Yan, Z.; Shi, B.; Liu, Y. Natural Killer Cells: A Promising Immunotherapy for Cancer. J. Transl. Med. 2022, 20, 240. [Google Scholar] [CrossRef] [PubMed]
- Portillo, A.L.; Hogg, R.; Poznanski, S.M.; Rojas, E.A.; Cashell, N.J.; Hammill, J.A.; Chew, M.V.; Shenouda, M.M.; Ritchie, T.M.; Cao, Q.T.; et al. Expanded Human NK Cells Armed with CAR Uncouple Potent Anti-Tumor Activity from off-Tumor Toxicity against Solid Tumors. iScience 2021, 24, 102619. [Google Scholar] [CrossRef]
- Rettinger, E.; KuçI, S.; Naumann, I.; Becker, P.; Kreyenberg, H.; Anzaghe, M.; Willasch, A.; Koehl, U.; Bug, G.; Ruthardt, M.; et al. The Cytotoxic Potential of Interleukin-15-Stimulated Cytokine-Induced Killer Cells against Leukemia Cells. Cytotherapy 2012, 14, 91–103. [Google Scholar] [CrossRef]
- Wang, Y.; Zheng, X.; Wei, H.; Sun, R.; Tian, Z. Different Roles of IL-15 from IL-2 in Differentiation and Activation of Human CD3+CD56+ NKT-like Cells from Cord Blood in Long Term Culture. Int. Immunopharmacol. 2008, 8, 927–934. [Google Scholar] [CrossRef]
- Sivori, S.; Vacca, P.; Del Zotto, G.; Munari, E.; Mingari, M.C.; Moretta, L. Human NK Cells: Surface Receptors, Inhibitory Checkpoints, and Translational Applications. Cell. Mol. Immunol. 2019, 16, 430–441. [Google Scholar] [CrossRef]
- Shokouhifar, A.; Firouzi, J.; Nouri, M.; Sarab, G.A.; Ebrahimi, M. NK Cell Upraise in the Dark World of Cancer Stem Cells. Cancer Cell Int. 2021, 21, 682. [Google Scholar] [CrossRef]
- Guillerey, C.; Huntington, N.D.; Smyth, M.J. Targeting Natural Killer Cells in Cancer Immunotherapy. Nat. Immunol. 2016, 17, 1025–1036. [Google Scholar] [CrossRef]
- Liu, S.; Galat, V.; Galat4, Y.; Lee, Y.K.A.; Wainwright, D.; Wu, J. NK Cell-Based Cancer Immunotherapy: From Basic Biology to Clinical Development. J. Hematol. Oncol. 2021, 14, 7. [Google Scholar] [CrossRef] [PubMed]
- Nieda, M. TRAIL Expression by Activated Human CD4+Valpha24NKT Cells Induces in Vitro and in Vivo Apoptosis of Human Acute Myeloid Leukemia Cells. Blood 2001, 97, 2067–2074. [Google Scholar] [CrossRef]
- Grudzien, M.; Rapak, A. Effect of Natural Compounds on NK Cell Activation. J. Immunol. Res. 2018, 2018, 4868417. [Google Scholar] [CrossRef] [PubMed]
- González, B.; Bueno, D.; Rubio, P.M.; Román, S.S.; Plaza, D.; Sastre, A.; García-Miguel, P.; Fernández, L.; Valentín, J.; Martínez, I.; et al. Aspectos Inmunológicos de La Leucemia Mieloblástica Aguda. An. Pediatr. 2016, 84, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Ruggeri, L.; Mancusi, A.; Burchielli, E.; Aversa, F.; Martelli, M.F.; Velardi, A. Natural Killer Cell Alloreactivity and Haplo-Identical Hematopoietic Transplantation. Cytotherapy 2006, 8, 554–558. [Google Scholar] [CrossRef]
- Della Chiesa, M.; Setti, C.; Giordano, C.; Obino, V.; Greppi, M.; Pesce, S.; Marcenaro, E.; Rutigliani, M.; Provinciali, N.; Paleari, L.; et al. NK Cell-Based Immunotherapy in Colorectal Cancer. Vaccines 2022, 10, 1033. [Google Scholar] [CrossRef]
- Wooster, A.L.; Girgis, L.H.; Brazeale, H.; Anderson, T.S.; Wood, L.M.; Lowe, D.B. Dendritic Cell Vaccine Therapy for Colorectal Cancer. Pharmacol. Res. 2021, 164, 105374. [Google Scholar] [CrossRef]
