Abstract
Biomaterial-based therapies have been receiving attention for treating microbial infections mainly to overcome the increasing number of drug-resistant bacterial strains and off-target impacts of therapeutic agents by conventional strategies. A fibrous, non-soluble protein, collagen, is one of the most studied biopolymers for the development of antimicrobial biomaterials owing to its superior physicochemical, biomechanical, and biological properties. In this study, we reviewed the different approaches used to develop collagen-based antimicrobial devices, such as non-pharmacological, antibiotic, metal oxide, antimicrobial peptide, herbal extract-based, and combination approaches, with a particular focus on preclinical studies that have been published in the last decade.
1. Introduction
Microbial infections threaten public health due to the wide range of enervating effects of disease-causing microbes (e.g., bacteria, viruses, and fungi), which have been the primary causatives of the dissemination of pathogenic diseases [1,2,3]. Antibiotics have been the first choice for infection treatment since the discovery of penicillin in 1928 by Alexander Fleming. Although their low toxicity and great bactericidal features, the usage of antibiotics for a long time led to the burst and release of antibiotic-resistant bacteria (ARB), hence the emergence of antimicrobial resistance (AMR) related diseases [4,5].
Healthcare-associated infections are the major type of AMR-caused infections that may delay discharge from the hospital or cause deaths as well as a rise in healthcare costs, second-line drug costs, and unsuccess in treatments [6]. According to the European Centre for Disease Prevention and Control (ECDC), in Europe, annually, 3.8 million people catch healthcare-associated diseases caused by AMR [7], and 90 thousand people die because of these diseases [8]. Besides, the Centre for Disease Control and Prevention (CDC) reported that more than 2.8 million people suffer from AMR diseases each year, while 35,000 patients die in the US [9]. Moreover, the cost for just one AMR infection case is predicted approximately EUR 9–34 thousand more than non-resistant microbial infections [10], whilst more than EUR 9 billion are required in Europe [11,12]. On the other hand, bacterial resistance itself adds more than USD 20 billion to healthcare costs in the US [9].
In response, a variety of clinical interventions have been employed to combat AMR-related diseases, including the use of combination therapies, strategies aim targeting antimicrobial-resistant enzymes or bacteria, longer treatment durations, and off-label uses [13,14]. Despite these efforts, the development of new and effective antimicrobials has been slow, and the emergence of resistance to these interventions has become incremental. Furthermore, some of these interventions come with their drawbacks, such as an increase in side effects, higher medicinal costs, and longer hospital stays [15]. As such, there is a clinical need for alternative approaches such as biomaterial-based strategies to combat antimicrobial resistance and promote the development of more effective therapies. The various antimicrobial collagen biomaterial strategies have recently come to the fore in the literature within this framework.
Collagen is a fibrous, insoluble protein that is the main component of the extracellular matrix (ECM) of several tissues [16] of humans and many animals, such as bone [17], cartilage [18], tendon [19], skin [20], and muscle [21]. A natural biopolymer, collagen is one of the most abundant proteins in mammals [22] and becomes prominent among the other polymers due to its superior and distinct properties. Excellent biocompatibility, good biodegradability, hydrophilicity, remarkable mechanical properties, low or no antigenicity, hemostatic properties, and cell-binding ability are some of the important features of collagen, which make it important for many biomaterial applications, such as tissue engineering and drug delivery purposes [23,24,25,26]. On the other hand, the resistance of collagen to bacteria makes it outstanding to use in the development of antimicrobial biomaterials for many kinds of applications, such as the treatment of wounds and bone infections. Owing to its natural ability to fight infection, collagen contributes to keeping the infection site sterile [26,27]. Moreover, collagen has very high availability since its abundance in mammals and marine organisms as well as its producibility from yeasts, plants, insects, and mammal cells by recombinant protein technology [23,28] (Figure 1). Despite its proven properties, collagen-based biomaterials need to incorporate bioactive molecules such as antibiotics and plant-based agents in order to increase their biological activities.
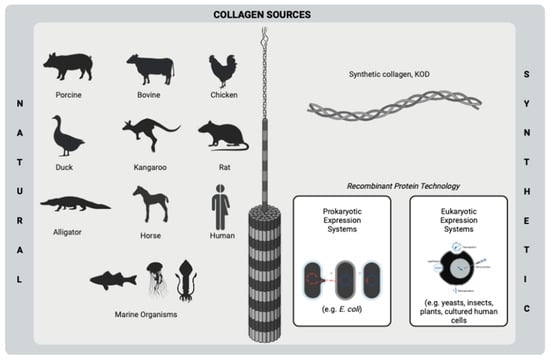
Figure 1.
Sources of collagen using biomedical purposes. This figure was created by BioRender.com.
The use of alternative antimicrobial agents (e.g., herbal extracts, antimicrobial peptides, and metal oxide nanoparticles) as a substitute for antibiotics has started to gain importance in an attempt to overcome the emergence of AMR due to ARB strains [2,29,30]. Even though clinically proven, generally, single and limited antibacterial agents (e.g., silver and gentamicin), including collagen-based products, are on the market (Table 1). Therefore, new modern products are clinically needed to improve treatment efficacy. In this respect, collagen has been widely used as a carrier vehicle for several kinds of bioactive molecules with their ensured biostability owing to its superior biological activities [23,24,25]. Herein, we briefly reviewed different approaches for designing collagen-based antimicrobial products (Figure 2) with a particular focus on preclinical studies which have been published in the last decade.

Table 1.
Commercially available collagen-based antibacterial products. Abbreviations: Oxidized regenerated cellulose: ORC; Carboxymethyl cellulose: CMC; Ethylenediamine tetra acetic acid: EDTA; Silver chloride: AgCl; Silver (I) oxide: Ag2O.
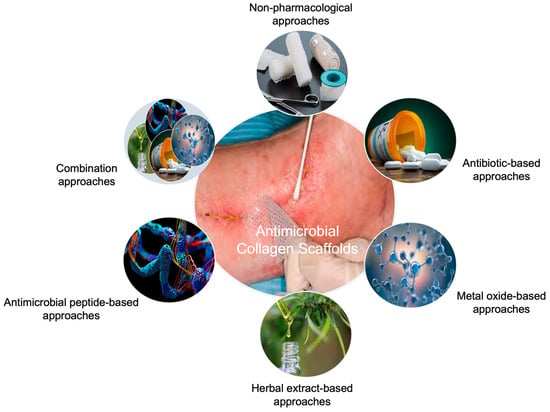
Figure 2.
Approaches to developing collagen-based antimicrobial biomaterials for tissue engineering applications.
2. Non-Pharmacological Approaches
In the literature, there are several studies concerning collagen-based biomaterial therapies for healing microbial infections without the incorporation of any therapeutics (Table 2). Chitosan is a commonly used additive polymer for collagen scaffolds to enhance bactericidal effects due to its good antibacterial activity against several Gram-positive and Gram-negative bacterial strains [47]. Chitosan and oxidized bacterial cellulose with composite collagen hemostasis dressings exhibited a faster hemostasis rate (86 s) than commercial gauze (186 s) in vivo rat liver trauma model through the collagen to promote platelet and erythrocyte adhesion as well as to improve pro coagulation activity [48]. Collagen hydrolysate wound dressings, including chitosan and tetraethoxysilane (TEOS), accelerated the healing of wounds in the Wistar rats compared to gauze, where the wound recovered completely within 14 days. Besides the augmented healing process, the re-epithelization rate was evaluated as 81% and 55% for composite and control groups, respectively on the 10th post-treatment day. However, despite the successful preclinical findings, developed dressings could not inhibit the growth of P. aeruginosa, which is one of the most common causative bacteria for wound infections [49]. On the other hand, some inorganic compounds were incorporated in biomaterial formation to increase targeted tissue regeneration and antimicrobial activity [50,51,52]. For instance, the association of collagen with bioactive glass (BG) may promote the antibacterial activity of pristine collagen by the increase in osmotic pressure, which is raised proportionally to the released ions (e.g., silicon, calcium, and phosphorous) composed of bioactive glasses. Hence, the growth of bacteria is inhibited because of the formed region by ions. It is reported that collagen/BG scaffolds implanted in Sprague–Dawley (SD) rats’ dorsum skin defect healed the wound faster than the clinically used product, Kaltostat, and triggered re-epithelization regarding histologic results [52].

Table 2.
Illustrative examples of collagen antimicrobial scaffolds designed with non-pharmacological approaches. Abbreviations: Antimicrobial susceptibility testing: AST; Collagen: Col; Chitosan: Chi; Weight: w; Volume: v; Spontaneously immortalized, human keratinocyte line: HaCaT; Staphylococcus aureus: S. aureus; Escherichia coli: E. coli; Komagataeibacter xylinus: K. xylinus; Bacillus subtilis: B. subtilis; Pseudomonas aeruginosa: P. aeruginosa; Bioactive glass: BG; Glutaraldehyde: GTA; Oxidized bacterial cellulose: OBC; Hyaluronic acid: HA; Tetraethoxysilane: TEOS; Beta-tricalcium phosphate: β-TCP; Bone marrow mesenchymal stem cell: BMSC; Human dermal fibroblast: HDF; Human umbilical vein endothelial cell: HUVEC; Human umbilical cord mesenchymal stem cell: hUCMSC.
3. Pharmacological Approaches
3.1. Antibiotic-Based Approaches
Antibiotics are well-known antimicrobial drugs that have an important role in the treatment of bacterial infections by fighting and preventing the growth of bacteria [60]. The incorporation of various antibiotics, such as aminoglycosides [61,62,63,64] and tetracyclines [65,66,67,68,69], into collagen scaffolds have been studied for a long time (Table 3). These therapeutic agents are generally studied for infected wound and bone defect treatments. For example, when mupirocin was loaded into collagen sponges, complete closure and re-epithelization on full-thickness excision wounds treated with the developed composite scaffold were achieved. Nevertheless, scaffolds could provide significant antibacterial activity against Gram-positive methicillin-resistant S. aureus (MRSA) and B. subtilis [70]. In another study of a commonly studied antibiotic, doxycycline-loaded collagen-based scaffolds increased the gap closure of bone defects in Wistar rats from 25% to 40% [69]. On the other hand, the concentration of collagen is an effective parameter for the controlled antibiotic release from a biomaterial. An increase in collagen concentration from 20% to 40% (w/w) did not enhance the in vivo healing of mice wounds, treated with cefazolin, including collagen-based nanofibrous mat, due to inadequate release of antibiotics on the wound bed. This outcome indicates the role of polymer concentration in the sustained release of an incorporated antimicrobial agent in a biomaterial formulation [71].
In some strategies, the effect of antibiotics is enhanced by the addition of chitosan into the biomaterial formulation. Chitosan exerts its antibacterial activity by binding to the negatively charged bacterial cell wall, thus initiating a process that leads either to the disruption of bacterial cells or to a change in the bacterial membrane permeability [72]. For instance, minocycline-caged chitosan nanoparticles incorporated into collagen sponges demonstrated almost complete degradation and no remarkable inflammation in the SD rat skull defect model [66]. The antimicrobial activity of biomaterials was also advanced by generating a hypoxic environment by including oxygen-generating additives. Oxygen-generating calcium peroxide particles were coated on the ciprofloxacin-loaded collagen-based sponges by Tripathi et al. to advance the wound healing rate by generating a hypoxic environment. The tested scaffolds on the skin flip model led to less necrosis and displayed almost total wound recovery with the help of the antibacterial activity of the antibiotic and hypoxic conditions, whilst the untreated group showed about 75% of wound closure within 15 days [73]. Even though good inhibitory effects are reported, it is known that long-term use of antibiotics results in the emergence of ARB strains. In the attempt to research a few alternatives, non-antibiotic therapeutic approaches have become inevitable.

Table 3.
Illustrative examples of collagen antimicrobial scaffolds designed with antibiotic-based approaches. Abbreviations: Antimicrobial susceptibility testing: AST; Weight: w; Volume: v; Collagen: Col; Chitosan: Chi; Hyaluronic acid: HA; Hexamethylene diisocyanate: HMDI; Cefaclor: Cef; Ranalexin: Ran; Escherichia coli: E. coli; Staphylococcus epidermidis: S. epidermidis; Staphylococcus aureus: S. aureus; Pseudomonas aeruginosa: P. aeruginosa; Enterococcus faecalis: E. faecalis; Methicillin-resistant Staphylococcus aureus: MRSA; Bacillus subtilis: B. subtilis; Porphyromonas gingivalis: P. gingivalis; Fusobacterium nucleatum: F. nucleatum; Hydroxy apatite: Hap; Citrate hydroxy apatite: cHap; N-(3-dimethylaminopropyl)-N-ethylcarbodiimide hydrochloride: EDC; N-hydroxysuccinimide: NHS; Nanoparticle: NP; Sodium tripolyphosphate: TPP; Poly(lactic acid): PLA; Sodium hydroxide: NaOH; Ethanol: EtOH; Polyethylene oxide: PEO; Polycaprolactone: PCL; Ethyl cellulose: EC; Polyvinylpyrrolidone: PVP; Bioactive glass: BG; Glutaraldehyde: GTA; Human bone marrow-derived stromal cell culture: hBM-MSC; Calcium peroxide: CPO; Cellulose nanocrystal: CNC; Ciprofloxacin hydrochloride: CFH; Rabbit adipose-derived stem cell: rASC.
