The Protective Role of TREM2 in the Heterogenous Population of Macrophages during Post-Myocardial Infarction Inflammation
Abstract
1. Introduction
2. Role of Inflammation in Myocardial Infarction
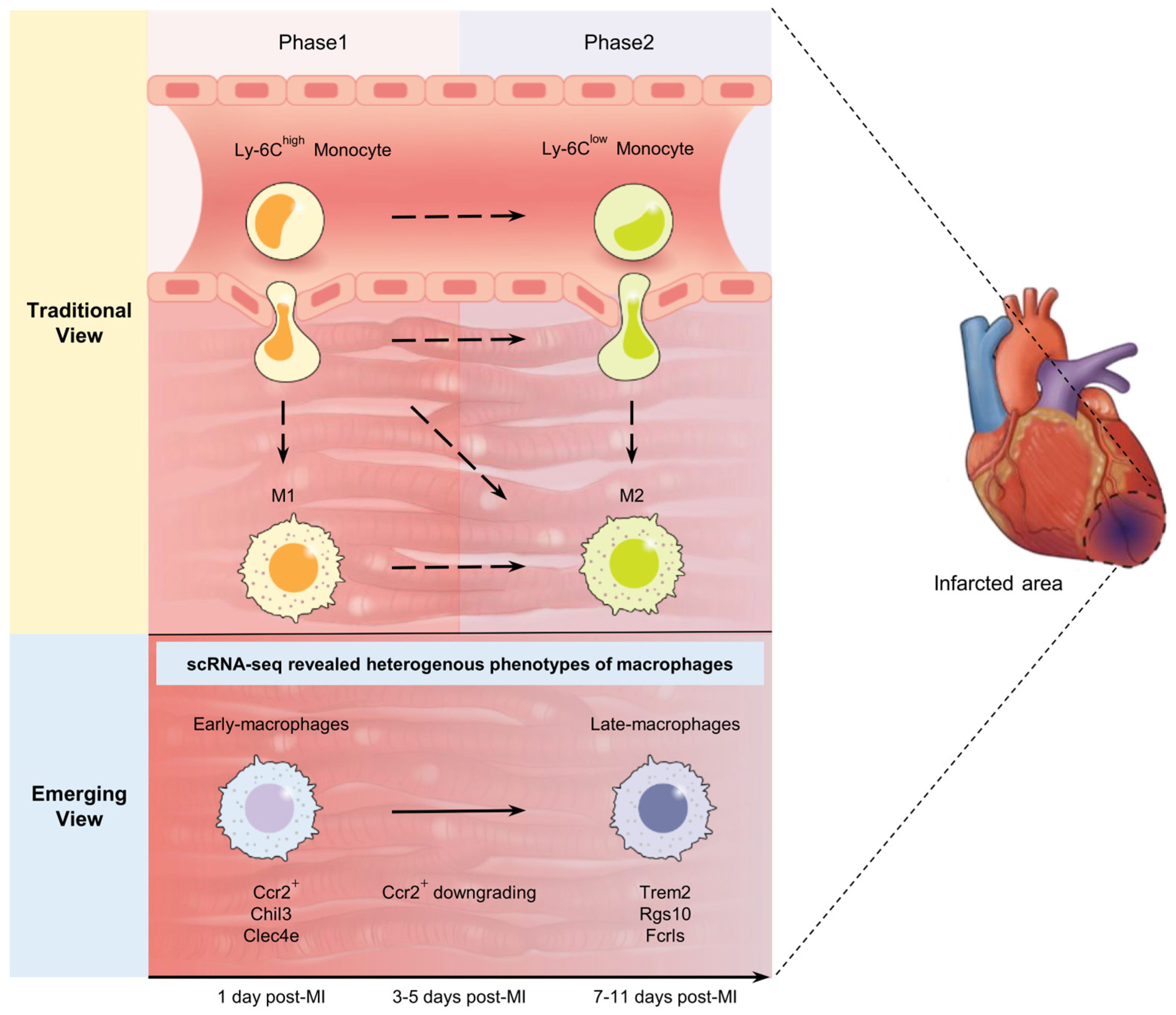
3. Macrophages in Myocardial Infarction in Classical View
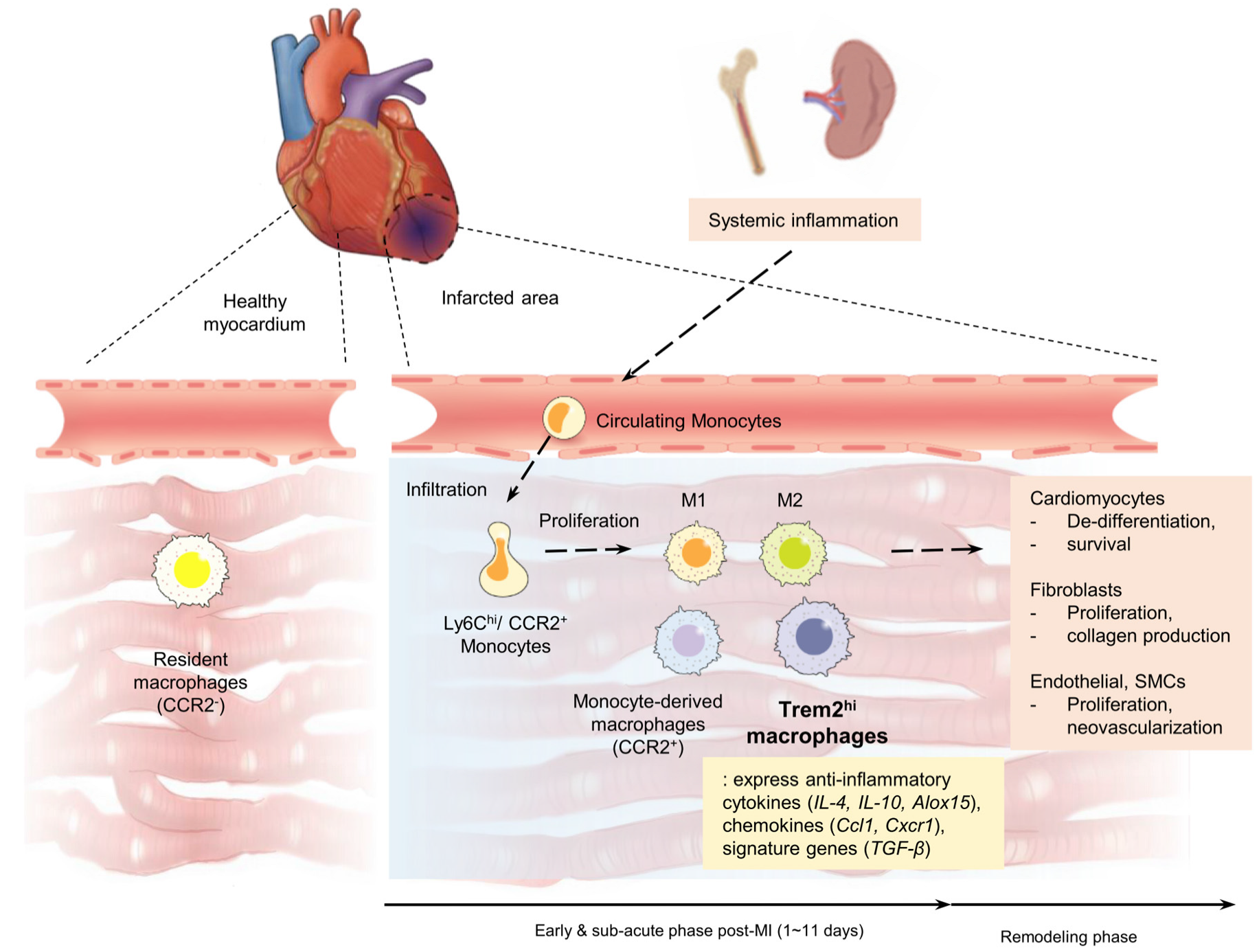
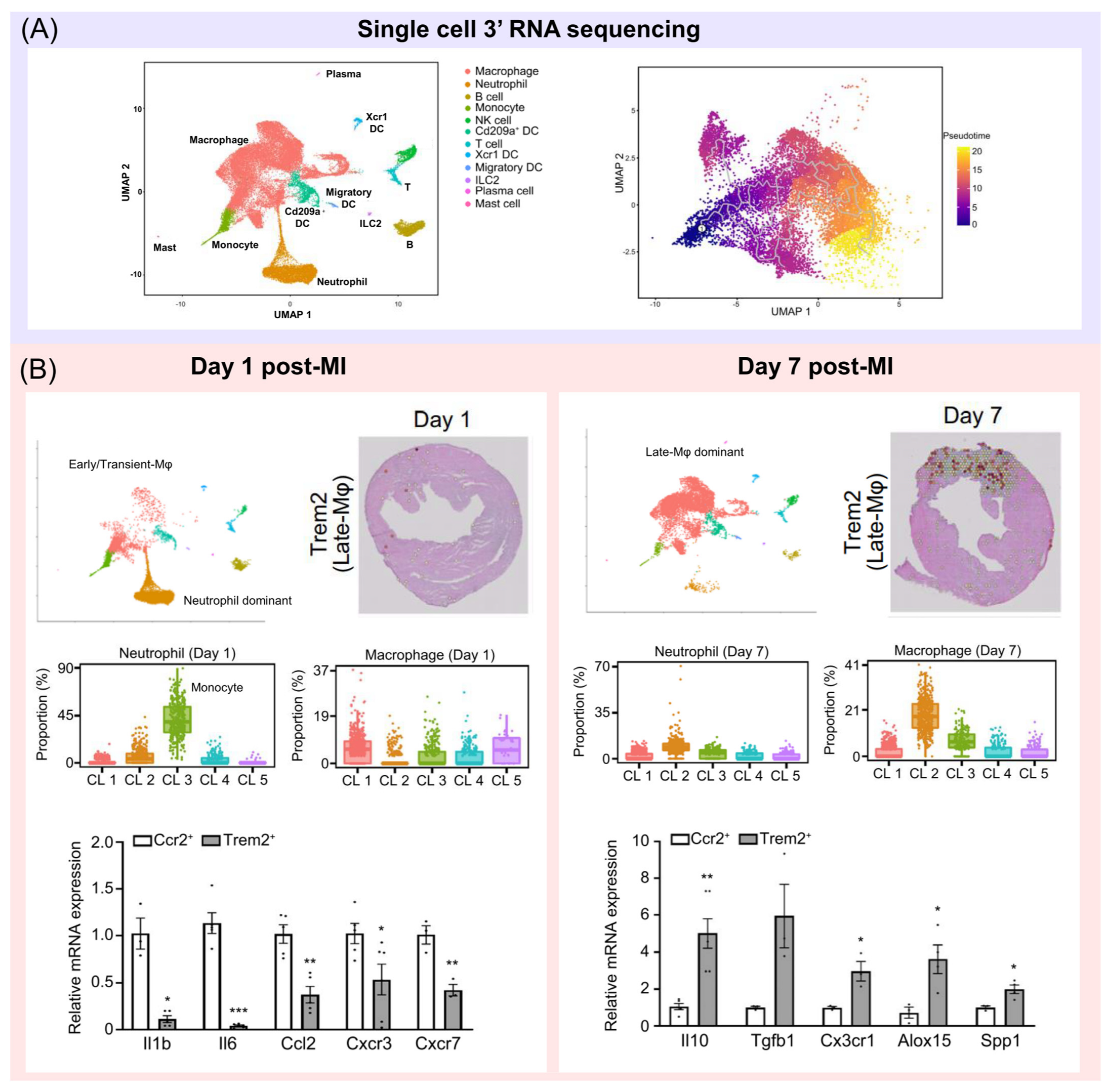
4. Novel Concepts of Macrophages Revealed Using Single-Cell RNA Sequencing
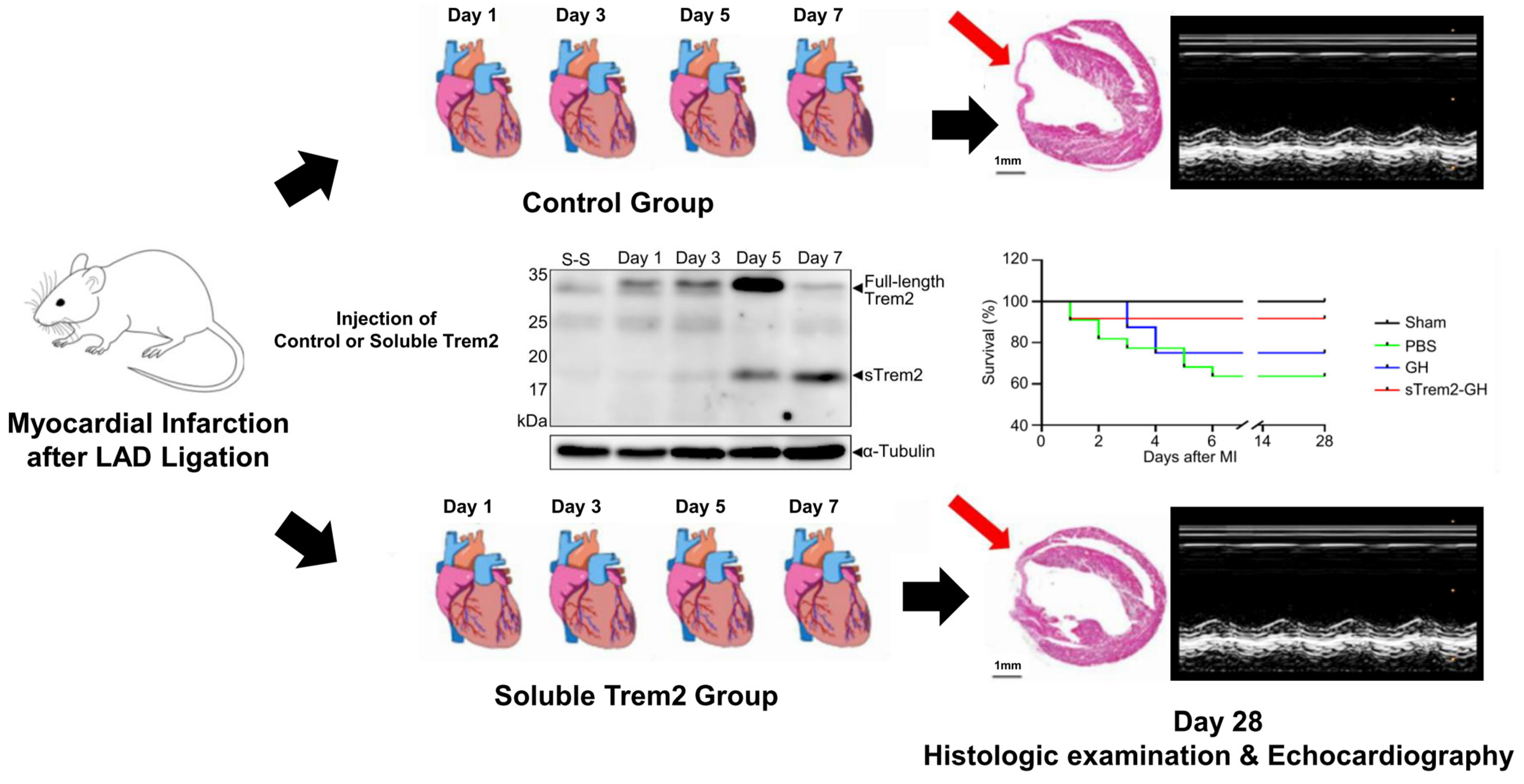
5. Trem2hi Macrophage in Cardiovascular Disease and Myocardial Infarction
| Study | Disease | Main Findings |
|---|---|---|
| Yeh et al. (2016) [49] | Alzheimer | The uptake of low-density lipoprotein and apolipoproteins E and J was increased in heterologous cells when Trem2 was overexpressed. On the contrary, disease variants in Trem2 impaired lipoprotein binding and uptake into cells. |
| Ulland et al. (2017) [48] | Alzheimer | The risk of developing Alzheimer’s disease is increased in individuals with hypomorphic variants of Trem2. In mouse models, Trem2-deficient microglia display autophagy. |
| Park et al. (2015) [52] | Obesity | In Trem2 transgenic mice fed with a high-fat diet, the upregulation of adipogenic regulators was observed, which indicates that Trem2 promotes obesity and adipogenesis. |
| Jaitin et al. (2019) [51] | Obesity | Using scRNA-sec, researchers observed a dynamic adipose tissue immune cell atlas in both mice and humans. The study revealed that Trem2 plays a key role in the protective functions of LAMs, which counteract inflammation, adipocyte hypertrophy, and metabolic disease. |
| Ramachandran et al. (2019) [53] | Liver cirrhosis | Trem2 has been identified as a profibrotic marker associated with scar formation. In this study on human liver cirrhosis, researchers were able to resolve the fibrotic niche and identify the association of Trem2+ CD9+ macrophages. |
| Cochain et al. (2018) [58] | Atherosclerosis | The identification of arterial leukocytes in a murine atherosclerotic aorta model revealed a subset that is associated with atherosclerosis and expresses Trem2. |
| Depuydt et al. (2020) [56] | Atherosclerosis | The researchers identified a foam-cell-like myeloid cell population expressing Trem2 in human carotid atherosclerotic plaques. |
| Waring et al. (2022) [57] | Calcification | Trem2hi macrophages generate microcalcifications in plaques and are associated with plaque instability in mice. |
| Fu et al. (2022) [59] | Myocardial infarction | The expression of Trem2 was found to be increased in mice with myocardial infarction, and it was observed that Trem2 may activate the PI3K/AKT signaling pathway. In Trem2-transfected mice, reduced injury, smaller infarct size, and fewer apoptotic cells were observed, as well as better echocardiographic function. |
