Evidence of Disruption in Neural Regeneration in Dry Eye Secondary to Rheumatoid Arthritis
Abstract
1. Introduction
2. Results
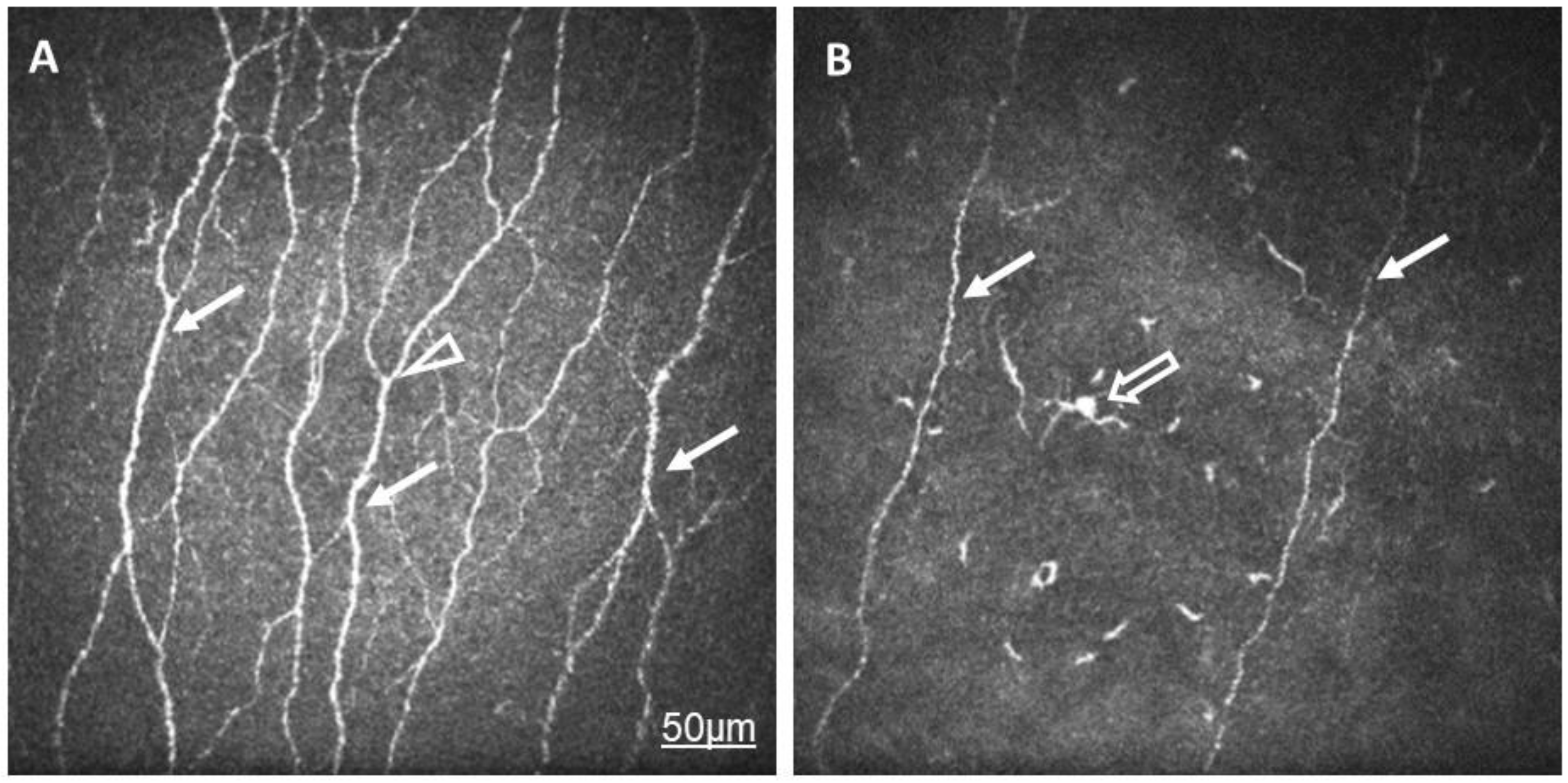
2.1. Comparison of RA and Control Groups
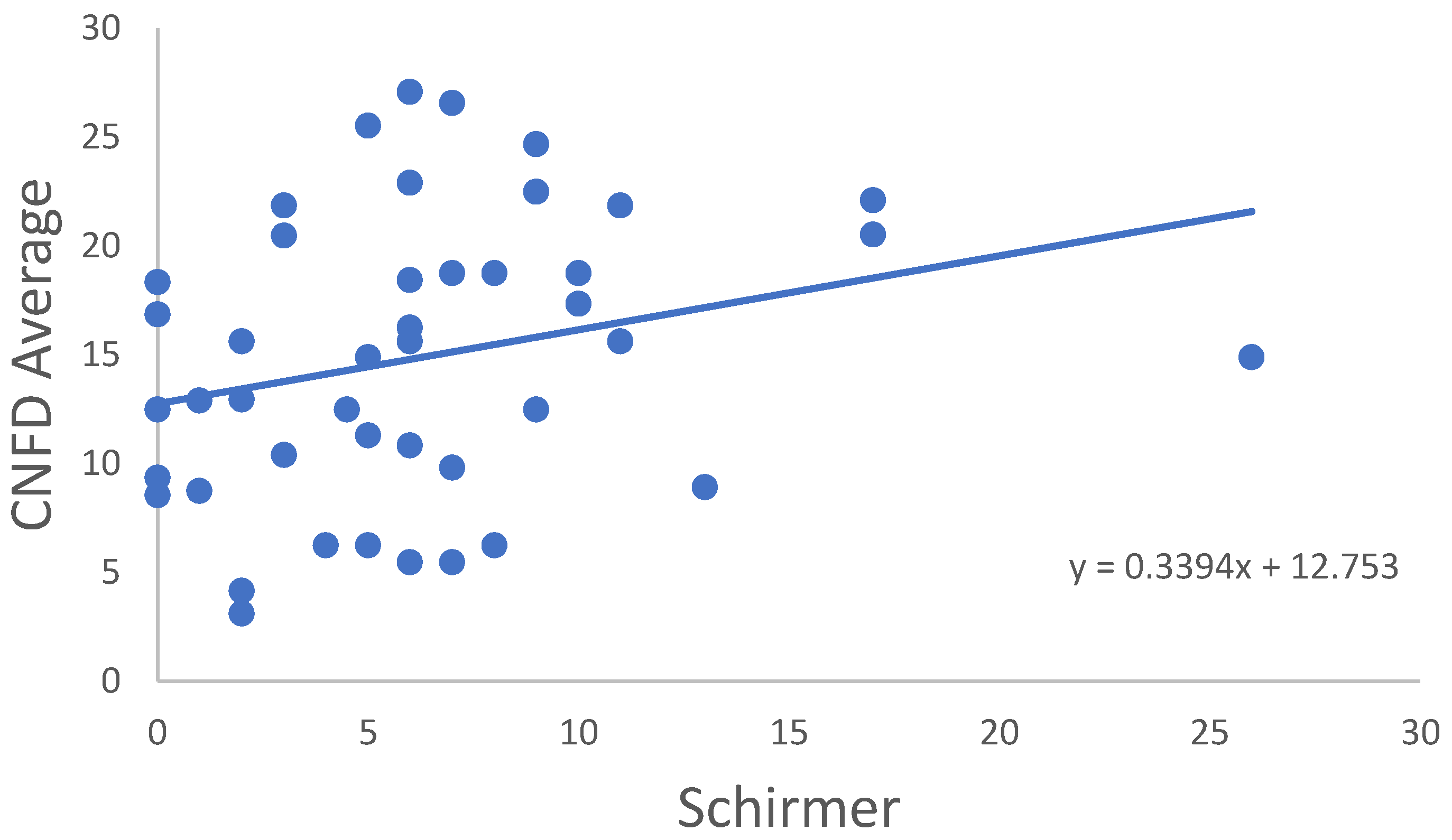
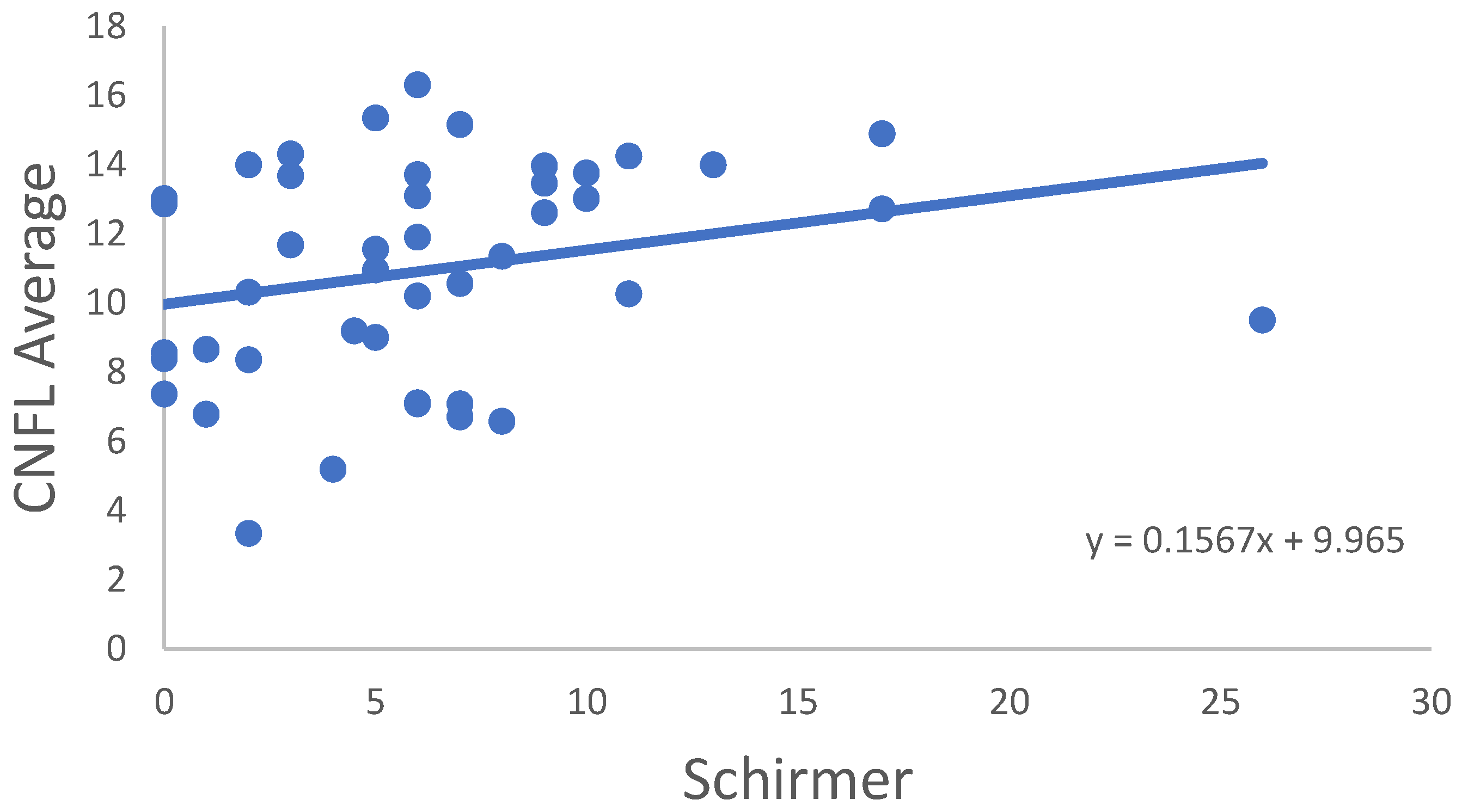
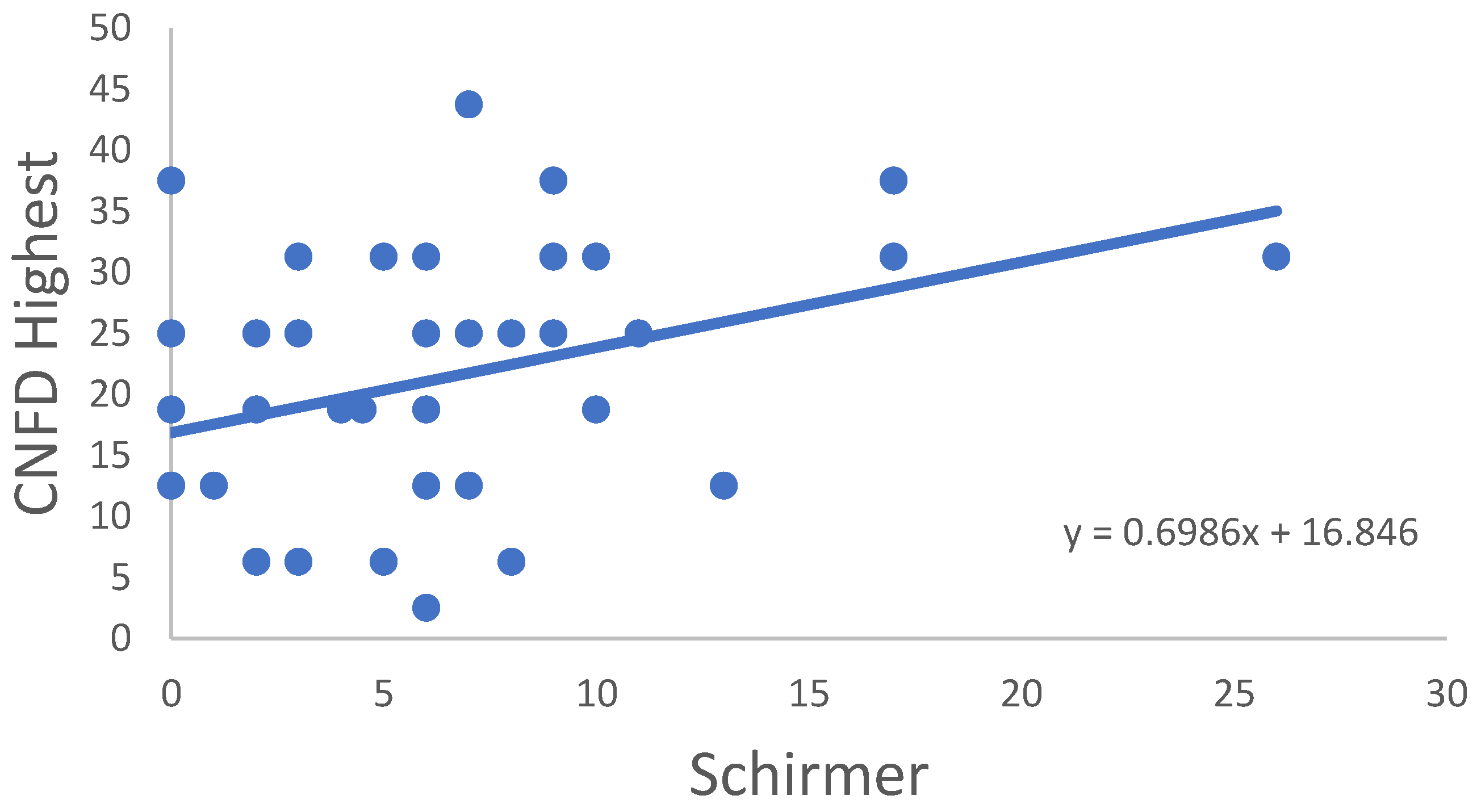
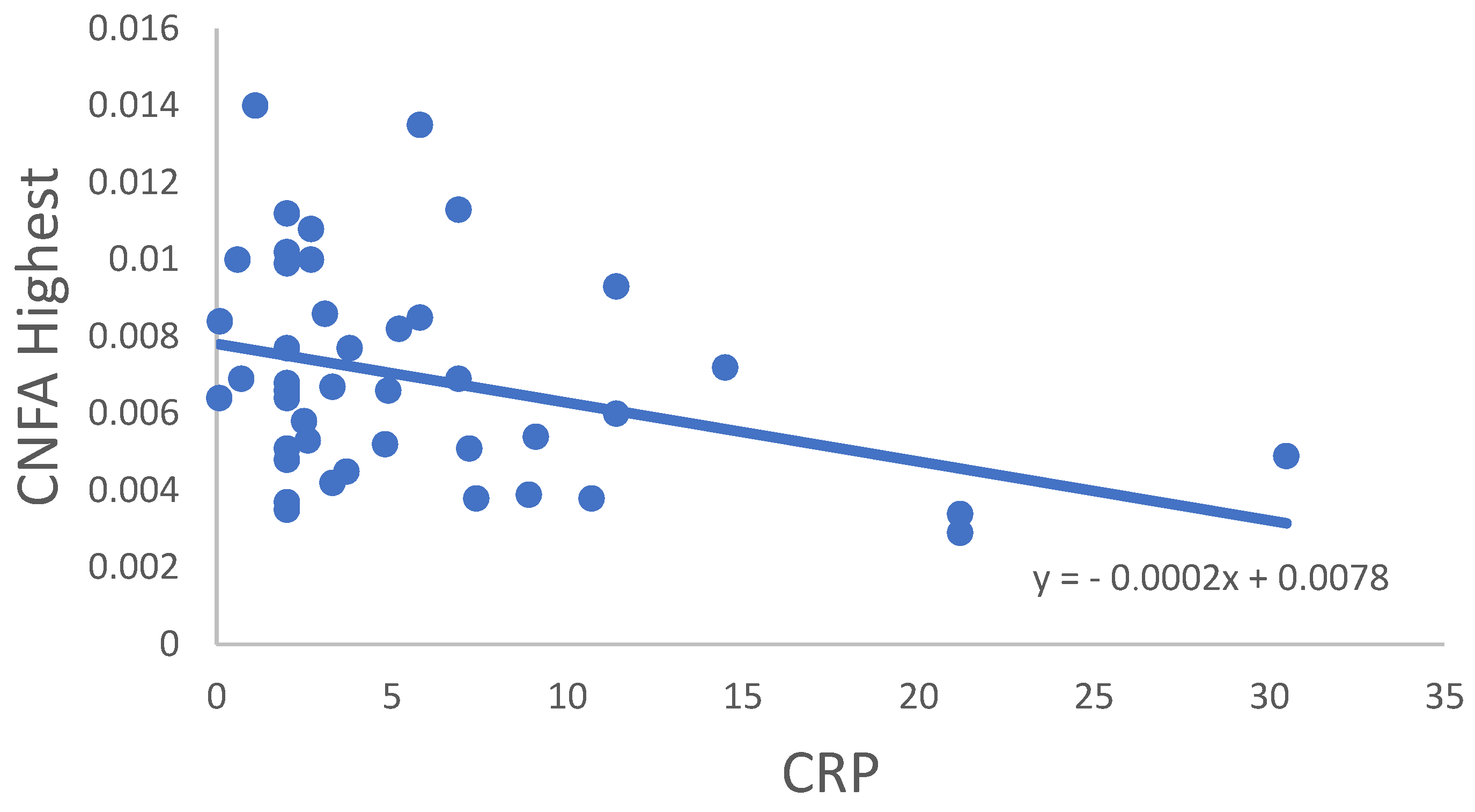
2.2. Correlation Analysis
2.3. Subgroup Analysis
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CNBD | Corneal nerve-branch density |
| CNFA | Corneal nerve-fiber area |
| CNFD | Corneal nerve-fiber density |
| CNFL | Corneal nerve-fiber length |
| CNFW | Corneal nerve-fiber width |
| CTBD | Corneal nerve-fiber total branch density |
| CRP | C-reactive protein |
| DAS28 | Disease activity score |
| DE | Dry eye |
| DED | Dry eye disease |
| ECM | Extracellular matrix |
| Hsp70 | Heat shock protein 70 |
| IL-6 | Interleukin-6 |
| IL-17 | Interleukin-17 |
| LC | Langerhans cells |
| MS | Multiple sclerosis |
| NGF | Nerve growth factor |
| NKT cell | CD3+/CD56+ natural killer-T cell |
| NF-κB | Nuclear factor kappa B |
| OSDI | Ocular-surface disease index |
| RA | Rheumatoid arthritis |
| SBNP | Sub-basal nerve plexus |
| TASK1 | TWIK-related acid-sensitive K+ channel 1 |
| TBUT | Tear break-up time |
| Th1 | CD4+IFN-γ+ |
| Th2 | CD4+IL-4+ |
| Th17 | CD4+IL-17+ |
| TLR4 | Toll-like receptor 4 |
| TNF-α | Tumor necrosis alpha |
| Treg | T regulatory cell |
References
- Tukaj, S.; Mantej, J.; Sobala, M.; Potrykus, K.; Sitko, K. Autologous extracellular Hsp70 exerts a dual role in rheumatoid arthritis. Cell. Stress. Chaperones 2020, 25, 1105–1110. [Google Scholar] [CrossRef] [PubMed]
- Lemp, M.A.; Foulks, G.N. The epidemiology of dry eye disease: Report of the Epidemiology Subcommittee of the International Dry Eye WorkShop (2007). Ocul. Surf. 2007, 5, 93–107. [Google Scholar] [CrossRef]
- Galor, A.; Moein, H.R.; Lee, C.; Rodriguez, A.; Felix, E.R.; Sarantopoulos, K.D.; Levitt, R.C. Neuropathic pain and dry eye. Ocul. Surf. 2018, 16, 31–44. [Google Scholar] [CrossRef] [PubMed]
- Shimazaki, J. Definition and Diagnostic Criteria of Dry Eye Disease: Historical Overview and Future Directions. Investig. Ophthalmol. Vis. Sci. 2018, 59, DES7–DES12. [Google Scholar] [CrossRef] [PubMed]
- Marsovszky, L.; Resch, M.D.; Nemeth, J.; Toldi, G.; Medgyesi, E.; Kovacs, L.; Balog, A. In vivo confocal microscopic evaluation of corneal Langerhans cell density, and distribution and evaluation of dry eye in rheumatoid arthritis. Innate Immun. 2013, 19, 348–354. [Google Scholar] [CrossRef]