Table 3.
Illustrative examples of collagen antimicrobial scaffolds designed with antibiotic-based approaches. Abbreviations: Antimicrobial susceptibility testing: AST; Weight: w; Volume: v; Collagen: Col; Chitosan: Chi; Hyaluronic acid: HA; Hexamethylene diisocyanate: HMDI; Cefaclor: Cef; Ranalexin: Ran; Escherichia coli: E. coli; Staphylococcus epidermidis: S. epidermidis; Staphylococcus aureus: S. aureus; Pseudomonas aeruginosa: P. aeruginosa; Enterococcus faecalis: E. faecalis; Methicillin-resistant Staphylococcus aureus: MRSA; Bacillus subtilis: B. subtilis; Porphyromonas gingivalis: P. gingivalis; Fusobacterium nucleatum: F. nucleatum; Hydroxy apatite: Hap; Citrate hydroxy apatite: cHap; N-(3-dimethylaminopropyl)-N-ethylcarbodiimide hydrochloride: EDC; N-hydroxysuccinimide: NHS; Nanoparticle: NP; Sodium tripolyphosphate: TPP; Poly(lactic acid): PLA; Sodium hydroxide: NaOH; Ethanol: EtOH; Polyethylene oxide: PEO; Polycaprolactone: PCL; Ethyl cellulose: EC; Polyvinylpyrrolidone: PVP; Bioactive glass: BG; Glutaraldehyde: GTA; Human bone marrow-derived stromal cell culture: hBM-MSC; Calcium peroxide: CPO; Cellulose nanocrystal: CNC; Ciprofloxacin hydrochloride: CFH; Rabbit adipose-derived stem cell: rASC.
| Composition | Collagen Source | Scaffold Form | Crosslinking | Therapeutic Agent | Release Profile | AST | Bacterial Strain/ Cell Line | Antibacterial Activity | Hypothetic Material | Refs. |
|---|---|---|---|---|---|---|---|---|---|---|
| Col (5% w/v) | Porcine dermis | Sponge | HMDI (0.625–10% w/v) | Cef, Ran (0–500 µg/mL) | 10 µg/mL of 90% Cef and 95% Ran released by day 7. | Disc diffusion | E. coli, S. epidermidis Adult HDFs | 100 µg/mL of Cef showed activity on tested strains, while Ran did not. | Localized drug delivery vehicle | [74] |
| Col (1% w/w) Chi (1% w/w) HA (1% w/w) | Rat tail tendon | Thin film | Not available | Gentamicin sulfate (0.4 mg/cm2 film) | Not studied | Disc diffusion | S. aureus, E. coli, P. aeruginosa No in vitro cell culture | Drug-loaded scaffolds showed approximately 25–30 mm of inhibition zone. | Antibacterial film | [61] |
| Col (8 w%) Hap (0–15 w%) | Type I (not specified) | Micro/nanostructured layers | EDC/NHS (4:1 w ratio) | Vancomycin hydrochloride (10 w% of Col) | The max released concentration of vancomycin exceeded the MIC by up to 60–75 times for 4 weeks. | Disc diffusion | MRSA, S. epidermidis, E. faecalis SAOS-2 osteosarcoma cells | Inhibition zone diameters did not differ from standard antibiotic discs significantly. | Local drug carrier | [62] |
| Col (3 mg/mL) | Bovine tendon | Sponge | Not available | Mupirocin (2 mg/mL) (caged into silica microspheres) | Almost 90% of mupirocin was released within 3 days from sponges. | Broth dilution | B. subtilis, S. aureus, E. coli, P. aeruginosa 3T3-L1 fibroblasts | Drug-loaded wound dressings did not show sufficient antibacterial activity on B. subtilis and E. coli. | Wound dressing | [70] |
| Col Chi (2% w/v) | Mouse tail tendon | Asymmetric membrane | TPP (0.2% w/v) | Minocycline (15 µg/mL) (caged into Chi NPs) | Minocycline had sustained release until the 7th day. | Live/dead bacterial double staining | P. gingivalis, F. nucleatum MC3T3-E1 osteoblasts, L929 fibroblasts | Membranes showed 95.3%, and 92.1% of bacteriostatic activity against P. gingivalis and F. nucleatum, respectively. | Scaffold for the prevention of infection and guide bone regeneration | [65] |
| Col hydrolysate (5 mg/mL) PLA (5 mg/mL) cHap (10 mg) | Type I (not specified) | 3D-printed porous scaffold | Alkali hydrolysis (1:1 NaOH:EtOH and 0.5% w/v citric acid) | Minocycline hydrochloride (0.5 mg/mL) | A burst release of minocycline was observed within the first hour. | Disc diffusion, biofilm inhibition assay | S. aureus hBM-MSCs | Drug-loaded scaffolds showed smaller inhibition zone than standard antibiotic discs. | Antimicrobial and osteogenic scaffold | [66] |
| Col (10 w%) PLA EC (7:3, 8:2, 9:1 EC/PLA w ratio) | Fish collagen | Nanofibrous mat | Not available | Silver sulfadiazine (0.25, 0.5, 0.75 w%) | 28 ppm of silver ions were released from 0.75 w% drug-loaded mats within 96 h. | Disc diffusion | Bacillus, E. coli NIH 3T3 fibroblasts | Only 0.75% of drugs including scaffolds showed antibacterial activity against tested strains. | Wound dressing | [75] |
| Col (10, 20, 40% w/w) PVP (30% w/v) PLA PEO (Shell–Col/PVP, Core: 80:20 PLA/PEO w/w) | Bovine tendon | Nanofibrous mat | Not available | Cefazolin sodium | 44.15%, 40.80%, and 37.76% of cefazolin were released for samples containing 10%, 20%, and 30% (w/w) collagen after 6 days. | Disc diffusion | MRSA, E. coli, P. aeruginosa No in vitro cell culture | Fabricated mats showed slightly higher antibacterial activity against P. aeruginosa. | Antibacterial patch for wound healing | [71] |
| Col (10 mg/mL) | Fish collagen | Hydrogel | Alginate dialdehyde (2–10 mg/mL) | Tetracycline hydrochloride (0.01–0.2 mg/mL) | Almost 20% of antibiotics with a concentration equal to or higher than 0.1 mg/mL were released during 600 min. | Zone inhibition | S. aureus 3T3 fibroblasts | Dressings did not show high inhibition rates of S. aureus. | Wound dressing | [67] |
| Col BG (0.5 mg/mL) | Bovine | Membrane (Commercial product) | Not available | Tetracycline hydrochloride (0.05, 0.2, 0.35 mg/mL) | More than 50% of tetracycline releases within the first 6 h, and significant release was observed in 24 h. | Zone inhibition Plate counting | S. aureus (different strains), S. epidermidis MG-63 osteosarcoma cells | Developed scaffolds could significantly inhibit S. aureus growth. | Scaffold for the prevention of biomaterial-related infections | [68] |
| Col (1.5% w/v) Chi (1.5% w/v) CPO (1–4 w%) | Bovine | Sponge | EDC/NHS (3 w%, 2:1 EDC:NHS w ratio) | Ciprofloxacin hydrochloride (1 mg/mL) | Almost 80% of CFH was released from scaffolds including 4% CPO within 200 h. | Zone inhibition | E. coli, S. aureus HDFs | Scaffolds displayed good inhibition zones against both strains. | Skin tissue engineering scaffold | [73] |
| Col (5% w/v) Hap (10 w%) | Rat tail | Sponge | EDC (0.1 mM) | Doxycycline containing Hap NPs (10 w%) | A sustained release of doxycycline (about 70%) was achieved over 14 days. | Time-kill assay | S. aureus, P. aeruginosa BM-MSCs | Antibiotic addition significantly reduced the number of colonies within 24 h. | Bone tissue engineering scaffold | [69] |
| Col (1 w%) CNC (5 w%) | Bovine tendon | Sponge | GTA (0.25%) | Gentamicin sulfate (25 mg/mL) impregnated gelatin microspheres | Gentamicin was completely released after 144 h of the incubation period. | Disc diffusion | E. coli, S. aureus NIH-3T3 fibroblasts | Composite scaffolds showed higher antibacterial activity against E. coli than S. aureus. | Antibacterial skin scaffold | [63] |
| Col Chi (4, 8, 16% total polymer, various Col/Chi w ratio) | Fish | Sponge | Not available | Norfloxacin (1 w%) | An almost complete release of the drug was observed within 20 h. | Not studied | No in vitro cell culture | Not studied | Scaffold for skin regeneration | [76] |
| Col (6.5 mg/mL) | Bovine tendon | Film | EDC/NHS (1:1:6 w ratio EDC/NHS/Col-Tobramycin) | Tobramycin (15 mg/mL) | The burst release of tobramycin (40%) was observed within the first 4 h. | Plate counting | S. aureus Human corneal epithelial cells | Tobramycin-loaded films showed significantly higher inhibition than pristine films. | Scaffold for corneal repair | [64] |
| Col Na-Alginate Hap | Cowhide | Sponge | Genipin CaCl2 (10 w%) | Amoxicillin (0.5, 1, 2 mg/mL) | The long-term drug release effect was investigated. | Zone inhibition | E. coli rASCs | Scaffolds could effectively inhibit E. coli growth. | Composite scaffold for infected bone defects | [77] |
3.2. Non-Antibiotic-Based Approaches
Antimicrobial peptides (AMPs), metal oxides, and herbal extracts are remarkably interesting alternative antimicrobial agents to overcome the crucial drawbacks of antibiotics such as the emergence of ARB strains and the difficulties to treat biofilm-forming bacterial infections (Table 4). Hereby, we discuss the effect of these agents on antimicrobial therapies when incorporated into collagen scaffolds.
3.2.1. Metal Oxide-Based Approaches
In recent years, there has been a great interest in metal oxide nanoparticles (NPs) to enhance the antimicrobial properties of collagen-based scaffolds due to their great inhibitory effects against broad-spectrum bacteria (Table 4). They can exert their bactericidal effect by linking to bacterial cell walls via electrostatic interactions [78], hydrophobic forces [79], van der Waals forces [80], and/or ligand binding [81]. Silver NPs are the well-known and most studied NPs in preclinical and commercial antimicrobial devices. In one study, silver NPs included collagen nanofibers presented an enhanced healing rate and led to the deposition of more hydroxyproline and collagen on the wound site in the Wistar rat model [82], whereas silver NPs loaded collagen hydrogels contributed to the reduction of pro-inflammatory cytokine IL-6 and inflammatory cytokines CCL24, TIMP1, and sTNFR-2, which indicates the exerted anti-inflammatory properties of silver NPs on the subcutaneous mice model [83]. Similarly, in vivo, 10 ppm silver NPs comprised collagen/chitosan hydrogel applied in full-thickness skin defects in the SD rat model expedited the fibroblast migration by the advance in α-SMA, upregulated the related macrophage activation, and downregulated inflammatory mediators [84]. However, the addition of silver NPs into the collagen scaffolds has not always exhibited a significant impact on wound healing. For example, both silver-loaded and pristine collagen membranes did not show complete wound closure [85], as silver NPs comprised collagen sponges [86]. Besides silver, zinc oxide NPs are also extensively studied in collagen biomaterials, owing to their well-recognized antibacterial and anti-inflammatory properties. For instance, the zinc oxide quantum dots were implicated in collagen/PCL nanofibrous mats for skin regeneration purposes and served as a suitable wound dressing. Both 0.75% (w/v) zinc oxide quantum dots included, pristine mats showed partial wound closure on full-thickness mice wound model at 12-day post-treatment with a wound closure rate of about 90%. Although scaffolds loaded with zinc oxide quantum dots presented a good inhibitory effect against S. aureus, their comparison with pristine scaffolds was not reported [87].
3.2.2. Antimicrobial Peptide-Based Approaches
Antimicrobial peptides are environmentally friendly, small molecular weight, amphiphilic, and polycationic proteins that are composed of less than fifty amino acids in their structure [88,89,90]. They can cause cell lysis via binding to intercellular targets of negatively charged cell membranes [91,92] and exert bactericidal activity by the modulation of the host immune system [93]. Despite their good antibacterial action, AMPs have some drawbacks, such as a short half-life (within hours) and high manufacturing costs [94]. Hence, in the literature, the incorporation of AMPs into collagen scaffolds has been less researched than the other therapeutic agents (Table 4). AMP Tet213 incorporated collagen-based sponge dressings demonstrated almost complete wound healing on E. coli- and S. aureus-infected wounds on SD rats within 14 days, similar to pristine sponges and commercial silver-including products, in contrast to gauze control. As a result of Sirius red staining, pristine, and Tet213, loaded dressings exhibited around 60% of collagen deposition, which might be contributed by the biocompatibility of collagen. Moreover, according to the samples taken from the SD rat model on day 4, E. coli was 1.8 × 107 CFU for gauze control, whereas no bacterial colonies were observed on wounds treated with Tet213 dressings [95]. In addition, it was observed that AMPs GL13K [96] and LL37 [97,98] incorporation into the collagen scaffolds increased their antibacterial activity against Gram-negative E. coli.