| Jung et al. (2022) [10] | Myocardial infarction | After myocardial infarction in mice, there was an increase in Trem2 expression in macrophages during the subacute phase of cardiac injury. Administering soluble Trem2 in vivo resulted in marked enhancements in both the functional and structural aspects of the infarcted hearts. |
6. The Role of Trem2 as a Therapeutic Target and Future Direction
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roth, G.A.; Forouzanfar, M.H.; Moran, A.E.; Barber, R.; Nguyen, G.; Feigin, V.L.; Naghavi, M.; Mensah, G.A.; Murray, C.J. Demographic and epidemiologic drivers of global cardiovascular mortality. N. Engl. J. Med. 2015, 372, 1333–1341. [Google Scholar] [CrossRef] [PubMed]
- Frantz, S.; Hundertmark, M.J.; Schulz-Menger, J.; Bengel, F.M.; Bauersachs, J. Left ventricular remodelling post-myocardial infarction: Pathophysiology, imaging, and novel therapies. Eur. Heart J. 2022, 43, 2549–2561. [Google Scholar] [CrossRef] [PubMed]
- Heron, M. Deaths: Leading Causes for 2017. Natl. Vital. Stat. Rep. 2019, 68, 1–77. [Google Scholar]
- Fonseca, F.A.; Izar, M.C. Role of Inflammation in Cardiac Remodeling After Acute Myocardial Infarction. Front. Physiol. 2022, 13, 927163. [Google Scholar] [CrossRef]
- Ridker, P.M.; Everett, B.M.; Pradhan, A.; MacFadyen, J.G.; Solomon, D.H.; Zaharris, E.; Mam, V.; Hasan, A.; Rosenberg, Y.; Iturriaga, E.; et al. Low-Dose Methotrexate for the Prevention of Atherosclerotic Events. N. Engl. J. Med. 2019, 380, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Kloner, R.A.; Fishbein, M.C.; Lew, H.; Maroko, P.R.; Braunwald, E. Mummification of the infarcted myocardium by high dose corticosteroids. Circulation 1978, 57, 56–63. [Google Scholar] [CrossRef]
- Nahrendorf, M.; Pittet, M.J.; Swirski, F.K. Monocytes: Protagonists of infarct inflammation and repair after myocardial infarction. Circulation 2010, 121, 2437–2445. [Google Scholar] [CrossRef]
- Peet, C.; Ivetic, A.; Bromage, D.I.; Shah, A.M. Cardiac monocytes and macrophages after myocardial infarction. Cardiovasc. Res. 2020, 116, 1101–1112. [Google Scholar] [CrossRef]
- Dick, S.A.; Macklin, J.A.; Nejat, S.; Momen, A.; Clemente-Casares, X.; Althagafi, M.G.; Chen, J.; Kantores, C.; Hosseinzadeh, S.; Aronoff, L.; et al. Self-renewing resident cardiac macrophages limit adverse remodeling following myocardial infarction. Nat. Immunol. 2019, 20, 29–39. [Google Scholar] [CrossRef]
- Jung, S.H.; Hwang, B.H.; Shin, S.; Park, E.H.; Park, S.H.; Kim, C.W.; Kim, E.; Choo, E.; Choi, I.J.; Swirski, F.K.; et al. Spatiotemporal dynamics of macrophage heterogeneity and a potential function of Trem2(hi) macrophages in infarcted hearts. Nat. Commun. 2022, 13, 4580. [Google Scholar] [CrossRef]