- Kajihara, M.; Takakura, K.; Kanai, T.; Ito, Z.; Saito, K.; Takami, S.; Shimodaira, S.; Okamoto, M.; Ohkusa, T.; Koido, S. Dendritic Cell-Based Cancer Immunotherapy for Colorectal Cancer. World J. Gastroenterol. 2016, 22, 4275. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhang, H.; Ding, J.; Liu, H.; Li, H.; Li, H.; Lu, M.; Miao, Y.; Li, L.; Zheng, J. Combination Therapy with EpCAM-CAR-NK-92 Cells and Regorafenib against Human Colorectal Cancer Models. J. Immunol. Res. 2018, 2018, 4263520. [Google Scholar] [CrossRef]
- Yip, J.L.K.; Balasuriya, G.K.; Spencer, S.J.; Hill-Yardin, E.L. The Role of Intestinal Macrophages in Gastrointestinal Homeostasis: Heterogeneity and Implications in Disease. Cell. Mol. Gastroenterol. Hepatol. 2021, 12, 1701. [Google Scholar] [CrossRef]
- Zhang, Y.; Guan, X.Y.; Jiang, P. Cytokine and Chemokine Signals of T-Cell Exclusion in Tumors. Front. Immunol. 2020, 11, 594609. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Lin, J.; Xu, A.; Lou, J.; Qian, C.; Li, X.; Wang, Y.; Yu, W.; Tao, H. CCL2: An Important Mediator Between Tumor Cells and Host Cells in Tumor Microenvironment. Front. Oncol. 2021, 11, 722916. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Tian, T.; Zhang, J. Tumor-Associated Macrophages (TAMs) in Colorectal Cancer (CRC): From Mechanism to Therapy and Prognosis. Int. J. Mol. Sci. 2021, 22, 8470. [Google Scholar] [CrossRef] [PubMed]
- Pernot, S.; Evrard, S.; Khatib, A.M. The Give-and-Take Interaction Between the Tumor Microenvironment and Immune Cells Regulating Tumor Progression and Repression. Front. Immunol. 2022, 13, 850856. [Google Scholar] [CrossRef] [PubMed]
- Greten, F.R.; Grivennikov, S.I. Inflammation and Cancer: Triggers, Mechanisms and Consequences. Immunity 2019, 51, 27. [Google Scholar] [CrossRef]
- Chanmee, T.; Ontong, P.; Konno, K.; Itano, N. Tumor-Associated Macrophages as Major Players in the Tumor Microenvironment. Cancers 2014, 6, 1670. [Google Scholar] [CrossRef]
- Georgoudaki, A.M.; Prokopec, K.E.; Boura, V.F.; Hellqvist, E.; Sohn, S.; Östling, J.; Dahan, R.; Harris, R.A.; Rantalainen, M.; Klevebring, D.; et al. Reprogramming Tumor-Associated Macrophages by Antibody Targeting Inhibits Cancer Progression and Metastasis. Cell. Rep. 2016, 15, 2000–2011. [Google Scholar] [CrossRef]
- Olsson, A.; Nakhlé, J.; Sundstedt, A.; Plas, P.; Bauchet, A.L.; Pierron, V.; Bruetschy, L.; Deronic, A.; Törngren, M.; Liberg, D.; et al. Tasquinimod Triggers an Early Change in the Polarization of Tumor Associated Macrophages in the Tumor Microenvironment. J. Immunother. Cancer 2015, 3, 53. [Google Scholar] [CrossRef]
- De Vito, A.; Orecchia, P.; Balza, E.; Reverberi, D.; Scaldaferri, D.; Taramelli, R.; Noonan, D.M.; Acquati, F.; Mortara, L. Overexpression of Murine Rnaset2 in a Colon Syngeneic Mouse Carcinoma Model Leads to Rebalance of Intra-Tumor M1/M2 Macrophage Ratio, Activation of T Cells, Delayed Tumor Growth, and Rejection. Cancers 2020, 12, 717. [Google Scholar] [CrossRef]
- Halama, N.; Zoernig, I.; Berthel, A.; Kahlert, C.; Klupp, F.; Suarez-Carmona, M.; Suetterlin, T.; Brand, K.; Krauss, J.; Lasitschka, F.; et al. Tumoral Immune Cell Exploitation in Colorectal Cancer Metastases Can Be Targeted Effectively by Anti-CCR5 Therapy in Cancer Patients. Cancer Cell 2016, 29, 587–601. [Google Scholar] [CrossRef]