3.2.3. Herbal Extract-Based Approaches
Plants have been used for traditional remedies (e.g., bone defects and burn wounds) for centuries [99,100]. The bioactive phytochemicals of herbs, such as phenolic substances, essential oils, vitamins, and phytohormones, gain them tremendous features (e.g., antimicrobial, antifungal, anti-inflammatory, and antioxidant activity) and make them a rising star for antimicrobial therapies as greener and safer therapeutics [101,102,103,104,105,106]. Therefore, there have been a remarkable number of attempts in the literature to incorporate various herbal extracts, such as cinnamon [107], Cissus quadrangularis [108], and thymol [109], into collagen scaffolds to create an ideal and alternative antimicrobial biomaterial strategy for tissue regeneration purposes (Table 4). The addition of curcumin into collagen/cellulose nanocrystal sponge dressings advanced epithelization rate and dermal cell proliferation while providing complete wound closure on full-thickness burn wounds within 21 days. Moreover, they significantly decreased the level of cytokines IL-1β, IL-6, and TNF-α between the 10th and 21st days and inhibited the NF-κB activity due to the long and sustained release of curcumin with antibacterial, antioxidant, and anti-inflammatory characteristics [110]. Thanks to their complex chemical structure, in some studies, herbal extracts are used as a crosslinker for collagen formulations as well as an antimicrobial therapeutic agent. For example, wheatgrass was studied as both an antimicrobial agent and a green crosslinker for collagen aerogels. The study observed that 2% (w/v) of wheat grass incorporation increased the size reduction of collagen aerogel-treated wounds from 47% to 75% on the 9th post-treatment day and triggered the angiogenesis within 24 h of incubation of the chick embryo model [111]. The concentration of the loaded herbal extract is determined as an effective parameter from the perspective of preclinical studies. To illustrate, the addition of 0.08 g of Melilotus officinalis extract exhibited better re-epithelization than 0.04 and 0.02 g on day 18 post-treatment, whereas the 0.08 g extract with collagen-based multilayer nanofibrous mat increased the collagen density in vivo from 55% to 82% within 18 days [112].

Table 4.
Illustrative examples of collagen antimicrobial scaffolds designed with non-antibiotic-based approaches. Abbreviations: Antimicrobial susceptibility testing: AST; Weight: w; Volume: v; Collagen: Col; Chitosan: Chi; Nanoparticle: NP; Fibronectin: FN; Chondroitin 4-sulfate: CS; 1,4-Butanediol diglycidyl ether: BDDGE; Histidine: His; Hydroxy apatite: Hap; N-(3-dimethylaminopropyl)-N-ethylcarbodiimide hydrochloride: EDC; N-hydroxysuccinimide: NHS; Polycaprolactone: PCL; Glutaraldehyde: GTA; Titanium dioxide: TiO2; Antimicrobial peptide: AMP; Hyaluronic acid: HA; Poly(L-lactide-co-ε-caprolactone): PLC; Cellulose nanocrystal: CNC; Gelatin: Gel; Gulmohar seed polysaccharide: GSP; Poly(vinyl alcohol): PVA; Escherichia coli: E. coli; Staphylococcus epidermidis: S. epidermidis; Staphylococcus aureus: S. aureus; Pseudomonas aeruginosa: P. aeruginosa; Bacillus subtilis: B. subtilis; Bacillus cereus: B. cereus; Salmonella enterica: S. enterica; Pseudomonas putida: P. putida; Porphyromonas gingivalis: P. gingivalis; Fusobacterium nucleatum: F. nucleatum; Streptococcus gordonii: S. gordonii; Methicillin-resistant Staphylococcus aureus: MRSA; Spontaneously immortalized, human keratinocyte line: HaCaT; Human bone marrow-derived stromal cell culture: hBM-MSC; Human dermal fibroblast: HDF.
Table 4.
Illustrative examples of collagen antimicrobial scaffolds designed with non-antibiotic-based approaches. Abbreviations: Antimicrobial susceptibility testing: AST; Weight: w; Volume: v; Collagen: Col; Chitosan: Chi; Nanoparticle: NP; Fibronectin: FN; Chondroitin 4-sulfate: CS; 1,4-Butanediol diglycidyl ether: BDDGE; Histidine: His; Hydroxy apatite: Hap; N-(3-dimethylaminopropyl)-N-ethylcarbodiimide hydrochloride: EDC; N-hydroxysuccinimide: NHS; Polycaprolactone: PCL; Glutaraldehyde: GTA; Titanium dioxide: TiO2; Antimicrobial peptide: AMP; Hyaluronic acid: HA; Poly(L-lactide-co-ε-caprolactone): PLC; Cellulose nanocrystal: CNC; Gelatin: Gel; Gulmohar seed polysaccharide: GSP; Poly(vinyl alcohol): PVA; Escherichia coli: E. coli; Staphylococcus epidermidis: S. epidermidis; Staphylococcus aureus: S. aureus; Pseudomonas aeruginosa: P. aeruginosa; Bacillus subtilis: B. subtilis; Bacillus cereus: B. cereus; Salmonella enterica: S. enterica; Pseudomonas putida: P. putida; Porphyromonas gingivalis: P. gingivalis; Fusobacterium nucleatum: F. nucleatum; Streptococcus gordonii: S. gordonii; Methicillin-resistant Staphylococcus aureus: MRSA; Spontaneously immortalized, human keratinocyte line: HaCaT; Human bone marrow-derived stromal cell culture: hBM-MSC; Human dermal fibroblast: HDF.
| Composition | Collagen Source | Scaffold Form | Crosslinking | Therapeutic Agent | Release Profile | AST | Bacterial Strain/ Cell Line | Antibacterial Activity | Hypothetic Material | Refs. |
|---|---|---|---|---|---|---|---|---|---|---|
| Metal oxide-based approaches | ||||||||||
| Col Chi (Various Col/Chi w% ratio) | Goat tendon | Thin film | EDC/NHS (2:1 M ratio) | Silver NPs (0.5 w%) | Not studied | Growth inhibition | E. coli, S. aureus MG-63 osteosarcoma cells | Up to 37% and 27% of growth inhibition was observed against E. coli and S. aureus, respectively. | Composite bone tissue engineering scaffold | [113] |
| Col FN CS (10:1:3 × 10−5 g/g Col/CS/FN) | Bovine tendon | Sponge | GTA (2.5% v/v) | Silver NPs (1 × 10−4 g/g polymers) | Not studied | Disc diffusion | F.nucleatum, P. gingivalis Gingival fibroblasts | Hybrid sponges showed slightly higher antimicrobial activity against F. nucleatum. | Oral cavity lesion dressing | [114] |
| Col (8% w/v) | Fish collagen | Nanofibrous mat | GTA (50% w/v) | Silver NPs (0.2% w/v) | Cumulatively, almost 100% of silver ions were released within 25 h. | Microdilution, disc diffusion | S. aureus, P. aeruginosa No in vitro cell culture | Approximately 3.2 and 2.3 cm of inhibition zone diameter was observed after 48 h against S. aureus and P. aeruginosa, respectively. | Wound dressing | [82] |
| Col (10% w/w) | Porcine | Hydrogel | BDDGE | Silver NPs (0.2 µM) | Steady silver concentration was reached within 0.5 h of incubation | Growth inhibition and Time-kill assays | S. aureus, S. epidermidis, E. coli, P. aeruginosa Human epidermal keratinocytes, and dermal fibroblasts | Hybrid hydrogels could inhibit the growth of all tested bacteria. | Implantable anti-infective hybrid biomaterial | [83] |
| Col (5% w/w) His (0, 1, 2% w/w) | Porcine | Membrane | EDC/NHS (3.55 and 2.13 mg/g) | Silver NPs | Not studied | Disc diffusion, bacterial suspension | P. aeruginosa, S. aureus L929 fibroblasts | Developed membranes did not show sufficient antimicrobial activity against both tested strains. | Dressing for full-thickness burn wounds | [85] |
| Col Chi (9:1 Col/Chi w ratio) | Bovine tendon | Hydrogel | EDC/NHS | Silver NPs (0, 2, 5, 10, 20 ppm) | Not studied | Disc diffusion | E. coli, S. aureus Mouse embryo fibroblasts, HaCaTs | Developed wound dressings showed higher inhibition of S. aureus growth. | Wound dressing | [84] |
| Col Hap (various w ratio) | Fish scale | Membrane | Genipin (0.003 g) | Silver NPs (0.05 w%) | Not studied | Disc diffusion | E. coli, S. aureus MG-63 osteosarcoma cells | Scaffolds presented less inhibition zone compared to standard ampicillin discs. | Bone filler | [115] |
| Col (0.5% w/w) | Bovine tendon | Sponge | Dialdehyde xanthan gum (10 mg/mL) | Silver NPs (10 mg/mL) | Not studied | Disc diffusion, bacterial infiltration | E. coli, S. aureus, P. aeruginosa L929 fibroblasts | An increase in silver NP concentration resulted in an increased inhibition rate against tested strains. | Antibacterial wound dressing | [86] |
| Col Sago starch (1, 2, 3 µM) | Fish scale | Sponge | Not available | Sago starch capped silver NPs (1:1 w ratio to Col) | Not studied | Broth dilution | S. aureus, E. coli NIH-3T3 fibroblasts | A lower minimum inhibitory concentration was examined against E. coli. | Scaffold for tissue regeneration applications | [116] |
| Col (1% w/w) Dextran | Calf hide | Hydrogel | GTA (0.25% v/v) | Zinc oxide NPs | Not studied | Not studied | No in vitro cell culture | Not studied | Wound dressing | [117] |
| Col (0.7 w%) | Bovine | Hydrogel | GTA (1% v/v) | Zinc oxide NPs (2, 3, 5 w%) | Not studied | Disc diffusion | S. aureus, E. coli No in vitro cell culture | The inhibition zone diameter decreased with increasing zinc oxide concentration against S. aureus. | Wound dressing | [118] |
| Col PCL (1:2, 1:1, 2:1, 3:1 Col/PCL w ratio) | Type I (not specified) | Nanofibrous mat | Not available | Zinc oxide quantum dots (0–0.75% w/v) | Not studied | Plate counting | E. coli, S. aureus L929 fibroblasts, 3T3 fibroblasts | The number of living bacteria was significantly reduced by the addition of 0.75% of NPs. | Antibacterial wound dressing | [87] |
| Col (1% w/w) | Calf hide | Sponge | GTA (0.5 w%) | Zinc titanate | Not studied | Disc diffusion | S. epidermidis, B. cereus, E. coli, S. enterica, P. putida MG-63 osteosarcoma cells, 3T3 fibroblasts HaCaTs | The porous nanocomposites exerted higher antimicrobial activity against S. epidermidis. | Anti-infection biomaterial | [119] |
| Col (5 mg/mL) Chi (5 mg/mL) | Pig skin | Sponge | GTA (2.5% w/w) | TiO2 NPs (1–7%) | Not studied | Bacterial culture, SEM imaging | S. aureus Mouse fibroblasts, red blood cells | Increased TiO2 amount led to reduced S. aureus colonies on the surface of the scaffold. | Wound dressing | [120] |
| Col (3.47 w%) Chi (3 w%) | Bovine | Nanofibrous mat | GTA (1 w%) | Zinc oxide NPs (1:1:1 w ratio Col:Chi:Zinc oxide) | Not studied | Disc diffusion | S. aureus Hep-2 cells | Membranes showed 4–8 mm of inhibition zone diameter against S. aureus. | Scaffold for skin tissue regeneration | [121] |
| Col Chi (1:9 Col/Chi w ratio) | Not specified | Sponge | Dehydrothermal crosslink at 105 °C for 24 h | Zinc oxide NPs (1, 3, 5 w%) | Not studied | Disc diffusion | E. coli, S. aureus No in vitro cell culture | S. aureus was found more sensitive to developed scaffolds than E. coli. | Antibacterial product | [122] |
| Antimicrobial peptide-based approaches | ||||||||||
| Col (3 mg/mL) | Bovine | Hydrogel | EDC/NHS (50 mM EDC, 25 mM NHS) | AMP GL13K (1 mM) | Burst release was observed from 21 to 28 days. | ATP bioluminescence, live/dead assays | S. gordonii, E. coli hBM-MSCs | AMP GL13K coating significantly demonstrated less effects on the membrane integrity of S. gordonii. | Scaffold for bone/dental tissue growth and infection prevention | [96] |