- Woo, S.H.; Lukacs, V.; de Nooij, J.C.; Zaytseva, D.; Criddle, C.R.; Francisco, A.; Jessell, T.M.; Wilkinson, K.A.; Patapoutian, A. Piezo2 is the principal mechanotransduction channel for proprioception. Nat. Neurosci. 2015, 18, 1756–1762. [Google Scholar] [CrossRef]
- Sonkodi, B.; Bardoni, R.; Poór, G. Osteoporosis in Light of a New Mechanism Theory of Delayed Onset Muscle Soreness and Non-Contact Anterior Cruciate Ligament Injury. Int. J. Mol. Sci. 2022, 23, 9046. [Google Scholar] [CrossRef]
- Sonkodi, B. Psoriasis, Is It a Microdamage of Our “Sixth Sense”? A Neurocentric View. Int. J. Mol. Sci. 2022, 23, 11940. [Google Scholar] [CrossRef]
- Ulutatar, F.; Unal-Ulutatar, C.; Duruoz, M.T. Cervical proprioceptive impairment in patients with rheumatoid arthritis. Rheumatol. Int. 2019, 39, 2043–2051. [Google Scholar] [CrossRef]
- Suss, P.; Rothe, T.; Hoffmann, A.; Schlachetzki, J.C.M.; Winkler, J. The Joint-Brain Axis: Insights From Rheumatoid Arthritis on the Crosstalk Between Chronic Peripheral Inflammation and the Brain. Front. Immunol. 2020, 11, 612104. [Google Scholar] [CrossRef]
- Broce, I.; Karch, C.M.; Wen, N.; Fan, C.C.; Wang, Y.; Tan, C.H.; Kouri, N.; Ross, O.A.; Hoglinger, G.U.; Muller, U.; et al. Immune-related genetic enrichment in frontotemporal dementia: An analysis of genome-wide association studies. PLoS Med. 2018, 15, e1002487. [Google Scholar] [CrossRef]
- Sonkodi, B.; Hortobágyi, T. Amyotrophic lateral sclerosis and delayed onset muscle soreness in light of the impaired blink and stretch reflexes—Watch out for Piezo2. Open. Med. 2022, 17, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Sonkodi, B. Miswired Proprioception in Amyotrophic Lateral Sclerosis in Relation to Pain Sensation (and in Delayed Onset Muscle Soreness)—Is Piezo2 Channelopathy a Principal Transcription Activator in Proprioceptive Terminals Besides Being the Potential Primary Damage? Life 2023, 13, 657. [Google Scholar] [PubMed]
- Nagy, Z.F.; Sonkodi, B.; Pál, M.; Klivényi, P.; Széll, M. Likely Pathogenic Variants of Cav1.3 and Nav1.1 Encoding Genes in Amyotrophic Lateral Sclerosis Could Elucidate the Dysregulated Pain Pathways. Biomedicines 2023, 11, 933. [Google Scholar] [CrossRef]
- Eleftherohorinou, H.; Hoggart, C.J.; Wright, V.J.; Levin, M.; Coin, L.J. Pathway-driven gene stability selection of two rheumatoid arthritis GWAS identifies and validates new susceptibility genes in receptor mediated signalling pathways. Hum. Mol. Genet. 2011, 20, 3494–3506. [Google Scholar] [CrossRef]