- Korehisa, S.; Oki, E.; Iimori, M.; Nakaji, Y.; Shimokawa, M.; Saeki, H.; Okano, S.; Oda, Y.; Maehara, Y. Clinical Significance of Programmed Cell Death-Ligand 1 Expression and the Immune Microenvironment at the Invasive Front of Colorectal Cancers with High Microsatellite Instability. Int. J. Cancer 2018, 142, 822–832. [Google Scholar] [CrossRef] [PubMed]
- Bai, J.; Chen, H.; Bai, X. Relationship between Microsatellite Status and Immune Microenvironment of Colorectal Cancer and Its Application to Diagnosis and Treatment. J. Clin. Lab. Anal. 2021, 35, e23810. [Google Scholar] [CrossRef] [PubMed]
- Weiss, J.M.; Subleski, J.J.; Wigginton, J.M.; Wiltrout, R.H. Immunotherapy of Cancer by IL-12-Based Cytokine Combinations. Expert Opin. Biol. Ther. 2007, 7, 1705–1721. [Google Scholar] [CrossRef] [PubMed]
- Berraondo, P.; Sanmamed, M.F.; Ochoa, M.C.; Etxeberria, I.; Aznar, M.A.; Pérez-Gracia, J.L.; Rodríguez-Ruiz, M.E.; Ponz-Sarvise, M.; Castañón, E.; Melero, I. Cytokines in Clinical Cancer Immunotherapy. Br. J. Cancer 2019, 120, 6–15. [Google Scholar] [CrossRef]
- Von Locquenghien, M.; Rozalén, C.; Celià-Terrassa, T. Interferons in Cancer Immunoediting: Sculpting Metastasis and Immunotherapy Response. J. Clin. Investig. 2021, 131, e143296. [Google Scholar] [CrossRef]
- Zhu, S.; Zhang, T.; Zheng, L.; Liu, H.; Song, W.; Liu, D.; Li, Z.; Pan, C.X. Combination Strategies to Maximize the Benefits of Cancer Immunotherapy. J. Hematol. Oncol. 2021, 14, 156. [Google Scholar] [CrossRef]
- Lin, W.-W.; Karin, M. A Cytokine-Mediated Link between Innate Immunity, Inflammation, and Cancer. J. Clin. Investig. 2007, 117, 1175–1183. [Google Scholar] [CrossRef]
- O’Malley, G.; Heijltjes, M.; Houston, A.M.; Rani, S.; Ritter, T.; Egan, L.J.; Ryan, A.E. Mesenchymal Stromal Cells (MSCs) and Colorectal Cancer: A Troublesome Twosome for the Anti-Tumour Immune Response? Oncotarget 2016, 7, 60752–60774. [Google Scholar] [CrossRef]
- Ma, X.; Liu, J.; Yang, X.; Fang, K.; Zheng, P.; Liang, X.; Liu, J. Mesenchymal Stem Cells Maintain the Stemness of Colon Cancer Stem Cells via Interleukin-8/Mitogen-Activated Protein Kinase Signaling Pathway. Exp. Biol. Med. 2020, 245, 562–575. [Google Scholar] [CrossRef]
- Hombach, A.A.; Geumann, U.; Günther, C.; Hermann, F.G.; Abken, H. IL7-IL12 Engineered Mesenchymal Stem Cells (MSCs) Improve A CAR T Cell Attack Against Colorectal Cancer Cells. Cells 2020, 9, 873. [Google Scholar] [CrossRef]
- Chan, L.Y.; Dass, S.A.; Tye, G.J.; Imran, S.A.M.; Wan Kamarul Zaman, W.S.; Nordin, F. CAR-T Cells/-NK Cells in Cancer Immunotherapy and the Potential of MSC to Enhance Its Efficacy: A Review. Biomedicines 2022, 10, 804. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Lv, K.; Sun, J.; Guan, J. Anti-Tumor Effects of Engineered Mesenchymal Stem Cells in Colon Cancer Model. Cancer Manag. Res. 2019, 11, 8443–8450. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Ni, J.; Chen, J.; Ma, G.; Zhao, M.; Zhu, S.; Shi, T.; Zhu, J.; Huang, Z.; Zhang, J.; et al. Dual-Functionalized MSCs That Express CX3CR1 and IL-25 Exhibit Enhanced Therapeutic Effects on Inflammatory Bowel Disease. Mol. Ther. 2020, 28, 1214–1228. [Google Scholar] [CrossRef] [PubMed]
- Quiroz-Reyes, A.G.; Delgado-Gonzalez, P.; Islas, J.F.; Gallegos, J.L.D.; Garza, J.H.M.; Garza-Treviño, E.N. Behind the Adaptive and Resistance Mechanisms of Cancer Stem Cells to Trail. Pharmaceutics 2021, 13, 1062. [Google Scholar] [CrossRef] [PubMed]