| Col (0.6% w/v) HA (0.5% w/v) Alginate (1.2% w/v) | Type I (not specified | Sponge | EDC/NHS (0.6 mg/mL EDC, 0.3 mg/mL NHS) | AMP Tet213 (500 µg/mL) | Sustained release (68.4 ± 10.2%) was observed after 14 days. | Zone inhibition, colony counting | E. coli, MRSA, S. aureus NIH-3T3 fibroblasts | The addition of AMP Tet213 into hybrid scaffolds gave rise to almost full inhibition of E. coli and S. aureus. | Mixed-bacteria-infected wound dressing | [95] |
| Col (2.5–3 mg/mL) HA (1.5 mg/mL) | Rat tail tendon | Polyelectrolyte multilayers | GTA (8% w/v) | AMP LL37 (2, 8, 16 µM) | Sustained release of the AMP killed planktonic bacteria. | Broth dilution, bacterial adhesion test, live/dead assay | E. coli Primary rat hepatocytes | The incorporation of 16 µM of AMP LL37 showed almost 3% of live bacteria on the scaffold surface. | Antimicrobial coating | [97] |
| Col PLC (14% w/v) | Not specified | Membrane (ready-to-use product) | Not available | AMP LL37 (10–40 µM) | Membranes containing different LL-37 concentrations released LL-37 in the same quantity. | Not studied | L929 fibroblasts | Not studied | Collagen membrane for guided bone regeneration | [98] |
| Herbal extract-based approaches | ||||||||||
| Col (2% w/v) | Bovine skin | Membrane | Not available | Propolis NPs (200 µg/mL) | Not studied | Not studied | HDFs | Not studied | Dermal patch | [123] |
| Col CNC (7 w%) | Bovine tendon | Sponge | Not available | Curcumin (5 mg/mL) | 99.3% of curcumin was released within the first 24 h. | Disc diffusion | E. coli, S. aureus, P. aeruginosa No in vitro cell culture | Curcumin significantly enhanced the antimicrobial activity of pristine porous scaffolds. | Full-thickness burn dressing | [110] |
| Col (1% w/w) Col/Gel microparticles (50, 125, 250 mg) | Bovine | Sponge | GTA (0.02% v/v) | Calendula officinalis extract (1% v/v) | Incomplete release of the extract was observed within 14 days at pH 5.5 and 7.4. | Not studied | L929 fibroblasts | Not studied | Dermal substitute | [124] |
| Col | Goat tendon | Aerogel | Wheatgrass (1, 2, 3% w/v) | Wheatgrass (1, 2, 3% w/v) | Not studied | Agar diffusion | E. coli, B. subtilis Swiss 3T6 fibroblasts, HaCaTs | Hybrid aerogels showed smaller inhibition zones than commercial ampicillin discs against B. subtilis. | Wound dressing | [111] |
| Col (10 mg/mL) GSP (25–100 w% to Col) | Cowhide trimming waste | Sponge | Chloroform extract of cinnamon bark (14.28% v/v) | Cinnamon bark powder (2 g) | Not studied | Broth dilution | B. subtilis, S. aureus, E. coli No in vitro cell culture | The addition of cinnamon bark powder led to great inhibition of all tested strains. | Antimicrobial wound dressing | [107] |
| Col (9 mg/mL) | Type I (Not specified) | Sponge | Not available | Berberine-oleanolic acid (1–5%) | All samples released about 70% of the drug within 1 h. | Filter paper diffusion | S. aureus, E. coli MG-63 osteosarcoma cells | Gram-positive bacteria were found more sensitive to developed scaffolds than Gram-negative bacteria. | Scaffold for postoperative bacterial bone infection | [125] |
| Col (1% w/v) Chi (1% w/v) Hap (5% w/v) PCL (20–80 mg/mL) PVA (0.5–3% w/v) | Bovine tendon | Sponge | GTA (0.1% v/v) | Cissus quadrangularis caged PCL nanoparticles | Cumulatively more than 80% of the extract was released within 21 days. | Not studied | MC3T3-E1 osteoblasts | Not studied | Bone tissue engineering scaffold | [108] |
| Col (1% w/v) | Rat tail tendon | Film | Not available | Thymol (0.25–4 mg/cm2) | Not studied | Dehydrogenase activity assay, ATP bioluminescence, microbial penetration assay | S. aureus, E. coli, P. aeruginosa Red blood cells | 4 mg/cm2 of thymol including films indicated almost full inhibition of all tested strains. | Antibacterial film for wound care applications | [109] |
| Col (11 w% middle layers; 10 w% inner layers) PCL (10 w% outer layers; 11 w% middle layer) | Rat tail | Nanofibrous mat | Not available | Melilotus officinalis (2, 4, 8% w/w) | Not studied | Not studied | L929 fibroblasts | Not studied | Diabetic foot ulcer dressing | [112] |
| Col Lipid NPs (10:1 w ratio Col/Lipid NPs) | Bovine tendon | Sponge | Not available | Curcumin into lipid NPs | The complete release of curcumin-loaded NPs was observed within 25 days. | Not studied | NIH 3T3 fibroblasts, HaCaTs | Not studied | Composite cryostructurate for wound healing | [126] |
| Col (10 mg/mL) Annona polysaccharide (7.5 mg/mL) | Bovine Achilles tendon | Sponge | Chloroform extract of cinnamon bark | Tetrahydrocurcumin microspheres | 28.95 ± 1.7% of the drug was released within 12 h from the composite scaffold. | Disc diffusion | B. subtilis, P. aeruginosa, S. aureus NIH 3T3 fibroblasts | Approximately 20 mm and 10 mm inhibition zone diameters were evaluated against S. aureus around the positive control and composite scaffold, respectively. | Antimicrobial wound dressing | [127] |
| Col (60% v/v in shell) PVA (50% v/v in core) | Type I (Not specified) | Nanofibrous core–shell mat | Not available | Licorice roots (50% v/v in core, and 40% v/v in shell) | Not studied | Disc diffusion | S. aureus, P. aeruginosa No in vitro cell culture | Bio-nano scaffolds did not show any activity on the inhibition of P. aeruginosa growth. | Hybrid bio-nano wound dressing | [128] |
4. Combination Approaches
The combination of antimicrobial bioactive agents has been studied to increase the treatment efficacy of collagen-based antimicrobial biomaterial therapies in addition to their single use by taking advantage of synergetic effects of different therapeutics. For this purpose, the simultaneous incorporation of herbal extracts, metal oxides, AMPs, antibiotics, growth factors, and other bioactive molecules into antimicrobial collagen scaffolds has been extensively investigated (Table 5). For example, the synergism of 60 mg/mL of lemon balm and dill essential oils enhanced the antimicrobial activity of collagen-based nanofibers on various Gram-positive and Gram-negative bacterial strains and showed in vivo biocompatibility on Swiss adult mouse model without any causative effect [103]. In the literature, the combination of metal oxide NPs and phytochemicals in biomaterial formulation exhibited advanced tissue regeneration and antimicrobial activity. In a study, the administration of silver NPs and silymarin raised the contraction rate of collagen/chitosan bilayer sponges treated wounds on Wistar rats from 55% to almost complete contraction within 10 days with a thin crust appearance [129]. Similarly, 0.5 w% curcumin-loaded graphene oxide NP (2 mg/mL)-reinforced sponge dressings accelerated the wound closure of the open wounds in vivo due to the superior anti-inflammatory and antibacterial features of curcumin and graphene oxide [130], while the cumulative effect of silver NPs and plumbagin led to complete healing of open excision wounds on Wistar rats on the 15th post-treatment day as well as a significant bactericidal effect on both Gram-positive and Gram-negative bacteria [131].
In some cases, the application of antibiotics could not prevent the re-growing of antibiotic-resistant bacterial strains. Although vancomycin-loaded collagen hydrogels were effective in reducing bacterial luminescence on luminescent MRSA, which infected in vivo wounds on the first day, re-growing of bacteria was reported on the 2nd post-treatment day. To overcome this problem, collagen-mimetic-peptide-tethered vancomycin was chosen, and complete inhibition of bacterial growth was achieved by their synergetic effect [132]. Apart from this, the combination of antibiotics with growth factors may ameliorate the rate of wound healing. Silver sulfadiazine, and epidermal and basic fibroblast growth factors, including collagen-based multi-layered nanofibers, presented ideal healing for in vivo full-thickness wounds thanks to the slow release of growth factors, neutralizing and anti-growth impact of antibiotics, which supported granulation tissue formation as well normal interactions of collagen fibers and fibroblasts with ECM [133].

Table 5.
Illustrative examples of collagen antimicrobial scaffolds designed with combination approaches. Abbreviations: Antimicrobial susceptibility testing: AST; Weight: w; Volume: v; Collagen: Col; Chitosan: Chi; Essential oil: EO; poly(D,L-lactide-co-glycolic acid): PLGA; Polycaprolactone: PCL; Antimicrobial peptide: AMP; Nanoparticle: NP; Ammonia: NH3; Graphene oxide: GO; Hydroxy apatite: Hap; Elastin-like peptide: ELP; Epidermal growth factor: EGF; Basic fibroblast growth factor: bFGF; Oxytetracycline hydrochloride: OTC; Doxycycline hydrochloride: DXC; Ciprofloxacin: CP; Tobramycin: TB; N-(3-dimethylaminopropyl)-N-ethylcarbodiimide hydrochloride: EDC; N-hydroxysuccinimide: NHS; Glutaraldehyde: GTA; Escherichia coli: E. coli; Staphylococcus aureus: S. aureus; Enterococcus faecalis: E. faecalis; Salmonella typhimurium: S. typhimurium; Methicillin-resistant Staphylococcus aureus: MRSA; Pseudomonas aeruginosa: P. aeruginosa; Bacillus subtilis: B. subtilis; Proteus vulgaris: P. vulgaris; Streptococcus sanguinis: S. sanguinis; Spontaneously immortalized human keratinocyte line: HaCaT; Recombinant human bone morphogenetic protein-2: rhBMP-2; Human adipose-derived stem cell: hASC; Human dermal fibroblast: HDF.
Table 5.
Illustrative examples of collagen antimicrobial scaffolds designed with combination approaches. Abbreviations: Antimicrobial susceptibility testing: AST; Weight: w; Volume: v; Collagen: Col; Chitosan: Chi; Essential oil: EO; poly(D,L-lactide-co-glycolic acid): PLGA; Polycaprolactone: PCL; Antimicrobial peptide: AMP; Nanoparticle: NP; Ammonia: NH3; Graphene oxide: GO; Hydroxy apatite: Hap; Elastin-like peptide: ELP; Epidermal growth factor: EGF; Basic fibroblast growth factor: bFGF; Oxytetracycline hydrochloride: OTC; Doxycycline hydrochloride: DXC; Ciprofloxacin: CP; Tobramycin: TB; N-(3-dimethylaminopropyl)-N-ethylcarbodiimide hydrochloride: EDC; N-hydroxysuccinimide: NHS; Glutaraldehyde: GTA; Escherichia coli: E. coli; Staphylococcus aureus: S. aureus; Enterococcus faecalis: E. faecalis; Salmonella typhimurium: S. typhimurium; Methicillin-resistant Staphylococcus aureus: MRSA; Pseudomonas aeruginosa: P. aeruginosa; Bacillus subtilis: B. subtilis; Proteus vulgaris: P. vulgaris; Streptococcus sanguinis: S. sanguinis; Spontaneously immortalized human keratinocyte line: HaCaT; Recombinant human bone morphogenetic protein-2: rhBMP-2; Human adipose-derived stem cell: hASC; Human dermal fibroblast: HDF.