- Kim, G.H.; Uriel, N.; Burkhoff, D. Reverse remodelling and myocardial recovery in heart failure. Nat. Rev. Cardiol. 2018, 15, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Cushman, M.; Stampfer, M.J.; Tracy, R.P.; Hennekens, C.H. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N. Engl. J. Med. 1997, 336, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Danielson, E.; Fonseca, F.A.H.; Genest, J.; Gotto, A.M.; Kastelein, J.J.P.; Koenig, W.; Libby, P.; Lorenzatti, A.J.; MacFadyen, J.G.; et al. Reduction in C-reactive protein and LDL cholesterol and cardiovascular event rates after initiation of rosuvastatin: A prospective study of the JUPITER trial. Lancet 2009, 373, 1175–1182. [Google Scholar] [CrossRef]
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N. Engl. J. Med. 2017, 377, 1119–1131. [Google Scholar] [CrossRef]
- Tardif, J.C.; Kouz, S.; Waters, D.D.; Bertrand, O.F.; Diaz, R.; Maggioni, A.P.; Pinto, F.J.; Ibrahim, R.; Gamra, H.; Kiwan, G.S.; et al. Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. N. Engl. J. Med. 2019, 381, 2497–2505. [Google Scholar] [CrossRef] [PubMed]
- Nidorf, S.M.; Fiolet, A.T.L.; Mosterd, A.; Eikelboom, J.W.; Schut, A.; Opstal, T.S.J.; The, S.H.K.; Xu, X.F.; Ireland, M.A.; Lenderink, T.; et al. Colchicine in Patients with Chronic Coronary Disease. N. Engl. J. Med. 2020, 383, 1838–1847. [Google Scholar] [CrossRef] [PubMed]
- Broch, K.; Anstensrud, A.K.; Woxholt, S.; Sharma, K.; Tollefsen, I.M.; Bendz, B.; Aakhus, S.; Ueland, T.; Amundsen, B.H.; Damas, J.K.; et al. Randomized Trial of Interleukin-6 Receptor Inhibition in Patients with Acute ST-Segment Elevation Myocardial Infarction. J. Am. Coll. Cardiol. 2021, 77, 1845–1855. [Google Scholar] [CrossRef] [PubMed]
- Casarotti, A.C.A.; Teixeira, D.; Longo-Maugeri, I.M.; Ishimura, M.E.; Coste, M.E.R.; Bianco, H.T.; Moreira, F.T.; Bacchin, A.F.; Izar, M.C.; Goncalves, I.; et al. Role of B lymphocytes in the infarcted mass in patients with acute myocardial infarction. Biosci. Rep. 2021, 41, BSR20203413. [Google Scholar] [CrossRef]
- Thomas, M.R.; James, S.K.; Becker, R.C.; Himmelmann, A.; Katus, H.A.; Cannon, C.P.; Steg, P.G.; Siegbahn, A.; Lakic, T.; Storey, R.F.; et al. Prognostic impact of baseline inflammatory markers in patients with acute coronary syndromes treated with ticagrelor and clopidogrel. Eur. Heart J. Acute Cardiovasc. Care 2021, 10, 153–163. [Google Scholar] [CrossRef]
- Roberts, R.; DeMello, V.; Sobel, B.E. Deleterious effects of methylprednisolone in patients with myocardial infarction. Circulation 1976, 53, 204–206. [Google Scholar]
- Zhang, H.; Yang, K.; Chen, F.; Liu, Q.; Ni, J.; Cao, W.; Hua, Y.; He, F.; Liu, Z.; Li, L.; et al. Role of the CCL2-CCR2 axis in cardiovascular disease: Pathogenesis and clinical implications. Front. Immunol. 2022, 30, 975367. [Google Scholar] [CrossRef]