- Rossignoli, F.; Spano, C.; Grisendi, G.; Foppiani, E.M.; Golinelli, G.; Mastrolia, I.; Bestagno, M.; Candini, O.; Petrachi, T.; Recchia, A.; et al. MSC-Delivered Soluble TRAIl and Paclitaxel as Novel Combinatory Treatment for Pancreatic Adenocarcinoma. Theranostics 2019, 9, 436–448. [Google Scholar] [CrossRef]
- Mueller, L.P.; Luetzkendorf, J.; Widder, M.; Nerger, K.; Caysa, H.; Mueller, T. TRAIL-Transduced Multipotent Mesenchymal Stromal Cells (TRAIL-MSC) Overcome TRAIL Resistance in Selected CRC Cell Lines in Vitro and in Vivo. Cancer Gene Ther. 2011, 18, 229–239. [Google Scholar] [CrossRef]
- Uchibori, R.; Okada, T.; Ito, T.; Urabe, M.; Mizukami, H.; Kume, A.; Ozawa, K. Retroviral Vector-Producing Mesenchymal Stem Cells for Targeted Suicide Cancer Gene Therapy. J. Gene Med. 2009, 11, 373–381. [Google Scholar] [CrossRef]
- Zhang, T.-Y.; Huang, B.; Wu, H.-B.; Wu, J.-H.; Li, L.-M.; Li, Y.-X.; Hu, Y.-L.; Han, M.; Shen, Y.-Q.; Tabata, Y.; et al. Synergistic Effects of Co-Administration of Suicide Gene Expressing Mesenchymal Stem Cells and Prodrug-Encapsulated Liposome on Aggressive Lung Melanoma Metastases in Mice. J. Control. Release 2015, 209, 260–271. [Google Scholar] [CrossRef]
- Alieva, M.; Bagó, J.R.; Aguilar, E.; Soler-Botija, C.; Vila, O.F.; Molet, J.; Gambhir, S.S.; Rubio, N.; Blanco, J. Glioblastoma Therapy with Cytotoxic Mesenchymal Stromal Cells Optimized by Bioluminescence Imaging of Tumor and Therapeutic Cell Response. PLoS ONE 2012, 7, e35148. [Google Scholar] [CrossRef]
- Kenarkoohi, A.; Bamdad, T.; Soleimani, M.; Soleimanjahi, H.; Fallah, A.; Falahi, S. HSV-TK Expressing Mesenchymal Stem Cells Exert Inhibitory Effect on Cervical Cancer Model. Int. J. Mol. Cell. Med. 2020, 9, 146–153. [Google Scholar] [CrossRef]
- Einem, J.C.; Guenther, C.; Volk, H.; Grütz, G.; Hirsch, D.; Salat, C.; Stoetzer, O.; Nelson, P.J.; Michl, M.; Modest, D.P.; et al. Treatment of Advanced Gastrointestinal Cancer with Genetically Modified Autologous Mesenchymal Stem Cells: Results from the Phase 1/2 TREAT-ME-1 Trial. Int. J. Cancer 2019, 145, 1538–1546. [Google Scholar] [CrossRef] [PubMed]
- Kucerova, L.; Altanerova, V.; Matuskova, M.; Tyciakova, S.; Altaner, C. Adipose Tissue–Derived Human Mesenchymal Stem Cells Mediated Prodrug Cancer Gene Therapy. Cancer Res. 2007, 67, 6304–6313. [Google Scholar] [CrossRef] [PubMed]
- Golinelli, G.; Mastrolia, I.; Aramini, B.; Masciale, V.; Pinelli, M.; Pacchioni, L.; Casari, G.; Dall’Ora, M.; Soares, M.B.P.; Damasceno, P.K.F.; et al. Arming Mesenchymal Stromal/Stem Cells Against Cancer: Has the Time Come? Front. Pharmacol. 2020, 11, 529921. [Google Scholar] [CrossRef]
- Zhu, Y.; Cheng, M.; Yang, Z.; Zeng, C.; Chen, J.; Xie, Y.; Luo, S.; Zhang, K.; Zhou, S.-F.; Lv, N. Mesenchymal Stem Cell-Based NK4 Gene Therapy in Nude Mice Bearing Gastric Cancer Xenografts. Drug Des. Dev. Ther. 2014, 8, 2449. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.-T.; Wu, M.-H.; Chen, M.-J.; Lin, S.-P.; Yen, Y.-T.; Hung, S.-C. Combination of Mesenchymal Stem Cell-Delivered Oncolytic Virus with Prodrug Activation Increases Efficacy and Safety of Colorectal Cancer Therapy. Biomedicines 2021, 9, 548. [Google Scholar] [CrossRef]