| Composition | Collagen Source | Scaffold Form | Crosslinking | Therapeutic Agent | Release Profile | AST | Bacterial Strain/ Cell Line | Antibacterial Activity | Hypothetic Material | Refs. |
|---|---|---|---|---|---|---|---|---|---|---|
| Col hydrolysate (2.66% w/v) Chi (1.5% w/v) | Bovine tendon Rabbit skin | Nanofibrous mat | Not available | Lemon balm and Dill EOs (60 mg/mL each, 1:1 ratio) | Not studied | Disc diffusion | S. aureus, E. coli, E. faecalis, S. typhimurium No in vitro cell culture | While EOs only did not show efficient antimicrobial activity, EO-including membranes, showed significantly higher activity against tested strains. | Medical wound dressing | [103] |
| Col (5% w/v) | Not specified | Sponge | GTA (2.5% v/v) | AMPs Pac-525 and KSL-W (1.5 mg/mL) into PLGA microspheres | Burst release of AMPs occurred within 2 days in both microspheres and scaffolds. | Oxford cup disc diffusion | S. aureus, E. coli MC-3T3 fibroblasts | Lower doses of AMPs could not lead to inhibition of S. aureus and E. coli growth. | Scaffold for infective bone defect repair | [134] |
| Col (3.5% w/v) Chi (1.5% w/v) | Hydrolyzed peptide | Bilayer sponge | GTA (0.025% v/v) | Silymarin (0.5, 1, 2% w/w), and silver NPs (3% w/w) | A sustained release of antioxidants was observed over 120 h. | Not studied | Cos-7 fibroblasts | Not studied | Antioxidant and antibacterial wound dressing | [129] |
| Col | Rat tail tendon | Hydrogel | Incubation of Col solution in saturated NH3 chamber | Silver NPs (67, 6.7, 0.67 mg/g), and Cannabis sativa oil (0.15 mL) | Only 1.5 g of the silver content is released after 24 h. | Disc diffusion, broth dilution | S. aureus, P. aeruginosa MDCK epithelial cells | Inhibition zone diameter of 67 mg/g silver-NP-including hydrogels increased from 1.45 to 1.75 cm with the addition of EO. | Wound dressing | [135] |
| Col (1% w/v) | Fish scale | Sponge | EDC/NHS (1:2:2 GO:EDC:NHS molar ratio) | Curcumin (0.5 w%), and GO NPs (2 mg/mL) | 82.5% of loaded curcumin was released within 96 h. | Disc diffusion | P. aeruginosa, S. aureus NIH-3T3 fibroblasts | The inhibition zone diameters around hybrid scaffolds were evaluated as approximately 16 and 15 mm against S. aureus, and P. aeruginosa, respectively. | Wound dressing | [130] |
| Col | Rat tail tendon | Membrane | Curcumin caged silver NPs (10, 20 µM) | Curcumin (20–100 µM) caged silver NPs | Not studied | Broth dilution | E. coli, B. subtilis HaCaTs | 20 µM curcumin-caged silver NPs showed 95% growth inhibition of E. coli. | Scaffold for biomedical engineering | [136] |
| Col (3 mg/mL) | Rat tail tendon | Sponge | Plumbagin (1–5 µM) | Plumbagin (1–5 µM) caged silver NPs | Not studied | Disc diffusion, broth microdilution | E. coli B. subtilis No in vitro cell culture | Hybrid scaffolds presented better antimicrobial activity against B. subtilis. | Wound dressing | [131] |
| Col (8 w%) Hap (0, 5, 15 w%) | Type I (Not specified) | Nanofibrous mat | EDC/NHS (4:1 w ratio EDC:NHS) | Vancomycin hydrochloride, gentamicin sulfate (10 w% total, 1:1 w ratio) | High concentrations of vancomycin and gentamicin were released for 21 days. | Disc diffusion | MRSA, S. epidermidis, E. faecalis SAOS-2 osteosarcoma cells | The synergetic effect of two antibiotics yielded increased inhibition zone diameters on MRSA. | Scaffold for the treatment of prosthetic joint infection | [137] |
| Col (2, 3, 4 mg/mL) Fibrinogen (1.25 mg/mL) Thrombin (0.156 IU/mL) | Bovine | Hydrogel | Not available | Collagen mimetic peptide tethered vancomycin (1.25 mg/gel) into liposomes (30 µg/gel) | Complete vancomycin release was achieved within 12 h. | Broth dilution | S. aureus, MRSA NIH-3T3 fibroblasts | Hybrid hydrogels presented higher antimicrobial activity than pristine hydrogels with less than 104 CFU/wound up to the 9th day. | Scaffold for the MRSA-associated treatment | [132] |
| Col (1% w/v) | Fish scale | Sponge | GTA (0.25% v/v) | Mupirocin (1:1 w ratio) and Macrotyloma uniflorum extract (10% v/v) | 94% of mupirocin was released within 72 h. | Disc diffusion | B. subtilis, S. aureus, P. vulgaris, E. coli NIH-3T3 fibroblasts, HaCaTs | The highest antimicrobial activity of composite dressings was observed on S. aureus. | Burn wound dressing | [138] |
| Col (20 w%) PCL Zein (15 w% PCL/Zein with various ratios) | Fish | Nanofibrous mat | Not available | Zinc oxide NPs (1 w%) and Aloe vera (5, 8 w%) | Approximately 70% of zinc oxide NPs released within 30 days. | Disc diffusion | S. aureus, E. coli Human gingival fibroblasts | The combination of zinc oxide NPs with Aloe vera increased the growth inhibition rate of both bacteria. | Wound dressing | [139] |
| Col (0.5% w/v) | Rat tail | Bilayer sponge | GTA (25% v/v) | Fibrinogen and silver NPs | 50% of the included fibrinogen was released within 5 days. | Zone inhibition | E. coli No in vitro cell culture | The one-fold increase in silver NPs concentration did not enhance the antimicrobial activity of scaffolds significantly. | Skin tissue engineering scaffold | [140] |
| Col (6 mg/mL) Elastin-like peptide (18 mg/mL) (1:3 Col/ELP) | Rat tail tendon | Hydrogel | EDC/NHS | rhBMP-2 (0.005% w/v) doxycycline hyclate (0.5% w/w) | Bi-phasic release of doxycycline was observed with an initial burst release followed by a sustained release. | Zone inhibition | E. coli, P. aeruginosa, S. sanguinis hASCs | The developed hydrogels could not exert effective activity against E. coli. | Bone regenerative hydrogel | [141] |
| Col (2 w%) PCL (15 w%) Chi (2 w%) PEO (5 w%) | Type I (not specified) | 3-layered nanofibrous mat | Not available | Silver sulfadiazine (3 mg/mL), EGF, and bFGF (25 µg/mL each) | Between days 5 and 20, the sustained release was achieved with a cumulative release of about 80%. | Antibiotic tube dilution | P. aeruginosa, S. aureus HDFs | Minimum inhibitory concentration was evaluated as 15 and 30 µg/mL against P. aeruginosa and S. aureus, respectively. | Wound dressing | [133] |
| Col (1% w/v) | Bovine skin | Sponge | GTA (0–1% w/v) | OTC (1 g/L) DXC (1 g/L) | About 70% of OTC was released from 0.5% of GTA crosslinked scaffolds within 600 min. | Broth dilution | E. coli, E. faecalis, S. aureus Dermal fibroblasts of mouse cell line | Oxytetracycline led to more inhibition growth of tested bacteria. | Dressing for prevention and treatment of infections at the application site | [142] |
| Col PVA (1:3 w/w PVA/Col) | Bovine tendon | Membrane | Not available | Ciprofloxacin and tobramycin (0.3% w/v for soaking method, 5% w/w for mixing method) | CP showed more sustained and controlled release. 95% of CP was released after 48 h. | Microdilution, time-kill assay | S. aureus, E. coli No in vitro cell culture | The efficacy of membranes to kill the tested bacteria was found independent of their release profile. | Ulcerative keratitis dressing | [143] |
| Col (4 mg/mL) | Not specified | Sponge | Triphenyl phosphate (10% v/v) | Mupirocin (50 mg) in 5% w/v Chi microspheres and Piper betle extract (5% v/v) | More than 50% of both drugs are released at the end of 12 h. | Agar disc diffusion | E. coli, S. aureus No in vitro cell culture | The combination of two antimicrobials slightly increased the antimicrobial activity against both strains. | Wound dressing | [144] |
| Col (1.06 mg/mL) | Rapana venosa | Sponge | Not available | Salvia officinalis extract loaded mesoporous silica NPs (10, 20 mg/mL) | Not studied | Broth microdilution | P. aeruginosa, S. aureus HaCaTs, Human Mel-Juso skin carcinoma cells | The hybrid scaffolds showed at least a two-fold higher minimum inhibitory concentration for P. aeruginosa. | Wound dressing | [145] |
5. Conclusions
The development of antimicrobial therapeutic strategies has an incremental interest in the literature since microbial infections have threatened human health for many years. Biomaterial-based antimicrobial therapies have been considered an alternative and ideal solution for infection treatment because the incorporation of therapeutic bioactive agents into the biomaterial formulation can lead to their controlled and sustained release as well as a decrease in their off-target influences. Moreover, the combination of biomaterials with these molecules’ benefits enhancement in bioactivity and stability of therapeutics; hence, therapeutic efficacy could be improved. Collagen is a prominent polymer for the designing of antimicrobial scaffolds due to its outstanding biocompatibility, biodegradability, hydrophilicity, remarkable cell-attachment affinity, and mechanical, hemostatic, low-antigenic, and non-cytotoxic properties. This review clearly studies the recent developments in different collagen-based approaches in the treatment of microbial infections using various kinds of bioactive molecules incorporated into collagen-based scaffolds for antimicrobial therapies. It is believed that effective treatment strategies can be developed in the future by discovering alternative and non-toxic, nature-inspired therapeutics and by increasing the functionality of biomaterials with more effective and less toxic crosslinking agents.
Author Contributions
Conceptualization: C.E. and D.I.Z.; Resources: C.E. and C.V.; Literature review and writing—original draft preparation: C.E.; Writing—review and editing: C.E., I.S., C.V., A.T. and D.I.Z.; Supervision: I.S., A.T. and D.I.Z.; Project administration: I.S. and D.I.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research has been funded by the European Union, EuroNanoMed3, project nAngioDerm, through the Greek General Secretariat for Research and Innovation ERA-NETS (code number T9EPA3-00022).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Vera, D.M.A.; Haynes, M.H.; Ball, A.R.; Dai, T.; Astrakas, C.; Kelso, M.J.; Hamblin, M.R.; Tegos, G.P. Strategies to potentiate antimicrobial photoinactivation by overcoming resistant phenotypes. Photochem. Photobiol. 2012, 88, 499–511. [Google Scholar] [CrossRef]
- Cai, J.; Liu, R. Introduction to Antibacterial Biomaterials. Biomater. Sci. 2020, 8, 6812–6813. [Google Scholar] [CrossRef] [PubMed]
- Voidarou, C.; Bezirtzoglou, E.; Alexopoulos, A.; Plessas, S.; Stefanis, C.; Papadopoulos, I.; Vavias, S.; Stavropoulou, E.; Fotou, K.; Tzora, A. Occurrence of Clostridium perfringens from different cultivated soils. Anaerobe 2011, 17, 320–324. [Google Scholar] [CrossRef]
- Tan, S.Y.; Tatsumura, Y. Alexander Fleming (1881–1955): Discoverer of penicillin. Singap. Med. J. 2015, 56, 366. [Google Scholar] [CrossRef] [PubMed]
- Nelli, A.; Voidarou, C.; Venardou, B.; Fotou, K.; Tsinas, A.; Bonos, E.; Fthenakis, G.C.; Skoufos, I.; Tzora, A. Antimicrobial and Methicillin Resistance Pattern of Potential Mastitis-Inducing Staphylococcus aureus and Coagulase-Negative Staphylococci Isolates from the Mammary Secretion of Dairy Goats. Biology 2022, 11, 1591. [Google Scholar] [CrossRef] [PubMed]
- Organisation for Economic Cooperation and Development; European Union. Health at a Glance: Europe 2018: State of Health in the EU Cycle; OECD Publishing, Paris/European Union: Brussels, Belgium, 2018. [Google Scholar]