- Wang, J.; Seo, M.J.; Deci, M.B.; Weil, B.R.; Canty, J.M.; Nguyen, J. Effect of CCR2 inhibitor-loaded lipid micelles on inflammatory cell migration and cardiac function after myocardial infarction. Int. J. Nanomed. 2018, 13, 6441–6451. [Google Scholar] [CrossRef]
- Chen, B.; Brickshawana, A.; Frangogiannis, N.G. The functional heterogeneity of resident cardiac macrophages in myocardial injury: CCR2+ cells promote inflammation, whereas CCR2- cells protect. Circ Res. 2019, 124, 183–185. [Google Scholar] [CrossRef]
- Leid, J.; Carrelha, J.; Boukarabila, H.; Epelman, S.; Jacobsen, S.E.; Lavine, K.J. Primitive embryonic macrophages are required for coronary development and maturation. Circ. Res. 2016, 118, 1498–1511. [Google Scholar] [CrossRef]
- Heidt, T.; Courties, G.; Dutta, P.; Sager, H.B.; Sebas, M.; Iwamoto, Y.; Sun, Y.; Da Silva, N.; Panizzi, P.; van der Laan, A.M. Differential contribution of monocytes to heart macrophages in steady-state and after myocardial infarction. Circ. Res. 2014, 115, 284–295. [Google Scholar] [CrossRef] [PubMed]
- Bajpai, G.; Schneider, C.; Wong, N.; Bredemeyer, A.; Hulsmans, M.; Nahrendorf, M.; Epelman, S.; Kreisel, D.; Liu, Y.; Itoh, A. The human heart contains distinct macrophage subsets with divergent origins and functions. Nat. Med. 2018, 24, 1234–1245. [Google Scholar] [CrossRef] [PubMed]
- Dewald, O.; Zymek, P.; Winkelmann, K.; Koerting, A.; Ren, G.; Abou-Khamis, T.; Michael, L.H.; Rollins, B.J.; Entman, M.L.; Frangogiannis, N.G. CCL2/monocyte chemoattractant protein1 regulates inflammatory responses critical to healing myocardial infarcts. Circ. Res. 2005, 96, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Bajpai, G.; Bredemeyer, A.; Li, W.; Zaitsev, K.; Koenig, A.L.; Lokshina, I.; Mohan, J.; Ivey, B.; Hsiao, H.-M.; Weinheimer, C. Tissue resident CCR2- and CCR2+ cardiac macrophages differentially orchestrate monocyte recruitment and fate specification following myocardial injury. Circ. Res. 2019, 124, 263–278. [Google Scholar] [CrossRef]
- Geissmann, F.; Jung, S.; Littman, D.R. Blood monocytes consist of two principal subsets with distinct migratory properties. Immunity 2003, 19, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Berg, K.E.; Ljungcrantz, I.; Andersson, L.; Bryngelsson, C.; Hedblad, B.; Fredrikson, G.N.; Nilsson, J.; Björkbacka, H. Elevated CD14++CD16- monocytes predict cardiovascular events. Circ. Cardiovasc. Genet. 2012, 5, 122–131. [Google Scholar] [CrossRef]
- Thomas, G.D.; Hanna, R.N.; Vasudevan, N.T.; Hamers, A.A.; Romanoski, C.E.; McArdle, S.; Ross, K.D.; Blatchley, A.; Yoakum, D.; Hamilton, B.A.; et al. Deleting an Nr4a1 super-enhancer subdomain ablates Ly6C(low) monocytes while preserving macrophage gene function. Immunity 2016, 45, 975–987. [Google Scholar] [CrossRef]