- Sonkodi, B.; Resch, M.D.; Hortobágyi, T. Is the Sex Difference a Clue to the Pathomechanism of Dry Eye Disease? Watch out for the NGF-TrkA-Piezo2 Signaling Axis and the Piezo2 Channelopathy. J. Mol. Neurosci. 2022, 72, 1598–1608. [Google Scholar] [CrossRef]
- Glogowska, E.; Arhatte, M.; Chatelain, F.C.; Lesage, F.; Xu, A.; Grashoff, C.; Discher, D.E.; Patel, A.; Honore, E. Piezo1 and Piezo2 foster mechanical gating of K2P channels. Cell. Rep. 2021, 37, 110070. [Google Scholar] [CrossRef]
- Ehling, P.; Cerina, M.; Budde, T.; Meuth, S.G.; Bittner, S. The CNS under pathophysiologic attack—Examining the role of K2P channels. Pflug. Arch. 2015, 467, 959–972. [Google Scholar] [CrossRef]
- Meuth, S.G.; Bittner, S.; Meuth, P.; Simon, O.J.; Budde, T.; Wiendl, H. TWIK-related acid-sensitive K+ channel 1 (TASK1) and TASK3 critically influence T lymphocyte effector functions. J. Biol. Chem. 2008, 283, 14559–14570. [Google Scholar] [CrossRef]
- Kieseier, B.C.; Hartung, H.P. Targeting two-pore domain potassium channels—A promising strategy for treating T cell mediated autoimmunity. Exp. Neurol. 2013, 247, 286–288. [Google Scholar] [CrossRef]
- Bittner, S.; Bauer, M.A.; Ehling, P.; Bobak, N.; Breuer, J.; Herrmann, A.M.; Golfels, M.; Wiendl, H.; Budde, T.; Meuth, S.G. The TASK1 channel inhibitor A293 shows efficacy in a mouse model of multiple sclerosis. Exp. Neurol. 2012, 238, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Bittner, S.; Bobak, N.; Feuchtenberger, M.; Herrmann, A.M.; Gobel, K.; Kinne, R.W.; Hansen, A.J.; Budde, T.; Kleinschnitz, C.; Frey, O.; et al. Expression of K2P5.1 potassium channels on CD4+ T lymphocytes correlates with disease activity in rheumatoid arthritis patients. Arthritis Res. Ther. 2011, 13, R21. [Google Scholar] [CrossRef] [PubMed]
- Yanagihara, Y.; Shiozawa, K.; Takai, M.; Kyogoku, M.; Shiozawa, S. Natural killer (NK) T cells are significantly decreased in the peripheral blood of patients with rheumatoid arthritis (RA). Clin. Exp. Immunol. 1999, 118, 131–136. [Google Scholar] [CrossRef]
- Sonkodi, B.; Pállinger, É.; Radovits, T.; Csulak, E.; Shenker-Horváth, K.; Kopper, B.; Buzás, E.I.; Sydó, N.; Merkely, B. CD3+/CD56+ NKT-like Cells Show Imbalanced Control Immediately after Exercise in Delayed-Onset Muscle Soreness. Int. J. Mol. Sci. 2022, 23, 11117. [Google Scholar] [CrossRef] [PubMed]