- Suetens, C.; Latour, K.; Kärki, T.; Ricchizzi, E.; Kinross, P.; Moro, M.L.; Jans, B.; Hopkins, S.; Hansen, S.; Lyytikäinen, O. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: Results from two European point prevalence surveys, 2016 to 2017. Eurosurveillance 2018, 23, 1800516. [Google Scholar] [CrossRef]
- Cassini, A.; Plachouras, D.; Eckmanns, T.; Abu Sin, M.; Blank, H.-P.; Ducomble, T.; Haller, S.; Harder, T.; Klingeberg, A.; Sixtensson, M. Burden of six healthcare-associated infections on European population health: Estimating incidence-based disability-adjusted life years through a population prevalence-based modelling study. PLoS Med. 2016, 13, e1002150. [Google Scholar] [CrossRef]
- U.S. Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United State; Department of Health and Human Services, CDC: Atlanta, GA, USA, 2019. [Google Scholar]
- Organisation for Economic Cooperation and Development; European Union. Tackling Wasteful Spending on Health; OECD Publishing: Paris, France, 2017. [Google Scholar]
- Prestinaci, F.; Pezzotti, P.; Pantosti, A. Antimicrobial resistance: A global multifaceted phenomenon. Pathog. Glob. Health 2015, 109, 309–318. [Google Scholar] [CrossRef]
- Dadgostar, P. Antimicrobial resistance: Implications and costs. Infect. Drug Resist. 2019, 12, 3903. [Google Scholar] [CrossRef]
- Murugaiyan, J.; Kumar, P.A.; Rao, G.S.; Iskandar, K.; Hawser, S.; Hays, J.P.; Mohsen, Y.; Adukkadukkam, S.; Awuah, W.A.; Jose, R.A.M. Progress in alternative strategies to combat antimicrobial resistance: Focus on antibiotics. Antibiotics 2022, 11, 200. [Google Scholar] [CrossRef]
- Majumder, M.A.A.; Rahman, S.; Cohall, D.; Bharatha, A.; Singh, K.; Haque, M.; Gittens-St Hilaire, M. Antimicrobial stewardship: Fighting antimicrobial resistance and protecting global public health. Infect. Drug Resist. 2020, 13, 4713–4738. [Google Scholar] [CrossRef] [PubMed]
- Tarín-Pelló, A.; Suay-García, B.; Pérez-Gracia, M.-T. Antibiotic resistant bacteria: Current situation and treatment options to accelerate the development of a new antimicrobial arsenal. Expert Rev. Anti-Infect. Ther. 2022, 20, 1095–1108. [Google Scholar] [CrossRef]
- Ricard-Blum, S. The collagen family. Cold Spring Harb. Perspect. Biol. 2011, 3, a004978. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.M.; Gentile, P.; Chiono, V.; Ciardelli, G. Collagen for bone tissue regeneration. Acta Biomater. 2012, 8, 3191–3200. [Google Scholar] [CrossRef]
- Stark, Y.; Suck, K.; Kasper, C.; Wieland, M.; van Griensven, M.; Scheper, T. Application of collagen matrices for cartilage tissue engineering. Exp. Toxicol. Pathol. 2006, 57, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Young, B.; Ezura, Y.; Favata, M.; Soslowsky, L.; Chakravarti, S.; Birk, D.E. Development of tendon structure and function: Regulation of collagen fibrillogenesis. J. Musculoskelet Neuronal Interact. 2005, 5, 5–21. [Google Scholar]
- Priya, S.G.; Jungvid, H.; Kumar, A. Skin tissue engineering for tissue repair and regeneration. Tissue Eng. Part B Rev. 2008, 14, 105–118. [Google Scholar] [CrossRef] [PubMed]
- Kalic, T.; Kamath, S.D.; Ruethers, T.; Taki, A.C.; Nugraha, R.; Le, T.T.; Humeniuk, P.; Williamson, N.A.; Hira, D.; Rolland, J.M. Collagen—An important fish allergen for improved diagnosis. J. Allergy Clin. Immunol. Pract. 2020, 8, 3084–3092.e3010. [Google Scholar] [CrossRef] [PubMed]
- Sorushanova, A.; Delgado, L.M.; Wu, Z.; Shologu, N.; Kshirsagar, A.; Raghunath, R.; Mullen, A.M.; Bayon, Y.; Pandit, A.; Raghunath, M.; et al. The collagen suprafamily: From biosynthesis to advanced biomaterial development. Adv. Mater. 2019, 31, 1801651. [Google Scholar] [CrossRef]
- Rezvani Ghomi, E.; Nourbakhsh, N.; Akbari Kenari, M.; Zare, M.; Ramakrishna, S. Collagen-based biomaterials for biomedical applications. J. Biomed. Mater. Res. 2021, 109, 1986–1999. [Google Scholar] [CrossRef]
- David, G. Collagen-based 3D structures—Versatile, efficient materials for biomedical applications. In Biopolymer-Based Formulations, 1st ed.; Elsevier: Amsterdam, The Netharlands, 2020; pp. 881–906. [Google Scholar]
- Lee, C.H.; Singla, A.; Lee, Y. Biomedical applications of collagen. Int. J. Pharm. 2001, 221, 1–22. [Google Scholar] [CrossRef]
- Sundar, G.; Joseph, J.; John, A.; Abraham, A. Natural collagen bioscaffolds for skin tissue engineering strategies in burns: A critical review. Int. J. Polym. Mater. 2021, 70, 593–604. [Google Scholar] [CrossRef]
- Singh, O.; Gupta, S.S.; Soni, M.; Moses, S.; Shukla, S.; Mathur, R.K. Collagen dressing versus conventional dressings in burn and chronic wounds: A retrospective study. J. Cutan. Aesthetic Surg. 2011, 4, 12. [Google Scholar] [CrossRef] [PubMed]
- Avila Rodríguez, M.I.; Rodríguez Barroso, L.G.; Sánchez, M.L. Collagen: A review on its sources and potential cosmetic applications. J. Cosmet. Dermatol. 2018, 17, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Ge, X. Antimicrobial biomaterials with non-antibiotic strategy. Biosurf. Biotribol. 2019, 5, 71–82. [Google Scholar] [CrossRef]
- Li, S.; Dong, S.; Xu, W.; Tu, S.; Yan, L.; Zhao, C.; Ding, J.; Chen, X. Antibacterial hydrogels. Adv. Sci. 2018, 5, 1700527. [Google Scholar] [CrossRef]
- 3M™ Promogran Prisma™ Matrix. Available online: https://www.3m.com/3M/en_US/p/d/b5005265080/ (accessed on 13 February 2023).
- ColActive® Plus Powder Ag. Available online: https://www.woundsource.com/product/colactive-plus-powder-ag (accessed on 13 February 2023).
- Septocoll® E—Biomet. Available online: https://www.yumpu.com/en/document/view/42479805/septocollar-e-biomet (accessed on 13 February 2023).
- DermaCol™ Collagen Matrix Dressing. Available online: https://dermarite.com/product/dermacol/ (accessed on 13 February 2023).
- DermaCol/Ag™ Collagen Matrix Dressing with Silver. Available online: https://dermarite.com/product/dermacolag/ (accessed on 13 February 2023).
- SilvaKollagen® Gel Silver Collagen Wound Gel. Available online: https://dermarite.com/product/silvakollagen-gel/ (accessed on 13 February 2023).
- Puracol Plus AG+ Collagen Wound Dressings with Silver. Available online: https://punchout.medline.com/product/Puracol-Plus-AG-Collagen-Wound-Dressings-with-Silver/Collagen-Dressings/Z05-PF00137?question=&index=P1&indexCount=1 (accessed on 13 February 2023).
- SEESKIN P—Collagen Particle Dressing. Available online: https://www.synerheal.com/product-page/seeskin-p-collagen-particle-dressing (accessed on 13 February 2023).
- CollaSorb. Available online: https://www.vitalitymedical.com/collasorb.html (accessed on 13 February 2023).
- GENTA-COLL ® Resorb Collagen Gentamicin Sponge. Available online: https://resorba.com/region/row/product/biosurgicals/genta-coll-resorb/ (accessed on 13 February 2023).
- COLLAMYCIN (Gentamicin Collagen Gel). Available online: https://www.synerheal.com/product-page/collamycin-gentamicin-collagen-gel (accessed on 13 February 2023).
- Gencoll Gel. Available online: https://www.cologenesis.net/medicated-gencoll-gel.htm (accessed on 13 February 2023).
- Colloskin-M. Available online: https://www.cologenesis.net/colloskin-m.htm (accessed on 13 February 2023).
- Collofiber-MM Medicated. Available online: https://www.cologenesis.net/collofiber-mm-medicated.htm (accessed on 13 February 2023).
- Coloplug. Available online: https://www.cologenesis.net/coloplug-collagen-sponge.htm (accessed on 13 February 2023).
- Diacoll-S. Available online: https://www.cologenesis.net/diacoll-s-sterile-collagen-sheet.htm (accessed on 13 February 2023).
- Irastorza, A.; Zarandona, I.; Andonegi, M.; Guerrero, P.; de la Caba, K. The versatility of collagen and chitosan: From food to biomedical applications. Food Hydrocoll. 2021, 116, 106633. [Google Scholar] [CrossRef]
- Yuan, H.; Chen, L.; Hong, F.F. A biodegradable antibacterial nanocomposite based on oxidized bacterial nanocellulose for rapid hemostasis and wound healing. ACS Appl. Mater. Interfaces 2019, 12, 3382–3392. [Google Scholar] [CrossRef]
- Ramadass, S.K.; Perumal, S.; Gopinath, A.; Nisal, A.; Subramanian, S.; Madhan, B. Sol–gel assisted fabrication of collagen hydrolysate composite scaffold: A novel therapeutic alternative to the traditional collagen scaffold. ACS Appl. Mater. Interfaces 2014, 6, 15015–15025. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudifard, M. Graphene family in cancer therapy: Recent progress in Cancer Gene/Drug delivery applications. J. Mater. Chem. B 2023, 11, 2568–2613. [Google Scholar]
- Oladele, I.; Agbabiaka, O.; Olasunkanmi, O.; Balogun, A.; Popoola, M. Non-synthetic sources for the development of hydroxyapatite. J. Appl. Biotechnol. Bioeng. 2018, 5, 88–95. [Google Scholar]
- Zhou, T.; Sui, B.; Mo, X.; Sun, J. Multifunctional and biomimetic fish collagen/bioactive glass nanofibers: Fabrication, antibacterial activity and inducing skin regeneration in vitro and in vivo. Int. J. Nanomed. 2017, 12, 3495. [Google Scholar] [CrossRef] [PubMed]
- Dolete, G.; Tihăuan, B.M.; Tutunaru, O.; Mocanu, I.-C.; Balaş, C.; Lavinia, I.; Ardelean, D.S.D.; Kamerzan, C.M.; Maier, S.S. Development and sequential analysis of a collagen-chitosan wound management biomaterial. Rom. Biotechnol. Lett. 2019, 24, 108–117. [Google Scholar] [CrossRef]
- ISO 20743:2007; Textiles—Determination of Antibacterial Activity of Antibacterial Finished Products. International Organization for Standardization: Geneva, Switzerland, 2007.
- Gilarska, A.; Lewandowska-Łańcucka, J.; Guzdek-Zając, K.; Karewicz, A.; Horak, W.; Lach, R.; Wójcik, K.; Nowakowska, M. Bioactive yet antimicrobial structurally stable collagen/chitosan/lysine functionalized hyaluronic acid–based injectable hydrogels for potential bone tissue engineering applications. Int. J. Biol. Macromol. 2020, 155, 938–950. [Google Scholar] [CrossRef] [PubMed]
- Valenzuela-Rojo, R.D.; López-Cervantes, J.; Sánchez-Machado, D.I.; Escárcega-Galaz, A.A.; del Rosario Martínez-Macias, M. Antibacterial, mechanical and physical properties of collagen-chitosan sponges from aquatic source. Sustain. Chem. Pharm. 2020, 15, 100218. [Google Scholar] [CrossRef]
- Rajasree, S.R.; Gobalakrishnan, M.; Aranganathan, L.; Karthih, M. Fabrication and characterization of chitosan based collagen/gelatin composite scaffolds from big eye snapper Priacanthus hamrur skin for antimicrobial and anti oxidant applications. Mater. Sci. Eng. C 2020, 107, 110270. [Google Scholar] [CrossRef] [PubMed]
- Bian, T.; Pang, N.; Xing, H. Preparation and antibacterial evaluation of a beta-tricalcium phosphate/collagen nanofiber biomimetic composite scaffold. Mater. Chem. Phys. 2021, 273, 125059. [Google Scholar] [CrossRef]
- Gao, Y.; Kang, Y.; Wang, T.; Li, C.; Shen, S.; Qu, C.; Gong, S.; Liu, P.; Yang, L.; Liu, J. Alginate microspheres-collagen hydrogel, as a novel 3D culture system, enhanced skin wound healing of hUCMSCs in rats model. Colloids Surf. B 2022, 219, 112799. [Google Scholar] [CrossRef]
- Dantas, G.; Sommer, M.O.; Oluwasegun, R.D.; Church, G.M. Bacteria subsisting on antibiotics. Science 2008, 320, 100–103. [Google Scholar] [CrossRef]