- Murray, P.J.; Allen, J.E.; Biswas, S.K.; Fisher, E.A.; Gilroy, D.W.; Goerdt, S.; Gordon, S.; Hamilton, J.A.; Ivashkiv, L.B.; Lawrence, T. Macrophage activation and polarization: Nomenclature and experimental guidelines. Immunity 2014, 41, 14–20. [Google Scholar] [CrossRef]
- Rurik, J.G.; Aghajanian, H.; Epstein, J.A. Immune Cells and Immunotherapy for Cardiac Injury and Repair. Circ. Res. 2021, 128, 1766–1779. [Google Scholar] [CrossRef]
- Kumar, V.; Prabhu, S.D.; Bansal, S.S. CD4+ T-lymphocytes exhibit biphasic kinetics post-myocardial infarction. Front. Cardiovasc. Med. 2022, 9, 992653. [Google Scholar] [CrossRef]
- Yang, M.; Song, L.; Wang, L.; Yukht, A.; Ruther, H.; Li, F.; Qin, M.; Ghiasi, H.; Sharifi, B.G.; Shah, P.K. Deficiency of GATA3-Positive Macrophages Improves Cardiac Function Following Myocardial Infarction or Pressure Overload Hypertrophy. J. Am. Coll. Cardiol. 2018, 72, 885–904. [Google Scholar] [CrossRef]
- Saliba, A.E.; Westermann, A.J.; Gorski, S.A.; Vogel, J. Single-cell RNA-seq: Advances and future challenges. Nucleic Acids Res. 2014, 42, 8845–8860. [Google Scholar] [CrossRef]
- Li, L.; Wang, M.; Ma, Q.; Li, Y.; Ye, J.; Sun, X.; Sun, G. Progress of Single-Cell RNA Sequencing Technology in Myocardial Infarction Research. Front. Cardiovasc. Med. 2022, 9, 768834. [Google Scholar] [CrossRef] [PubMed]
- Vafadarnejad, E.; Rizzo, G.; Krampert, L.; Arampatzi, P.; Arias-Loza, A.-P.; Nazzal, Y.; Rizakou, A.; Knochenhauer, T.; Bandi, S.R.; Nugroho, V.A. Dynamics of cardiac neutrophil diversity in murine myocardial infarction. Circ. Res. 2020, 127, e232–e249. [Google Scholar] [CrossRef] [PubMed]
- Mildner, A.; Schonheit, J.; Giladi, A.; David, E.; Lara-Astiaso, D.; Lorenzo-Vivas, E.; Paul, F.; Chappell-Maor, L.; Priller, J.; Leutz, A.; et al. Genomic Characterization of Murine Monocytes Reveals C/EBPbeta Transcription Factor Dependence of Ly6C(-) Cells. Immunity 2017, 46, 849–862 e847. [Google Scholar] [CrossRef] [PubMed]
- Nahrendorf, M.; Swirski, F.K. Abandoning M1/M2 for a Network Model of Macrophage Function. Circ. Res. 2016, 119, 414–417. [Google Scholar] [CrossRef]
- Zhuang, L.; Lu, L.; Zhang, R.; Chen, K.; Yan, X. Comprehensive integration of single-cell transcriptional profiling reveals the heterogeneities of non-cardiomyocytes in healthy and ischemic hearts. Front. Cardiovasc. Med. 2020, 7, 330. [Google Scholar] [CrossRef]
- Ni, S.-H.; Xu, J.-D.; Sun, S.-N.; Li, Y.; Zhou, Z.; Li, H.; Liu, X.; Deng, J.-P.; Huang, Y.-S.; Chen, Z.-X.; et al. Single-cell transcriptomic analyses of cardiac immune cells reveal that Rel-driven CD72-positive macrophages induce cardiomyocyte injury. Cardiovasc. Res. 2021, 118, 1303–1320. [Google Scholar] [CrossRef] [PubMed]