- Albanesi, C.; Scarponi, C.; Bosisio, D.; Sozzani, S.; Girolomoni, G. Immune functions and recruitment of plasmacytoid dendritic cells in psoriasis. Autoimmunity 2010, 43, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Wang, Y.; Xu, J.; Zhou, T.; Chen, Z.; Yang, H.; Di, T.; Li, P. Protective effect of Yangxue Jiedu Soup against psoriasis-like lesions by regulating TLR4/NF-kappaB signaling pathway mediated by secretion of exosome HSP70. Biomed. Pharm. 2022, 147, 112604. [Google Scholar] [CrossRef]
- Mishra, S.; Kumar, A.; Varadwaj, P.K.; Misra, K. Structure-Based Drug Designing and Simulation Studies for Finding Novel Inhibitors of Heat Shock Protein (HSP70) as Suppressors for Psoriasis. Interdiscip. Sci. 2018, 10, 271–281. [Google Scholar] [CrossRef]
- Greb, J.E.; Goldminz, A.M.; Elder, J.T.; Lebwohl, M.G.; Gladman, D.D.; Wu, J.J.; Mehta, N.N.; Finlay, A.Y.; Gottlieb, A.B. Psoriasis. Nat. Rev. Dis. Prim. 2016, 2, 16082. [Google Scholar] [CrossRef]
- Tukaj, S.; Gruner, D.; Tukaj, C.; Zillikens, D.; Kasperkiewicz, M. Calcitriol exerts anti-inflammatory effects in keratinocytes treated with autoantibodies from a patient with bullous pemphigoid. J. Eur. Acad. Derm. Venereol. 2016, 30, 288–292. [Google Scholar] [CrossRef]
- Schinnerling, K.; Aguillon, J.C.; Catalan, D.; Soto, L. The role of interleukin-6 signalling and its therapeutic blockage in skewing the T cell balance in rheumatoid arthritis. Clin. Exp. Immunol. 2017, 189, 12–20. [Google Scholar] [CrossRef]
- Dos Santos, R.S.; Veras, F.P.; Ferreira, D.W.; Sant’Anna, M.B.; Lollo, P.C.B.; Cunha, T.M.; Galdino, G. Involvement of the Hsp70/TLR4/IL-6 and TNF-alpha pathways in delayed-onset muscle soreness. J. Neurochem. 2020, 155, 29–44. [Google Scholar] [CrossRef]
- Choi, I.A.; Lee, S.J.; Park, W.; Park, S.H.; Shim, S.C.; Baek, H.J.; Yoo, D.H.; Kim, H.A.; Lee, S.K.; Lee, Y.J.; et al. Effects of Tocilizumab Therapy on Serum Interleukin-33 and Interleukin-6 Levels in Patients With Rheumatoid Arthritis. Arch. Rheumatol. 2018, 33, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Murdaca, G.; Greco, M.; Tonacci, A.; Negrini, S.; Borro, M.; Puppo, F.; Gangemi, S. IL-33/IL-31 Axis in Immune-Mediated and Allergic Diseases. Int. J. Mol. Sci. 2019, 20, 5856. [Google Scholar] [CrossRef] [PubMed]