- Dafni, U.; Michielin, O.; Lluesma, S.M.; Tsourti, Z.; Polydoropoulou, V.; Karlis, D.; Besser, M.J.; Haanen, J.; Svane, I.M.; Ohashi, P.S.; et al. Efficacy of Adoptive Therapy with Tumor-Infiltrating Lymphocytes and Recombinant Interleukin-2 in Advanced Cutaneous Melanoma: A Systematic Review and Meta-Analysis. Ann. Oncol. 2019, 30, 1902–1913. [Google Scholar] [CrossRef]
- Santoiemma, P.P.; Powell, D.J. Tumor Infiltrating Lymphocytes in Ovarian Cancer. Cancer Biol. Ther. 2015, 16, 807–820. [Google Scholar] [CrossRef]
- Zacharakis, N.; Chinnasamy, H.; Black, M.; Xu, H.; Lu, Y.C.; Zheng, Z.; Pasetto, A.; Langhan, M.; Shelton, T.; Prickett, T.; et al. Immune Recognition of Somatic Mutations Leading to Complete Durable Regression in Metastatic Breast Cancer. Nat. Med. 2018, 24, 724–730. [Google Scholar] [CrossRef]
- Stevanović, S.; Draper, L.M.; Langhan, M.M.; Campbell, T.E.; Kwong, M.L.; Wunderlich, J.R.; Dudley, M.E.; Yang, J.C.; Sherry, R.M.; Kammula, U.S.; et al. Complete Regression of Metastatic Cervical Cancer after Treatment with Human Papillomavirus-Targeted Tumor-Infiltrating T Cells. J. Clin. Oncol. 2015, 33, 1543–1550. [Google Scholar] [CrossRef]
- Met, Ö.; Jensen, K.M.; Chamberlain, C.A.; Donia, M.; Svane, I.M. Principles of Adoptive T Cell Therapy in Cancer. Semin. Immunopathol. 2019, 41, 49–58. [Google Scholar] [CrossRef]
- Guedan, S.; Calderon, H.; Posey, A.D.; Maus, M.V. Engineering and Design of Chimeric Antigen Receptors. Mol. Ther. Methods Clin. Dev. 2018, 12, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Shimabukuro-Vornhagen, A.; Gödel, P.; Subklewe, M.; Stemmler, H.J.; Schlößer, H.A.; Schlaak, M.; Kochanek, M.; Böll, B.; von Bergwelt-Baildon, M.S. Cytokine Release Syndrome. J. Immunother. Cancer 2018, 6, 56. [Google Scholar] [CrossRef] [PubMed]
- Ghazi, B.; el Ghanmi, A.; Kandoussi, S.; Ghouzlani, A.; Badou, A. CAR T-Cells for Colorectal Cancer Immunotherapy: Ready to Go? Front. Immunol. 2022, 13, 978195. [Google Scholar] [CrossRef] [PubMed]
- Sur, D.; Havasi, A.; Cainap, C.; Samasca, G.; Burz, C.; Balacescu, O.; Lupan, I.; Deleanu, D.; Irimie, A. Chimeric Antigen Receptor T-Cell Therapy for Colorectal Cancer. J. Clin. Med. 2020, 9, 182. [Google Scholar] [CrossRef]
- D’Aloia, M.M.; Zizzari, I.G.; Sacchetti, B.; Pierelli, L.; Alimandi, M. CAR-T Cells: The Long and Winding Road to Solid Tumors. Cell Death Dis. 2018, 9, 282. [Google Scholar] [CrossRef]
- Yang, L.; Shi, P.; Zhao, G.; Xu, J.; Peng, W.; Zhang, J.; Zhang, G.; Wang, X.; Dong, Z.; Chen, F.; et al. Targeting Cancer Stem Cell Pathways for Cancer Therapy. Signal Transduct. Target. Ther. 2020, 5, 8. [Google Scholar] [CrossRef]
- Chmielewski, M.; Kopecky, C.; Hombach, A.A.; Abken, H. IL-12 Release by Engineered T Cells Expressing Chimeric Antigen Receptors Can Effectively Muster an Antigen-Independent Macrophage Response on Tumor Cells That Have Shut down Tumor Antigen Expression. Cancer Res. 2011, 71, 5697–5706. [Google Scholar] [CrossRef]
- Hou, B.; Tang, Y.; Li, W.; Zeng, Q.; Chang, D. Efficiency of CAR-T Therapy for Treatment of Solid Tumor in Clinical Trials: A Meta-Analysis. Dis. Markers 2019, 2019, 3425291. [Google Scholar] [CrossRef]
- Berahovich, R.; Liu, X.; Zhou, H.; Tsadik, E.; Xu, S.; Golubovskaya, V.; Wu, L. Hypoxia Selectively Impairs CAR-T Cells In Vitro. Cancers 2019, 11, 602. [Google Scholar] [CrossRef]