- Swirski, F.K.; Robbins, C.S.; Nahrendorf, M. Development and function of arterial and cardiac macrophages. Trends Immunol. 2016, 37, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Hilgendorf, I.; Gerhardt, L.M.; Tan, T.C.; Winter, C.; Holderried, T.A.; Chousterman, B.G.; Iwamoto, Y.; Liao, R.; Zirlik, A.; Scherer-Crosbie, M.; et al. Ly-6Chigh monocytes depend on Nr4a1 to balance both inflammatory and reparative phases in the infarcted myocardium. Circ. Res. 2014, 114, 1611–1622. [Google Scholar] [CrossRef] [PubMed]
- Lavine, K.J.; Epelman, S.; Uchida, K.; Weber, K.J.; Nichols, C.G.; Schilling, J.D.; Ornitz, D.M.; Randolph, G.J.; Mann, D.L. Distinct macrophage lineages contribute to disparate patterns of cardiac recovery and remodeling in the neonatal and adult heart. Proc. Natl. Acad. Sci. USA 2014, 111, 16029–16034. [Google Scholar] [CrossRef]
- Deczkowska, A.; Weiner, A.; Amit, I. The Physiology, Pathology, and Potential Therapeutic Applications of the TREM2 Signaling Pathway. Cell 2020, 181, 1207–1217. [Google Scholar] [CrossRef]
- Wu, K.; Byers, D.E.; Jin, X.; Agapov, E.; Alexander-Brett, J.; Patel, A.C.; Cella, M.; Gilfilan, S.; Colonna, M.; Kober, D.L.; et al. TREM-2 promotes macrophage survival and lung disease after respiratory viral infection. J. Exp. Med. 2015, 212, 681–697. [Google Scholar] [CrossRef]
- Ulland, T.K.; Song, W.M.; Huang, S.C.; Ulrich, J.D.; Sergushichev, A.; Beatty, W.L.; Loboda, A.A.; Zhou, Y.; Cairns, N.J.; Kambal, A.; et al. TREM2 Maintains Microglial Metabolic Fitness in Alzheimer’s Disease. Cell 2017, 170, 649–663 e613. [Google Scholar] [CrossRef]
- Yeh, F.L.; Wang, Y.; Tom, I.; Gonzalez, L.C.; Sheng, M. TREM2 Binds to Apolipoproteins, Including APOE and CLU/APOJ, and Thereby Facilitates Uptake of Amyloid-Beta by Microglia. Neuron 2016, 91, 328–340. [Google Scholar] [CrossRef]
- Molgora, M.; Esaulova, E.; Vermi, W.; Hou, J.; Chen, Y.; Luo, J.; Brioschi, S.; Bugatti, M.; Omodei, A.S.; Ricci, B.; et al. TREM2 Modulation Remodels the Tumor Myeloid Landscape Enhancing Anti-PD-1 Immunotherapy. Cell 2020, 182, 886–900 e817. [Google Scholar] [CrossRef]
- Jaitin, D.A.; Adlung, L.; Thaiss, C.A.; Weiner, A.; Li, B.; Descamps, H.; Lundgren, P.; Bleriot, C.; Liu, Z.; Deczkowska, A.; et al. Lipid-Associated Macrophages Control Metabolic Homeostasis in a Trem2-Dependent Manner. Cell 2019, 178, 686–698 e614. [Google Scholar] [CrossRef]
- Park, M.; Yi, J.W.; Kim, E.M.; Yoon, I.J.; Lee, E.H.; Lee, H.Y.; Ji, K.Y.; Lee, K.H.; Jang, J.H.; Oh, S.S.; et al. Triggering receptor expressed on myeloid cells 2 (TREM2) promotes adipogenesis and diet-induced obesity. Diabetes 2015, 64, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, P.; Dobie, R.; Wilson-Kanamori, J.R.; Dora, E.F.; Henderson, B.E.P.; Luu, N.T.; Portman, J.R.; Matchett, K.P.; Brice, M.; Marwick, J.A.; et al. Resolving the fibrotic niche of human liver cirrhosis at single-cell level. Nature 2019, 575, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Robbins, C.S.; Hilgendorf, I.; Weber, G.F.; Theurl, I.; Iwamoto, Y.; Figueiredo, J.L.; Gorbatov, R.; Sukhova, G.K.; Gerhardt, L.M.; Smyth, D.; et al. Local proliferation dominates lesional macrophage accumulation in atherosclerosis. Nat. Med. 2013, 19, 1166–1172. [Google Scholar] [CrossRef]