- Macedo, R.B.; Kakehasi, A.M.; Melo de Andrade, M.V. IL33 in rheumatoid arthritis: Potential contribution to pathogenesis. Rev. Bras. Reum. Engl. Ed. 2016, 56, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Trillo, J.; Florez-Paz, D.; Inigo-Portugues, A.; Gonzalez-Gonzalez, O.; Del Campo, A.G.; Gonzalez, A.; Viana, F.; Belmonte, C.; Gomis, A. Piezo2 Mediates Low-Threshold Mechanically Evoked Pain in the Cornea. J. Neurosci. 2020, 40, 8976–8993. [Google Scholar] [CrossRef]
- Sonkodi, B.; Berkes, I.; Koltai, E. Have We Looked in the Wrong Direction for More Than 100 Years? Delayed Onset Muscle Soreness Is, in Fact, Neural Microdamage Rather Than Muscle Damage. Antioxidants 2020, 9, 212. [Google Scholar] [CrossRef]
- Velasco-Estevez, M.; Koch, N.; Klejbor, I.; Caratis, F.; Rutkowska, A. Mechanoreceptor Piezo1 Is Downregulated in Multiple Sclerosis Brain and Is Involved in the Maturation and Migration of Oligodendrocytes in vitro. Front. Cell Neurosci. 2022, 16, 914985. [Google Scholar] [CrossRef]
- Villani, E.; Galimberti, D.; Viola, F.; Mapelli, C.; Del Papa, N.; Ratiglia, R. Corneal involvement in rheumatoid arthritis: An in vivo confocal study. Investig. Ophthalmol. Vis. Sci. 2008, 49, 560–564. [Google Scholar] [CrossRef]
- Jairaman, A.; Othy, S.; Dynes, J.L.; Yeromin, A.V.; Zavala, A.; Greenberg, M.L.; Nourse, J.L.; Holt, J.R.; Cahalan, S.M.; Marangoni, F.; et al. Piezo1 channels restrain regulatory T cells but are dispensable for effector CD4+ T cell responses. Sci. Adv. 2021, 7, abg5859. [Google Scholar] [CrossRef]
- Efraim, Y.; Chen, F.Y.T.; Cheong, K.N.; Gaylord, E.A.; McNamara, N.A.; Knox, S.M. A synthetic tear protein resolves dry eye through promoting corneal nerve regeneration. Cell Rep. 2022, 40, 111307. [Google Scholar] [CrossRef]
- Szczot, M.; Liljencrantz, J.; Ghitani, N.; Barik, A.; Lam, R.; Thompson, J.H.; Bharucha-Goebel, D.; Saade, D.; Necaise, A.; Donkervoort, S.; et al. PIEZO2 mediates injury-induced tactile pain in mice and humans. Sci. Transl. Med. 2018, 10, aat9892. [Google Scholar] [CrossRef] [PubMed]
- Zechini, L.; Amato, C.; Scopelliti, A.; Wood, W. Piezo acts as a molecular brake on wound closure to ensure effective inflammation and maintenance of epithelial integrity. Curr. Biol. 2022, 32, 3584–3592.e4. [Google Scholar] [CrossRef] [PubMed]
- Holt, J.R.; Zeng, W.Z.; Evans, E.L.; Woo, S.H.; Ma, S.; Abuwarda, H.; Loud, M.; Patapoutian, A.; Pathak, M.M. Spatiotemporal dynamics of PIEZO1 localization controls keratinocyte migration during wound healing. Elife 2021, 10, e65415. [Google Scholar] [CrossRef] [PubMed]