- Michalska-Sionkowska, M.; Kaczmarek, B.; Walczak, M.; Sionkowska, A. Antimicrobial activity of new materials based on the blends of collagen/chitosan/hyaluronic acid with gentamicin sulfate addition. Mater. Sci. Eng. C 2018, 86, 103–108. [Google Scholar] [CrossRef]
- Suchý, T.; Šupová, M.; Klapková, E.; Adamková, V.; Závora, J.; Žaloudková, M.; Rýglová, Š.; Ballay, R.; Denk, F.; Pokorný, M. The release kinetics, antimicrobial activity and cytocompatibility of differently prepared collagen/hydroxyapatite/vancomycin layers: Microstructure vs. nanostructure. Eur. J. Pharm. Sci. 2017, 100, 219–229. [Google Scholar] [CrossRef]
- Zhu, Q.; Teng, J.; Liu, X.; Lan, Y.; Guo, R. Preparation and characterization of gentamycin sulfate-impregnated gelatin microspheres/collagen–cellulose/nanocrystal scaffolds. Polym. Bull. 2018, 75, 77–91. [Google Scholar] [CrossRef]
- Liu, Y.; Ren, L.; Long, K.; Wang, L.; Wang, Y. Preparation and characterization of a novel tobramycin-containing antibacterial collagen film for corneal tissue engineering. Acta Biomater. 2014, 10, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Adayi, A.; Liu, Z.; Li, M.; Wu, M.; Xiao, L.; Sun, Y.; Cai, Q.; Yang, X.; Zhang, X. Asymmetric collagen/chitosan membrane containing minocycline-loaded chitosan nanoparticles for guided bone regeneration. Sci. Rep. 2016, 6, 31822. [Google Scholar] [CrossRef] [PubMed]
- Martin, V.; Ribeiro, I.A.; Alves, M.M.; Gonçalves, L.; Claudio, R.A.; Grenho, L.; Fernandes, M.H.; Gomes, P.; Santos, C.F.; Bettencourt, A.F. Engineering a multifunctional 3D-printed PLA-collagen-minocycline-nanoHydroxyapatite scaffold with combined antimicrobial and osteogenic effects for bone regeneration. Mater. Sci. Eng. C 2019, 101, 15–26. [Google Scholar] [CrossRef]
- Yu, X.; Yuan, Q.; Yang, M.; Liu, R.; Zhu, S.; Li, J.; Zhang, W.; You, J.; Xiong, S.; Hu, Y. Development of biocompatible and antibacterial collagen hydrogels via dialdehyde polysaccharide modification and tetracycline hydrochloride loading. Macromol. Mater. Eng. 2019, 304, 1800755. [Google Scholar] [CrossRef]
- Rivadeneira, J.; Di Virgilio, A.; Audisio, M.; Boccaccini, A.; Gorustovich, A. Evaluation of antibacterial and cytotoxic effects of nano-sized bioactive glass/collagen composites releasing tetracycline hydrochloride. J. Appl. Microbiol. 2014, 116, 1438–1446. [Google Scholar] [CrossRef] [PubMed]
- Semyari, H.; Salehi, M.; Taleghani, F.; Ehterami, A.; Bastami, F.; Jalayer, T.; Semyari, H.; Hamed Nabavi, M.; Semyari, H. Fabrication and characterization of collagen–hydroxyapatite-based composite scaffolds containing doxycycline via freeze-casting method for bone tissue engineering. J. Biomater. Appl. 2018, 33, 501–513. [Google Scholar] [CrossRef]
- Perumal, S.; kumar Ramadass, S.; Madhan, B. Sol–gel processed mupirocin silica microspheres loaded collagen scaffold: A synergistic bio-composite for wound healing. Eur. J. Pharm. Sci. 2014, 52, 26–33. [Google Scholar] [CrossRef]
- Hajikhani, M.; Emam-Djomeh, Z.; Askari, G. Fabrication and characterization of mucoadhesive bioplastic patch via coaxial polylactic acid (PLA) based electrospun nanofibers with antimicrobial and wound healing application. Int. J. Biol. Macromol. 2021, 172, 143–153. [Google Scholar] [CrossRef]
- Yilmaz Atay, H. Antibacterial activity of chitosan-based systems. In Functional Chitosan: Drug Delivery and Biomedical Applications; Springer Nature: Berlin/Heidelberg, Germany, 2019; pp. 457–489. [Google Scholar]
- Tripathi, S.; Singh, B.N.; Divakar, S.; Kumar, G.; Mallick, S.P.; Srivastava, P. Design and evaluation of ciprofloxacin loaded collagen chitosan oxygenating scaffold for skin tissue engineering. Biomed. Mater. 2021, 16, 025021. [Google Scholar] [CrossRef]
- Tsekoura, E.; Helling, A.; Wall, J.; Bayon, Y.; Zeugolis, D. Battling bacterial infection with hexamethylene diisocyanate cross-linked and Cefaclor-loaded collagen scaffolds. Biomed. Mater. 2017, 12, 035013. [Google Scholar] [CrossRef]
- Ahmadian, S.; Ghorbani, M.; Mahmoodzadeh, F. Silver sulfadiazine-loaded electrospun ethyl cellulose/polylactic acid/collagen nanofibrous mats with antibacterial properties for wound healing. Int. J. Biol. Macromol. 2020, 162, 1555–1565. [Google Scholar] [CrossRef]
- Mahmoud, A.A.; Salama, A.H. Norfloxacin-loaded collagen/chitosan scaffolds for skin reconstruction: Preparation, evaluation and in-vivo wound healing assessment. Eur. J. Pharm. Sci. 2016, 83, 155–165. [Google Scholar] [CrossRef]
- Song, Y.; Hu, Q.; Liu, Q.; Liu, S.; Wang, Y.; Zhang, H. Design and fabrication of drug-loaded alginate/hydroxyapatite/collagen composite scaffolds for repairing infected bone defects. J. Mater. Sci. 2023, 58, 911–926. [Google Scholar] [CrossRef]
- Feris, K.; Otto, C.; Tinker, J.; Wingett, D.; Punnoose, A.; Thurber, A.; Kongara, M.; Sabetian, M.; Quinn, B.; Hanna, C. Electrostatic interactions affect nanoparticle-mediated toxicity to gram-negative bacterium Pseudomonas aeruginosa PAO1. Langmuir 2010, 26, 4429–4436. [Google Scholar] [CrossRef]
- Luan, B.; Huynh, T.; Zhou, R. Complete wetting of graphene by biological lipids. Nanoscale 2016, 8, 5750–5754. [Google Scholar] [CrossRef] [PubMed]
- Armentano, I.; Arciola, C.R.; Fortunati, E.; Ferrari, D.; Mattioli, S.; Amoroso, C.F.; Rizzo, J.; Kenny, J.M.; Imbriani, M.; Visai, L. The interaction of bacteria with engineered nanostructured polymeric materials: A review. Sci. World J. 2014, 2014, 1–18. [Google Scholar] [CrossRef]
- Gao, W.; Thamphiwatana, S.; Angsantikul, P.; Zhang, L. Nanoparticle approaches against bacterial infections. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2014, 6, 532–547. [Google Scholar] [CrossRef]
- Rath, G.; Hussain, T.; Chauhan, G.; Garg, T.; Goyal, A.K. Collagen nanofiber containing silver nanoparticles for improved wound-healing applications. J. Drug Target. 2016, 24, 520–529. [Google Scholar] [CrossRef] [PubMed]
- Alarcon, E.I.; Udekwu, K.I.; Noel, C.W.; Gagnon, L.B.-P.; Taylor, P.K.; Vulesevic, B.; Simpson, M.J.; Gkotzis, S.; Islam, M.M.; Lee, C.-J. Safety and efficacy of composite collagen–silver nanoparticle hydrogels as tissue engineering scaffolds. Nanoscale 2015, 7, 18789–18798. [Google Scholar] [CrossRef] [PubMed]
- You, C.; Li, Q.; Wang, X.; Wu, P.; Ho, J.K.; Jin, R.; Zhang, L.; Shao, H.; Han, C. Silver nanoparticle loaded collagen/chitosan scaffolds promote wound healing via regulating fibroblast migration and macrophage activation. Sci. Rep. 2017, 7, 10489. [Google Scholar] [CrossRef]
- Song, J.; Zhang, P.; Cheng, L.; Liao, Y.; Xu, B.; Bao, R.; Wang, W.; Liu, W. Nano-silver in situ hybridized collagen scaffolds for regeneration of infected full-thickness burn skin. J. Mater. Chem. B 2015, 3, 4231–4241. [Google Scholar] [CrossRef]
- Ge, L.G.; Xu, Y.X.; Li, X.; Yuan, L.; Tan, H.; Li, D.; Mu, C. Fabrication of Antibacterial Collagen-Based Composite Wound Dressing. ACS Sustain. Chem. Eng. 2018, 6, 9153–9166. [Google Scholar] [CrossRef]
- Li, P.; Ruan, L.; Wang, R.; Liu, T.; Song, G.; Gao, X.; Jiang, G.; Liu, X. Electrospun Scaffold of Collagen and Polycaprolactone Containing ZnO Quantum Dots for Skin Wound Regeneration. J. Bionic Eng. 2021, 18, 1378–1390. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Sun, L.; Huang, S.; Zhu, C.; Li, P.; He, J.; Mackey, V.; Coy, D.H.; He, Q. The antimicrobial peptides and their potential clinical applications. Am. J. Transl. Res. 2019, 11, 3919. [Google Scholar] [PubMed]
- Lazzaro, B.P.; Zasloff, M.; Rolff, J. Antimicrobial peptides: Application informed by evolution. Science 2020, 368, eaau5480. [Google Scholar] [CrossRef]
- Kalelkar, P.P.; Riddick, M.; Garcia, A.J. Biomaterial-based antimicrobial therapies for the treatment of bacterial infections. Nat. Rev. Mater. 2021, 7, 39–54. [Google Scholar] [CrossRef]
- Kumar, P.; Kizhakkedathu, J.N.; Straus, S.K. Antimicrobial peptides: Diversity, mechanism of action and strategies to improve the activity and biocompatibility in vivo. Biomolecules 2018, 8, 4. [Google Scholar] [CrossRef]
- Ghalei, S.; Handa, H. A review on antibacterial silk fibroin-based biomaterials: Current state and prospects. Mater. Today Chem. 2022, 23, 100673. [Google Scholar] [CrossRef]
- Strempel, N.; Strehmel, J.; Overhage, J. Potential application of antimicrobial peptides in the treatment of bacterial biofilm infections. Curr. Pharm. Des. 2015, 21, 67–84. [Google Scholar] [CrossRef] [PubMed]
- Bacalum, M.; Radu, M. Cationic antimicrobial peptides cytotoxicity on mammalian cells: An analysis using therapeutic index integrative concept. Int. J. Pept. Res. Ther. 2015, 21, 47–55. [Google Scholar] [CrossRef]
- Lin, Z.; Wu, T.; Wang, W.; Li, B.; Wang, M.; Chen, L.; Xia, H.; Zhang, T. Biofunctions of antimicrobial peptide-conjugated alginate/hyaluronic acid/collagen wound dressings promote wound healing of a mixed-bacteria-infected wound. Int. J. Biol. Macromol. 2019, 140, 330–342. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.; Zhu, X.; Mutreja, I.; Boda, S.K.; Fischer, N.G.; Zhang, A.; Lui, C.; Qi, Y.; Aparicio, C. Biomimetic mineralized hybrid scaffolds with antimicrobial peptides. Bioact. Mater. 2021, 6, 2250–2260. [Google Scholar] [CrossRef] [PubMed]
- Cassin, M.E.; Ford, A.J.; Orbach, S.M.; Saverot, S.E.; Rajagopalan, P. The design of antimicrobial LL37-modified collagen-hyaluronic acid detachable multilayers. Acta Biomater. 2016, 40, 119–129. [Google Scholar] [CrossRef]
- Prakobkarn, J.; Makeudom, A.; Jenvoraphot, T.; Supanchart, C.; Krisanaprakornkit, S.; Punyodom, W.; Daranarong, D. Biphasic nanofibrous scaffolds based on collagen and PLC for controlled release LL-37 in guided bone regeneration. J. Appl. Polym. Sci. 2022, 139, 51629. [Google Scholar] [CrossRef]
- Hsu, S. Green tea and the skin. J. Am. Acad. Dermatol. 2005, 52, 1049–1059. [Google Scholar] [CrossRef] [PubMed]
- Thangapazham, R.L.; Sharad, S.; Maheshwari, R.K. Phytochemicals in wound healing. Adv. Wound Care 2016, 5, 230–241. [Google Scholar] [CrossRef]
- Agarwal, T.; Tan, S.-A.; Onesto, V.; Law, J.X.; Agrawal, G.; Pal, S.; Lim, W.L.; Sharifi, E.; Moghaddam, F.D.; Maiti, T.K. Engineered herbal scaffolds for tissue repair and regeneration: Recent trends and technologies. Biomed. Eng. Adv. 2021, 2, 100015. [Google Scholar] [CrossRef]
- Fathi, M.; Ahmadi, N.; Forouhar, A.; Hamzeh Atani, S. Natural Hydrogels, the Interesting Carriers for Herbal Extracts. Food Rev. Int. 2021, 38, 713–737. [Google Scholar] [CrossRef]
- Râpă, M.; Gaidau, C.; Mititelu-Tartau, L.; Berechet, M.-D.; Berbecaru, A.C.; Rosca, I.; Chiriac, A.P.; Matei, E.; Predescu, A.-M.; Predescu, C. Bioactive Collagen Hydrolysate-Chitosan/Essential Oil Electrospun Nanofibers Designed for Medical Wound Dressings. Pharmaceutics 2021, 13, 1939. [Google Scholar] [CrossRef]
- De Luca, I.; Pedram, P.; Moeini, A.; Cerruti, P.; Peluso, G.; Di Salle, A.; Germann, N. Nanotechnology Development for Formulating Essential Oils in Wound Dressing Materials to Promote the Wound-Healing Process: A Review. Appl. Sci. 2021, 11, 1713. [Google Scholar] [CrossRef]