- Abd-Elrahman, I.; Kosuge, H.; Wises Sadan, T.; Ben-Nun, Y.; Meir, K.; Rubinstein, C.; Bogyo, M.; McConnell, M.V.; Blum, G. Cathepsin Activity-Based Probes and Inhibitor for Preclinical Atherosclerosis Imaging and Macrophage Depletion. PLoS ONE 2016, 11, e0160522. [Google Scholar] [CrossRef]
- Creager, M.D.; Hohl, T.; Hutcheson, J.D.; Moss, A.J.; Schlotter, F.; Blaser, M.C.; Park, M.A.; Lee, L.H.; Singh, S.A.; Alcaide-Corral, C.J.; et al. (18)F-Fluoride Signal Amplification Identifies Microcalcifications Associated With Atherosclerotic Plaque Instability in Positron Emission Tomography/Computed Tomography Images. Circ. Cardiovasc. Imaging 2019, 12, e007835. [Google Scholar] [CrossRef] [PubMed]
- Waring, O.J.; Skenteris, N.T.; Biessen, E.A.L.; Donners, M. Two-faced Janus: The dual role of macrophages in atherosclerotic calcification. Cardiovasc. Res. 2022, 118, 2768–2777. [Google Scholar] [CrossRef]
- Cochain, C.; Vafadarnejad, E.; Arampatzi, P.; Pelisek, J.; Winkels, H.; Ley, K.; Wolf, D.; Saliba, A.E.; Zernecke, A. Single-Cell RNA-Seq Reveals the Transcriptional Landscape and Heterogeneity of Aortic Macrophages in Murine Atherosclerosis. Circ. Res. 2018, 122, 1661–1674. [Google Scholar] [CrossRef]
- Fu, C.; Xu, Q.; Liu, J.; Tang, S.; Liu, C.; Cao, Y. Triggering receptor expressed on myeloid cells-2 promotes survival of cardiomyocytes after myocardial ischemic injury through PI3K/AKT pathway. Cardiovasc. Diagn. Ther. 2022, 12, 24–36. [Google Scholar] [CrossRef]
- Noels, H.; Weber, C.; Koenen, R.R. Chemokines as therapeutic targets in cardiovascular disease: The road behind, the road ahead. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 583–592. [Google Scholar] [CrossRef]
| Study | Study Design | Model | Cell Types | Main Findings |
|---|---|---|---|---|
| Vafadarnejad et al. (2020) [38] | Animal research | Murine/heart after MI | Neutrophil | While circulating neutrophils undergo an aging process characterized by the loss of surface CD62 ligand and upregulation of Cxcr4, it has been shown that cardiac-infiltrating neutrophils acquire a unique SiglecFhi signature. |
| Mildner et al. (2017) [39] | Animal research | Murine monocyte isolation from blood | Monocyte | The use of scRNA-seq and transplantation experiments has confirmed that Ly-6Cint monocytes are a heterogeneous population that expresses MHCII. The differentiation of Ly-6C+ monocytes into Ly-6C- cells is regulated by the transcription factor C/EBPβ. C/EBPβ is also involved in the regulation of Nr4a1 expression during monocyte conversion. |