- Oswald, D.J.; Lee, A.; Trinidad, M.; Chi, C.; Ren, R.; Rich, C.B.; Trinkaus-Randall, V. Communication between corneal epithelial cells and trigeminal neurons is facilitated by purinergic (P2) and glutamatergic receptors. PLoS ONE 2012, 7, e44574. [Google Scholar] [CrossRef]
- Sugimoto, A.; Miyazaki, A.; Kawarabayashi, K.; Shono, M.; Akazawa, Y.; Hasegawa, T.; Ueda-Yamaguchi, K.; Kitamura, T.; Yoshizaki, K.; Fukumoto, S.; et al. Piezo type mechanosensitive ion channel component 1 functions as a regulator of the cell fate determination of mesenchymal stem cells. Sci. Rep. 2017, 7, 17696. [Google Scholar] [CrossRef]
- Maverakis, E.; Kim, K.; Shimoda, M.; Gershwin, M.E.; Patel, F.; Wilken, R.; Raychaudhuri, S.; Ruhaak, L.R.; Lebrilla, C.B. Glycans in the immune system and The Altered Glycan Theory of Autoimmunity: A critical review. J. Autoimmun. 2015, 57, 1–13. [Google Scholar] [CrossRef]
- Hurysz, B.; Bottini, N. Emerging proteoglycans and proteoglycan-targeted therapies in rheumatoid arthritis. Am. J. Physiol. Cell Physiol. 2022, 322, C1061–C1067. [Google Scholar] [CrossRef]
- Inamdar, S.R.; Barbieri, E.; Terrill, N.J.; Knight, M.M.; Gupta, H.S. Proteoglycan degradation mimics static compression by altering the natural gradients in fibrillar organisation in cartilage. Acta Biomater. 2019, 97, 437–450. [Google Scholar] [CrossRef]
- Sonkodi, B.; Hegedűs, Á.; Kopper, B.; Berkes, I. Significantly Delayed Medium-Latency Response of the Stretch Reflex in Delayed-Onset Muscle Soreness of the Quadriceps Femoris Muscles Is Indicative of Sensory Neuronal Microdamage. J. Funct. Morphol. Kinesiol. 2022, 7, 43. [Google Scholar] [CrossRef]
- Sonkodi, B. Delayed Onset Muscle Soreness and Critical Neural Microdamage-Derived Neuroinflammation. Biomolecules 2022, 12, 1207. [Google Scholar] [CrossRef]
- Chery, D.R.; Han, B.; Li, Q.; Zhou, Y.; Heo, S.J.; Kwok, B.; Chandrasekaran, P.; Wang, C.; Qin, L.; Lu, X.L.; et al. Early changes in cartilage pericellular matrix micromechanobiology portend the onset of post-traumatic osteoarthritis. Acta Biomater. 2020, 111, 267–278. [Google Scholar] [CrossRef]
- Du, G.; Chen, W.; Li, L.; Zhang, Q. The potential role of mechanosensitive ion channels in substrate stiffness-regulated Ca2+ response in chondrocytes. Connect. Tissue Res. 2022, 63, 453–462. [Google Scholar] [CrossRef]
- Hanyecz, A.; Olasz, K.; Tarjanyi, O.; Nemeth, P.; Mikecz, K.; Glant, T.T.; Boldizsar, F. Proteoglycan aggrecan conducting T cell activation and apoptosis in a murine model of rheumatoid arthritis. BioMed Res. Int. 2014, 2014, 942148. [Google Scholar] [CrossRef]