- Ersanli, C.; Tzora, A.; Skoufos, I.; Fotou, K.; Maloupa, E.; Gridoriadou, K.; Voidarou, C.; Zeugolis, D.I. The Assessment of Antimicrobial and Anti-Biofilm Activity of Essential Oils against Staphylococcus aureus Strains. Antibiotics 2023, 12, 384. [Google Scholar] [CrossRef]
- Vaou, N.; Stavropoulou, E.; Voidarou, C.; Tsigalou, C.; Bezirtzoglou, E. Towards advances in medicinal plant antimicrobial activity: A review study on challenges and future perspectives. Microorganisms 2021, 9, 2041. [Google Scholar] [CrossRef] [PubMed]
- Cheirmadurai, K.; Thanikaivelan, P.; Murali, R. Highly biocompatible collagen–Delonix regia seed polysaccharide hybrid scaffolds for antimicrobial wound dressing. Carbohydr. Polym. 2016, 137, 584–593. [Google Scholar] [CrossRef]
- Thongtham, N.; Chai-in, P.; Unger, O.; Boonrungsiman, S.; Suwantong, O. Fabrication of chitosan/collagen/hydroxyapatite scaffolds with encapsulated Cissus quadrangularis extract. Polym. Adv. Technol. 2020, 31, 1496–1507. [Google Scholar] [CrossRef]
- Walczak, M.; Michalska-Sionkowska, M.; Kaczmarek, B.; Sionkowska, A. Surface and antibacterial properties of thin films based on collagen and thymol. Mater. Today Commun. 2020, 22, 100949. [Google Scholar] [CrossRef]
- Guo, R.; Lan, Y.; Xue, W.; Cheng, B.; Zhang, Y.; Wang, C.; Ramakrishna, S. Collagen-cellulose nanocrystal scaffolds containing curcumin-loaded microspheres on infected full-thickness burns repair. J. Tissue Eng. Regen. Med. 2017, 11, 3544–3555. [Google Scholar] [CrossRef]
- Govindarajan, D.; Duraipandy, N.; Srivatsan, K.V.; Lakra, R.; Korapatti, P.S.; Jayavel, R.; Kiran, M.S. Fabrication of hybrid collagen aerogels reinforced with wheat grass bioactives as instructive scaffolds for collagen turnover and angiogenesis for wound healing applications. ACS Appl. Mater. Interfaces 2017, 9, 16939–16950. [Google Scholar] [CrossRef]
- Derakhshan, M.A.; Nazeri, N.; Khoshnevisan, K.; Heshmat, R.; Omidfar, K. Three-layered PCL-collagen nanofibers containing melilotus officinalis extract for diabetic ulcer healing in a rat model. J. Diabetes Metab. Disord. 2022, 21, 313–321. [Google Scholar] [CrossRef]
- Socrates, R.; Prymak, O.; Loza, K.; Sakthivel, N.; Rajaram, A.; Epple, M.; Kalkura, S.N. Biomimetic fabrication of mineralized composite films of nanosilver loaded native fibrillar collagen and chitosan. Mater. Sci. Eng. C 2019, 99, 357–366. [Google Scholar] [CrossRef]
- Craciunescu, O.; Seciu, A.-M.; Zarnescu, O. In vitro and in vivo evaluation of a biomimetic scaffold embedding silver nanoparticles for improved treatment of oral lesions. Mater. Sci. Eng. C 2021, 123, 112015. [Google Scholar] [CrossRef]
- Mudhafar, M.; Zainol, I.; Alsailawi, H.; Aiza Jaafar, C. Synthesis and characterization of fish scales of hydroxyapatite/collagen–silver nanoparticles composites for the applications of bone filler. JKCerS 2021, 59, 229–239. [Google Scholar] [CrossRef]
- Mandal, A.; Sekar, S.; Meera, K.M.S.; Mukherjee, A.; Sastry, T.P.; Mandal, A.B. Fabrication of collagen scaffolds impregnated with sago starch capped silver nanoparticles suitable for biomedical applications and their physicochemical studies. Phys. Chem. Chem. Phys. 2014, 16, 20175–20183. [Google Scholar] [CrossRef] [PubMed]
- Păunica-Panea, G.; Ficai, A.; Marin, M.M.; Marin, Ș.; Albu, M.G.; Constantin, V.D.; Dinu-Pîrvu, C.; Vuluga, Z.; Corobea, M.C.; Ghica, M.V. New collagen-dextran-zinc oxide composites for wound dressing. J. Nanomater. 2016, 2016, 34. [Google Scholar] [CrossRef]
- Neacsu, I.-A.; Melente, A.E.; Holban, A.-M.; Ficai, A.; Ditu, L.-M.; Kamerzan, C.-M.; TIHĂUAN, B.M.; Nicoara, A.I.; Bezirtzoglou, E.; CHIFIRIUC, C. Novel hydrogels based on collagen and ZnO nanoparticles with antibacterial activity for improved wound dressings. Rom. Biotechnol. Lett. 2019, 24, 317–323. [Google Scholar] [CrossRef]
- Albu, M.G.; Vladkova, T.G.; Ivanova, I.A.; Shalaby, A.S.; Moskova-Doumanova, V.S.; Staneva, A.D.; Dimitriev, Y.B.; Kostadinova, A.S.; Topouzova-Hristova, T.I. Preparation and biological activity of new collagen composites, part I: Collagen/zinc titanate nanocomposites. Appl. Biochem. Biotechnol. 2016, 180, 177–193. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Chen, K.; He, X.; Li, N.; Huang, J.; Tang, K.; Li, Y.; Wang, F. Nano-TiO2/collagen-chitosan porous scaffold for wound repairing. Int. J. Biol. Macromol. 2016, 91, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Tiplea, R.E.; Lemnaru, G.-M.; Trușcă, R.D.; Holban, A.; Kaya, M.G.A.; Dragu, L.D.; Ficai, D.; Ficai, A.; Bleotu, C. Antimicrobial films based on chitosan, collagen, and zno for skin tissue regeneration. Biointerface Res. Appl. Chem 2021, 11, 11985–11995. [Google Scholar]
- Alfata, R.; Ramahdita, G.; Yuwono, A.H. The Effect of Additional Zinc Oxide to Antibacterial Property of Chitosan/Collagen-Based Scaffold. Mater. Sci. Forum 2020, 1000, 107–114. [Google Scholar] [CrossRef]
- Pasca, P.; Cavalu, S. The influence of propolis nanoparticles on dermal fibroblasts migration: Premises for development of propolis-based collagen dermal patches. Dig. J. Nanomater. Biostructures. 2021, 16, 929–938. [Google Scholar] [CrossRef]
- Jiménez, R.A.; Millán, D.; Suesca, E.; Sosnik, A.; Fontanilla, M.R. Controlled release of an extract of Calendula officinalis flowers from a system based on the incorporation of gelatin-collagen microparticles into collagen I scaffolds: Design and in vitro performance. Drug Deliv. Transl. Res. 2015, 5, 209–218. [Google Scholar] [CrossRef]
- Chen, Z.; Li, Y.; Dai, Y.; Zhou, Z.; Hu, Y.; Liu, H. Fabrication and Characterization of a Novel Berberine-oleanolic Acid Delivery Collagen I scaffold. J. Phys. Conf. Ser. 2020, 1637, 012105. [Google Scholar] [CrossRef]
- Laghezza Masci, V.; Taddei, A.R.; Courant, T.; Tezgel, O.; Navarro, F.; Giorgi, F.; Mariolle, D.; Fausto, A.M.; Texier, I. Characterization of collagen/lipid nanoparticle–curcumin cryostructurates for wound healing applications. Macromol. Biosci. 2019, 19, 1800446. [Google Scholar] [CrossRef] [PubMed]
- Senthilkumar, C.; Kannan, P.R.; Balashanmugam, P.; Raghunandhakumar, S.; Sathiamurthi, P.; Sivakumar, S.; Arockiarajan, A.; Mary, S.A.; Madhan, B. Collagen-Annona polysaccharide scaffolds with tetrahydrocurcumin loaded microspheres for antimicrobial wound dressing. Carbohydr. Polym. Technol. Appl. 2022, 3, 100204. [Google Scholar] [CrossRef]
- Hasan, M.M.; Shahid, M.A. PVA, Licorice, and Collagen (PLC) Based Hybrid Bio-nano Scaffold for Wound Healing Application. J. Biomater. Sci. Polym. Ed. 2022, 1–15. [Google Scholar] [CrossRef]
- Shaik, M.M.; Dapkekar, A.; Rajwade, J.M.; Jadhav, S.H.; Kowshik, M. Antioxidant-antibacterial containing bi-layer scaffolds as potential candidates for management of oxidative stress and infections in wound healing. J. Mater. Sci. Mater. Med. 2019, 30, 1–13. [Google Scholar] [CrossRef]
- Mitra, T.; Manna, P.J.; Raja, S.; Gnanamani, A.; Kundu, P. Curcumin loaded nano graphene oxide reinforced fish scale collagen–a 3D scaffold biomaterial for wound healing applications. RSC Adv. 2015, 5, 98653–98665. [Google Scholar] [CrossRef]
- Duraipandy, N.; Lakra, R.; Srivatsan, K.V.; Ramamoorthy, U.; Korrapati, P.S.; Kiran, M.S. Plumbagin caged silver nanoparticle stabilized collagen scaffold for wound dressing. J. Mater. Chem. B 2015, 3, 1415–1425. [Google Scholar] [CrossRef]
- Thapa, R.K.; Kiick, K.L.; Sullivan, M.O. Encapsulation of collagen mimetic peptide-tethered vancomycin liposomes in collagen-based scaffolds for infection control in wounds. Acta Biomater. 2020, 103, 115–128. [Google Scholar] [CrossRef]
- Nejaddehbashi, F.; Hashemitabar, M.; Bayati, V.; Abbaspour, M.; Moghimipour, E.; Orazizadeh, M. Application of polycaprolactone, chitosan, and collagen composite as a nanofibrous mat loaded with silver sulfadiazine and growth factors for wound dressing. Artif. Organs 2019, 43, 413–423. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Jin, Y.; Ying, X.; Wu, Q.; Yao, S.; Li, Y.; Liu, H.; Ma, G.; Wang, X. Development of an antimicrobial peptide-loaded mineralized collagen bone scaffold for infective bone defect repair. Regen. Biomater. 2020, 7, 515–525. [Google Scholar] [CrossRef] [PubMed]
- Antezana, P.E.; Municoy, S.; Pérez, C.J.; Desimone, M.F. Collagen Hydrogels Loaded with Silver Nanoparticles and Cannabis Sativa Oil. Antibiotics 2021, 10, 1420. [Google Scholar] [CrossRef] [PubMed]
- Srivatsan, K.V.; Duraipandy, N.; Begum, S.; Lakra, R.; Ramamurthy, U.; Korrapati, P.S.; Kiran, M.S. Effect of curcumin caged silver nanoparticle on collagen stabilization for biomedical applications. Int. J. Biol. Macromol. 2015, 75, 306–315. [Google Scholar] [CrossRef]
- Suchý, T.; Šupová, M.; Sauerová, P.; Kalbáčová, M.H.; Klapková, E.; Pokorný, M.; Horný, L.; Závora, J.; Ballay, R.; Denk, F. Evaluation of collagen/hydroxyapatite electrospun layers loaded with vancomycin, gentamicin and their combination: Comparison of release kinetics, antimicrobial activity and cytocompatibility. Eur. J. Pharm. Biopharm. 2019, 140, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Muthukumar, T.; Prabu, P.; Ghosh, K.; Sastry, T.P. Fish scale collagen sponge incorporated with Macrotyloma uniflorum plant extract as a possible wound/burn dressing material. Colloids Surf. B 2014, 113, 207–212. [Google Scholar] [CrossRef]
- Ghorbani, M.; Nezhad-Mokhtari, P.; Ramazani, S. Aloe vera-loaded nanofibrous scaffold based on Zein/Polycaprolactone/Collagen for wound healing. Int. J. Biol. Macromol. 2020, 153, 921–930. [Google Scholar] [CrossRef]
- Uzunalan, G.; Ozturk, M.T.; Dincer, S.; Tuzlakoglu, K. A newly designed collagen-based bilayered scaffold for skin tissue regeneration. J. Compos. Biodegrad. Polym. 2013, 1, 8–15. [Google Scholar] [CrossRef]
- Pal, P.; Nguyen, Q.C.; Benton, A.H.; Marquart, M.E.; Janorkar, A.V. Drug-Loaded Elastin-Like Polypeptide–Collagen Hydrogels with High Modulus for Bone Tissue Engineering. Macromol. Biosci. 2019, 19, 1900142. [Google Scholar] [CrossRef]
- Tihan, G.T.; Rău, I.; Zgârian, R.G.; Ungureanu, C.; Barbaresso, R.C.; Kaya, M.G.A.; Dinu-Pîrvu, C.; Ghica, M.V. Oxytetracycline versus doxycycline collagen sponges designed as potential carrier supports in biomedical applications. Pharmaceutics 2019, 11, 363. [Google Scholar] [CrossRef]
- Daza, J.H.U.; Righetto, G.M.; Chaud, M.V.; da Conceição Amaro Martins, V.; Lopes Baratella da Cunha Camargo, I.; Maria de Guzzi Plepis, A. PVA/anionic collagen membranes as drug carriers of ciprofloxacin hydrochloride with sustained antibacterial activity and potential use in the treatment of ulcerative keratitis. J. Biomater. Appl. 2020, 35, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Budhiraja, M.; Zafar, S.; Akhter, S.; Alrobaian, M.; Rashid, M.A.; Barkat, M.A.; Beg, S.; Ahmad, F.J. Mupirocin-loaded chitosan microspheres embedded in Piper betle extract containing collagen scaffold accelerate wound healing activity. AAPS PharmSciTech 2022, 23, 77. [Google Scholar] [CrossRef] [PubMed]
- Deaconu, M.; Prelipcean, A.-M.; Brezoiu, A.-M.; Mitran, R.-A.; Isopencu, G.; Matei, C.; Berger, D. Novel Collagen-Polyphenols-Loaded Silica Composites for Topical Application. Pharmaceutics 2023, 15, 312. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).