- Huang, Q.; Xia, J.; Wang, L.; Wang, X.; Ma, X.; Deng, Q.; Lu, Y.; Kumar, M.; Zhou, Z.; Li, L.; et al. MiR-153 Suppresses IDO1 Expression and Enhances CAR T Cell Immunotherapy. J. Hematol. Oncol. 2018, 11, 58. [Google Scholar] [CrossRef]
- Chow, A.; Perica, K.; Klebanoff, C.A.; Wolchok, J.D. Clinical Implications of T Cell Exhaustion for Cancer Immunotherapy. Nat. Rev. Clin. Oncol. 2022, 19, 775–790. [Google Scholar] [CrossRef] [PubMed]
- Yi, X.; Hu, W. Advances in Adoptive Cellular Therapy for Colorectal Cancer: A Narrative Review. Ann. Transl. Med. 2022, 10, 1404. [Google Scholar] [CrossRef] [PubMed]
- Patsalias, A.; Kozovska, Z. Personalized Medicine: Stem Cells in Colorectal Cancer Treatment. Biomed. Pharmacother. 2021, 141, 111821. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Zhang, Z.; Xu, X.; Xu, Z.; Wang, S.; Huang, D.; Li, Y.; Mou, X.; Liu, F.; Xiang, C. Menstrual Blood-Derived Stem Cells as Delivery Vehicles for Oncolytic Adenovirus Virotherapy for Colorectal Cancer. Stem Cells Dev. 2019, 28, 882–896. [Google Scholar] [CrossRef]
- Feng, H.; Zhao, J.; Schiergens, T.S.; Wang, P.; Ou, B.; Al-Sayegh, R.; Li, M.; Lu, A.; Yin, S.; Thasler, W.E. Bone Marrow-Derived Mesenchymal Stromal Cells Promote Colorectal Cancer Cell Death under Low-Dose Irradiation. Br. J. Cancer 2018, 118, 353–365. [Google Scholar] [CrossRef]
- Yuan, J.; Wei, Z.; Xu, X.; Ocansey, D.K.W.; Cai, X.; Mao, F. The Effects of Mesenchymal Stem Cell on Colorectal Cancer. Stem Cells Int. 2021, 2021, 9136583. [Google Scholar] [CrossRef]
- Hossain, M.S.; Karuniawati, H.; Jairoun, A.A.; Urbi, Z.; Ooi, D.J.; John, A.; Lim, Y.C.; Kibria, K.M.K.; Mohiuddin, A.K.M.; Ming, L.C.; et al. Colorectal Cancer: A Review of Carcinogenesis, Global Epidemiology, Current Challenges, Risk Factors, Preventive and Treatment Strategies. Cancers 2022, 14, 1732. [Google Scholar] [CrossRef]
- Mokhtari, R.B.; Homayouni, T.S.; Baluch, N.; Morgatskaya, E.; Kumar, S.; Das, B.; Yeger, H. Combination Therapy in Combating Cancer. Oncotarget 2017, 8, 38022. [Google Scholar] [CrossRef]

| Subtype | CMS1-MSI Immune Subtype | CMS2, the Canonical Subtype | CMS3, the Metabolic Subtype | CMS4, the Mesenchymal Subtype | Ref |
|---|---|---|---|---|---|
| Mutations | MSI is high along with CIMP+, BRAF, and a low prevalence of SNCA. | WNT, MYC, SCNA (high activation), and BRAF. | KRAS-activating mutations; moderate or low mixed state of MSI and intermediate CIMP; moderate activation of WNT and MYC, with PIK3CA mutation and IGBP3 overexpression. | TGFβ activation; EMT; High SCNA. | [47,48,49] |
| Immune characteristics | Low CD8 and CD4 T cells, and NK cells infiltration. | Lack of DC recruitment. Absent of immune infiltration and regulatory cytokines. | Poorly immunogenic without immune infiltrates or regulatory cytokines. | High infiltration of CTLs, macrophages, and stromal cells; overexpression of EMT markers, such as TGF-B and CXCL-12. | [45,50] |
| Frequency Predominance | Proximal colon (14%) | Distal colon and rectum (37%) | Without predominance (13%) | Distal colon and rectum (23%) | [51] |
| Prediction of immunotherapy response | Good response (80%); Poor response to immunotherapy (20%). | Only 18% of CMS2 patients. | Only 19% of CMS3 patients. | 26% of CMS4 patients are not candidates. | [46] |