- de Jong, H.; Berlo, S.E.; Hombrink, P.; Otten, H.G.; van Eden, W.; Lafeber, F.P.; Heurkens, A.H.; Bijlsma, J.W.; Glant, T.T.; Prakken, B.J. Cartilage proteoglycan aggrecan epitopes induce proinflammatory autoreactive T-cell responses in rheumatoid arthritis and osteoarthritis. Ann. Rheum. Dis. 2010, 69, 255–262. [Google Scholar] [CrossRef]
- Kim, C.E.; Oh, H.N.; Lee, J.H.; Yang, J.W. Effects of chondrocyte-derived extracellular matrix in a dry eye mouse model. Mol. Vis. 2015, 21, 1210–1223. [Google Scholar]
- Kvien, T.K.; Uhlig, T.; Odegard, S.; Heiberg, M.S. Epidemiological aspects of rheumatoid arthritis: The sex ratio. Ann. N. Y. Acad. Sci. 2006, 1069, 212–222. [Google Scholar] [CrossRef]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O., 3rd; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010, 62, 2569–2581. [Google Scholar] [CrossRef]
- Vitali, C.; Bombardieri, S.; Jonsson, R.; Moutsopoulos, H.M.; Alexander, E.L.; Carsons, S.E.; Daniels, T.E.; Fox, P.C.; Fox, R.I.; Kassan, S.S.; et al. Classification criteria for Sjogren’s syndrome: A revised version of the European criteria proposed by the American-European Consensus Group. Ann. Rheum. Dis. 2002, 61, 554–558. [Google Scholar] [CrossRef]
- Jing, D.; Liu, Y.; Chou, Y.; Jiang, X.; Ren, X.; Yang, L.; Su, J.; Li, X. Change patterns in the corneal sub-basal nerve and corneal aberrations in patients with dry eye disease: An artificial intelligence analysis. Exp. Eye Res. 2022, 215, 108851. [Google Scholar] [CrossRef]
- Schiffman, R.M.; Christianson, M.D.; Jacobsen, G.; Hirsch, J.D.; Reis, B.L. Reliability and validity of the Ocular Surface Disease Index. Arch. Ophthalmol. 2000, 118, 615–621. [Google Scholar] [CrossRef]
- Ostrovski, I.; Lovblom, L.E.; Farooqi, M.A.; Scarr, D.; Boulet, G.; Hertz, P.; Wu, T.; Halpern, E.M.; Ngo, M.; Ng, E.; et al. Reproducibility of In Vivo Corneal Confocal Microscopy Using an Automated Analysis Program for Detection of Diabetic Sensorimotor Polyneuropathy. PLoS ONE 2015, 10, e0142309. [Google Scholar] [CrossRef]
| Control | RA | |
|---|---|---|
| No. of Patients | 44 | 40 |
| No. of Eyes | 44 | 53 |
| Age (Years) | 45.9 ± 20.2 [19–73] | 50.6 ± 13.2 [28–74] |
| Gender (Male/Female) | 20/24 | 13/27 |
| RA Duration (Years) | - | 10.5 ± 9.2 [0.3–53] |
| DAS28 | - | 2.6 ± 0.9 [0.9–5.1] |
| CRP | - | 5.9 ± 6.5 [0.1–30.5] |
| TBUT (s) | 11.3 ± 3.0 [4–16] * | 8.9 ± 3.6 [4–20] |
| Schirmer Test (mm/5 min) | 12.2 ± 3.0 [5–17] * | 6.9 ± 5.8 [0–26] |