| Zhuang et al. (2020) [41] | Animal research | Mouse/MI surgery | Macrophage, myofibroblast | Macrophages from different origins exhibited divergent transcriptional signatures, pathways, developmental trajectories, and transcriptional regulons. Myofibroblasts predominantly expand at 7 days after myocardial infarction with pro-reparative characteristics (signature genes: Postn, Cthrc1, and Ddah1, among Ddah1). |
| Bajpai et al. (2019) [28] | Animal research | Cardiomyocytes of mouse MI model | Monocyte, macrophage | Identification of heterogeneity of macrophages in the heart after MI (1 monocyte cluster and 7 clusters of macrophages). A set of cardiac-resident CCR2+ macrophages are responsible for the recruitment of monocytes to the injured myocardium. Tissue-resident CCR2- macrophages oppose the recruitment. |
| Ni et al. (2021) [42] | Animal research | Murine models of HF (transverse aortic constriction and chronic Ang II infusion) | Cardiomyocyte, fibroblast | Cardiac macrophage heterogeneity was identified using scRNA-seq analysis, which revealed a subset of macrophages associated with heart damage. Additionally, a proinflammatory macrophage subset, identified as CD72hi cardiomyocytes, was also discovered. |
| Jung et al. (2022) [10] | Animal research | MI-induced mice | Neutrophil, monocyte, macrophage | Identification of major immune cell populations and their proportion changes after MI over time. The upregulation of Trem2 expression in macrophages was observed with trajectory inference analysis during the subacute phase of acute MI. Infarcted hearts were significantly improved by in vivo injection of soluble Trem2. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.H.; Lee, K.Y.; Chang, K. The Protective Role of TREM2 in the Heterogenous Population of Macrophages during Post-Myocardial Infarction Inflammation. Int. J. Mol. Sci. 2023, 24, 5556. https://doi.org/10.3390/ijms24065556
Kim SH, Lee KY, Chang K. The Protective Role of TREM2 in the Heterogenous Population of Macrophages during Post-Myocardial Infarction Inflammation. International Journal of Molecular Sciences. 2023; 24(6):5556. https://doi.org/10.3390/ijms24065556
Chicago/Turabian StyleKim, Sang Hyun, Kwan Yong Lee, and Kiyuk Chang. 2023. "The Protective Role of TREM2 in the Heterogenous Population of Macrophages during Post-Myocardial Infarction Inflammation" International Journal of Molecular Sciences 24, no. 6: 5556. https://doi.org/10.3390/ijms24065556
APA StyleKim, S. H., Lee, K. Y., & Chang, K. (2023). The Protective Role of TREM2 in the Heterogenous Population of Macrophages during Post-Myocardial Infarction Inflammation. International Journal of Molecular Sciences, 24(6), 5556. https://doi.org/10.3390/ijms24065556