| Title | Clinical Trial ID | Colorectal Cancer Stage | Trial Phase | Administration Route | Cell Type | Status |
|---|---|---|---|---|---|---|
| NKG2D CAR-T cells to treat patients with previously treated liver metastatic colorectal cancer. | NCT05248048 | Metastatic | Early Phase I | Hepatic artery transfusion | CAR-T (NKG2D) | Recruiting |
| T cell receptor-based therapy of metastatic colorectal cancer. | NCT03431311 | Advanced metastatic (MSI+) | I/II | Intravenous (i.v.) injections | T cells (TGFβRII) | Terminated |
| A single-arm pilot clinical study of chimeric antigen receptor T cells combined with interventional therapy in advanced liver malignancy. | NCT02959151 | Metastatic | I/II | Vascular interventional therapy or intra-tumor injection | CAR-T cells (CEA) | Unknown |
| Clinical study of CEA-targeted CAR-T therapy for CEA-positive advanced malignant solid tumors. | NCT05415475 | Advanced | I | Intravenous infusion or intraperitoneal injection | CAR-T cells (CEA) | Recruiting |
| A clinical study of CEA-targeted CAR-T cells in the treatment of CEA-positive advanced malignant solid tumors. | NCT05396300 | Advanced | I | Intravenous infusion or intraperitoneal injection | CAR-T cells (CEA) | Recruiting |
| A single-arm pilot clinical study of chimeric antigen receptor T cells combined with interventional therapy in advanced liver malignancy. | NCT02959151 | Metastatic | I/II | Vascular interventional therapy or intra-tumor injection | CAR-T cells (CEA) | Unknown |
| A clinical research of CAR T cells targeting CEA-positive cancer. | NCT02349724 | Relapse or refractory | I | Intravenous infusion | CAR-T cells (CEA) | Unknown |
| Hepatic transarterial administrations of NKR-2 in patients with unresectable liver metastases from colorectal cancer (LINK). | NCT03370198 | Metastatic | I | Hepatic transarterial administration | NKR-2 cells (NKG2D) | Active, not recruiting |
| Dose escalation and dose expansion phase I study to assess the safety and clinical activity of multiple doses of NKR-2 administered concurrently with FOLFOX in colorectal cancer with potentially resectable liver metastases (SHRINK). | NCT03310008 | Metastatic | I | Infusion administered concurrently with standard chemotherapy | NKR-2 cells (NKG2D) | Active, not recruiting |
| NKG2D CAR-NK cell therapy in patients with refractory metastatic colorectal cancer. | NCT05213195 | Metastatic | I | Intra-peritoneal infusion | CAR-NK (NKG2D) | Recruiting |
| High-activity natural killer immunotherapy for small metastases of colorectal cancer. | NCT03008499 | Metastatic | I/II | Intravenous infusion | NK cells | Completed |
| CAR-pNK cell immunotherapy in MUC1 positive relapsed or refractory solid tumor. | NCT02839954 | Relapse or refractory | I/II | Intravenous infusion | CAR-pNK cells (MUC-1) | Unknown |
| ACE1702 in subjects with advanced or metastatic HER2-expressing solid tumors. | NCT04319757 | Advanced or metastatic | I | Intravenous infusion | NK cells (HER-2) | Recruiting |
| Cellular Therapy | Advantages | Disadvantages |
|---|---|---|