| OSDI | 10.1 ± 8.3 [0–35] | 34.2 ± 25.2 [0–94] * |
| Group | N | Mean | SD | p | Cohen’s d | |
|---|---|---|---|---|---|---|
| CNFD 1 Average | RA | 52 | 13.92 | 6.69 | 0.001 | 0.749 |
| Control | 39 | 19.02 | 6.98 | |||
| CNBD 2 Average | RA | 52 | 15.32 | 9.04 | 0.006 | 0.722 |
| Control | 39 | 23.45 | 13.69 | |||
| CNFL 3 Average | RA | 52 | 10.57 | 3.22 | 0.002 | 0.777 |
| Control | 39 | 13.07 | 3.22 | |||
| CTBD 4 Average | RA | 52 | 30.03 | 15.35 | 0.01 | 0.61 |
| Control | 39 | 40.21 | 18.31 | |||
| CNFA 5 Average | RA | 52 | 0.0053 | 0.0021 | 0.007 | 0.533 |
| Control | 39 | 0.0063 | 0.0018 | |||
| CNFD Highest | RA | 52 | 2000 | 10.71 | 0.018 | 0.481 |
| Control | 39 | 25.09 | 10.43 | |||
| CNBD Highest | RA | 52 | 27.04 | 20.70 | 0.044 | 0.499 |
| Control | 39 | 38.94 | 27.48 | |||
| CNFL Highest | RA | 52 | 14.53 | 4.16 | 0.014 | 0.617 |
| Control | 39 | 17.14 | 4.33 | |||
| CTBD Highest | RA | 52 | 47.83 | 31.94 | 0.089 | 0.387 |
| Control | 39 | 60.89 | 35.95 | |||
| CNFA Highest | RA | 52 | 0.0072 | 0.0031 | 0.087 | 0.27 |
| Control | 39 | 0.0798 | 0.0026 |
| Variable | r |
|---|---|
| CNFD Average—Schirmer | 0.339 |
| CNFL Average—Schirmer | 0.306 |
| CNFD Highest—Schirmer | 0.340 |
| CNFA Highest—CRP | −0.328 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sonkodi, B.; Csorba, A.; Marsovszky, L.; Balog, A.; Kopper, B.; Nagy, Z.Z.; Resch, M.D. Evidence of Disruption in Neural Regeneration in Dry Eye Secondary to Rheumatoid Arthritis. Int. J. Mol. Sci. 2023, 24, 7514. https://doi.org/10.3390/ijms24087514
Sonkodi B, Csorba A, Marsovszky L, Balog A, Kopper B, Nagy ZZ, Resch MD. Evidence of Disruption in Neural Regeneration in Dry Eye Secondary to Rheumatoid Arthritis. International Journal of Molecular Sciences. 2023; 24(8):7514. https://doi.org/10.3390/ijms24087514
Chicago/Turabian StyleSonkodi, Balázs, Anita Csorba, László Marsovszky, Attila Balog, Bence Kopper, Zoltán Zsolt Nagy, and Miklós D. Resch. 2023. "Evidence of Disruption in Neural Regeneration in Dry Eye Secondary to Rheumatoid Arthritis" International Journal of Molecular Sciences 24, no. 8: 7514. https://doi.org/10.3390/ijms24087514
APA StyleSonkodi, B., Csorba, A., Marsovszky, L., Balog, A., Kopper, B., Nagy, Z. Z., & Resch, M. D. (2023). Evidence of Disruption in Neural Regeneration in Dry Eye Secondary to Rheumatoid Arthritis. International Journal of Molecular Sciences, 24(8), 7514. https://doi.org/10.3390/ijms24087514