| T cell therapy | It has already been clinically successful in treating hematologic malignancies. Tumor-infiltrating lymphocytes (TILs) and genetically modified T cells (TCRs and CARs) can elicit a cytotoxic response, causing the apoptosis of CSCs. | Limited by biological barriers to the tumor mass and the immunosuppressive tumor microenvironment, such as a high level of hypoxia, low concentrations of nutrients, and the high release of acid products. [58]. Expression of a heterogeneous pattern of tumor antigens produced the evasion of antigen-specific CAR-T cells [52,124]. |
| NK cell therapy | The expression of ligands for natural cytotoxicity receptors can mediate direct CSC apoptosis. Cytokine-induced memory-like NK cells (CIML-NK) can be combined with CAR engineering. | Limited by the immunosuppressive nature of tumor microenvironment and CRC, as seen in T cell therapy disadvantages. Difficulty in ex vivo expansion [5,79]. Low efficacy [70]. |
| Macrophage therapy | M1 macrophages can cause tumor cell apoptosis through phagocytosis, antibody-dependent cellular cytotoxicity (ADCC), the release of molecules including TNF-α and nitric oxide (NO), and recruitment of cytotoxic T cells. | M2 macrophages contribute to angiogenesis, EMT of tumor cells, and immunosuppression, promoting the metastasis of CRC. |
| MSC therapy | Inhibits aberrant crypt foci formation and tumor development when administered in the early phase of colorectal tumorigenesis in rat models. Secretes cytokines that inhibit proliferation and induce apoptosis of CRC cells. Supports other cellular therapies by enhancing their homing capacity and healing tissue damage after radiotherapy. MSC-derived exosomes suppress proliferation, migration, and invasion of CRC cells through paracrine and direct tumor cell contact. | Induces an immunosuppressed microenvironment, resulting in impaired immunological sensitivity and the promotion of tumor growth and recurrence. BM-MSCs promote tumor growth by inducing the EMT progression of CRC cells in vitro. Pro-apoptotic and pro-survival effects can be difficult to predict and control. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garza Treviño, E.N.; Quiroz Reyes, A.G.; Rojas Murillo, J.A.; de la Garza Kalife, D.A.; Delgado Gonzalez, P.; Islas, J.F.; Estrada Rodriguez, A.E.; Gonzalez Villarreal, C.A. Cell Therapy as Target Therapy against Colon Cancer Stem Cells. Int. J. Mol. Sci. 2023, 24, 8163. https://doi.org/10.3390/ijms24098163
Garza Treviño EN, Quiroz Reyes AG, Rojas Murillo JA, de la Garza Kalife DA, Delgado Gonzalez P, Islas JF, Estrada Rodriguez AE, Gonzalez Villarreal CA. Cell Therapy as Target Therapy against Colon Cancer Stem Cells. International Journal of Molecular Sciences. 2023; 24(9):8163. https://doi.org/10.3390/ijms24098163
Chicago/Turabian StyleGarza Treviño, Elsa N., Adriana G. Quiroz Reyes, Juan Antonio Rojas Murillo, David A de la Garza Kalife, Paulina Delgado Gonzalez, Jose F. Islas, Ana Esther Estrada Rodriguez, and Carlos A. Gonzalez Villarreal. 2023. "Cell Therapy as Target Therapy against Colon Cancer Stem Cells" International Journal of Molecular Sciences 24, no. 9: 8163. https://doi.org/10.3390/ijms24098163
APA StyleGarza Treviño, E. N., Quiroz Reyes, A. G., Rojas Murillo, J. A., de la Garza Kalife, D. A., Delgado Gonzalez, P., Islas, J. F., Estrada Rodriguez, A. E., & Gonzalez Villarreal, C. A. (2023). Cell Therapy as Target Therapy against Colon Cancer Stem Cells. International Journal of Molecular Sciences, 24(9), 8163. https://doi.org/10.3390/ijms24098163






